Abstract
Background
Although the lactational amenorrhea method (LAM) is one of the most commonly used contraception methods during the first six months of a woman’s postpartum period, there has been little research on its effectiveness in general and particularly in Ethiopia. The purpose of this study was to evaluate the effectiveness of LAM and the experiences of Ethiopian women who used it.
Methods
This was a multi-center prospective cohort study of postpartum women from five Ethiopian regions and one city administration. All pregnant women who gave birth in these randomly selected hospitals and five health centers directly referring to the hospitals were invited to the study if they selected LAM and were followed monthly at home. Each month, trained researchers visited the woman at her home and collected information about breast feeding, the return of menses, the resumption of sex, the use of another contraceptive, and a pregnancy test using urine human chorionic gonadotropin (hCG). Women who reported starting new contraceptive methods, resumption of menses, starting complementary feeding, neonatal death, getting pregnant, or refusing were excluded from the cohort. The data were collected using ODK Collect and exported to Stata 14 for analysis.
Results
Among the 2162 women who selected LAM as a contraceptive, 2022 were enrolled in the cohort study, and 901 completed the follow-up. At the end of the sixth month, eight women got pregnant, corresponding to an effectiveness of 99.1%. More than half of the cohort were excluded from the follow-up for reasons of transitioning to other types of contraception, resumption of menses, or refusal to follow-up.
Conclusion
The effectiveness of LAM is high and should be recommended for postpartum women, with proper counseling provided. A study should be conducted to examine the effectiveness of breast feeding as a contraceptive beyond the Bellagio consensus.
Keywords: effectiveness, lactation amenorrhea, contraception, breast-feeding, postpartum Ethiopia
Introduction
The lactational amenorrhea method (LAM) is a contraceptive method where the mother is informed and supported about how to use breastfeeding for contraception. Although breast feeding has been used as a natural family planning method for centuries, its scientific support came in 1988, when a group of global interdisciplinary lactational infertility experts met in Bellagio, Italy, and introduced the Bellagio Consensus on lactational infertility.1 Although not based on a systematic review, the second conference at Bellagio in 1995 confirmed the first Bellagio lactational infertility consensus that women choosing and using LAM had a six-month life table pregnancy rate of less than 2% and named it the “Bellagio consensus”, which was bolstered by the promotion of appropriate breastfeeding practices.2 According to this consensus, the Lactational Amenorrhea Method (LAM) can be effective up to 98% in the first 6 months if the women remain amenorrhoeic and exclusively breastfeed, after reviewing thirteen prospective studies in both developed and developing countries supporting the consensus.2,3 Several studies on the effectiveness of LAM have been published since this international consensus statement, known as the Bellagio Consensus.1,2,4–9
Given that LAM is being recommended as one of the modern contraceptives, there is a need to demonstrate its effectiveness as well as women’s practice in using LAM as a contraceptive. While multiple research on the efficiency of LAM have been undertaken in various settings, the majority of the known studies are old, and no study has been conducted in Ethiopia. LAM, like many other contraceptive techniques, is only effective if used correctly. Depending on whether or not LAM is administered effectively, an efficacy range of 98.3% to 100% has been observed, with decreasing efficacy after 6 months.6,7,9–11
Though the Bellagio consensus on the effectiveness of the LAM was made only up to 6 months postpartum, there are different studies recommending it beyond the Bellagio consensus up to 12 months after delivery.6,9,12
As many women are opting to use LAM,13,14 investigating its effectiveness and women’s experiences with LAM utilization is essential for designing tailored intervention and counseling.15 In this study, we report the effectiveness and women’s experiences of using LAM in a multi-center prospective study in Ethiopia.
Methods
Study Setting, Design, and Population
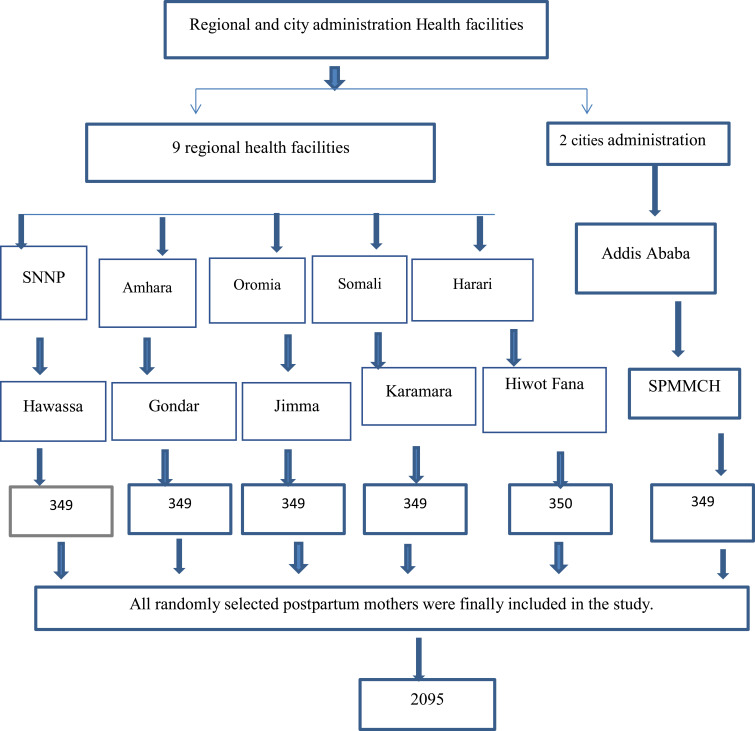
A multi-center prospective cohort study was conducted in selected referral hospitals in Ethiopia (Figure 1). All women who gave birth from March 1, 2017 to December 31, 2018 at the study site were the source population, while postpartum women in the selected hospitals who opted to use LAM as a family planning method were the study population. Accordingly, those who chose LAM were enrolled in this cohort study at the study health institution in the first seven postpartum days and followed on a monthly basis through arranged home visits, interviews, and urine HCG check-ups. Women who reported having partners who were living away for work, divorced, or widowed were excluded from the study.
Figure 1.
Sample size and sampling procedure.
Sample Size and Sampling Procedure
The sample size was calculated using the double population proportion formula on Epi-Info software under the following statistical assumptions: 95% confident level, power 80%, exposed: non-exposed = 1:1, proportion of women who became pregnant while using LAM = 0.7%, proportion of women who became pregnant while using breast feeding as contraception without fulfilling LAM criteria 2.9%,5 design effect = 1.5, nonresponse rate = 20%. Therefore, the final sample size estimated for the study was 2095.
We used a multi-center, multiple-stage sampling technique. First, from the nine national regional states and two city administrations, five regional states (Amhara, Oromia, SNNPR, Harari, Somali) and one city administration (Addis Ababa) were randomly selected. Then, from each selected region and city administration, one referral and five nearest health centers were randomly selected and included in the study (Figure 1). Finally, all women who selected LAM as a family planning option were included in the study (Figure 1).
Data Collection and Measurements
The effectiveness of LAM was the outcome of interest. Sociodemographic variables (age, religion, occupation, residence, educational status, marital status, husband education, husband occupation), obstetrics, and utilization of LAM-related information (discontinue, method switch, or sexual status, return of menses, frequency of breastfeeding, and supplementary feeding) were the independent variables. Data were collected through an interview questionnaire administered by 18 trained research assistants during a monthly visit to women’s homes. The questionnaire includes information on basic sociodemographic conditions (collected at enrollment), followed by monthly data on breast feeding conditions, sexual resumptions, menses return, and pregnancy tests using urine HCG.
Data Processing and Analysis
The data collected in ODK was exported to MS Excel and cleaned. Stata 14 was used for the analysis. Descriptive statistics were presented in the form of tables and texts. The cross-tabulation of outcome (LAM effectiveness) and follow-up time was presented.
Ethical Considerations
This study was conducted in accordance with the Declaration of Helsinki. Ethical clearance for this study was obtained from the Institutional Health Research Ethics Review Committee of the University of Gondar (Ref No: O/V/P/RCS/05/3073/2017). All the study participants gave informed consent, and confidentiality of the information was maintained. The interview was conducted in a private consultation room at discharge. According to the ethical approval we got from the University of Gondar with the above reference number, women who are less than 18 years old but married and gave birth are considered to be mature and can give assent, and additionally, informed consent was taken from the guardians.
Results
Socio-Demographic Characteristics of Participants
Of the 2095 LAM users who were approached, 2022 were enrolled in the cohort, and 901 completed the six-month follow-up. The mean age of participants was 25.8 (±4.7) years. The majority of the respondents were urban residents (92.2%) and housewives (63.9%) (Table 1).
Table 1.
Socio Demographic Characteristics of Postpartum Women in Ethiopia (n=2022)
| Variable | Frequency | Percent |
|---|---|---|
| Residence | ||
| Rural | 157 | 7.8 |
| Urban | 1865 | 92.2 |
| Age | ||
| <18yrs | 35 | 1.73 |
| 18–35yrs | 1918 | 96.59 |
| >35yrs | 69 | 3.41 |
| Maternal education | ||
| No formal education | 495 | 24.5 |
| Read and write | 82 | 4.1 |
| Primary | 438 | 21.6 |
| Secondary | 548 | 27.1 |
| College and above | 459 | 22.7 |
| Maternal occupation | ||
| Farmer | 28 | 1.38 |
| Housewife | 1291 | 63.85 |
| Government employee | 293 | 14.49 |
| Private employee | 109 | 5.39 |
| Merchant | 145 | 7.17 |
| Others | 156 | 7.72 |
| Husband occupation | ||
| Farmer | 200 | 9.9 |
| Government employee | 740 | 36.6 |
| Private | 311 | 15.4 |
| Merchant | 301 | 14.9 |
| Other | 470 | 23.2 |
| Estimated monthly income | ||
| <2500 | 586 | 29.0 |
| 2500–4999 | 873 | 43.2 |
| >5000 | 563 | 27.8 |
| Study site | ||
| Harar | 331 | 16.4 |
| Addis ababa | 348 | 17.2 |
| Jimma | 310 | 15.3 |
| Jigjiga | 356 | 17.6 |
| Gondar | 318 | 15.7 |
| Hawasa | 359 | 17.8 |
Utilization and Effectiveness of LAM
Among the 2022 women who were enrolled in the cohort, only 44.5% completed the six-month follow-up. The majority of the reasons for dropping from follow-up were stating another contraceptive (528; 26.1%), resumption of menses (432; 21.4%), and refusal (137; 6.8%). Overall, 0.9% (8/909) of the women get pregnant, corresponding with an effectiveness of 99.1% for LAM at 6th month. The percentage of women staying on follow-up ranges from 29.9% in Jigjiga to 10.2% in Jimma (Table 2 and 3).
Table 2.
Cross-Tabulation of Follow-Up Outcome and Location of Women Who Gave Birth in Selected Areas of Ethiopia
| Study Location | ||||||||
|---|---|---|---|---|---|---|---|---|
| Harar | Addis Ababa | Jima | Jigjiga | Gondar | Hawassa | Total | ||
| Follow-up outcome | Censor | 242 | 69 | 92 | 269 | 107 | 122 | 901 |
| DCC | 43 | 230 | 95 | 4 | 82 | 74 | 528 | |
| DCP | 2 | 0 | 1 | 3 | 1 | 1 | 8 | |
| DCR | 5 | 2 | 7 | 11 | 8 | 104 | 137 | |
| DCND | 0 | 0 | 5 | 0 | 7 | 0 | 12 | |
| DCS | 0 | 0 | 1 | 0 | 3 | 0 | 4 | |
| DCM | 39 | 47 | 109 | 69 | 110 | 58 | 432 | |
Abbreviations: DCC, Dropped from follow-up since she transits to another contraception type; DCP, Dropped from follow-up due to Pregnancy occurrence; DCR, Dropped from follow-up due to refusal to follow-up; DCND, Dropped from follow-up due to neonatal death; DCS, Dropped from follow-up due to separation from husband; DCM, Dropped from follow-up due to resumption of menses.
Table 3.
Cross-Tabulation of Follow-Up Outcome with Follow-Up Time for Women Who Gave Birth in Selected Areas of Ethiopia
| 1st Month | 2nd Month | 3rd Month | 4th Month | 5th Month | 6th | Total | ||
|---|---|---|---|---|---|---|---|---|
| Follow- up outcome | Censor | 0 | 0 | 0 | 0 | 0 | 0 | 901 |
| DCC | 0 | 63 | 266 | 159 | 39 | 1 | 528 | |
| DCP | 0 | 1 | 2 | 2 | 2 | 1 | 8 | |
| DCR | 0 | 49 | 61 | 26 | 1 | 0 | 137 | |
| DCND | 0 | 8 | 3 | 0 | 1 | 0 | 12 | |
| DCS | 0 | 0 | 0 | 2 | 2 | 0 | 4 | |
| DCM | 0 | 58 | 200 | 119 | 52 | 3 | 432 | |
According to this study, the majority of the women breastfed their child 7–10 (39.1%) times during the day and about 4–6 (44.6%) times during the night. Three percent of women in the cohort started supplementary feeding during follow-up and dropped out of the next follow-up (Table 4).
Table 4.
Cross-Tabulation of LAM Practice for Women Who Gave Birth in Selected Areas of Ethiopia
| Variable | Frequency | Percent |
|---|---|---|
| Frequency of breast feeding at day time | ||
| <4 | 119 | 5.9 |
| 4–6 | 690 | 34.1 |
| 7–10 | 789 | 39.1 |
| >10 | 424 | 20.9 |
| Frequency of breast feeding at night time | ||
| <4 | 778 | 38.5 |
| 4–6 | 902 | 44.6 |
| 7–10 | 219 | 10.8 |
| >10 | 123 | 6.1 |
| Longest duration of breast feeding interval | ||
| <2hr | 96 | 4.8 |
| 2–4hr | 62 | 3.1 |
| 5–7hr | 373 | 18.4 |
| 8–12hr | 822 | 40.6 |
| >12hr | 669 | 33.1 |
| Shortest duration of breast feeding interval | ||
| <1hr | 14 | 0.7 |
| 1–2hr | 276 | 13.7 |
| 3–4hr | 253 | 12.5 |
| 5–6hr | 1052 | 52.0 |
| >6hr | 427 | 21.1 |
| Started supplementary feeding | ||
| Yes | 57 | 2.98 |
| No | 1853 | 97.02 |
Discussion
In this study, we assessed the effectiveness of the lactational amenorrhea method among postpartum women over a six-month period. Of the 909 women who completed the follow-up, 8 got pregnant, corresponding to an effectiveness of 99.1%. The majority of the women dropped from follow-up were related to switching to another contraceptive method, the return of menses, and refusal to follow-up, covering more than half of the women who were in the study group at the beginning of this cohort study.
Our finding is comparable with many studies on the effectiveness of LAM, including studies from multiple countries (99.3%),5 multi-center studies of LAM (97.3–100%),7,8 Australian breast-feeding women (98.3%),12 India (100%),9 and Pakistan (99.4%).16 It has been previously reported that the LAM is highly effective in preventing 98% of subsequent pregnancies in postpartum women who appropriately breastfeed.1,16 Given that many women in Ethiopia are not using any family planning despite their intention to delay their pregnancies, appropriate counseling on LAM is essential.17,18
On the other hand, our finding is slightly higher than a report from Chile (94.8%).8 This variation might be attributed to differences in the characteristics of study participants’ working conditions. In our cohort, the majority of them reported staying at home during the first six months, whether they were working or not.8,17 Breastfeeding is affected by several factors, among which employment is one, and returning to work should be considered a risk factor in the use of LAM. Staying with an infant more likely increases the frequency and length of breast feeding, which in turn increases the effectiveness of LAM.
This is the first comprehensive, nationally representative multicenter study of the efficacy of LAM among postpartum women in general and in Ethiopia in particular. Despite its reported high efficacy, few studies have been conducted on the effectiveness of LAM recently. So, our study is the first of its kind in this regard. Although the majority of the losses to follow-up were related to the return of menses and starting new contraceptive methods, which are not directly related to the outcome of interest, only half of the cohorts were followed for the whole period.
In conclusion, we found the effectiveness of LAM for preventing pregnancy in the first six months of the postpartum period to be high. The fact that the majority of the women dropped out of follow-up is not directly related to the challenges of LAM but to starting new contraceptives, which is promising. Women selecting LAM as a contraceptive should always be informed about the basic requirements for high efficacy of LAM, which are exclusive or nearly exclusive breast feeding, no return of menses, and infant age below 6 months, so that women will be aware of the potential of pregnancy if any of these are missed. Our research assistants were, in addition, giving such advice during each visit, enabling each woman to make an informed decision. Further study on the challenges of using LAM as a contraceptive method or women’s satisfaction with their experience is essential for promoting LAM as a contraceptive. Moreover, the provider’s knowledge and counseling practice of LAM as a contraceptive should be explored.
Strength of the Study
Being the first comprehensive, nationally representative multicenter study of the efficacy of LAM among postpartum women in general and in Ethiopia in particular will make it a strong and representative study.
Limitation of the Study
The limitations of this study were the high dropout rate from the cohort, though for different reasons. The other limitation of the study was that it did not assess the effectiveness of LAM beyond the Bellagio consensus.
Conclusion
This study found that the effectiveness of correctly utilized LAM is high and can be recommended for postpartum women. As a result, proper LAM counseling should be offered, particularly for women who select LAM and do not desire other kinds of contraception. We recommend that a study be conducted to examine the effectiveness of breast feeding as a contraceptive beyond the Bellagio consensus (6 months postpartum) in Ethiopia.
Acknowledgments
We would like to thank the Center for International Reproductive Health Training (CIRHT)-Ethiopia for financial support for this study.
Funding Statement
This research was funded by Center for International Reproductive Health Training (CIRHT)-Ethiopia.
Abbreviations
LAM, Lactational Amenorrhea Method; SPMMCH, Saint Paul Millennium Medical College Hospital; SNNPR, Southern Nations, Nationalities, and Peoples’ Region; ODK, Open Data Kit; HCG, human chorionic gonadotropin.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Kennedy KI, Rivera R, McNeilly AS. Consensus statement on the use of breastfeeding as a family planning method. Contraception. 1989;39(5):477–496. doi: 10.1016/0010-7824(89)90103-0 [DOI] [PubMed] [Google Scholar]
- 2.Kennedy KI, Labbokb MH, Van Look PFA, et al. Consensus statement Lactational amenorrhea method for family planning. J Nurse Midwifery. 1996;54:54–56. [DOI] [PubMed] [Google Scholar]
- 3.Van Look P. Lactational amenorrhoea method for family planning Provides high protection from pregnancy for the first six months after delivery Health promotion in primary care changes again. Br Med J. 1996;313:3–4. [Google Scholar]
- 4.Foundation TR. The Bellagio Consensus; 2019.
- 5.Kennedy KI, Visness CM. Contraceptive efficacy of lactational amenorrhoea. Lancet. 1992;339(8787):227–230. doi: 10.1016/0140-6736(92)90018-X [DOI] [PubMed] [Google Scholar]
- 6.Labbok MH, Hight-Laukaran V, Peterson AE, Fletcher V, Von Hertzen H, Van Look PFA. Multicenter study of the Lactational Amenorrhea Method (LAM): i. Efficacy, duration, and implications for clinical application. Contraception. 1997;55(6):327–336. doi: 10.1016/S0010-7824(97)00040-1 [DOI] [PubMed] [Google Scholar]
- 7.Peterson AE, Fletcher V, Von Hertzen H, Van Look PFA, Labbok MH, Hight-Laukaran V. Multicenter study of the lactational amenorrhea method (LAM) III: effectiveness, duration, and satisfaction with reduced client – provider contact 1. Contraception. 2000;62(5):221–230. doi: 10.1016/S0010-7824(00)00171-2 [DOI] [PubMed] [Google Scholar]
- 8.Labbok MH, Pugin E, Perez A. The efficacy of the lactational amenorrhea method (LAM) among working women. Contraception. 2001;62:217–219. [DOI] [PubMed] [Google Scholar]
- 9.Tiwari K, Khanam I, Savarna N. Original Research Article. A study on effectiveness of lactational amenorrhea as a method of contraception. Int J Reprod Contracept Obstet Gynecol. 2018;7(10):3946–3950. [Google Scholar]
- 10.Van der Wijden C, Manion C. Lactational amenorrhoea method for family planning (Review). Cochrane Database Syst Rev. 2015. doi: 10.1002/14651858.CD001329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kazi A, Kennedy KI, Visness CM, Khan T. Effectiveness of the lactational amenorrhea method in Pakistan. Fertil Steril. 1995;64(4):717–723. doi: 10.1016/S0015-0282(16)57845-5 [DOI] [PubMed] [Google Scholar]
- 12.Short R, Renfree M, Shaw G, Lewis P. Contraceptive effects of extended lactational amenorrhoea: beyond the Bellagio Consensus. Lancet. 1991;337(8743):715–717. doi: 10.1016/0140-6736(91)90288-Z [DOI] [PubMed] [Google Scholar]
- 13.Khella AK, Fahim HI, Issa AH, Sokal DC, Gadalla MA. Lactational amenorrhea as a method of family planning in Egypt. Contraception. 2004;69(4):317–322. doi: 10.1016/j.contraception.2003.11.015 [DOI] [PubMed] [Google Scholar]
- 14.Romero-gutie G, De Leo ALP. Acceptance of lactational amenorrhoea for family planning after postpartum counseling. Eur J Contracept Reprod Health Care. 2006;11:297–301. doi: 10.1080/13625180600929168 [DOI] [PubMed] [Google Scholar]
- 15.Abraha TH, Teferra AS, Gelagay AA, et al. Knowledge and associated factors of lactational amenorrhea as a contraception method among postpartum women in Aksum. BMC Res Notes. 2018;11(1):1–6. doi: 10.1186/s13104-018-3754-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kennedy KI, Kennedy KI, Kazi A, Steiner M. A study of breastfeeding and the return of menses and pregnancy in Karachi, Pakistan. Contraception. 1989;40(3):365–376. doi: 10.1016/0010-7824(89)90099-1 [DOI] [PubMed] [Google Scholar]
- 17.Cleland J, Conde-agudelo A, Peterson H, Ross J, Tsui A. Family planning 2 contraception and health. Lancet. 2012;380(9837):149–156. doi: 10.1016/S0140-6736(12)60609-6 [DOI] [PubMed] [Google Scholar]
- 18.Taye EB, Mekonen DG, Debele TZ, Watanabe M, Noutoshi Y. Prevalence of post partum modern family planning utilization and associated factors among postpartum mothers in Debre Tabor. BMC Res Notes. 2019;12(1):1–7. doi: 10.1186/s13104-019-4464-0 [DOI] [PMC free article] [PubMed] [Google Scholar]