Abstract
Anemia is the most common hematologic abnormality identified in children and represents a major global health problem. A delay in diagnosis and treatment might place patients with anemia at risk for the development of rare but serious complications, including chronic and irreversible cognitive impairment. Identified risk factors contributing to the development of anemia in children include the presence of nutritional deficiencies, environmental factors, chronic comorbidities, and congenital disorders of hemoglobin or red blood cells. Pediatricians, especially those in the primary care setting, serve a particularly critical role in the identification and care of those children affected by anemia. Prompt recognition of these risk factors is crucial for developing appropriate and timely therapeutic interventions and prevention strategies.
Keywords: anemia, children, iron deficiency anemia, anemia risk factors
Introduction
Anemia is the most common hematologic abnormality identified in children and remains a major global public health problem, in both developed and developing countries. In 2019, the World Health Organization (WHO) estimated that the global prevalence of anemia in children aged 6 to 59 months was 39.8%, equivalent to 269 million children, with the highest prevalence rate (60.2%) observed in children leaving in the African region.1 Published epidemiologic data suggest that the prevalence of anemia in the United States (US) is approximately 5.6%.2 Untreated, childhood anemia has the potential to cause chronic and irreversible cognitive impairment resulting in poor school performance and decreased work capacity in adulthood, impacting the community at large.3
Anemia is defined as a reduced blood hemoglobin level or red blood cell (RBC) mass that is unable to meet the oxygen demands of peripheral tissues and organs. The laboratory threshold for defining anemia is a hemoglobin level at or below the 2.5th percentile based upon reference data from healthy children. This threshold varies across age, race, and gender and may also be influenced by environmental factors.4 Newborns present higher hemoglobin levels than older children but then they reach a physiologic nadir, known as anemia of the newborn, between 9 and 12 weeks of life. Hemoglobin levels gradually increased throughout childhood until finally leveling-off to adult ranges by adolescence. Gender differences are primarily observed after puberty. The onset of menstruation in females leads to recurrent blood loss and the increased testosterone in post-pubertal males promotes the synthesis of erythropoietin (EPO). The higher EPO synthesis contributes to the higher hemoglobin levels (usually 1 to 1.5 g/dL) observed in adult males, when compared with adult females. Population-based studies have reported lower hemoglobin levels, approximately 0.5 to 1 g/dL difference, in African Americans and Hispanics in comparison to Caucasians. Specific hemoglobin curves, taking into account a patient’s ethnicity and race, have been developed.4 Hemoglobin curves have also been developed for children living at high altitude. High altitude requires higher hemoglobin concentrations to compensate for the decreased oxygen availability. This physiological effect may cause the prevalence of anemia to be underestimated in children living at high altitude places.5,6
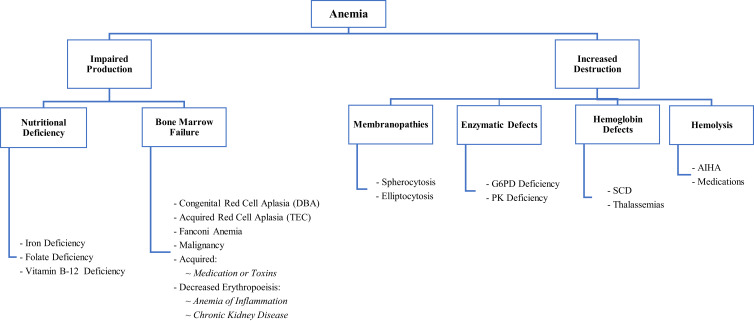
Anemia can be classified as either congenital or acquired, acute or chronic. Anemia may be secondary to either decreased RBC production or increased RBC destruction also known as hemolysis (Figure 1). Clinically, anemia is classified by the RBCs’ mean corpuscular volume (MCV): normocytic (when the MCV is within range for age), microcytic, or macrocytic. Other red cell indices as well as the reticulocyte count can help to further delineate the etiology of anemia (Table 1).
Figure 1.
Pathophysiologic classification of anemia.
Abbreviations: DBA, Diamond Blackfan Anemia; G6PD, Glucose-6-Phosphate Dehydrogenase; PK, Pyruvate Kinase; SCD, Sickle Cell Disease; AIHA, Autoimmune hemolytic anemia.
Table 1.
Red Cell Indices and Peripheral Blood Smear Findings in Children with Anemia
| MCV | RDW | MCHC | Reticulocyte Count | Peripheral Blood Smear Findings | |
|---|---|---|---|---|---|
| Nutritional Deficiencies | |||||
|
↓ | ↑ | ↓ | ↓ | Small and hypochromic RBCs, target cells |
|
↑ | ↑ | ↑ | ↓ | Hypersegmented neutrophils, macro-ovalocytes and Howell Jolly Bodies |
| Environmental Factors | |||||
|
↓/Normal | Normal | ↓ | Normal/ ↓ | Basophilic stippling |
|
Normal | Normal/ ↑ | Normal | ↓ | Toxic granulation, atypical lymphocytes or bandemia |
| Congenital Disorders | |||||
|
↑ | Normal | Normal | ↓ | Normal platelet and leukocytes |
|
↑ | Normal | Normal/ ↑ | Normal/ ↓ | Decreased platelets and leukocytes |
|
Normal | ↑ | ↑ | ↑ | Crescent shaped RBCs |
|
↓ | Normal | ↓/Normal | ↑ | Target cells, hypochromic cells, tear drop |
|
Normal | ↑ | ↑ | ↑ | Spherocytes, Howell Jolly bodies |
|
Normal | ↑ | ↑ | ↑ | Elongated, oval or elliptical- shaped RBCs |
|
Normal | ↑ | ↑ | ↑ | Heinz Bodies, schistocytes, spherocytes |
|
Normal | ↑ | ↑ | ↑ | Burr Cells |
Abbreviations: MCV, Mean Corpuscular Volume; RDW, Red Cell Distribution Width; MCHC, Mean Corpuscular Hemoglobin Concentration; G6PD, Glucose-6-Phosphate Dehydrogenase.
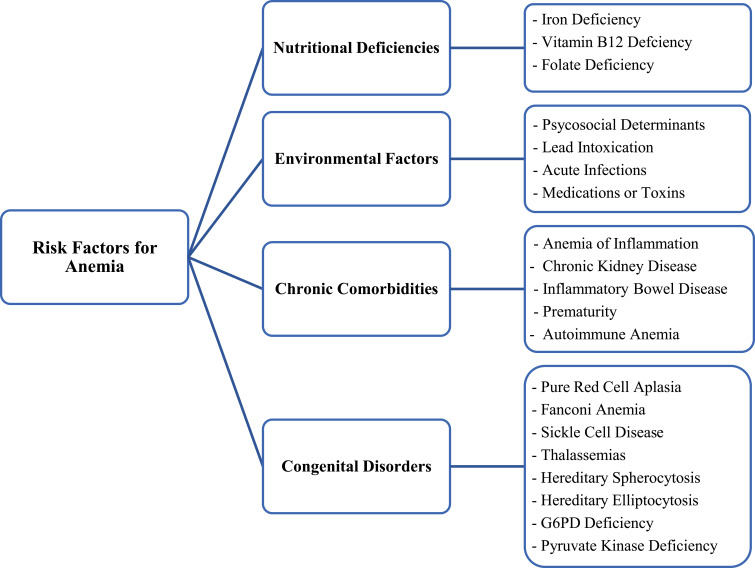
Risk factors that contribute to the development of anemia in children include the presence of nutritional deficiencies, environmental factors, chronic comorbidities, and congenital or genetic disorders of hemoglobin or RBCs (Figure 2). Proper identification and consideration of these risk factors is of utmost importance for pediatricians in order to implement adequate therapeutic interventions and to establish early and timely screening and prevention strategies.
Figure 2.
Risk factors for anemia.
Abbreviations: G6PD, Glucose-6-Phosphate Dehydrogenase.
Nutritional Deficiencies
Iron Deficiency
Iron is an integral component of hemoglobin and is also known to regulate RBC production. The ferroportin-hepcidin pathway regulates iron homeostasis. Ferroportin is a membrane-iron exporter protein on hepatocytes, duodenal enterocytes, and macrophages. Hepcidin decreases both iron gastrointestinal absorption and iron bioavailability by binding to ferroportin and inducing cellular internalization and degradation. In iron deficiency, hepcidin synthesis is decreased, resulting in an increase in both ferroportin expression and iron availability.7
Iron deficiency anemia (IDA) affects approximately 2 billion people worldwide.8 Children between 2 and 5 years of age and post-menarcheal adolescent females are the two pediatric age-groups at highest risk for developing IDA. In developed countries, the prevalence of IDA in children younger than 4 years of age is estimated to be 20.1%. This prevalence increases to 39% in developing countries. In the US, it is estimated that approximately 8% of toddlers have iron deficiency, with 1–2% of them ultimately progressing to IDA.9 The prevalence of IDA in post-menarcheal adolescent females may be as high as 15.6%.7
The most common risk factors for the development of iron deficiency in children include prematurity, nutrient-poor diet, consumption of more than 24 ounces of cow’s milk per day, and chronic blood loss.10 In infants, the introduction of cow’s milk within the first year of life is the most important dietary risk factor associated with IDA. Cow’s milk is low in iron, and even the iron within it is poorly absorbed in the GI tract. Cow’s milk also decreases the absorption of iron from other dietary sources due to its high casein and calcium content.11 Casein binds iron and prevents the free-form release necessary for absorption by the duodenal mucosa. High calcium intake is also known to inhibit the iron transporter human divalent metal transporter 1 (hDMT1) at the luminal level.12,13 Strict avoidance of cow’s milk in the first 12 months of life is essential in preventing IDA.11 World Health Organization (WHO) guidelines recommend universal iron supplementation in children whose diet does not include iron-fortified foods or for those living in high (>40%) iron-deficiency prevalence regions. For older children in a high iron deficiency prevalence region, the WHO recommends 10–12.5mg of elemental iron daily for children between 6 and 23 months of age, 30mg daily for preschool age children, and 30–60mg daily for school age children (5–12 years) daily for 3 consecutive months per year.14
Post-menarcheal adolescent females are at increased risk for IDA due to inadequate nutritional habits, rapid growth, and recurrent blood loss secondary to menstrual periods that often exceed their iron intake.15 Consumption of foods or medications that interfere with iron absorption (tea, fiber, excessive use of antacids, phosphates, and calcium) might also play a role in the development of IDA in this age group.
The clinical presentation of IDA is variable, ranging from asymptomatic to excessive fatigue, irritability, and the presence of pica. In the US, the American Academy of Pediatrics Bright Futures initiative for health promotion and prevention establishes periodic universal screening protocols for IDA in children and adolescents.16 It is also important to screen adolescent females for heavy menstrual bleeding (HMB), which is defined as excessive or prolonged menstruation for longer than 7 days or blood loss greater than 80 mL per menstrual cycle.17 There are two main causes for HMB in adolescent girls: hormonal imbalances (anovulation) and congenital bleeding disorders including von Willebrand disease (VWD), other clotting factor deficiencies (coagulation factors VII, XI, XIII, and others), and platelet function defects. Congenital bleeding disorders, primarily VWD, are found in approximately 20% to 40% of adolescent girls who present for evaluation of HMB with or without anemia and in up to 33% of adolescent girls hospitalized for HMB.18,19 Aside from VWD, congenital factor VII deficiency has also been reported to be an important cause of HMB and IDA.20 Severe iron-deficiency anemia associated with HMB may result in the need for acute hospitalizations, IV iron infusions, and packet red blood cells (PRBCs) transfusions.21
When clinically suspected, laboratory evaluation should be performed to confirm the presence of IDA. A complete blood count (CBC) will not only serve to identify anemia but can also be used for follow-up purposes. In addition to a decreased hemoglobin level associated with a decreased MCV, a decreased mean corpuscular hemoglobin (MCH) and decreased RBC count with an increased red cell distribution width (RDW) are highly suggestive of IDA. The Mentzer index, which results from dividing the MCV by the RBC count, is useful in differentiating between thalassemias (<13) and IDA (>13) when evaluating patients with microcytic anemia. An elevated platelet count and, in severe cases, decreased white blood cell count, have also been associated with IDA.
An iron profile, including serum iron, transferrin, total iron-binding capacity (TIBC), and ferritin should also be requested. Transferrin is a protein that binds and transports serum iron. Along with transferrin, the TIBC reflects the ability to transport iron. Ferritin is the protein that stores intracellular iron, and its level reflects an individual’s iron stores. While a ferritin level of 12 to 15 ng/mL has been traditionally considered the cutoff to diagnose iron deficiency, a ferritin level of <30 ng/mL is associated with a higher sensitivity and specificity (92% and 98%, respectively) for identifying people with iron deficiency, particularly for post-menarcheal females. The American Gastroenterological Association guidelines even use a cutoff of <45 ng/mL to define iron deficiency in patients with anemia.22,23 However, ferritin is an acute phase reactant and may be within normal range or even elevated in those patients with coexisting iron deficiency and inflammatory states such as acute infections.7,24 In these cases, ferritin should be repeated when the patient returns to baseline or a free-soluble transferrin receptor can be added to the diagnostic panel. The reticulocyte hemoglobin content (CHr) is another valuable tool for the diagnosis of IDA as it is a good indicator of iron availability and an early marker of iron deficient erythropoiesis.25
Iron deficiency may go underrecognized until the patient reaches severely low hemoglobin levels. This delay in diagnosis might place patients at risk for rare but serious complications including thrombosis, stroke, congestive heart failure, and even death.9,26 Iron deficiency has also been associated with long-lasting consequences on neurodevelopmental outcomes. Standard test scores of 11- to 14-year-olds who had iron deficiency as infants demonstrate poorer performance on 6 different tests, including Full-Scale IQ and Wide Range Achievement Test Arithmetic and Reading.27
Once a diagnosis of IDA is established, it is important to identify and correct the causes of the iron deficiency at the same time that iron supplementation therapy is started. Once therapy is initiated, close interval follow-up is warranted. First-line therapy for IDA includes oral ferrous iron salts. A substantial proportion of patients suffer gastrointestinal side effects (70%), such as nausea and gastroesophageal reflux, which may result in non-adherence to treatment. GI toxicity is the most common cause of nonadherence and therapy failure.28,29 Intravenous (IV) iron therapy is instituted if there is unresponsiveness to or intolerance of oral iron replacement. Intravenous iron is recognized as an appropriate first-line therapy in patients with inflammatory bowel disease, chronic kidney disease, chemotherapy-induced anemia, and those undergoing bariatric surgery. It is important to be aware that severe hypersensitivity reactions, including anaphylaxis, have been described with certain IV iron preparations. High-molecular-weight (HMW) iron dextran formulations and ferumoxytol have been associated with higher incidence of severe immediate hypersensitivity reactions. Iron sucrose, ferric gluconate, and low-molecular-weight (LMW) iron dextran have rarely been associated with any serious adverse events.30,31
Vitamin B12 and Folate Deficiencies
Vitamin B12 deficiency is rare in pediatric patients as this vitamin can be found in most animal-based foods. In the US, the incidence of nutritional vitamin B12 deficiency from 2003 to 2007 was reported to be 0.88 in 100,000 births (1 in 113,636). Another study reported that the incidence of vitamin B12 deficiency in infants was 1 in 5,355.32 Children at risk for B12 deficiency include those with severe dietary restrictions such as strict vegans or vegetarians, as well as those newborns and breast-fed infants of vitamin B12-deficient mothers. Autoimmune vitamin B12 deficiency, known as pernicious anemia, is rare in children. Excessive use of certain medications including histamine receptor agonists or proton pump inhibitors have also been associated with this deficiency.33,34
Folate is found in fresh fruits, leafy vegetables, meat, and milk. Several countries have implemented routine folic acid supplementation in grains, bread, cereal, pasta, and rice, resulting in a low prevalence of folate deficiency in children.35 Folate deficiency may still occur in those children unable to tolerate a normal diet or those severely malnourished, as well as infants exclusively drinking goat milk. Children undergoing hemodialysis and those with chronic hemolytic states (sickle cell anemia and other hemoglobinopathies) are a high-risk population for folate deficiency. It is for this reason, that these patients are routinely supplemented with folic acid and other multivitamins.36
The primary role of folate is to donate methyl groups to promote DNA synthesis. Vitamin B12 is a cofactor in the reaction that recycles 5-methyl-tetrahydrofolate back to tetrahydrofolate (THF). Lack of vitamin B12 causes folate to become trapped in the 5-methyl-THF form, which leads to methionine deficiency. With altered DNA synthesis, hematopoiesis is disrupted as the hematopoietic precursor cells are rapidly dividing cells. 37
In addition to the typical symptoms associated with anemia, the presence of neuropsychiatric manifestations (including symmetric paresthesia, numbness, and gait problems), although more common in B12 deficiency, are characteristic of both B12 and folate deficiencies. Vitamin B12 and folate deficiencies cause macrocytic anemia, defined as MCV higher than 100 fL in adults. In the pediatric population, the normal MCV cutoff values vary by age (85 fL, 86 fL, 90 fL and 96 fL for infants 6 months to 2 years of age, 2 to 6 years of age, 6 to 12 years of age, and 12 to less than 18 years of age, respectively). The CBC in these patients can also reflect mild leukopenia with the characteristic presence of hypersegmented neutrophils. An MCV higher than 115 fL is more specific to vitamin B12 or folate deficiencies than to other macrocytic conditions such as hypothyroidism or myelodysplastic syndromes.34,38,39
Patients with folate or vitamin B12 deficiency should receive appropriate supplementation in the setting of improved dietary intake. Folate deficiency with concomitant vitamin B12 deficiency should receive both supplementations. Folate treatment by itself will not improve neurological symptoms caused by vitamin B12 deficiency, which can progress to permanent damage.34,40
Environmental Factors
Psychosocial Determinants
Certain psychosocial determinants have been clearly associated with an increased risk for anemia development. Poor socioeconomic status and inadequate access to health-care services constitute important risk factors for anemia as they are linked to poor living conditions, inadequate housing infrastructure, poor nutrition, and limited access to nutritional supplements.14 Studies have shown that a child living in a household within the lowest wealth quintile is 21% more likely to develop anemia.41 Education level is another psychosocial determinant linked to anemia. Low maternal educational level may affect awareness or understanding of the importance of adequate dietary habits in children. Dietary habits can also be influenced by patient’s culture, traditions, or religious backgrounds.14
Lead Intoxication
Approximately 29 million households in the US contain lead hazards. It is estimated that 400,000 children aged 1–11 years, have blood lead levels (BLL) above 5 μg/dL, which was established by the CDC as the maximum blood lead reference value (BLRV) from 2012 to 2021. In 2021, and based on blood lead data from children aged 1–5 years old, sampled in the 2015–2018 National Health and Nutrition Examination Survey (NHANES), the CDC lowered the maximum BLRV in children to 3.5 μg/dL.42–44
Over the past 30 years, BLLs have decreased in children. Elevated BLLs disproportionately impact vulnerable groups, including immigrant children, low-income families, and young children from ethnic and racial minorities.45 Non-Hispanic Black children, living in low-income households and refugees are more likely to live in communities where lead-based paint is pervasive as the housing units were often built before 1978.44 Developmentally impaired children who have persistent pica behaviors are also at increased risk for lead toxicity.45
Most children in developed countries are exposed to lead through the ingestion of lead-contaminated dust and paint chips from interior surfaces of older houses containing deteriorating lead-based paint. Other risk factors include contaminated drinking water, imported canned food, imported candy, and ceramic pots. Iron deficiency has also been associated with an increased susceptibility to lead poisoning as children with severe IDA can present with pica-like symptoms.42,45,46
Lead poisoning does not manifest specific signs or symptoms. Nonspecific findings, such as abdominal pain, constipation, nausea, vomiting, decreased growth, delayed sexual maturation, frequent dental caries, and impaired neurologic development, can be found in those children with high basal lead levels.46 Studies in children with higher BLLs have also demonstrated lower IQ scores, language difficulties, learning disorders and behavioral issues.45
Lead is taken up by the iron absorption machinery and secondarily blocks iron through competitive inhibition. Lead interferes with a number of important iron dependent metabolic steps such as heme biosynthesis, resulting in anemia.47 Examination of blood smears can help distinguish the etiology of anemia, as one of the hallmarks of lead poisoning anemia is red blood cells with basophilic stippling.48
The CDC and the American Academy of Pediatrics (AAP) recommend targeted screening for lead poisoning in those children living in high prevalence areas, those with increased risk factors and those who were born outside of the US. The current Bright Futures/AAP Periodicity Schedule recommends risk assessment on well-child visits from 6 months to 6 years of age. An important factor in preventing lead toxicity in children is the early identification and elimination of all major sources of exposure.49–51
Acute Infections
Acute infections may lead to transient bone marrow suppression and/or hemolysis. Anemia secondary to suppression of RBCs production has been associated with several viral infections, including human parvovirus B19, human immunodeficiency virus (HIV), Epstein–Barr virus (EBV), cytomegalovirus (CMV), and hepatitis viruses. Streptococcal infections, tuberculosis, and bacterial infections causing overwhelming sepsis, have also been associated with transient bone marrow suppression. Autoimmune extrinsic hemolytic anemia has been associated with acute hepatitis infections, CMV, EBV, as well as with typhoid fever, and Escherichia coli or streptococcal infections.52
Clinical studies have shown that 60% of hospitalized febrile children with positive blood or urine cultures had anemia. In one study, 83% of children requiring hospitalization for acute management of pneumonia had hemoglobin levels below 11g/dL at admission.53 Parvovirus B19 infections are estimated to occur in 2–10% of children younger than 5 years of age and have been shown to be a significant cause of acute anemia in those patients with chronic hemolytic conditions associated with a shortened erythrocyte life span, such as sickle cell anemia. This virus selectively infects erythroid precursors, inhibiting their growth, which leads to an acute decrease in hemoglobin and reticulocytes.46,54,55
Transient erythroblastopenia of childhood (TEC), which usually occurs after an acute viral infection, has a reported incidence of 4.3 cases per 100,000 children. This condition is a rare selective RBC aplasia that can sometimes be accompanied by neutropenia and thrombocytosis. An immune-mediated mechanism is implicated in the pathophysiology of TEC, where both IgG and T-cell mediated mechanisms appear to play a role. It occurs mostly in early childhood, between 6 months and 6 years of age.56 TEC is considered self-limited, and most children require only supportive treatment. PRBC transfusions rapidly increase hemoglobin in severely ill patients.57 It is believed that the incidence of TEC could be higher than reported, as not all cases are diagnosed because of spontaneous resolution of the anemia prior to identification.
Medications or Toxins
The administration of numerous medications, including antimicrobials, chemotherapeutic agents, anticonvulsants, and immunosuppressants has been associated with transient bone marrow suppression (Table 2). Some pesticides, insecticides, and other toxic chemicals found in contaminated groundwater (arsenic, benzene) have also been associated with aplastic anemia.46,58 Other medications, such as penicillins, antimalarial medications, sulfas, or acetaminophen, can cause autoimmune hemolytic anemia (Table 2).58,59
Table 2.
Medications Associated with Development of Anemia in Children
| Transient Bone Marrow Suppression | Hemolytic Anemia | |
|---|---|---|
| Antimicrobials |
|
|
| NSAIDs and Analgesic |
|
|
| Antiepileptics |
|
-- |
| Miscellaneous |
|
|
Abbreviation: NSAIDs, nonsteroidal anti-inflammatory drugs.
Autoimmune Hemolytic Anemia
Autoimmune hemolytic anemia (AIHA) is an acquired anemia in which autoantibodies target RBCs’ membrane antigens inducing cell lysis. Based on the temperature at which these antibodies present reactivity, AIHA can be classified as either warm AIHA (wAIHA) or cold AIHA (cAIHA). AIHA may also be classified as primary or secondary, based on the presence of an underlying cause such as immunodeficiencies, autoimmune conditions, malignancy, medications, or infections.59,60 The estimated annual incidence of AIHA is approximately 0.8 per 10,000 in individuals younger than 18 years of age.61
The most common form of AIHA in children is secondary wAIHA. Most common underlying disorders linked to this type of hemolytic anemia include common variable immunodeficiency (CVID), SLE, and viral infections. Other causes include malignancies, history of previous PRBC transfusions, history of bone marrow transplantation and use of certain medications (cephalosporin and piperacillin).59
Cold AIHA, including cold agglutinin syndrome (CAS) and paroxysmal cold hemoglobinuria, is less frequent in children.61 Mycoplasma pneumoniae or EBV infections are characteristically associated with the development of CAS.61–63
Chronic Comorbidities
Many chronic diseases are associated with anemia through multiple mechanisms, including blood loss secondary to a specific disease, hemolysis, or the effects of inflammation on erythropoiesis or on iron metabolism.64
Anemia of Inflammation
The global prevalence of anemia of inflammation, also known as anemia of chronic disease, is difficult to estimate. It is often considered the most common cause of anemia after IDA. Data from the BRINDA project demonstrated that in preschool children, inflammation assessed through the measurement of C-reactive protein (CRP) is often associated with the presence of anemia.64,65
Chronic inflammatory conditions and malignancies characteristically present with elevated levels of circulating pro-inflammatory cytokines such as interleukin 6 (IL-6), transforming growth factor-β (TGF-β), tumor necrosis factor (TNF), and interferon-γ (IFN-γ). The overexpression of these inflammatory markers alters iron hemostasis as they induce hepcidin overexpression resulting in reduced iron bioavailability and erythropoiesis.66
Inflammatory states are also known to reduce the biological activity of erythropoietin (EPO), the primary hormone regulator of RBC production. This phenomenon is caused by direct EPO synthesis inhibition by TNF and interleukin-1 (IL-1) as well as reduced expression of EPO receptors on the erythroid progenitors.66–68 Managing the anemia of chronic disease focuses on improving the oxygen-carrying capacity of blood while detecting and treating the ultimate underlying cause.69
Chronic Kidney Disease
Kidneys are the primary source of EPO. Anemia, secondary to abnormal synthesis of EPO, may be observed in up to 73% of children with stage 3 chronic kidney disease (CKD) and 93% in patients with stage 4 and 5 CKD.70 The presence of anemia in children with CKD is associated with a much poorer prognosis in this population. Many other factors, including a shortened RBC life span and/or concomitant iron deficiency, contribute to the anemia observed in this population.
Hemoglobin levels below 8 g/dL in CKD patients undergoing hemodialysis are associated with significantly increased mortality when compared with patients with hemoglobin levels of 10–11g/dL.69 Routine administration of EPO-stimulating agents remains the mainstem therapy for CKD-associated anemia.
Inflammatory Bowel Disease
Anemia is the most common extra-intestinal manifestation in inflammatory bowel disease (IBD) patients and is known to adversely affect their quality of life. Patients with IBD are at risk for developing IDA with or without an associated anemia of inflammation.71
The prevalence of anemia in IBD patients is estimated to range between 44% and 74% at diagnosis and between 25% and 58% at 1-year follow-up.72 Other risk factors including low albumin levels, high CRP or ESR values, low body mass index, severe disease at presentation, and presence of extensive colitis, have been associated with the development and persistence of anemia in pediatric IBD patients.72
Prematurity
Soon after birth, newborns experience a physiological decrease in their hemoglobin levels, known as physiologic anemia of the newborn. Premature newborns are more vulnerable to this process.73 Prematures can reach a hemoglobin nadir concentration as low as 7–8 g/dL only 4–6 weeks after birth in comparison to the nadir observed in full-term newborns, which does not occur until 9–12 weeks after birth when the hemoglobin concentration only decreases to levels between 9.5 and 11 g/dL. This early-onset anemia in prematures is known as “anemia of prematurity” or AOP.74 In the US, approximately 10,000 infants are born prematurely (<36 weeks gestational age) with 6% of them classified as having extremely low birth weight (ELBW: defined as a birth weight of less than 1 kg). It is estimated that approximately 90% of these ELBW infants will require at least one PRBC transfusion due to AOP development.74,75
Anemia of prematurity is multifactorial in etiology. Physiologic factors include impaired intrauterine iron transportation, low EPO production, and a much shortened RBC life-span.74,75 Common maternal conditions such as obesity, gestational diabetes, hypertension, and placental insufficiency may also limit iron transfer from mother to fetus, contributing to the 17% prevalence of iron deficiency observed in preterm infants.74 Iatrogenic blood losses are also important contributors to the development of AOP. Premature infants are often critically ill, requiring close laboratory monitoring and frequent blood sampling.75 Other important contributing factors for AOP include inadequate nutritional intake, concomitant infections, and other non-laboratory blood losses.73
Congenital Disorders
Pure Red Cell Aplasia
Pure red cell aplasia (PRCA), defined as the presence of a normocytic normochromic anemia associated with severe reticulocytopenia and marked reduction, or absence, of erythroid precursors in the bone marrow,is a rare disorder with no definitive estimate of incidence or prevalence in the pediatric population. If other cell lines are also affected, then other diagnoses, such as aplastic anemia or Fanconi anemia, should be considered.54
Congenital PRCA, primarily represented by Diamond–Blackfan anemia (DBA), is an intrinsic erythroid hypoplasia that results from different mutations in the genes for ribosomal proteins (RPS19 and others RP genes), causing defective ribosomal RNA maturation, which leads to cell-cycle arrest and apoptosis of RBCs.54 The incidence of DBA is estimated to be five to seven cases per 1 million live births. More than 90% of cases are diagnosed by 1 year of age. Results obtained from the DBA Registry of North America show that 50% of patients are diagnosed by 3 months of age, 75% by 6 months, and 92% within the first year of life.76 No difference in gender-specific prevalence is observed.55,77
Clinically, DBA is characterized by the presence of macrocytic anemia with reticulocytopenia, often associated with different congenital anomalies, mostly localized in the cephalic area (50%) and extremities (38%) including thumb anomalies with the pathognomonic triphalangeal thumb. The urogenital tract (39%) and heart (30%) are also frequently affected. Laboratory findings in DBA patients include elevated fetal hemoglobin levels, high MCV, and elevated erythropoietin and erythrocyte adenosine deaminase (eADA) levels.78 Bone marrow studies will reveal a decrease or complete absence of erythroid precursors. The use of molecular diagnostic tools allows for the diagnosis of DBA in patients with unusual clinical presentations, such as unexplained anemia during fetal life, hydrops fetalis, or adults with persistent mild and chronic anemia. Patients with DBA have an increased cancer risk. Leukemia and solid tumor including osteogenic sarcoma, soft tissue sarcoma, lymphoma, breast, hepatocellular, gastric, and colon cancers have been reported in patients with a history of DBA.79
Treatment of DBA may include corticosteroids, chronic RBC transfusions, and, in some cases, hematopoietic stem cell transplantation. Approximately 80% of patients will initially respond to a corticosteroid-based therapy, whereas the remaining 20% will require chronic RBC transfusion therapy.79
Fanconi Anemia
Fanconi anemia (FA) is a rare autosomal recessive or X-linked disorder. It is characterized by the presence of chromosomal instability after exposure to crosslinking agents. It is the most common cause of inherited bone marrow failure. Around 15 FA genes have been identified to date. Mutations of the FANCA, FANCC, FANCD2, and FANCG genes are most common.80 The incidence of FA is estimated to be 1 in 136,000 live newborns.81 Higher incidence rates have been reported in South African and sub-Saharan black populations and Spanish Gitanos; with rates that can reach up to 1 in 40,000 live births.81–83
Up to 75% of patients with FA will present with birth defects. Findings can include short stature, structural abnormalities of the extremities (short or hypoplastic thumb, absent radii, or dysplastic ulna), and skin pigmentation (café-au-lait spots in more than 50% of patients). Less common physical exam findings include abnormal epicanthal folds, proptosis, ear anomalies (absent eardrums, atresia ear canal), GI abnormalities (imperforated anus, Meckel’s diverticulum, megacolon, and umbilical hernia). The presence of unexplained pancytopenia can be another finding in FA patients and should warrant further investigation.81
Children with FA carry a poor prognosis. Development of severe anemia is the primary cause of death in children with FA younger than 10 years of age. Concomitant pancytopenia can lead to the development of recurrent infections and excessive bleeding. Survival rates have improved in developed countries due to a reduction in mortality by bleeding or infectious complications.46,81 Treatment is variable and is based on disease severity. Hematopoietic stem cell transplant is the only curative therapeutic strategy.46
Sickle Cell Disease
Globally, 330,000 children are estimated to be born each year with an inherited hemoglobinopathy. Sickle cell disease (SCD) is the most common genetic hemoglobin disorder, and it is considered the fifth and seventh most common cause of anemia among females and males, respectively.64,84 In SCD, defects in the β-globin chain of hemoglobin cause the production of sickle-shaped RBCs that have a shortened life span. The rigid sickle cells can cause blockage of small blood vessels and damage to large blood vessels, leading to chronic hemolysis. Vasculature damage can trigger the characteristic severe pain episodes observed in patients and will ultimately cause organ damage. Children with SCD have an increased risk of infections and malnutrition.
Thalassemias
Thalassemias are a group of inherited conditions characterized by defects in the synthesis of one or more of the globin chains that constitute hemoglobin. Approximately 1.7% of the world’s population is estimated to carry either an α- or β-thalassemia trait. Alpha-thalassemia is most commonly encountered in African and Southeast Asian populations, while β-thalassemias are most often found in individuals of Mediterranean, African, and Southeast Asia descent with prevalence rates that can range between 5% and 30%. Thalassemias were estimated to be the sixth and ninth most prevalent causes of anemia globally among females and males, respectively.85
Other Congenital Red Blood Cell Abnormalities
Other congenital red cell production or metabolism abnormalities include membranopathies (hereditary spherocytosis, hereditary elliptocytosis) and enzymopathies (glucose-6-phosphate dehydrogenase deficiency, pyruvate kinase deficiency).
Hereditary spherocytosis (HS) is the most common cause of hemolytic anemia in children. This disorder is clinically, biochemically, and genetically heterogeneous. Defects in membrane and cytoskeletal proteins (ankyrin-1 band 3, β-spectrin, α-spectrin, or protein 4.2) cause the erythrocytes to be unable to maintain their physiological normal concave shape that provides morphological stability. Hereditary spherocytosis can affect all populations, although it is more common in children of Northern European and North American ancestry. Its estimated prevalence is 0.02% to 0.05% of the global population, affecting as many as 1 in every 2000 individuals. A substantial number of asymptomatic patients or those with mild symptoms may remain undiagnosed for years. It is estimated that 50% of HS patients present with mild or moderate hemolytic anemia, whereas those with severe hemolysis (10–15%) might develop additional complications including splenomegaly, hyperbilirubinemia, or jaundice.86,87 Long-term complications include potential development of pigmented gallstones. Management is centered on improving quality of life by preventing complications of chronic hemolysis. Supportive measures include the use of blood transfusions directed to maintain proper hemoglobin values, folic acid supplementation and, in some severe cases, splenectomy.86 Those individuals requiring cholecystectomy due to symptomatic gallstone disease should be evaluated for potential simultaneous splenectomy.
Hereditary elliptocytosis (HE) is characterized by the presence of elongated, oval, or elliptical-shaped RBCs on the peripheral blood smear.88 Inherited mutations in genes encoding for α-spectrin, β-spectrin, and protein 4.1 are responsible for the abnormalities on the RBC elastic recoil that result in their characteristic elliptical shape.89 These elliptocytes can become trapped and removed by the spleen resulting in hemolytic anemia. The prevalence of HE is estimated to be 1 in 2000 to 4000 children. Affected children with mild forms of HE can remain undiagnosed for years, implying that the true prevalence of this condition might be underestimated. In West Africa, HE prevalence can be as high as 1–2% of the total population.88
Since most HE patients can be asymptomatic, diagnosis is usually made incidentally during an anemia workup or after the development of an infection causing acute anemia. Neonates with HE can present with jaundice secondary to hemolytic anemia.
Most HE cases do not require treatment. Symptomatic HE patients can be managed with PRBCs transfusion and/or splenectomy. Neonates with severe jaundice may require PRBCs transfusion and/or phototherapy. Splenectomy is reserved for those patients with severe life-threatening anemia or those requiring frequent transfusions.88–90
Glucose-6-phosphate dehydrogenase (G6PD) deficiency is the most common red cell enzyme defect. It is estimated to affect approximately 400 million people worldwide. This enzyme found in the cytoplasm of RBCs helps prevent cellular damage from reactive oxygen species (ROS). Its deficiency results in the development of acute hemolytic crises during episodes of increased ROS production, which may be secondary to stress due to acute infections or exposure to certain foods (fava beans) or oxidant medications including but not limited to sulfamethoxazole, trimethoprim, dapsone, rasburicase, and methylene blue. The gene for G6PD is located on the X chromosome and is more commonly expressed in males. Heterozygous females are usually clinically unaffected.91 This disorder is more commonly found in certain ethnicities, including people of African, Mediterranean, or Asian descent. There is evidence that specific G6PD deficiency variants may have a protective role against mild malaria cases.91,92 Management can range from providing supportive care during acute hemolytic crisis and avoidance of potential offending agents. Severe cases might require blood transfusions. Neonates with G6PD deficiency are at increased risk for developing neonatal jaundice and kernicterus; in such cases, aggressive treatment is required.
Pyruvate kinase (PK) deficiency is the second most common RBC enzyme deficiency. This autosomal recessive disorder affects the RBC glycolytic pathway, due to a mutation in the PKLR gene located on chromosome 1 (1q21).93 Erythrocytes lacking PK are not able to catalyze phosphoenolpyruvate to pyruvate, which results in low adenosine triphosphate (ATP) generation and reduced reticulocyte and RBC survival. PK-deficient RBCs also have increased accumulation of 2,3-bisphosphoglycerate, which shifts the oxygen dissociation curve to the right and decreases the affinity of hemoglobin for oxygen.93,94
Pyruvate kinase deficiency manifests with enzyme levels of <25%.94 It is estimated that a PK deficiency mutation occurs in about 51 cases per million in the Caucasian population. There is an increased prevalence in certain populations such as the Amish communities in Pennsylvania in the US and Romani communities.93,94
Manifestations of PK deficiency in neonates include hyperbilirubinemia, anemia, poor suckling, lethargy, extramedullary hematopoiesis (blueberry muffin rashes), and hydrops that may develop in utero. In older children, it can be manifested as poor growth, jaundice hemolytic crisis secondary to stress, splenomegaly, and frontal bossing secondary to extramedullary hematopoiesis.94 Diagnostic molecular testing (direct DNA sequencing) is increasingly being utilized as this can be performed in transfused patients. This can be used for prenatal diagnosis and is less complicated in terms of preparation and shipping of sample than direct enzyme assay.95
Supportive therapy is important in management, including folic acid supplementation, transfusions to ameliorate anemia, iron chelation if necessary and splenectomy in the setting of massive splenomegaly.94 Disease modifying therapies been investigated include stem cell transplant and gene therapy.96
Conclusion
Anemia remains a significant burden for the pediatric population. The differential diagnosis of anemia is extensive. An understanding of hematopoiesis as well as the prevalence and risk factors that contribute to the development of anemia allows the clinician to assess for underlying nutritional deficiencies, predisposing enviromental factors, chronic disease states, and congenital red cell or hemoglobin disorders. With the prompt recognition of anemia through laboratory evaluation, expeditious and appropriate therapeutic interventions can be initiated. Pediatricians, especially those in the primary care setting, invariably play a critical role in the identification of anemia and the care of affected children.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.World Health Organization. Anaemia in Women and Children. Geneva: World Health Organization. WHO Global Anaemia estimates; 2021. [Google Scholar]
- 2.Le CH, Collins JF. The prevalence of anemia and moderate-severe anemia in the US population (NHANES 2003–2012). PLoS One. 2016;11(11):e0166635. doi: 10.1371/journal.pone.0166635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aliyo A, Jibril A. Anemia and associated factors among under five year old children who attended Bule Hora general hospital in West Guji zone, Southern Ethiopia. J Blood Med. 2022;13:395–406. doi: 10.2147/jbm.S363876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carlo Brugnara FAO, David G. Nathan diagnostic approach to anemic patient. In: Nathan and Oski’s Hematology and Oncology of Infancy and Childhood. 8th ed. WB Saunders; 2015:293. [Google Scholar]
- 5.Ocas-Córdova S, Tapia V, Gonzales GF. Hemoglobin concentration in children at different altitudes in Peru: proposal for [Hb] correction for altitude to diagnose anemia and polycythemia. High Alt Med Biol. 2018;19(4):398–403. doi: 10.1089/ham.2018.0032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity. World Health Organization; 2011. [Google Scholar]
- 7.Zanetti R, Feldman B, Porea T. Microcytic anemia. Pediatr Rev. 2021;42(1):41–43. doi: 10.1542/pir.2019-0295 [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization (WHO). Worldwide Prevalence of Anaemia 1993–2005. World Health Organization; 2008. [Google Scholar]
- 9.McEvoy MT, Stuckert AJ, Castellanos MI, et al. Management of nutritional iron deficiency anemia for young children in the emergency department. Pediatr Blood Cancer. 2023;70(3):e30181. doi: 10.1002/pbc.30181 [DOI] [PubMed] [Google Scholar]
- 10.Janus J, Moerschel SK. Evaluation of anemia in children. Am Fam Physician. 2010;81(12):1462–1471. [PubMed] [Google Scholar]
- 11.Kazal LA Jr. Prevention of iron deficiency in infants and toddlers. Am Fam Physician. 2002;66(7):1217–1224. [PubMed] [Google Scholar]
- 12.Kibangou IB, Bouhallab S, Henry G, et al. Milk proteins and iron absorption: contrasting effects of different caseinophosphopeptides. Pediatr Res. 2005;58(4):731–734. doi: 10.1203/01.PDR.0000180555.27710.46 [DOI] [PubMed] [Google Scholar]
- 13.Scheers N. Regulatory effects of Cu, Zn, and Ca on Fe absorption: the intricate play between nutrient transporters. Nutrients. 2013;5(3):957–970. doi: 10.3390/nu5030957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization. Nutritional Anaemias: Tools for Effective Prevention and Control. Geneva: World Health Organization; 2017. [Google Scholar]
- 15.Camaschella C. Iron-deficiency anemia. N Engl J Med. 2015;372(19):1832–1843. doi: 10.1056/NEJMra1401038 [DOI] [PubMed] [Google Scholar]
- 16.American Academy of Pediatrics. Bright Futures Guidelines for Health Supervision of Infants, Children, and Adolescents. American Academy of Pediatrics; 2017. [Google Scholar]
- 17.Haamid F, Sass AE, Dietrich JE. Heavy menstrual bleeding in adolescents. J Pediatr Adolesc Gynecol. 2017;30(3):335–340. doi: 10.1016/j.jpag.2017.01.002 [DOI] [PubMed] [Google Scholar]
- 18.Philipp CS, Faiz A, Heit JA, et al. Evaluation of a screening tool for bleeding disorders in a US multisite cohort of women with menorrhagia. Am J Obstet Gynecol. 2011;204(3):209.e1–7. doi: 10.1016/j.ajog.2010.10.897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cendan MD. Screening and management of bleeding disorders in adolescents with heavy menstrual bleeding: ACOG COMMITTEE OPINION SUMMARY, number 785. Obstet Gynecol. 2019;134(3):658–659. doi: 10.1097/AOG.0000000000003412 [DOI] [PubMed] [Google Scholar]
- 20.Trillo A, Kronenfeld R, Simms-Cendan J, Davis JA, Corrales-Medina FF. High prevalence of congenital factor VII (FVII) deficiency in adolescent females with heavy menstrual bleeding and iron deficiency anemia. J Pediatr Adolesc Gynecol. 2022;35(6):647–652. doi: 10.1016/j.jpag.2022.07.013 [DOI] [PubMed] [Google Scholar]
- 21.Cooke AG, McCavit TL, Buchanan GR, Powers JM. Iron deficiency anemia in adolescents who present with heavy menstrual bleeding. J Pediatr Adolesc Gynecol. 2017;30(2):247–250. doi: 10.1016/j.jpag.2016.10.010 [DOI] [PubMed] [Google Scholar]
- 22.Short MW, Domagalski JE. Iron deficiency anemia: evaluation and management. Am Fam Physician. 2013;87(2):98–104. [PubMed] [Google Scholar]
- 23.Ko CW, Siddique SM, Patel A, et al. AGA clinical practice guidelines on the gastrointestinal evaluation of iron deficiency anemia. Gastroenterology. 2020;159(3):1085–1094. doi: 10.1053/j.gastro.2020.06.046 [DOI] [PubMed] [Google Scholar]
- 24.Richardson M. Microcytic anemia. Pediatr Rev. 2007;28(1):5–14. doi: 10.1542/pir.28-1-5 [DOI] [PubMed] [Google Scholar]
- 25.Gelaw Y, Woldu B, Melku M. The role of reticulocyte hemoglobin content for diagnosis of iron deficiency and iron deficiency anemia, and monitoring of iron therapy: a literature review. Clin Lab. 2019;65(12). doi: 10.7754/Clin.Lab.2019.190315 [DOI] [PubMed] [Google Scholar]
- 26.Corrales-Medina FF, Grant L, Egas-Bejar D, Valdivia-Ascuna Z, Rodriguez N, Mancias P. Cerebral sinovenous thrombosis associated with iron deficiency anemia secondary to severe menorrhagia: a case report. J Child Neurol. 2014;29(9):Np62–4. doi: 10.1177/0883073813500715 [DOI] [PubMed] [Google Scholar]
- 27.Lozoff B, Jimenez E, Hagen J, Mollen E, Wolf AW. Poorer behavioral and developmental outcome more than 10 years after treatment for iron deficiency in infancy. Pediatrics. 2000;105(4):E51. doi: 10.1542/peds.105.4.e51 [DOI] [PubMed] [Google Scholar]
- 28.Tolkien Z, Stecher L, Mander AP, Pereira DI, Powell JJ, Strnad P. Ferrous sulfate supplementation causes significant gastrointestinal side-effects in adults: a systematic review and meta-analysis. PLoS One. 2015;10(2):e0117383. doi: 10.1371/journal.pone.0117383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Auerbach M, Gafter-Gvili A, Macdougall IC. Intravenous iron: a framework for changing the management of iron deficiency. Lancet Haematol. 2020;7(4):e342–e350. doi: 10.1016/s2352-3026(19)30264-9 [DOI] [PubMed] [Google Scholar]
- 30.Ning S, Zeller MP. Management of iron deficiency. Hematology. 2019;2019(1):315–322. doi: 10.1182/hematology.2019000034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Caimmi S, Crisafulli G, Franceschini F, et al. Hypersensitivity to intravenous iron preparations. Children. 2022;9(10):1473. doi: 10.3390/children9101473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mütze U, Walter M, Keller M, et al. Health outcomes of infants with vitamin B(12) deficiency identified by newborn screening and early treated. J Pediatr. 2021;235:42–48. doi: 10.1016/j.jpeds.2021.02.009 [DOI] [PubMed] [Google Scholar]
- 33.Staff NP, Windebank AJ. Peripheral neuropathy due to vitamin deficiency, toxins, and medications. Continuum. 2014;20(5):1293–1306. doi: 10.1212/01.CON.0000455880.06675.5a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ankar A, Kumar A. Vitamin B12 deficiency. In: StatPearls. StatPearls Publishing Copyright © 2023, StatPearls Publishing LLC; 2023. [Google Scholar]
- 35.Administration USFaD. Food standards: amendment of standards of identity for enriched grain products to require addition of folic acid. Fed Regist. 1996;61:8781–8797. [Google Scholar]
- 36.Harshman LA, Lee-Son K, Jetton JG. Vitamin and trace element deficiencies in the pediatric dialysis patient. Pediatr Nephrol. 2018;33(7):1133–1143. doi: 10.1007/s00467-017-3751-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hariz A, Bhattacharya PT. Megaloblastic anemia. In: StatPearls. StatPearls Publishing Copyright © 2022 StatPearls Publishing LLC; 2022. [Google Scholar]
- 38.Aslinia F, Mazza JJ, Yale SH. Megaloblastic anemia and other causes of macrocytosis. Clin Med Res. 2006;4(3):236–241. doi: 10.3121/cmr.4.3.236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Socha DS, DeSouza SI, Flagg A, Sekeres M, Rogers HJ. Severe megaloblastic anemia: vitamin deficiency and other causes. Cleve Clin J Med. 2020;87(3):153–164. doi: 10.3949/ccjm.87a.19072 [DOI] [PubMed] [Google Scholar]
- 40.Khan KM, Jialal I. Folic acid deficiency. In: StatPearls. StatPearls Publishing Copyright © 2023 StatPearls Publishing LLC; 2023. [PubMed] [Google Scholar]
- 41.Balarajan Y, Ramakrishnan U, Özaltin E, Shankar AH, Subramanian SV. Anaemia in low-income and middle-income countries. Lancet. 2011;378(9809):2123–2135. doi: 10.1016/S0140-6736(10)62304-5 [DOI] [PubMed] [Google Scholar]
- 42.Egan KB, Dignam T, Brown MJ, Bayleyegn T, Blanton C. Using small area prevalence survey methods to conduct blood lead assessments among children. Int J Environ Res Public Health. 2022;19(10):6151. doi: 10.3390/ijerph19106151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.CDC. Centers for Disease Control and Prevention. Lead in paint; 2023.
- 44.Ruckart PZ, Jones RL, Courtney JG, et al. Update of the blood lead reference value - United States, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(43):1509–1512. doi: 10.15585/mmwr.mm7043a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hauptman M, Bruccoleri R, Woolf AD. An update on childhood lead poisoning. Clin Pediatr Emerg Med. 2017;18(3):181–192. doi: 10.1016/j.cpem.2017.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gallagher PG. Anemia in the pediatric patient. Blood. 2022;140(6):571–593. doi: 10.1182/blood.2020006479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hegazy AA, Zaher MM, Abd El-Hafez MA, Morsy AA, Saleh RA. Relation between anemia and blood levels of lead, copper, zinc and iron among children. BMC Res Notes. 2010;3(1):133. doi: 10.1186/1756-0500-3-133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Knollmann-Ritschel BEC, Markowitz M. Lead poisoning. Acad Pathol. 2017;4:2374289517700160. doi: 10.1177/2374289517700160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lanphear BP, Lowry JA, Ahdoot S, et al.; HEALTH COE. Prevention of childhood lead toxicity. Pediatrics. 2016;138(1):e20161493. [DOI] [PubMed] [Google Scholar]
- 50.PEHSU. Recommendations on management of childhood lead exposure: a resource for clinicians. Pediatric Environmental Health Specialty Units. Available from: https://www.pehsu.net/_Library/facts/PEHSU_Fact_Sheet_Lead_Management_Health_Professionals_9_2021.pdf. Accessed February 28, 2023. [Google Scholar]
- 51.AAP. Detection of lead poisoning; 2021. American Academy of Pediatrics. Available from: https://www.aap.org/en/patient-care/lead-exposure/detection-of-lead-poisoning/. Accessed February 28, 2023. [Google Scholar]
- 52.Fish JDL, Jeffrey M. Philip Extracorpuscular Hemolytic Anemia. Lanzkowsky’s Manual of Pediatric Hematology and Oncology. Elsevier Science & Technology; 2021. [Google Scholar]
- 53.Ballin A, Lotan A, Serour F, et al. Anemia of acute infection in hospitalized children-no evidence of hemolysis. J Pediatr Hematol Oncol. 2009;31(10):750–752. doi: 10.1097/MPH.0b013e3181b79696 [DOI] [PubMed] [Google Scholar]
- 54.Means RT Jr. Pure red cell aplasia. Hematology Am Soc Hematol Educ Program. 2016;2016(1):51–56. doi: 10.1182/asheducation-2016.1.51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mangla A, Hamad H. Pure Red Cell Aplasia. StatPearls Publishing Copyright © 2022 StatPearls Publishing LLC; 2022. [PubMed] [Google Scholar]
- 56.Donato UM Jr, Galligan A. A case report on transient erythroblastopenia of childhood in a female pediatric patient. Cureus. 2022;14(6):e26451. doi: 10.7759/cureus.26451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.van den Akker M, Dror Y, Odame I. Transient erythroblastopenia of childhood is an underdiagnosed and self-limiting disease. Acta Paediatr. 2014;103(7):e288–94. doi: 10.1111/apa.12634 [DOI] [PubMed] [Google Scholar]
- 58.Garratty G. Drug-induced immune hemolytic anemia. Hematology Am Soc Hematol Educ Program. 2009;2009(1):73–79. doi: 10.1182/asheducation-2009.1.73 [DOI] [PubMed] [Google Scholar]
- 59.Voulgaridou A, Kalfa TA. Autoimmune hemolytic anemia in the pediatric setting. J Clin Med. 2021;10(2):216. doi: 10.3390/jcm10020216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hill QA, Hill A, Berentsen S. Defining autoimmune hemolytic anemia: a systematic review of the terminology used for diagnosis and treatment. Blood Adv. 2019;3(12):1897–1906. doi: 10.1182/bloodadvances.2019000036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Aladjidi N, Jutand MA, Beaubois C, et al. Reliable assessment of the incidence of childhood autoimmune hemolytic anemia. Pediatr Blood Cancer. 2017;64(12):e26683–n/a. doi: 10.1002/pbc.26683 [DOI] [PubMed] [Google Scholar]
- 62.Terada K, Tanaka H, Mori R, Kataoka N, Uchikawa M. Hemolytic anemia associated with cold agglutinin during chicken pox and a review of the literature. J Pediatr Hematol Oncol. 1998;20(2):149–151. doi: 10.1097/00043426-199803000-00012 [DOI] [PubMed] [Google Scholar]
- 63.Singh A, Mandal A, Patel A, Mishra S. Autoimmune haemolytic anaemia-a spectrum of presentation in children. J Clin Diagn Res. 2017;11(9):Sr01–sr02. doi: 10.7860/jcdr/2017/27895.10646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chaparro CM, Suchdev PS. Anemia epidemiology, pathophysiology, and etiology in low- and middle-income countries. Ann N Y Acad Sci. 2019;1450(1):15–31. doi: 10.1111/nyas.14092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Suchdev PS, Namaste SM, Aaron GJ, Raiten DJ, Brown KH, Flores-Ayala R. Overview of the Biomarkers Reflecting Inflammation and Nutritional Determinants of Anemia (BRINDA) Project. Adv Nutr. 2016;7(2):349–356. doi: 10.3945/an.115.010215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zivot A, Lipton JM, Narla A, Blanc L. Erythropoiesis: insights into pathophysiology and treatments in 2017. Mol Med. 2018;24(1):11. doi: 10.1186/s10020-018-0011-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Irwin JJ, Kirchner JT. Anemia in children. Am Fam Physician. 2001;64(8):1379–1386. [PubMed] [Google Scholar]
- 68.Panjeta M, Tahirović I, Sofić E, Ćorić J, Dervišević A. Interpretation of erythropoietin and haemoglobin levels in patients with various stages of chronic kidney disease. J Med Biochem. 2017;36(2):145–152. doi: 10.1515/jomb-2017-0014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Madu AJ, Ughasoro MD. Anaemia of chronic disease: an in-depth review. Med Princ Pract. 2017;26(1):1–9. doi: 10.1159/000452104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Atkinson MA, Martz K, Warady BA, Neu AM. Risk for anemia in pediatric chronic kidney disease patients: a report of NAPRTCS. Pediatr Nephrolo. 2010;25(9):1699–1706. doi: 10.1007/s00467-010-1538-6 [DOI] [PubMed] [Google Scholar]
- 71.Aljomah G, Baker SS, Schmidt K, et al. Anemia in pediatric inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2018;67(3):351–355. doi: 10.1097/mpg.0000000000002002 [DOI] [PubMed] [Google Scholar]
- 72.Goyal A, Zheng Y, Albenberg LG, et al. Anemia in children with inflammatory bowel disease: a position paper by the IBD committee of the North American Society of Pediatric Gastroenterology, Hepatology and Nutrition. J Pediatr Gastroenterol Nutr. 2020;71(4):563–582. doi: 10.1097/mpg.0000000000002885 [DOI] [PubMed] [Google Scholar]
- 73.Widness JA. Pathophysiology of anemia during the neonatal period, including anemia of prematurity. Neoreviews. 2008;9(11):e520. doi: 10.1542/neo.9-11-e520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cibulskis CC, Maheshwari A, Rao R, Mathur AM. Anemia of prematurity: how low is too low? J Perinatol. 2021;41(6):1244–1257. doi: 10.1038/s41372-021-00992-0 [DOI] [PubMed] [Google Scholar]
- 75.Strauss RG. Anaemia of prematurity: pathophysiology and treatment. Blood Rev. 2010;24(6):221–225. doi: 10.1016/j.blre.2010.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Vlachos A, Klein GW, Lipton JM. The diamond Blackfan anemia registry: tool for investigating the epidemiology and biology of diamond-Blackfan anemia. J Pediatr Hematol Oncol. 2001;23(6):377–382. doi: 10.1097/00043426-200108000-00015 [DOI] [PubMed] [Google Scholar]
- 77.Da Costa L, Narla A, Mohandas N. An update on the pathogenesis and diagnosis of diamond-Blackfan anemia. F1000Res. 2018;7:1350. doi: 10.12688/f1000research.15542.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Gadhiya K, Wills C. Diamond Blackfan Anemia. In: StatPearls. StatPearls Publishing Copyright © 2023, StatPearls Publishing LLC; 2023. [PubMed] [Google Scholar]
- 79.Vlachos A, Muir E. How I treat Diamond-Blackfan Anemia. Blood. 2010;116(19):3715–3723. doi: 10.1182/blood-2010-02-251090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Soulier J. Fanconi anemia. Hematology Am Soc Hematol Educ Program. 2011;2011(1):492–497. doi: 10.1182/asheducation-2011.1.492 [DOI] [PubMed] [Google Scholar]
- 81.Bhandari JTP, Puckett Y. Fanconi anemia. Stat Pearls. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559133/. Accessed February 26, 2023. [Google Scholar]
- 82.Tipping AJ, Pearson T, Morgan NV, et al. Molecular and genealogical evidence for a founder effect in Fanconi anemia families of the Afrikaner population of South Africa. Proc Natl Acad Sci U S A. 2001;98(10):5734–5739. doi: 10.1073/pnas.091402398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Svahn J, Dufour C. Fanconi anemia - learning from children. Pediatr Rep. 2011;3(Suppl 2):e8. doi: 10.4081/pr.2011.s2.e8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Modell B, Darlison M. Global epidemiology of haemoglobin disorders and derived service indicators. Bull World Health Organ. 2008;86(6):480–487. doi: 10.2471/blt.06.036673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Muncie HL Jr, Campbell J. Alpha and beta thalassemia. Am Fam Physician. 2009;80(4):339–344. [PubMed] [Google Scholar]
- 86.Zamora EA, Schaefer CA. Hereditary spherocytosis. In: StatPearls. StatPearls Publishing Copyright © 2023, StatPearls Publishing LLC; 2023. [PubMed] [Google Scholar]
- 87.Ciepiela O. Old and new insights into the diagnosis of hereditary spherocytosis. Ann Transl Med. 2018;6(17):339. doi: 10.21037/atm.2018.07.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Jha SK, Vaqar S. Hereditary elliptocytosis. In: StatPearls. StatPearls Publishing Copyright © 2023, StatPearls Publishing LLC; 2023. [PubMed] [Google Scholar]
- 89.Mohandas N. Inherited hemolytic anemia: a possessive beginner’s guide. Hematology Am Soc Hematol Educ Program. 2018;2018(1):377–381. doi: 10.1182/asheducation-2018.1.377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Andolfo I, Russo R, Gambale A, Iolascon A. New insights on hereditary erythrocyte membrane defects. Haematologica. 2016;101(11):1284–1294. doi: 10.3324/haematol.2016.142463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Richardson SR, O’Malley GF. Glucose 6 phosphate dehydrogenase deficiency. In: StatPearls. StatPearls Publishing Copyright © 2023, StatPearls Publishing LLC; 2023. [PubMed] [Google Scholar]
- 92.Uyoga S, Macharia AW, Ndila CM, et al. Glucose-6-phosphate dehydrogenase deficiency and susceptibility to childhood diseases in Kilifi, Kenya. Blood Adv. 2020;4(23):5942–5950. doi: 10.1182/bloodadvances.2020003015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Chonat S, Eber SW, Holzhauer S, et al. Pyruvate kinase deficiency in children. Pediatr Blood Cancer. 2021;68(9):e29148. doi: 10.1002/pbc.29148 [DOI] [PubMed] [Google Scholar]
- 94.Enegela OA, Anjum F. Pyruvate kinase deficiency. In: StatPearls. StatPearls Publishing Copyright © 2023, StatPearls Publishing LLC; 2023. [PubMed] [Google Scholar]
- 95.Gallagher PG, Glader B. Diagnosis of pyruvate kinase deficiency. Pediatr Blood Cancer. 2016;63(5):771–772. doi: 10.1002/pbc.25922 [DOI] [PubMed] [Google Scholar]
- 96.Johnson S, Grace RF, Despotovic JM. Diagnosis, monitoring, and management of pyruvate kinase deficiency in children. Pediatr Blood Cancer. 2022;69(8):e29696. doi: 10.1002/pbc.29696 [DOI] [PubMed] [Google Scholar]