Abstract
The number of breast implant removal procedures are rising. Among the reasons why patients seek breast implant removal, the autoimmune/inflammatory syndrome induced by adjuvants (ASIA), also named breast implant illness, is increasingly common. ASIA is an entity that incorporates diverse autoimmune conditions induced by the exposure to various adjuvants, including silicone, and it is characterized by systemic symptoms reminiscent of autoimmune disorders. Implant removal has the most effective treatment for ASIA. We describe a technique for glandular cone reconstruction after complete capsulectomy and implant removal. It combines an inverted-T superomedial pedicled mastopexy with fat grafting of the breast quadrants and of the inferior dermoglandular flap in two patients affected by ASIA. Implant removal allowed symptom resolution in both patients at 10 and 12 months follow-up. Both patients were satisfied with the aesthetic outcome after implant removal in terms of breast softness, projection, and volume. Our technique is easy, reproducible, and allowed for restoration of breast contour, volume, and shape after implant removal. Although initially conceived in patients with ASIA, this technique can be used for patients seeking implant removal for any indication.
Takeaways
Question: Is there a surgical technique that enables maximizing the breast volume in patients seeking breast implant removal?
Findings: The glandular cone can be reconstructed using an inverted-T mastopexy associated with fat grafting not only to the breast quadrants but also to the inferior dermoglandular flap used as an auto-prosthesis.
Meaning: The inferior dermoglandular flap represents an “extra compartment,” and is able to receive extra adipose tissue in addition to breast quadrants, enhancing the final breast volume and projection, without the use of any foreign body. This technique is easily reproducible and allowed for achievement of good aesthetic outcomes.
INTRODUCTION
Nowadays, a large number of women are asking for implant removal without replacement after breast augmentation, a 47% increase in 2021 compared with 2020.1 Among the reasons for explantation, the autoimmune/inflammatory syndrome induced by adjuvants (ASIA) is increasingly common.2,3
ASIA, also known as breast implant illness or silicone implant incompatibility syndrome,4 is an entity that incorporates diverse autoimmune conditions induced by various adjuvants, including silicone.5 Silicone implants have been suggested to trigger systemic symptoms such as chronic fatigue, musculoskeletal pain, morning stiffness, dry eyes, hypersensitivity/rash, and cognitive impairment.5–7 Notably, increased levels of interleukin (IL)-17A, IL-13, and IL-22 were recently found in sera of ASIA patients compared with nonsymptomatic women.8 Implant removal has been reported as the most effective treatment for ASIA.9–15 We describe a novel technique for glandular cone reconstruction, combining inverted-T mastopexy and fat grafting in two ASIA patients, but applicable to any case of implant removal.
IDEA
Patients signed a written informed consent according to the principles of the Declaration of Helsinki. Preoperative markings of a standard keyhole pattern mastopexy based on the superomedial pedicle are performed.
Patients underwent general anesthesia with infiltration of the donor area with a solution of 1 L of saline (0.9% NaCl) with epinephrine 1 mg and lidocaine 1 g. Fat harvesting is carried out with a 2-mm cell-friendly triport cannula (Tulip Medical, USA) connected to a 20 mL Luer-lock syringe. Lipoaspirate is decantated for 30 minutes; purified fat is grafted using a 1-mm blunt monoport cannula (Bontempi, Bmed S.r.l., Rimini, Italy) connected to a Luer-lock 10-mL syringe.
The mammary skin is de-epithelized according to the keyhole pattern, preserving the subdermal vascular plexus. The dermis is incised until the capsule is identified. Total capsulectomy is performed, removing the implant and the capsule en bloc if possible. Afterward, the inferior dermoglandular flap (IDGF) is harvested and undermined until the inframammary fold.16–19 After checking its viability, the IDGF is fat grafted and used as an “auto-prothesis” to increase volume and projection. (See Video [online], which shows fat grafting to the inferior dermoglandular flap before its inset as an auto-prosthesis.)
Video 1. shows fat grafting to the inferior dermo-glandular flap before its inset as “auto-prosthesis.”.
The parenchyma is reconstructed with 3-0 Vicryl by fixing the IDGF upward and approximating the medial and lateral glandular pillars. A suction drain is placed. Additional fat grafting is performed in all breast quadrants. Adhesive dressings and a compressive bandage are applied. Drains are removed according to drain output.
Case 1
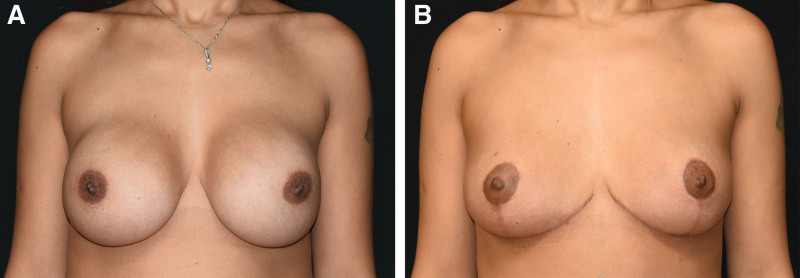
A 36-year-old woman presented to our attention complaining of chronic conjunctivitis, fatigue, and arthralgias. Her personal history included allergic asthma but was negative for any autoimmune disorder. She underwent bilateral breast augmentation 12 years before using 325-mL implants (Fig. 1A). Symptoms appeared 8 years after implant placement. Bilateral mammogram and ultrasound excluded any oncologic suspicion or fluid collection. Implants were removed with total bilateral capsulectomy. In total, 250 mL of fat was grafted in each breast. Of them, 40 mL was grafted into the IDGF. Histology of the capsule was normal. Implants were intact. One month after surgery, symptoms were remarkably reduced. At the 10-month follow-up visit, complete regression of the symptoms was reported (Fig. 1B).
Fig. 1.
Case 1. A, Preoperative photograph. B, Postoperative result after inverted-T mastopexy combined with fat grafting of the inferior dermoglandular flap and breast quadrants.
Case 2
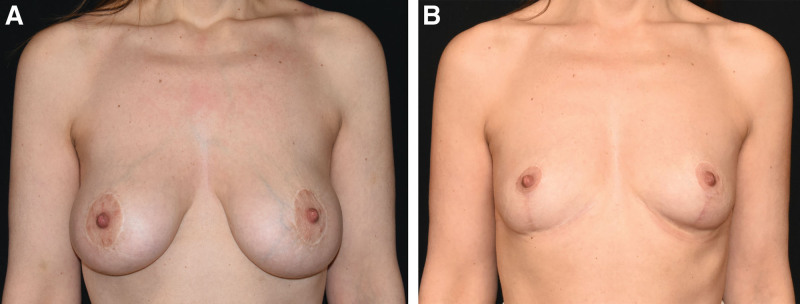
A 39-year-old woman with nephrotic syndrome, arthralgias, chronic fatigue, and depression presented to our attention. She had undergone bilateral breast augmentation 1 year before using 295-mL Mentor anatomical-shaped textured implants (Fig. 2A). A steroid-resistant nephrotic syndrome with persistent proteinuria occurred a week after implantation. Preoperative mammograms and ultrasound did not show any abnormality or fluid collection. Implants were intact. Histology was normal. A total of 160 mL of fat was grafted in the right breast and 120 mL in the left breast, to correct a mild preexisting asymmetry. Of them, 35 mL was grafted in each IDGF. Gradual improvement of symptoms and kidney function was observed after implant removal at 1 month follow-up. At 12-month follow-up, complete symptom regression was reported (Fig. 2B). Both patients were satisfied with the aesthetic outcome in terms of breast softness, projection, and volume. Breast shape, position, and volume were restored.
Fig. 2.
Case 2. A, Preoperative photograph. B, Postoperative result after inverted-T mastopexy combined with fat grafting of the inferior dermoglandular flap and breast quadrants.
DISCUSSION
One-step glandular reconstruction with fat grafting of the IDGF is not limited to ASIA patients and can be used in any case of implant removal. It is useful for women seeking implant removal and breast reconstruction without the use of foreign material, but still looking for satisfactory breast volume and projection.
The presented technique is easy to perform and reproducible, and it was able to effectively re-shape and maximize breast volume without the use of foreign material. The IDGF represents an “extra compartment” and is able to receive extra adipose tissue in addition to all breast quadrants, enhancing the breast final volume and projection. Fat grafting also allows for the correction of isolated local defects that may result after explantation.
Careful evaluation of the IDGF is mandatory to avoid liponecrosis: intraoperative assessment of dermal bleeding after de-epithelization, as well as its trimming at the more distal and less-perfused region, allows the surgeon to have information about its viability and perfusion. Well-perfused IDGF can be safely grafted.
This technique has some limitations. The final breast volume depends on the amount of individual adipose tissue availability, and very thin patients may not benefit from this procedure. Second, the thickness of the remaining glandular tissue after implant removal affects fat grafting. Grafting in all quadrants of the breast is limited in case of very thin parenchyma. The thickness of the IDGF itself affects the ability to accommodate adipose tissue and its intake; therefore, excessive grafting of the IDGF should be avoided to prevent liponecrosis.
Finally, very ptotic breasts may represent a relative contraindication for superomedial pedicled mastopexy itself, regardless of its association with fat grafting of the IDGF. However, we believe this scenario could be overcome by undercorrecting the new nipple areolar position. The main weaknesses of our study are represented by the small sample and the lack of fat retention assessment by preoperative and postoperative magnetic resonance imaging.
CONCLUSIONS
In selected patients, inverted-T superomedial mastopexy combined with fat grafting of the IDGF provides favorable cosmetic results in women requiring implant removal. It is an easy and reproducible procedure; however, accurate surgical planning and technique are mandatory to achieve satisfactory outcomes.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Footnotes
Published online 8 September 2023.
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.The Aesthetic Society. Aesthetic Plastic Surgery National Data Bank statistics 2020–2021. Available at https://cdn.theaestheticsociety.org/media/statistics/2021-TheAestheticSocietyStatistics.pdf. Published April 10, 2022. Accessed April 15, 2023.
- 2.Katsnelson JY, Spaniol JR, Buinewicz JC, et al. Outcomes of implant removal and capsulectomy for breast implant illness in 248 patients. Plast Reconstr Surg Glob Open. 2021;9:e3813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tian WM, Rames JD, Blau JA, et al. Contextualizing breast implant removal patterns with google trends: big data applications in surgical demand. Plast Reconstr Surg Glob Open. 2022;10:e4005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cohen Tervaert JW, Mohazab N, Redmond D, et al. Breast implant illness: scientific evidence of its existence. Expert Rev Clin Immunol. 2022;18:15–29. [DOI] [PubMed] [Google Scholar]
- 5.Shoenfeld Y, Agmon-Levin N. “ASIA”—autoimmune/inflammatory syndrome induced by adjuvants. J Autoimmun. 2011;36:4–8. [DOI] [PubMed] [Google Scholar]
- 6.Taskindoust M, Bowman T, Thomas SM, et al. The patient narrative for breast implant illness: a 10-year review of the U.S. Food and Drug Administration’s MAUDE database. Plast Reconstr Surg. 2022;150:1181–1187. [DOI] [PubMed] [Google Scholar]
- 7.Atiyeh B, Emsieh S. Breast implant illness (BII): real syndrome or a social media phenomenon? A narrative review of the literature. Aesthetic Plast Surg. 2022;46:43–57. [DOI] [PubMed] [Google Scholar]
- 8.McGuire P, Glicksman C, Wixtrom R, et al. Microbes, histology, blood analysis, enterotoxins, and cytokines: findings from the ASERF systemic symptoms in women-biospecimen analysis study: part 3. Aesthet Surg J. 2023;43:230–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fuzzard SK, Teixeira R, Zinn R. A review of the literature on the management of silicone implant incompatibility syndrome. Aesthetic Plast Surg. 2019;43:1145–1149. [DOI] [PubMed] [Google Scholar]
- 10.Maijers MC, de Blok CJM, Niessen FB, et al. Women with silicone breast implants and unexplained systemic symptoms: a descriptive cohort study. Neth J Med. 2013;71:534–540. [PubMed] [Google Scholar]
- 11.Rohrich RJ, Kenkel JM, Adams WP, et al. A prospective analysis of patients undergoing silicone breast implant explantation. Plast Reconstr Surg. 2000;105:2529–2537; discussion 2538–2543. [DOI] [PubMed] [Google Scholar]
- 12.Cohen Tervaert JW, Kappel RM. Silicone implant incompatibility syndrome (SIIS): a frequent cause of ASIA (Shoenfeld’s syndrome). Immunol Res. 2013;56:293–298. [DOI] [PubMed] [Google Scholar]
- 13.Bird GR, Niessen FB. The effect of explantation on systemic disease symptoms and quality of life in patients with breast implant illness: a prospective cohort study. Sci Rep. 2022;12:21073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Glicksman C, McGuire P, Kadin M, et al. Impact of capsulectomy type on post-explantation systemic symptom improvement: findings from the ASERF systemic symptoms in women-biospecimen analysis study: part 1. Aesthet Surg J. 2022;42:809–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rohrich RJ, Bellamy JL, Alleyne B. Assessing long-term outcomes in breast implant illness: the missing link? A systematic review. Plast Reconstr Surg. 2022;149:638e–645e. [DOI] [PubMed] [Google Scholar]
- 16.Hönig JF, Frey HP, Hasse FM, et al. Inferior pedicle autoaugmentation mastopexy after breast implant removal. Aesthetic Plast Surg. 2010;34:447–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ribeiro L. A new technique for reduction mammaplasty. Plast Reconstr Surg. 1975;55:330–334. [PubMed] [Google Scholar]
- 18.Avashia YJ, Rohrich RJ, Gabriel A, et al. Surgical management of the explant patient: an update on options for breast contouring and volume restoration. Plast Reconstr Surg. 2020;146:978–985. [DOI] [PubMed] [Google Scholar]
- 19.Manahan MA. Adjunctive procedures and informed consent with breast implant explantation. Plast Reconstr Surg. 2021;147:51S–57S. [DOI] [PubMed] [Google Scholar]