Abstract
Introduction:
We develop a framework to model disease progression across Alzheimer’s disease (AD) and to assess the cost-effectiveness of future disease-modifying therapies (DMTs) for people with mild cognitive impairment (MCI) due to AD.
Methods:
Using data from the US National Alzheimer’s Coordinating Center, we apply survival analysis to estimate transition from predementia to AD dementia and ordered probit regression to estimate transitions across AD dementia stages. We investigate the cost-effectiveness of a hypothetical treatment scenario for people in MCI due to AD.
Results:
We present an open-access model-based decision-analytic framework. Assuming a modest DMT treatment effect in MCI, we predict extended life expectancy and a reduction in time with AD dementia.
Discussion:
Any future DMT for AD is expected to pose significant economic challenges across all health-care systems, and decision-analytic modeling will be required to assess costs and outcomes. Further developments are needed to inform these health policy considerations.
Keywords: Alzheimer’s disease, Dementia, Mild cognitive impairment, Decision-analytic modeling, Progression, Prediction, Health policy, Cost-effectiveness analysis
1. Introduction
The importance of the problems posed by Alzheimer’s disease (AD) are well documented [1,2]. AD results in significant loss of health and well-being for individuals affected by the disease, their families and carers, and a growing economic burden for those affected and for health-care systems and society more broadly [3]. While significant scientific developments have further informed our understanding of AD (e.g., study by Hardy and Selkoe [4], Guerrerio et al. [5]), treatment options are limited, and we do not have a disease-modifying therapy (DMT). There have been a series of disappointing reports in late-stage clinical trials of treatments to slow or stop progression of AD dementia [6,7], but recently, we have also had reports of encouraging clinical-trial findings where the focus for research on DMTs has moved from AD dementia to the predementia stages of the disease (e.g., study by Haeberlein et al. [8]). Such findings have given rise to a cautious optimism that a DMT may become available for AD in the next few years [9].
A change in focus for therapeutic developments to earlier stages of disease broadens the scope and likely time frame for treatment. Against this setting, any future DMT for the predementia stage of AD is expected to pose significant economic challenges across all health-care systems [10–12], and this lends greater weight to the importance of research on the health policy context and the economic framework associated with evaluation of the impact of AD on people’s lives and the potential impacts of future DMTs.
In most health-care systems, it will be important to assess the effectiveness and cost-effectiveness of any DMT for AD over the longer term, beyond the initial trial time horizon. Any such assessment will need to extrapolate from an intermediate trial endpoint to predict impacts on longer term policy relevant outcomes using a model-based evaluative framework. In recent years, we have seen a growth in the literature on the methods available to model the progression of AD and dementia and the cost-effectiveness of interventions [13,14]. The literature has been characterized as comprising relatively simple models, commonly considering only cognitive function, and with a range of limitations [13,15]. There have been numerous studies modeling from predementia stages of AD into and across AD dementia stages [16–21]. Yet, there remains a reliance on the use of cognitive function as the main driver in the assessment of the impacts of AD and the effectiveness and cost-effectiveness of intervention strategies, and a disappointing lack of transparency on data and methods used to model disease progression across AD and the cost-effectiveness of interventions [13].
The aim in this study is to develop a decision-analytic model able to estimate the cost-effectiveness of treatment in the predementia stage of AD and to inform a health policy decision-making context in a clear and transparent way. In the following section, we present the initial development of a model-based framework to address this aim and an example of how it can be used to estimate the cost-effectiveness of a future DMT in AD.
2. Methods
2.1. Model overview
We develop an evaluative framework that models AD progression from a predementia state into AD dementia and over time through stages of dementia (see Fig. 1). Model development is based on prior research (e.g., study by Green and Zhang [22]), a strong understanding of the existing methods and literature in this area [13,15,23,24], clinical input, and consultation across a wide range of stakeholders (e.g., via International Conference on Pharmacoeconomics of Alzheimer’s disease [25,26]).
Fig. 1.
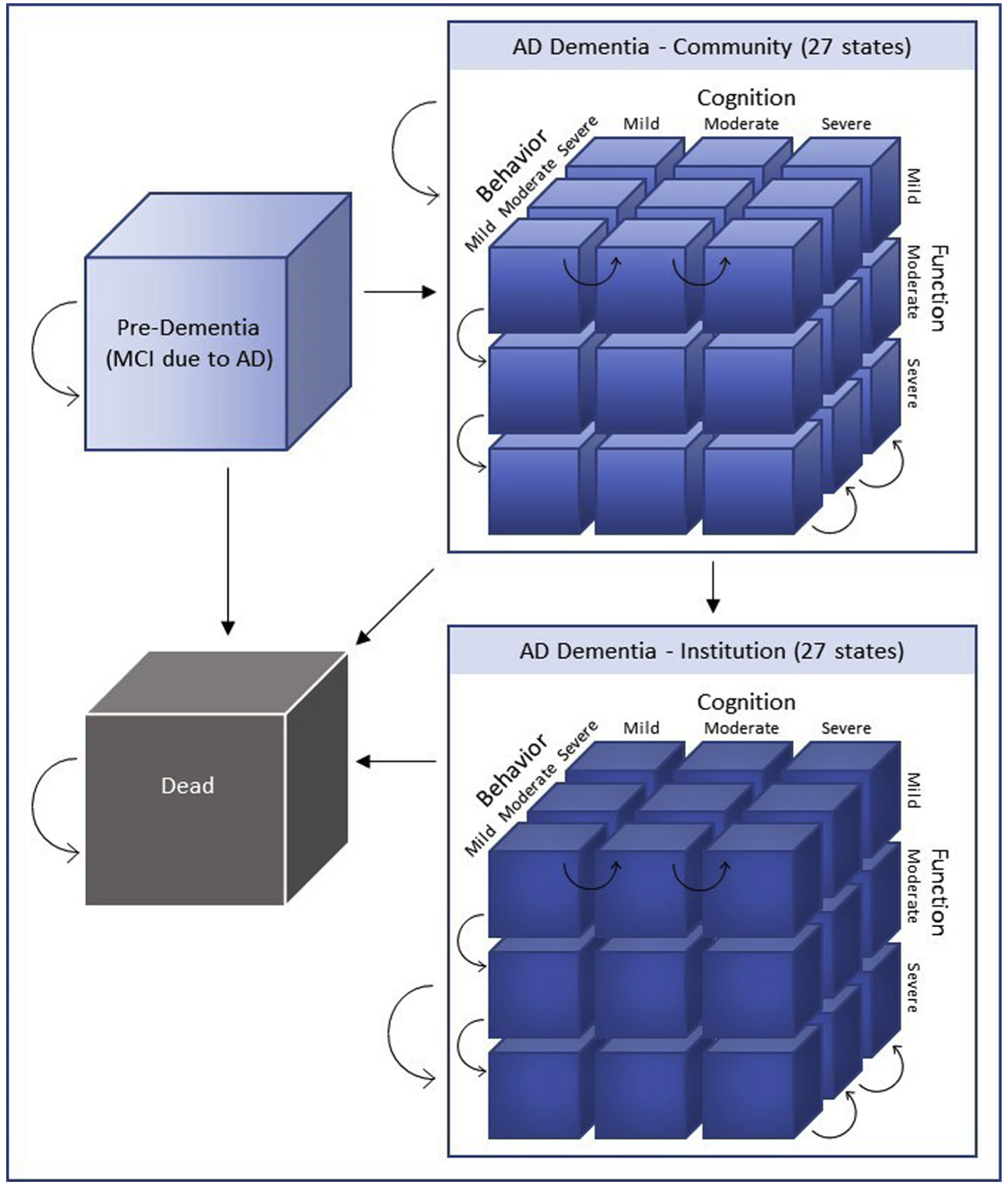
Schematic for AD model of disease progression. Abbreviations: MCI, mild cognitive impairment; AD, Alzheimer’s disease.
A key aim was to develop a model that is easily transferable to a policy context. Therefore, the model applies the Markov type framework commonly reported and used in a decision-making setting. Consistent with the policy context that motivates the research, the model is set out using a cohort approach, modeling a specified group of people across AD over time. The model uses a 1-year cycle length, with half-cycle correction, over a 20-year time horizon that reflects a lifetime perspective. We model progression from predementia to AD dementia, using mild cognitive impairment (MCI) due to AD [27] as the predementia state of interest. In the first stage of the model, we predict progression (number of participants each year) from the state “MCI due to AD” to the dementia stage of AD. We use dementia health states that capture significant changes in one or more of the multiple symptom domains of cognitive function, behavior and mood, and functional impairment. The model includes a risk of moving from a community-based dementia state to requiring nursing home care. We model mortality risk at each time point, dependent on both age and severity profiles. While relatively simple, the modeling approach using these structural assumptions allows characterization of AD progression, which is relatively slow moving with significant change in symptoms typically considered clinically over 6–12 monthly assessments. The model is used in this study to represent disease progression and to predict estimated costs and outcomes over time in a decision-analytic context, to demonstrate the use of the model-based evaluative framework in a health policy decision-making setting. In the following section, we describe the main components of the model and the methods used and illustrate the model in a health technology assessment context.
2.2. Data
To describe progression through AD, we use data (starting September 2005 up to data extraction at 31 January 2017) from the Uniform Data Set (UDS) from the US National Alzheimer’s Coordinating Center (NACC) [28,29]. The UDS contains data from more than approximately 30 past and present US Alzheimer’s Disease Centers (ADCs) on demographic, clinical, and biological characteristics from participants with clinical diagnoses of normal cognition, MCI, and dementia of various etiologies, including AD. All ADCs enroll and follow participants annually (approximately) and provide pooled data for research through the NACC. Diagnoses are assigned using clinical protocols [30]. All analyses were undertaken using STATA version 15.1.
2.3. Predementia to dementia
We selected data from NACC on participants aged 60–89 years with an MCI diagnosis, where AD was reported to be the primary or contributing cause of cognitive impairment. Participants were included where data were available on at least two assessments with the first having a diagnosis of MCI due to AD, with participants having that diagnosis either at entry to the database or at a later assessment (i.e., participants known to the database before diagnosis of MCI due to AD). Participants were included if not living in an assisted environment or institution. We identified data on 3553 participants (see summary details in Table 1), of which 1418 experienced a diagnosis of AD dementia over time. Mean (median) time to diagnosis of AD dementia was 2.7 years (2.1 years), with maximum follow-up time at 10.4 years. Using parametric survival analysis methods, we derived the rate (hazard function) of conversion from predementia to AD dementia diagnosis over time in the cohort. The resulting Weibull hazard distribution, with constant −1.53 (confidence interval: −1.61, −1.46) and shape parameter 0.76 (confidence interval: 0.71, 0.81), was used to estimate the annual proportion of participants converting from MCI due to AD to AD dementia. We estimate a conversion rate of 19% over the first 12 months, 14% during year 2, reducing to rates of 8–9% per year in later years (see detail in Supplementary Information, S1). As a secondary analysis, we estimated rates of conversion using age as a covariate, across 5-year age bands, with findings showing small differences by age-band but not markedly different from the aggregate estimates (see detail in Supplementary Information, S1).
Table 1.
Characteristics of data/sample used from NACC for data analyses (predementia, AD dementia, and AD dementia community dwelling)
| Item | Predementia (MCI due to AD)* n = 3553 | AD Dementia† n = 4423 | AD dementia Community‡ n = 4839 |
|---|---|---|---|
| Age, mean (SD) | 76 (7.2) | 77 (7.4) | 76 (7.3) |
| Female gender, n (%) | 1816 (51) | 2336 (53) | 2527 (52) |
| Education (years), mean (SD) | 16 (3.3) | 15 (6.6) | 14 (3.7) |
| Married, n (%) | 2299 (65) | 3058 (69) | 3402 (70) |
| Living alone, n (%) | 968 (27) | 613 (14) | 691 (14) |
| Diagnosed (MCI*/AD dementia†) at entry to NACC, n (%) | 1905 (54) | 3593 (81) | 3871 (80) |
| Etiology: | |||
| AD primary, n (%) | 3338 (94) | 4258 (96) | 4561 (94) |
| AD contributing, n (%) | 215 (6) | 165 (4) | 278 (6) |
Abbreviations: NACC, National Alzheimer’s Coordinating Center (USA); AD, Alzheimer’s disease; MCI, mild cognitive impairment.
Mild cognitive impairment due to Alzheimer’s disease.
Alzheimer’s disease dementia.
Community dwelling with data between baseline and follow-up, selection criteria less stringent than data used for transitions between AD dementia states.
2.4. AD dementia
A multidomain descriptive system is used to describe health states for AD dementia, capturing the three primary symptom domains; cognitive function, behavior and mood, and functional impairment. We use the Mini-Mental State Examination (MMSE) [31], neuropsychiatric inventory questionnaire (NPI-Q) [32], and the Functional Activities Questionnaire (FAQ) [33] as measures for cognitive function, behavior and mood, and functional impairment. The descriptive system has been described in detail elsewhere [22]. A simple categorical approach is used to place impairments on each of the domains into one of three severity levels, covering no or mild problems, moderate problems, or severe problems (see Table 2), consistent with the typical interpretation of the rating scales used to assess symptomatic problems in AD dementia [22]. The descriptive system used to model progression through AD dementia places people into one of 27 mutually exclusive health states, see Table 2.
Table 2.
Descriptive system for AD: Definition by level of severity for each symptom domain
| Domain | Severity level | Label | Definition |
|---|---|---|---|
| Cognitive function | Mild | [1] | 21 ≤ MMSE ≤ 26 |
| Moderate | [2] | 10 ≤ MMSE ≤20 | |
| Severe | [3] | 0 ≤ MMSE ≤ 9 | |
| Behavior & mood | No problem/mild | [1] | NPI-Q: each item ≤ 1 |
| Moderate | [2] | NPI-Q: each item ≤ 2; with at least one item equal to 2 | |
| Severe | [3] | NPI-Q: at least one item equal to 3 | |
| Functional ability | No problem/mild | [1] | 0 ≤ FAQ total ≤ 8 |
| Moderate | [2] | 9 ≤ FAQ total ≤ 23 | |
| Severe | [3] | 24 ≤ FAQ total ≤ 30 |
Abbreviations: AD, Alzheimer’s disease; MMSE, Mini-Mental State Examination; NPI-Q, neuropsychiatric inventory questionnaire; FAQ, Functional Assessment Questionnaire.
AD dementia progression is modeled as transitions between the described states over time, using a 1-year time cycle. To estimate transitions between the AD dementia health states, we use data available from the NACC UDS on participants with a diagnosis of AD dementia, an MMSE score of 26 or less, and continuous data collected over time on at least two consecutive assessments. We included participants aged 60–89 years with a diagnosis of dementia with AD as the primary or contributing cause on entry to the dataset and also those that were known to ADCs before having this diagnosis. We identified 4423 participants that met inclusion criteria with complete data (see Table 1).
Aligned to the descriptive system used in this study, we use ordered probit regression methods [34] to estimate transitions between health states (over 1-year time period). Participants are described using the categorical ordered levels for each of the three symptom domains and assigned to one of the 27 mutually exclusive health state descriptions, and we predict the future (next time period) health state based on the current health state description. In the ordered probit regression, a latent variable determines the predicted level for each symptom domain, either level 1, 2, or 3, and is based on the health state description across each of the three domains, cognition, behavior/mood, and function, in the preceding time period (see equation 1).
| (1) |
Where P is probability of being in state i (level 1–3) for each of y outcomes (domains for cognitive function, behavior, and function) conditional on description/status in prior time period (xj), where κ reflects cut-points from the ordered probit, β reflects the vector of coefficients for explanatory variables (symptom domains by level/severity), ϕ reflects the cumulative normal distribution, for individual j.
Three probit regression equations are used, one for each of the symptom domains (cognition, behavior/mood, and function), and these are combined (see equation 2) to predict the probability of transitions across the health state descriptive system.
| (2) |
Where probability (P) of being in multidomain state i (i = states1–27) is a product of being in each of the levels by symptom domain (i-n = level1–3); see detail in Supplementary Information, S2.
We derive a transition matrix (27 × 27) across the multidomain descriptive system for AD dementia (see Table 3) and use the predicted transition probabilities to model progression over time in AD dementia. As people transition from MCI to AD dementia, their starting (landing) state in the dementia descriptive system is determined using the empirical distribution observed in the NACC data for people converting to dementia. The empirical distribution of landing states, from those converting to dementia with complete multidomain symptom data (n = 760), locates 71% of AD dementia diagnoses in mild starting states (i.e., states 111, 112, 121, and 122), with the remainder in moderate severity states, see Supplementary Detail (S2). We assume all new diagnoses of AD dementia are in a community (noninstitutional) setting.
Table 3.
Transition probability matrix for AD dementia states* (derived using ordered probit regression methods)
| To State: | COG | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | 3 | |
| BEHAV | 1 | 2 | 3 | 1 | 2 | 3 | 1 | 2 | 3 | 1 | 2 | 3 | 1 | 2 | 3 | 1 | 2 | 3 | 1 | 2 | 3 | 1 | 2 | 3 | 1 | 2 | 3 | ||
| FUNC | 1 | 1 | 1 | 2 | 2 | 2 | 3 | 3 | 3 | 1 | 1 | 1 | 2 | 2 | 2 | 3 | 3 | 3 | 1 | 1 | 1 | 2 | 2 | 2 | 3 | 3 | 3 | ||
| From State: | |||||||||||||||||||||||||||||
| COG | BEHAV | FUNC | |||||||||||||||||||||||||||
| 1 | 1 | 1 | 0.22 | 0.06 | 0.01 | 0.35 | 0.10 | 0.02 | 0.02 | 0.00 | 0.00 | 0.06 | 0.02 | 0.00 | 0.10 | 0.03 | 0.01 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 1 | 2 | 1 | 0.12 | 0.09 | 0.03 | 0.25 | 0.18 | 0.07 | 0.02 | 0.01 | 0.00 | 0.04 | 0.03 | 0.01 | 0.07 | 0.05 | 0.02 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 1 | 3 | 1 | 0.07 | 0.09 | 0.06 | 0.16 | 0.21 | 0.14 | 0.01 | 0.02 | 0.01 | 0.02 | 0.03 | 0.02 | 0.04 | 0.06 | 0.04 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 1 | 1 | 2 | 0.02 | 0.01 | 0.00 | 0.29 | 0.12 | 0.03 | 0.12 | 0.05 | 0.01 | 0.01 | 0.00 | 0.00 | 0.15 | 0.06 | 0.02 | 0.06 | 0.03 | 0.01 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 1 | 2 | 2 | 0.01 | 0.01 | 0.00 | 0.17 | 0.16 | 0.08 | 0.09 | 0.09 | 0.04 | 0.01 | 0.01 | 0.00 | 0.09 | 0.08 | 0.04 | 0.05 | 0.05 | 0.02 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 1 | 3 | 2 | 0.00 | 0.01 | 0.01 | 0.09 | 0.16 | 0.15 | 0.06 | 0.10 | 0.09 | 0.00 | 0.00 | 0.00 | 0.05 | 0.08 | 0.07 | 0.03 | 0.05 | 0.04 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 1 | 1 | 3 | 0.00 | 0.00 | 0.00 | 0.05 | 0.03 | 0.01 | 0.24 | 0.12 | 0.04 | 0.00 | 0.00 | 0.00 | 0.05 | 0.03 | 0.01 | 0.23 | 0.12 | 0.04 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.01 | 0.00 |
| 1 | 2 | 3 | 0.00 | 0.00 | 0.00 | 0.02 | 0.03 | 0.02 | 0.14 | 0.17 | 0.10 | 0.00 | 0.00 | 0.00 | 0.03 | 0.03 | 0.02 | 0.14 | 0.17 | 0.11 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.01 | 0.01 |
| 1 | 3 | 3 | 0.00 | 0.00 | 0.00 | 0.01 | 0.03 | 0.03 | 0.08 | 0.17 | 0.19 | 0.00 | 0.00 | 0.00 | 0.01 | 0.02 | 0.03 | 0.07 | 0.16 | 0.18 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.01 |
| 2 | 1 | 1 | 0.04 | 0.01 | 0.00 | 0.13 | 0.04 | 0.01 | 0.02 | 0.01 | 0.00 | 0.10 | 0.03 | 0.01 | 0.33 | 0.11 | 0.02 | 0.04 | 0.01 | 0.00 | 0.01 | 0.00 | 0.00 | 0.04 | 0.01 | 0.00 | 0.01 | 0.00 | 0.00 |
| 2 | 2 | 1 | 0.02 | 0.02 | 0.01 | 0.09 | 0.07 | 0.03 | 0.01 | 0.01 | 0.00 | 0.05 | 0.04 | 0.02 | 0.22 | 0.18 | 0.08 | 0.03 | 0.03 | 0.01 | 0.01 | 0.01 | 0.00 | 0.03 | 0.02 | 0.01 | 0.00 | 0.00 | 0.00 |
| 2 | 3 | 1 | 0.01 | 0.02 | 0.01 | 0.06 | 0.08 | 0.06 | 0.01 | 0.01 | 0.01 | 0.03 | 0.04 | 0.03 | 0.13 | 0.19 | 0.15 | 0.02 | 0.03 | 0.02 | 0.00 | 0.00 | 0.00 | 0.02 | 0.02 | 0.02 | 0.00 | 0.00 | 0.00 |
| 2 | 1 | 2 | 0.00 | 0.00 | 0.00 | 0.05 | 0.02 | 0.01 | 0.05 | 0.02 | 0.01 | 0.01 | 0.00 | 0.00 | 0.22 | 0.10 | 0.03 | 0.20 | 0.09 | 0.03 | 0.00 | 0.00 | 0.00 | 0.05 | 0.02 | 0.01 | 0.05 | 0.02 | 0.01 |
| 2 | 2 | 2 | 0.00 | 0.00 | 0.00 | 0.03 | 0.03 | 0.02 | 0.03 | 0.03 | 0.02 | 0.00 | 0.00 | 0.00 | 0.12 | 0.13 | 0.07 | 0.13 | 0.15 | 0.08 | 0.00 | 0.00 | 0.00 | 0.03 | 0.03 | 0.02 | 0.03 | 0.03 | 0.02 |
| 2 | 3 | 2 | 0.00 | 0.00 | 0.00 | 0.01 | 0.03 | 0.03 | 0.02 | 0.04 | 0.04 | 0.00 | 0.00 | 0.00 | 0.06 | 0.12 | 0.12 | 0.08 | 0.15 | 0.16 | 0.00 | 0.00 | 0.00 | 0.01 | 0.03 | 0.03 | 0.02 | 0.03 | 0.03 |
| 2 | 1 | 3 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.04 | 0.02 | 0.01 | 0.00 | 0.00 | 0.00 | 0.03 | 0.02 | 0.01 | 0.32 | 0.20 | 0.07 | 0.00 | 0.00 | 0.00 | 0.01 | 0.01 | 0.00 | 0.14 | 0.09 | 0.03 |
| 2 | 2 | 3 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.02 | 0.03 | 0.02 | 0.00 | 0.00 | 0.00 | 0.01 | 0.02 | 0.01 | 0.18 | 0.24 | 0.17 | 0.00 | 0.00 | 0.00 | 0.01 | 0.01 | 0.01 | 0.08 | 0.11 | 0.08 |
| 2 | 3 | 3 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.03 | 0.04 | 0.00 | 0.00 | 0.00 | 0.01 | 0.01 | 0.02 | 0.09 | 0.23 | 0.29 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.01 | 0.04 | 0.09 | 0.12 |
| 3 | 1 | 1 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.00 | 0.00 | 0.08 | 0.03 | 0.01 | 0.03 | 0.01 | 0.00 | 0.03 | 0.01 | 0.00 | 0.37 | 0.15 | 0.04 | 0.14 | 0.06 | 0.01 |
| 3 | 2 | 1 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.05 | 0.04 | 0.02 | 0.02 | 0.02 | 0.01 | 0.02 | 0.01 | 0.01 | 0.22 | 0.21 | 0.11 | 0.10 | 0.10 | 0.05 |
| 3 | 3 | 1 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.03 | 0.05 | 0.04 | 0.01 | 0.02 | 0.02 | 0.01 | 0.01 | 0.01 | 0.12 | 0.21 | 0.19 | 0.06 | 0.11 | 0.10 |
| 3 | 1 | 2 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.01 | 0.00 | 0.04 | 0.02 | 0.01 | 0.00 | 0.00 | 0.00 | 0.13 | 0.08 | 0.02 | 0.38 | 0.22 | 0.07 |
| 3 | 2 | 2 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.01 | 0.01 | 0.02 | 0.03 | 0.02 | 0.00 | 0.00 | 0.00 | 0.06 | 0.08 | 0.05 | 0.23 | 0.29 | 0.20 |
| 3 | 3 | 2 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.01 | 0.01 | 0.03 | 0.04 | 0.00 | 0.00 | 0.00 | 0.03 | 0.06 | 0.08 | 0.12 | 0.27 | 0.34 |
| 3 | 1 | 3 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.02 | 0.02 | 0.01 | 0.00 | 0.00 | 0.00 | 0.01 | 0.01 | 0.00 | 0.46 | 0.34 | 0.14 |
| 3 | 2 | 3 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.02 | 0.01 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.24 | 0.39 | 0.32 |
| 3 | 3 | 3 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.01 | 0.02 | 0.02 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.11 | 0.32 | 0.51 |
Abbreviations: COG, cognitive function, level 1–3 (using MMSE categories); BEHAV, behavior/mood, level 1–3 (using NPI-Q categories); FUNC, function, level 1–3 (using FAQ categories).
Note: Table data inputs rounded up to two decimal places, see Supplementary Material for more detail.
See Table 2 for detail on AD dementia descriptive system.
2.5. Community versus institution (AD dementia states)
When people are in AD dementia states, they have a risk of moving from a community setting to being located in an institutional setting. We estimate the risk of moving to an institutional setting using NACC data on 4839 participants with a diagnosis of dementia due to AD (primary cause 94%; contributing cause 6%); of these, a total of 638 (13%) moved to an institutional setting in the follow-up data. With this data, we use a parametric survival (time to event) analysis to estimate the proportion of participants moving into an institutional setting (categorized in NACC as assisted environment or institutionalization). We use an exponential hazard function, consistent with the application of a constant rate in a decision-analytic model, with symptom-domain descriptions (cognition, behavior/mood, function) as time-dependent covariates. We find all covariates are statistically significant (P < .05) and predict an overall annual transition of circa 5% from AD dementia states in the community to an institutional setting; transitions stratified by severity categories of mild, moderate, and severe, at annual rates of 1.4%–3.8%, 1.8%–9.2%, and 2.0%–14.3%, respectively, see Supplementary Detail (S3).
2.6. Mortality
Mortality data is a key input to any AD progression model. We consider mortality as a decision-analytic input, likely to be context (e.g., country) specific in future economic evaluations, and therefore, we have not estimated mortality within the disease progression model. As a decision-analytic input, future users of the model are able to insert analysis-specific data/model inputs. In this study, we use age-specific mortality rates at each time point to operationalize the model, using population data on age-specific all-cause mortality (for USA [35] in our initial presentation). As evidence indicates that mortality rates are higher in more severe stages of disease [36,37], we apply relative risks (hazard rates) to this data to reflect the expected differences in mortality according to disease severity [38], see Table 4.
Table 4.
Model and CEA inputs/parameters
| Parameter | Input | Source |
|---|---|---|
| Starting age (years) | 75 | Assumption |
| All-cause mortality (population) by age | by age | US data/Life tables 2013 [35] |
| RR of death by AD dementia severity: | Andersen et al. [38] | |
| Mild | 2.92 | |
| Moderate | 3.85 | |
| Severe | 9.52 | |
| Probability/transition rate from MCI to AD dementia | - | See analysis; NACC data |
| Probability/transition rate across AD dementia states | - | See analysis; NACC data |
| Costs of care (per year): | ||
| MCI | $13,364 | Assumption, 50% of mild cost* |
| Mild | $26,727 | Gustavsson et al., 2011† [39] |
| Moderate | $31,644 | Gustavsson et al., 2011† [39] |
| Severe | $40,645 | Gustavsson et al., 2011† [39] |
| Institution-mild/moderate | $111,902 | Gustavsson et al., 2011† [39] |
| Institution-severe | $113,523 | Gustavsson et al., 2011† [39] |
| Effectiveness (future DMT), relative risk | 0.80 | Assumption (reflecting reduction in risk of 20%) |
| Treatment cost (hypothetical DMT) pa | $5000 | Assumption |
| Treatment duration (years), MCI | 5 | Assumption |
| Health state values/utilities: | Neumann et al. [40]‡ | |
| MCI | 0.73 | |
| Mild | 0.69 | |
| Moderate | 0.53 | |
| Severe | 0.38 | |
| Discount rate future costs and outcomes, pa | 3% | Assumption (rate applicable to USA) |
Abbreviations: AD, Alzheimer’s disease; CEA, cost-effectiveness analysis; RR, relative risk; MCI, mild cognitive impairment; DMT, disease modifying therapy; CDR, clinical dementia rating.
Support for this assumption comes from studies reported by Darba et al. [41] and Jonsson et al. [42] where estimated costs associated with time in MCI were in the region of 50–60% of the costs for mild AD.
Costs uprated from 2007 US $ to 2017 US $, costs include informal care and productivity loss costs.
Health state values against severity stages using the global CDR scale staging [43].
2.7. Decision-analytic inputs
Alongside key structural components and data inputs for the model, in any evaluation, other key data inputs will be required for health state costs, intervention costs, health state values (to estimate quality-adjusted life years [QALY]), and data on effectiveness of interventions. In addition, inputs to the economic evaluation will also be required to reflect discounting of future costs and outcomes (where applicable) and a statement on perspective for the research question being addressed.
The modeling framework provides flexible input options for all these decision-analytic inputs. We present an example of an economic evaluation for a hypothetical intervention, using a US context, to demonstrate the potential use of the modeling framework. Data inputs for costs and health state values are from literature generalizable to the US context. Table 4 presents the decision-analytic inputs used for the cost-effectiveness analyses (CEA) presented in the following section and other base case data inputs and parameters.
3. Cost-effectiveness analysis: Early intervention in predementia
In this exemplar analysis, we assume an intervention is available for the treatment of people with MCI due to AD and that it is effective at reducing the rate of conversion from MCI due to AD (predementia) to the AD dementia stage of the disease, compared with usual care. This effectiveness assumption refers only to those people in the predementia state who are expected to benefit from a hypothetical treatment scenario. We use an assumed effectiveness parameter (i.e., model input to reduce the rate of conversion from predementia to dementia), using a relative risk of 0.8, when estimating the rate of conversion from MCI to AD dementia diagnosis in those people allocated to a hypothetical treatment scenario. We use the decision-analytic model-based framework presented in this study to estimate the incremental cost per QALY associated with the intervention versus usual care.
We use a starting cohort of people aged 75 years with MCI due to AD. We assume a treatment cost of $5000 (USD) per person per year for treatment in MCI due to AD for up to 5 years. When transitioning from MCI to AD dementia, treatment is discontinued. We use data from the study by Neumann et al. [40] on health state values associated with severity staging of AD across clinical dementia rating stages of questionable, mild, moderate, and severe. We use US data on resource use and costs per year from the study by Gustavsson et al. [39], who report data for mild, moderate, and severe AD, and separate estimates for those in an institutional setting. Data from the study by Gustavsson et al. [39] are reflected in US dollars uprated to 2017 costs (using US personal consumption expenditure health index [44]).
4. Results
The disease progression component of the model, using base case inputs, predicts a mean life expectancy for controls at 7.70 years, before use of a half-cycle correction and before discounting of future life years, which comprises 4.75 years in MCI, 2.61 years with AD dementia in a community setting (0.94 years, mild; 1.27 years, moderate; and 0.40 years, severe states), and 0.35 years with AD dementia in an institutional setting (0.03 years, mild; 0.18 years, moderate; and 0.14 years, severe states). For the treated cohort, the comparative mean life expectancy is 8.04 years, comprising 5.35 years in MCI, 2.38 years with AD dementia in a community setting (0.87 years, mild; 1.15 years, moderate; and 0.36 years, severe states), and 0.30 years with AD dementia in an institutional setting (0.03 years, mild; 0.16 years, moderate; 0.12 years, severe states), see summary in Fig. 2. When adjusting for half-cycle correction (i.e., events occur midpoint of each 1-year cycle) and discounting future life years, the mean life expectancy predicted for usual care and treatment are 7.14 years and 7.39 years, respectively.
Fig. 2.
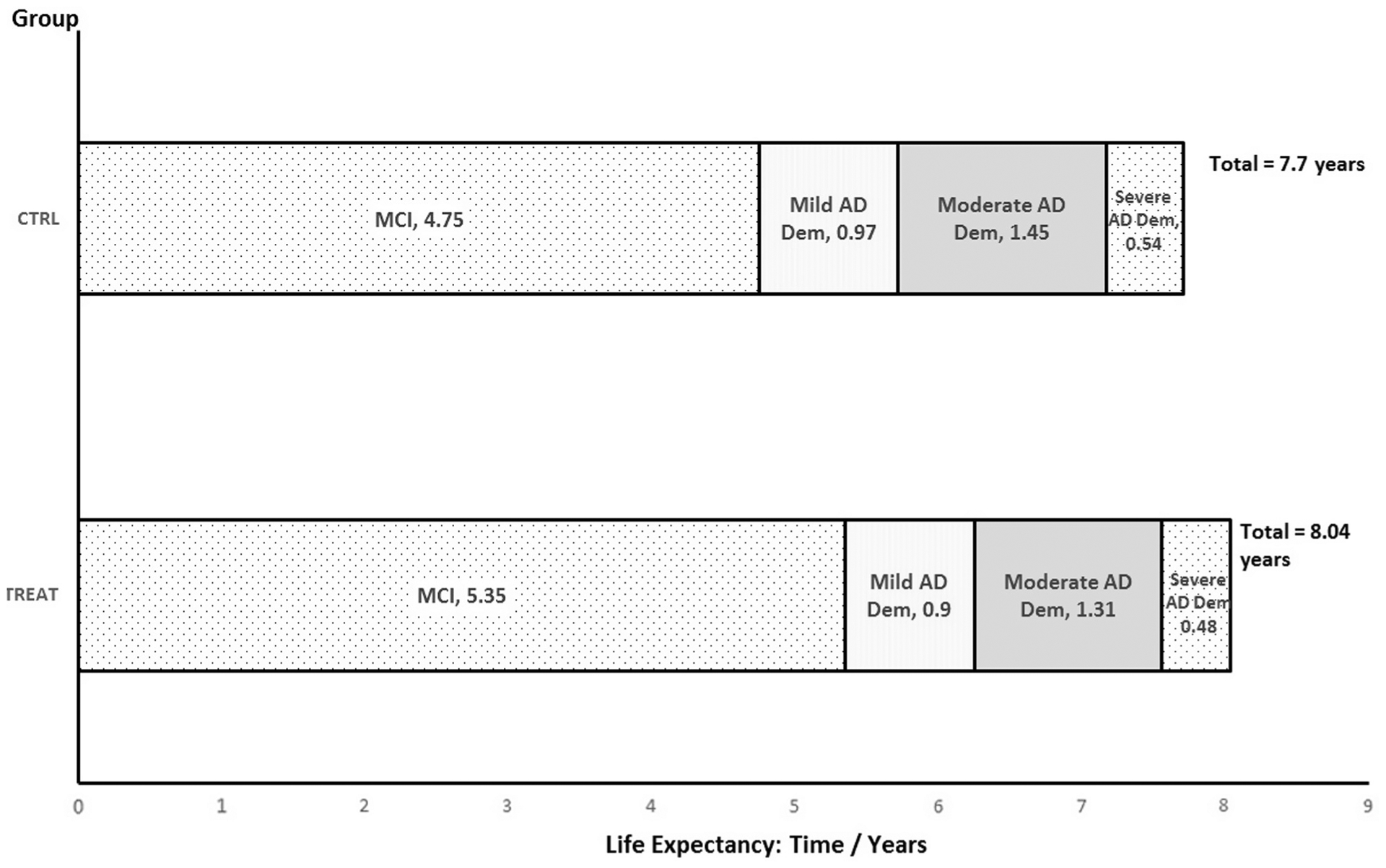
Profile across AD stages by group (predicted time/years in each stage). Abbreviations: CTRL, control/usual care; TREAT, treated with hypothetical DMT; MCI, mild cognitive impairment; AD, Alzheimer’s disease; DEM, dementia.
The survival rate after 5 years and 10 years is 73% and 32%, respectively, in the control cohort, and 75% and 36%, respectively, in the treated cohort. At 5 years (60 months) and 10 years (120 months), the proportion of the control cohort still in the MCI due to AD state is 40% and 17%, respectively, and for the treated cohort, it is 46% and 20%, respectively.
Fig. 3 presents the cohort profile by disease stage over time. When considering the treatment scenario, we see a greater proportion of time spent in MCI and less time in each of the AD dementia stages. Profiles for each of the symptom domains show a similar pattern, with less time spent in each of the more severe levels for each of the three symptom domains (see Supplementary Material, S4).
Fig. 3.
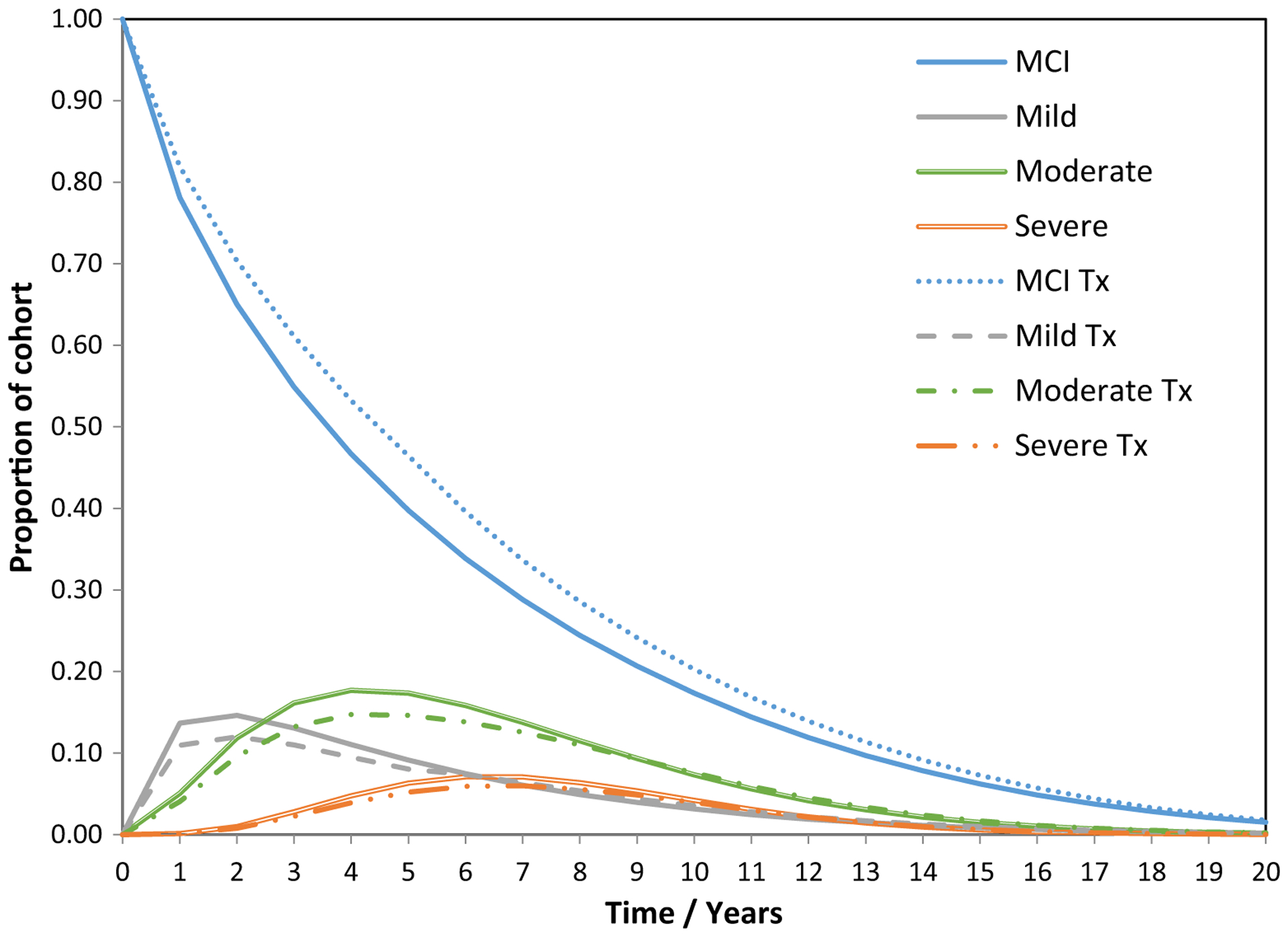
Cohort profile over time by disease severity/stage. Abbreviations: Tx, Treatment scenario; MCI, mild cognitive impairment (due to AD).
Table 5 presents result for the CEA. Using base case assumptions, the estimated cost per QALY gained for treatment versus usual care is $50,542. In sensitivity analysis (SA), when modeling for a cohort with a starting age of 70 years, with all other base case inputs, this scenario (SA2) provides an opportunity to capture greater benefits from treatment, with a cost per QALY gained at $35,503.
Table 5.
Cost-effectiveness analysis results and sensitivity analyses (SA1-SA10)
| Scenario | LE (mean) | Costs, $ (mean) | QALYs (mean) | Incremental costs $ (mean) | Incremental QALYs (mean) | ICER $ |
|---|---|---|---|---|---|---|
| Base case: | ||||||
| Usual care | 7.14 | 160,029 | 4.86 | |||
| DMT | 7.39 | 171,360 | 5.08 | 11,330 | 0.224 | 50,542 |
| SA1: no discounting | ||||||
| Usual care | 8.19 | 187,315 | 5.56 | |||
| DMT | 8.53 | 199,558 | 5.85 | 12,243 | 0.287 | 42,607 |
| SA2: Start aged 70 years | ||||||
| Usual care | 8.48 | 213,281 | 5.66 | |||
| DMT | 8.75 | 222,306 | 5.91 | 9024 | 0.254 | 35,503 |
| SA3: Effectiveness, 40% reduction in risk of AD dementia* | ||||||
| Usual Care | 7.14 | 160,029 | 4.86 | |||
| DMT | 7.67 | 168,290 | 5.33 | 8261 | 0.471 | 17,552 |
| SA4: Cohort reflects higher risk MCI group (i.e., year 1 conversion, 27.5% for controls) | ||||||
| Usual care | 6.93 | 163,442 | 4.68 | |||
| DMT | 7.21 | 173,290 | 4.93 | 9848 | 0.250 | 39,347 |
| SA5: Mortality rate† is state dependent (MCI, mild, mod, and severe; 3%,5.5%, 21.5%, 48% pa, respectively) | ||||||
| Usual care | 8.28 | 198,014 | 5.59 | |||
| DMT | 8.65 | 211,804 | 5.89 | 13,790 | 0.302 | 45,691 |
| SA6: Mortality rate is flat rate of 10% pa for all states/time points‡ | ||||||
| Usual care | 7.02 | 225,572 | 4.46 | |||
| DMT | 7.02 | 223,587 | 4.53 | (−1984) | 0.075 | Dominant |
| SA7: DMT cost at $10,000 per year | ||||||
| Usual care | 7.14 | 160,029 | 4.86 | |||
| DMT | 7.39 | 186,501 | 5.08 | 26,472 | 0.224 | 118,084 |
| SA8: DMT cost at $10,000 per year and effectiveness at 40% reduction in risk of AD dementia | ||||||
| Usual care | 7.14 | 160,029 | 4.86 | |||
| DMT | 7.67 | 184,516 | 5.33 | 24,487 | 0.471 | 52,029 |
| SA9: Cost per year in each stage (MCI, mild, moderate, and severe) excludes informal care and related costs | ||||||
| Usual care | 7.14 | 87,402 | 4.86 | |||
| DMT | 7.39 | 99,301 | 5.08 | 11,899 | 0.224 | 53,079 |
| SA10: Cost per year in MCI state at $6682 (25% of mild dementia cost) | ||||||
| Usual care | 7.14 | 129,142 | 4.86 | |||
| DMT | 7.39 | 137,076 | 5.08 | 7934 | 0.224 | 35,392 |
Abbreviations: LE, Life expectancy; QALYs, quality-adjusted life years; ICER, incremental cost per QALY; DMT, disease modifying therapy; SA, sensitivity analysis.
In this scenario (relative risk: 0.6; reduction in risk of 40%), for every 100 people starting in MCI in the treatment cohort (year 1), there are 85.7 people that remain in MCI, versus 81.9 people when the reduction in risk is 20%, and versus 78.1 people in MCI (year 1) in the usual care cohort.
Mortality rates for AD dementia in this study are from Spackman et a1 [45]; Mortality rate for MCI reflects reported all-cause population mortality rate for age 75 [35].
Also dominant at flat mortality rate of 5% pa.
When assuming a larger treatment effect with a 40% reduction (i.e., relative risk: 0.6) in transitions to AD dementia (SA3), the cost per QALY reduces to $17,552. Assuming a MCI cohort with a higher risk of conversion to AD dementia (SA4), as expected for amnestic MCI, with risk of conversion adjusted to reflect a 27.5% risk of conversion in year 1 (with rates similar to base case thereafter), we find a relatively modest change in the cost per QALY, to $39,347, with the relative differences in numbers converting to AD dementia between control and treatment groups being similar (to base case) regardless of the higher absolute levels of risk (conversion to AD dementia). In further sensitivity analyses, we find that the cost per QALY estimate is sensitive to inputs for mortality data, treatment cost, and costs associated with time spent in the MCI state (Table 5).
5. Discussion
The change in focus for the development of DMTs from dementia states to the predementia stage of AD implies, in the absence of the identification of high-risk groups, treating a large “at risk” population of which only a subset would progress over time to dementia. However, against this potentially expensive evaluative setting, we find that when modeling a treatment scenario, there is a clear and unambiguous potential benefit from treatment, with extended time in the predementia health state and a reduction in time spent in all future AD dementia states, regardless of disease severity.
When comparing a DMT costing $5000 per year with usual care, we find cost-effectiveness estimates to be in the region of what may be considered value for money [46] when applying relatively modest base case assumptions on treatment effectiveness. Although we are unable to anticipate the magnitude of the effectiveness of any future DMT, we suggest the estimate used could be reasonably considered as modest and, therefore, a conservative approach in our model-based assessment. That is, when applying the model to a cohort of people with MCI due to AD aged 75 years (assuming 20% reduction in the risk), we predict that for every 100 people with MCI due to AD, there will be 15 people in a treated scenario, versus 19 people in usual care, that will experience a diagnosis of AD dementia in the first year of the model. This difference of four people in year 1, reduces to 1.4 people in year two, and 0.5 people in year three, decreasing thereafter. We do acknowledge that effectiveness in this study is aligned to an event-based endpoint (i.e., conversion from predementia to AD dementia), and any DMT may deliver broader benefits to people with AD related to improvements in the way they experience the impacts of cognitive decline.
Sensitivity analysis indicates areas where cost per QALY estimates are sensitive to model inputs and assumptions. Ours is a relatively simple modeling framework, with a number of current limitations, as discussed in the following section, but the presentation in this study is not focused principally on the estimates of cost per QALY reported, which reflect an example of a future application of the modeling framework. Primarily, we consider this modeling framework a core contribution to the literature in this area, and we see its potential impact as providing a common starting position for the development of a more complex framework and from which the field can start to engage more widely, across a range of partners and collaborations, to move forward the methods available to support a goal of rapid access to effective and cost-effective future DMTs in AD.
We present a fully transparent model-based framework and make this available in an open-access format (see Supplementary Material). It is currently difficult to benchmark our model performance and outputs against other methods because there is an absence of detail in many previously published modeling studies. For example, the study by Budd et al. [17] uses a similar model structure, including similar mortality data for a US analysis, reporting what we interpret as a life expectancy of 5.75 years (starting age 75 years) comprising 3.19 years in MCI or mild AD dementia and 2.56 years in moderate or severe AD dementia (in a usual care cohort). Data presented do not permit a more detailed comparison. Our results predict a longer life expectancy and a greater proportion of time in the MCI or mild AD states and a lesser time spent in moderate and severe AD dementia states combined. The analysis in the study by Budd et al. [17] is unclear on data inputs for disease progression, but rates of conversion from MCI to AD were based on data drawn from an amnestic biomarker confirmed MCI sample, with rates for this group known to be higher than relying on clinical assessment only. It also uses AD dementia transition probabilities derived from a relatively small randomized controlled trial evaluating donepezil over a 6-month follow-up [47], with transition probabilities reported between stages for AD dementia defined using MMSE categories [48]. This combination of inputs from the study by Budd et al. [17] most likely results in a more rapid transition across stages of disease severity and related increases in mortality risk. Importantly, the study by Budd et al. [17] reports a similar result to that found in this study when considering a hypothetical treatment scenario, finding a reduction in time spent across all stages of dementia severity and a greater amount of time spent in the predementia stage of AD. Other studies have described modeling across predementia into and across AD dementia stages, but in most of these studies, data inputs and results are not reported in a way that provides a basis for comparison. For example, with studies putting a focus on reporting of estimated costs and QALYs rather than disaggregated data on profile of disease progression [18,19].
In a recent contribution to the literature, the study by Davis et al. [49] presents a modeling framework using data from NACC and structured from predementia states into and across AD dementia, as characterized by the global clinical dementia ratings scale staging [43], with findings supporting those presented in this study, showing early intervention in predementia stages is likely to reduce mean time in all the more severe stages of AD dementia.
In addition to the use of parametric estimation of transition probabilities using the ordered probit approach, we also determine transitions using the data observed in the sample (n = 4974) using a 1-year time period. This approach is consistent with the approach previously described and presented in the study by Green and Zhang [22]. We compare the results for the parametric methods and nonparametric approach and find no marked differences (see Supplementary Information, S3). The parametric approach allows future development of transition probabilities, where additional covariates can be introduced for characteristics such as age and may be best suited for development of an individual participant level simulation model.
The model presented has several limitations. It uses only one health state for predementia, assuming a common rate of conversion to AD dementia, based on the estimates derived from the NACC data. Future planned development of the model will incorporate additional stages of AD progression, capturing the stage(s) from preclinical to prodromal AD or MCI, before the progression of AD into the dementia stages, including consideration of subjective cognitive decline [50] between asymptomatic preclinical AD and the onset of AD symptoms. We will also seek to incorporate different risk groups within and across preclinical and predementia states, for example, those with specific genetic and biomarker profiles [51], where data are available.
The model uses a 1-year cycle length which may not fully capture disease activity and differences in costs and effects, and we will explore alternative options in future model development. The model uses a multidomain approach to describe dementia states, which we believe to be important. However, data currently available to populate the model (i.e., mortality data by disease severity, data on health state utility values and costs) is not able to fully reflect the description of AD dementia used (across the multiple domains), therefore, we have had to apply data inputs for broad categories of disease severity (mild, moderate, and severe), and this approach may not fully reflect the potential benefits of the model structure. We have also used these broad severity categories to describe disease progression and results, to articulate the nature of the predicted time across stages of AD.
The CEA undertaken does not include assessment of uncertainty in parameter inputs, or structural assumptions, beyond the one-way and multiway sensitivity analyses presented. Future developments will involve a more detailed demonstration of the modeling framework, alongside decision-analytic inputs able to undertake and present analysis of uncertainty, for example, using probabilistic sensitivity analyses [52]. Furthermore, our model does not consider the potential impact on caregiver quality of life or other outcomes that may be considered important when assessing the value of future DMTs. A challenge for all models in this area is on the demonstration of external validity [13], which remains an important but difficult part of model development in the AD context and not addressed in this study. We make the model available in a fully transparent format, and verification (internal validity, internal consistency checks) has been part of the model development process. The face validity of the model has been supported via input from clinical and policy holder perspectives and via feedback across the AD modeling community [26], however, the absence of appropriate methods and data to assess external validity remains a limitation with the model.
The NACC UDS is a valuable resource for the AD research community, with a large sample available and clinical protocols followed for diagnosis and for follow-up data. However, we acknowledge that there may be limitations linked to the generalizability of the sample used in this study. Sample characteristics indicate a broadly representative sample of people with a diagnosis of AD dementia, but readers are advised to consider generalizability in specific applications of the model. In future, effectiveness data for DMTs are likely to be drawn from trials where participants are considered at high risk of AD dementia, with biomarker and/or imaging support for their AD pathophysiology. These factors should be taken into account in future model development and in future economic analyses.
One of the key challenges when assessing cost-effectiveness of future DMTs for AD will be modeling from intermediate trial endpoints (primary trial outcomes), such as ADCS-PACC [53] or ADCOMS [54], to policy relevant outcomes, such as time to diagnosis of AD dementia from MCI, as used in the present model. In this study, we have not considered this challenge, and we are unable to inform on that aspect of health technology assessment at the present time. However, we do acknowledge this as a challenge for those developing DMTs and believe our model provides a further motivation for the development of robust research to demonstrate the relationship associated with trial endpoints to satisfy the health policy and reimbursement requirements of health technology assessment agencies.
6. Conclusions
The model-based evaluation framework presented in this study contributes to the methods available to predict disease progression across AD and to estimate the cost-effectiveness of DMTs for people with MCI due to AD. Future DMTs targeting the predementia stages of AD are likely to result in increases in life expectancy through reduced exposure to higher mortality rates when in AD dementia stages, with additional time spent in predementia and not in the later AD dementia stages of the disease. However, because of the prevention context and the treatment of a relatively large at risk group of people, in many policy settings, it will be important to assess costs relative to health gains, and in high cost scenarios, it will be important to seek out ways to identify people at greater risk of conversion to AD dementia among those with an MCI diagnosis.
Supplementary Material
RESEARCH IN CONTEXT.
Systematic Review: Recent literature reviews have identified model-based economic evaluation frameworks for Alzheimer’s disease (AD), however, all have limitations, and further research is needed to support the health policy context.
Interpretation: We present a fully transparent approach to model AD progression from predementia into and across AD dementia stages and to assess the cost-effectiveness of future disease-modifying therapies (DMTs). Our model is the first to be made open-access in AD. Results indicate that a future DMT for mild cognitive impairment is expected to extend time in predementia, reduce time spent in AD dementia states, and result in modest increases in life expectancy. Corresponding health gains and reductions in required care make it feasible for a future DMT (dependent on its purchase costs) to demonstrate value for money in health technology assessment settings.
Future Directions: We aim to further develop the model-based decision-analytic framework presented, to include translation of trial endpoints into policy relevant outcomes.
Acknowledgments
We would like to thank The National Alzheimer’s Disease Coordinating Center (NACC) for access to NACC data. The NACC database is funded by National Institute on Aging/National Institutes of Health Grant U01 AG016976. NACC data are contributed by the NIA funded ADCs: P30 AG019610 (PI Eric Reiman, MD), P30 AG013846 (PI Neil Kowall, MD), P50 AG008702 (PI Scott Small, MD), P50 AG025688 (PI Allan Levey, MD, PhD), P50 AG047266 (PI Todd Golde, MD, PhD), P30 AG010133 (PI Andrew Saykin, PsyD), P50 AG005146 (PI Marilyn Albert, PhD), P50 AG005134 (PI Bradley Hyman, MD, PhD), P50 AG016574 (PI Ronald Petersen, MD, PhD), P50 AG005138 (PI Mary Sano, PhD), P30 AG008051 (PI Steven Ferris, PhD), P30 AG013854 (PI M. Marsel Mesulam, MD), P30 AG008017 (PI Jeffrey Kaye, MD), P30 AG010161 (PI David Bennett, MD), P50 AG047366 (PI Victor Henderson, MD, MS), P30 AG010129 (PI Charles DeCarli, MD), P50 AG016573 (PI Frank LaFerla, PhD), P50 AG016570 (PI Marie-Francoise Chesselet, MD, PhD), P50 AG005131 (PI Douglas Galasko, MD), P50 AG023501 (PI Bruce Miller, MD), P30 AG035982 (PI Russell Swerdlow, MD), P30 AG028383 (PI Linda Van Eldik, PhD), P30 AG010124 (PI John Trojanowski, MD, PhD), P50 AG005133 (PI Oscar Lopez, MD), P50 AG005142 (PI Helena Chui, MD), P30 AG012300 (PI Roger Rosenberg, MD), P50 AG005136 (PI Thomas Montine, MD, PhD), P50 AG033514 (PI Sanjay Asthana, MD, FRCP), P50 AG005681 (PI John Morris, MD), and P50 AG047270 (PI Stephen Strittmatter, MD, PhD). An earlier summary version of the research (method) approach and model structure used in this paper was presented and discussed at the 8th International Pharmacoeconomic Conference on Alzheimer’s Disease (IPECAD) meeting, Paris, France, February 15th-16th 2018.
We would like to thank Leala Watson, University of Exeter, UK, for assistance in formatting the manuscript. We would like to thank Gunilla Johansson, Karolinska Institute, Stockholm, Sweden, for administrative support related to the development of research associated with the manuscript.
Conflict of Interest:
B.W. acknowledges financial support from the Swedish Research Council, No 2018-02843 and from Margaretha af Ugglas’ Foundation. L.J. is an employee of H. Lundbeck, a pharmaceutical company that develops and markets therapies for Alzheimer’s disease. R.H. acknowledges financial support received from the Dutch Alzheimer’s Association, ‘Alzheimer Nederland’, against grant number WE.15-2016-09. A.G. is a partner of Quantify Research, providing consultancy services to pharmaceutical companies and other private and public organizations and institutions.
Footnotes
Supplementary Data
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jalz.2019.05.004.
References
- [1].World Health Organization. WHO health statistics and information systems: Estimates for 2000–2012, http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html. Accessed February 15, 2016.
- [2].Prince M, Wimo A, Guerchet M, Ali G-C, Wu Y-T, Prina M, et al. World Alzheimer Report 2015: The Global Impact of Dementia 2015. London, UK: Alzheimer’s Disease International; 2015. [Google Scholar]
- [3].Winblad B, Amouyel P, Andrieu S, Ballard C, Brayne C, Brodaty H, et al. Defeating Alzheimer’s disease and other dementias: a priority for European science and society. Lancet Neurol 2016;15:455–532. [DOI] [PubMed] [Google Scholar]
- [4].Hardy J, Selkoe DJ. The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics. Science 2002; 297:353–6. [DOI] [PubMed] [Google Scholar]
- [5].Guerreiro R, Wojtas A, Bras J, Carrasquillo M, Rogaeva E, Majounie E, et al. TREM2 variants in Alzheimer’s disease. N Engl J Med 2013;368:117–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Schneider LS, Mangialasche F, Andreasen N, Feldman H, Giacobini E, Jones R, et al. Clinical trials and late-stage drug development for Alzheimer’s disease: an appraisal from 1984 to 2014. J Intern Med 2014; 275:251–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Goldman DP, Fillit H, Neumann P. Accelerating Alzheimer’s disease drug innovations from the research pipeline to patients. Alzheimers Dement 2018;14:833–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Haeberlein SB, Castrillo-Viguera C, Gheuens S, Chen T, O’Gorman J, Chiao P, et al. 24-month analysis of change from baseline in clinical dementia rating scale cognitive and functional domains in PRIME, a randomized phase 1b study of the anti-amyloid beta monoclonal antibody aducanumab. Alzheimers Dement 2018;14:P242. [Google Scholar]
- [9].Aisen PS. Continuing progress in Alzheimer’s disease trials: cause for optimism. J Prev Alzheimers Dis 2017;4:211–2. [DOI] [PubMed] [Google Scholar]
- [10].Liu JL, Hlavka JP, Hillestad R, Mattke S. Assessing the Preparedness of the U.S. Health Care System Infrastructure for an Alzheimer’s Treatment 2017. Santa Monica, CA: RAND Corporation; 2017. [Google Scholar]
- [11].Hlavka JP, Mattke S, Liu JL. Assessing the Preparedness of the Health Care System Infrastructure in Six European Countries for an Alzheimer’s Treatment 2018. Santa Monica, CA: RAND Corporation; 2018. [PMC free article] [PubMed] [Google Scholar]
- [12].Anderson R, Knapp M, Wittenberg R, Handels R, Schott JM. Economic Modelling of Disease-Modifying Therapies in Alzheimer’s Disease 2018. London: Personal Social Services Research Unit, London School of Economics and Political Science; 2018. [Google Scholar]
- [13].Nguyen K-H, Comans T, Green C. Where are we at with model-based economic evaluations of interventions for dementia? A systematic review and quality assessment. Int Psychogeriatrics 2018; 30:1593–605. [DOI] [PubMed] [Google Scholar]
- [14].Kors J, Potashman M, van der Lei J, Amzal B, Handels R. ROADMAP Real world Outcomes across the AD spectrum for better care: Multi-modal data Access Platform (Innovative Medicines Initiative Joint Undertaking) ROADMAP Consortium, 2017. https://roadmap-alzheimer.org/wp-content/uploads/2018/09/116020_ROADMAP_D4.1_Catalogue-of-RWE-relevant-AD-models-and-simplistic-disease-stage-framework.pdf. Accessed April 6, 2019.
- [15].Gustavsson A, Green C, Jones RW, Forstl H, Simsek D, de Reydet de Vulpillieres F, et al. Current issues and future research priorities for health economic modelling across the full continuum of Alzheimer’s disease. Alzheimers Dement 2017;13:312–21. [DOI] [PubMed] [Google Scholar]
- [16].Djalalov S, Yong J, Beca J, Black S, Saposnik G, Musa Z, et al. Genetic testing in combination with preventive donepezil treatment for patients with amnestic mild cognitive impairment: an exploratory economic evaluation of personalized medicine. Mol Diagn Ther 2012; 16:389–99. [DOI] [PubMed] [Google Scholar]
- [17].Budd D, Burns LC, Guo Z, L’Italien G, Lapuerta P. Impact of early intervention and disease modification in patients with predementia Alzheimer’s disease: a Markov model simulation. Clinicoecon Outcomes Res 2011;3:189–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Skoldunger A, Johnell K, Winblad B, Wimo A. Mortality and treatment costs have a great impact on the cost-effectiveness of disease modifying treatment in Alzheimer’s disease–a simulation study. Curr Alzheimer Res 2013;10:207–16. [DOI] [PubMed] [Google Scholar]
- [19].Guo S, Getsios D, Hernandez L, Cho K, Lawler E, Altincatal A, et al. Florbetaben PET in the early diagnosis of Alzheimer’s disease: a discrete event simulation to explore its potential value and key data gaps. Int J Alzheimers Dis 2012;2012:548157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Handels RLH, Vos SJB, Kramberger MG, Jelic V, Blennow K, van Buchem M, et al. Predicting progression to dementia in persons with mild cognitive impairment using cerebrospinal fluid markers. Alzheimers Dement 2017;13:903–12. [DOI] [PubMed] [Google Scholar]
- [21].Tong T, Thokala P, McMillan B, Ghosh R, Brazier J. Cost effectiveness of using cognitive screening tests for detecting dementia and mild cognitive impairment in primary care. Int J Geriatr Psychiatry 2017; 32:1392–400. [DOI] [PubMed] [Google Scholar]
- [22].Green C, Zhang S. Predicting the progression of Alzheimer’s disease dementia: a multidomain health policy model. Alzheimers Dement 2016;12:776–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Handels RL, Wolfs CA, Aalten P, Joore MA, Verhey FR, Severens JL. Diagnosing Alzheimer’s disease: a systematic review of economic evaluations. Alzheimers Dement 2014;10:225–37. [DOI] [PubMed] [Google Scholar]
- [24].Green C, Shearer J, Ritchie CW, Zajicek JP. Model-based economic evaluation in Alzheimer’s disease: a review of the methods available to model Alzheimer’s disease progression. Value Health 2011;14:621–30. [DOI] [PubMed] [Google Scholar]
- [25].Gustavsson A, Jonsson L, Fillit H, Johansson G, Wimo A, Winblad B. IPECAD5–Fifth International Pharmaco-Economic Conference on Alzheimer’s disease. J Nutr Health Aging 2010;14:358–60. [DOI] [PubMed] [Google Scholar]
- [26].Proceedings from the 8th International Conference on Pharmacoeconomics of Alzheimer’s disease (IPECAD), Paris, February 15–16, 2018, http://www.trippus.se/web/presentation/web.aspx?evid=/5IaMiO4uSIXT5CMOFf6kA==&ecid=TdAXZxrhfJX/7A1gfq53oQ==&ln=eng&view=category&template=desktoph. Accessed April 6, 2019.
- [27].Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 2011;7:270–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Beekly DL, Ramos EM, Lee WW, Deitrich WD, Jacka ME, Wu J, et al. The National Alzheimer’s Coordinating Center (NACC) database: the uniform data set. Alzheimer Dis Assoc Disord 2007;21:249–58. [DOI] [PubMed] [Google Scholar]
- [29].Morris JC, Weintraub S, Chui HC, Cummings J, Decarli C, Ferris S, et al. The Uniform Data Set (UDS): clinical and cognitive variables and descriptive data from Alzheimer disease centers. Alzheimer Dis Assoc Disord 2006;20:210–6. [DOI] [PubMed] [Google Scholar]
- [30].McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR, Kawas CH, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 2011;7:263–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12:189–98. [DOI] [PubMed] [Google Scholar]
- [32].Pfeffer RI, Kurosaki TT, Harrah CH, Chance JM, Filos S. Measurement of functional activities in older adults in the community. Journals Gerontol 1982;37:323–9. [DOI] [PubMed] [Google Scholar]
- [33].Kaufer DI, Cummings JL, Ketchel P, Smith V, MacMillan A, Shelley T, et al. Validation of the NPI-Q, a brief clinical form of the neuropsychiatric inventory. J Neuropsych Clin N 2000;12:233–9. [DOI] [PubMed] [Google Scholar]
- [34].McKelvey RD, Zavoina W. A statistical model for the analysis of ordinal level dependent variables. J Math Sociol 1975;4:103–20. [Google Scholar]
- [35].Arias E, Heron M, Jiaquan X. United States Life Tables, 2013 2017. National Vital Statistics Reports; 2017:66: [PubMed] [Google Scholar]
- [36].Garcia-Ptacek S, Farahmand B, Kareholt I, Religa D, Cuadrado ML, Eriksdotter M. Mortality risk after dementia diagnosis by dementia type and underlying factors: a cohort of 15,209 patients based on the Swedish Dementia Registry. J Alzheimers Dis 2014;41:467–77. [DOI] [PubMed] [Google Scholar]
- [37].Rhodius-Meester HFM, Liedes H, Koene T, Lemstra AW, Teunissen CE, Barkhof F, et al. Disease-related determinants are associated with mortality in dementia due to Alzheimer’s disease. Alzheimers Res Ther 2018;10:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Andersen K, Lolk A, Martinussen T, Kragh-Sorensen P. Very mild to severe dementia and mortality: A 14-year follow-up - The Odense study. Dement Geriatr Cogn Disord 2010;29:61–7. [DOI] [PubMed] [Google Scholar]
- [39].Gustavsson A, Brinck P, Bergvall N, Kolasa K, Wimo A, Winblad B, et al. Predictors of costs of care in Alzheimer’s disease: a multinational sample of 1222 patients. Alzheimers Dement 2011; 7:318–27. [DOI] [PubMed] [Google Scholar]
- [40].Neumann PJ, Kuntz KM, Leon J, Araki SS, Hermann RC, Hsu MA, et al. Health utilities in Alzheimer’s disease: a cross-sectional study of patients and caregivers. Med Care 1999;37:27–32. [DOI] [PubMed] [Google Scholar]
- [41].Darba J, Kaskens L, Lacey L. Relationship between global severity of patients with Alzheimer’s disease and costs of care in Spain; results from the co-dependence study in Spain. Eur J Health Econ 2015; 16:895–905. [DOI] [PubMed] [Google Scholar]
- [42].Jonsson L, Eriksdotter Jonhagen M, Kilander L, Soininen H, Hallikainen M, Waldemar G, et al. Determinants of costs of care for patients with Alzheimer’s disease. Int J Geriatr Psychiatry 2006; 21:449–59. [DOI] [PubMed] [Google Scholar]
- [43].Morris JC. The Clinical Dementia Rating (CDR): current version and scoring rules. Neurology 1993;43:2412–4. [DOI] [PubMed] [Google Scholar]
- [44].Agency for Healthcare Research and Quality. Using Appropriate Price Indices for Analyses of Health Care Expenditures or Income Across Multiple Years, https://meps.ahrq.gov/about_meps/Price_Index.shtml. Accessed December 14, 2018.
- [45].Spackman DE, Kadiyala S, Neumann PJ, Veenstra DL, Sullivan SD. Measuring Alzheimer disease progression with transition probabilities: estimates from NACC-UDS. Curr Alzheimer Res 2012; 9:1050–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Neumann PJ, Cohen JT, Weinstein MC. Updating cost-effectiveness– the curious resilience of the $50,000-per-QALY threshold. N Engl J Med 2014;371:796–7. [DOI] [PubMed] [Google Scholar]
- [47].Rogers SL, Farlow MR, Doody RS, Mohs R, Friedhoff LT. A 24-week, double-blind, placebo-controlled trial of donepezil in patients with Alzheimer’s disease. Donepezil Study Group Neurol 1998;50:136–45. [DOI] [PubMed] [Google Scholar]
- [48].Stewart A, Phillips R, Dempsey G. Pharmacotherapy for people with Alzheimer’s disease: a Markov-cycle evaluation of five years’ therapy using donepezil. Int J Geriatr Psychiatry 1998;13:445–53. [DOI] [PubMed] [Google Scholar]
- [49].Davis, O Connell T, Johnson S, Cline S, Merikle E, Martenyi F, et al. Estimating Alzheimer’s disease progression rates from normal cognition through mild cognitive impairment and stages of dementia. Curr Alzheimer Res 2018;15:777–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].United States Food and Drug Administration. Guidance for Industry Alzheimer’s Disease: Developing Drugs for the Treatment of Early Stage Disease (Draft Guidance) 2013. Silver Spring, MD USA: Center for Drug Evaluation and Research, Food and Drug Administration; 2013. [Google Scholar]
- [51].Jack CR Jr, Bennett DA, Blennow K, Carrillo MC, Dunn B, Haeberlein SB, et al. NIA-AA Research framework: toward a biological definition of Alzheimer’s disease. Alzheimers Dement 2018; 14:535–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Briggs A. Probabilistic analysis of cost-effectiveness models: statistical representation of parameter uncertainty. Value Health 2005; 8:1–2. [DOI] [PubMed] [Google Scholar]
- [53].Donohue MC, Sperling RA, Salmon DP, Rentz DM, Raman R, Thomas RG, et al. The preclinical Alzheimer cognitive composite: measuring amyloid-related decline. JAMA Neurol 2014;71:961–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Wang J, Logovinsky V, Hendrix SB, Stanworth SH, Perdomo C, Xu L, et al. ADCOMS: a composite clinical outcome for prodromal Alzheimer’s disease trials. J Neurol Neurosurg Psychiatry 2016;87:993–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


