Abstract
Infections of orbit and periorbita are frequent, leading to significant morbidity. Orbital cellulitis is more common in children and young adults. At any age, infection from the neighboring ethmoid sinuses is a likely cause and is thought to result from anatomical characteristics like thin medial wall, lack of lymphatics, orbital foramina, and septic thrombophlebitis of the valveless veins between the two. Other causes are trauma, orbital foreign bodies, preexisting dental infections, dental procedures, maxillofacial surgeries, Open Reduction and Internal Fixation (ORIF), and retinal buckling procedures. The septum is a natural barrier to the passage of microorganisms. Orbital infections are caused by Gram-positive, Gram-negative organisms and anaerobes in adults and in children, usually by Staphylococcus aureus or Streptococcus species. Individuals older than 15 years of age are more likely to harbor polymicrobial infections. Signs include diffuse lid edema with or without erythema, chemosis, proptosis, and ophthalmoplegia. It is an ocular emergency requiring admission, intravenous antibiotics, and sometimes surgical intervention. Computed tomography (CT) and magnetic resonance imaging (MRI) are the main modalities to identify the extent, route of spread from adjacent structures, and poor response to intravenous antibiotics and to confirm the presence of complications. If orbital cellulitis is secondary to sinus infection, drainage of pus and establishment of ventilation to the sinus are imperative. Loss of vision can occur due to orbital abscess, cavernous sinus thrombosis, optic neuritis, central retinal artery occlusion, and exposure keratopathy, and possible systemic sequelae include meningitis, intracranial abscess, osteomyelitis, and death. The article was written by authors after a thorough literature search in the PubMed-indexed journals.
Keywords: Bacterial, complications, imaging, orbital cellulitis, sinusitis
The orbital septum is composed of a fibrous membrane attached superiorly to the periosteum along the orbital rim near the arcus marginalis and fuses near the borders of the tarsus [Fig. 1]. It effectively creates a barrier, preventing the spread of infection from the superficial tissues into deeper orbital spaces.[1] Infection of soft tissues posterior to the orbital septum is termed orbital cellulitis, also referred to as postseptal cellulitis. This condition is serious and needs immediate intervention in initiating appropriate therapy. Orbital cellulitis can be distinguished clinically from preseptal cellulitis by its clinical presentation, such as conjunctival chemosis, ophthalmoplegia, pain with eye movements, and proptosis.[2]
Figure 1.
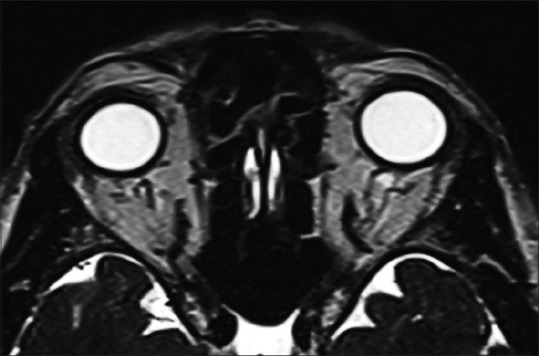
Axial T2 MRI using SPACE sequencing shows a thin, linear, T2-hypointense band-like structure anterior to the globe, more discernible on either side of the globe, representing the orbital septum
Orbital cellulitis can affect all age groups. Children are more commonly affected, and the median age range of children hospitalized with orbital cellulitis is 7–12 years. The predisposing factor for orbital cellulitis, especially in children, is infection of the upper respiratory tract and paranasal sinus. The Zuckerkandl’s dehiscence in the ethmoid bone seems to be the reason for cellulitis to be common in children, whereas in adults, it is most commonly due to trauma and preceding illness.[2] Pandian et al.[3] reported that preseptal cellulitis constituted 70% and postseptal cellulitis 30% of the total number of cases with periocular cellulitis. A study conducted in India in the year 2019 reported an annual incidence of orbital cellulitis in children as 9.29 per 100,000 population.[2] Another study from Scotland has reported an annual incidence of 1.6 per 100,000 population and 0.1 per 100,000 population in children and adults, respectively.[1] The higher incidence in India is attributed to its tropical climate or late presentation.[2]
Bacterial orbital infections have an acute onset and are rapidly progressive in nature. Preexisting dental infections, dental procedures, orbital implants, or orbital foreign bodies may carry a risk of developing an orbital infection. A detailed history of any systemic ailments or immunocompromised conditions like diabetes mellitus, human immunodeficiency virus (HIV), and long-term immunosuppression must be ruled out.[3,4,5]
Chandler classification is the most commonly used system for dividing the different types of orbital cellulitis. The system describes five stages as follows:[6]
Stage I: Preseptal orbital cellulitis with inflammation and edema anterior to the orbital septum
Stage II: Orbital cellulitis with the extension of the inflammation and edema beyond the orbital septum
Stage III: Subperiosteal abscess (SPA) beneath the periosteum of lamina papyracea
Stage IV: Orbital abscess within the intraconal space of orbit
Stage V: Cavernous sinus thrombosis (CST) resulting after the extension of the infection through the superior ophthalmic veins
Clinical presentation
The cardinal signs of orbital cellulitis include diffuse lid edema with or without erythema, conjunctival chemosis, proptosis, and ophthalmoplegia. Other ophthalmic signs may include mechanical ptosis, diplopia, raised retrobulbar resistance, globe dystopia, and/or deterioration of vision.[3-5]
Vision loss has been reported in about 11% of cases of orbital cellulitis.[4] Gross proptosis can lead to exposure keratopathy and corneal ulceration which also leads to deterioration of vision.
El Mograbi et al.[7] found coexisting rhinosinusitis in about 86%–98% of cases of orbital cellulitis. Often, endophthalmitis progresses to panophthalmitis and may present as orbital cellulitis. Inflammation can progress to a stage of either subperiosteal or intraorbital abscess formation affecting the optic nerve, sclera, choroid, and retina with or without intracranial extension.[5]
There may be associated central nervous system involvement like throbbing headache, nausea, vomiting, and altered sensorium.[5] Patients may also present with systemic features like fever, malaise, associated nasal discharge, and cough. Early signs of orbital cellulitis may be often subtle with no significant clinical signs of inflammation until the infection has progressed. This may be often seen with associated systemic comorbidities such as diabetes mellitus, immunosuppression, HIV infections, or even fungal orbital cellulitis.[7]
There are multiple warning signs for bacterial orbital cellulitis, and it may end with various complications if timely intervention is not given [Tables 1 and 2].
Table 1.
Complications of bacterial orbital cellulitis
| Permanent blindness | Cavernous sinus thrombosis |
|---|---|
| Compressive optic neuropathy | Septic embolus |
| Exposure keratopathy | Meningitis |
| Neurotropic keratitis | Brain abscess |
| Central retinal artery occlusion | Sepsis |
| Exudative retinal detachment | Hemiplegia |
Table 2.
Warning signs of orbital cellulitis
| • Painful restriction of extraocular movement |
| • Proptosis |
| • Reduced visual acuity |
| • Abnormal color vision |
| • Relative afferent pupillary defect or fixed, nonreacting pupil |
| • Fever |
SPA results in the collection of pus between the periorbita and the bony wall, characterized by features of orbital cellulitis with localized tenderness over the abscess area. It usually occurs as a complication of bacterial sinusitis.[6,8-10] An orbital abscess presents as a collection of pus in the intraconal or extraconal compartment of the orbit.
CST is both a sight and life-threatening condition presenting with symptoms like headache, nausea, vomiting, and altered sensorium. It involves multiple cranial nerves (oculomotor, trigeminal, and abducent nerves). CST leads to the spread of infection to the opposite orbit, causing bilateral ocular manifestations.
Involvement of the superior orbital fissure can result in orbital apex syndrome characterized by ophthalmoplegia, optic neuritis, and neuralgia along the distribution of ophthalmic division of the trigeminal nerve, along with proptosis and lid edema.[8]
Permanent vision loss is uncommon in the era of antibiotics compared to a preantibiotic era that reported a visual loss in about 20% of patients with postseptal inflammation.[11,12] Mechanism of vision loss may involve reactive optic neuritis due to infection, ischemic thrombophlebitis, or compressive ischemia resulting in central retinal artery occlusion.[11] Irreversible visual loss is mostly due to vascular causes, whereas reversible visual loss is due to compressive optic neuropathy. Other causes include exposure keratopathy, secondary glaucoma, and endophthalmitis.
Orbital cellulitis can cause a few life-threatening complications as follows:
Osteomyelitis: It commonly involves the frontal bone, either by direct invasion or indirectly due to septic thrombophlebitis through the valveless sinus of Breschet.[9]
Intracranial complications: The most common intracranial complication is meningitis, followed by intracranial abscess formation.[9]
Investigations
A complete blood profile may show the presence of peripheral leukocytosis with a predominance of neutrophils and raised C-reactive protein in bacterial orbital cellulitis.
Imaging
Computed tomography (CT) scan or magnetic resonance imaging (MRI) is the imaging of choice.[13-16]
The main role of imaging is to identify the extent of the disease and to identify the origin of infection from adjacent structures, like paranasal sinusitis, inflammatory or infective changes in the orbit, intracranial extension, and the presence of the foreign body. Imaging helps to localize subperiosteal or intraorbital abscesses, assist in preoperative planning, and select an ideal approach for drainage. Contrast study helps to identify early necrosis and differentiates suspected fungal from bacterial orbital cellulitis.[15-18]
CT scan
Periorbital cellulitis- Diffuse soft-tissue thickening with patchy areas of enhancement anterior to the orbital septum is seen in periorbital cellulitis.
Orbital cellulitis- Diffuse inflammatory stranding in the intraconal fat with edema of the extraocular muscles may be seen [Fig. 2].
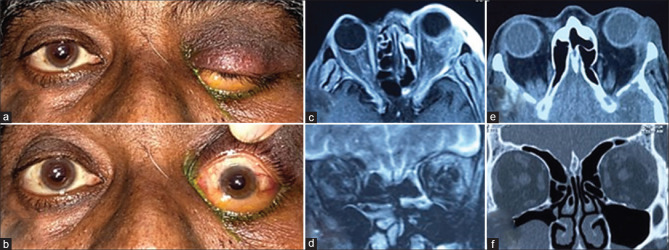
Figure 2.
(a and b) External clinical photograph of an adult male showing tell-tale signs of left orbital cellulitis (proptosis, inferior globe dystopia, mechanical ptosis, conjunctival chemosis). (c) MRI orbits, axial view, T1-weighted, contrast-enhanced image shows a superolateral orbital abscess with rim enhancement. (d) MRI orbits, coronal view, T2-weighted image depicting a superolateral, extraconal orbital abscess with periorbital fat stranding. (e and f) Post-abscess drainage CT scan axial and coronal views depicting reduction in the size of the abscess, proptosis, and orbital edema. CT = computed tomography, MRI = magnetic resonance imaging
MRI scan
Though the hardware is not readily available everywhere, MRI is an extremely useful investigation because of its inherent soft tissue resolution. Also, it is void of radiation hazards.
Similar to CT, diffuse inflammatory stranding in the intraconal fat with edema of the extraocular muscles may be seen, especially in the fat-saturated sequences, where abscess, as in any other location, shows a high signal in T2 with diffusion restriction and thin peripheral rim enhancement [Figs. 3 and 4]. MRI with fat suppression is useful for visualizing the intracranial component. Tenting of the globe due to severe inflammatory edema of the orbit on imaging has been described as an unfavorable prognostic factor in adults.[16]
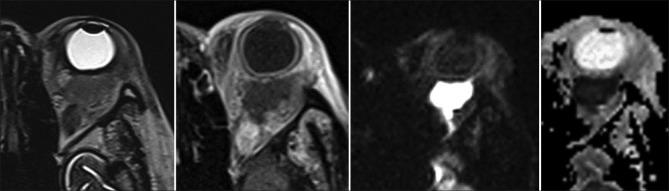
Figure 3.
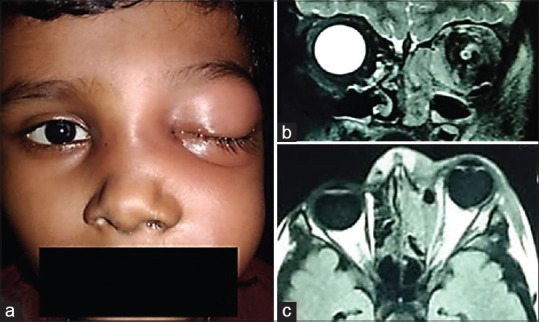
(a) Clinical external picture of an 8-year-old child with left orbital cellulitis with left-sided facial edema. (b and c) MRI coronal and axial views, T1-weighted image, showing medial subperiosteal abscess with coexisting medial ethmoid sinusitis. MRI = magnetic resonance imaging
Figure 4.
Series of images are as follows: axial T2 SPACE, post-contrast T1, Diffusion weighted Imaging, and Apparent diffusion coefficient map show thin peripheral rim-enhancing collection with central diffusion restriction in the intraorbital retro-ocular space. Patient is a known case of rheumatoid arthritis
It is the most trusted modality for detecting the complications of orbital infections, such as superior ophthalmic vein thrombosis, CST, loss of vision, meningitis, and intracranial abscess.
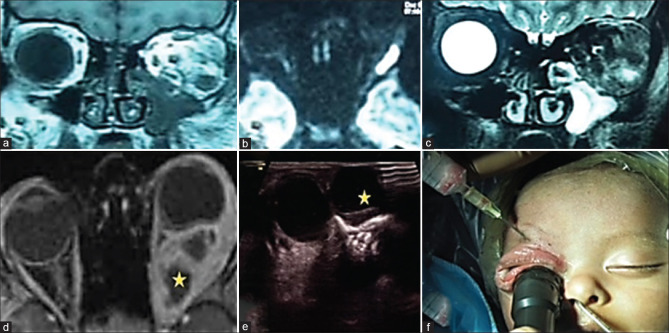
Orbital ultrasonography (USG) can also be used to locate an orbital abscess and perform USG-guided drainage.[15] An abscess shows low internal reflectivity on USG, a well-defined homogenous hypodense central area corresponding to necrosis with a wall that enhances with contrast on CT scan. The same is hypointense on T1 and hyperintense on T2-weighted image on MRI [Fig. 5].[19]
Figure 5.
(a and c) MRI orbit, coronal view, showing a well-circumscribed hypointense lesion on T1-weighted image and hyperintense lesion on T2-weighted image depicting a intraconal abscess in the inferolateral quadrant. (b) MRI orbit, axial view, diffusion-weighted image depicting a hyperintense signal, restricted diffusion along the lateral wall suggestive of an orbital abscess. (d) MRI orbits, axial view, T1-weighted, contrast-enhanced image depicts the classic multiseptate intraconal orbital abscess with rim enhancement. (e) Orbital mode B-scan ultrasonography. The star depicts a well-circumscribed hypoechoic lesion with a hyperechoic rim suggestive of a medial orbital abscess. (f) Peroperative clinical picture of a neonate depicting ultrasound-guided orbital abscess aspiration. MRI = magnetic resonance imaging
Pathophysiology
More than 90% of the cases of orbital cellulitis are sequela to paranasal sinusitis (specifically, ethmoid sinusitis).[20,21] The mediators of inflammation that are released in the nasal mucosa as a response to any viral infection cause congestion and swelling of the nasal passages. This, in turn, narrows the ostia, resulting in a block in the normal sinus drainage. The edematous nasal mucosa provides a conducive environment for the microorganisms indigenous to the sinus and upper respiratory tract to proliferate within the sinus. These then gain access to the orbit through thin bones of the orbital walls, dehiscences, or venous channels. Due to absence of the lymphatic system, the immune protection is only via the release of phagocytic cells locally by the orbital reticular tissue. Owing to the tight compartments, the intraorbital pressure is raised, which augments the virulence of the infecting organism. The complex cell surface of Gram-positive organisms as well as their toxins and enzymes provoke an inflammatory response, leading to early and extensive tissue necrosis. The necrotic material either undergoes consolidation to form abscess or spreads intracranially depending on the virulence of the infecting agent and the host defense mechanism.[22-24]
In the case of a polymicrobial infection of orbital cellulitis, especially in adults, the aerobes and anaerobes have synergistic effects. The aerobes create hypoxia, which helps the anaerobes to proliferate, and the anaerobes produce beta-lactamases, which protect the aerobes against beta-lactam antibiotics.[25]
Bacteriology of orbital cellulitis
Harris et al. reported that there was a very evident correlation between age and type of causative bacteria.[10]
In children
Infection in children <9 years is typical with a single aerobic organism.
The most common bacteria isolated in children are Streptococcus species, Staphylococcus aureus, and Haemophilus influenzae.[26]
Mukund et al.[2] reported that the most common microorganism causing orbital cellulitis in children was Staphylococcus species followed by streptococci. Less-common organisms were Propionibacterium, H. influenzae, Bacillus spp., and various fungi.
Since the early 2000s, the Streptococcus anginosus group has been an emerging pathogen in pediatric orbital infections.[26] Ambati et al.,[26] Mukund et al.,[2] and Hegde et al.[27] concurred with the observation that the incidence of H. influenzae as a cause for orbital cellulitis in the pediatric population has remarkably reduced since the advent of the H. influenzae type B (HiB) vaccine.[28,29]
In adults
With increasing age, particularly age > 15 years, the causative organisms are mixed aerobes and anaerobes (Bacteroides, Peptostreptococcus, Fusobacterium).[10]
Gram-positive bacteria, especially Staphylococcus and Streptococcus, are the most common organisms responsible for orbital cellulitis in adults. Usually, it is a polymicrobial infection because well-developed frontal sinuses are heavily colonized by aerobes as well as anaerobes.[29] S. aureus is a causative agent in about 30% of patients, and among them, the incidence of Multi drug resistant Staphylococcus aureus (MRSA) varies from 23% to 72%.[30] Orbital cellulitis resulting from infection of the maxillary sinus secondary to dental infections can be caused by microorganisms indigenous to the mouth, including anaerobes, commonly Bacteroides species.
Laboratory workup
It is recommended to perform pus culture from open wounds or abscesses, nasal swabs, purulent material from sinuses, as well as antimicrobial susceptibility testing, along with blood cultures, for initiating specific antibiotic therapy.
The purulent material should be collected using sterile cotton or calcium alginate swabs or aspirated into a sterile syringe. A sterile universal container may also be used. In situations where samples can be split, one portion should also be placed in pre-reduced (PRAS) media. The collected materials are subjected to direct microscopy as soon as possible using Gram’s stain for immediate guidance for empirical treatment. Culture and antibiotic susceptibility tests are performed by either conventional or automated methods (e.g., Vitek), keeping both aerobes and anaerobes in mind. Based on the susceptibility reports, targeted antibiotic therapy can be started for better resolution of infection.
Blood cultures are appropriate in the background of septicemia, and repeat collections are recommended. However, some studies have reported that blood cultures show low positivity due to previous initiation of antibiotic therapy.[2,31]
Management
Orbital cellulitis can pose a grave danger to a patient’s eye, vision, and also life, if not diagnosed and treated in time. Most patients presenting with preseptal cellulitis can be managed with oral antibiotics given for 7–10 days, along with anti-inflammatory medications.[32,33] Patients must be observed for any worsening of signs, which may warrant a need for imaging and intravenous (IV) antibiotics. Treatment of orbital cellulitis consists of both medical and surgical interventions, depending upon the presenting clinical and radiological features of the patient. They should preferably be admitted to the hospital for IV antibiotics and have their clinical signs monitored at least twice a day or more frequently in complicated cases.[34] Management must also include attention and due care for any concurrent condition like sinusitis, diabetes, or immunosuppression.[33]
There has been a generally widely accepted practice of using a broad-spectrum antibiotic coverage for Gram-positive and Gram-negative organisms as the empirical first-line therapy at presentation, even before any culture sensitivity of the organisms is available. Antibiotics against anaerobes are also preferred in the initial regimen by some clinicians. Lee et al.[31] noted that greater than 75% of the community-acquired Staphylococcus infections are methicillin resistant. As such, empiric therapy with vancomycin is their preferred first-line agent, along with cefotaxime and metronidazole or clindamycin for Gram-negative and anaerobic coverage.[33] In a study from the UK, empiric treatment with cefuroxime and metronidazole is suggested.[35] Chaudhry et al.[31] reported the use of cephalosporins and aminoglycosides as the commonest empiric therapy.[35] An increasing trend toward resistance to fluoroquinolones has been reported recently in one study.[7]
The authors prefer to start empiric treatment in patients with orbital cellulitis with a combination of a third-generation cephalosporin like ceftriaxone and an aminoglycoside like amikacin. Antibiotics can be changed if precise culture sensitivity information is available from sinuses or orbital abscess.[33,36] IV antibiotics are usually required for 1–2 weeks, followed by oral antibiotics for another 1–2 weeks depending upon the clinical response.[37]
In children, orbital cellulitis usually presents with infection caused by a single aerobic organism and shows a good response to medical therapy, in contrast to adults in whom multi-pathogen disease as well as a need for surgical intervention are common.[19,35]
Adjunctive use of steroids in patients with orbital cellulitis remains controversial. Steroids may reduce the tissue damage and toxic effects of inflammatory mediators. A recent meta-analysis has shown that the use of steroids significantly reduces hospital stay and duration of IV antibiotics in orbital cellulitis if initiated early, without any significant adverse effect.[38] A recent systematic review has pointed to insufficient evidence to conclude the use of corticosteroids in the treatment of orbital cellulitis and emphasized the need for high-quality randomized controlled trials to allow improved decision-making in this regard.[39] However, if one chooses to use steroids, they must be administered only after visible clinical improvement starts with IV antibiotics and if the underlying metabolic abnormality permits. Steroids must be avoided in immunocompromised, uncontrolled diabetics and in cases of fungal orbital cellulitis for obvious reasons.
Garcia and Harris[10] found nearly 93% response to nonsurgical management of pediatric SPAs, a potential complication of orbital cellulitis unless the patient had one of the following criteria indicative of the need for surgery: children older than 9 years of age, presence of frontal sinusitis, non-medial location of SPA, large SPA, suspicion of anaerobic subperiosteal infection, recurrence of SPA after the previous drainage, evidence of chronic sinusitis, acute optic nerve or retinal compromise, and infection of dental origin.[40] An SPA size of more than 1250 ml, regardless of patient age, was found to be predictive for surgical intervention.[41] The criteria for surgery are not so well established in adults. However, adults do better with early surgery more often, whether it is for concurrent sinusitis, SPA, or orbital abscess.[33,42]
Other factors warranting surgical treatment include the presence of a retained foreign body, an identified dental source of the infection, the presence of intracranial complications, and large abscesses.[31,34,35]
Prompt neurological consultation must be taken in patients with intracranial complications and brain abscesses. Broad-spectrum antibiotics including those for anaerobes that show good cerebrospinal fluid (CSF) penetration, such as penicillin, chloramphenicol, third-generation cephalosporins, and metronidazole, are preferred.[43,44] Anticoagulants may also be used for patients with CST to prevent further thrombosis and dissolve the clot.[45]
Around 3% of sinusitis cases will progress to orbital cellulitis, with 60% of orbital cellulitis cases being secondary to sinusitis.[10] The principles of surgical management are drainage of any pus and establishment of ventilation to the sinus. If orbital cellulitis has developed secondary to an acute sinus infection, the operative field is likely inflamed and very hemorrhagic, potentially making endoscopic surgery much more difficult than in the presence of chronic sinusitis alone. The best approach to drain orbital collections remains a current controversy. Advocates of endoscopic surgery suggest that endoscopic ethmoidectomy with the removal of the lamina papyracea and pernasal drainage of the orbital abscess is appropriate. The advantages of an endoscopic approach include avoiding facial scarring, ventilating the sinuses endonasally by operating on the osteomeatal complex, less postoperative orbital edema, a shorter hospital stay, and the absence of possible wound complications such as stitch abscesses.[45] While performing endonasal drainage, the surgeon must be prepared to convert it to external drainage if required and it is advised that patients and relatives appropriately consent prospectively for both approaches.
Conclusion
The incidence of orbital cellulitis has been reported to be more during winter, probably due to the increased incidence of sinusitis in cold weather. The reported incidence of subperiosteal abscess is 15% in children – the close anatomic relationship of the orbit to the paranasal sinus predisposes to the spread of infection via the ophthalmic venous system.[25,46-48] Surgical procedures like orbital decompression, dacryocystorhinostomy, eyelid surgery, strabismus surgery, retina surgery, and intraocular surgery can also be precipitating factors for orbital cellulitis.[49] Odontogenic (i.e., tooth-related) causes of orbital cellulitis, although very rare, tend to have rapid progression, leading to blindness.[48,50]
The etiological agents causing orbital cellulitis are usually bacterial. A high index of suspicion should be kept in mind, especially in immunocompromised patients, where the etiological agent could be fungus, the most common being Mucor or Aspergillus. Delay in proper diagnosis may lead to a fatal prognosis.[15] Parenteral antibiotics are the treatment of choice. A combination of cefotaxime and amikacin is the author’s treatment of choice. In cases of odontogenic infections or suspicion of anaerobes, we need to add metronidazole. In addition to high doses and multiple antibiotics, need for systemic monitoring is essential to identify early intracranial spread. In addition, if a patient fails to respond to appropriate measures for a presumed infection, the diagnosis must be reconsidered.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Murphy C, Livingstone I, Foot B, Murgatroyd H, MacEwen CJ. Orbital cellulitis in Scotland: Current incidence, etiology, management, and outcomes. Br J Ophthalmol. 2014;98:1575–8. doi: 10.1136/bjophthalmol-2014-305222. [DOI] [PubMed] [Google Scholar]
- 2.Mukund B, Chaudhary S, Bhat V, Vineet V, Adhikari KM. Orbital cellulitis-Incidence, management, and outcome from coastal hospitals. J Pediatr Crit Care. 2019;6:25–30. [Google Scholar]
- 3.Pandian DG, Babu RK, Chaitra A, Anjali A, Rao VA, Srinivasan R. Nine years'review on preseptal and orbital cellulitis and emergence of community-acquired methicillin-resistant Staphylococcus aureus in a tertiary hospital in India. Indian J Ophthalmol. 2011;59:431–5. doi: 10.4103/0301-4738.86309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Israele V, Nelson JD. Periorbital and orbital cellulitis. Pediatr Infect Dis J. 1987;6:404–10. doi: 10.1097/00006454-198704000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Chaudhry IA, Al-Rashed W, Arat YO. The hot orbit: Orbital cellulitis. Middle East Afr J Ophthalmol. 2012;19:34–42. doi: 10.4103/0974-9233.92114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chandler JR, Langenbrunner DJ, Stevens ER. The pathogenesis of orbital complications in acute sinusitis. Laryngoscope. 1970;80:1414–28. doi: 10.1288/00005537-197009000-00007. [DOI] [PubMed] [Google Scholar]
- 7.El Mograbi A, Ritter A, Najjar E, Soudry E. Orbital complications of rhinosinusitis in the adult population: Analysis of cases presenting to a tertiary medical center over 13 years. Ann Otol Rhinol Laryngol. 2019;128:563–8. doi: 10.1177/0003489419832624. [DOI] [PubMed] [Google Scholar]
- 8.Krouschnabel EF. Orbital apex syndrome due to sinus infection. Laryngoscope. 1974;84:353–71. doi: 10.1288/00005537-197403000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Hornblass A, Herschorn BJ, Stern K, Grimes C. Orbital abscess. Surv Ophthalmol. 1984;29:169–78. doi: 10.1016/0039-6257(84)90202-9. [DOI] [PubMed] [Google Scholar]
- 10.Harris GJ. Subperiosteal abscess of the orbit: Age as a factor in the bacteriology and response to treatment. Ophthalmology. 1994;101:585–95. doi: 10.1016/s0161-6420(94)31297-8. [DOI] [PubMed] [Google Scholar]
- 11.Duke-Elder S, MacFaul PA. The ocular adnexa: Part 2. Lacrimal orbital and para orbital diseases. In: Duke-Elder S, editor. System of Ophthalmology. London: Henry Kimpton; 1974. pp. 859–89. [Google Scholar]
- 12.Schramm VL, Myres EN, Kennerdell JS. Orbital complications of acute sinusitis: Evaluation, management and outcome. ORL Digest. 1979;86:221–30. doi: 10.1177/019459987808600209. [DOI] [PubMed] [Google Scholar]
- 13.Mukherjee B, Raichura ND, Alam MS. Fungal infections of the orbit. Indian J Ophthalmol. 2016;64:337–45. doi: 10.4103/0301-4738.185588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lindsay RA, Weiss AH, Kelly JP, Anderson VC, Lindsay TH, Cabrera MT. Clinical outcomes in children with orbital cellulitis and radiographic globe tenting. Ophthalmic Plast Reconstr Surg. 2018;34:329–32. doi: 10.1097/IOP.0000000000000976. [DOI] [PubMed] [Google Scholar]
- 15.Tzelnick S, Soudry E, Raveh E, Gilony D. Recurrent periorbital cellulitis associated with rhinosinusitis in children: Characteristics, course of disease, and management paradigm. Int J Pediatr Otorhinolaryngol. 2019;121:26–8. doi: 10.1016/j.ijporl.2019.02.037. [DOI] [PubMed] [Google Scholar]
- 16.Basraoui D, Elhajjami A, Jalal H. Imaging of orbital cellulitis in children: About 56 cases. Pan Afr Med J. 2018;30:94. doi: 10.11604/pamj.2018.30.94.14672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alam MS, Backiavathy V, Noronha V, Mukherjee B. Orbital abscess: 20 years'experience at a tertiary eye care center. Orbit. 2022;41:751–8. doi: 10.1080/01676830.2021.2013901. [DOI] [PubMed] [Google Scholar]
- 18.Ferguson MP, McNab AA. Current treatment and outcome in orbital cellulitis. Aust N Z J Ophthalmol. 1999;27:375–9. doi: 10.1046/j.1440-1606.1999.00242.x. [DOI] [PubMed] [Google Scholar]
- 19.Jain A, Rubin P. Pediatric ophthalmology: A subspecialty perspective. Orbital cellulitis in children. Int Ophthalmol Clin. 2001;41:71–86. doi: 10.1097/00004397-200110000-00009. [DOI] [PubMed] [Google Scholar]
- 20.Weiss A, Friendly D, Eglin K, Chang M, Gold B. Bacterial periorbital and orbital cellulitis in childhood. Ophthalmology. 1983;90:195–203. doi: 10.1016/s0161-6420(83)34573-5. [DOI] [PubMed] [Google Scholar]
- 21.Hamilos DL. Chronic sinusitis. J Allergy Clin Immunol. 2000;106:213–27. doi: 10.1067/mai.2000.109269. [DOI] [PubMed] [Google Scholar]
- 22.Winstead W. Rhinosinusitis. Prim Care Clin Office Pract. 2003;30:137–54. doi: 10.1016/s0095-4543(02)00058-1. [DOI] [PubMed] [Google Scholar]
- 23.Hamed-Azzam S, Al Hashash I, Briscoe D, Rose GE, Verity DH. Common orbital infections ~State of the art ~Part I. J Ophthalmic Vis Res. 2018;13:175–82. doi: 10.4103/jovr.jovr_199_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nageswaran SN, Woods CR, Benjamin DK, Givner LB, Shetty AK. Orbital cellulitis in children. Pediatr Infect Dis J. 2006;25:695–9. doi: 10.1097/01.inf.0000227820.36036.f1. [DOI] [PubMed] [Google Scholar]
- 25.Aabideen KK, Munshi V, Kumar VB, Dean F. Orbital cellulitis in children: A review of 17 cases in the UK. Eur J Pediatr. 2007;166:1193–4. doi: 10.1007/s00431-006-0387-6. [DOI] [PubMed] [Google Scholar]
- 26.Ambati BK, Ambati J, Azar N, Stratton L, Schmidt EV. Periorbital and orbital cellulitis before and after the advent of Haemophilus influenzae type B vaccination. Ophthalmology. 2001;108:1514–5. doi: 10.1016/s0161-6420(00)00178-0. [DOI] [PubMed] [Google Scholar]
- 27.Hegde R, Sundar G. Orbital cellulitis- A review. TNOA J Ophthalmic Sci Res. 2017;55:211–9. [Google Scholar]
- 28.Liao S, Durand ML, Cunningham MJ. Sinogenic orbital and subperiosteal abscesses: Microbiology and methicillin-resistant Staphylococcus aureus incidence. Otolaryngol Head Neck Surg. 2010;143:3926. doi: 10.1016/j.otohns.2010.06.818. [DOI] [PubMed] [Google Scholar]
- 29.Aryasit O, Aunruan S, Sanghan N. Predictors of surgical intervention and visual outcome in bacterial orbital cellulitis. Medicine (Baltimore) 2021;100:e26166. doi: 10.1097/MD.0000000000026166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Watts P. Preseptal and orbital cellulitis in children. Paediatr Child Health. 2016;26:1–8. [Google Scholar]
- 31.Lee S, Yen MT. Management of preseptal and orbital cellulitis. Saudi J Ophthalmol. 2011;25:21–9. doi: 10.1016/j.sjopt.2010.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Howe L, Jones NS. Guidelines for the management of periorbital cellulitis/abscess. Clin Otolaryngol Allied Sci. 2004;29:725–8. doi: 10.1111/j.1365-2273.2004.00889.x. [DOI] [PubMed] [Google Scholar]
- 33.Chaudhry IA, Shamsi FA, Elzaridi E, Al-Rashed W, Al-Amri A, Al-Anezi F, et al. Outcome of treated orbital cellulitis in a tertiary eye care center in the middle East. Ophthalmology. 2007;114:345–54. doi: 10.1016/j.ophtha.2006.07.059. [DOI] [PubMed] [Google Scholar]
- 34.Crosbie RA, Nairn J, Kubba H. Management of paediatric periorbital cellulitis: Our experience of 243 children managed according to a standardised protocol 2012-2015. Int J Pediatr Otorhinolaryngol. 2016;87:134–8. doi: 10.1016/j.ijporl.2016.06.025. [DOI] [PubMed] [Google Scholar]
- 35.Kloek CE, Rubin PA. Role of inflammation in orbital cellulitis. Int Ophthalmol Clin. 2006;46:57–68. doi: 10.1097/00004397-200604620-00007. [DOI] [PubMed] [Google Scholar]
- 36.Kim BY, Bae JH. Role of systemic corticosteroids in orbital cellulitis: A meta-analysis and literature review. Braz J Otorhinolaryngol. 2022;88:257–62. doi: 10.1016/j.bjorl.2021.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kornelsen E, Mahant S, Parkin P, Ren LY, Reginald YA, Shah SS, et al. Corticosteroids for periorbital and orbital cellulitis. Cochrane Database Syst Rev. 2021;4:CD013535. doi: 10.1002/14651858.CD013535.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Garcia GH, Harris GJ. Criteria for nonsurgical management of subperiosteal abscess of the orbit: 1988 –1998. Ophthalmology. 2000;107:1454–8. doi: 10.1016/s0161-6420(00)00242-6. [DOI] [PubMed] [Google Scholar]
- 39.Todman MS, Enzer YR. Medical management versus surgical intervention of pediatric orbital cellulitis: The importance of subperiosteal abscess volume as a new criterion. Ophthalmic Plast Reconstr Surg. 2011;27:255–9. doi: 10.1097/IOP.0b013e3182082b17. [DOI] [PubMed] [Google Scholar]
- 40.Meara DJ. Sinonasal disease and orbital cellulitis in children. Oral Maxillofac Surg Clin North Am. 2012;24:487–96. doi: 10.1016/j.coms.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 41.Reynolds DJ, Kodsi SR, Rubin SE, Rodgers IR. Intracranial infection associated with preseptal and orbital cellulitis in the pediatric patient. J AAPOS. 2003;7:413–7. doi: 10.1016/j.jaapos.2003.09.013. [DOI] [PubMed] [Google Scholar]
- 42.Barling RW, Selkon JB. The penetration of antibiotics into cerebrospinal fluid and brain tissue. J Antimicrob Chemother. 1978;4:203–27. doi: 10.1093/jac/4.3.203. [DOI] [PubMed] [Google Scholar]
- 43.Press CA, Lindsay A, Stence NV, Fenton LZ, Bernard TJ, Mirsky DM. Cavernous sinus thrombosis in children: Imaging characteristics and clinical outcomes. Stroke. 2015;46:2657–60. doi: 10.1161/STROKEAHA.115.009437. [DOI] [PubMed] [Google Scholar]
- 44.Migirov L, Yakirevitch A, Bedrin L, Wolf M. Endoscopic sinus surgery for medial orbital subperiosteal abscess in children. J Otolaryngol Head Neck Surg. 2009;38:504–8. [PubMed] [Google Scholar]
- 45.Rajeshwari N, Savitha A. Orbital cellulitis: Early intervention saves vision. Int J Contemp Pediatr. 2020;7:1–7. [Google Scholar]
- 46.Rahbar R, Robson CD, Petersen RA, DiCanzio J, Rosbe KW, McGill TJ, et al. Management of orbital subperiosteal abscess in children. Arch Otolaryngol Head Neck Surg. 2001;127:282–6. doi: 10.1001/archotol.127.3.281. [DOI] [PubMed] [Google Scholar]
- 47.Bergin DJ, Wright JE. Orbital cellulitis. Br J Ophthalmol. 1986;70:174–8. doi: 10.1136/bjo.70.3.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Sharma V, Chhangte L, Joshi V. A Case of odontogenic orbital cellulitis causing blindness: A case report. Delhi J Ophthalmol. 2013;24:102–5. [Google Scholar]
- 49.Sharma A, Ingole S, Deshpande M, Ranadive P, Sharma S, Chavan A. An insight on management of odontogenic orbital infections: Report of two cases. J Oral Med Oral Surg. 2021;27:41. [Google Scholar]
- 50.Suneetha N, Battu RR, Thomas R K, Bosco A. Orbital abscess: Management and outcome. Indian J Ophthalmol. 2000;48:129–34. [PubMed] [Google Scholar]