Abstract
Purpose:
Age-related macular degeneration (AMD) is a common cause of blindness, residual damage to macular area in spite of treatment necessitates visual rehabilitation by means of low-vision aids (LVAs).
Methods:
Thirty patients suffering from different stages of AMD requiring LVAs were included in this prospective study. Patients with nonprogressive, adequately treated AMD were enrolled over a 12-month period, prescribed requisite LVAs and followed-up for a minimum 1-month period. Before and after provision of LVAs, near work efficiencies were evaluated by calculating reading speed as words per minute (wpm) under both photopic and mesopic light conditions, and impact of poor vision on activities of daily living (ADL) was quantified by modified standard questionnaire based on Nhung X et al. questionnaire.
Results:
Of the 30 patients mean studied with mean age of 68 ± 10 years, 20 patients (66.7%) had dry AMD in better eye and 10 (33.3%) had wet AMD. Post-LVA, near visual acuity improved significantly and all cases were able to read some letters on near vision chart with an average improvement of 2.4 ± 0.96 lines. The different LVAs prescribed were high plus reading spectacles (up to 10 D) in 23.3%, hand-held magnifiers in 53.3%, base in prisms in 10%, stand held magnifiers in 6.7%, and bar and dome magnifiers in 3.3%.
Conclusion:
LVAs are effective in visual rehabilitation in patients with AMD. Self-reported reduction in visual dependency and improvement in vision-related quality of life post use of aids corroborated perceived benefit.
Keywords: Age-related macular degeneration, low-vision aids, visual rehabilitation
Age-related macular degeneration (AMD) is a common cause of blindness.[1] accounting for 8.7% visual impairment among elderly patients above the age of 65 years.[2]
The diseases manifest most commonly as dry/atrophic AMD, a slowly progressive type that results in moderate-to-severe visual loss. The less common wet/exudative type accounts for 10% of AMD cases but is responsible for 90% of AMD blindness with visual loss occurring rapidly and extensively.[3] Since macular degeneration involves loss of central vision, it has a huge impact on vision-related activities, namely, difficulty in seeing straight ahead, reading, identifying people faces/colors, and reading.[4]
Despite effective treatment options available, which halt progression of the disease, residual damage of critical macular areas often necessitates low-vision rehabilitation (LVR) modalities in these elderly patients. Effective LVR improve quality of life (QoL) for these patients by maintaining and improving reading ability,[5] and minimizing disability and motility, thereby, affording an increase in independence, communication, and mental agility.[6]
Effective use of low-vision aids (LVAs) entails maximal employment of remaining eyesight by using measures of optical aids, adequate illumination, and contrast and ergonomic head and hand movements.[7] Most LVAs enhance visual performance by making the image bigger, brighter, and clearer. Options for LVAs range from optical (aspheric glasses and magnifiers—hand-held/stand held/dome) to nonoptical (large print books/reading stand/illumination devices). These aids are extremely important in enabling the elderly maintain independent living in home environments and a dignified life during outdoor activities like social interaction, shopping, banking, traveling, and entertainment. In a developing country scenario where most health resources and endeavor are focused on productive age group, the visually handicapped low-vision elderly patients are often relegated to the back shelf.
The current study was aimed to determine both effectiveness and feasibility of LVAs use in such a population of a metropolitan city of a developing country.
Methods
Thirty patients suffering from different stages of AMD attending outpatient department of a tertiary referral hospital of North India requiring LVAs were included in this prospective study. Patients with nonprogressive, adequately treated AMD in seventh–eight decade were enrolled over a 12-month period, prescribed requisite LVAs and followed-up for a minimum 1-month period to evaluate effectivity and acceptance of the aid. Patients with coexisting diabetic retinopathy, advanced glaucoma, pathological myopia, amblyopia, and those with gross heads tremors/crippling arthritis were excluded.
All patients underwent a standardized ophthalmological examination including distance and near best-corrected visual acuity (VA), refraction, color vision, contrast sensitivity, dilated retinal examination, and baseline demographics like patient's age, gender, diagnosis, occupation, and monthly income. According to patient's needs, required magnification was calculated for near vision. Dioptric power (D) requirement was calculated by Kestenbaum formula, which calculates required add as “inverse of distance VA,” e.g., for Snellen acuity of 3/60, reciprocal of 60/3 being 20, the dioptric requirement of LVAs would be 20 D. For a 20 D power, magnification is calculated by formula D = 4 multiplied by x, e.g., for 20 D, the value of x would be 5, and a 5x/20D aid would be required.
Near vision of these low-vision patients was evaluated by a near vision reading chart at 25 cm distance under standardized illumination. Depending on magnification requirement, the appropriate LVAs were tested and prescribed after requisite training.
Before and after provision of LVAs, near work efficiency was evaluated by calculating reading speed as words per minute (wpm) under both photopic and mesopic light conditions simulating patient's home surroundings using standardized reading texts and with practical reading material like newspaper print or grocery bill.
A modified standard questionnaire, based on Nhung X et al. questionnaire and altered according to regional requirements, was used to quantify impact of poor vision on activities of daily living (ADL) like reading, navigating stairs, watching television, signing checks, etc.[8] Questionnaire composed of ten questions grouped into four categories. First category consisted of three subscales addressing quality of vision in terms of reading ability (three questions). Second category reflected outdoor navigational ability in walking and use of steps (two questions). Third category related to indoor navigation and participation in day-to-day activities (four questions), and fourth category assessed vision-related dependency on others (one question) [Annexure 1].
Annexure 1.
Details of items in the questionnaire used in the present study (Annexure 1)
| How difficult to you find it to read a newspaper normal print size? | Not difficult at all 1 | Somewhat difficult 2 | Moderately difficult 3 | Extremely difficult 4 | Unable to read/Discontinued reading 5 |
| How difficult you find to read small numbers in diary/medicine bottle? | Not difficult at all 1 | somewhat difficult 2 | Moderately difficult 3 | Extremely difficult 4 | Unable to read/Discontinued reading 5 |
| How difficult you find to read street sign or name of stores, bus numbers? | Not difficult at all 1 | Somewhat difficult 2 | Moderately difficult 3 | Extremely difficult 4 | Unable to read/Discontinued reading 5 |
| How difficult do you find to walk in the street in the park on your own? | Not difficult at all 1 | somewhat difficult 2 | Moderately difficult 3 | Extremely difficult 4 | Unable to read/Discontinued reading 5 |
| How difficult do you find to walk in your own home in the evening and in day light? | Not difficult at all 1 | somewhat difficult 2 | Moderately difficult 3 | Extremely difficult 4 | Unable to read/Discontinued reading 5 |
| How difficult do you find to watch your soap operas on television? | Not difficult at all 1 | somewhat difficult 2 | Moderately difficult 3 | Extremely difficult 4 | Unable to read/Discontinued reading 5 |
| How difficult you find to do thread work, sewing material? | Not difficult at all 1 | somewhat difficult 2 | Moderately difficult 3 | Extremely difficult 4 | Unable to read/Discontinued reading 5 |
| How difficult you find in recognizing people you know in the street or in a room? | Not difficult at all 1 | somewhat difficult 2 | Moderately difficult 3 | Extremely difficult 4 | Unable to read/Discontinued reading 5 |
| How difficult you find it to climb stairs or steps in dim light? | Not difficult at all 1 | somewhat difficult 2 | Moderately difficult 3 | Extremely difficult 4 | Unable to read/Discontinued reading 5 |
| Do you require help from others because of your visual status? | Occasionally 1 | Sometimes 2 | Often 3 | Most of the times 4 | Always 5 |
Responses were scored on an ascending scale of 1–5 with 1 denoting no difficulty and 5 denoting total inability to perform an activity or discontinuation of work due to poor vision. After provision and use of LVAs for one month, the responses were again elicited and difference in vision-related QoL was evaluated.
Results
Of the 30 patients mean studied with mean age of 68 ± 10 years, 20 patients (66.7%) had dry AMD in better eye and 10 (33.3%) had wet AMD.
Average best-corrected distance VA of better eye was 1.6+/-0.5 LogMAR (range: 0.5–3). Sixteen patients (53%) had VA better than <1 (20/200 Log MAR/6/60 Snellen) with remaining 14 patients (47%) having vision poorer than >1 in better eye.
Near VA tested with standard near vision chart was divided into three groups for ease of analysis. Near VA between N/6 and N/12 was graded as better, between N/36 and N/18 as moderate, and <N/36 as poor. Around one-third patients (10) were unable to read any letter on this chart.
Post-LVA, near VA improved significantly and all cases were able to read some letters on near vision chart with an average improvement of 2.4 ± 0.96 lines [Fig. 1].
Figure 1.
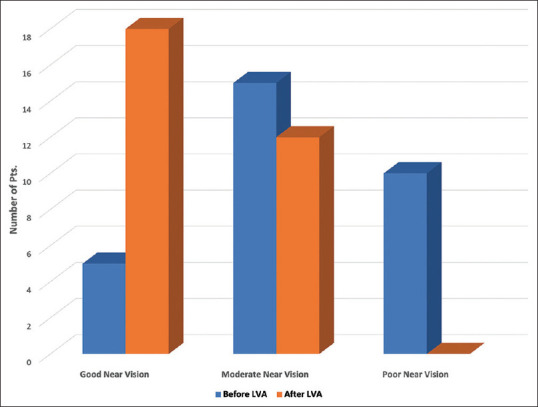
The number of patients in each category after and before LVAs
The different LVAs used according to patient's visual requirement and acceptability were high plus reading spectacles (up to 10 D) in seven patients (23.3%), hand-held magnifiers in 16 (53.3%), base in prisms in 3 (10%), stand held magnifiers in 2 (6.7%), and bar and dome magnifiers in 1 (3.3%) patient each [Fig. 2].
Figure 2.
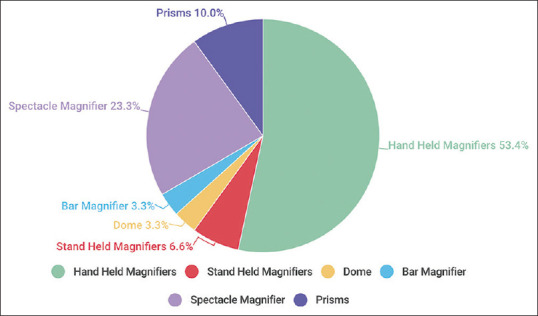
Distribution of different LVAs
The mean magnification required was 4.5 ± 3.7× with a range of 1.5–15×. As expected, a negative correlation with initial VA was seen implying lesser magnification requirement for better initial VA. A significant correlation was also noted between VA and eccentric fixation with patients of eccentric fixation having a poorer near vision.
Mean reading speed under photopic conditions was 29.17 ± 30 wpm, which improved significantly to 70 ± 43 after the use of LVAs and mesopic reading speed from 23.7 ± 24.9 to 59.9 ± 44.8 wpm with both increases attaining statistical significance at P < 0.0001 (Wilcoxon signed rank test). Reading ability was divided into four groups based on Trauzettel–Klosinski classification[9] as depicted in Table 1.
Table 1.
Trauzettel–Klosinski classification and Improvement in reading ability before and after LVAs
| Reading ability | Before LVA | After LVA |
|---|---|---|
| Fluent reading (>70 wpm) | 4 (13.3%) | 15 (50%) |
| Struggling reading (30–70 wpm) | 7 (23.3%) | 9 (30%) |
| Spot reading (11–30 wpm) | 7 (23.3%) | 6 (20%) |
| No reading (<10 wpm) | 12 (40%) | 0 (0%) |
Reading speed was evaluated by reading of standard newspaper text fluently. Prior to LVA use, only 4 (13.3%) patients were able to read the standard newspaper text fluently, 7 (23.3%) had struggling reading with 19 (63.4%) only managing spot reading (newspaper headlines) or no reading. After LVA, reading speed improved with 15 (50%) patients doing fluent reading with 15 (50%) patients struggling reading as shown in Table 1.
Reading ability was achieved in 30 (100%) of patients with a mean reading speed of 70 ± 43 wpm after the use of LVAs compared to only 18 (59.9%) who were able to read before with a mean reading speed of 29 ± 30, which amounted to increased reading speed of 58.5%.
Quality of life assessment
All patients were assessed for their vision-related QOL as per modified questionnaire of Nhung et al.[8] Responses to this questionnaire showed that 66.7% patients faced great difficulty and often needed help in their day-to day activities due to poor vision, with 26.7% facing moderate difficulties and frequently needing help in ADL. The use of LVAs resulted in reduced dependency and improved QOL for 7 patients, with 17 patients (56.7%) still reporting moderate difficulties. Six patients showed poor response with LVAs [Fig. 3].
Figure 3.
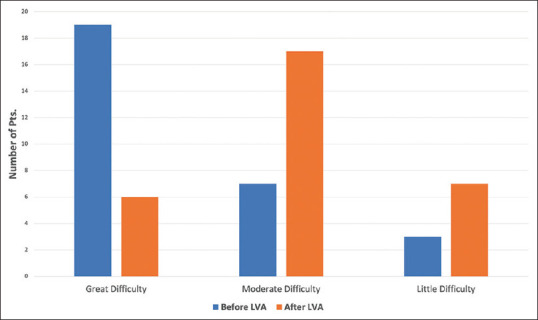
Difficulty grades pre- and post-prescription of LVAs
Discussion
Increased life expectancy has led to an increase in number of individuals affected with AMD with a global prevalence of 8.7% and 1.1% for the Indian subcontinent.[2] The projected number of people are predicted to rise from 196 million in 2020 to 288 million in 2040.[10] Low-vision due to AMD causes central scotoma, which impairs most ADL like reading newsprint/religious books/medicine labels, street signs, currency identification, cooking, and other household chores. In these patients, the peripheral vision has to be utilized for reading and other tasks and a larger print size is required for peripheral viewing.[9,11] In a developing country context, most of low-vision elderly do not have recourse to low-vision services both due to sparse service delivery and lack of awareness in eye care professionals. AMD is associated with, impaired reading ability, thereby hindering social participation by affecting communication, independence and cognitive agility, thereby affecting QOL. Hassell et al.[12] reported effect of the severity of AMD on QOL with difficulty in reading and other activities like mobility and social interaction.
Optical visual aids like high plus reading additions and magnifiers were sufficient to perform visual rehabilitation in almost all of our patients. Hand magnifiers prescribed in 53% patients were found to be extremely useful for spot reading due to their light weight, ease of transport, and relatively larger field of vision but required short working distance and often caused neck pain. Stand magnifiers requiring a longer working distance and were perceived to be more acceptable in very elderly, emaciated patients having hand/head tremors with and limited mobility.
Electronic closed circuit television aids were not acceptable in our subgroup of patients belonging to poorer socioeconomic strata due to expense and bulk, which limited them to a single location for reading.
An improvement in QOL was observed in 23% (7/30) patients. Patients in severe difficulty criteria (66.7%) reported more improvement in QOL with use of LVAs. Kaltenegger et al.[13] reported improvement in cognitive status and QOL by the use of LVAs.
Limitations and strengths
Inability to demonstrate presence of an absolute central scotoma and its extent by perimetry or scanning laser ophthalmoscopy. A linear relationship exists between reading speed, size of scotoma, and fixation locus.[14-16] As most of study patients benefited in reading by LVAs without recourse to training for eccentric viewing, it may be assumed that they did not have an absolute central scotoma. A smaller sample size was the limitation of the study.
Change in fixation stability causes almost 50% variability in reading speed.[17] For better reading performance, correlation between fixation locus and size of the scotoma need to be considered. This could not be done in the study.
Study strengths were used for newspaper print to assess reading performance and to evaluate impact on ADL. Reading speed taken as an indicator, in the study, is a more relevant and useful evidence of visual rehabilitation over single letter identification. Improvement in QOL indices reflected positive impact of enhanced visual function in daily life activities.
Conclusion
The study confirms effectiveness of visual rehabilitation with LVAs in patients of AMD. Self-reported reduction in visual dependency and improvement in vision-related QOL post use of aids and corroborated perceived benefit.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Trautner C, Haastert B, Richter B, Berger M, Giani G. Incidence of blindness in southern Germany due to glaucoma and degenerative conditions. Invest Ophthalmol Vis Sci. 2003;44:1031–4. doi: 10.1167/iovs.02-0304. [DOI] [PubMed] [Google Scholar]
- 2.Khan SA, Das T, Kumar SM, Nutheti R. Low vision rehabilitation in patients with age-related macular degeneration at a tertiary eye care centre in southern India. Clin Exp Ophthalmol. 2002;30:404–10. doi: 10.1046/j.1442-9071.2002.00569.x. [DOI] [PubMed] [Google Scholar]
- 3.Resnikoff S, Pascolini D, Etya’ale D, Kocur I, Pararajasegaram R, Pokharel GP, et al. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82:844–51. [PMC free article] [PubMed] [Google Scholar]
- 4.Kini MM, Leibowitz HM, Colton T, Nickerson RJ, Ganley J, Dawber TR. Prevalence of senile cataract, diabetic retinopathy, senile macular degeneration, and open-angle glaucoma in the Framingham eye study. Am J Ophthalmol. 1978;85:28–34. doi: 10.1016/s0002-9394(14)76661-9. [DOI] [PubMed] [Google Scholar]
- 5.Nguyen NX, Trauzettel-Klosinski S. Effectiveness of magnifying low vision aids in patients with age-related macular degeneration. Neuro-Ophthalmology. 2009;33:115–9. doi: 10.1111/j.1755-3768.2008.01423.x. [DOI] [PubMed] [Google Scholar]
- 6.Massof RW. A systems model for low vision rehabilitation. II. Measurement of vision disabilities. Optom Vis Sci. 1998;75:349–73. doi: 10.1097/00006324-199805000-00025. [DOI] [PubMed] [Google Scholar]
- 7.Macnamara A, Chen CS, Davies A, Sloan C, Loetscher T. Low vision devices for age-related macular degeneration: A systematic review. Disabil Rehabil Assist Technol. 2021:1–13. doi: 10.1080/17483107.2021.1966523. doi: 10.1080/17483107.2021.1966523. [DOI] [PubMed] [Google Scholar]
- 8.Nguyen NX, Besch D, Bartz-Schmidt K, Gelisken F, Trauzettel-Klosinski S. Reading performance with low-vision aids and vision-related quality of life after macular translocation surgery in patients with age-related macular degeneration. Acta Ophthalmol Scand. 2007;85:877–82. doi: 10.1111/j.1600-0420.2007.00963.x. [DOI] [PubMed] [Google Scholar]
- 9.Trauzettel-Klosinski S, Dieling C, Pietsch B. The influence of visual field defects and other clinical parameters on reading performance: A retrospective study in a low vision population. Visual Impairment Research. 2003;5:83–100. [Google Scholar]
- 10.Wong WL, Su X, Li X, Cheung CM, Klein R, Cheng CY, et al. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: A systematic review and meta-analysis. Lancet Glob Health. 2014;2:e106–16. doi: 10.1016/S2214-109X(13)70145-1. doi: 10.1016/s2214-109x(13)70145-1. [DOI] [PubMed] [Google Scholar]
- 11.Rubin GS. Vision rehabilitation for patients with age-related macular degeneration. Eye (Lond) 2001;15:430–5. doi: 10.1038/eye.2001.148. [DOI] [PubMed] [Google Scholar]
- 12.Hassell JB, Lamoureux EL, Keeffe JE. Impact of age related macular degeneration on quality of life. Br J Ophthalmol. 2006;90:593–6. doi: 10.1136/bjo.2005.086595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaltenegger K, Kuester S, Altpeter-Ott E, Eschweiler GW, Cordey A, Ivanov IV, et al. Effects of home reading training on reading and quality of life in AMD - A randomized and controlled study. Graefes Arch Clin Exp Ophthalmol. 2019;257:1499–512. doi: 10.1007/s00417-019-04328-9. [DOI] [PubMed] [Google Scholar]
- 14.Cummings RW, Whittaker SG, Watson GR, Budd JM. Scanning characters and reading with a central scotoma. Am J Optom Physiol Opt. 1985;62:833–43. doi: 10.1097/00006324-198512000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Seiple W, Szlyk JP, McMahon T, Pulido J, Fishman GA. Eye-movement training for reading in patients with age-related macular degeneration. Invest Ophthalmol Vis Sci. 2005;46:2886–96. doi: 10.1167/iovs.04-1296. [DOI] [PubMed] [Google Scholar]
- 16.Legge GE, Ross JA, Isenberg LM, LaMay JM. Psychophysics of reading. Clinical predictors of low-vision reading speed. Invest Ophthalmol Vis Sci. 1992;33:677–87. [PubMed] [Google Scholar]
- 17.Nguyen NX, Weismann M, Trauzettel-Klosinski S. Improvement of reading speed after providing of low vision aids in patients with age-related macular degeneration. Acta Ophthalmol. 2009;87:849–53. doi: 10.1111/j.1755-3768.2008.01423.x. [DOI] [PubMed] [Google Scholar]


