Abstract
Objectives:
Notification by emergency medical services (EMS) to the destination hospital of an incoming suspected stroke patient is associated with timelier in-hospital evaluation and treatment. Current data on adherence to this evidence-based best practice are limited, however. We examined the frequency of EMS stroke prenotification in North Carolina by community socioeconomic status (SES) and rurality.
Methods:
Using a statewide database of EMS patient care reports, we selected 9-1-1 responses in 2019 with an EMS provider impression of stroke or documented stroke care protocol use. Eligible patients were 18 years old and older with a completed prehospital stroke screen. Incident street addresses were geocoded to North Carolina census tracts and linked to American Community Survey socioeconomic data and urban–rural commuting area codes. High, medium, and low SES tracts were defined by SES index tertiles. Tracts were classified as urban, suburban, and rural. We used multivariable logistic regression to estimate independent associations between tract-level SES and rurality with EMS prenotification, adjusting for patient age, sex, and race/ethnicity; duration of symptoms; incident day of week and time of day; 9-1-1 dispatch complaint; EMS provider primary impression; and prehospital stroke screen interpretation.
Results:
The cohort of 9527 eligible incidents was mostly at least 65 years old (65%), female (55%), and non-Hispanic White (71%). EMS prenotification occurred in 2783 (29%) patients. Prenotification in low SES tracts (27%) occurred less often than in medium (30%) and high (32%) SES tracts. Rural tracts had the lowest frequency (21%) compared with suburban (28%) and urban (31%) tracts. In adjusted analyses, EMS prenotification was less likely in low SES (vs high SES; odds ratio 0.76, 95% confidence interval 0.67–0.88) and rural (vs urban; odds ratio 0.64, 95% confidence interval 0.52–0.77) tracts.
Conclusions:
Across a large, diverse population, EMS prenotification occurred in only one-third of suspected stroke patients. Furthermore, low SES and rural tracts were independently associated with a lower likelihood of prehospital notification. These findings suggest the need for education and quality improvement initiatives to increase EMS stroke prenotification, particularly in underserved communities.
Keywords: disparities, emergency medical services, rural, stroke
Stroke is defined as a neurological deficit secondary to an acute injury to the brain.1 In the United States, 1 in every 19 deaths is caused by stroke.2 Furthermore, stroke is a leading cause of permanent disability.3 Stroke also contributes to a significant cost burden on the US healthcare system, with an estimated $53 billion spent on stroke-related care between 2017 and 2018.4 First identified in the 1940s, the “Stroke Belt” is a multi-state region in the southeastern United States with elevated rates of stroke morbidity and mortality.5 Limited access to acute stroke care is considered an important contributor to this disproportionate burden, especially in rural and other underserved areas.
Evidence-based acute stroke therapies, such as intravenous thrombolytics and mechanical thrombectomy, are extremely time sensitive, with treatment delays leading to worse outcomes.6 The use of emergency medical services (EMS) is associated with improved outcomes for stroke patients secondary to more prompt emergency department arrival, neurologic evaluation, brain imaging, and treatment.7–11 Furthermore, since 2013, the American Heart Association/American Stroke Association guidelines have recommended prenotification of stroke by EMS to the receiving hospital, which allows emergency department and stroke treatment teams to prepare before patient arrival and expedite in-hospital care.12
Although numerous studies have shown that prehospital notification of stroke by EMS reduces in-hospital delays and increases treatment rates,13–16 population-based data on adherence to this evidence-based practice are limited. A recent analysis of national data from a hospital-based stroke quality improvement program observed that 57% of EMS arrivals were prenotified, which did not change from 2014 to 2019.17 A statewide survey of EMS agencies in North Carolina found that 98% of agencies reported a stroke prenotification policy; however, fewer than half reported communicating prehospital stroke screen results to the receiving hospital, suggesting a disconnect between policy and practice.18 Although previous research has clearly shown that lower socioeconomic status (SES) and rural communities have poorer stroke19 and other health outcomes,20,21 these disparities in prehospital stroke care, specifically EMS prenotification, are understudied.
The objective of this study was to describe prehospital notification of stroke by EMS in North Carolina, a state in the Stroke Belt, and evaluate differences in this evidence-based practice by community SES and rurality. We hypothesized that stroke patients living in underserved communities of lower socioeconomic and rural status will be less likely to receive prenotification by EMS.
Methods
Study Design and Setting
We performed a retrospective analysis of the North Carolina EMS Data System, a statewide electronic database developed and maintained by the North Carolina Office of EMS. The 100 county-based EMS systems in North Carolina are mandated to submit electronic data on all EMS encounters to this database with the goal of improving EMS system performance and prehospital patient care across the state. Encounter data submitted by EMS systems are standardized based on National EMS Information System version 3. Our study included data on patient demographics (eg, age, sex, race/ethnicity), incident address, EMS response and on-scene care, and incident disposition (see Table S1 for the full list of data elements).
North Carolina is located within the Stroke Belt and ranks eighth highest for stroke mortality in the United States.22 Furthermore, a large percentage of North Carolina’s 10.5 million population lives in rural (43%) areas and below the poverty level (14%).23,24 Since 2009, the North Carolina Office of EMS has required each EMS system to develop and implement a protocol to direct prehospital care of suspected stroke patients, including stroke screening, triage and transport destinations, and prenotification to the receiving hospital. This study was reviewed by the University of North Carolina at Chapel Hill institutional review board and was approved by expedited review.
Study Population
All of the EMS-suspected stroke encounters occurring in North Carolina in 2019 were considered. A suspected stroke was defined as a 9-1-1 call response by EMS for a patient at least 18 years old in which the EMS provider had a primary or secondary impression of stroke or documented the use of a stroke protocol. Encounters that did not occur within North Carolina or did not result in transport to a hospital were excluded. Eligible patients for this study must have had a documented prehospital stroke scale or screen completed by the EMS provider, indicating an initial suspicion of stroke that led to the management of the patient.
Census Tract Characteristics
We geocoded EMS stroke incident addresses to census tracts using ArcGIS Pro (Esri, Redlands, CA). Census tract data from the American Community Survey 2015–2019 five-year estimates were used to compute a community-level SES index developed by the Agency for Healthcare Research and Quality.25 This index includes tract-level measures such as income, wealth, education, occupation, and housing and ranges from 0 to 100, with higher scores indicating higher SES. These scores were divided by tertiles into <51.1, 51.1 to 54.4, and >54.4 representing low, medium, and high SES groups, respectively. Census tract urban–rural commuting area primary codes were grouped to define urban–rural status, with 1 being urban, 2 to 6 being suburban, and 7 to 10 being rural.26 Figure 1 displays the geographic distribution of SES and rurality by all 2195 North Carolina census tracts.
Fig. 1.
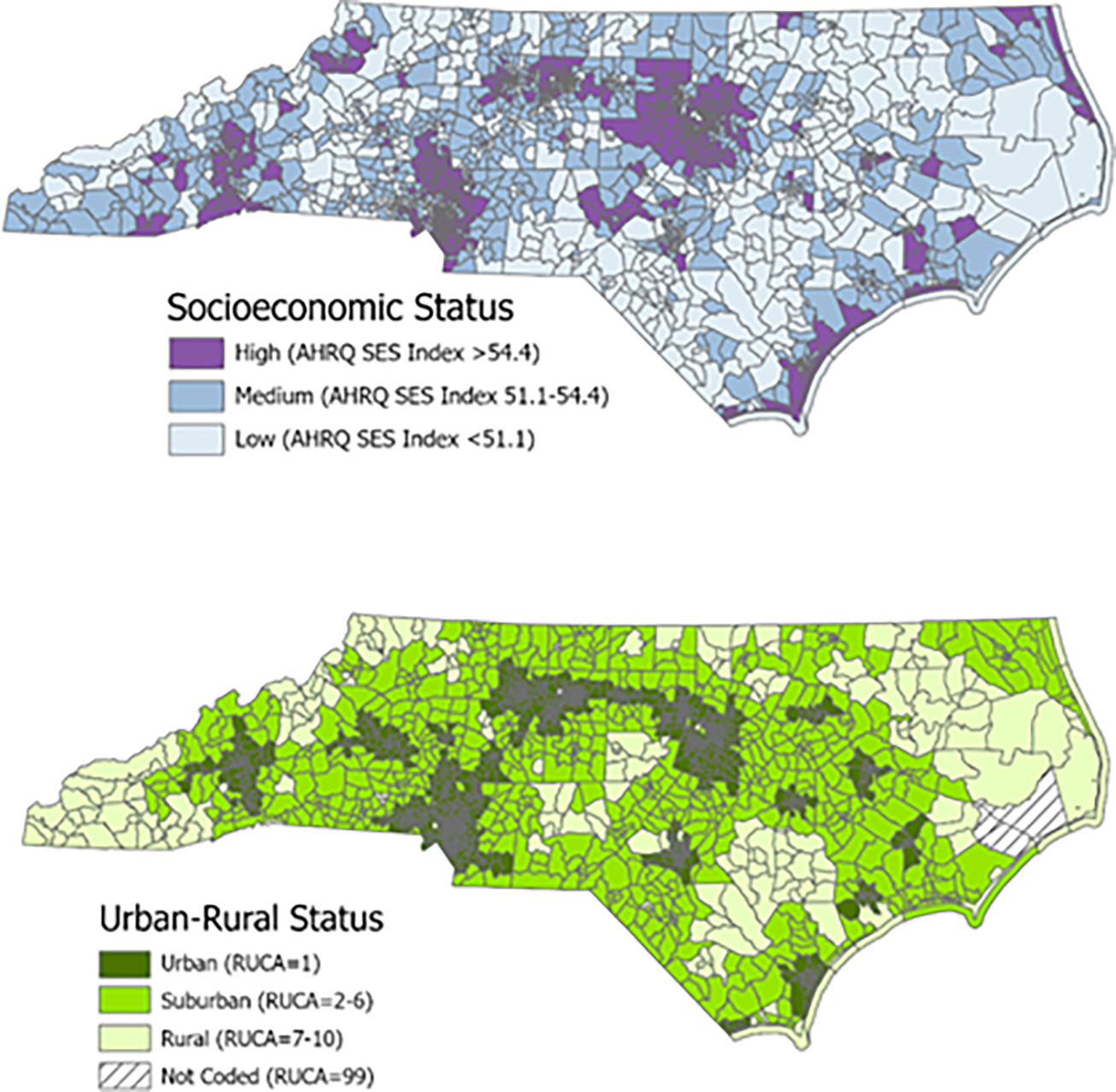
Census tract socioeconomic status and urban–rural status in North Carolina. AHRQ, Agency for Healthcare Research and Quality; RUCA, rural–urban commuting area; SES, socioeconomic status.
Patient- and Incident-Level Variables
Patient age was grouped as 18 to 54, 55 to 64, 65 to 74, and ≥75 years. Patient sex was either female or male. Patient race/ethnicity was categorized as White, non-Hispanic; Black, non-Hispanic; non-Hispanic other races, including American Indian or Alaska Native, Asian, and Native Hawaiian or Other Pacific Islander; and Hispanic or Latino. The duration of symptoms was grouped as 0 to 3, 3 to 6, 6 to 24, and >24 hours. The date and time of 9-1-1 dispatch notification to EMS were classified by day of week (weekend or weekday) and time of day (7:00 am to 2:59 pm, 3:00 to 10:59 pm, or 11:00 pm to 6:59 am). Incidents with a complaint of stroke reported by 9-1-1 dispatch were identified. The primary impression of the EMS provider was grouped into stroke, altered mental status, weakness, and other categories. Prehospital stroke screen or scale interpretation was documented as positive, negative, or nonconclusive. The outcome of interest was documentation of EMS prenotification of possible stroke to the receiving hospital.
Statistical Analysis
Pearson χ2 tests were used to assess associations between the frequency of EMS stroke prenotification and census tract SES and urban–rural status, with P < 0.05 considered statistically significant. Wald 95% confidence intervals (CIs) also were constructed for the proportion prenotified by levels of census tract characteristics. We estimated odds ratios (ORs) and 95% CIs of prenotification with census tract characteristics using multivariable logistic regression. We first fit a base model with only census tract SES (referent = high SES) and rurality (referent = urban). Then, a fully adjusted model was fit with census tract SES and rurality, adjusting for patient age group, sex, race/ethnicity, duration of symptoms, incident day of week (weekend vs weekday), time of day, stroke complaint reported by 9-1-1 dispatch, EMS provider primary impression, and stroke screen interpretation. Because we expected stroke screen interpretation to influence whether EMS provided prenotification, we ran logistic regression models stratified by positive, nonconclusive, and negative stroke screen and compared ORs by these stratification levels. Statistical analyses were conducted in SAS version 9.4 (SAS Institute, Cary, NC).
Results
We identified a total of 18,251 EMS responses for suspected stroke patients in the 2019 (Figure S1). Among them, 79 were excluded because they either occurred outside of North Carolina or were unable to be geocoded, and 1055 were excluded because the encounter did not lead to EMS transport to a hospital. Of the remaining 17,117 patients who were geocoded and had EMS transport to a hospital, 9527 had stroke scales completed and recorded, making them eligible for our study. This final dataset represented 1691 of the 2195 total North Carolina census tracts.
Among the 9527 eligible suspected stroke incidents, most occurred in an urban tract (57%) compared with suburban (34%) and rural (9%) tracts. The majority of patients were at least 65 years old (65%), female (55%), and non-Hispanic White (71%) (Table 1). For most EMS responses, the duration of symptoms was <3 hours (71%). Approximately one-fourth occurred on the weekend (26%), and nearly half occurred from 3 to 11 pm (49%). More than half (58%) had a stroke complaint reported by 9-1-1 dispatch, and 86% had a primary impression of stroke from an EMS provider. Prehospital stroke screen interpretation was positive for more than half (58%) of EMS incidents, although substantial proportions were also negative (30%) or nonconclusive (12%).
Table 1.
Characteristics of EMS suspected stroke patients by census tract characteristics
| Characteristics | Overall (N = 9527), no. (%) | Urban–rural status | Socioeconomic status | ||||
|---|---|---|---|---|---|---|---|
| Urban (n = 5424), no. (%) | Suburban (n = 3217), no. (%) | Rural (n = 886), no. (%) | High (n = 2809), no. (%) | Medium (n = 3424), no. (%) | Low (n = 3294), no. (%) | ||
| Age group, y | |||||||
| 18–54 | 1498 (16) | 853 (16) | 510 (16) | 135 (15) | 375 (13) | 541 (16) | 582 (18) |
| 55–64 | 1801 (19) | 1009 (19) | 631 (20) | 161 (18) | 416 (15) | 647 (19) | 738 (22) |
| 65–74 | 2317 (24) | 1307 (24) | 805 (25) | 205 (23) | 655 (23) | 816 (24) | 846 (26) |
| ≥75 | 3911 (41) | 2255 (42) | 1271 (40) | 385 (43) | 1363 (49) | 1420 (41) | 1128 (34) |
| Sex | |||||||
| Female | 5200 (55) | 2985 (55) | 1725 (54) | 490 (55) | 1529 (55) | 1910 (56) | 1761 (54) |
| Male | 4315 (45) | 2433 (45) | 1487 (46) | 395 (45) | 1276 (45) | 1509 (44) | 1530 (46) |
| Missing | 12 | 6 | 5 | 1 | 4 | 5 | 3 |
| Race/ethnicity | |||||||
| Black or African American | 2479 (27) | 1581 (30) | 676 (22) | 222 (26) | 479 (17) | 789 (23) | 1211 (38) |
| White | 6635 (71) | 3641 (68) | 2382 (76) | 612 (72) | 2214 (80) | 2519 (75) | 1902 (59) |
| Hispanic | 138 (1) | 86 (2) | 41 (1) | 11 (1) | 47 (2) | 53 (2) | 38 (1) |
| Other | 104 (1) | 50 (1) | 45 (1) | 9 (1) | 34 (1) | 16 (0.5) | 54 (2) |
| Missing | 171 | 66 | 73 | 32 | 35 | 47 | 89 |
| Duration of complaint | |||||||
| <3 h | 6340 (71) | 3532 (70) | 2191 (72) | 617 (75) | 1829 (72) | 2298 (70) | 2213 (72) |
| 3–6 h | 658 (7) | 388 (8) | 217 (7) | 53 (6) | 195 (8) | 243 (7) | 220 (7) |
| 6–24 h | 1314 (15) | 776 (15) | 440 (14) | 98 (12) | 359 (14) | 517 (16) | 438 (14) |
| >24 h | 562 (6) | 317 (6) | 190 (6) | 55 (7) | 154 (6) | 215 (7) | 193 (6) |
| Missing | 653 | 411 | 179 | 63 | 272 | 151 | 230 |
| Weekend | 2457 (26) | 1383 (26) | 841 (26) | 233 (26) | 689 (25) | 881 (26) | 887 (27) |
| Time of day | |||||||
| 7 AM–3 PM | 2664 (28) | 1503 (28) | 913 (28) | 248 (28) | 785 (28) | 925 (27) | 954 (29) |
| 3 PM–11 PM | 4713 (49) | 2717 (50) | 1556 (48) | 440 (50) | 1415 (50) | 1689 (49) | 1609 (49) |
| 11 PM–7 AM | 2150 (23) | 1204 (22) | 748 (23) | 198 (22) | 609 (22) | 810 (24) | 731 (22) |
| Stroke complaint by 9–1–1 dispatch | 5570 (58) | 3147 (58) | 1888 (59) | 535 (60) | 1712 (61) | 2035 (59) | 1823 (55) |
| EMS provider primary impression | |||||||
| Stroke | 7690 (86) | 4484 (87) | 2524 (85) | 682 (85) | 2334 (87) | 2766 (86) | 2590 (85) |
| Altered mental status | 480 (5) | 262 (5) | 166 (6) | 52 (6) | 140 (5) | 169 (5) | 171 (6) |
| Weakness | 272 (3) | 154 (3) | 93 (3) | 25 (3) | 77 (3) | 112 (3) | 83 (3) |
| Other | 501 (6) | 271 (5) | 183 (6) | 47 (6) | 147 (5) | 168 (5) | 186 (6) |
| Missing | 584 | 253 | 251 | 80 | 111 | 209 | 264 |
| Stroke screen interpretation | |||||||
| Positive | 5484 (58) | 2992 (55) | 1978 (61) | 514 (58) | 1559 (56) | 1958 (57) | 1967 (60) |
| Nonconclusive | 1149 (12) | 557 (10) | 457 (14) | 135 (15) | 217 (8) | 426 (12) | 506 (15) |
| Negative | 2894 (30) | 1875 (35) | 782 (24) | 237 (27) | 1033 (37) | 1040 (30) | 821 (25) |
EMS, emergency medical services.
In the overall study population, suspected stroke was prenotified by EMS in 2783 (29%) incidents. Prenotification varied significantly by tract urban–rural status (P < 0.001) and SES (P = 0.001) (Fig. 2). Frequencies were greater in urban (31%, 95% CI 30–32) versus rural (21%, 95% CI 18–24) and high SES (32%, 95% CI 30–33) versus low SES (27%, 95% CI 25–28). These differences also were observed in multivariable logistic regression models (Table 2). Similar to estimates from the base model, fully adjusted associations indicated a lower likelihood of EMS stroke prenotification in rural (versus urban) tracts (OR 0.64, 95% CI 0.52–0.77) and in low SES (versus high SES) tracts (OR 0.76, 95% CI 0.67–0.88).
Fig. 2.
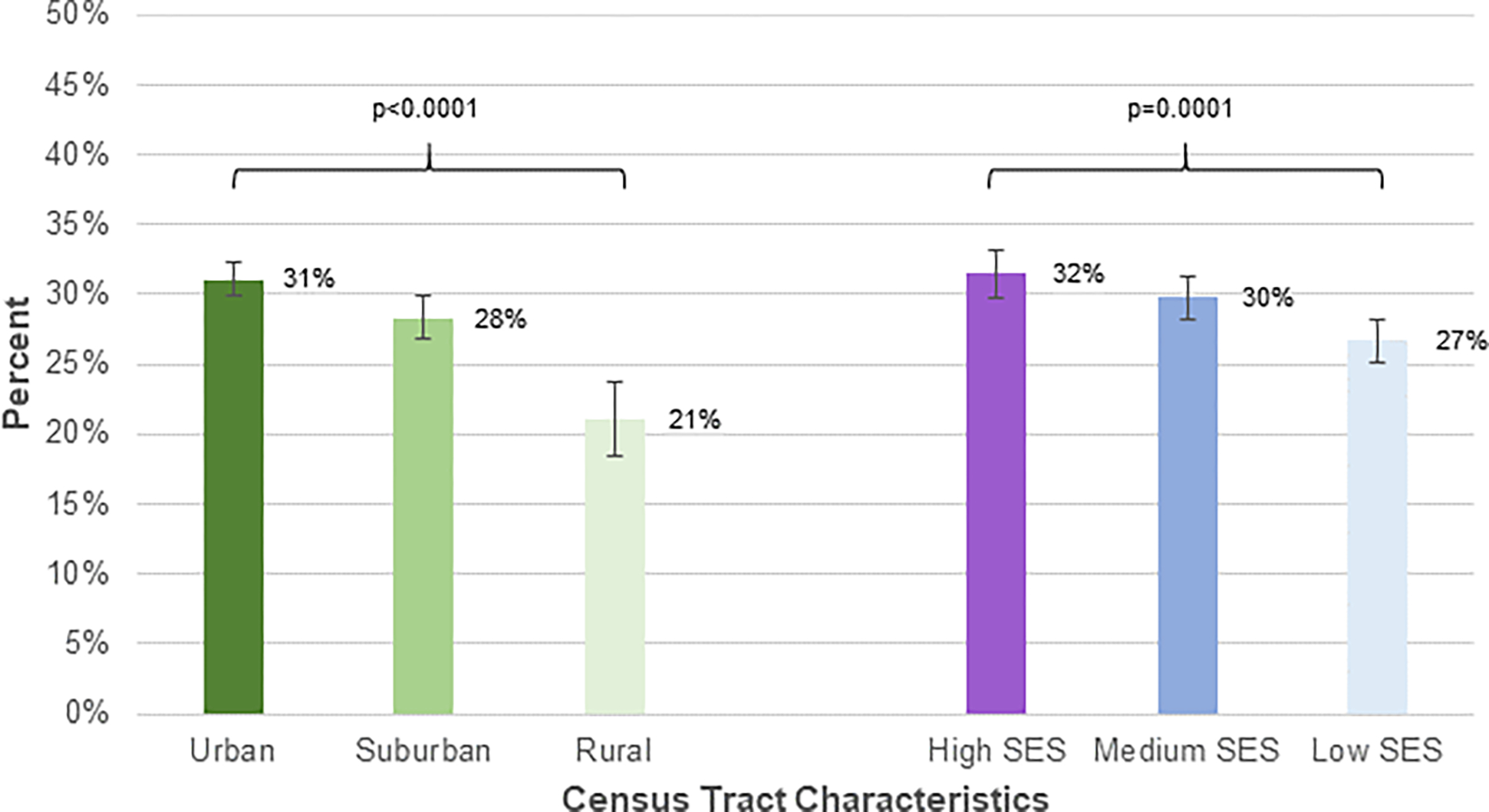
Emergency medical services prenotification of suspected stroke patients by census tract urban–rural status and socioeconomic status (N = 9527). SES, socioeconomic status.
Table 2.
Adjusted associations of EMS stroke prenotification with census tract urban–rural and SES
| AOR | 95% CI | |
|---|---|---|
| Base modela | ||
| Urban (ref) | 1 | — |
| Suburban | 0.91 | 0.83–1.01 |
| Rural | 0.62 | 0.52–0.74 |
| High SES (ref) | 1 | — |
| Medium SES | 0.97 | 0.87–1.09 |
| Low SES | 0.86 | 0.76–0.97 |
| Fully adjusted modelb | ||
| Urban (ref) | 1 | — |
| Suburban | 0.92 | 0.82–1.04 |
| Rural | 0.64 | 0.52–0.77 |
| High SES (ref) | 1 | — |
| Medium SES | 0.91 | 0.80–1.03 |
| Low SES | 0.76 | 0.67–0.88 |
AOR, adjusted odds ratio; CI, confidence interval; EMS, emergency medical services; ref, reference; SES, socioeconomic status.
Base model includes census tract rurality and SES.
Fully adjusted model includes census tract rurality and SES, age group, sex, race/ethnicity, duration of complaint, weekend, time of day, stroke dispatch complaint, EMS provider primary impression, and stroke screen interpretation.
In adjusted models stratified by prehospital stroke screen interpretation (ie, positive, negative, and nonconclusive), associations between EMS stroke prenotification and tract characteristics persisted (Table S2). Similar to those among the overall study population, rural and low SES tracts were less likely to experience EMS prenotification across all of the stroke screen results. The differences were less pronounced when the stroke screen was positive compared with nonconclusive or negative, however.
Discussion
Our statewide analysis found that EMS notification of stroke before hospital arrival occurred less often in rural and low SES communities in North Carolina. Statistical differences in EMS stroke prenotification also were observed after accounting for patient demographics, symptom duration, and several incident characteristics. Overall, the evidence-based practice of prehospital notification by EMS, as recommended in state EMS protocols, occurred in only one-third of suspected stroke patients, indicating room for improvement throughout North Carolina. Moreover, our study highlights relatively low EMS adherence in traditionally underserved rural and low SES communities. These findings suggest that suboptimal prehospital stroke management by EMS may contribute to already well-established disparities in stroke care and patient outcomes by rural and poor socioeconomic environments.19,27–29
The overall rate of one-third prenotification by EMS of suspected strokes found in this study is lower than reported in prior studies. Statewide and national estimates of prehospital notification from the Paul Coverdell National Acute Stroke Program, a formal stroke care quality improvement initiative, range from 49% to 58%.15–17 These estimates, however, are among patients with a clinical diagnosis of stroke from hospitals and less likely to include transient ischemic attacks and stroke mimics. Whereas true stroke patients are more likely to benefit from EMS prenotification, our broader study population of patients suspected of having a stroke by EMS is relevant for monitoring and improving prehospital stroke care because stroke diagnosis is not known at the time of initial patient management in the field. Although we did not have data on clinical diagnoses, EMS prenotification among true strokes was likely more common, compared to among suspected strokes, in our study and more consistent with published estimates. Recent research demonstrating associations between EMS prenotification and reduced stroke treatment times had substantially greater prenotification and data from predominantly large tertiary care centers in urban areas.30,31 Given the observed differences in rural and low SES areas, additional research on the effects of stroke prenotification are needed in less-resourced settings.
With EMS prenotification as a key component of stroke systems of care,32 our findings support additional efforts to improve this practice, particularly in rural and poorer communities. Continuing education and quality improvement in EMS can help address suboptimal adherence to current prehospital stroke protocols. Furthermore, the Utstein recommendations for emergency stroke care stressed the importance of a population-based stroke registry collecting data across the stroke chain of survival, including prehospital data on prenotification.33 With prior research suggesting a disconnect between EMS prenotification policy and practice,18 such stroke registries should be designed and executed to facilitate bidirectional data sharing and communication between EMS and hospitals.34 This systems approach and collaboration have the potential to improve acute stroke care in underserved settings and address stroke disparities.
Our study had important strengths and weaknesses. Our study used a large statewide database of EMS encounter data collected in the standardized National EMS Information System format. By using only EMS data, our study was limited to the prehospital care of stroke and did not include any data on in-hospital care, final diagnosis, or patient outcomes. As discussed, our study population was broadly defined as any patient suspected of having a stroke by EMS and likely included stroke mimics, thus reflecting the entirety of prehospital stroke care. Making completion of a prehospital stroke screen an eligibility criterion excluded data if this information was not documented in the patient care report. Because the data are collected and maintained by a separate entity, data accuracy and completeness could not be independently verified by our study team. Although North Carolina is a large state with a diverse population, our results may not be generalizable to other states or regions. We had a high success rate with geocoding incident addresses to census tracts. Furthermore, we had adequate data to represent all levels of rurality and SES in our study. Although the urban–rural commuting area is commonly used in the literature to define rurality, there are multiple definitions to classify a community as rural versus urban, such as the Urban Influence Codes, census place, or urban area designation, and a different definition may change our results. Finally, our data are from 2019 and may not reflect the most current practices of stroke prenotification by EMS, although our findings are not influenced by disruptions and variations in prehospital emergency care resulting from the coronavirus disease 2019 pandemic.
Conclusions
Our study showed important differences in EMS prehospital notification for suspected stroke between community rurality and socioeconomic status. Responses by EMS in rural and low SES areas had the lowest rates of stroke prenotification. Our findings can inform continuing education and quality improvement initiatives to improve prehospital stroke care and optimize stroke systems at regional and state levels.
Key Points.
Community socioeconomic and urban–rural disparities in prehospital stroke care by emergency medical services (EMS) are understudied.
This statewide study of EMS prehospital notification of stroke to the destination hospital was conducted with data on EMS stroke encounters in North Carolina in 2019.
An EMS prehospital notification of stroke was less likely to occur in low socioeconomic status and rural communities.
Acknowledgments
The North Carolina Office of EMS and the North Carolina EMS Data System supports state, regional, and local EMS and healthcare-related service delivery from a patient care, resource allocation, and regulatory perspective. This work has been reviewed by North Carolina EMS Data System investigators for scientific content and consistency of data interpretation with previous North Carolina EMS Data System publications, and significant comments have been incorporated.
This work was supported by National Center for Advancing Translational Sciences, National Institutes of Health grant no. KL2TR002490. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Appendices
Table S1.
Study Data Elements (National EMS Information System V3)
| Data Element Number | Data Element Name |
|---|---|
| eResponse.05 | Type of Service Requested |
| eResponse.15 | Level of Care of This Unit |
| eResponse.23 | Response Mode to Scene |
| eDispatch.01 | Complaint Reported by Dispatch |
| eScene.09 | Incident Location Type |
| eScene.15 | Incident Address |
| eScene.17 | Incident City |
| eScene.18 | Incident State |
| eScene.19 | Incident ZIP Code |
| eScene.21 | Incident County |
| eTimes.01 | PSAP Call Date/Time |
| eTimes.03 | Unit Notified by Dispatch Date/Time |
| eTimes.05 | Unit En Route Date/Time |
| eTimes.06 | Unit On Scene Date/Time |
| eTimes.07 | Unit on Patient Date/Time |
| eTimes.09 | Unit Left Scene Date/Time |
| eTimes.11 | Patient at Destination Date/Time |
| ePatient.13 | Gender |
| ePatient.14 | Race |
| ePatient.15 | Age |
| ePatient.16 | Age Units |
| eSituation.04 | Complaint |
| eSituation.05 | Duration of Complaint |
| eSituation.06 | Time Units of Duration |
| eSituation.09 | Primary Symptom |
| eSituation.10 | Other Associated Symptoms |
| eSituation.11 | Primary Impression |
| eSituation.12 | Secondary Impression |
| eProtocols.01 | Protocols Used |
| eProcedures.03 | Procedure |
| eMedications.03 | Medication Given |
| eVitals.29 | Stroke Scale Score |
| eVitals.30 | Stroke Scale Type |
| eDisposition.01 | Destination Name |
| eDisposition.02 | Destination Code |
| eDisposition.03 | Destination Address |
| eDisposition.04 | Destination City |
| eDisposition.05 | Destination State |
| eDisposition.06 | Destination County |
| eDisposition.07 | Destination ZIP Code |
| eDisposition.12 | Incident Patient/Disposition |
| eDisposition.17 | Transport Mode from Scene |
| eDisposition.21 | Type of Destination |
| eDisposition.24 | Pre-Arrival Alert or Action |
Table S2.
Adjusted Odds Ratios (AORs) and 95% Confidence Intervals (CIs) of EMS Stroke Prenotification with Census Tract Urban-Rural and Socioeconomic Status Stratified by Stroke Screen Interpretation
| Positive Stroke Screen (N=5,484) | Non-Conclusive Stroke Screen (N=1,149) | Negative Stroke Screen (N=2,894) | ||||
|---|---|---|---|---|---|---|
| AOR | (95% CI) | AOR | (95% CI) | AOR | (95% CI) | |
| (a) Base model * | ||||||
| Urban (ref) | 1 | --- | 1 | --- | 1 | --- |
| Suburban | 1.06 | (0.94–1.21) | 0.76 | (0.57–1.03) | 0.44 | (0.34–0.57) |
| Rural | 0.77 | (0.62–0.94) | 0.42 | (0.25–0.73) | 0.31 | (0.19–0.50) |
| High SES (ref) | 1 | --- | 1 | --- | 1 | --- |
| Medium SES | 1.05 | (0.91–1.21) | 0.99 | (0.68–1.45) | 0.77 | (0.62–0.95) |
| Low SES | 0.91 | (0.78–1.06) | 0.79 | (0.53–1.16) | 0.64 | (0.50–0.83) |
| (b) Fully-adjusted model † | ||||||
| Urban (ref) | 1 | --- | 1 | --- | 1 | --- |
| Suburban | 1.05 | (0.91–1.20) | 0.82 | (0.58–1.15) | 0.62 | (0.47–0.82) |
| Rural | 0.76 | (0.61–0.96) | 0.37 | (0.19–0.70) | 0.48 | (0.29–0.81) |
| High SES (ref) | 1 | --- | 1 | --- | 1 | --- |
| Medium SES | 1.01 | (0.87–1.18) | 0.89 | (0.58–1.38) | 0.68 | (0.53–0.87) |
| Low SES | 0.86 | (0.73–1.02) | 0.68 | (0.43–1.08) | 0.51 | (0.38–0.69) |
Base model includes census tract rurality and SES
Fully-adjusted model includes census tract rurality and SES, age group, gender, race/ethnicity, duration of symptoms, weekend, time of day, stroke dispatch complaint, and EMS provider primary impression
Figure S1.
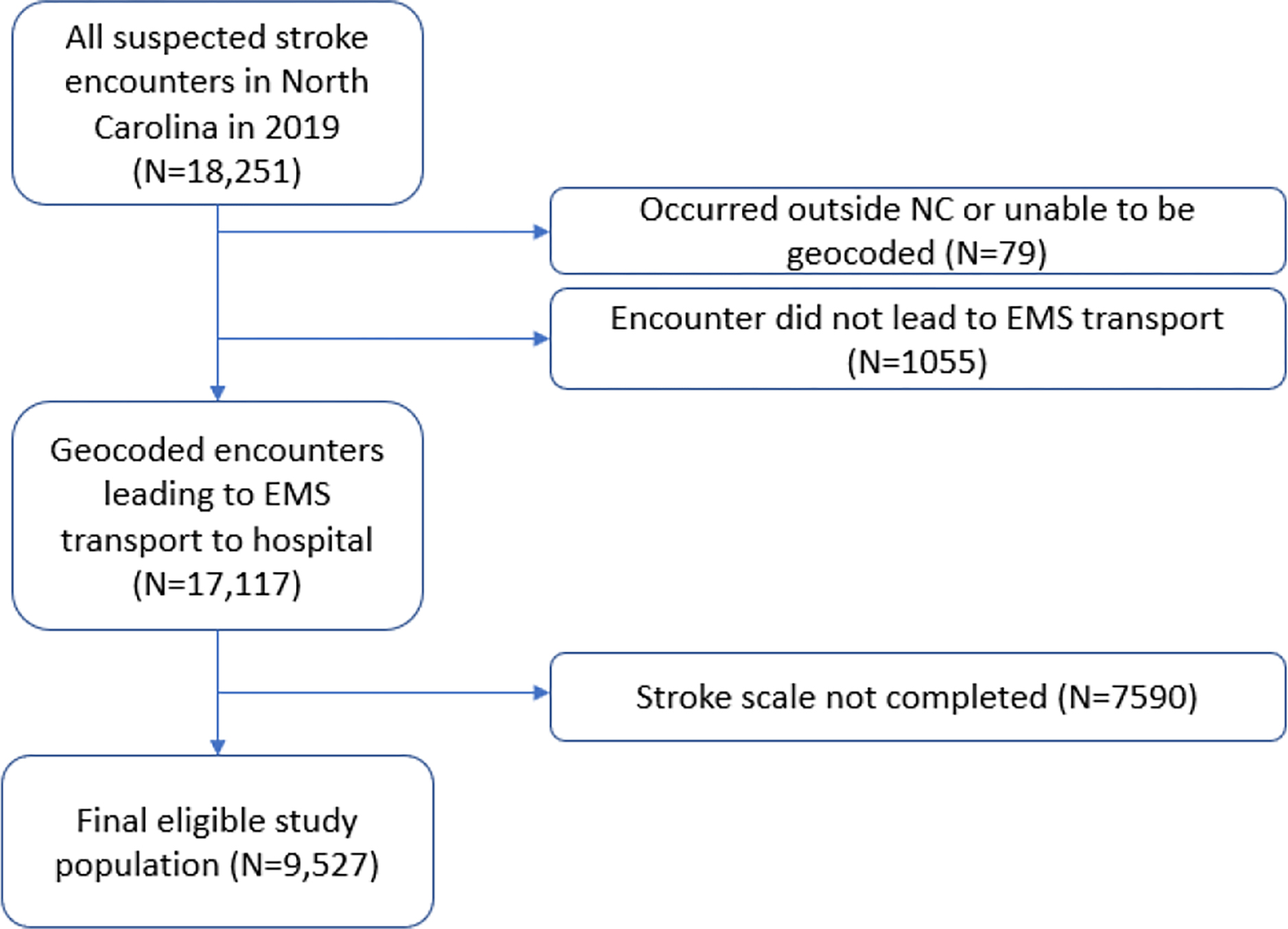
Flow Diagram of the Final Study Population
Footnotes
J.E.W. has received compensation from the University of North Carolina Medical School and the North Carolina Office of Emergency Medical Services. E.C.J. has received compensation from Hughes Socol Piers Resnick & Dym, Ltd. and Schultz & Pogue, LLP for medicolegal consultation.AB The remaining authors did not report any financial relationships or conflicts of interest other than the National Institutes of Health grant.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (http://sma.org/smj).
References
- 1.Sacco RL, Kasner SE, Broderick JP, et al. , An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013;44:2064–2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Virani SS, Alonso A, Aparicio HJ, et al. Heart disease and stroke statistics—2021 update: a report from the American Heart Association. Circulation 2021;143:e254–e743. [DOI] [PubMed] [Google Scholar]
- 3.Kumar S, Selim MH, Caplan LR. Medical complications after stroke. Lancet Neurol 2010;9:105–118. [DOI] [PubMed] [Google Scholar]
- 4.Tsao CW, Aday AW, Almarzooq ZI, et al. Heart disease and stroke statistics-2022 update: a report from the American Heart Association. Circulation 2022;145:e153–e639. [DOI] [PubMed] [Google Scholar]
- 5.Howard G, Howard VJ. Twenty years of progress toward understanding the stroke belt. Stroke 2020;51:742–750. [DOI] [PubMed] [Google Scholar]
- 6.Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2019;50:e344–e418. [DOI] [PubMed] [Google Scholar]
- 7.Lacy CR, Suh DC, Bueno M, et al. Delay in presentation and evaluation for acute stroke: Stroke Time Registry for Outcomes Knowledge and Epidemiology (S.T.R.O.K.E.). Stroke 2001;32:63–69. [DOI] [PubMed] [Google Scholar]
- 8.Menon SC, Pandey DK, Morgenstern LB. Critical factors determining access to acute stroke care. Neurology 1998;51:427–432. [DOI] [PubMed] [Google Scholar]
- 9.Morris DL, Rosamond W, Madden K, et al. Prehospital and emergency department delays after acute stroke: the Genentech Stroke Presentation Survey. Stroke 2000;31:2585–2590. [DOI] [PubMed] [Google Scholar]
- 10.Rossnagel K, Jungehülsing GJ, Nolte CH, et al. Out-of-hospital delays in patients with acute stroke. Ann Emerg Med 2004;44:476–483. [DOI] [PubMed] [Google Scholar]
- 11.Schroeder EB, Rosamond WD, Morris DL, et al. Determinants of use of emergency medical services in a population with stroke symptoms: the Second Delay in Accessing Stroke Healthcare (DASH II) Study. Stroke 2000;31:2591–2596. [DOI] [PubMed] [Google Scholar]
- 12.Jauch EC, Saver JL, Adams HP, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013;44:870–947. [DOI] [PubMed] [Google Scholar]
- 13.Lin CB, Peterson ED, Smith EE, et al. Emergency medical service hospital prenotification is associated with improved evaluation and treatment of acute ischemic stroke. Circ Cardiovasc Qual Outcomes 2012;5:514–522. [DOI] [PubMed] [Google Scholar]
- 14.McKinney JS, Mylavarapu K, Lane J, et al. Hospital prenotification of stroke patients by emergency medical services improves stroke time targets. J Stroke Cerebrovasc Dis 2013;22:113–118. [DOI] [PubMed] [Google Scholar]
- 15.Nielsen VM, DeJoie-Stanton C, Song G, et al. The association between presentation by EMS and EMS Prenotification with receipt of intravenous tissue-type plasminogen activator in a state implementing stroke systems of care. Prehosp Emerg Care 2020;24:319–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patel MD, Rose KM, O’brien EC, et al. Prehospital notification by emergency medical services reduces delays in stroke evaluation: findings from the North Carolina Stroke Care Collaborative. Stroke 2011;42:2263–2268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Asaithambi G, Tong X, Lakshminarayan K, et al. Emergency medical services Utilization for acute stroke care: analysis of the Paul Coverdell National Acute Stroke Program, 2014–2019. Prehosp Emerg Care 2022;26:326–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patel MD, Brice JH, Evenson KR, et al. Emergency medical services capacity for prehospital stroke care in North Carolina. Prev Chronic Dis 2013;10:E149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hammond G, Luke AA, Elson L, et al. Urban-rural inequities in acute stroke care and in-hospital mortality. Stroke 2020;51:2131–2138. [DOI] [PubMed] [Google Scholar]
- 20.Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Aff (Millwood) 2002;21:60–76. [DOI] [PubMed] [Google Scholar]
- 21.Caldwell JT, Ford CL, Wallace SP, et al. Intersection of living in a rural versus urban area and race/ethnicity in explaining access to health care in the United States. Am J Public Health 2016;106:1463–1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. About underlying cause of death 1999–2020. https://wonder.cdc.gov/ucd-icd10.html. Published 2021. Accessed October 6, 2022.
- 23.Rural Health Information Hub. North Carolina. https://www.ruralhealthinfo.org/states/north-carolina. Accessed January 28, 2022. [Google Scholar]
- 24.Harris LR 2020 Poverty Report: persistent poverty demands a just recovery for North Carolinians. https://www.ncjustice.org/publications/2020-poverty-report-persistent-poverty-demands-a-just-recovery-for-north-carolinians. Published October 20, 2020. Accessed October 6, 2022.
- 25.Bonito AJ, Bann C, Eicheldinger C, et al. Creation of New Race-Ethnicity Codes and Socioeconomic Status (SES) Indicators for Medicare Beneficiaries: Final Report. Washington, DC: Agency for Healthcare Research and Quality; 2008. [Google Scholar]
- 26.Weeks WB, Kazis LE, Shen Y, et al. Differences in health-related quality of life in rural and urban veterans. Am J Public Health 2004;94:1762–1767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chari SV, Cui ER, Fehl HE, et al. Community socioeconomic and urban-rural differences in emergency medical services times for suspected stroke in North Carolina. Am J Emerg Med 2023;63:120–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gonzales S, Mullen MT, Skolarus L, et al. Progressive rural–urban disparity in acute stroke care. Neurology 2017;88:441–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kapral MK, Fang J, Chan C, et al. Neighborhood income and stroke care and outcomes. Neurology 2012;79:1200–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fujiwara S, Kuroda T, Matsuoka Y, et al. , Prehospital stroke notification and endovascular therapy for large vessel occlusion: a retrospective cohort study. Sci Rep 2022;12:10107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hsieh MJ, Tang SC, Chiang WC, et al. Effect of prehospital notification on acute stroke care: a multicenter study. Scand J Trauma Resusc Emerg Med 2016;24:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Adeoye O, Nyström KV, Yavagal DR, et al. Recommendations for the establishment of stroke systems of care: a 2019 update: a policy statement from the American Stroke Association. Stroke 2019;50:e187–e210. [DOI] [PubMed] [Google Scholar]
- 33.Rudd AG, Bladin C, Carli P, et al. Utstein recommendation for emergency stroke care. Int J Stroke 2020;15:555–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gunderson MR, Florin A, Price M, et al. NEMSMA position statement and white paper: process and outcomes data sharing between EMS and receiving hospitals. Prehosp Emerg Care 2021;25:307–313. [DOI] [PubMed] [Google Scholar]


