Abstract
Introduction
Inside-out and all-inside arthroscopic meniscal repairs are widely performed. However, it remains unclear which method promotes greater clinical outcomes. This study compared inside-out versus all-inside arthroscopic meniscal repair in terms of patient-reported outcome measures (PROMs), failures, return to play, and symptoms.
Methods
This systematic review was conducted in accordance with the PRISMA guidelines. Two authors independently performed the literature search by accessing the following databases: PubMed, Google Scholar, and Scopus in February 2023. All clinical studies which investigated the outcomes of all-inside and/or inside-out meniscal repair were considered.
Results
Data from 39 studies (1848 patients) were retrieved. The mean follow-up was 36.8 (9 to 120) months. The mean age of the patients was 25.8 ± 7.9 years. 28% (521 of 1848 patients) were women. No difference was found in PROMs: Tegner Activity Scale (P = 0.4), Lysholm score (P = 0.2), and International Knee Document Committee score (P = 0.4) among patients undergoing meniscal repair with all inside or inside-out techniques. All-inside repairs showed a greater rate of re-injury (P = 0.009) but also a greater rate of return to play at the pre-injury level (P = 0.0001). No difference was found in failures (P = 0.7), chronic pain (P = 0.05), reoperation (P = 0.1) between the two techniques. No difference was found in the rate of return to play (P = 0.5) and to daily activities (P = 0.1) between the two techniques.
Conclusion
Arthroscopic all-inside meniscal repair may be of special interest in patients with a particular interest in a fast return to sport, while, for less demanding patients, the inside-out suture technique may be recommended. High-quality comparative trials are required to validate these results in a clinical setting.
Level of Evidence
Level III, systematic review.
Keywords: Meniscal repair, All-inside, Inside-out, Re-injury, Return to sport
Introduction
The meniscus, a fibrocartilaginous structure essential for stabilizing the knee joint, absorbing shocks, distributes forces and protects the articular cartilage [1–5]. Acute tears of the meniscus may be symptomatic, impacting negatively quality of life and sport participation, and may lead to early onset osteoarthritis [6–9]. Rotational and shear forces on the menisci, especially during kneeling, carrying heavy loads and movements with acceleration, deceleration, jumping, and change of direction, are the main causes of acute tears of the meniscus [10–13]. Direct traumas to the knee might also cause meniscal damage and are often associated with damage to adjacent bone and ligaments [14, 15]. In adults with meniscal degeneration, meniscal tears develop from relatively minor forces or trauma [16, 17].
Meniscal repair is associated with reduced chondral damage compared to meniscectomy [18–22]. In this context, by stabilising the knee joint, meniscal repair prevents cartilage damage, thus preventing early-onset osteoarthritis [23–25]. Repair of the damaged meniscal tissue was introduced in the 1980s [26, 27]. Arthroscopic repair of meniscal injuries has become popular [28–30]. Inside-out and all-inside are two well-established methodologies to repair the damaged meniscus during arthroscopy. Though these techniques are widely performed and validated in several clinical settings, it remains unclear which method promotes greater clinical outcomes. This study compared inside-out versus all-inside arthroscopic meniscal repair in terms of patient-reported outcome measures (PROMs), failures, return to play, and symptoms.
Methods
Search strategy
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) [31]. The PICO algorithm was established:
P (population): meniscal tears in the active population;
I (intervention): arthroscopic meniscal repair;
C (comparison): All-inside, inside-out;
O (outcomes): PROMs, clinical examination, complications.
Literature search
Two authors (**;**) independently performed the literature search by accessing the following database PubMed, Google Scholar, Scopus in February 2023. The following keywords were used for the search in combination using the Boolean operator AND/OR: meniscal, injury, trauma, acute, defects, tear, rupture, sport, arthroscopy, repair, refixation, all-inside, inside-out. If the title matched the topic, the abstract was read and the full text of the article was accessed. The bibliographies of the articles of interest were screened by hand. Disagreements between the authors were debated and solved by a third author (**).
Eligibility criteria
All clinical studies which investigated the outcomes of all-inside and/or inside-out meniscal repairs were considered. Articles with levels of evidence I to III, according to the Oxford Centre of Evidenced-Based Medicine [32], were considered. Given the authors language capabilities, articles in English, Italian, French, Spanish, and German were considered. Technical notes, editorials, protocols, comments, guidelines, and reviews were excluded. Biomechanical, animal, and cadaveric studies were also not eligible. Studies that reported data on meniscal procedures augmented with mesenchymal stem cells were not considered. Only articles reporting quantitative data under the outcomes of interest were included.
Data extraction
Two authors (**,**) independently performed data extraction and collection. The generalities of the studies were retrieved. The length of follow-up, sample size, and percentage of women in each study were collected. The outcomes of interest were the average age of patients at the time of injury, the incidence between male and female sex, the type of meniscal lesion, and the degree of effectiveness of each technique based on the percentage of patients who returned to play and of re-injured. Specifically, the rate of return to play was also assessed, also considering the patients who managed to return to play at a pre-injury level. The following PROMs were evaluated: International Knee Documentation Committee (IKDC) [33], Lysholm Knee Scoring Scale [34], Tegner Activity Scale [35]. Data on the following complication were collected: rate of re-injury, failures, chronic pain, and reoperation. Data concerning the rate of return to play at a pre-injury level, return to play and daily activities were also retrieved.
Methodological quality assessment
For the methodological quality assessment, the Coleman Methodology Score (CMS) was used [36]. The CMS is a reliable tool to evaluate the methodological quality of systematic reviews and meta-analyses. This score analyses each included study with several endpoints: study size, follow-up duration, surgical approach, type of study, description of the diagnosis, surgical technique, and rehabilitation. The procedures for assessing outcomes and the subject selection process are also evaluated. The CMS rates articles with values between 0 (poor) and 100 (excellent). Articles with values greater than 60 are considered satisfactory.
Statistical analysis
The statistical analyses were conducted by the first author (**) using the IBM SPSS software (version 25). For descriptive statistics, mean and standard deviation were evaluated. The t-test was performed to assess baseline comparability, with values of P > 0.05 considered satisfactory. For the comparisons of continuous data, the mean difference (MD) effect measure and the unpaired t-test were performed. For binary data, the Odd Ratio (OR) effect measure was evaluated. The confidence interval (CI) was set at 0.95. Values of P < 0.05 were considered statistically significant.
Results
Study selection
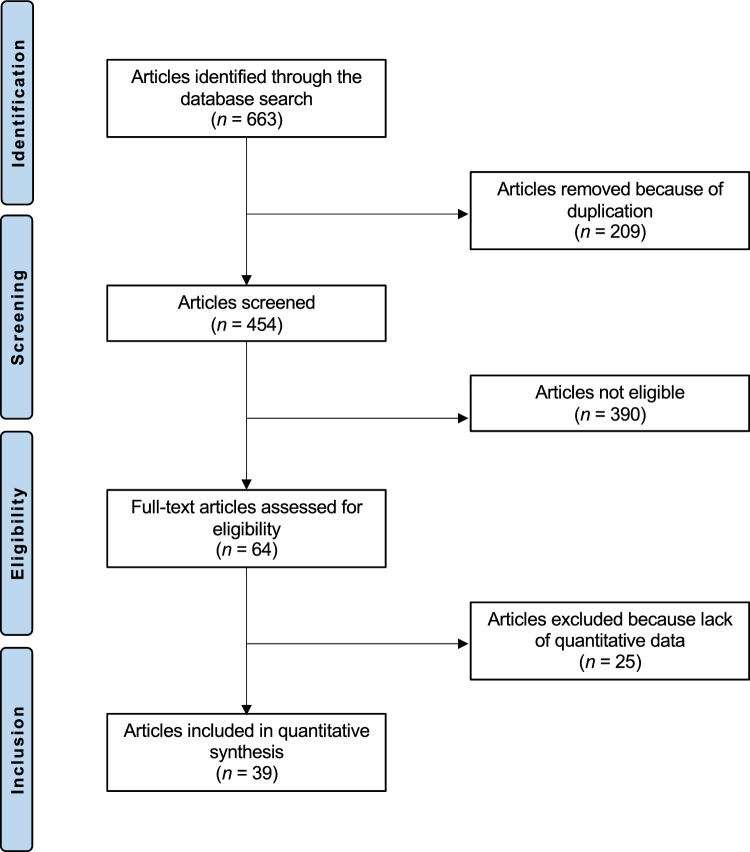
The initial literature search resulted in 12,843 articles. Of them, only 663 articles matched the topic. Duplicate records (N = 209) were excluded. Of these, a further 390 articles were excluded for reason: not matching the topic (N = 271), study design inappropriate (N = 112), language limitation (N = 4), not available full-text (N = 3). A further 25 articles did not report quantitative data under the outcome of interest, and thus, excluded. This left 39 articles for inclusion. Of them, 22 are prospective and 17 are retrospective studies. The literature search results are shown in Fig. 1.
Fig. 1.
Flow chart of the literature search
Study risk of bias assessment
The CMS identified some limitations and strengths in the present study. The size of the study and the duration of follow-up of the included articles were acceptable. The surgical approach, diagnosis and rehabilitation were well described in most of the articles. The outcome measures and timing of the evaluation were often defined, providing moderate assurance. General health measures were rarely reported. Procedures for outcome evaluation and subject selection were often biased and unsatisfactorily described. The CMS for the articles was 66, testifying to this study a good quality of the methodologies for the articles included. The CMS is reported in Fig. 2 (Table 1).
Table 1.
Coleman Methodology Scores for the included articles (mean ± standard deviation)
| Endpoint | Value | |
|---|---|---|
| Part A: only 1 score to be given for each of the 7 sections | ||
| 1. Study size: number of patients | 4.3 ± 2.6 | |
| 2. Mean follow-up | 5.2 ± 2.5 | |
| 3. Surgical approach | 5.4 ± 4.5 | |
| 4. Type of study | 6.0 ± 5.6 | |
| 5. Description of diagnosis | 4.5 ± 1.6 | |
| 6. Descriptions of surgical technique | 5.1 ± 2.8 | |
| 7. Description of postoperative rehabilitation | 3.9 ± 2.1 | |
| Part B: scores may be given for each option in each of the 3 sections if applicable | ||
| 1. Outcome criteria | 2.6 ± 0.6 | |
| 2. Procedure of assessing outcomes | 3.7 ± 0.9 | |
| 3. Description of the subject selection process | 4.4 ± 1.6 | |
| Total | 66.3 ± 7.7 | |
Study characteristics and results of individual studies
Data from 1848 patients were retrieved. The mean follow-up was 36.8 (9–120) months. The mean age of the patients was 25.8 ± 7.9 years. 28% (521 of 1848 patients) were women. Generalities of the included studies are shown in Table 2.
Table 2.
Eneralities of the included studies (CMS: Coleman Methodology Score)
| Author, year | Journal | Design | CMS | Technique | Follow-up (months) | Patients (n) | Mean age | Women (%) |
|---|---|---|---|---|---|---|---|---|
| Ahn et al., 2013 [37] | Knee Surg Sports Traumatol Arthrosc, | Prospective | 57 | All-inside | 48.0 | 13 | 20.0 | 46 |
| Barber et al., 2006 [38] | Arthroscopy | Retrospective | 61 | Inside-out | 38.6 | 41 | 29.8 | 29 |
| Bryant et al., 2007 [39] | Am J Sport | Prospective | 59 | Inside-out | 28.0 | 49 | 25.7 | 41 |
| Chiang et al., 2011 [40] | Chang Gung Med J | Prospective | 71 | All-inside | 36.0 | 31 | 30.7 | 39 |
| All-inside | 51 | 25.1 | 35 | |||||
| Choi et al., 2009 [41] | Am J Sport | Prospective | 48 | All-inside | 35.7 | 14 | 28.6 | 14 |
| Inside-out | 34 | 27.7 | 6 | |||||
| Chou et al., 2015 [42] | Orthop Traumatol Surg Res | Retrospective | 53 | All-inside | 25.0 | 24 | 27.0 | 25 |
| Diaz- Alvarez et al., 2015 [43] | Knee Surg Sports Traumatol Arthrosc, | Prospective | 62 | All-inside | 72.0 | 29 | 29.0 | 0 |
| Gallacher et al., 2010 [44] | Knee | Retrospective | 50 | All-inside | 48.0 | 87 | 26.0 | 16 |
| Hagino et al., 2014 [45] | Eur J Orthop Surg Traumatol | Prospective | 67 | All-inside | 19.0 | 57 | 23.6 | 53 |
| Haklar et al., 2008 [46] | Knee | Prospective | 64 | Inside-out | 31.0 | 5 | 28.6 | 0 |
| Hetsroni et al., 2011 [47] | Arthroscopy | Retrospective | 60 | All-inside | 24.0 | 6 | ||
| Hirtler et al., 2015 [48] | Int Orthop | Retrospective | 55 | All-inside | 9.0 | 37 | 24.2 | 68 |
| Järvelä et al., 2010 [49] | Am J Sport Med | Prospective | 83 | All-inside | 27.0 | 21 | 30.0 | 19 |
| All-inside | 26.0 | 21 | 32.0 | 43 | ||||
| Kamimura et al., 2014 [50] | Orthop J Sports Med | Prospective | 69 | All-inside | 12.0 | 4 | 52.8 | 25 |
| All-inside | 12.0 | 3 | 32.0 | 67 | ||||
| Kise et al., 2015 [51] | Knee Surg Sports Traumatol Arthrosc | Prospective | 73 | All-inside | 24.0 | 21 | 26.9 | 57 |
| All-inside | 24.0 | 25 | 25.5 | 32 | ||||
| Kotosolov et al., 2006 [52] | Arthroscopy | Prospective | 71 | All-inside | 18.0 | 58 | 32.6 | |
| Krych et al., 2008 [53] | Am J Sport Med | Retrospective | 68 | Inside-out | 24.0 | 44 | 15.8 | 14 |
| Aaron J Krych et al., 2010 [54] | Am J Sport Med | Retrospective | 77 | Inside-out | 69.6 | 99 | 16.0 | 57 |
| Logan et al., 2009 [55] | Am J Sport Med | Retrospective | 71 | Inside-out | 60.0 | 42 | 23.2 | 31 |
| Lucas et al., 2015 [56] | Orthop Traumatol Surg Res | Retrospective | 71 | All-inside | 22.0 | 17 | 14.0 | 47 |
| Moatshe et al., 2018 [57] | Am J Sport Med | Prospective | 71 | Inside- out | 36.0 | 40 | 32.9 | 38 |
| Inside- out | 36.0 | 45 | 0 | |||||
| Nakayama et al., 2017 [58] | Asia Pac J Sports Med Arthrosc Rehabil Technol | Retrospective | 63 | Inside-out | 19.8 | 46 | 22.9 | 26 |
| Noyes et al., 2002 [59] | Am J Sport Med | Prospective | 67 | Inside-out | 24.0 | 58 | 16.0 | 45 |
| Noyes et al., 2011 [60] | Am J Sport Med | Prospective | 70 | Inside-out | 120.0 | 31 | 15.4 | 45 |
| Olsen et al., 1998 [61] | Acta Orthop Scand | Retrospective | 62 | Inside-out | 29 | 28.0 | 0 | |
| Papachristou et al., 2003 [62] | Acta Orthop Belg | Prospective | 68 | Inside-out | 36.0 | 45 | 21.8 | 18 |
| Perdue et al. 1996 [63] | Arthroscopy | Retrospective | 61 | Inside-out | 26.9 | 63 | 26.9 | 25 |
| Popescu et al., 2013 [64] | Knee Surg Sports Traumatol Arthrosc, | Prospective | 64 | All-inside | 18.5 | 28 | 33.0 | 21 |
| Pujol et al., 2012 [65] | Knee Surg Sports Traumatol Arthrosc, | Retrospective | 53 | All-inside | 24.0 | 19 | 25.0 | 32 |
| Raza et al., 2011 [66] | J Pak Med Ass | Retrospective | 64 | Inside-out | 17.0 | 14 | 41.2 | 64 |
| Reja et al., 2014 [67] | Arthroscopy | Retrospective | 61 | Inside-out | 48.0 | 24 | 22.8 | 21 |
| Schmitt et al., 2016 [68] | Orthop Traumatol Surg Res | Prospective | 69 | All-inside | 72.0 | 19 | 14.8 | 37 |
| Spindler et al., 2003 [69] | Am J Sport Med | Prospective | 68 | Inside-out | 68.0 | 47 | 24.4 | 44 |
| All-inside | 27.0 | 98 | 23.2 | 48 | ||||
| Steadman et al., 2015 [70] | Am J Sport Med | Prospective | 75 | Inside-out | 120.0 | 136 | 27.0 | 32 |
| Thomas Stein et al., 2010 [71] | Am J Sport Med | Prospective | 67 | Inside-out | 36.0 | 42 | 31.3 | 38 |
| Tengrootenhuysen et al., 2011 [72] | Knee Surg Sports Traumatol Arthrosc, | Retrospective | 76 | Inside-out | 70.0 | 119 | 23.0 | 35 |
| Tiftikçi et al., 2017 [73] | J Orthop Surg Res, | Retrospective | 63 | All-inside | 29.0 | 27 | 40.5 | 41 |
| Tucciarone et al., 2012 [74] | Arch Orthop Trauma Surg | Prospective | 67 | All-inside | 24.0 | 40 | 23.0 | 13 |
| Vanderhaave et al., 2011 [75] | J Pediatr Orthop | Prospective | 48 | Inside-out | 27.0 | 45 | 13.2 | 31 |
Results of syntheses
Comparability was found in mean age, rate of women, time span from injury to surgery, Tegner scale, Lysholm and IKDC scores (P > 0.05). Comparability of the demographic baseline is shown in detail in Table 3
Table 3.
Demographic of the included studies
| Endpoint | All inside | Inside out | MD | P |
|---|---|---|---|---|
| Mean age | 27.8 ± 8.0 | 24.5 ± 6.8 | − 3.35 | 0.07 |
| Women (%) | 35.3 ± 17.8 | 29.1 ± 17.7 | − 6.29 | 0.1 |
| Time from surgery to failure (months) | 21.3 ± 11.4 | 23.3 ± 1.7 | 2.01 | 0.4 |
| Tegner Activity Scale | 4.7 ± 2.0 | 4.1 ± 1.7 | − 0.60 | 0.3 |
| Lysholm score | 60.0 ± 9.3 | 52.3 ± 6.4 | − 7.67 | 0.08 |
| IKDC Score | 40.9 ± 17.5 | 44.4 ± 22.7 | 3.48 | 0.4 |
No difference was found in PROMs: Tegner Activity Scale (P = 0.4), Lysholm score (P = 0.2), IKDC score (P = 0.4) among patients undergoing meniscal repair with all inside or inside-out technique. These results are shown in greater detail in Table 4.
Table 4.
Results of PROMs (MD: mean difference)
| Endpoint | All inside | Inside out | MD | P |
|---|---|---|---|---|
| Tegner Activity Scale | 6.1 ± 0.9 | 6.0 ± 0.9 | − 0.08 | 0.4 |
| Lysholm score | 90.7 ± 5.6 | 89.3 ± 5.1 | − 1.41 | 0.2 |
| IKDC score | 85.5 ± 4.8 | 85.9 ± 4.4 | 0.43 | 0.4 |
The all-inside repair resulted in a greater rate of re-injury (OR 2.7; 95% CI 1.29–5.74; P = 0.009), but also a greater rate of return to play at pre-injury level (OR 2.2; 95% CI 1.48–3.22; P = 0.0001). No difference was found in failures (P = 0.7), chronic pain (P = 0.05), and reoperation (P = 0.1) between the two techniques. No difference was found in the rate of return to play (P = 0.5), and to daily activities (P = 0.1) between the two techniques. These results are shown in greater detail in Table 5.
Table 5.
Results of binary comparisons (MD: mean difference, CI: confidence interval)
| Endpoint | All-Inside | Inside-Out | OR | 95% CI | P |
|---|---|---|---|---|---|
| Failures | 18% (78 of 444) | 17% (167 of 1001) | 1.1 | 0.79–1.43 | 0.7 |
| Re-Injury | 26% (12 of 46) | 11% (35 of 305) | 2.7 | 1.29–5.76 | 0.008 |
| Chronic Pain | 10% (19 of 189) | 5% (9 of 192) | 2.3 | 1.00–5.16 | 0.05 |
| Reoperation | 18% (60 of 329) | 14% (91 of 643) | 1.4 | 0.94–1.93 | 0.1 |
| Return to Play | 84% (16 of 19) | 78% (155 of 199) | 0.7 | 0.18–2.37 | 0.5 |
| Return to daily activities | 85% (163 of 191) | 79% (151 of 191) | 1.5 | 0.90–2.62 | 0.1 |
| Return to play at pre-injury level | 75% (132 of 175) | 58% (289 of 495) | 2.2 | 1.48–3.22 | 0.0001 |
These results are based on the real number of events and observation reported by each single study
Discussion
According to the main findings of the present meta-analysis, arthroscopic all-inside meniscal repair demonstrated a greater rate of re-injury and return to play at the pre-injury level compared to the inside-out meniscal repair technique. Arthroscopic all-inside meniscal repair may be of special interest in patients with a particular interest in a fast return to sport, while, for less demanding patients, the inside-out suture technique may be recommended.
Many surgeons advocate the inside-out technique to repair the meniscus, as it allows a more secure and perpendicular suture at the side of the lesion [76, 77]. Moreover, the inside-out meniscal repair is versatile and can be performed in all types of meniscal tears of the posterior horn or body [78–80]. However, during arthroscopy accessory posteromedial or posterolateral skin incisions are required for the execution of the suture [81, 82]. Using the inside-out technique, sutures are introduced intra-articularly and are knotted on the capsule. In recent times, the all-inside technique has become increasingly popular [83, 84]. Devices have been introduced to allow all-inside meniscal suture [2, 85]. These devices consist of an anchoring component to the meniscal wall with a sliding and self-locking knot, which allows compression of the injured meniscal fragments [73]. These tools make the meniscal suture surgical technique much easier and simpler, reducing surgical time and the risk of neurovascular complications. Regardless of the repair technique, the present study demonstrated an improvement in PROMs in patients undergoing meniscal sutures. However, whether inside-out performs better than the all-inside meniscal repair technique is debated, and no consensus has been reached. According to our findings, patients undergoing all inside meniscal repair demonstrated a greater risk of re-injury but also a greater rate of return to play at the pre-injury level. Previous clinical investigations included in the present study inferred the same conclusions [37, 43, 48, 49, 54, 65, 74, 86]. No further differences in symptoms, failures, and return to normal activities have been evidenced. In the present study, no difference was found in PROMs and rates of surgical failure, chronic pain, and reoperation. No difference was found in the rate of patients unable to return to play and in the rate of return to daily activities. Hence, all inside meniscal repair may be of special interest to patients who desire a fast return to sport, while, for less demanding patients, the inside-out suture technique may be recommended.
We were able to identify only two clinical studies which compared inside-out versus all inside techniques for meniscal repair [41, 69]. Choi et al. [41]conducted a comparative clinical study on 48 consecutive patients who underwent meniscal repairs of longitudinal tears of the posterior horn of the medial meniscus combined with anterior cruciate ligament reconstructions [41]. At approximately three years of follow-up, no difference was found in ROM and meniscal healing at MRI [41]. Lachman test, KT-1000 arthrometer side-to-side differences, Lysholm scores, and Tegner activity scales were also similar between the two groups [41]. One patient in the inside-out group required manipulation, and two patients had limited ROM [41]. Two transient saphenous nerve injuries were observed in the inside-out group [41]. Spindler et al. [69] comparatively assessed 125 arthroscopic meniscal repairs [69]. The rate of failures (meniscal re-operation) was similar between the groups [69]. Both Kaplan–Meier curves and the Cox proportional hazards model evidenced no difference in time to reoperation between techniques [69].
This study has some limitations. The sample size and length of the follow-up were not adequate in some studies. Moreover, 43% (17 of 40) of the included investigations were retrospective, which increases the risk of selection bias in the present study. Only two comparative clinical trials were included, and all other studies were observational studies. The studies which reported the outcomes of meniscal repair were included irrespective of the type and location of the lesion. However; most studies did not report information on these endpoints or did not conduct the analyses of the patients separately. No information was given in relation to the previous conservative management, for example, platelet-rich plasma injection. Rehabilitation protocols were often biased and general health measures were not reported. Procedures for outcome evaluation and subject selection were often biased and unsatisfactorily described. Most authors did not report information on the injury onset (acute or chronic); therefore, no further subgroup analyses were possible. Many authors performed other procedures (e.g. anterior cruciate ligament) in association with the meniscal repair; therefore, results might be not fully generalizable. Further high-quality comparative studies are required to validate the results of the present study in a clinical setting.
Conclusion
Arthroscopic all-inside meniscal repair demonstrated a greater rate of re-injury and return to play at the pre-injury level compared to the inside-out meniscal repair technique. Arthroscopic all-inside meniscal repair may be of special interest in patients who wish for a fast return to sport, while, for less demanding patients, the inside-out suture technique may be recommended. High-quality comparative trials are required to validate these results in a clinical setting and to evaluate the potential of these techniques according to the type and place of the lesion.
Acknowledgements
None.
Abbreviations
- PROMs
Patient-reported outcome measures
- MD
Mean difference
- OR
Odd ratio
- CI
Confidence interval
- IKDC
International knee documentation committee
- CMS
Coleman methodology score
Author contributions
FM conception and design, interpretation of the data, literature search, quality assessment, drafting, final approval; NM: supervision, revision, final approval; FO: supervision, final approval; AB: supervision, final approval; FH: supervision, final approval; GA: drafting, literature search, quality assessment, final approval. All authors have agreed to the final version to be published and agree to be accountable for all aspects of the work.
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors received no financial support for the research, authorship, and/or publication of this article.
Data availability
The datasets generated during and/or analysed during the current study are available throughout the manuscript.
Declarations
Conflcit of interest
The authors declare that they have any competing interests in this article.
Consent to Participate
Not applicable.
Ethical Approval
This study complies with ethical standards.
Consent to publish
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Thompson SR, Miller MD. Miller's Review of Orthopaedics. Incorporated: Elsevier; 2016. [Google Scholar]
- 2.Yik JH, Koh BTH, Wang W. A novel technique for modified all-inside repair of bucket-handle meniscus tears using standard arthroscopic portals. J Orthop Surg Res. 2017;12(1):188. doi: 10.1186/s13018-017-0692-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krych AJ, Reardon PJ, Johnson NR, Mohan R, Peter L, Levy BA, Stuart MJ. Non-operative management of medial meniscus posterior horn root tears is associated with worsening arthritis and poor clinical outcome at 5-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):383–389. doi: 10.1007/s00167-016-4359-8. [DOI] [PubMed] [Google Scholar]
- 4.Becker R, Kopf S, Seil R, Hirschmann MT, Beaufils P, Karlsson J. From meniscal resection to meniscal repair: a journey of the last decade. Knee Surg Sports Traumatol Arthrosc. 2020;28(11):3401–3404. doi: 10.1007/s00167-020-06316-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Migliorini F, Vecchio G, Giorgino R, Eschweiler J, Hildebrand F, Maffulli N. Micro RNA in meniscal ailments: current concepts. Br Med Bull. 2023 doi: 10.1093/bmb/ldac039. [DOI] [PubMed] [Google Scholar]
- 6.Bhatia S, LaPrade CM, Ellman MB, LaPrade RF. Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med. 2014;42(12):3016–3030. doi: 10.1177/0363546514524162. [DOI] [PubMed] [Google Scholar]
- 7.Saltzman BM, Cotter EJ, Wang KC, Rice R, Manning BT, Yanke AB, Forsythe B, Verma NN, Cole BJJC (2020) Arthroscopically repaired bucket-handle meniscus tears: patient demographics, postoperative outcomes, and a comparison of success and failure cases. 11 (1):77–87 [DOI] [PMC free article] [PubMed]
- 8.S.B.S. K, Karthik Vishwanathan K, S. S (2022) Inside-out meniscal repair using a long hollow needle-A cost effective technique. J Orthop Rep 1 (2):100018. 10.1016/j.jorep.2022.03.018
- 9.Migliorini F, Cuozzo F, Cipollaro L, Oliva F, Hildebrand F, Maffulli N. Platelet-rich plasma (PRP) augmentation does not result in more favourable outcomes in arthroscopic meniscal repair: a meta-analysis. J Orthop Traumatol. 2022;23(1):8. doi: 10.1186/s10195-022-00630-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilson PL, Wyatt CW, Romero J, Sabatino MJ, Ellis HB. Incidence, presentation, and treatment of pediatric and adolescent meniscal root injuries. Orthop J Sports Med. 2018;6(11):2325967118803888. doi: 10.1177/2325967118803888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kurzweil PR, Cannon WD, DeHaven KE. Meniscus Repair and Replacement. Sports Med Arthrosc Rev. 2018;26(4):160–164. doi: 10.1097/jsa.0000000000000224. [DOI] [PubMed] [Google Scholar]
- 12.Wells ME, Scanaliato JP, Dunn JC, Garcia EJ. Meniscal injuries: mechanism and classification. Sports Med Arthrosc Rev. 2021;29(3):154–157. doi: 10.1097/jsa.0000000000000311. [DOI] [PubMed] [Google Scholar]
- 13.Sahanand KS, Pandian P, D.V. R (2022) Two case reports of ring lateral meniscus—A rare anatomical variant. J Orthop Rep 1 (1):13-15. doi:10.1016/j.jorep.2022.03.017
- 14.Michalitsis S, Vlychou M, Malizos KN, Thriskos P, Hantes ME. Meniscal and articular cartilage lesions in the anterior cruciate ligament-deficient knee: correlation between time from injury and knee scores. Knee Surg Sports Traumatol ArthroscX. 2015;23(1):232–239. doi: 10.1007/s00167-013-2497-9. [DOI] [PubMed] [Google Scholar]
- 15.Braaten JA, Schreier FJ, Rodriguez AN, Monson J, LaPrade RF. Modern treatment principles for multiligament knee injuries. The archives of bone and joint surgery. 2022;10(11):937–950. doi: 10.22038/abjs.2021.60188.2971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Raj MA, Bubnis MA (2021) Knee Meniscal Tears. In: StatPearls. StatPearls Publishing [PubMed]
- 17.Copyright © 2021, StatPearls Publishing LLC., Treasure Island (FL),
- 18.Castle JP, Khalil LS, Abbas MJ, DeBolle S, Tandron M, Cross AG, Rodriguez GA, Okoroha KR. Maximum subjective outcome improvement is reported by 3 months following arthroscopic partial meniscectomy: a systematic review. J Orthop. 2022;31:78–85. doi: 10.1016/j.jor.2022.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Migliorini F, Oliva F, Eschweiler J, Cuozzo F, Hildebrand F, Maffulli N. No evidence in support of arthroscopic partial meniscectomy in adults with degenerative and nonobstructive meniscal symptoms: a level I evidence-based systematic review. Knee Surg Sports Traumatol Arthrosc. 2022 doi: 10.1007/s00167-022-07040-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jones MH, Spindler KP, Fleming BC, Duryea J, Obuchowski NA, Scaramuzza EA, Oksendahl HL, Winalski CS, Duong CL, Huston LJ, Parker RD, Kaeding CC, Andrish JT, Flanigan DC, Dunn WR, Reinke EK. Meniscus treatment and age associated with narrower radiographic joint space width 2–3 years after ACL reconstruction: data from the MOON onsite cohort. Osteoarthritis Cartilage. 2015;23(4):581–588. doi: 10.1016/j.joca.2014.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kurzweil PR, Cannon WD, DeHaven KE. Meniscus Repair and Replacement. 2018;26(4):160–164. doi: 10.1097/jsa.0000000000000224. [DOI] [PubMed] [Google Scholar]
- 22.Wasserburger JN, Shultz CL, Hankins DA, Korcek L, Martin DF, Amendola A, Richter DL, Schenck RC, Treme GP. Long-term Natl Trends Arthrosc Meniscal Repair Debridement. 2021;49(6):1530–1537. doi: 10.1177/0363546521999419. [DOI] [PubMed] [Google Scholar]
- 23.Samuelsen BT, Johnson NR, Hevesi M, Levy BA, Dahm DL, Stuart MJ, Krych AJJOjosm (2018) Comparative outcomes of all-inside versus inside-out repair of bucket-handle meniscal tears: a propensity-matched analysis. 6 (6):2325967118779045 [DOI] [PMC free article] [PubMed]
- 24.Westermann RW, Duchman KR, Amendola A, Glass N, Wolf BR. All-inside versus inside-out meniscal repair with concurrent anterior cruciate ligament reconstruction: a meta-regression analysis. Am J Sports Med. 2016;45(3):719–724. doi: 10.1177/0363546516642220. [DOI] [PubMed] [Google Scholar]
- 25.Faucett SC, Geisler BP, Chahla J, Krych AJ, Kurzweil PR, Garner AM, Liu S, LaPrade RF, Pietzsch JB. Meniscus root repair vs meniscectomy or nonoperative management to prevent knee osteoarthritis after medial meniscus root tears: clinical and economic effectiveness. Am J Sports Med. 2019;47(3):762–769. doi: 10.1177/0363546518755754. [DOI] [PubMed] [Google Scholar]
- 26.Hupperich A, Salzmann G, Niemeyer P, Feucht M, Eberbach H, Südkamp N, Kühle JJAoo, surgery t (2018) What are the factors to affect outcome and healing of meniscus bucket handle tears? 138:1365–1373 [DOI] [PubMed]
- 27.Annandale T. An operation for displaced semilunar cartilage. BMJ. 1885;1(1268):779. doi: 10.1136/bmj.1.1268.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ikeuchi H. Meniscus surgery using the Watanabe arthroscope. Orthop Clin North Am. 1979;10(3):629–642. doi: 10.1016/S0030-5898(20)30756-2. [DOI] [PubMed] [Google Scholar]
- 29.Aşík M, Sener N. Failure strength of repair devices versus meniscus suturing techniques. Knee Surg Sports Traumatol Arthrosc. 2002;10(1):25–29. doi: 10.1007/s001670100247. [DOI] [PubMed] [Google Scholar]
- 30.Albrecht-Olsen P, Kristensen G, Burgaard P, Joergensen U, Toerholm C (1999) The arrow versus horizontal suture in arthroscopic meniscus repair. A prospective randomized study with arthroscopic evaluation. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA 7 (5):268–273. doi:10.1007/s001670050162 [DOI] [PubMed]
- 31.Engler ID, Moradian JR, Pockros BM, Schirmeister CM, Richmond JC, Salzler MJ. Patient-reported outcomes of meniscal repair and meniscectomy in patients 40 years of age and older show similar good results. Knee Surg Sports Traumatol Arthrosc. 2021;29(9):2911–2917. doi: 10.1007/s00167-020-06299-5. [DOI] [PubMed] [Google Scholar]
- 32.Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535. doi:10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed]
- 33.Howick J CI, Glasziou P, Greenhalgh T, Heneghan C, Liberati A, Moschetti I, Phillips B, Thornton H, Goddard O, Hodgkinson M (2011) The 2011 Oxford Levels of Evidence. Oxford Centre for Evidence-Based Medicine Available at https://www.cebmnet/indexaspx?o=5653
- 34.Irrgang JJAA, Boland AL, et al. Development and valida- tion of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29:600–613. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 35.Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10(3):150–154. doi: 10.1177/036354658201000306. [DOI] [PubMed] [Google Scholar]
- 36.Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med. 2009;37(5):890–897. doi: 10.1177/0363546508330143. [DOI] [PubMed] [Google Scholar]
- 37.Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD (2000) Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scandinavian journal of medicine & science in sports 10 (1):2–11. doi:10.1034/j.1600-0838.2000.010001002.x [DOI] [PubMed]
- 38.Ahn JH, Kim KI, Wang JH, Kyung BS, Seo MC, Lee SH. Arthroscopic repair of bucket-handle tears of the lateral meniscus. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):205–210. doi: 10.1007/s00167-013-2764-9. [DOI] [PubMed] [Google Scholar]
- 39.Barber FA, Coons DA. Midterm results of meniscal repair using the BioStinger meniscal repair device. Arthroscopy. 2006;22(4):400–405. doi: 10.1016/j.arthro.2005.08.052. [DOI] [PubMed] [Google Scholar]
- 40.Bryant D, Dill J, Litchfield R, Amendola A, Giffin R, Fowler P, Kirkley A. Effectiveness of bioabsorbable arrows compared with inside-out suturing for vertical, reparable meniscal lesions: a randomized clinical trial. Am J Sports Med. 2007;35(6):889–896. doi: 10.1177/0363546506298582. [DOI] [PubMed] [Google Scholar]
- 41.Chiang CW, Chang CH, Cheng CY, Chen AC, Chan YS, Hsu KY, Chen WJ. Clinical results of all-inside meniscal repair using the FasT-Fix meniscal repair system. Chang Gung Med J. 2011;34(3):298–305. [PubMed] [Google Scholar]
- 42.Choi NH, Kim TH, Victoroff BN. Comparison of arthroscopic medial meniscal suture repair techniques: inside-out versus all-inside repair. Am J Sports Med. 2009;37(11):2144–2150. doi: 10.1177/0363546509339010. [DOI] [PubMed] [Google Scholar]
- 43.Sallé de Chou E, Pujol N, Rochcongar G, Cucurulo T, Potel JF, Dalmay F, Ehkirch FP, Laporte C, Le Henaff G, Seil R, Lutz C, Gunepin FX, Sonnery-Cottet B. Analysis of short and long-term results of horizontal meniscal tears in young adults. Orthopaedics Traumatol Surg Res. 2015;101(8 Suppl):S317–322. doi: 10.1016/j.otsr.2015.09.009. [DOI] [PubMed] [Google Scholar]
- 44.Alvarez-Diaz P, Alentorn-Geli E, Llobet F, Granados N, Steinbacher G, Cugat R. Return to play after all-inside meniscal repair in competitive football players: a minimum 5-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2016;24(6):1997–2001. doi: 10.1007/s00167-014-3285-x. [DOI] [PubMed] [Google Scholar]
- 45.Gallacher PD, Gilbert RE, Kanes G, Roberts SN, Rees D. White on white meniscal tears to fix or not to fix? Knee. 2010;17(4):270–273. doi: 10.1016/j.knee.2010.02.016. [DOI] [PubMed] [Google Scholar]
- 46.Hagino T, Ochiai S, Watanabe Y, Senga S, Wako M, Ando T, Sato E, Haro H. Clinical results of arthroscopic all-inside lateral meniscal repair using the Meniscal Viper Repair System. Euro J Orthopaedic Surg Traumatol. 2014;24(1):99–104. doi: 10.1007/s00590-012-1138-1. [DOI] [PubMed] [Google Scholar]
- 47.Haklar U, Kocaoglu B, Nalbantoglu U, Tuzuner T, Guven O. Arthroscopic repair of radial lateral meniscus [corrected] tear by double horizontal sutures with inside-outside technique. Knee. 2008;15(5):355–359. doi: 10.1016/j.knee.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 48.Hetsroni I, Lillemoe K, Marx RG. Small medial meniscocapsular separations: a potential cause of chronic medial-side knee pain. Arthroscopy. 2011;27(11):1536–1542. doi: 10.1016/j.arthro.2011.06.025. [DOI] [PubMed] [Google Scholar]
- 49.Hirtler L, Unger J, Weninger P. Acute and chronic menisco-capsular separation in the young athlete: diagnosis, treatment and results in thirty seven consecutive patients. Int Orthop. 2015;39(5):967–974. doi: 10.1007/s00264-014-2657-7. [DOI] [PubMed] [Google Scholar]
- 50.Järvelä S, Sihvonen R, Sirkeoja H, Järvelä T. All-inside meniscal repair with bioabsorbable meniscal screws or with bioabsorbable meniscus arrows: a prospective, randomized clinical study with 2-year results. Am J Sports Med. 2010;38(11):2211–2217. doi: 10.1177/0363546510374592. [DOI] [PubMed] [Google Scholar]
- 51.Kamimura T, Kimura M. Meniscal repair of degenerative horizontal cleavage tears using fibrin clots: clinical and arthroscopic outcomes in 10 cases. Orthop J Sports Med. 2014;2(11):2325967114555678. doi: 10.1177/2325967114555678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kise NJ, Drogset JO, Ekeland A, Sivertsen EA, Heir S. All-inside suture device is superior to meniscal arrows in meniscal repair: a prospective randomized multicenter clinical trial with 2-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):211–218. doi: 10.1007/s00167-014-3423-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kotsovolos ES, Hantes ME, Mastrokalos DS, Lorbach O, Paessler HH. Results of all-inside meniscal repair with the FasT-Fix meniscal repair system. Arthrosc. 2006;22(1):3–9. doi: 10.1016/j.arthro.2005.10.017. [DOI] [PubMed] [Google Scholar]
- 54.Krych AJ, McIntosh AL, Voll AE, Stuart MJ, Dahm DL. Arthroscopic repair of isolated meniscal tears in patients 18 years and younger. Am J Sports Med. 2008;36(7):1283–1289. doi: 10.1177/0363546508314411. [DOI] [PubMed] [Google Scholar]
- 55.Krych AJ, Pitts RT, Dajani KA, Stuart MJ, Levy BA, Dahm DL. Surgical repair of meniscal tears with concomitant anterior cruciate ligament reconstruction in patients 18 years and younger. Am J Sports Med. 2010;38(5):976–982. doi: 10.1177/0363546509354055. [DOI] [PubMed] [Google Scholar]
- 56.Logan M, Watts M, Owen J, Myers P. Meniscal repair in the elite athlete: results of 45 repairs with a minimum 5-year follow-up. Am J Sports Med. 2009;37(6):1131–1134. doi: 10.1177/0363546508330138. [DOI] [PubMed] [Google Scholar]
- 57.Lucas G, Accadbled F, Violas P, Sales de Gauzy J, Knörr J. Isolated meniscal injuries in paediatric patients: outcomes after arthroscopic repair. Orthopaedics Traumatol Surg Res. 2015;101(2):173–177. doi: 10.1016/j.otsr.2014.12.006. [DOI] [PubMed] [Google Scholar]
- 58.Moatshe G, Cinque ME, Godin JA, Vap AR, Chahla J, LaPrade RF. Comparable outcomes after bucket-handle meniscal repair and vertical meniscal repair can be achieved at a minimum 2 years' follow-up. Am J Sports Med. 2017;45(13):3104–3110. doi: 10.1177/0363546517719244. [DOI] [PubMed] [Google Scholar]
- 59.Nakayama H, Kanto R, Kambara S, Kurosaka K, Onishi S, Yoshiya S, Yamaguchi M. Clinical outcome of meniscus repair for isolated meniscus tear in athletes. Asia-Pacific J Sports Med Arthrosc Rehabilit Technol. 2017;10:4–7. doi: 10.1016/j.asmart.2017.05.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Noyes FR, Barber-Westin SD. Arthroscopic repair of meniscal tears extending into the avascular zone in patients younger than twenty years of age. Am J Sports Med. 2002;30(4):589–600. doi: 10.1177/03635465020300042001. [DOI] [PubMed] [Google Scholar]
- 61.Noyes FR, Chen RC, Barber-Westin SD, Potter HG. Greater than 10-year results of red-white longitudinal meniscal repairs in patients 20 years of age or younger. Am J Sports Med. 2011;39(5):1008–1017. doi: 10.1177/0363546510392014. [DOI] [PubMed] [Google Scholar]
- 62.Albrecht-Olsen PM, Bak K (1993) Arthroscopic repair of the bucket-handle meniscus. 10 failures in 27 stable knees followed for 3 years. Acta Orthop Scand 64 (4):446–448. 10.3109/17453679308993664 [DOI] [PubMed]
- 63.Papachristou G, Efstathopoulos N, Plessas S, Levidiotis C, Chronopoulos E, Sourlas J. Isolated meniscal repair in the avascular area. Acta Orthop Belg. 2003;69(4):341–345. [PubMed] [Google Scholar]
- 64.Perdue PS, Jr, Hummer CD, 3rd, Colosimo AJ, Heidt RS, Jr, Dormer SG. Meniscal repair: outcomes and clinical follow-up. Arthroscopy. 1996;12(6):694–698. doi: 10.1016/s0749-8063(96)90172-3. [DOI] [PubMed] [Google Scholar]
- 65.Popescu D, Sastre S, Garcia AI, Tomas X, Reategui D, Caballero M. MR-arthrography assessment after repair of chronic meniscal tears. Knee Surg Sports Traumatol Arthrosc. 2015;23(1):171–177. doi: 10.1007/s00167-013-2552-6. [DOI] [PubMed] [Google Scholar]
- 66.Pujol N, Bohu Y, Boisrenoult P, Macdes A, Beaufils P. Clinical outcomes of open meniscal repair of horizontal meniscal tears in young patients. Knee Surg Sports Traumatol Arthrosc. 2013;21(7):1530–1533. doi: 10.1007/s00167-012-2099-y. [DOI] [PubMed] [Google Scholar]
- 67.Raza H, Abbas K, Umer M. Arthroscopic repair of meniscal tears with inside-out technique. JPMA J Pakistan Medical Assoc. 2011;61(1):10–14. [PubMed] [Google Scholar]
- 68.Espejo-Reina A, Serrano-Fernández JM, Martín-Castilla B, Estades-Rubio FJ, Briggs KK, Espejo-Baena A. Outcomes after repair of chronic bucket-handle tears of medial meniscus. Arthroscopy. 2014;30(4):492–496. doi: 10.1016/j.arthro.2013.12.020. [DOI] [PubMed] [Google Scholar]
- 69.Schmitt A, Batisse F, Bonnard C. Results with all-inside meniscal suture in pediatrics. Orthopaedics Traumatol Surg Res. 2016;102(2):207–211. doi: 10.1016/j.otsr.2015.12.018. [DOI] [PubMed] [Google Scholar]
- 70.Spindler KP, McCarty EC, Warren TA, Devin C, Connor JT. Prospective comparison of arthroscopic medial meniscal repair technique: inside-out suture versus entirely arthroscopic arrows. Am J Sports Med. 2003;31(6):929–934. doi: 10.1177/03635465030310063101. [DOI] [PubMed] [Google Scholar]
- 71.Steadman JR, Matheny LM, Singleton SB, Johnson NS, Rodkey WG, Crespo B, Briggs KK. Meniscus suture repair: minimum 10-year outcomes in patients younger than 40 years compared with patients 40 and older. Am J Sports Med. 2015;43(9):2222–2227. doi: 10.1177/0363546515591260. [DOI] [PubMed] [Google Scholar]
- 72.Stein T, Mehling AP, Welsch F, von Eisenhart-Rothe R, Jäger A. Long-term outcome after arthroscopic meniscal repair versus arthroscopic partial meniscectomy for traumatic meniscal tears. Am J Sports Med. 2010;38(8):1542–1548. doi: 10.1177/0363546510364052. [DOI] [PubMed] [Google Scholar]
- 73.Tengrootenhuysen M, Meermans G, Pittoors K, van Riet R, Victor J. Long-term outcome after meniscal repair. Knee Surg Sports Traumatol Arthrosc. 2011;19(2):236–241. doi: 10.1007/s00167-010-1286-y. [DOI] [PubMed] [Google Scholar]
- 74.Tiftikci U, Serbest S. Repair of isolated horizontal meniscal tears with all-inside suture materials using the overlock method: outcome study with a minimum 2-year follow-up. J Orthop Surg Res. 2016;11(1):131. doi: 10.1186/s13018-016-0466-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tucciarone A, Godente L, Fabbrini R, Garro L, Salate Santone F, Chillemi C. Meniscal tear repaired with Fast-Fix sutures: clinical results in stable versus ACL-deficient knees. Arch Orthop Trauma Surg. 2012;132(3):349–356. doi: 10.1007/s00402-011-1391-5. [DOI] [PubMed] [Google Scholar]
- 76.Vanderhave KL, Moravek JE, Sekiya JK, Wojtys EM. Meniscus tears in the young athlete: results of arthroscopic repair. J Pediatr Orthop. 2011;31(5):496–500. doi: 10.1097/BPO.0b013e31821ffb8d. [DOI] [PubMed] [Google Scholar]
- 77.Chahla J, Serra Cruz R, Cram TR, Dean CS, LaPrade RF. Inside-out meniscal repair: medial and lateral approach. Arthrosc Tech. 2016;5(1):e163–168. doi: 10.1016/j.eats.2015.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Connaughton AJ, Geeslin AG, Uggen CW. All-inside ACL reconstruction: How does it compare to standard ACL reconstruction techniques? J Orthop. 2017;14(2):241–246. doi: 10.1016/j.jor.2017.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Nelson CG, Bonner KF. Inside-out Meniscus Repair Arthrosc Tech. 2013;2(4):e453–460. doi: 10.1016/j.eats.2013.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Laible C, Stein DA, Kiridly DN. Meniscal repair. J Am Acad Orthop Surg. 2013;21(4):204–213. doi: 10.5435/jaaos-21-04-204. [DOI] [PubMed] [Google Scholar]
- 81.Yoon KH, Park KH. Meniscal repair. Knee Surg Related Res. 2014;26(2):68–76. doi: 10.5792/ksrr.2014.26.2.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Johnson D, Weiss B. Meniscal repair using the inside-out suture technique. Sports Med Arthrosc Rev. 2012;20(2):68–76. doi: 10.1097/JSA.0b013e318252ea26. [DOI] [PubMed] [Google Scholar]
- 83.Dzidzishvili L, López-Torres I, Sáez D, Arguello M, Calvo E. A comparison of the transtibial pullout technique and all-inside meniscal repair in medial meniscus posterior root tear: Prognostic factors and midterm clinical outcomes. J Orthop. 2021;26:130–134. doi: 10.1016/j.jor.2021.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zimmerer A, Sobau C, Nietschke R, Schneider M, Ellermann A. Long-term outcome after all inside meniscal repair using the FasT-Fix system. J Orthop. 2018;15(2):602–605. doi: 10.1016/j.jor.2018.05.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tiftikci U, Serbest S. Does the location of placement of meniscal sutures have a clinical effect in the all-inside repair of meniscocapsular tears? J Orthop Surg Res. 2017;12(1):87. doi: 10.1186/s13018-017-0591-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hung CH, Kuo YF, Chen YJ, Yeh PC, Cho HY, Chen YJ. Comparative outcomes between all-inside arthroscopic suture anchor technique versus arthroscopic transosseous suture technique in patients with triangular fibrocartilage complex tear: a retrospective comparative study. J Orthop Surg Res. 2021;16(1):600. doi: 10.1186/s13018-021-02752-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hantes ME, Zachos VC, Varitimidis SE, Dailiana ZH, Karachalios T, Malizos KN. Arthroscopic meniscal repair: a comparative study between three different surgical techniques. Knee Surg Sports Traumatol Arthrosc. 2006;14(12):1232–1237. doi: 10.1007/s00167-006-0094-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analysed during the current study are available throughout the manuscript.