Abstract
A 74-year-old man after multiple mitral valve surgeries underwent catheter ablation of a bi-atrial tachycardia (BiAT). Ultra-high resolution activation mapping exhibited a reentrant circuit propagating around the inferior to anterior mitral annulus and right atrial (RA) septum with two interatrial connections. At the transeptal puncture site, continuous fractionated electrograms were recorded during the BiAT, and entrainment pacing revealed a post-pacing interval similar to the tachycardia cycle length, which suggested that the interatrial conduction from the RA to the left atrium (LA) was located just at the transseptal puncture site. A radiofrequency application inside the transseptal puncture hole could successfully eliminate the BiAT. The ablation target for BiATs propagating around the mitral annulus and RA septum is generally the anatomical mitral isthmus (MI). Since the present case had multiple incisions on both the RA and LA septum due to mitral valve surgeries, there was the possibility of the occurrence of a BiAT including the RA and LA septum after performing an MI linear ablation. Therefore, the preferable ablation target for the BiAT in the present case appeared to be the interatrial connection. Ultra-high resolution detailed mapping not only on the atrial endocardium but also in the transseptal puncture hole may be useful for identifying a critical interatrial connection of BiAT circuits.
Keywords: Atrial tachycardia, Bi-atrial tachycardia, Catheter ablation, Interatrial connection, Transseptal puncture, Ultra-high resolution mapping
1. Introduction
Some atrial tachycardias (ATs) after a catheter-based or surgical ablation of atrial fibrillation (AF) include both the right and left atria (RA/LA) in reentrant circuits with two interatrial connections, which are called bi-atrial tachycardias (BiATs) [[1], [2], [3], [4]]. During catheter ablation of a type of BiAT including the mitral annulus (MA) in the LA circuit and the RA septum in the RA circuit, the endpoint of the ablation is generally the creation of complete conduction block along the mitral isthmus (MI) between the electrically isolated pulmonary veins (PVs) and MA [1,4]. On the other hand, a type of BiAT with a circuit using the RA septum and LA septum is treated with minimal linear or point ablation in order to minimize the risk of an intra-atrial conduction delay or atrioventricular block due to atrial septal ablation [1,2,5]. We present a case of a BiAT with multiple atrial septal incisions due to mitral valve surgeries that had a reentrant circuit using the mitral annulus and RA septum. Since ultra-high resolution mapping identified a critical interatrial connection just at the transseptal puncture site, the BiAT could be successfully treated by radiofrequency ablation targeting the interatrial connection within the transseptal puncture hole.
2. Case report
A 74-year-old man with a total of three mitral valve surgeries due to mitral valve regurgitation and artificial valve dysfunction underwent a first radiofrequency catheter ablation of persistent AF and AT with a tachycardia cycle length (TCL) of 280 ms (Fig. 1A). After performing a PV isolation and posterior LA linear ablation, ultra-high resolution activation mapping during the AT using the Rhythmia system (Boston Scientific, Marlborough, MA) with a mini-basket catheter (IntellaMap Orion, Boston Scientific) suggested a BiAT with a reentrant circuit using the inferior, lateral, and anterior MA in the LA and RA septum with two interatrial connections (Fig. 1, Supplemental Video 1). The post-pacing interval (PPI) was almost similar to the TCL upon entrainment from the inferior to anterior MA and posterior RA septum but was not upon entrainment from the LA septum and anterior RA septum. Radiofrequency applications on the high RA septum, corresponding to the earliest activation site in the RA, terminated the BiAT after gradual prolongation of the TCL. However, the same BiAT with a longer TCL than originally noted was induced easily and repeatedly. During the BiAT, continuous fractionated electrograms were recorded by the mini-basket catheter placed at the transseptal puncture site, and entrainment pacing at that site revealed a PPI similar to the TCL (Fig. 2). The BiAT terminated 12 seconds after commencement of the radiofrequency application inside the transseptal puncture hole using a 4 mm-tip externally irrigated ablation catheter capable of contact force (CF)-sensing and local impedance (LI)-monitoring (IntellaNav StablePoint; Boston Scientific) (Fig. 3, Supplemental Videos 2 and 3). During the radiofrequency application that terminated the BiAT, the mean CF was 7 g, maximum power output delivered 40 W, radiofrequency duration 40 seconds, and LI drop 24 Ω. An additional radiofrequency application was performed at the BiAT termination site with a mean CF of 16 g and mean and maximum power outputs of 43 W and 50 W, respectively, radiofrequency duration of 30 seconds, and LI drop of 38 Ω. Thereafter, no ATs could be further induced by any atrial programmed or burst pacing. The patient has had no AF/AT recurrences during an eight-month follow-up period.
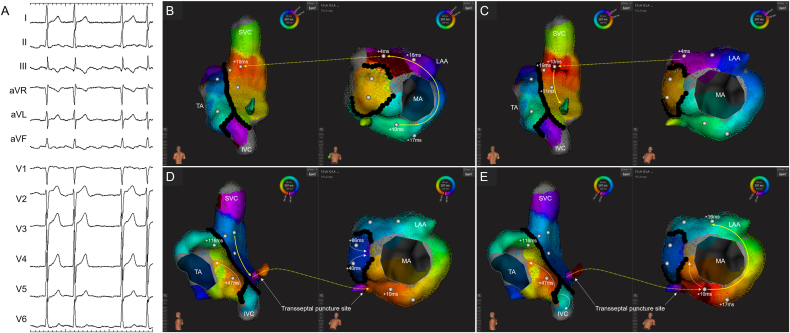
Fig. 1.
(A) Twelve-lead electrocardiogram and (B–E) activation maps during the BiAT. The activation wavefront propagated from the inferior to anterior MA counterclockwise, then from the anterior MA to the high RA septum via the upper interatrial connection and returned to the inferior MA via the lower interatrial connection just at the transseptal puncture site. The yellow solid and dotted arrows represent the endocardial and interatrial conduction in the BiAT circuit, respectively, and the white arrows represent the endocardial conduction outside the BiAT circuit. The black and white tags and numbers on the maps indicate the conduction block, entrainment pacing sites, and PPI interval minus the TCL, respectively.
Abbreviations: IVC, inferior vena cava; LAA, left atrial appendage; LIPV, left inferior pulmonary vein (PV); LSPV, left superior PV; MA, mitral annulus; RIPV, right inferior PV; RSPV, right superior PV; SVC, superior vena cava; TA, tricuspid annulus.
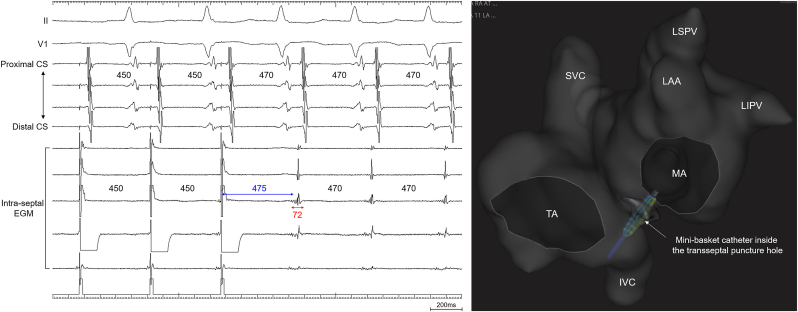
Fig. 2.
Entrainment pacing from a mini-basket catheter placed inside the transseptal puncture hole, where continuous fractionated electrograms with a duration of 72 ms were recorded during the BiAT. The right panel shows the position of the mini-basket catheter on the three-dimensional geometry.
Abbreviations: CS, coronary sinus recordings, Intra-septal EGM, intracardiac electrograms recorded by the mini-basket catheter. The other abbreviations are as in Fig. 1.
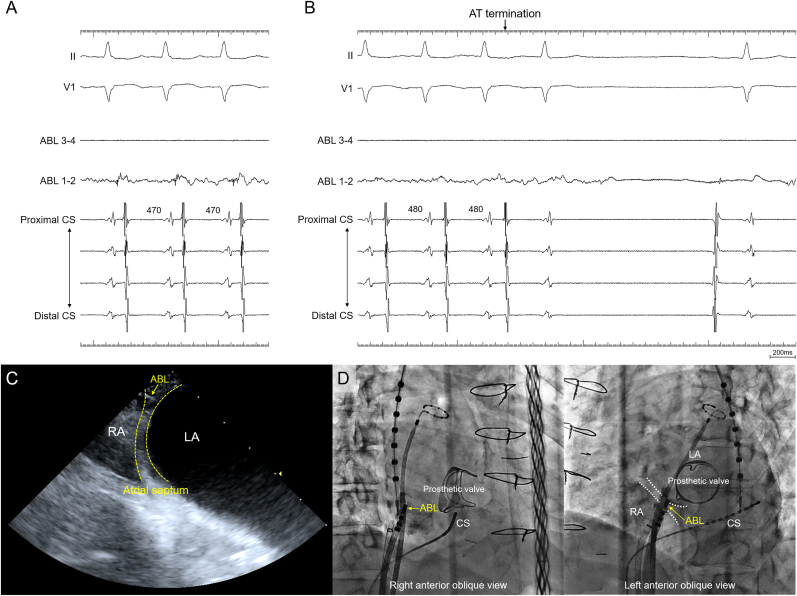
Fig. 3.
Body surface and intracardiac electrocardiograms (A) just before commencing the radiofrequency application inside the transseptal puncture hole during the BiAT and (B) when the BiAT terminated. Continuous fractionated electrograms were recorded by the ablation catheter placed at the transseptal puncture site during the BiAT. (C) The intracardiac echocardiographic image and (D) right and left anterior oblique fluoroscopic images showing the position of the ablation catheter during the radiofrequency application that terminated the BiAT.
Abbreviations: ABL, the tip of the ablation catheter; ABL 1–2 and 3–4, distal and proximal ablation catheter recordings. The other abbreviations are as in Fig. 1, Fig. 2.
Supplementary video related to this article can be found at https://doi.org/10.1016/j.ipej.2023.08.001
The following is/are the supplementary data related to this article:
Propagation maps exhibiting a BiAT propagating from the inferior to anterior MA counterclockwise, then from the anterior MA to the high RA septum via the upper interatrial connection, probably corresponding to Bachmann's bundle, and returning to the inferior MA via the lower interatrial connection just at the transseptal puncture site. The dark red on the maps represents the activation wavefront. The yellow solid and dotted arrows represent the endocardial and interatrial conduction in the BiAT circuit, respectively, and the white arrows represent the endocardial conduction outside the BiAT circuit. The confidence mask for the videos was set at 0.03 mV. The abbreviations are as in Fig. 1.
Intracardiac echocardiography showing the position of the ablation catheter placed inside the transseptal puncture hole (yellow arrow). The abbreviations are as in Fig. 1.
Simultaneous right and left atriography showing the position of the ablation catheter placed inside the transseptal puncture hole in the right and left anterior oblique views. The abbreviations are as in Fig. 2.
3. Discussion
This was a case report demonstrating that during catheter ablation of a BiAT with multiple atrial septal incisions due to multiple mitral valve surgeries, a critical interatrial connection was identified at the transseptal puncture site by ultra-high resolution mapping, and radiofrequency ablation targeting the interatrial connection from the RA to the LA successfully treated the BiAT. To the best of our knowledge, few studies have reported the successful elimination of a critical interatrial connection of BiATs by radiofrequency ablation inside the transseptal puncture hole.
In general, the ablation target for BiATs propagating around the mitral annulus and RA septum is the anatomical MI, while BiATs with a circuit using the RA septum and LA septum are treated with minimal linear or a point ablation on the atrial septum [[1], [2], [3], [4], [5]]. Since the present case had multiple incisions on both the RA and LA septum after a total of three mitral valve surgeries, there was the possibility of the occurrence of an iatrogenic BiAT including the RA septum and LA septum after performing an MI linear ablation. Therefore, the preferable ablation target for the BiAT in the present case appeared to be the interatrial connections: one was located on the high atrial septum probably via Bachmann's bundle, and the other was located just at the transseptal puncture site. The initial ablation target was the interatrial connection from the LA to the RA on the high atrial septum, because the earliest activation site in the LA during the BiAT appeared to be located near the atrioventricular node. RF applications on the high RA septum could terminate the BiAT but could not completely eliminate the BiAT. Finally, we targeted the interatrial connection from the RA to the LA at the transseptal puncture site for the ablation, and a radiofrequency application inside the transseptal puncture hole successfully eliminated the BiAT. This case report suggested that ultra-high resolution mapping not only on the atrial endocardium but also in the transseptal puncture hole may be useful for identifying a critical interatrial connection of BiAT circuits.
Funding sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgment
We would like to thank Mr. John Martin and Mr. Ryoya Takeuchi for their help in the preparation of the manuscript.
Footnotes
Peer review under responsibility of Indian Heart Rhythm Society.
References
- 1.Kitamura T., Martin R., Denis A., et al. Characteristics of single-loop macroreentrant biatrial tachycardia diagnosed by ultrahigh-resolution mapping system. Circ Arrhythm Electrophysiol. 2018;11 doi: 10.1161/CIRCEP.117.005558. [DOI] [PubMed] [Google Scholar]
- 2.Zhang J., Hu W., Zhao A., et al. Macroreentrant biatrial tachycardia relevant to interatrial septal incisions after mitral valve surgery: electrophysiological characteristics and ablation strategy. Heart Rhythm. 2020;17:2135–2144. doi: 10.1016/j.hrthm.2020.06.031. [DOI] [PubMed] [Google Scholar]
- 3.Mikhaylov E.N., Mitrofanova L.B., Vander M.A., et al. Biatrial tachycardia following linear anterior wall ablation for the perimitral reentry: incidence and electrophysiological evaluations. J Cardiovasc Electrophysiol. 2015;26:28–35. doi: 10.1111/jce.12543. [DOI] [PubMed] [Google Scholar]
- 4.Lai Y., Guo Q., Sang C., et al. Revisiting the characteristics and ablation strategy of biatrial tachycardias: a case series and systematic review. Europace. 2023;25:905–913. doi: 10.1093/europace/euac231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hara S., Kusa S., Miwa N., et al. Treatment of atrial tachycardia arising after superior transseptal approach mitral valve surgery: insights from ultra-high-density mapping to prevent atrioventricular block. Pacing Clin Electrophysiol. 2022;45:1042–1050. doi: 10.1111/pace.14569. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Propagation maps exhibiting a BiAT propagating from the inferior to anterior MA counterclockwise, then from the anterior MA to the high RA septum via the upper interatrial connection, probably corresponding to Bachmann's bundle, and returning to the inferior MA via the lower interatrial connection just at the transseptal puncture site. The dark red on the maps represents the activation wavefront. The yellow solid and dotted arrows represent the endocardial and interatrial conduction in the BiAT circuit, respectively, and the white arrows represent the endocardial conduction outside the BiAT circuit. The confidence mask for the videos was set at 0.03 mV. The abbreviations are as in Fig. 1.
Intracardiac echocardiography showing the position of the ablation catheter placed inside the transseptal puncture hole (yellow arrow). The abbreviations are as in Fig. 1.
Simultaneous right and left atriography showing the position of the ablation catheter placed inside the transseptal puncture hole in the right and left anterior oblique views. The abbreviations are as in Fig. 2.