Abstract
Objective: This study was designed to explore the efficacy of comprehensive nursing intervention in elderly patients with severe heart failure (SHF) treated by recombinant human brain natriuretic peptide (rh-BNP). Methods: A retrospective analysis was made on 131 patients with SHF treated with rh-BNP in Wuhan Asia Cardiology Hospital from May 2019 to May 2022. Of them, 71 patients who received routine nursing care between May 2019 and December 2021 were assigned to the control group, and 60 patients who received comprehensive nursing between January 2022 and May 2022 were assigned to the observation group. The changes in quality of life (QoL) before and after nursing and the occurrence of adverse events after nursing were counted and compared between the two groups. The two groups were compared reagarding changes in anxiety and depression scores before and after nursing, as well as hospitalization expenses and hospitalization time. The left ventricular end-diastolic volume (LVEDV) and left ventricular ejection fraction (LVEF) of patients were determined. The nursing satisfaction of the two groups was evaluated. Additionally, logistic regression was carried out to analyze the risk factors for adverse events. Results: The control group had lower QoL scores than the observation group after nursing (P < 0.0001). The control group got significantly higher self-rating anxiety scale (SAS) and self-rating depression scale (SDS) scores than the observation group (P < 0.0001). The control group showed lower levels of LVEDV and LVEF than the observation group (P < 0.0001). The control group experienced greatly longer hospitalization time than the observation group, and also had a higher hospitalization expense than the observation group (P < 0.001). The observation group expressed much higher nursing satisfaction than the control group (P=0.007). Additionally, according to multivariate logistic regression analysis, age, hypertension, and diabetes mellitus were independent risk factors for adverse events (P < 0.05). Conclusion: For elderly SHF patients treated by rh-BNP, comprehensive nursing intervention can contribute to higher QoL, shorter hospitalization time, lower hospitalization expense, and milder negative emotions, but did not correlate with short-term adverse cardiovascular events.
Keywords: Comprehensive nursing, rh-BNP, severe heart failure, elderly, adverse cardiovascular events
Introduction
With the aging of Chinese society, the incidence of cardiovascular diseases in China continues to rise. According to the epidemiological survey results in China Cardiovascular Diseases Report 2018: An Updated Summary [1], the number of patients with cardiovascular disease was estimated as high as 290 million. The report also pointed out that cardiovascular disease has the highest mortality rate, higher than tumors and other diseases. According to the statistical results of 8,516 patients with heart failure in China in 2015 (China-HF), the mortality rate of hospitalized patients with heart failure was 5.3% [2].
With the improvement in medical care and the extension of life expectancy, the prevalence of heart failure in China is also on the rise [3]. The treatment of heart failure brings a heavy medical burden to family and society, which is an urgent problem for the 21st century [4]. Cases with severe heart failure (SHF) refer to patients at class IV in the New York Heart Association classification (NYHA), which has a high mortality [5]. SHF patients often suffer serious symptoms including fatigue, dyspnea, and edema, enduring serious impact on their quality of life (QoL) [6]. Recombinant human brain natriuretic peptide (rh-BNP) is a drug prepared through biotechnology that has been extensively adopted in the therapy of severe heart failure [7]. Brain natriuretic peptide is an endogenous polypeptide hormone, with a crucial regulatory role in the cardiovascular system [8]. Reportedly, patients with SHF often have abnormal changes such as decreased myocardial contraction function and myocardial remodeling, which leads to decreased cardiac pumping function [9]. Brain natriuretic peptide can ameliorate cardiovascular dysfunction and symptoms by increasing diuresis, dilating blood vessels and inhibiting renin-angiotensin-aldosterone system.
Due to the severity of the disease and the aggravation of symptoms in patients with SHF, routine nursing schemes may not be sufficient to meet their special nursing needs [10,11]. Accordingly, the treatment of SHF requires individualized comprehensive nursing schemes. Comprehensive nursing is a patient-centered nursing practice, aiming at providing personalized nursing services. It evaluates and intervenes with patients’ physical and mental health at multiple angles and levels, so as to promote patients’ rehabilitation and all-around development [12].
The clinical significance of this research lies in its potential to enhance the nursing care of elderly patients with SHF treated with rh-BNP. If comprehensive nursing intervention is shown to improve a range of outcomes, it may influence the standard of care for these patients, leading to improved patient well-being, reduced hospitalization time and cost, and better management of negative emotions. Furthermore, by identifying risk factors for adverse events, this research may contribute to risk stratification and individualized care planning in this population, further enhancing the quality of patient care.
Materials and methods
Sample information
The clinical data of 174 SHF patients treated with rh-BNP in Wuhan Asia Cardiology Hospital from May 2019 to May 2022 were analyzed retrospectively.
Ethical statement
This study was performed with approval from the Medical Ethics Committee of Wuhan Asia Cardiology Hospital, with ethical approval number 202208421.
Inclusion and exclusion criteria
Inclusion criteria: Patients clinically diagnosed with severe heart failure, adhering to relevant diagnostic criteria as referenced [13]; Patients with class IV category of the New York Heart Association (NYHA) Functional Classification, indicating advanced disease with severe limitations [14]; Patients with an age of 60 or above (60 was chosen as the study focuses on elderly patients, who often have different clinical characteristics and responses to treatment compared to younger patients); Patients with detailed clinical data, including comprehensive medical history, physical examination findings, laboratory test results, and imaging studies; Patients capable of giving informed consent, or who have a legal representative capable of doing so, ensuring ethical adherence in the study.
Exclusion criteria: Patients with significant abnormalities or diseases of lungs, brain, liver, kidneys, or other major organs (despite SHF) that might affect heart function; Patients with severe infections at the time of the study, since the infection and associated treatments could interfere with the study’s outcomes; Patients diagnosed with other malignant tumors; or Patients with known blood disorders or clotting deficiencies, conditions that could increase the risk of complications.
Sample screening
174 patients were screened out according to the criteria, and only 131 patients met the requirements of this study. Among them, 71 patients who received routine nursing from May 2019 to December 2021 were assigned to the control group and 60 patients who received comprehensive nursing from January 2022 to May 2022 were assigned to the observation group.
Nursing scheme
After admission, all patients received treatment such as maintaining electrolyte balance, reducing heart load, diuresis and cardiotonic therapy. The specific plan was as follows: high-flow oxygen is given through the nasal tube. For serious conditions, if necessary, the anesthesia machine, mask pressurized oxygen, and intravenous slow drip 5~10 mg morphine (Yichang Renfu Pharmaceutical Co., Ltd., State Drug Permit H20120094) were given to make the patient sedated, avoiding the heart burden induced by the emotional agitation, and playing a role in reducing the cardiac load, dilating small blood vessels; intravenous drip of furosemide (Jilin Hundred Years of Hank Pharmaceutical Co., Ltd., National Drug License H20053949) 20~40 mg within 2 min in order to play the effect of diastolic vein and diuretic; intravenous drip of phentolamine (China Resources Shuanghe Pharmaceutical Co., Ltd., National Drug License H11020665), nitroglycerine (Shanxi Kangbao Biological Co., Ltd., H20237047) to dilate the blood vessels, according to the patient’s specific blood pressure level,with reasonable choice of drugs and dosage. Besides, 1.5 μg/kg rh-BNP (Chengdu Ndikang Biopharmaceutical Co., LTD., S20050033) was first intravenously injected within 1 to 2 minutes based on the patient’s weight. Then, a micropump was used for intravenous drip at the rate of 0.0075 ml/(kg h) for 24-72 hours. Meantime, ECG was conducted to monitor the patient’s oxygen saturation, heart rhythm, and blood pressure.
The control group received routine care, including disease assessment and monitoring, drug treatment, fluid management, and nutritional support.
The observation group received comprehensive nursing care as follows: In terms of rh-BNP administration, the nursing staff were organized and trained to ensure that they were familiar with the specifications, uses, administration routes and pharmacological effects of rh-BNP, and understood the common adverse reactions. For hospitalized patients, the staff were required to know the past medical history and drug allergy history of the patients and inform the attending physician about the allergy history in time. Elderly patients with SHF often need to be hospitalized many times. In addition to their own diseases, they may also worry about the payment of medical expenses, so they usually have emotions such as anxiety, which seriously compromise the treatment effect. Therefore, nurses were required to actively communicate with patients, understand the causes of patients’ negative emotions, and carry out targeted psychological counselling. Lifestyle adjustment: a low-salt diet was recommended to help control the accumulation of body fluids; also, the intake of fluids shall be limited. In some cases, a low-fat and low-cholesterol diet may be needed. The nursing staff also asked the patients to do gentle exercise under the guidance of a doctor, such as slow walking. The patients were required to ensure adequate rest time and reduce unnecessary physical activity. For the newly admitted patients, the nursing staff introduced in detail the use of rh-BNP and the possible adverse reactions, so as to improve patients’ cognitive level of the disease. Before using rh-BNP, the nursing staff were required to reconfirm the patient’s renal function and allergic history and decide the appropriate dose according to the patient’s specific situation. During the treatment, the nursing staff were required to closely monitor the patient’s urine volume, breathing, heart rate, blood pressure, and consciousness. Additionally, attention was paid to infusion management to avoid problems such as needle blockage and skin swelling in infusion pipelines.
Collection of clinical indexes
The clinical data collected by electronic medical record system and outpatient review records included age, gender, body mass index (BMI), marital status, education level, smoking history, alcoholism history, and past medical history. The MOS 36-Item Short-Form Health Survey (SF-36) was adopted to evaluate the QoL of patients before and after nursing, and the self-rating anxiety scale (SAS) and self-rating depression scale (SDS) were used to evaluate the negative emotions of the patients before and after nursing.
Outcome measures
Primary outcome measures: The changes in quality of life (QoL) before and after nursing were compared between the two groups. The QoL score provides an overall assessment of patients’ perception of their status in the context of the culture and value system in which they live, and related to their goals, expectations, standards, and concerns. The total score is 100 points, and a higher score indicates better QoL [15].
The incidence of adverse events after nursing care was counted, including cardiac death, myocardial infarction, and malignant arrhythmia, and the risk factors for adverse events were analyzed by logistic regression. The left ventricular end-diastolic volume left ventricular end-diastolic volume (LVEDV) and left ventricular ejection fraction (LVEF) were measured by Philips IE33 echocardiography.
Secondary outcome measures: The clinical data of the two groups were compared; the changes in patients’ anxiety and depression scores before and after nursing were compared between the two groups, by using a self-rating anxiety scale (SAS) and self-rating depression scale (SDS), respectively. The total score of SAS and SDS was 100 points, separately, and a higher SAS and SDS score indicates more serious anxiety and depression, respectively [16].
The hospitalization expenses and hospitalization times of the two groups were compared. The nursing satisfaction of the two groups was counted. All the indexes were tested after 2 weeks of nursing.
Statistical analyses
SPSS20.0 software was adopted for statistical analyses, and GraphPad 7 for data visualization. The measured data were described by mean ± standard deviation (Mean ± SD), and their inter-group comparison and intro-group comparison were conducted using the independent-samples T test and paired t test, respectively. Counted data were described by % and analyzed using the chi-square test. Additionally, logistic regression was used to analyze the independent risk factors affecting the occurrence of adverse time. P < 0.05 implied a significant difference.
Results
Baseline data
According to comparison of baseline data between the two groups, the control group and observation group were similar in terms of age, sex, BMI, marital status, education level, smoking history, alcoholism history, and previous medical history (Table 1, all P > 0.05).
Table 1.
Comparison of baseline data between the two groups
| Factor | Control group (n=71) | Observation group (n=60) | P value |
|---|---|---|---|
| Age | 0.375 | ||
| ≥ 65 years old | 53 | 41 | |
| < 65 years old | 18 | 19 | |
| Gender | 0.385 | ||
| Male | 46 | 35 | |
| Female | 25 | 25 | |
| BMI | 0.496 | ||
| ≥ 25 kg/m2 | 18 | 12 | |
| < 25 kg/m2 | 53 | 48 | |
| Marital status | 0.417 | ||
| Married | 44 | 33 | |
| Divorced | 27 | 27 | |
| Academic degree | 0.728 | ||
| ≥ Junior high school | 40 | 36 | |
| < Junior high school | 31 | 24 | |
| Smoking history | 0.385 | ||
| Yes | 46 | 35 | |
| No | 25 | 25 | |
| Alcoholism history | 0.209 | ||
| Yes | 9 | 12 | |
| No | 62 | 48 | |
| Past medical history | |||
| Hypertension | 21 | 15 | 0.524 |
| Diabetes mellitus | 13 | 14 | 0.398 |
Note: BMI: Body mass index.
QoL assessment
The QoL of the two groups before and after nursing was evaluated. According to the results, before nursing, the QoL scores of the two groups were not significantly different (Figure 1, P > 0.05), while after nursing, the QoL scores in both groups increased (Figure 1, P < 0.0001). In addition, the control group had lower QoL scores than the observation group after nursing (Figure 1, P < 0.0001).
Figure 1.
Comparison of quality-of-life scores between the two groups before and after nursing. A: Comparison of physical functioning scores; B: Comparison of role-physical scores; C: Comparison of bodily pain scores; D: Comparison of general health perceptions scores; E: Comparison of vitality scores between the two groups before and after nursing; F: Comparison of social functioning scores; G: Comparison of role-emotional scores; H: Comparison of mental health scores. Notes: ns, P > 0.05, ****, P < 0.0001.
Evaluation of anxiety and depression
The SAS and SDS scores of the two groups were evaluated before and after nursing. According to the results, before nursing, the SAS and SDS scores of the two groups were not greatly different (Figure 2, both P > 0.05), while after nursing, the SAS and SDS scores of both groups decreased (Figure 2, both P < 0.0001). In addition, the control group had significantly higher SAS and SDS scores than the observation group (Figure 2, both P < 0.0001).
Figure 2.
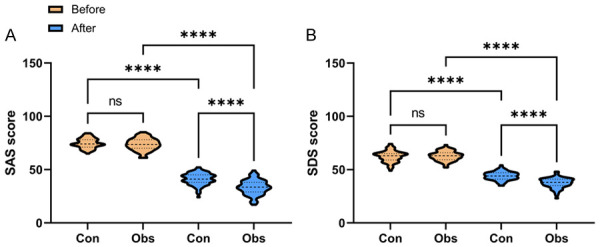
Comparison of anxiety and depression scores between two group before and after nursing. A: Comparison of SAS score changes; B: Comparison of SDS scores. Notes: ns, P > 0.05, ****, P < 0.0001; SAS: Self-rating anxiety scale; SDS: Self-rating depression scale.
Comparison of LVEDV and LVEF levels
The levels of LVEDV and LVEF in the two groups were determined before and after nursing. According to the results, before nursing, there was no significant difference in the levels of LVEDV and LVEF between the two groups (Figure 3, both P > 0.05), while after nursing, the levels of LVEDV and LVEF in both groups increased (Figure 3, both P < 0.0001), with lower levels of LVEDV and LVEF in the control group than those in the observation group (Figure 3, P < 0.0001).
Figure 3.

Comparison of LVEDV and LVEF in patients before and after nursing. A: Comparison of LVEDV changes; B: Comparison of LVEF, ****, P < 0.0001; LVEDV: Left ventricular end-diastolic volume; LVEF: Left ventricular ejection fraction.
Statistics of hospitalization time and expenses
According to statistics of hospitalization time and hospitalization expenses of patients in the two groups, the control group experienced greatly longer hospitalization time and higher hospitalization expenses than the observation group (Table 2, both P < 0.001).
Table 2.
Comparison of hospitalization time and hospitalization expense between the two groups
| Group | Hospitalization time (d) | Hospitalization expense |
|---|---|---|
| Control group (n=71) | 18.2±3.2 | 4910.6±513.7 |
| Observation group (n=60) | 16.2±3.3 | 6569.9±526.8 |
| T value | 3.432 | 18.204 |
| P value | 0.001 | < 0.001 |
Nursing satisfaction
Lastly, the nursing satisfaction of the two groups was evaluated. As a result, the observation group expressed significantly higher nursing satisfaction than the control group (P=0.007, Table 3).
Table 3.
Comparison of nursing satisfaction between the two groups
| Group | Very satisfied | Satisfied | Dissatisfied | Total satisfaction |
|---|---|---|---|---|
| Control group (n=71) | 40 | 16 | 15 | 56 |
| Observation group (n=60) | 45 | 12 | 3 | 57 |
| χ2 value | 7.135 | |||
| P value | 0.007 |
Analysis of adverse events and risk factors
The occurrence of adverse events in patients within 180 days was counted. As a result, there were 48 cases with adverse events. According to further univariate analysis, age, hypertension, diabetes mellitus (DM) and nursing scheme were found to be the risk factors of adverse events (Table 4, all P < 0.05). Additionally, according to multivariate logistic regression analysis, age, hypertension and DM were independent risk factors for adverse events (Table 5, all P < 0.05).
Table 4.
Univariate analysis of factors affecting adverse events
| Factor | Occurrence group (n=48) | Non-occurrence group (n=83) | P value |
|---|---|---|---|
| Age | < 0.001 | ||
| ≥ 65 years old | 43 | 51 | |
| < 65 years old | 5 | 32 | |
| Gender | 0.220 | ||
| Male | 26 | 55 | |
| Female | 22 | 28 | |
| BMI | 0.663 | ||
| ≥ 25 kg/m2 | 12 | 18 | |
| < 25 kg/m2 | 36 | 65 | |
| Marital status | 0.120 | ||
| Married | 24 | 53 | |
| Divorced | 24 | 30 | |
| Academic degree | 0.726 | ||
| ≥ Junior high school | 29 | 47 | |
| < Junior high school | 19 | 36 | |
| Smoking history | 0.220 | ||
| Yes | 26 | 55 | |
| No | 22 | 28 | |
| Alcoholism history | 0.152 | ||
| Yes | 5 | 16 | |
| No | 43 | 67 | |
| History of hypertension | 0.001 | ||
| Yes | 22 | 14 | |
| No | 26 | 69 | |
| History of diabetes mellitus | 0.001 | ||
| Yes | 17 | 10 | |
| No | 31 | 73 | |
| Nursing scheme | 0.015 | ||
| Control group | 33 | 38 | |
| Observation group | 15 | 45 | |
| Hospitalization time (d) | 17.3±3.5 | 17.2±3.3 | 0.848 |
| LVEDV (mL) | 60.6±3.23 | 59.5±2.86 | 0.066 |
| LVEF (%) | 46.4±5.2 | 45.6±5.4 | 0.427 |
Note: BMI: Body mass index, LVEDV: Left Ventricular End-Diastolic Volume, LVEF: Left Ventricular Ejection Fraction.
Table 5.
Multivariate logistic regression analysis of factors affecting adverse events
| Factor | β | Standard error | χ2 | P | OR | 95% CI | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Lower limit | Upper limit | ||||||
| Age | 1.447 | 0.547 | 7.004 | 0.008 | 4.248 | 1.455 | 12.402 |
| History of hypertension | 1.029 | 0.442 | 5.421 | 0.020 | 2.798 | 1.177 | 6.654 |
| History of diabetes mellitus | 1.147 | 0.493 | 5.423 | 0.020 | 3.149 | 1.199 | 8.271 |
| Nursing scheme | 0.666 | 0.420 | 2.518 | 0.113 | 1.947 | 0.855 | 4.433 |
Discussion
The incidence of heart failure is on the increase worldwide. At the current stage, there are over 20 million patients worldwide. In addition, the prognosis of hospitalized patients with SHF is poor, and their one-year mortality rate is about 10 times higher than that of healthy people [17,18]. According to research [19], heart failure is the final outcome of patients with cardiovascular disease and the main cause of death, and its 5-year survival rate is similar to that of malignant tumors.
As life expectancy extends, heart failure has become an increasingly prevalent health issue among the elderly. The elderly, a unique demographic, often have a less comprehensive understanding and memory, and exhibit heightened sensitivity and suspicion about their own medical conditions [20]. They are frequently susceptible to cognitive biases and misunderstandings about their treatment and prognosis. Even minor changes in their condition or slight drug side effects can trigger abnormal fluctuations in their thoughts and behaviors [21]. Consequently, the success in treating elderly patients is strongly tied to the quality of nursing care, underscoring the need to enhance healthcare quality. Comprehensive nursing aims to provide individualized and systematic interventions for patients to optimize therapeutic and nursing outcomes that improve prognosis [22].
In our study, both routine and comprehensive nursing were able to reduce patient anxiety and depression, enhance QoL, and improve left ventricular end-diastolic volume (LVEDV) and left ventricular ejection fraction (LVEF). However, compared to routine care, comprehensive nursing was more effective in alleviating anxiety, depression, improving QoL, and cardiac function. It also reduced hospitalization time and treatment cost, and improved nursing satisfaction. Studies like Yang et al. [23] have demonstrated significant improvements in QoL among elderly Alzheimer’s disease patients through comprehensive nursing intervention. Similarly, a meta-study by Rodríguez et al. [24] found that comprehensive nursing interventions effectively enhanced QoL in cancer survivors over a short period. These studies collectively highlight the efficacy of comprehensive nursing in improving QoL. Furthermore, Gong et al. [25] reported that comprehensive nursing could alleviate anxiety and depression in patients with postoperative malignant glioma.
Our results suggest that comprehensive nursing impacts various aspects including personalized nursing, comprehensive intervention, emotional support, education, and guidance. Through personalized care plans and comprehensive interventions, it can meet the unique needs of patients, offering thorough support and care to enhance patient engagement and satisfaction. Emotional support and effective communication can help alleviate anxiety and depression. Education and guidance, on the other hand, allow patients to better comprehend their disease, treatment plan, and self-management techniques, enhancing their awareness and control over their health condition. Overall, this all-encompassing approach to nursing promotes patients’ physical and mental well-being, expedites rehabilitation, and improves their QoL.
Although the diagnosis and treatment strategies for heart failure have achieved remarkable progress over the past few years, the incidence of adverse events is still relatively high because other complicated factors, such as severe underlying diseases, many complications, easy recurrence [26,27]. Reportedly, the mortality rate or readmission rate of patients with acute heart failure is as high as 60% within one year [28]. In the present study, statistics was done on the occurrence of adverse events in patients within 180 days, and it was found that age, hypertension and DM, but not nursing scheme, were the risk factors affecting the occurrence of adverse events. This suggests that the nursing scheme does not affect patients’ short-term adverse cardiovascular events. With the increase in age, the heart and vascular system are gradually damaged and degraded. The elderly have worse cardiac function and vascular elasticity and also suffer weakened contractile and diastolic ability of cardiac muscles [29], so they are more prone to heart failure and face a higher risk of cardiovascular events. Hypertension is one of the main risk factors for heart failure. Long-term hypertension will trigger cardiac hypertrophy, myocardial fibrosis, and vascular injury, and then reduce the pumping function of the heart. Hypertension also increases the risk of atherosclerosis and coronary artery disease, further exacerbating the development of heart failure and the occurrence of adverse cardiovascular events [30]. In addition, DM is a metabolic disease, and DM patients are more likely to develop cardiovascular diseases, including heart failure. A high blood glucose level is harmful to the heart and blood vessels, which increases the risk of myocardial ischemia and hypoxia, and damages heart function [31]. Diabetes mellitus is also closely bound up with cardiovascular risk factors such as hypertension, high cholesterol, and obesity, which further increases the risk of cardiovascular events. Accordingly, in the management of elderly patients with SHF, special attention should be paid to these risk factors. Corresponding preventive measures should be taken to lower the incidence of adverse cardiovascular events and improve prognosis.
This study has some limitations. First, we collected only the adverse events of patients within 180 days, so whether the nursing scheme is related to the long-term adverse events of patients still needs further research. Secondly, the sample in this study is relatively small, which may lead to bias in the result analysis. Finally, whether the results of a single-center study are universal needs further verification. Therefore, we hope to carry out more clinical experiments with more clinical samples in the follow-up study to improve the conclusions.
To sum up, for elderly SHF patients treated by rh-BNP, comprehensive nursing intervention can contribute to higher QoL, shorter hospitalization time, lower hospitalization expense, and milder negative emotions, but was not related to short-term adverse cardiovascular events.
Disclosure of conflict of interest
None.
References
- 1.Wang YJ, Li ZX, Gu HQ, Zhai Y, Zhou Q, Jiang Y, Zhao XQ, Wang YL, Yang X, Wang CJ, Meng X, Li H, Liu LP, Jing J, Wu J, Xu AD, Dong Q, Wang D, Wang WZ, Ma XD, Zhao JZ China Stroke Statistics Writing Committee. China stroke statistics: an update on the 2019 report from the National Center for Healthcare Quality Management in Neurological Diseases, China National Clinical Research Center for Neurological Diseases, the Chinese Stroke Association, National Center for Chronic and Non-communicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention and Institute for Global Neuroscience and Stroke Collaborations. Stroke Vasc Neurol. 2022;7:415–450. doi: 10.1136/svn-2021-001374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fu R, Feng S, Chen Q, Lin Y, Lin Z, Hu Z. Regulatory relationships of demographic, clinical characteristics and quality of care for heart failure patients in southern China. Int J Qual Health Care. 2022;34:mzab159. doi: 10.1093/intqhc/mzab159. [DOI] [PubMed] [Google Scholar]
- 3.Zannad F, Ferreira JP, Pocock SJ, Anker SD, Butler J, Filippatos G, Brueckmann M, Ofstad AP, Pfarr E, Jamal W, Packer M. SGLT2 inhibitors in patients with heart failure with reduced ejection fraction: a meta-analysis of the EMPEROR-reduced and DAPA-HF trials. Lancet. 2020;396:819–829. doi: 10.1016/S0140-6736(20)31824-9. [DOI] [PubMed] [Google Scholar]
- 4.Vaduganathan M, Claggett BL, Jhund PS, Cunningham JW, Pedro Ferreira J, Zannad F, Packer M, Fonarow GC, McMurray JJV, Solomon SD. Estimating lifetime benefits of comprehensive disease-modifying pharmacological therapies in patients with heart failure with reduced ejection fraction: a comparative analysis of three randomised controlled trials. Lancet. 2020;396:121–128. doi: 10.1016/S0140-6736(20)30748-0. [DOI] [PubMed] [Google Scholar]
- 5.Caviedes Bottner P, Cordova Fernandez T, Larrain Valenzuela M, Cruces Romero Presentacion de Casos Clinicos P. Dilated cardiomyopathy and severe heart failure. An update for pediatricians. Arch Argent Pediatr. 2018;116:e421–e428. doi: 10.5546/aap.2018.eng.e421. [DOI] [PubMed] [Google Scholar]
- 6.Akodad M, Schurtz G, Adda J, Leclercq F, Roubille F. Management of valvulopathies with acute severe heart failure and cardiogenic shock. Arch Cardiovasc Dis. 2019;112:773–780. doi: 10.1016/j.acvd.2019.06.009. [DOI] [PubMed] [Google Scholar]
- 7.Li Y, Yu G, Shi L, Zhao L, Wen Z, Kan B, Wang W, Jian X. Severe methyl bromide poisoning causing early acute renal failure and anuria: a case report. J Int Med Res. 2022;50:3000605221122619. doi: 10.1177/03000605221122619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pang Z, Pan C, Yao Z, Ren Y, Tian L, Cui J, Liu X, Zhang L, Chen Y. A study of the sequential treatment of acute heart failure with sacubitril/valsartan by recombinant human brain natriuretic peptide: a randomized controlled trial. Medicine (Baltimore) 2021;100:e25621. doi: 10.1097/MD.0000000000025621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Luo JC, Zhang YJ, Huang DL, Wang H, Luo MH, Hou JY, Hao GW, Su Y, Tu GW, Luo Z. Recombinant human brain natriuretic peptide ameliorates venous return function in congestive heart failure. ESC Heart Fail. 2022;9:2635–2644. doi: 10.1002/ehf2.13987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li XQ. Effects of high-quality nursing care on psychological outcomes in patients with chronic heart failure. Medicine (Baltimore) 2019;98:e17351. doi: 10.1097/MD.0000000000017351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brennan EJ. Chronic heart failure nursing: integrated multidisciplinary care. Br J Nurs. 2018;27:681–688. doi: 10.12968/bjon.2018.27.12.681. [DOI] [PubMed] [Google Scholar]
- 12.Xu Y, Wang RY, Zhao YH. Effects of perioperative comprehensive nursing based on risk prevention for patients with intracranial aneurysm. Int J Clin Pract. 2021;75:e13761. doi: 10.1111/ijcp.13761. [DOI] [PubMed] [Google Scholar]
- 13.Long B, Koyfman A, Gottlieb M. Diagnosis of acute heart failure in the emergency department: an evidence-based review. West J Emerg Med. 2019;20:875–884. doi: 10.5811/westjem.2019.9.43732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Costa RVC. NYHA classification and cardiopulmonary exercise test variables in patients with heart failure. Arq Bras Cardiol. 2022;118:1124–1125. doi: 10.36660/abc.20220196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Indraratna P, Tardo D, Yu J, Delbaere K, Brodie M, Lovell N, Ooi SY. Mobile phone technologies in the management of ischemic heart disease, heart failure, and hypertension: systematic review and meta-analysis. JMIR Mhealth Uhealth. 2020;8:e16695. doi: 10.2196/16695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McHorney CA, Robbins J, Lomax K, Rosenbek JC, Chignell K, Kramer AE, Bricker DE. The SWAL-QOL and SWAL-CARE outcomes tool for oropharyngeal dysphagia in adults: III. Documentation of reliability and validity. Dysphagia. 2002;17:97–114. doi: 10.1007/s00455-001-0109-1. [DOI] [PubMed] [Google Scholar]
- 17.Yue T, Li Q, Wang R, Liu Z, Guo M, Bai F, Zhang Z, Wang W, Cheng Y, Wang H. Comparison of Hospital Anxiety and Depression Scale (HADS) and Zung Self-Rating Anxiety/Depression Scale (SAS/SDS) in evaluating anxiety and depression in patients with psoriatic arthritis. Dermatology. 2020;236:170–178. doi: 10.1159/000498848. [DOI] [PubMed] [Google Scholar]
- 18.Kosiborod MN, Jhund PS, Docherty KF, Diez M, Petrie MC, Verma S, Nicolau JC, Merkely B, Kitakaze M, DeMets DL, Inzucchi SE, Kober L, Martinez FA, Ponikowski P, Sabatine MS, Solomon SD, Bengtsson O, Lindholm D, Niklasson A, Sjostrand M, Langkilde AM, McMurray JJV. Effects of dapagliflozin on symptoms, function, and quality of life in patients with heart failure and reduced ejection fraction: results from the DAPA-HF trial. Circulation. 2020;141:90–99. doi: 10.1161/CIRCULATIONAHA.119.044138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jankauskas SS, Kansakar U, Varzideh F, Wilson S, Mone P, Lombardi A, Gambardella J, Santulli G. Heart failure in diabetes. Metabolism. 2021;125:154910. doi: 10.1016/j.metabol.2021.154910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eiraku K, Uozumi Y, Hieda M, Maruyama T, Nomura H. A senile case of heart failure associated with hypermagnesemia induced by magnesium-containing laxative agent. Geriatr Gerontol Int. 2022;22:897–899. doi: 10.1111/ggi.14478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.van den Berg MP, Mulder BA, Klaassen SHC, Maass AH, van Veldhuisen DJ, van der Meer P, Nienhuis HLA, Hazenberg BPC, Rienstra M. Heart failure with preserved ejection fraction, atrial fibrillation, and the role of senile amyloidosis. Eur Heart J. 2019;40:1287–1293. doi: 10.1093/eurheartj/ehz057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cochran CB. Infusing the principles of trauma-informed care into emergency nursing: a comprehensive approach to change practice. J Forensic Nurs. 2019;15:206–213. doi: 10.1097/JFN.0000000000000267. [DOI] [PubMed] [Google Scholar]
- 23.Yang L, Xuan C, Yu C, Jin X, Zheng P, Yan J. Effects of comprehensive intervention on life quality among the elderly with Alzheimer disease and their caregivers based on mixed models. Nurs Open. 2022;9:1412–1422. doi: 10.1002/nop2.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rodriguez-Matesanz I, Ambrosio L, Domingo-Osle M, Elizondo-Rodriguez N, La Rosa-Salas V, Garcia-Vivar C. Are nursing interventions effective in improving quality of life in cancer survivors? A systematic review. Cancer Nurs. 2022;45:E134–E145. doi: 10.1097/NCC.0000000000000901. [DOI] [PubMed] [Google Scholar]
- 25.Gong X, Wu W, Xing D, Guo X, Yang M. Effect of high-quality nursing based on comprehensive nursing on the postoperative quality of life and satisfaction of patients with malignant glioma. Evid Based Complement Alternat Med. 2022;2022:9345099. doi: 10.1155/2022/9345099. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 26.Al-Ali D, Elshafeey A, Mushannen M, Kawas H, Shafiq A, Mhaimeed N, Mhaimeed O, Mhaimeed N, Zeghlache R, Salameh M, Paul P, Homssi M, Mohammed I, Narangoli A, Yagan L, Khanjar B, Laws S, Elshazly MB, Zakaria D. Cardiovascular and haematological events post COVID-19 vaccination: a systematic review. J Cell Mol Med. 2022;26:636–653. doi: 10.1111/jcmm.17137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang K, Liu W. Triglyceride and glucose index and sex differences in relation to major adverse cardiovascular events in hypertensive patients without diabetes. Front Endocrinol (Lausanne) 2021;12:761397. doi: 10.3389/fendo.2021.761397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang T, Gu J, Du C, Shan T, Wei T, Li Y, Wang L. Adverse cerebral cardiovascular events associated with checkpoint kinase 1 inhibitors: a systemic review. J Cardiovasc Pharmacol. 2021;77:549–556. doi: 10.1097/FJC.0000000000000997. [DOI] [PubMed] [Google Scholar]
- 29.Doan TH, Yen-Nicolay S, Bernet-Camard MF, Martin-Verstraete I, Pechine S. Impact of subinhibitory concentrations of metronidazole on proteome of Clostridioides difficile strains with different levels of susceptibility. PLoS One. 2020;15:e0241903. doi: 10.1371/journal.pone.0241903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhao N, Li J, Chen ZZ, Chu ZF, Chen ZB. Association of interleukin-10 gene polymorphism with enterovirus 71 infection in children. Zhongguo Dang Dai Er Ke Za Zhi. 2019;21:789–795. doi: 10.7499/j.issn.1008-8830.2019.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.GRADE Study Research Group. Nathan DM, Lachin JM, Bebu I, Burch HB, Buse JB, Cherrington AL, Fortmann SP, Green JB, Kahn SE, Kirkman MS, Krause-Steinrauf H, Larkin ME, Phillips LS, Pop-Busui R, Steffes M, Tiktin M, Tripputi M, Wexler DJ, Younes N. Glycemia reduction in type 2 diabetes - microvascular and cardiovascular outcomes. N Engl J Med. 2022;387:1075–1088. doi: 10.1056/NEJMoa2200436. [DOI] [PMC free article] [PubMed] [Google Scholar]



