Abstract
Purpose: To analyze the clinical efficacy of gasless submental-transoral endoscopic thyroidectomy (ETE) with Kirschner wire suspension in patients with papillary thyroid carcinoma (PTC). Methods: Retrospectively, we enrolled 112 patients with PTC who received treatment in The Second Affiliated Hospital of Nanchang University between December 2020 and December 2021. Among them, 60 cases (laparoscopic group) received gasless submental-transoral ETE with Kirschner wire suspension, and the other 52 cases (open group) were treated by traditional thyroidectomy. Surgical indicators (operative time (OT), intraoperative blood loss (IBL), and postoperative drainage volume (DV)), number of central lymph node (CLN) dissected, length of hospital stay (LOS), Visual Analogue Scale (VAS) score, aesthetic satisfaction score, and complications were observed and compared between the two groups. Results: There was no significant difference between the two groups in OT (55.73±5.49 min vs. 55.00±7.79 min), IBL (20.67±7.75 mL vs. 23.08±6.24 mL), postoperative DV (33.17±15.09 mL vs. 39.52±19.22 mL), number of CLN dissected (5.54±2.75 vs. 5.43±3.15), LOS (3.63±0.69 d vs. 3.68±0.57 d), postoperative VAS score (3.19±1.07 points vs. 3.38±1.09 points), and total complication rate (3.85% vs. 8.33%; all P>0.05). However, the laparoscopic group exhibited a significantly higher aesthetic satisfaction score than the open group (7.10±1.46 points vs. 6.42±1.46 points; P<0.05). In addition, patients in both groups were followed up for at least 3 months, and no recurrence or metastasis was observed. Conclusions: Gasless submental-transoral ETE with Kirschner wire suspension offers comparable curative effect as traditional thyroidectomy and safety, but it provides superior esthetic results, making it a viable treatment option for patients with PTC.
Keywords: Kirschner wire suspension, submental, endoscopic thyroidectomy, papillary thyroid carcinoma, esthetic effect
Introduction
Thyroid cancer is the most common malignancy of human endocrine system, with a rising incidence observed over time [1,2]. Differentiated thyroid cancer (DTC), mainly including papillary thyroid carcinoma (PTC) and follicular thyroid cancer, accounts for 97% of all thyroid cancers [3,4]. DTC patients usually have favorable overall prognosis, high survival rate and long-life expectancy, so they have higher requirements for postoperative quality of life while pursuing a radical cure [5]. Surgical treatments, including traditional surgery and endoscopic thyroid surgery, are the mainstay of treatment for the disease [6]. Traditional thyroidectomy procedures often result in a noticeable 5-8 cm scar on the neck, causing a considerable psychological impact on the patient [7]. While laparoscopic thyroid surgery is diversified, where carbon dioxide (CO2) inflation is often used during the procedure to maintain the operating space [8]. However, the use of CO2 inflation during surgery may cause hypercapnia and CO2 embolization. Additionally, there is a risk of tumor implantation metastasis [9]. Therefore, the gasless method may be a safer and more favorable choice for surgery.
Compared with the traditional open thyroidectomy, minimally invasive endoscopic thyroidectomy (ETE) is highly regarded for its better surgical field of vision and postoperative aesthetic satisfaction [10]. Therefore, exploring gasless endoscopic thyroid surgery is of great significance to avoid adverse events and improve the surgical effect. ETE has many approaches, including oral, axillary, and anterior thoracic, among which, the transoral endoscopic thyroidectomy vestibular approach (TOETVA) is the most popular one with advantages of concealed incision, short surgical path and thorough dissection of central lymph nodes (CLNs) [11]. However, this procedure also has some limitations and may induce mental nerve damage, leading to lower lip and chin numbness [12]. ETE via the submental-transoral approach can move the observation port from the oral vestibule to the submental region. This relocation helps prevent damage to the mental nerve endings caused by the oral vestibular mucosa and the mental muscle when the observation port is severed. Consequently, this technique is beneficial in reducing the risk of mental nerve damage [13].
In this study, we analyzed the clinical efficacy of a surgical technique that was rarely reported for PTC [14], namely, gasless submental-transoral ETE with Kirschner wire suspension.
Data and methods
General data
Retrospectively, data of 112 PTC patients who visited the Second Affiliated Hospital of Nanchang University between December 2020 and December 2021 were analyzed. Among them, 60 cases who received gasless submental-transoral ETE with Kirschner wire suspension were included in a laparoscopic group, and the remaining 52 cases undergoing traditional thyroidectomy were included in an open group. The mean age (years) and body mass index (BMI) of the open group were 33.98±6.10 and 21.39±1.99 kg/m2, respectively, while those of the laparoscopic group were 34.97±7.79 and 22.08±2.03 kg/m2, respectively. The general data were similar in both cohorts (P>0.05), suggesting clinical comparability. This retrospective study was approved by the ethics committee of our hospital. See Figure 1 for the flowchart of this study.
Figure 1.
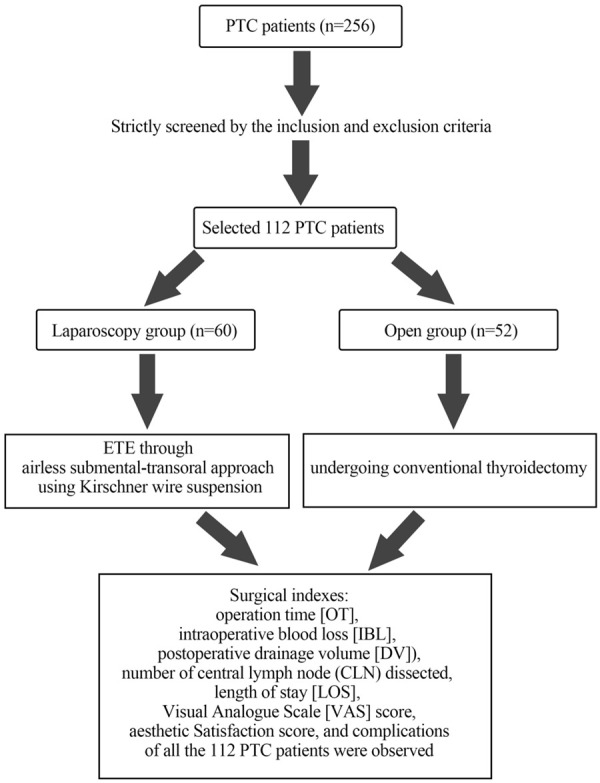
Flowchart of this study. PTC: papillary thyroid carcinoma.
Eligibility criteria
Inclusion criteria: patients who were diagnosed with PTC by preoperative fine needle biopsy, with a maximum diameter ≤2 cm and no lymph node metastasis in the cervical region; patients with no history of neck surgery; patients with no hematological or infectious diseases; patients with complete medical records; patients who underwent surgical treatment and completed postoperative outcome assessment.
Exclusion criteria: patients with surgical contraindications; patients with no aesthetic needs; patients with primary tumor or central metastatic lymph nodes involving trachea, esophagus, or recurrent laryngeal nerve; patients with serious underlying diseases or other malignant tumors; patients who were pregnant or lactating.
Treatment methods
The open group received traditional thyroidectomy, with the specific surgical procedure described previously [15].
The laparoscopic group was treated by ETE via the gasless submental-transoral combined approach using Kirschner wire suspension [14,16]. After general anesthesia and routine skin preparation, an incision was made along the submental skin to the deep surface of platysma muscle using an electric knife under direct vision (the 1st operation space). The skin flap was then lifted by Kirschner wire suspension to expand the operation space (the 2nd operation space). In order to deviate from the main mental nerve, a longitudinal incision about 5 mm long was created in the bilateral first premolars near the labial mucosa, and a 5 mm cored cannula was placed in the first operating space. Then, a special lift retractor with negative pressure suction was inserted into the submental incision to lift the skin upwards, after which the retractor was suspended on the anesthesia frame with a sterile bandage. Thereafter, a 10-mm cannula and the endoscope were placed into the submental incision, which was separated downward to the level of the suprasternal notch with an ultrasonic scalpel to expose the anterior edge of the sternocleidomastoid muscle on both sides. According to the operating distance, a Kirschner wire suspension retractor with appropriate length was selected. The cervical linea alba was opened using an ultrasonic scalpel and an electrocoagulation hook, with a range up to the thyroid cartilage notch and down to the sternal notch. The thyroid gland was then separated from the banded muscle space. A 50-ml needle was used to penetrate the skin at the level of the lower border of the cricoid cartilage and about 2 cm below it, and a percutaneous retractor was placed to pull the band muscle laterally to expose the cervical sheath. After that, the nerve monitoring probe was inserted through the submental observation port to measure vagal electromyographic signals. The middle thyroid vein was then closed, and the surface of the common carotid artery was opened. The ultrasonic scalpel was then applied to sever the thyroid isthmus and the attachment of thyroid gland to trachea (part of Berry’s ligament). The percutaneous retractor was used to pull the strap muscles outward and upward and separated the upper thyroid pole blood vessels against the upper thyroid pole step by step. Subsequently, fine capsule dissection of the superior parathyroid gland was performed, followed by dissection of the recurrent laryngeal nerve at the entry point of larynx, localization of the recurrent laryngeal nerve with the aid of a nerve monitor, retrograde dissection of the recurrent laryngeal nerve, and removal of the thyroid gland lobe. This was followed by CLND, hemostasis, and rinsing of the wound. Finally, the strap muscles were sutured with 4-0 barbed threads, a drainage tube was placed, and the submental and oral mucosal incisions were closed. The procedures are shown in Figures 2 and 3.
Figure 2.
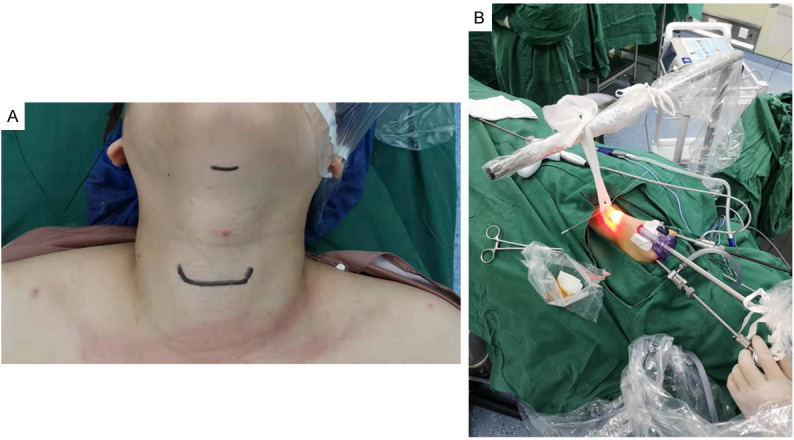
Preoperative and operating space establishment of gasless submental-transoral endoscopic thyroidectomy with Kirschner wire suspension. A. Preoperative body surface marking. B. Establishment of surgical operation space.
Figure 3.
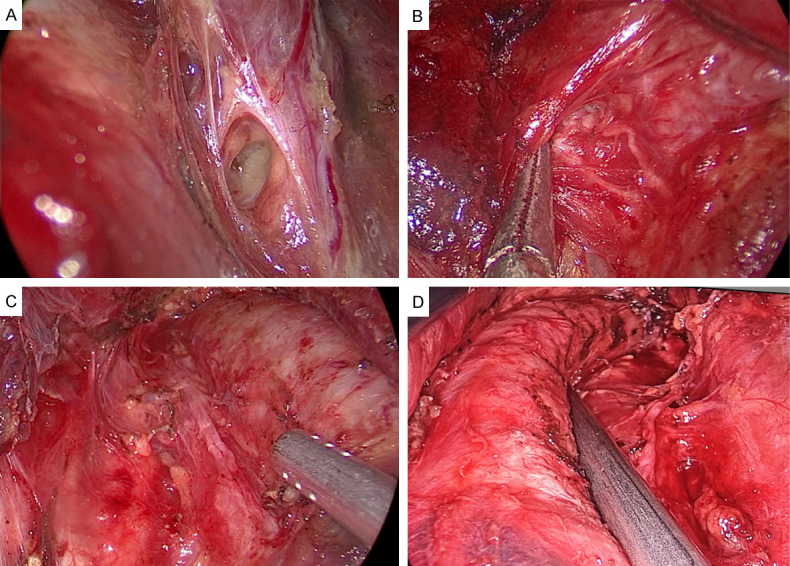
The procedure of gasless submental-transoral endoscopic thyroidectomy with Kirschner wire suspension. A. Exposure of the superior parathyroid gland. B, C. Treatment of multiple branches of the recurrent laryngeal nerve. D. Central lymph node dissection.
Outcome measures
Surgical indexes (operation time (OT), intraoperative blood loss (IBL), postoperative drainage volume (DV)), number of CLN dissected, length of stay (LOS), Visual Analogue Scale (VAS) score, aesthetic satisfaction score, and complications of all the patients were observed, recorded and compared between the two groups. The VAS score (score range: 0-10) was used to evaluate patients’ pain intensity at one month postoperatively, with greater scores representing more severe pain. The aesthetic satisfaction score, ranged from 0 to 10 points, was self-evaluated by patients one month after surgery, with the score in direct proportion to the aesthetic effect. In terms of complications, we mainly recorded the occurrence of hoarseness, choking cough when drinking, numbness of hands and feet, infection, mental nerve injury, and mucocutaneous hemorrhage. The postoperative scars of subjects in the laparoscopic group can be found in Figure 4. Among the above indicators, OT, IBL, DV, CLN dissected, VAS score, and aesthetic satisfaction score are the primary outcome measures, while LOS and complications are secondary outcome measures.
Figure 4.
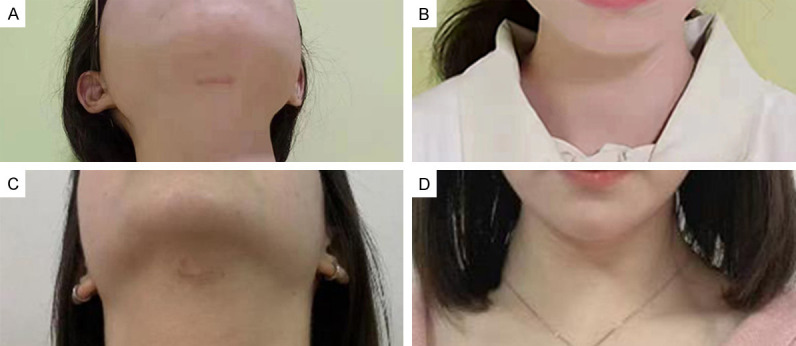
The scars of typical cases after undergoing gasless submental-transoral endoscopic thyroidectomy with Kirschner wire suspension. A, B. Scar status and front view of a female patient. C, D. Scar status and front view of another female patient.
Statistics and analyses
Categorical data and quantitative data in this study were denoted by the number of cases/percentage (n/%) and mean ± standard error of mean (SEM), respectively. The data analysis and visualization were conducted by GraphPad Prism 6. For inter-group comparisons, Chi-square tests were used for categorical data and independent samples t tests were used for quantitative data, with P<0.05 as the level of significance.
Results
General data and pathological parameters of the patients
We analyzed the general data and pathological parameters of the 112 PTC patients enrolled (Table 1). After comparison, it was found that the two cohorts of patients were clinically comparable with similar baseline data such as average age, BMI, tumor diameter, educational level, place of residence, and marital status (P>0.05).
Table 1.
General information [n (%), mean ± SEM]
| Factor | n | Open group (n=52) | Laparoscopic group (n=60) | χ2/t | P |
|---|---|---|---|---|---|
| Sex | - | - | |||
| Male | 0 | 0 (0.00) | 0 (0.00) | ||
| Female | 112 | 52 (100.00) | 60 (100.00) | ||
| Average age (years old) | 112 | 33.98±6.10 | 34.97±7.79 | 0.740 | 0.461 |
| BMI (kg/m2) | 112 | 21.39±1.99 | 22.08±2.03 | 1.810 | 0.073 |
| Tumor diameter (mm) | 112 | 0.65±0.30 | 0.69±0.26 | 0.756 | 0.451 |
| Tumor location | 0.431 | 0.512 | |||
| Left | 64 | 28 (53.85) | 36 (60.00) | 0.463 | 0.793 |
| Right | 48 | 24 (46.15) | 24 (40.00) | ||
| Education level | 0.005 | 0.945 | |||
| Below high school | 65 | 30 (57.69) | 35 (58.33) | ||
| High school and above | 47 | 22 (42.31) | 25 (41.67) | ||
| Residence | 0.051 | 0.821 | |||
| Urban areas | 40 | 18 (34.62) | 22 (36.67) | ||
| Rural areas | 72 | 34 (65.38) | 38 (63.33) | ||
| Marital status | 0.318 | 0.555 | |||
| Single | 31 | 13 (25.00) | 18 (30.00) | ||
| Married | 81 | 39 (75.00) | 42 (70.00) |
BMI: body mass index.
Surgical indexes of the patients
We analyzed operation-related indexes of the two groups (Figure 5) and found no statistical difference in OT, IBL and postoperative DV between the groups (P>0.05).
Figure 5.
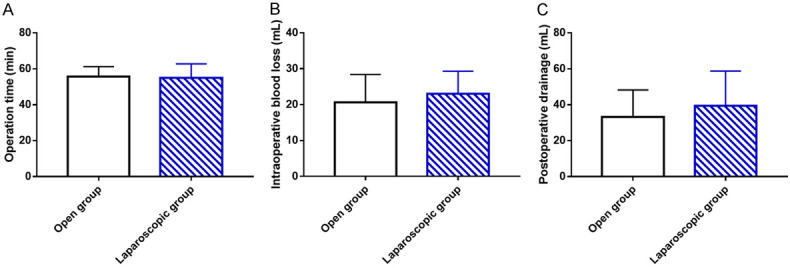
Operation-related indicators of two groups. A. Comparison of operation time between open group and laparoscopic group. B. Comparison of intraoperative blood loss between open group and laparoscopic group. C. Comparison of postoperative drainage volume between open group and laparoscopic group.
Number of CLN dissected and LOS of the patients
The number of CLN dissected and LOS of the 112 PTC patients were further analyzed to evaluate patients’ surgical outcomes and recovery (Figure 6). No statistical differences were identified between groups in the above two parameters (P>0.05).
Figure 6.
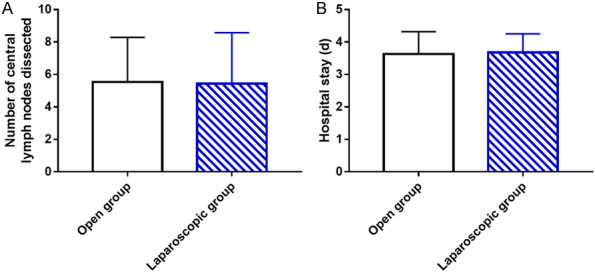
The number of central lymph node dissected and length of stay in two groups. A. Comparison of the number of central lymph node dissected between open group and laparoscopic group. B. Comparison of length of stay between open group and laparoscopic group.
Postoperative VAS and aesthetic satisfaction scores of the patients
We evaluated the postoperative VAS and aesthetic satisfaction scores of patients to analyze the influences of the two surgical methods on postoperative pain degree and aesthetic effect (Figure 7). The data revealed a similar VAS score in the two groups (P>0.05) but a significantly higher aesthetic satisfaction in the laparoscopic group than that in the open group (P<0.05).
Figure 7.
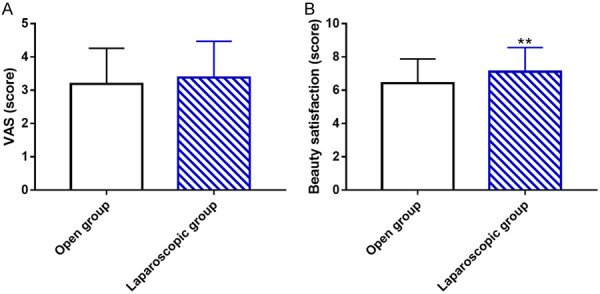
Postoperative VAS score and aesthetic satisfaction score of the two groups. A. Comparison of postoperative VAS scores between open group and laparoscopic group. B. Comparison of aesthetic satisfaction scores between open group and laparoscopic group. Note: **P<0.01 vs. open group. VAS: Visual Analogue Scale.
Postoperative complications in the patients
In the open group, hoarseness occurred in 1 case (1.92%) and choking cough when drinking in 1 case, with an overall complication rate of 3.85%. In addition to 2 cases (3.33%) of hoarseness, choking cough when drinking, numbness of hands and feet, and mucocutaneous hemorrhage were found in 1 case (1.67%) each in the laparoscopic group, with a total complication rate of 8.33%. The incidence of total complications in the two groups was not statistically significant (P>0.05). In addition, both groups of patients received at least 3 months of follow-up, and neither group exhibited recurrence or metastasis. See Table 2 for details.
Table 2.
Complications in 112 PTC patients after treatment [n (%)]
| Categories | Open group (n=52) | Laparoscopic group (n=60) | χ2 value | P value |
|---|---|---|---|---|
| Hoarseness | 1 (1.92) | 2 (3.33) | 0.213 | 0.645 |
| Choking cough when drinking | 1 (1.92) | 1 (1.67) | 0.010 | 0.919 |
| Numbness of hands and feet | 0 (0.00) | 1 (1.67) | 0.875 | 0.350 |
| Infection | 0 (0.00) | 0 (0.00) | - | - |
| Mental nerve injury | 0 (0.00) | 0 (0.00) | - | - |
| Mucocutaneous hemorrhage | 0 (0.00) | 1 (1.67) | 0.875 | 0.350 |
| Total | 2 (3.85) | 5 (8.33) | 0.957 | 0.328 |
PTC: papillary thyroid carcinoma.
Discussion
PTC is derived from molecular distortion, which is related to mitogen-activated protein kinase axis activation caused by somatic mutations and gene fusions [17]. Its pathogenic factors are complicated, involving internal and external factors such as heredity, obesity, hormones, and environmental pollutants [18]. The surgical treatment for PTC, a commonly seen malignancy related to the endocrine system of the head and neck [19], still needs to be continuously optimized to further improve patients’ medical experience.
As mentioned before, PTC accounts for 95% of all DTC cases, and the treatment is hindered by two issues: traditional surgical scars and the exposure of CLNs for dissection [20,21]. In the past, some researchers performed thyroidectomy through the anterior thoracic, areola or axillary approach, but still left scars on the patient’s body [22,23]. While TOETVA is regarded as the preferred approach for PTC patients because of its favorable cosmetic and surgical outcomes, it has two limitations in addition to the risk of developing mandibular numbness associated with mental nerve damage as previously described [24]. First, for large benign and malignant thyroid nodules, the medial vestibular incision may have to be enlarged due to the limitation of incision length and mandibular shape, which increases the risk of mental nerve injury. Second, patients previously received augmentation mentoplasty may experience an impact on the aesthetics of jaw implants due to the effect of surgical instruments used during the procedure [12]. On the basis of TOETVA and by referring to past surgical experience, this study proposed gasless ETE via submental-transoral combined approach using Kirschner wire suspension as an optimal therapy for PTC patients, and compared it with traditional open thyroidectomy.
Gasless submental-transoral ETE with Kirschner wire suspension has been clinically demonstrated by our center to provide several benefits. First, it can lower the risk of mental nerve injury and avoid postoperative numbness of the mental region [25]. In this study, mental nerve injury was only found in one case from the laparoscopic group. Second, the submental incision can reduce the difficulty and time of specimen retrieval, allowing for the removal of larger tumor specimens while ensuring the surgical efficacy [26]. This is attributed to the selection of this approach to avoid the hinderance of specimen removal by mental protuberance. Third, the risks of adverse events, such as hypercapnia and CO2 gas embolism, are reduced while ensuring a larger operating space [27], because Kirschner wire suspension can not only freely adjust the operation space, but also avoid the interference of CO2 inflation on the surgical field. Moreover, the use of the special suspension retractor can maintain the stability of the operating space for a long time, avoiding the limitations of instability and fatigue of the manual retractor. Fourth, the chimney effect is avoided due to the absence of gas in this operation [28], which reduces the risk associated with tumor implantation [29]. Fifth, the negative pressure suction function of the special suspension retractor used in this study is conducive to timely cleaning of the smoke and water mist generated by the instruments during the operation, which ensures a clear surgical field of view and reduces the number of lens wiping, making the operation more smooth and safe while reducing the risk of surgical complications [30]. Our results showed no statistical differences between the laparoscopic group and the open group in OT, IBL, postoperative DV, number of CLN dissected, LOS, and postoperative VAS score. It is suggested that compared with traditional open thyroidectomy, gasless submental-transoral ETE with Kirschner wire suspension contributes to similar surgical effects, patient recovery and pain, which is consistent with the results reported by Guo et al. [31] and Zhang et al. [32]. But in terms of aesthetic satisfaction score, gasless submental-transoral ETE with Kirschner wire suspension showed obvious advantage, namely better aesthetic effect, than the open surgery, similar to the results of Perigli et al. [33]. As far as safety is concerned, hoarseness and choking cough when drinking were found to be the main complications in the patients, but no significant difference was identified in the total complications between the laparoscopic group and the open group (8.33% vs. 3.85%), which agrees with the findings of Zhao et al. [34]. In the study conducted by Zhang et al. [14], 42 patients with PTC were included, and the application of gasless submental-transoral ETE with Kirschner wire suspension showed certain clinical feasibility and safety, which is consistent with our study results. Zeng et al. [35] reported that gasless submental approach endoscopic removal of thyroglossal cyst was not only reliable and safe, but also showed a cosmetic advantage, similar to our findings. Finally, during a follow-up period of at least 3 months, neither group of patients experienced recurrence or metastasis.
The uniqueness of this study lies in the analysis and confirmation of the clinical efficacy of gasless submental-transoral ETE with Kirschner wire suspension in PTC patients from the aspects of surgical indexes, number of CLN dissected, LOS, VAS score, cosmetic satisfaction score, and complications, providing new insights and reliable clinical basis for making surgical decisions and optimizing management approaches for patients with PTC. However, this study has some limitations that require further improvement. First, this study is single-centered with limited cases included, so it is necessary to increase the study sample and expand the sample source to increase the universality of the research results. Second, there is no long-term patient follow-up, which if supplemented, can better understand the long-term outcomes of patients undergoing this procedure.
In summary, this study demonstrates that gasless submental-transoral ETE with Kirschner wire suspension is comparable to traditional open thyroidectomy in terms of surgical effect, recovery, and safety, and is superior in aesthetic effects, making it an effective and safe procedure that can provide surgical optimization for PTC patients.
Acknowledgements
The present study was supported by the Natural Science Foundation of China grant (No. 8216070238) and Science and Technology Plan of Jiangxi Provincial Health Commission (202130408, 202310493).
Disclosure of conflict of interest
None.
References
- 1.Zhao H, Zhu X, Luo Y, Liu S, Wu W, Zhang L, Zhu J. LINC01816 promotes the migration, invasion and epithelial-mesenchymal transition of thyroid carcinoma cells by sponging miR-34c-5p and regulating CRABP2 expression levels. Oncol Rep. 2021;45:81. doi: 10.3892/or.2021.8032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li M, Pei J, Xu M, Shu T, Qin C, Hu M, Zhang Y, Jiang M, Zhu C. Changing incidence and projections of thyroid cancer in mainland China, 1983-2032: evidence from Cancer Incidence in Five Continents. Cancer Causes Control. 2021;32:1095–1105. doi: 10.1007/s10552-021-01458-6. [DOI] [PubMed] [Google Scholar]
- 3.Nies M, Vassilopoulou-Sellin R, Bassett RL, Yedururi S, Zafereo ME, Cabanillas ME, Sherman SI, Links TP, Waguespack SG. Distant metastases from childhood differentiated thyroid carcinoma: clinical course and mutational landscape. J Clin Endocrinol Metab. 2021;106:e1683–e1697. doi: 10.1210/clinem/dgaa935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xu B, Serrette R, Tuttle RM, Alzumaili B, Ganly I, Katabi N, Tallini G, Ghossein R. How many papillae in conventional papillary carcinoma? A clinical evidence-based pathology study of 235 unifocal encapsulated papillary thyroid carcinomas, with emphasis on the diagnosis of noninvasive follicular thyroid neoplasm with papillary-like nuclear features. Thyroid. 2019;29:1792–1803. doi: 10.1089/thy.2019.0328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hedman C, Djarv T, Strang P, Lundgren CI. Effect of thyroid-related symptoms on long-term quality of life in patients with differentiated thyroid carcinoma: a population-based study in Sweden. Thyroid. 2017;27:1034–1042. doi: 10.1089/thy.2016.0604. [DOI] [PubMed] [Google Scholar]
- 6.Qu R, Li J, Yang J, Sun P, Gong J, Wang C. Treatment of differentiated thyroid cancer: can endoscopic thyroidectomy via a chest-breast approach achieve similar therapeutic effects as open surgery? Surg Endosc. 2018;32:4749–4756. doi: 10.1007/s00464-018-6221-1. [DOI] [PubMed] [Google Scholar]
- 7.Wu YJ, Chi SY, Chan YC, Chou FF, Wee SY, Wu KT. Scarless completion thyroidectomy after initial transoral approach for differentiated thyroid cancer: how and when to start? Surg Laparosc Endosc Percutan Tech. 2021;31:554–557. doi: 10.1097/SLE.0000000000000933. [DOI] [PubMed] [Google Scholar]
- 8.Fama F, Zhang D, Pontin A, Makay O, Tufano RP, Kim HY, Sun H, Dionigi G. Patient and surgeon candidacy for transoral endoscopic thyroid surgery. Turk Arch Otorhinolaryngol. 2019;57:105–108. doi: 10.5152/tao.2019.18191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Suzuki T, Ikeda H, Iwamoto T, Sano H, Hashimoto M, Oe K, Inoue H, Serada K. Elective use of an uncuffed small-bore cricothyrotomy tube with balloon occlusion of the subglottic airway. Can J Anaesth. 2014;61:39–45. doi: 10.1007/s12630-013-0057-x. [DOI] [PubMed] [Google Scholar]
- 10.He QQ, Zhu J, Zhuang DY, Fan ZY, Zheng LM, Zhou P, Hou L, Yu F, Li YN, Xiao L, Dong XF, Ni GF. Comparative study between robotic total thyroidectomy with central lymph node dissection via bilateral axillo-breast approach and conventional open procedure for papillary thyroid microcarcinoma. Chin Med J (Engl) 2016;129:2160–2166. doi: 10.4103/0366-6999.189911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yu X, Jiang Y, Li Y, He Q, Pan L, Zhu P, Wang Y, Wang P. Comparison of different mandibular jawlines classifications on transoral endoscopic thyroidectomy for papillary thyroid carcinoma: experiences of 690 cases. Front Endocrinol (Lausanne) 2022;13:842148. doi: 10.3389/fendo.2022.842148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fu Y, Wu M, Fu J, Lin S, Song Z, Chen J, Yan W, Kuang P, Lin F, Luo Y, Lin E, Hong X, Wu G. TransOral endoscopic thyroidectomy via submental and vestibular approach: a preliminary report. Front Surg. 2020;7:591522. doi: 10.3389/fsurg.2020.591522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen Y, Chomsky-Higgins K, Nwaogu I, Seib CD, Gosnell JE, Shen WT, Duh QY, Suh I. Hidden in plain sight: transoral and submental thyroidectomy as a compelling alternative to “scarless” thyroidectomy. J Laparoendosc Adv Surg Tech A. 2018;28:1374–1377. doi: 10.1089/lap.2018.0146. [DOI] [PubMed] [Google Scholar]
- 14.Zhang DG, He GF, Gao L, Li JB, Chu JJ, Lu XX. Gasless submental-transoral combined appoach endoscopic thyroidectomy for papillary thyroid carcinoma: a series of 41 cases. Zhonghua Wai Ke Za Zhi. 2022;60:154–158. doi: 10.3760/cma.j.cn112139-20210520-00219. [DOI] [PubMed] [Google Scholar]
- 15.Lee J, Lee JH, Nah KY, Soh EY, Chung WY. Comparison of endoscopic and robotic thyroidectomy. Ann Surg Oncol. 2011;18:1439–1446. doi: 10.1245/s10434-010-1486-1. [DOI] [PubMed] [Google Scholar]
- 16.Jiang J, He G, Chu J, Li J, Lu X, Jiang X, Xie L, Gao L, Zhang D. Gasless submental-transoral combined approach endoscopic thyroidectomy: a new surgical technique. Front Oncol. 2023;13:1115927. doi: 10.3389/fonc.2023.1115927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu Y, Zhang H, Wang H, Du J, Dong P, Liu M, Lin Y. Long non-coding RNA DUXAP8 promotes the cell proliferation, migration, and invasion of papillary thyroid carcinoma via miR-223-3p mediated regulation of CXCR4. Bioengineered. 2021;12:496–506. doi: 10.1080/21655979.2021.1882134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lam AK. Papillary thyroid carcinoma: current position in epidemiology, genomics, and classification. Methods Mol Biol. 2022;2534:1–15. doi: 10.1007/978-1-0716-2505-7_1. [DOI] [PubMed] [Google Scholar]
- 19.Qiu K, Xie Q, Jiang S, Lin T. miR-98-5p promotes apoptosis and inhibits migration and cell growth in papillary thyroid carcinoma through Bax/Caspase-3 by HMGA2. J Clin Lab Anal. 2020;34:e23044. doi: 10.1002/jcla.23044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li Z, Wang P, Wang Y, Xu S, Cao L, Que R, Zhou F. Endoscopic lateral neck dissection via breast approach for papillary thyroid carcinoma: a preliminary report. Surg Endosc. 2011;25:890–896. doi: 10.1007/s00464-010-1292-7. [DOI] [PubMed] [Google Scholar]
- 21.Ito Y, Miyauchi A, Masuoka H, Fukushima M, Kihara M, Miya A. Excellent prognosis of central lymph node recurrence-free survival for cN0M0 papillary thyroid carcinoma patients who underwent routine prophylactic central node dissection. World J Surg. 2018;42:2462–2468. doi: 10.1007/s00268-018-4497-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee KE, Kim HY, Park WS, Choe JH, Kwon MR, Oh SK, Youn YK. Postauricular and axillary approach endoscopic neck surgery: a new technique. World J Surg. 2009;33:767–772. doi: 10.1007/s00268-009-9922-8. [DOI] [PubMed] [Google Scholar]
- 23.Nakajo A, Arima H, Hirata M, Yamashita Y, Shinden Y, Hayashi N, Kawasaki Y, Arigami T, Uchikado Y, Mori S, Mataki Y, Sakoda M, Kijima Y, Uenosono Y, Maemura K, Natsugoe S. Bidirectional Approach of Video-Assisted Neck Surgery (BAVANS): endoscopic complete central node dissection with craniocaudal view for treatment of thyroid cancer. Asian J Endosc Surg. 2017;10:40–46. doi: 10.1111/ases.12312. [DOI] [PubMed] [Google Scholar]
- 24.Wang T, Wu Y, Xie Q, Yan H, Zhou X, Yu X, Chen Y, Xiang C, Yan H, Zhao Q, Zhang M, Qi M, Wang P, Wang Y. Safety of central compartment neck dissection for transoral endoscopic thyroid surgery in papillary thyroid carcinoma. Jpn J Clin Oncol. 2020;50:387–391. doi: 10.1093/jjco/hyz195. [DOI] [PubMed] [Google Scholar]
- 25.Steinberg MJ, Kelly PD. Implant-related nerve injuries. Dent Clin North Am. 2015;59:357–373. doi: 10.1016/j.cden.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 26.Suh I, Viscardi C, Chen Y, Nwaogu I, Sukpanich R, Gosnell JE, Shen WT, Seib CD, Duh QY. Technical innovation in transoral endoscopic endocrine surgery: a modified “scarless” technique. J Surg Res. 2019;243:123–129. doi: 10.1016/j.jss.2019.05.019. [DOI] [PubMed] [Google Scholar]
- 27.Ikeda Y, Takami H, Sasaki Y, Kan S, Niimi M. Endoscopic resection of thyroid tumors by the axillary approach. J Cardiovasc Surg (Torino) 2000;41:791–792. [PubMed] [Google Scholar]
- 28.Xi C, Xu XQ, Hong T, Li BL, Liu W. Extrathyroidal implantation of thyroid hyperplastic/neoplastic cells after endoscopic thyroid surgery. Chin Med Sci J. 2014;29:180–184. doi: 10.1016/s1001-9294(14)60065-1. [DOI] [PubMed] [Google Scholar]
- 29.Binda MM, Corona R, Amant F, Koninckx PR. Conditioning of the abdominal cavity reduces tumor implantation in a laparoscopic mouse model. Surg Today. 2014;44:1328–1335. doi: 10.1007/s00595-014-0832-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Park JO, Park YJ, Kim MR, Sun DI, Kim MS, Koh YW. Gasless transoral endoscopic thyroidectomy vestibular approach (gasless TOETVA) Surg Endosc. 2019;33:3034–3039. doi: 10.1007/s00464-019-06826-7. [DOI] [PubMed] [Google Scholar]
- 31.Guo Y, Qu R, Huo J, Wang C, Hu X, Chen C, Liu D, Chen W, Xiong J. Technique for endoscopic thyroidectomy with selective lateral neck dissection via a chest-breast approach. Surg Endosc. 2019;33:1334–1341. doi: 10.1007/s00464-018-06608-7. [DOI] [PubMed] [Google Scholar]
- 32.Zhang H, Shi W, Zhang J, Xu J, Zhou D, Liu W, Fu R, Chen H. Comparing endoscopic thyroidectomy using the breast approach and conventional open thyroidectomy: a retrospective analysis. J Cancer Res Ther. 2021;17:1248–1252. doi: 10.4103/jcrt.jcrt_707_21. [DOI] [PubMed] [Google Scholar]
- 33.Perigli G, Cianchi F, Badii B, Staderini F, Skalamera I, Cupellini C, Nelli T, Foppa C. An easier option for “invisible scar” thyroidectomy: hybrid-transoral endoscopic thyroidectomy submental access (H-TOETSA)-experience on twenty-two consecutive patients. Surg Endosc. 2021;35:1796–1800. doi: 10.1007/s00464-020-07576-7. [DOI] [PubMed] [Google Scholar]
- 34.Zhao QZ, Wang Y, Wang P. A comparative study of endoscopic and traditional open surgery in the treatment of papillary thyroid carcinoma. Zhonghua Wai Ke Za Zhi. 2018;56:135–138. doi: 10.3760/cma.j.issn.0529-5815.2018.02.011. [DOI] [PubMed] [Google Scholar]
- 35.Zeng Q, Ma W, Liu C, Wu J, Wang XQ, Wang ZH, Zhu J, Hu GH. Gasless submental approach endoscopic removal of thyroglossal cyst. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2023;58:145–150. doi: 10.3760/cma.j.cn115330-20220608-00339. [DOI] [PubMed] [Google Scholar]


