Abstract
Objective
Meckel diverticulum (MD) is a common malformation of the digestive tract, often accompanied by serious complications. It is important to find safe and effective diagnostic methods for screening MD. The aim of this study was to evaluate the effectiveness of a technetium-99m (Tc-99m) scan for pediatric bleeding MD.
Methods
The authors conducted a systematic review of studies published in PubMed, Embase, and Web of Science before 1 January 2023. Studies based on PICOS were included in this systematic review. The flow chart was made by PRISMA software. The quality of included studies was assessed by RevMan5 software (QUADAS-2: Quality Assessment of Diagnostic Accuracy Studies-2). The sensitivity, specificity, and other measurements of accuracy were pooled using Stata/SE 12.0 software.
Results
Sixteen studies with 1115 children were included in this systematic review. A randomized-effects model was used for the meta-analysis because of significant heterogeneity. The combined sensitivity and specificity were 0.80 [Confidence Interval (95% CI, 0.73-0.86) and 0.95 (95% CI, 0.86-0.98)], respectively. The area under the curve (AUC) was 0.88 (95% CI, 0.85-0.90). Publication bias (Begg's test p = 0.053) was observed.
Conclusion
Tc-99m scan has high specificity, but moderate sensitivity, which is always influenced by some factors. Hence, the Tc-99m scan has some limitations in the diagnosis of pediatric bleeding MD.
Keywords: Meckel diverticulum, Tc-99m scan, Diagnosis, Gastrointestinal tract
Introduction
Meckel diverticulum (MD) has an incidence rate of 1-3% in the population. It is an embryonic residue after incomplete closure of the umbilical mesenteric canal 1 Only 25-40% of the cases have clinical symptoms,2 but 80% of the patients under 15 years of age have clinical symptoms.3 About 20% of MD cases have ectopic gastric mucosal (EGM) disease.4,5 EGM is a type of pathological tissue, most often located in MD, and is the most common cause of lower gastrointestinal bleeding in children, typically before two years of age.6 So early diagnosis of MD is important.
Although the diagnosis of a symptomatic MD is often difficult, Technetium-99m (Tc-99m) scanning can be performed in ectopic gastric mucosa. Approximately 90% of bleeding MDs contain heterotopic mucosa, which prompted the development of the Tc-99m scan.7,8
Tc-99m is helpful in the diagnosis of ectopic gastric mucosa because it compares other sites with relatively low radiographic findings.9, 10, 11, 12, 13 Moreover, the Tc-99m scan is a non-invasive test with a low radiation burden and simple operation. However, specialized expertise is necessary to acquire and interpret the images, and appropriate guidelines to perform a high-quality scan have been published.14 The aim of this study was to assess the utility of a Tc-99m scan in the diagnostic workup of pediatric patients with MD.
Materials and methods
This meta-analysis and systematic review were completed in accordance with the PRISMA guidelines.
Literature search
The PubMed, Embase, and Cochrane Library were searched to identify relevant studies published from inception to 1 January 2023. The search strategy consisted of the following keywords: (Meckel diverticulum) AND (Tc-99m scan). The authors contacted the original authors of the relevant studies to obtain additional information if required.
Study selection
Studies were included when the following criteria were met: (1) children; (2) Tc-99m scan was used as the test method; (3) surgical pathology examination was used as the reference standard; (4) randomized controlled trial (RCT), cohort study or case-control study.
Studies were excluded when the following criteria were met: (1) review, conference records, case reports, and animal experiments; (2) multiple studies based on the same data; (3) non-English studies.
Study screening and data extraction
Based on the inclusion and exclusion criteria, two researchers screened the literature, extracted data, and cross-checked the information. In case of discrepancies, the author of the original article was contacted for clarification. The following basic characteristics were extracted: country, experimental design, and original experimental data [the number of cases of TP (true positive), TN (true negative), FP (false positive), and FN (false negative)]. The authors defined a positive Tc-99m scan with negative results for both surgical exploration and Meckel diverticulum ultrasound as an "FP" and a negative Tc-99m scan, Meckel diverticulum ultrasound, and surgical exploration as a "TN".
Statistical analysis
Quality Assessment of Diagnostic Accuracy Studies-2 (QuadAS-2) was used to evaluate the literature quality. Statistical analysis was performed using RevMan 5.3 (Cochrane Collaboration) and Stata/SE 12.0. A random-effects model was used for the results. I2 value was used to evaluate the degree of heterogeneity. All statistical tests were two-sided, and p < 0.05 was considered statistically significant. Sensitivity analysis was used to determine the source of heterogeneity. Begg's test was used to assess publication bias.
Results
Literature search and study selection
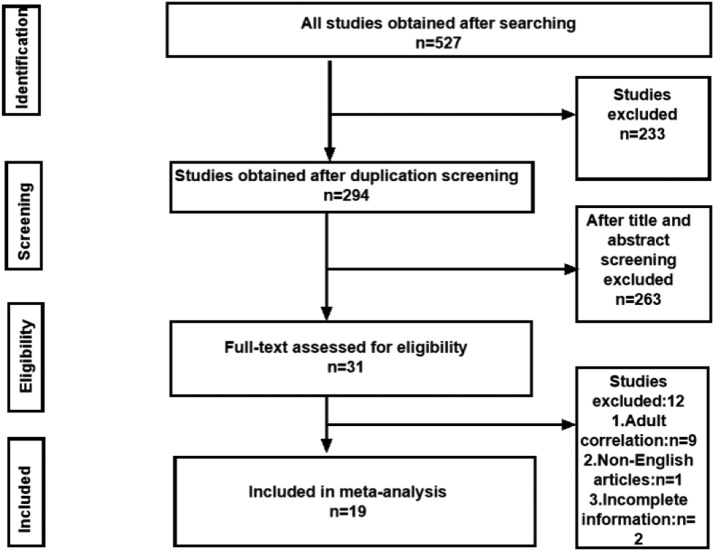
A total of 527 studies were initially identified using the literature search criteria. After screening for duplicates, 233 studies were excluded, while 263 studies were excluded after screening the title and abstract. Thereafter, 31 studies were selected for full-text evaluation of eligibility. Based on the study selection criteria, 12 studies were excluded. Finally, 19 studies (one prospective and 18 retrospective studies) were included. The flowchart is shown in Figure 1.
Figure 1.
Flow chart of literature screening for the meta-analysis.
Characteristics of the included studies and quality assessments
The characteristics and quality assessments of the selected studies are shown in Table 1. 12,15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32 A total of 1336 patients were included in the studies.
Table 1.
Characteristics of the studies included in the meta-analysis.
| Study | Country | Design | Total number | TP | FP | FN | TN |
|---|---|---|---|---|---|---|---|
| Rho J H (2013) 15 | Korea | retrospective | 12 | 11 | 0 | 1 | 0 |
| Rerksuppaphol S(2004)16 | Australia | retrospective | 9 | 7 | 0 | 2 | 0 |
| Chen Q(2018)17 | China | retrospective | 78 | 55 | 0 | 23 | 0 |
| Papparella A(2014) 18 | Italy | retrospective | 19 | 11 | 1 | 6 | 1 |
| Shalaby RY(2005)19 | Egypt | retrospective | 7 | 3 | 1 | 2 | 1 |
| Al Janabi M(2014)20 | UK | prospective | 61 | 32 | 18 | 6 | 5 |
| Sancar (2015)21 | Turkey | retrospective | 8 | 4 | 2 | 1 | 1 |
| Swaniker F (1999)12 | USA | retrospective | 43 | 12 | 0 | 8 | 23 |
| Leonidas J C(1974)22 | USA | retrospective | 13 | 3 | 0 | 1 | 9 |
| Cooney D R(1982)23 | USA | retrospective | 266 | 12 | 14 | 2 | 238 |
| Gelfand M J(1978)24 | USA | retrospective | 55 | 7 | 2 | 2 | 44 |
| Ho JE(1975)25 | USA | retrospective | 20 | 3 | 0 | 0 | 17 |
| Fries M(1984) 26 | SWEDEN | retrospective | 22 | 9 | 0 | 3 | 10 |
| Poulsen KA(2000)27 | Denmark | retrospective | 55 | 3 | 1 | 2 | 49 |
| Kong MS(1994) 28 | Taiwan(China) | retrospective | 101 | 39 | 2 | 8 | 52 |
| Sinha CK(2013) 29 | UK | retrospective | 183 | 17 | 5 | 1 | 160 |
| Dolezal J(2008)30 | Czech Republic | retrospective | 80 | 3 | 0 | 0 | 77 |
| Mittal BR(2008)31 | India | retrospective | 105 | 16 | 3 | 0 | 6 |
| McCulley S(1996)32 | South Africa | retrospective | 77 | 4 | 6 | 2 | 65 |
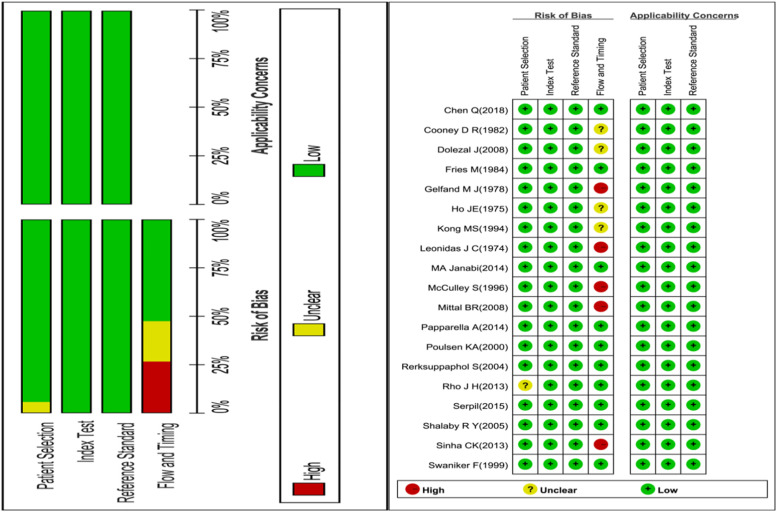
Quality assessment
The results of the quality assessment are shown in Figure 2. The overall quality of the 19 articles was relatively high. Ten studies had both a low risk of bias and low concerns regarding applicability. Five of the included studies had high risks.
Figure 2.
Quality assessment of the included studies based on QUADAS-2.
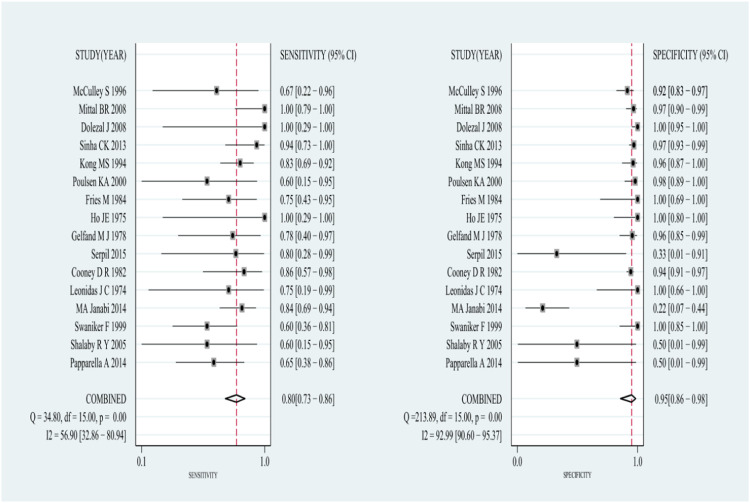
Combination of effect size
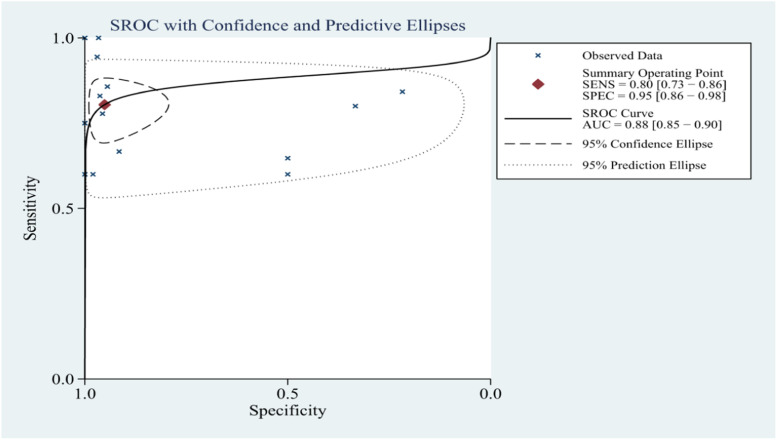
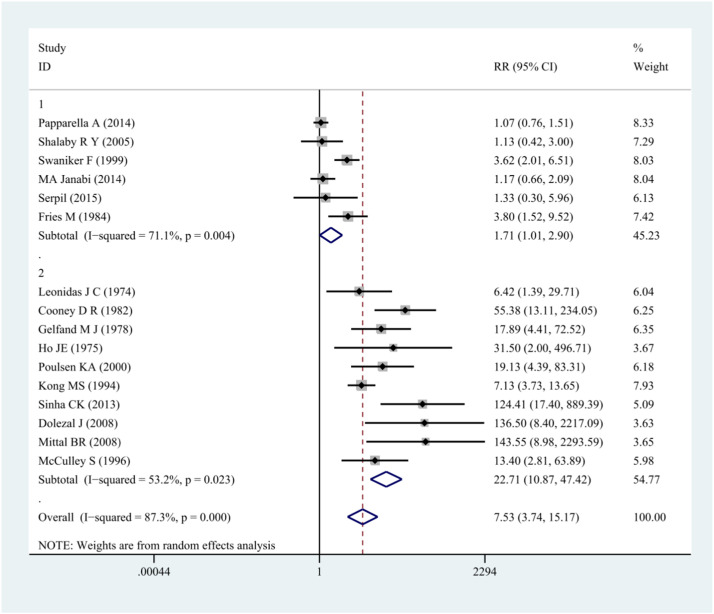
The weights of the studies of Rho JH (2013), Rerksuppaphol S (2004), and Chen Q (2018) were zero, indicating no significance of the research results, so they were excluded. A random-effects model was used due to significant heterogeneity. At last, the effect sizes of sensitivity, specificity, and summary receiver operating characteristic (SROC) were combined to conduct a meta-analysis of 16 studies, including 1115 patients. The combined sensitivity and specificity were 0.80 [Confidence Interval (95% CI, 0.73-0.86) and 0.95 (95% CI, 0.86-0.98)], respectively (Figure 3). The area under the curve (AUC) was 0.88 (95% CI, 0.85-0.90) (Figure 4).
Figure 3.
The combined sensitivity and specificity of the included studies.
Figure 4.
The SROC of the meta-analysis.
Heterogeneity test and subgroup after sensitivity analysis
The heterogeneity test revealed I2 = 91.3%, p = 0.000, which indicated significant heterogeneity. Subgroup analysis was conducted according to the sensitivity analysis (Figure 5).
Figure 5.
The meta-analysis and subgroup according to the sensitivity analysis.
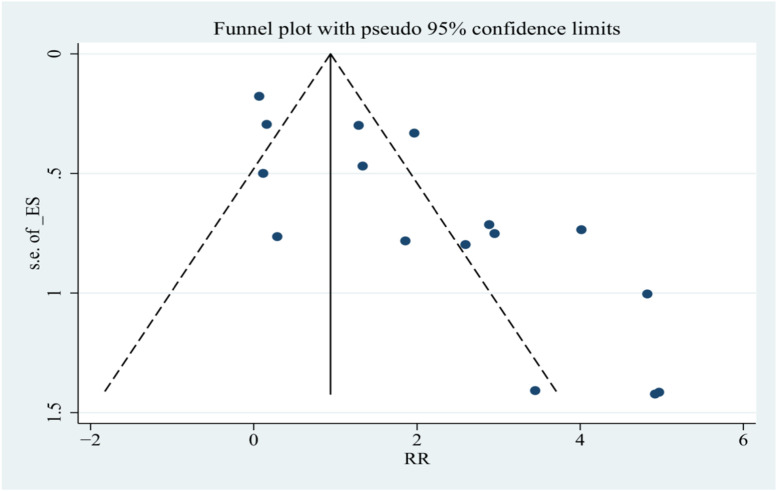
Publication bias
A funnel plot was used to determine the publication bias (Figure 6). The funnel plot was symmetric, and Begg's test was not significant (p = 0.053), indicating no publication bias.
Figure 6.
The Funnel Plot of the meta-analysis.
Discussion
MD mostly occurs in children under 15 years of age.3 However, the age of the children was not clearly stated in the original literature included, so this meta-analysis could not be conducted by age groups. Some patients experience severe bleeding, which can be life-threatening. In recent years, the Tc-99m scan is the main method for clinical diagnosis of MD, and there are some new studies about the Tc-99m scan. So, the authors conducted a systematic review and meta-analysis of all published articles, to assess the sensitivity and specificity of the Tc-99m scan.
After screening the published studies based on selection criteria, the authors included 19 studies. Three of these studies, Rho JH's study in 2013,15 Rerksuppaphol's study in 200416 and Chen Q's study in 2018,17 were excluded from the analysis because of their zero weights.
Finally, only 16 studies were included. Overall pooled diagnostic indices were as follows: sensitivity and specificity were 0.80 [Confidence Interval (95% CI, 0.73-0.86) and 0.95 (95% CI, 0.86-0.98)], respectively, indicating that most of them can be diagnosed in this way, and once diagnosed, they are confirmed.
However, the sensitivity of our study was much lower than the sensitivity of 92.1% (95% CI, 90.2-93.8) shown by Hosseinnezhad et al.,33 perhaps because the authors included some new articles, which added to the differences between groups. Another reason may be the limitations of the Tc-99m scan itself, which has clinical significance only if patients have obvious clinical symptoms, which may have also resulted in the very high specificity of 0.95 (95% CI, 0.86-0.98) in our study.
The ideal timing of the scan remains controversial. Some studies reported that the scan should be performed when the child is not actively bleeding to prevent rapid dilution of the radioisotope.34 However, other studies suggested that the scan should not be performed when there is no history of rectal bleeding. Hence, the timing of the scan and the method of capturing images are important.24,33,35,36
The sensitivity of the Tc-99m scan is affected by many factors, which is not only significantly related to the detection time in children (whether or not during active bleeding) but also closely related to the use of some drugs, such as H2 antagonists, 5-glutathione and glucagon, which can improve the accuracy of ectopic gastric mucosa detection and therefore affect the accuracy of diagnosis.34,37 For example, the use of H2 antagonists is particularly useful if there are insufficient gastric mucosal masses in the diverticulum or if the intradural imaging activity is diluted due to severe bleeding or excessive intestinal secretion, potentially leading to false negative scans. H2 antagonists such as ranitidine and cimetidine have been shown to improve scanning sensitivity by delaying the release of Tc-99m scan pertechnetate dye from mucosa and parietal cells.36
High heterogeneity was observed in our study. Hence, sensitivity analysis was performed on each data, and then subgroup analysis was performed on the results obtained from the sensitivity analysis. There was no statistically significant publication bias (Begg's test p = 0.053) in our study. This result strongly demonstrates the reliability of our results.
The high heterogeneity was related to each study, including sample size, study design, and the number of included cases. Therefore, more multi-centric prospective randomized controlled studies are needed in the future to demonstrate the clinical effects of the Tc-99m scan. Another possible factor leading to high heterogeneity in our study was the different demographics and characteristics.
The present study overcame many shortcomings of the previous meta-analyses. The authors verified our literature search results and study selection criteria. However, there were several limitations in this study. First, most of the included studies were retrospective. Therefore, these studies are not as representative as prospective randomized controlled studies. Second, the included studies and sample size were limited. Third, there was considerable heterogeneity between studies.
Conclusion
Tc-99m scan has important diagnostic significance in the clinic. However, given the relatively moderate sensitivity, which is always influenced by some factors, multiple methods should be used to actively diagnose the disease in clinical practice to avoid serious complications.
Conflicts of interest
The authors declare no conflicts of interest.
References
- 1.Berquist TH, NG Nolan, Adson MA, Schutt AJ. Diagnosis of Meckel's diverticulum by radioisotope scanning. Mayo Clin Proc. 1973;48:98–102. [PubMed] [Google Scholar]
- 2.Kilpatrick ZM. Scanning in diagnosis of Meckel's diverticulum. Hosp Practice. 1974;9:131–138. [Google Scholar]
- 3.Lüdtke FE, Mende V, Köhler H, Lepsien G. Incidence and frequency or complications and management of Meckel's diverticulum. Surg Gynecol Obstet. 1989;169:537–542. [PubMed] [Google Scholar]
- 4.Das PC, Rao PL, Radhakrishna K. Meckel's diverticulum in children. J Postgrad Med. 1992;38:19–20. [PubMed] [Google Scholar]
- 5.Cserni G. Gastric pathology in Meckel's diverticulum. Review of cases resected between 1965 and 1995. Am J Clin Pathol. 1996;106:782–785. doi: 10.1093/ajcp/106.6.782. [DOI] [PubMed] [Google Scholar]
- 6.Rutherford RB, Akers DR. Meckel's diverticulum: a review of 148 pediatric patients, with special reference to the pattern of bleeding and to mesodiverticular vascular bands. Surgery. 1966;59:618–626. [PubMed] [Google Scholar]
- 7.Harden R, Alexander WD. Isotope uptake and scanning of stomach in man with 99mTc-pertechnetate. Lancet. 1967;1:1305–1307. doi: 10.1016/s0140-6736(67)91597-8. [DOI] [PubMed] [Google Scholar]
- 8.Jewett TC, Jr, Duszynski DO, Allen JE. The visualization of Meckel's diverticulum with 99mTc-pertechnetate. Surgery. 1970;68:567–570. [PubMed] [Google Scholar]
- 9.Jaros R, Schussheim A, Levy LM. Preoperative diagnosis of bleeding Meckel's diverticulum utilizing 99m technetium pertechnetate scinti-imaging. J Pediatr. 1973;82:45–49. doi: 10.1016/s0022-3476(73)80008-3. [DOI] [PubMed] [Google Scholar]
- 10.Wine CR, Nahrwold DL, Waldhausen JA. Role of the technetium scan in the diagnosis of Meckel's diverticulum. J Pediatr Surg. 1974;9:885–888. doi: 10.1016/s0022-3468(74)80226-5. [DOI] [PubMed] [Google Scholar]
- 11.Sfakianakis GN, Conway JJ. Detection of ectopic gastric mucosa in Meckel's diverticulum and in other aberrations by scintigraphy: I. Pathophysiology and 10-year clinical experience. J Nucl Med. 1981;22:647–654. [PubMed] [Google Scholar]
- 12.Swaniker F, Soldes O, Hirschl RB. The utility of technetium 99m pertechnetate scintigraphy in the evaluation of patients with Meckel's diverticulum. J Pediatr Surg. 1999;34:760–764. doi: 10.1016/s0022-3468(99)90370-6. discussion 765. [DOI] [PubMed] [Google Scholar]
- 13.Howarth DM. The role of nuclear medicine in the detection of acute gastrointestinal bleeding. Semin Nucl Med. 2006;36:133–146. doi: 10.1053/j.semnuclmed.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 14.Ford PV, Bartold SP, Fink-Bennett DM, Jolles PR, Lull RJ, Maurer AH, Seabold JE. Procedure guideline for gastrointestinal bleeding and Meckel's diverticulum scintigraphy. Society of Nuclear Medicine. J Nucl Med. 1999;40:1226–1232. [PubMed] [Google Scholar]
- 15.Rho JH, Kim JS, Kim SY, Kim SK, Choi YM, Kim SM, et al. Clinical features of symptomatic Meckel's diverticulum in children: comparison of scintigraphic and non-scintigraphic diagnosis. Pediatr Gastroenterol Hepatol Nutr. 2013;16:41–48. doi: 10.5223/pghn.2013.16.1.41. Erratum in: Pediatr Gastroenterol Hepatol Nutr. 2013;16:135. Kim, Sung Min [corrected to Kim, Seong Min]; Kim, Yoon Mi [corrected to Kim, Yun Mi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rerksuppaphol S, Hutson JM, Oliver MR. Ranitidine-enhanced 99mtechnetium pertechnetate imaging in children improves the sensitivity of identifying heterotopic gastric mucosa in Meckel's diverticulum. Pediatr Surg Int. 2004;20:323–325. doi: 10.1007/s00383-004-1189-4. [DOI] [PubMed] [Google Scholar]
- 17.Chen Q, Gao Z, Zhang L, Zhang Y, Pan T, Cai D, et al. Multifaceted behavior of Meckel's diverticulum in children. J Pediatr Surg. 2018;53:676–681. doi: 10.1016/j.jpedsurg.2017.11.059. [DOI] [PubMed] [Google Scholar]
- 18.Papparella A, Nino F, Noviello C, Marte A, Parmeggiani P, Martino A, et al. Laparoscopic approach to Meckel's diverticulum. World J Gastroenterol. 2014;20:8173–8178. doi: 10.3748/wjg.v20.i25.8173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shalaby RY, Soliman SM, Fawy M, Samaha A. Laparoscopic management of Meckel's diverticulum in children. J Pediatr Surg. 2005;40:562–567. doi: 10.1016/j.jpedsurg.2004.11.032. [DOI] [PubMed] [Google Scholar]
- 20.Al Janabi M, Samuel M, Kahlenberg A, Kumar S, Al-Janabi M. Symptomatic paediatric Meckel's diverticulum: stratified diagnostic indicators and accuracy of Meckel's scan. Nucl Med Commun. 2014;35:1162–1166. doi: 10.1097/MNM.0000000000000193. [DOI] [PubMed] [Google Scholar]
- 21.Sancar S, Demirci H, Sayan A, Arıkan A, Candar A. Meckel's diverticulum: ten years' experience. Ulus Cerrahi Derg. 2015;31:65–67. doi: 10.5152/UCD.2015.2834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leonidas JC, Germann DR. Technetium-99m pertechnetate imaging in diagnosis of Meckel's diverticulum. Arch Dis Child. 1974;49:21–26. doi: 10.1136/adc.49.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cooney DR, Duszynski DO, Camboa E, Karp MP, Jewett TC., Jr. The abdominal technetium scan (a decade of experience) J Pediatr Surg. 1982;17:611–619. doi: 10.1016/s0022-3468(82)80121-8. [DOI] [PubMed] [Google Scholar]
- 24.Gelfand MJ, Silberstein EB, Cox J. Radionuclide imaging of Meckel's diverticulum in children. Clin Nucl Med. 1978;3:4–8. doi: 10.1097/00003072-197801000-00002. [DOI] [PubMed] [Google Scholar]
- 25.Ho JE, Konieczny KM. The sodium pertechnetate Tc 99m scan: an aid in the evaluation of gastrointestinal bleeding. Pediatrics. 1975;56:34–40. [PubMed] [Google Scholar]
- 26.Fries M, Mortensson W, Robertson B. Technetium pertechnetate scintigraphy to detect ectopic gastric mucosa in Meckel's diverticulum. Acta Radiol Diagn. 1984;25:417–422. doi: 10.1177/028418518402500513. [DOI] [PubMed] [Google Scholar]
- 27.Poulsen KA, Qvist N. Sodium pertechnetate scintigraphy in detection of Meckel's diverticulum: is it usable? Eur J Pediatr Surg. 2000;10:228–231. doi: 10.1055/s-2008-1072364. [DOI] [PubMed] [Google Scholar]
- 28.Kong MS, Huang SC, Tzen KY, Lin JN. Repeated technetium-99m pertechnetate scanning for children with obscure gastrointestinal bleeding. J Pediatr Gastroenterol Nutr. 1994;18:284–287. doi: 10.1097/00005176-199404000-00006. [DOI] [PubMed] [Google Scholar]
- 29.Sinha CK, Pallewatte A, Easty M, De Coppi P, Pierro A, Misra D, et al. Meckel's scan in children: a review of 183 cases referred to two paediatric surgery specialist centres over 18 years. Pediatr Surg Int. 2013;29:511–517. doi: 10.1007/s00383-013-3270-3. [DOI] [PubMed] [Google Scholar]
- 30.Dolezal J, Vizda J. Experiences with detection of the ectopic gastric mucosa by means of Tc-99m pertechnetate disodium scintigraphy in children with lower gastrointestinal bleeding. Eur J Pediatr Surg. 2008;18:258–260. doi: 10.1055/s-2008-1038642. [DOI] [PubMed] [Google Scholar]
- 31.Mittal BR, Kashyap R, Bhattacharya A, Singh B, Radotra BD, Narasimha Rao KL. Meckel's diverticulum in infants and children; technetium-99m pertechnetate scintigraphy and clinical findings. Hell J Nucl Med. 2008;11:26–29. [PubMed] [Google Scholar]
- 32.McCulley S, Millar AJ, Mann MD, Rode H, Brown RA. The value of sodium pertechnetate Tc99m scans in the diagnosis of Meckel's diverticulum. Pediatr Surg Int. 1996;11:240–242. doi: 10.1007/BF00178427. [DOI] [PubMed] [Google Scholar]
- 33.Hosseinnezhad T, Shariati F, Treglia G, Kakhki VR, Sadri K, Kianifar HR, et al. 99mTc-pertechnetate imaging for detection of ectopic gastric mucosa: a systematic review and meta-analysis of the pertinent literature. Acta Gastroenterol Belg. 2014;77:318–327. [PubMed] [Google Scholar]
- 34.Datz FL, Christian PE, Hutson WR, Moore JG, Morton KA. Physiological and pharmacological interventions in radionuclide imaging of the tubular gastrointestinal tract. Semin Nucl Med. 1991;21:140–152. doi: 10.1016/s0001-2998(05)80051-0. [DOI] [PubMed] [Google Scholar]
- 35.Ayati NK, Zakavi SR, Sadeghi R, Kakhki VR. Delayed imaging for detection of Meckel's diverticulum in case report Tc-99m pertechnetate scintigraphy. Iran J Nucl Med. 2008;16:45–48. [Google Scholar]
- 36.Kumar R, Tripathi M, Chandrashekar N, Agarwala S, Kumar A, Dasan JB, Malhotra A. Diagnosis of ectopic gastric mucosa using 99Tcm-pertechnetate: spectrum of scintigraphic findings. Br J Radiol. 2005;78:714–720. doi: 10.1259/bjr/16678420. [DOI] [PubMed] [Google Scholar]
- 37.Saremi F, Jadvar H, Siegel ME. Pharmacologic interventions in nuclear radiology: indications, imaging protocols, and clinical results. Radiographics. 2002;22:477–490. doi: 10.1148/radiographics.22.3.g02ma20477. [DOI] [PubMed] [Google Scholar]