Abstract
Low-grade myofibroblastic sarcoma (LGMS) is a rare malignant mesenchymal tumor derived from myofibroblasts. It is commonly identified in the head and neck, and particularly in the oral cavity, but rarely in the larynx. In this case report, we describe a patient who presented with hoarseness and underwent electronic fiber laryngoscopy, which revealed a neoplasm on the surface of his left vocal cord. The vocal cord tumor was resected under general anesthesia, and a malignant LGMS was diagnosed on postoperative pathologic examination. The results of immunohistochemical staining of the sections for vimentin (diffuse +), actin (partial +), and desmin (−) were consistent with this diagnosis. The patient recovered well after the surgery, and there was no recurrence of the neoplasm.
Keywords: Low-grade myofibroblastic sarcoma, laryngeal tumor, sarcoma, surgery, case report, vocal cord, malignancy
Introduction
Myofibroblasts are atypical cells that have the characteristics of both smooth muscle cells and fibroblasts. They are principally located in tissue that has undergone repair following injury and in benign, inactive, and locally aggressive tumors. Rarely, they may be present within an atypical malignant tumor known as a low-grade myofibroblastic sarcoma (LGMS), which accounts for approximately 1% of all malignant soft-tissue tumors. 1 Low-grade malignant myofibroblastic sarcoma has been reported to develop in the larynx and accounts for approximately 5% of all head-and-neck sarcomas. 2 The age of onset of LGMS ranges between 15 and 73 years of age, and no sex predisposition has been reported. LGMS principally develops in the head and neck, 3 and especially in the mouth, 4 but can also develop in the chest and abdominal wall, 5 abdominal cavity, 6 and limbs, particularly in the femur. 7 LGMS rarely occurs in the salivary gland, mammary gland, nasal cavity, paranasal sinus, or gingiva. 8 , 9 The features of this tumor include a lack of specific clinical characteristics, progressive enlargement, a hard texture, a clear boundary, and an intact capsule, with the possibility of recurrence. Herein, we report the case of a patient with LGMS of the larynx who was admitted to our hospital.
Case report
A man in his early 60s presented to our hospital with persistent hoarseness. The patient had presented with the same complaint, an obvious cause for which could not be identified, more than 1 month earlier, but he showed no respiratory symptoms or difficulty swallowing. Electronic fiber laryngoscopy revealed a mass in his left vocal cord, but narrow-band imaging (NBI) showed no abnormal expansion of microvessels or obvious malignant lesions (Figure 1). Enhanced computed tomography (CT) revealed a nodular shadow of approximately 5 mm in diameter in the left glottal area. The morphology of the bilateral pre-epiglottic space and epiglottic vallecula did not appear abnormal. All the laryngeal cartilaginous tissue was normal, and there was no lymph node enlargement in the area imaged (Figure 2). Physical examination revealed that the patient’s general condition was acceptable, and no obvious abnormalities were found in his heart, lungs, or abdomen. In addition to the short duration of clinical symptoms and the lack of any recent significant weight loss, abnormal proliferation of blood vessels, a sign of malignancy, was absent on electronic fiber laryngoscopy and NBI, and no glottal bone destruction was found on enhanced laryngeal CT. Thus, the neoplasm was initially considered to be benign. The patient refused to undergo preoperative biopsy, and enhanced CT showed no destruction of the laryngeal cartilage; therefore, we created a treatment plan for the patient. The patient was informed regarding the results of the investigations and the treatment plan devised, and he provided his consent to proceed with this.
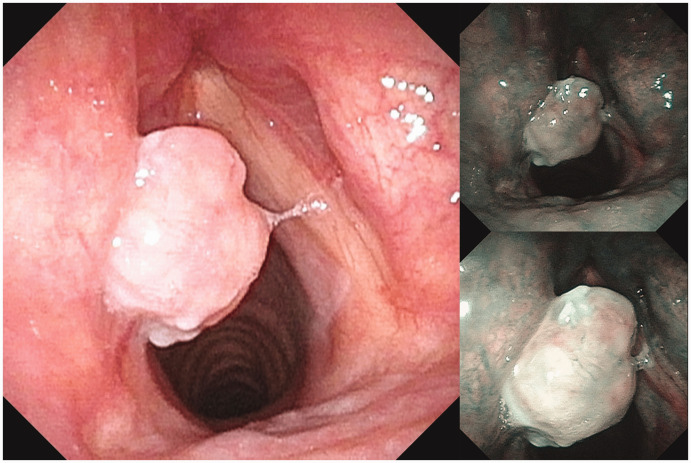
Figure 1.
Laryngoscopic image, showing a pink neoplasm in the middle and posterior thirds of the left vocal cord. Thick submucosal blood vessels were visible on the surface of the neoplasm on narrow-band imaging, and no abnormal intrapapillary capillary loop dilatation was observed.
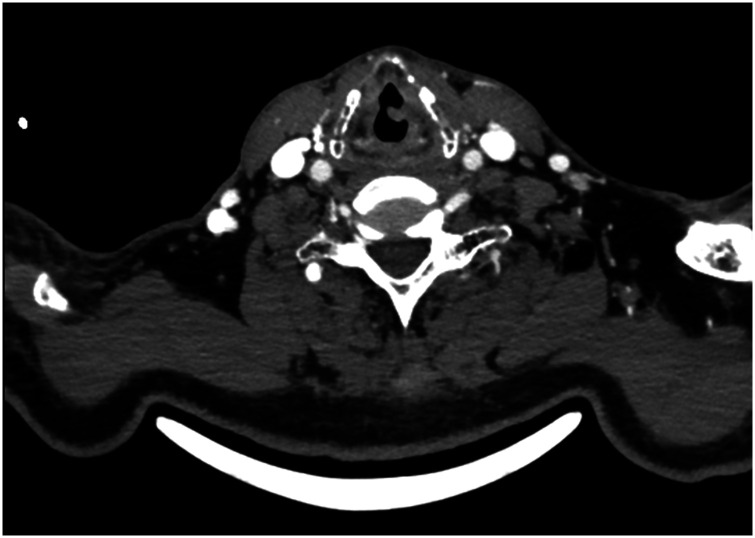
Figure 2.
A 5-mm nodular shadow was visible in the left glottic region on transverse computed tomography. The shapes of the bilateral pre-epiglottic space and epiglottic vallecula were acceptable and all the laryngeal cartilages were normal.
The laryngeal mass was completely resected using micro scissors under general anesthesia, with visualization using a microscope attached to the laryngoscope, and was subjected to pathologic examination. During surgery, the tumor was found to be located in the middle third of the left vocal cord, it was approximately 1 cm in diameter, and had a smooth surface and hard texture. Postoperative pathologic examination revealed a spindle cell tumor, consistent with a diagnosis of LGMS. An immunohistochemical examination was performed to further clarify the nature of the vocal cord neoplasm, and the tumor was vimentin (diffuse +), actin (partial +), desmin (−), Ki-67 (30% +), and p53 (90% +) (Figure 3). The final diagnosis was malignant LGMS (actin +/desmin −). The patient remained stable during follow-up. Identifying details of the patient are not disclosed in this report and the case is reported in accordance with the CARE guidelines). 10
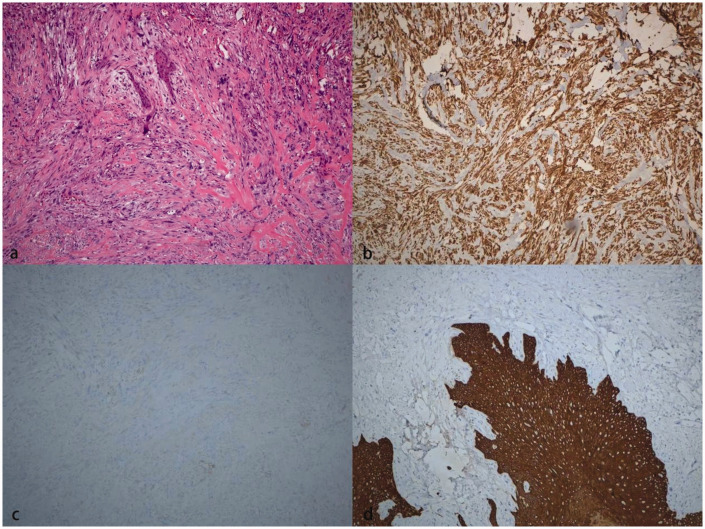
Figure 3.
Results of the pathologic examination of the resected tumor. (a) Hematoxylin and eosin-stained section, showing spindle-shaped tumor cells at ×100 magnification, some of which have prominent cell atypia, with scattered dividing nuclei. Interstitial fibers are stained red. (b) Immunohistochemical staining of a section for vimentin, showing strong, diffuse expression of vimentin. (c) Immunohistochemical staining of a section for actin, showing weak expression in some tumor cells and (d) Immunohistochemical staining of a section for cytokeratin, showing no expression in tumor cells. Normal squamous epithelium acts as the positive control.
Discussion
LGMS was first reported by Vasudev et al. in 1978 as a tumor exhibiting myofibroblastic differentiation. LGMS has ultrastructural features of both smooth muscle cells and fibroblasts. Its incidence is low, and its clinical manifestations in the head and neck vary according to the location of the tumor and its size. The initial symptoms usually relate to a progressively enlarging painless mass. Moreover, LGMS in the neck and oral cavity usually presents as a painless mass. LGMS in the glottal region typically presents with hoarseness as the initial symptom, and dyspnea may develop gradually as the tumor enlarges. LGMS in the supraglottal and subglottal regions may present as a foreign body sensation in the pharynx, cough, sore throat, progressive dysphagia, or laryngeal perichondritis. LGMS in the glottal region can be visualized as a pink mass with a smooth surface; consequently, it is easily misdiagnosed as a vocal cord polyp or granulation tissue in the laryngeal cavity. As the size of the tumor increases, its surface becomes smooth, the size of the base increases, and the surface may become necrotic. 11 , 12 In the present case, the patient presented with hoarseness and a pink mass could be visualized on the surface of his left vocal cord on electronic fiber laryngoscopy; thus, a diagnosis of vocal cord polyp could not be ruled out.
Because of the lack of specific clinical manifestations and the difficulty of diagnosing LGMS using intraoperative frozen sections, LGMS of the larynx should be differentiated from other benign and malignant lesions as follows. (1) In fibromatosis, the tumor cells are arranged in long fascicles or waves, without interwoven fascicles or a fishbone arrangement. Although mitotic figures are visible, most tumor cells have no atypical nuclei, and they express catenin, but most cells do not focally express actin and/or desmin. (2) In a fibrosarcoma, the nuclei are normal; the cytoplasm is pale; the tumor cells are distributed in solid nodules or sheets, interwoven bundles, or a fishbone-like arrangement; and the invasion of striated muscle creates a checkerboard structure. α-actin and desmin expression cannot be identified immunohistochemically, and vimentin is only focally expressed. (3) Leiomyosarcoma features eosinophilic cytoplasm and central nuclei, which are blunt and round. Immunohistochemistry shows that the tumor cells express h-caldesmon and α-actin, whereas LGMS cells are negative for h-caldesmon. (4) With respect to nodular fasciitis, the diameters of the nodules are <3 cm, rapid growth occurs (in <3 months), and the condition usually presents in patients <30 years of age. The tumor comprises hyperplastic, obese, and uniform spindle-shaped cells with a myxomatous background and red blood cell extravasation, accompanied by inflammatory cell infiltration. In addition, there are irregular tissue clefts, and pathological mitotic figures are not always present. (5) Synovial sarcoma, which can also feature a fascicular spindle arrangement, shows epithelial and mesenchymal biphasic differentiation, suggesting the expression of tumor-specific t (x; 18) (p11; q11) and SYT-SSX fusion genes. Immunohistochemistry shows that the tumor is positive for cytokeratin, epithelial membrane antigen, CD99, and vimentin expression, in contrast to LGMS.
A diagnosis of LGMS is principally made on the basis of the tumor’s pathological characteristics and immunophenotype. The basis of a diagnosis of LGMS is described in the World Health Organization pathological classification of bone and soft tissue tumors, as follows. 13 (1) The tumor shows a propulsive growth pattern, and there is infiltration of tumor cells into the submucosa and muscle tissue, causing striations. (2) The tumor tissue principally comprises spindle- or star-shaped cells, and the number of such cells varies across the tumor. The cells are arranged in loose, atypical spoke-like or fascicular patterns or dense fascicles, and the stroma is rich in collagen. (3) The tumor cells contain pale eosinophilic cytoplasm and uniform spindle-shaped nuclei, with visible atypia and mitotic figures. (4) The nuclei are hyperchromatic and irregular, with moderately high proliferative activity. (5) LGMS can be classified into three types on the basis of actin and desmin expression: actin +/desmin −, actin −/desmin +, and actin +/desmin +. The present patient was diagnosed with LGMS, and the tumor was actin +/desmin −.
The principal aim of the treatment of LGMS is to remove the mass at the primary site, and the postoperative use of radiotherapy and chemotherapy is still controversial. Most clinicians advocate wide local excision and regular review. In the present case, the tumor was small, and enhanced CT examination of the larynx did not show bone destruction or lymph node enlargement. No further treatment was planned following surgery, and the patient was recommended to undergo regular review. 14
Conclusions
LGMS of the larynx is a rare tumor with no obvious clinical manifestations. Therefore, clinicians should be aware of this condition and aim to make a prompt definitive diagnosis, because LGMS is aggressive. Surgical resection is the primary treatment, which may be followed by radiotherapy and/or chemotherapy. Moreover, the tumor commonly recurs, and indeed multiple recurrences can lead to the development of higher-grade myofibroblastic sarcoma. Therefore, patients should be closely followed up after surgery to identify any recurrence early.
Supplemental Material
Supplemental material, sj-jpg-1-imr-10.1177_03000605231193929 for Low-grade malignant myofibroblastic sarcoma of the larynx: a case report by Yu Feng, Yongya Du, Maocai Li, Guotao Jia, Lili Gong and Lianqing Li in Journal of International Medical Research
Supplemental material, sj-pdf-2-imr-10.1177_03000605231193929 for Low-grade malignant myofibroblastic sarcoma of the larynx: a case report by Yu Feng, Yongya Du, Maocai Li, Guotao Jia, Lili Gong and Lianqing Li in Journal of International Medical Research
Supplemental material, sj-pdf-3-imr-10.1177_03000605231193929 for Low-grade malignant myofibroblastic sarcoma of the larynx: a case report by Yu Feng, Yongya Du, Maocai Li, Guotao Jia, Lili Gong and Lianqing Li in Journal of International Medical Research
Author Contributions: Yu Feng: data collection and manuscript preparation.
Maocai Li and Yongya Du: manuscript preparation.
Guotao Jia: imaging.
Lianqing Li and Lili Gong: manuscript preparation and review.
All the authors read and approved the final version of the manuscript.
The authors declare that there is no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD: Yu Feng https://orcid.org/0000-0002-0312-5496
Ethics statement
The patient provided his written informed consent for the publication of this case report, and its publication was approved by the Ethics Committee of Liaocheng People’s Hospital. The study was approved by the hospital’s ethics committee (approval number 2022227).
References
- 1.Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2009. CA Cancer J Clin 2009; 59: 225–249. doi: 10.3322/caac.20006. PMID: 19474385. [DOI] [PubMed] [Google Scholar]
- 2.Velez Torres JM, Martinez Duarte E, Diaz-Perez JA, et al. Primary sarcomas of the larynx: a clinicopathologic study of 27 cases. Head Neck Pathol 2021; 15: 905–916. doi: 10.1007/s12105-021-01314-8. PMID: 33686585; PMCID: PMC8384992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Astl J, Holy R, Tuckova I, et al. Sarcomas of the larynx: one institution’s experience and treatment protocol analyses. Medicina (Kaunas) 2021; 57: 192. doi: 10.3390/medicina57030192. PMID: 33668739; PMCID: PMC7996352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mentzel T, Dry S, Katenkamp D, et al. Low-grade myofibroblastic sarcoma: analysis of 18 cases in the spectrum of myofibroblastic tumors. Am J Surg Pathol 1998; 22: 1228–1238. doi: 10.1097/00000478-199810000-00008. PMID: 9777985. [DOI] [PubMed] [Google Scholar]
- 5.Li J, Huang XY, Zhang B. Low-grade myofibroblastic sarcoma of the liver misdiagnosed as cystadenoma: a case report. World J Gastroenterol 2022; 28: 4456–4462. doi: 10.3748/wjg.v28.i31.4456. PMID: 36159015; PMCID: PMC9453762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miyazawa M, Naritaka Y, Miyaki A, et al. A low-grade myofibroblastic sarcoma in the abdominal cavity. Anticancer Res 2011; 31: 2989–2994. PMID: 21868549. [PubMed] [Google Scholar]
- 7.Arora R, Gupta R, Sharma A, et al. A rare case of low-grade myofibroblastic sarcoma of the femur in a 38-year-old woman: a case report. J Med Case Rep 2010; 4: 121. doi: 10.1186/1752-1947-4-121. PMID: 20426857; PMCID: PMC2873452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Covello R, Licci S, Pichi B, et al. Low-grade myofibroblastic sarcoma of the larynx. Int J Surg Pathol 2011; 19: 822–826. doi:10.1177/1066896910393958. [DOI] [PubMed] [Google Scholar]
- 9.Montebugnoli L, Venturi M, Gissi DB, et al. Low-grade myofibroblastic sarcoma of the gingiva. BMJ Case Rep 2010; 2010: bcr0720103166. doi: 10.1136/bcr.07.2010.3166. PMID: 22797208; PMCID: PMC3029420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gagnier JJ, Kienle G, Altman DG, et al. ; CARE Group. The CARE guidelines: consensus-based clinical case reporting guideline development. Headache 2013; 53: 1541–1547. doi: 10.1136/bcr-2013-201554. PMID: 24155002. [DOI] [PubMed] [Google Scholar]
- 11.Montgomery E, Goldblum JR, Fisher C. Myofibrosarcoma: a clinicopathologic study. Am J Surg Pathol 2001; 25: 219–228. doi:10.1097/00000478-200102000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Maruyama T, Nakasone T, Nimura F, et al. Indolent growth of low-grade myofibroblastic sarcoma of the cheek mimics benign lesions: a case report and literature review. Oncol Lett 2017; 13: 4307–4314. doi: 10.3892/ol.2017.6020. PMID: 28588708; PMCID: PMC5452922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schwerzmann MC, Dettmer MS, Baumhoer D, et al. A rare low-grade myofibroblastic sarcoma in lower jaw with the resemblance to benign lesions. BMC Oral Health 2022; 22: 380. doi: 10.1186/s12903-022-02381-1. PMID: 36064342; PMCID: PMC9446721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kordač P, Nikolov DH, Smatanová K, et al. Low-grade myofibroblastic sarcoma of the larynx: case report and review of literature. Acta Medica (Hradec Kralove) 2014; 57: 162–164. doi: 10.14712/18059694.2015.82. PMID: 25938900. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-jpg-1-imr-10.1177_03000605231193929 for Low-grade malignant myofibroblastic sarcoma of the larynx: a case report by Yu Feng, Yongya Du, Maocai Li, Guotao Jia, Lili Gong and Lianqing Li in Journal of International Medical Research
Supplemental material, sj-pdf-2-imr-10.1177_03000605231193929 for Low-grade malignant myofibroblastic sarcoma of the larynx: a case report by Yu Feng, Yongya Du, Maocai Li, Guotao Jia, Lili Gong and Lianqing Li in Journal of International Medical Research
Supplemental material, sj-pdf-3-imr-10.1177_03000605231193929 for Low-grade malignant myofibroblastic sarcoma of the larynx: a case report by Yu Feng, Yongya Du, Maocai Li, Guotao Jia, Lili Gong and Lianqing Li in Journal of International Medical Research