Abstract
Introduction
Shoulder arthroplasty is mostly performed as an inpatient procedure. Same-day discharge arthroplasty has shown positive results in hip and knee surgery. Primary objective of this study was to investigate whether a safe and satisfactory same-day discharge (SDD) can be predicted with a set of easy to use predefined criteria, without increasing complications and re-admissions.
Methods
This study was a prospective cohort study. Patient selection criteria were: <85 years old, ASA 1, 2, and mild ASA 3. Primary outcome variables were successful SDD, complications, re-admissions and patient satisfaction. Secondary outcomes were patient-reported outcome scores. The results are compared with the inpatient cohort.
Results
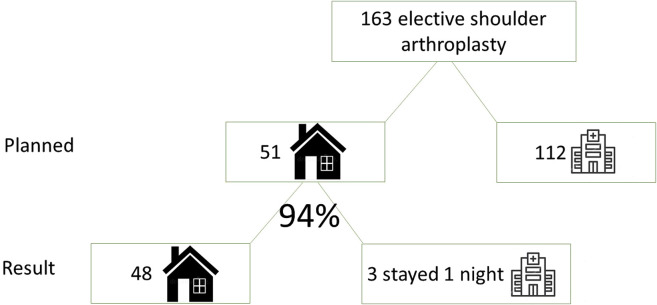
In total, 163 patients were treated for elective shoulder arthroplasty. Of which 51 patients were selected for same-day discharge arthroplasty. 94% of pre-planned same-day discharge arthroplasty patients were discharged on the day of surgery. In the same-day discharge group, there were no complications related to the early discharge and a 2% readmission rate as opposed to a 3% readmission rate in the inpatient group. Surgery related as well as medical complications did not differ between the same-day discharge and inpatient cohort.
Discussion
Same-day discharge shoulder arthroplasty is a safe and satisfying treatment option in selected patient groups.
Keywords: shoulder arthroplasty, ambulatory surgery, hospital, outcomes. cost-effectiveness, safety, complications, same-day discharge, outpatient, short stay
Introduction
Since the development of fast-track protocols in arthroplasty with advanced surgical and anesthetic techniques, the length of hospital stay (LOS) decreased substantially. 1 Previously, a week-long stay following arthroplasty was not uncommon, though nowadays patients often spend no more than 2–3 nights in the hospital.2,3 In recent years, same-day discharge arthroplasty in selected patient groups has been successfully introduced.2–6 Recent studies showed that this is a safe option in selected patients groups.4,5,7,8 This was confirmed by Darrith et al. 7 where patients who underwent same-day discharge shoulder arthroplasty showed similar 90-day outcomes including major complications, minor complications, reoperation rate, emergency department visits, or unplanned clinic visits compared to a matched control group. 7 Proper patient selection is however key in safe same-day discharge shoulder arthroplasty treatment.1,8
The ASA classification was not intended to be used to describe early discharge risk and it does not provide sufficient discrimination for safely selecting a patient for same-day discharge arthroplasty. 9 However, the modified frailty index (mFI) can be used for patient selection. The study of Shin et al. showed that the mFI prediction model can select high-risk patients who are better off staying in the hospital. 9 The mFI is, therefore, suitable to predict which patient has a higher risk of a serious complication, for example, myocardial infarction, lung embolism, septic shock, and death. With this prediction model, it is possible to identify patients at risk and to exclude them from shoulder arthroplasty in a same-day discharge setting.
In general, patients undergoing shoulder arthroplasty are ideal for a same-day discharge setting. They are expected to have no problems with mobilization, and they are not very painful. Brolin et al. 1 described lower 30-day complication rates after total shoulder arthroplasty (TSA) compared to hip and knee arthroplasty (2.8% vs. 7.6% and 6.8%, respectively), which led to an increased interest in transitioning TSA to a same-day discharge procedure. 10 Same-day discharge shoulder arthroplasty allows patients to return to the comfort of their own home, without increasing the risk of re-admission or complications, while in the process also reducing healthcare costs. 10 The Covid pandemic increases the interest in same-day discharge arthroplasty to reduce cost and to offload the inpatient hospital capacity. 10
There are a few retrospective studies on same-day discharge shoulder arthroplasty showing comparable or less complications and re-admissions for the same-day discharge group. This could be due to a selection bias since patients selected for same-day discharge surgery are usually more vital and fit patients.1,11–13 There are limited studies on functional outcome and satisfaction after same-day discharge shoulder arthroplasty and most describe relatively young patient groups. For this purpose, the goal of this study was to investigate whether a safe and satisfactory same-day discharge (SDD) can be predicted with a set of easy-to-use predefined criteria, without increasing complications and re-admissions in patients below the age of 85, undergoing shoulder arthroplasty.
Methods
We conducted a single-center prospective cohort study with two surgeons (DK, RH). The protocol was based on previous experience with same-day discharge hip arthroplasty care in our hospital. This study did not require approval by the ethical committee.
Patients
Patients with an indication for shoulder arthroplasty (osteoarthritis, unrepairable rotator cuff defect, avascular necrosis, late post traumatic [>3 months old fractures]) were evaluated for the option of same-day discharge care. All types of arthroplasties were offered in day care: total shoulder arthroplasty (TSA), hemi shoulder arthroplasty and reverse total shoulder arthroplasty (rTSA). Inclusion criteria were <85 years old, ASA 1 and 2 and mild ASA 3, no use of anticoagulants except for acetylsalicylic acid. Therefore, we used the previously described mFI. Patients were allowed to have a maximum of three risk factors on the mFI. 9 Patients had to be motivated for same-day discharge shoulder arthroplasty and have sufficient social support at home for the first few days. The only exclusion criterion was obstructive sleep apnea, due to the increased risk of hypoxemia as a result of the paralysis of the hemi-diaphragm with interscalene pain block. All patients who fulfilled the inclusion criteria and none of the exclusion criteria were offered the choice to undergo shoulder arthroplasty in day care.
Treatment
We developed one protocol for all same-day discharge arthroplasty unrelated to the type of prosthesis. The same-day discharge shoulder arthroplasty was scheduled in the morning. All patients received an ultrasound-guided interscalene block with a maximum of 20 ml levobupivacaine 0.5% ( = 5 mg/ml), standard antibiotic prophylaxis (cefazolin) and general anesthesia with sufentanil and propofol. Tranexamic acid (TXA) was given at the start of surgery to reduce blood loss. Furthermore, dexamethasone 0.15 mg/kg was given, to reduce the stress response, nausea, vomiting and to make the patient feel fitter after surgery.
All procedures were done with the patient in a beach chair position. No drains or peripheral pain catheters were used. The skin was closed intracutaneously and sealed with dermabond and a band-aid (Opsite post-op®, Smith & Nephew). After surgery, the same-day discharge arthroplasty patients were admitted to the day care clinic. The nurse or physiotherapist supervised the patient during the first mobilization. When ambulant, urinating without assistance and the pain at an acceptable level (NRS < 4), patients were discharged to their own home the same day. Pain, comfort, and complications were followed up by phone on postoperative days 1 and 3 by the surgeon or nurse, respectively. We have 24 h/day a direct phone number available for the arthroplasty patient in case of postoperative question. In daytime, this is the direct number of the nurse practitioner and in the evening/night the nurses of the orthopedic ward. The ambulant pain medication included: paracetamol, naproxen (for only three days), and short-acting oxycodone as needed. Postoperative rehabilitation was standardized depending on the type of arthroplasty implant.
Measurements
All data were collected prospectively perioperatively and six weeks and three months after surgery. Primary outcomes were successful SDD, complications, emergency department visits, hospital re-admissions, and patient satisfaction.
Postoperative complications (<1 year) were classified as major or minor. Major complications were defined as those requiring shoulder reoperation or significantly affecting the health status or rehabilitation of the patient (e.g., fracture, infection, dislocation). Minor complications were events that only minimally affected the rehabilitation of the patient (e.g., hematoma, blood transfusion).
Patient satisfaction was measured using three questions: “How much did your general daily functioning change since your shoulder surgery?”; “How much did your experience of pain change since your shoulder surgery?”; “Would you recommend this surgery to family and friends?”. Secondary outcomes were NRS pain scores (0–10), the Oxford Shoulder Score (OSS), and Quality of Life questionnaires (EQ-5D) preoperative, six weeks and three months.
Statistical analysis
Data management and analysis were performed using SPSS 23.0 (2015). NRS pain scores were presented as median (range) and analyzed using Wilcoxon signed-rank test. The OSS and EQ-5D were presented as mean and were analyzed using Wilcoxon signed-rank test. All questionnaires were measured at baseline and six weeks and three months postoperative. Since the primary outcome was the difference between baseline and three months postoperative, these results were analyzed. A p-value <0.05 was considered significant. The same-day discharge cohort is compared to the inpatient cohort.
Results
From April 2018 till November 2021, 163 patients underwent elective shoulder arthroplasty. Table 1 presents all the demographic data; 51 patients were preoperatively selected for an SDD setting and make up our SSD cohort, on an intention to treat principle. Hence, 31% of elective shoulder arthroplasty patients were planned in day care. Of the 51 planned in a same-day discharge setting, three patients (6%) failed SDD, as shown in Figure 1. One patient had to be evaluated for ECG abnormalities by the cardiologists. Fortunately, there was no myocardial infarction. The other two patients were kept in hospital overnight due to logistical issues (surgery in the afternoon instead of in the morning). Four patients visited the emergency room within 30 days postoperative (see Table 2). All patients were out of the inpatient cohort. One subluxation glenohumeral, fall 10 days after surgery, five days post-surgery bleeding, too much pain for which the patient was re-admissioned for one day.
Table 1.
Patient demographic.
| Outpatient/same day discharge (n) | Inpatient (n) | |
|---|---|---|
| Patients | 51 | 112 |
| Gender (Male/Female) | 19/32 | 24/88 |
| BMI | ||
| <25 | 11 | 24 |
| 25–30 | 24 | 44 |
| 30–35 | 13 | 33 |
| >35 | 3 | 11 |
| Average | 27.89 | 28.67 |
| Diagnosis | ||
| Osteoarthrosis | 21 | 68 |
| Irreparable rotator cuff | 15 | 27 |
| Both of the above | 12 | 9 |
| AVN | 1 | 1 |
| Post traumatic | 2 | 6 |
| Age groups | ||
| <60 | 9 | 4 |
| 60–65 | 11 | 7 |
| 66–70 | 11 | 11 |
| 71–75 | 13 | 34 |
| 76–80 | 6 | 28 |
| 81–85 | 1 | 28 |
| ASA classification | ||
| I | 10 | 3 |
| II | 34 | 42 |
| III | 7 | 63 |
| IV | 0 | 2 |
| mFI** | ||
| 0–1 | 39 | 36 |
| 1–2 | 8 | 27 |
| 2–3 | 4 | 26 |
| 3–4 | - | 15 |
| 4–5 | - | 6 |
| >5 | - | 2 |
**Modified Frailty Index.
Figure 1.
Flowchart.
Table 2.
Results.
| Outpatient/same day discharge (n) | Inpatient (n) | |
|---|---|---|
| Patients | 51 | 112 |
| Type of prosthesis | ||
| Hemi arthroplasty | 1 (2%) | 2 (2%) |
| TSA | 8 (16%) | 4 (4%) |
| rTSA | 42 (82%) | 106 (94%) |
| Length of stay (mean (range)) | 0 (0–2) | 2 (1–14) |
| Complications (<1 year) | ||
| Major | 2 (4%) | 8 (7%) |
| Minor | 4 (8%) | 4 (4%) |
| Emergency department visit (<30 days) | 0 | 4 (4%) |
| Readmission (<3 month's) | 1 (2%) | 4 (4%) |
TSA: total shoulder arthroplasty; rTSA: Reversed total shoulder arthroplasty.
In the SDD cohort, there were two major complications: one patient had a traumatic scapular spine fracture four weeks after surgery, which was treated with six weeks of sling immobilization. The other suffered from glenohumeral dislocation two months after surgery treated successfully with a close reduction under anesthesia in day care. There were four minor complications: one patient experienced persisting wound leakage 12 days postoperatively, for which she was re-admitted. Wound culture was negative, and the patient was discharged after two days of observation with a dry wound and without any additional treatment. One patient had persisting pain at three months follow-up. Two patients had a wound hematoma. No patients experienced stiffness, infections, nerve injury, revision, or the need for a blood transfusion in our same-day discharge cohort.
The median NRS pain score in rest and in motion both decreased from seven preoperatively to two at three months postoperatively. The mean OSS decreased from 40 preoperatively to 28 at three months postoperatively (Figure 2). The mean EQ-5D seems to minimally improve from 67 preoperative to 70 at three months postoperatively after three months, 81% of the patients reported improved general daily functioning since surgery (see Table 3); 92% of patients experience less pain as compared to preoperatively and 88% of the patients would recommend this treatment to family or friends.
Figure 2.
Results of pain and PROMs preoperative and postoperative.
Table 3.
PROMs scores.
| Mean (SD) | Outpatient/same day discharge | Inpatient |
|---|---|---|
| NRS pain score in rest | ||
| - Preoperative | 6.8 (2.6) | 6.8 (2.3) |
| - 6 weeks postoperative | 2.5 (2.1) | 3.1 (3.1) |
| - 3 months postoperative | 2.1 (2.1) | 1.9 (2.1) |
| EQ-5D thermometer | ||
| - Preoperative | 67 (24) | 63 (24) |
| - 6 weeks postoperative | 81 (16) | 67 (21) |
| - 3 months postoperative | 70 (22) | 71 (22) |
| OSS | ||
| - Preoperative | 40 (7) | 43 (8) |
| - 6 weeks postoperative | 32 (9) | 40 (9) |
| - 3 months postoperative | 28 (10) | 30 (11) |
OSS: Oxford shoulder score.
In our inpatient cohort (N = 112), we experienced eight major complications: one hemiparesis post-surgery, two acromion fractures at two and four months post operatively, one periprosthetic fracture three days after surgery, one tuberculum majus fracture two weeks postoperatively all treated conservatively. Two prosthetic joint infections: 2 and 14 months after surgery, both had a revision, one patient with persistent subluxation, six months post-op revision surgery with a bigger glenosphere and thick polyethylene a stable shoulder. We had four minor complications: one readmission day 2 after surgery because of too much pain, one blood transfusion for postoperative anemia; one delirium, one patient with persistent neuralgic pain at three months treated conservatively. There were 4 readmissions, leading to a readmission rate of (4/112) 4% after three months.
The median NRS pain score in rest decreased from seven preoperative to two at three months postoperative, see Table 3. The mean OSS decreased from 43 preoperative to 30 at three months postoperative (Figure 1); and the mean EQ-5D seems to minimally improve from 63 preoperative to 70 at three months postoperative. After three months, 63% of the patients scored improved general daily functioning since surgery. Furthermore, 88% of the patients scored improved pain experience since surgery and 78% of the patients would recommend this treatment to family or friends.
Discussion
This study confirms that SDD shoulder arthroplasty is a safe and satisfying option for selected patients, resulting in minimal complications, improved functional scores and a positive recommendation for this treatment.
In our cohort, 31% was planned in an SDD setting. Of our total cohort of 163 patients, 140 patients (86%) scored an mFI index of ≤3. Therefore, the potential SDD group is even higher. The most important reason for patients not to choose for an SDD setting was the lack of social support for the first 24 h after surgery.
Our preoperative selection of potential SDD was very successful resulting in a 94% SDD and a readmission rate of 2% in the pre-planned SDD arthroplasty group. In our view, several factors contribute to this success. Firstly, our multimodal, opioid-sparing anesthesia protocol, with ultrasound-guided single-shot interscalene block. 14 In our protocol, we gave a high dosage of dexamethasone 0.15 mg/kg, lowering the surgical stress response, reducing nausea and vomiting and pain, while improving well-being.15,16
Secondly, the fact that the patients were admitted to the day care ward, where every patient was discharged home at the end of the day, helped in the mindset of our patients. Thirdly not using any drains or pain catheters resulted in a more mobile and less dependent patient. Fourth, our direct phone number for postoperative patients’ questions. Available 24 h/day, this probably decreases the emergency room visits.
We only had 2.5% (N = 4) emergency room visits in our cohort, all from the clinical cohort. Our low readmission rate is in line with the review of O’Donnell, Calkins and Polisetty which reported a 3–4% readmission rate at three-month follow-up.10,17–19 Our overall complication rate in the SDD cohort was 6/51 = 12%, of which two were major complications (4%): scapular spine fracture and one dislocation is comparable with other studies.10,17,18,20 The major complication rate in the inpatient cohort (8/126) = 7% is higher than the SDD cohort (2/51) 4%. This, however, is probably attributed to a selection bias. Healthier patients are more represented in the SDD cohort. In our view, none of the complications are related to the SDD setting. The criteria based on the mFI for SDD arthroplasty patient selection was successful in our cohort. 9
Strengths and limitations
The strength of our study is the fact that we treated ASA 1, 2, and mild 3 and all types of implants in an SDD setting making our results more generalizable for standard shoulder arthroplasty care up till the age of 85 years old. Secondly, our study is a prospective cohort analyzing both the SDD and the clinical cohort looking at complications, readmissions and general- and shoulder-specific patient-reported outcome data.
Limitation of our study is the lack of direct comparison of the SDD and the inpatient group as it is not an RCT. There is a difference case-mix in the groups with a selection bias to healthier patients in the SDD group. Another weakness is the lack of data on the cost-saving of the SDD setting.
We believe that shoulder arthroplasty is the ideal joint for treatment in an SDD setting. Postoperative mobilization of the patients is not a problem because the lower extremities are not affected as with hip and knee surgery. In our cohort, about 30% patient of the shoulder arthroplasties can be done in an SDD setting, this is comparable with the 27% of Polisetty et al. 19 With the strong growth of shoulder arthroplasty also worldwide, combined with rising costs of universal healthcare and smaller hospital budgets, SDD arthroplasty in selected patient groups could help reduce costs.10,21,22 Only 20% of the inpatient cohort had an mFI > 3, leading to a potential SDD up to 80% of the shoulder arthroplasty patients. In our inpatient cohort lacking social support was the most important factor for the ‘healthier patients’ (≤3 mFI) to choose for an inpatient setting. Potentially, the social support can be done by a nursery home, rehabilitation center, or medical hotel. Although we did not measure these data, we feel this could considerably increase the number of patients undergoing SDD surgery.
However, shoulder arthroplasty in SDD should not be a goal on its own. It should be a natural result of the better recovery of the patient postoperatively resulting in a shorter hospital stay. It is a team effort for all care takers (nurses, physiotherapists, anesthesiologists, and orthopedic surgeons) to make SDD shoulder arthroplasty work. Therefore, a clear treatment protocol is essential for success.
Conclusion
Same-day discharge shoulder arthroplasty is a safe and satisfying treatment option in selected patient groups. This can be the next step in improving efficiency in shoulder arthroplasty care. About 30% of all shoulder arthroplasties can be done in a same-day discharge setting. This can be the next step in improving efficiency in shoulder arthroplasty care and reducing healthcare costs.
Footnotes
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: van Kampen and Hillen have a consultancy contract withExactech Company. This study was not sponsored by Exactech.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Derk A van Kampen https://orcid.org/0000-0001-8775-7257
References
- 1.Brolin TJ, Throckmorton TW. Outpatient shoulder arthroplasty. Orthop Clin North Am 2018; 49: 73–79. [DOI] [PubMed] [Google Scholar]
- 2.Berger RA, Sanders SA, Thill ESet al. et al. Newer anesthesia and rehabilitation protocols enable outpatient hip replacement in selected patients. Clin Orthop Relat Res 2009; 467: 1424–1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.den Hartog YM, Mathijssen NMC, Vehmeijer SBW. Reduced length of hospital stay after the introduction of a rapid recovery protocol for primary THA procedures. Acta Orthop 2013; 84: 444–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vehmeijer SBW, Husted H, Kehlet H. Outpatient total hip and knee arthroplasty. Acta Orthop 2018; 89: 141–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hoffmann JD, Kusnezov NA, Dunn JCet al. et al. The shift to same-day outpatient joint arthroplasty: a systematic review. J Arthroplasty 2018; 33: 1265–1274. [DOI] [PubMed] [Google Scholar]
- 6.Berger RA, Kusuma SK, Sanders SAet al. et al. The feasibility and perioperative complications of outpatient knee arthroplasty. Clin Orthop Relat Res 2009; 467: 1443–1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Darrith B, Frisch NB, Tetreault MWet al. et al. Inpatient versus outpatient arthroplasty: a single-surgeon, matched cohort analysis of 90-day complications. J Arthroplasty 2019; 34: 221–227. [DOI] [PubMed] [Google Scholar]
- 8.Fournier MN, Brolin TJ, Azar FMet al. et al. Identifying appropriate candidates for ambulatory outpatient shoulder arthroplasty: validation of a patient selection algorithm. J Shoulder Elbow Surg 2019; 28: 65–70. [DOI] [PubMed] [Google Scholar]
- 9.Shin JI, Keswani A, Lovy AJet al. et al. Simplified frailty index as a predictor of adverse outcomes in total hip and knee arthroplasty. J Arthroplasty 2016; 31: 2389–2394. [DOI] [PubMed] [Google Scholar]
- 10.O’Donnell EA, Fury MS, Maier SPet al. et al. Outpatient shoulder arthroplasty patient selection, patient experience, and cost analyses: a systematic review. JBJS Rev 2021; 9. [DOI] [PubMed] [Google Scholar]
- 11.Van Kampen DA, de Vries LM, Hillen RJet al. et al. Prospective cohort study of outpatient shoulder arthroplasty. Nederlands Tijdschrift Voor Orthopedie 2020. [Google Scholar]
- 12.Basques BA, Erickson BJ, Leroux T, et al. Comparative outcomes of outpatient and inpatient total shoulder arthroplasty: an analysis of the Medicare dataset. Bone Joint J 2017; 99-B(7): 934–938. doi: 10.1302/0301-620X.99B7.BJJ-2016-0976.R1. PMID: 28663400. [DOI] [PubMed] [Google Scholar]
- 13.Bean BA, Connor PM, Schiffern SCet al. et al. Outpatient shoulder arthroplasty at an ambulatory surgery center using a multimodal pain management approach. J Am Acad Orthop Surg Glob Res Rev 2018; 2: e064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abdallah FW, Halpern SH, Aoyama Ket al. et al. Will the real benefits of single shot interscalene block please stand up? A systematic review and meta-analysis. Anesth Analg 2015; 120: 1114–1129. [DOI] [PubMed] [Google Scholar]
- 15.Fan Z-R, Ma J, Ma X-L, et al. The efficacy of dexamethasone on pain and recovery after total hip arthroplasty: a systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore) 2018; 97: e0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lunn TH, Kehlet H. Perioperative glucocorticoids in hip and knee surgery - benefit vs. Harm? A review of randomized clinical trials. Acta Anaesthesiol Scand 2013; 57: 823–834. [DOI] [PubMed] [Google Scholar]
- 17.Calkins TE, Mosher ZA, Throckmorton TWet al. et al. Safety and cost effectiveness of outpatient total shoulder arthroplasty: a systematic review. J Am Acad Orthop Surg 2022; 30: e233–e241. [DOI] [PubMed] [Google Scholar]
- 18.Willenbring TJ, DeVos MJ, Kozemchak AMet al. et al. Is outpatient shoulder arthroplasty safe in patients aged ≥65 years? A comparison of readmissions and complications in inpatient and outpatient settings. J Shoulder Elbow Surg 2021; 30: 2306–2311. [DOI] [PubMed] [Google Scholar]
- 19.Polisetty TS, Grewal G, Drawbert Het al. et al. Determining the validity of the Outpatient Arthroplasty Risk Assessment (OARA) tool for identifying patients for safe same-day discharge after primary shoulder arthroplasty. J Shoulder Elbow Surg 2021; 30: 1794–1802. [DOI] [PubMed] [Google Scholar]
- 20.Erickson BJ, Shishani Y, Jones S, et al. Outpatient versus inpatient anatomic total shoulder arthroplasty: outcomes and complications. JSES INTL 2020; 4: 919–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dutch Arthroplasty Register (LROI) 2018 [Internet]. (accessed 22 February 2022). Beschikbaar op: https://www.lroi.nl/publicaties/jaarrapportage.
- 22.Palsis JA, Simpson KN, Matthews JHet al. et al. Current trends in the use of shoulder arthroplasty in the United States. Orthopedics 2018; 41: e416–e423. [DOI] [PubMed] [Google Scholar]