Abstract
Background
This systematic review and network meta-analysis compare clinical outcomes of three different subscapularis management techniques in anatomic total shoulder arthroplasty: lesser tuberosity osteotomy, subscapularis peel, and subscapularis tenotomy.
Methods
PubMed, Web of Science, Embase, and Cochrane's trial registry were searched in July 2021. Comparative studies and case series evaluating the outcomes of these three techniques were included. The network meta-analysis was performed only on comparative studies.
Results
Twenty-three studies were included. Both lesser tuberosity osteotomy and subscapularis peel had significantly higher Western Ontario Osteoarthritis Scores compared to subscapularis tenotomy, but no difference in American Shoulder and Elbow Society Scores. Subscapularis peel had superior external rotation compared to lesser tuberosity osteotomy. However, no difference was found in external rotation between subscapularis peel and subscapularis tenotomy or between subscapularis tenotomy and lesser tuberosity osteotomy. The overall weighted average for lesser tuberosity osteotomy bony union was 93.6%, whereas the overall weighted average for subscapularis tendon healing was 79.4% and 87% for subscapularis tenotomy and subscapularis peel, respectively.
Discussion
This network meta-analysis demonstrated that lesser tuberosity osteotomy and subscapularis peel were associated with the high union and subscapularis healing rates and may be associated with improved shoulder function and quality of life, compared to subscapularis tenotomy. Lesser tuberosity osteotomy and subscapularis peel demonstrate a trend of superior outcomes compared to subscapularis tenotomy during anatomic total shoulder arthroplasty.
Keywords: subscapularis, total shoulder arthroplasty, subscapularis tenotomy, subscapularis peel, subscapularis osteotomy
Introduction
Anatomic total shoulder arthroplasty (aTSA) is a common and effective treatment of shoulder arthritis.1,2 Given the excellent clinical outcomes, it is unsurprising that the utilization of aTSA is quickly growing. In 2017, 3 12.5 of every 100,000 surgeries performed were an aTSA. Due to the rapidly increasing utilization of TSA, it is important for orthopedic surgeons to understand the intricacies of its surgical technique. One area of technique variability between surgeons is the management of the subscapularis tendon during the surgical approach.
The subscapularis tendon is encountered during the deltopectoral approach and must be mobilized to gain access to the glenohumeral joint. The aTSA surgical technique originally described by Neer involved a subscapularis tenotomy (ST). 4 In this technique, the tendon was vertically incised with a cuff of insertional tissue preserved for later repair on the lesser tuberosity. The two ends of the tendon were repaired end-to-end following component placement and during closure. Subsequently, a lesser tuberosity osteotomy (LTO) was described, 5 allowing for direct repair to bone at the end of the case. This technique allows for bony healing, which may be biomechanically advantageous compared to tendinous healing.6,7 Lastly, a third technique, the subscapularis peel (SP), has been described where the subscapularis is dissected directly from its insertion on the lesser tuberosity. 8 The tendon is then repaired directly to the bone using one of a variety of techniques, often utilizing heavy nonabsorbable sutures, bone tunnels, and/or suture anchors.6,9,10
To evaluate the effectiveness of each technique, objective measures are required. The American Shoulder and Elbow Society (ASES) Score and Western Ontario Osteoarthritis of the Shoulder (WOOS) index are validated tools for scoring shoulder function that are commonly utilized after shoulder arthroplasty.11–13 Shoulder range of motion (ROM), strength and surgical complications also serve as meaningful comparison points. There is a high degree of variability in reporting post-surgical outcomes following aTSA and because of this, it is challenging to ascertain optimal subscapularis management technique. Due to this variability, the American Academy of Orthopaedic Surgeons has been unable to recommend one surgical technique over another. 14 Moreover, prior systematic reviews have not demonstrated significant functional differences between all three subscapularis management techniques.15–17 Compared to the last meta-analysis, 15 three additional comparative studies were sought in this study. Furthermore, all non-comparative studies in the literature were included to gain a further understanding of subscapularis healing and LTO union rates. To further elucidate which method is preferable, the aim of this study was to provide an updated comparison between different techniques for subscapularis management in aTSA through network meta-analyses techniques.
Methods
This systematic review and network meta-analysis were conducted with adherence to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses. 18
The primary aim of this study was to compare shoulder function scores between LTO, SP, and ST techniques. The secondary outcomes were shoulder ROM and strength, subscapularis tendon integrity on imaging, union rate of the LTO, and complication rates.
Eligibility criteria
Included studies were clinical comparative and non-comparative studies investigating the outcomes of interest utilizing different subscapularis management techniques during aTSA—LTO, SP, or ST. The exclusion criteria were non-clinical biomechanical studies, case reports, reviews, inaccessible full text, articles publishing in languages other than English, and those not reporting on outcomes of interest.
Information sources and search strategy
PubMed, Web of Science, Embase and Cochrane's trial registry were searched in July 2021. Keywords included: “Shoulder” AND (“Arthroplasty” OR “Replacement”) AND (“Subscapularis Peel” OR “Subscapularis Tenotomy” OR “Lesser Tuberosity Osteotomy”). Studies were screened by titles and abstracts. A full-text review was performed if a study matched the eligibility criteria. The search strategy was performed by two authors independently.
Data collection process and data items
Data were collected independently by two authors. The data items that were collected included: the first authors’ surnames, study year and location, age, sex, number of patients, diagnoses, form of subscapularis management, follow-up time points, The ASES scores, the WOOS index, shoulder ROM, internal rotation strength, LTO union rate, subscapularis tendon integrity on imaging, and overall complications.
Qualitative synthesis
The qualitative analysis was performed with two different tools. Randomized controlled trials (RCTs) were evaluated with the Cochrane Risk of Bias assessment tool. 19 The tool contains five domains which assess the randomization, adherence to intended treatments, missing outcomes, measurement bias, and reporting bias. Whereas, non-randomized studies, including cohort studies and case series, were evaluated with the methodological index for non-randomized studies (MINORS) criteria which consists of 12 items. 20 The first eight items are designed to evaluate the quality of either comparative or non-comparative studies. Four additional items are added to further evaluate comparative studies only. Each study was assessed by two authors independently.
Quantitative synthesis
The network meta-analysis was performed with the use of R software (version 3.5.1; R Foundation for Statistical Computing, Vienna, Austria) and the “netmeta” R package (version 0.9-6; R Foundation for Statistical Computing). The outcomes were estimated with the use of a 95% confidence interval (CI), and a significant difference in outcomes was considered statistically significant if the P-value was less than 0.05. The mean difference (MD) was used for estimating the treatment effect of continuous outcomes. The Hedges G standard mean difference (SMD) was used for estimating the effect on the postoperative strength indices due to potential variability in measurement among studies. P-scores were generated for outcome measure comparisons to rank the three subscapularis management techniques. A higher P-score indicates that on average one treatment is superior compared to competing treatments for each outcome measure. The meta-analytic models were based on random effects with the use of the DerSimonian–Laird method as a heterogeneity variance estimator.
Only comparative studies were included in the network meta-analysis for the following comparative outcomes: ASES score, WOOS index, shoulder ROM, and shoulder internal rotation strength. ST was considered as the reference treatment in this network meta-analysis unless there was a significantly inferior treatment. For each non-comparative outcome such as LTO union and subscapularis tendon healing rates, both comparative and non-comparative studies results were combined to provide an overall weighted average for each outcome. Complications were summarized and were not pooled due to heterogeneity in the level of evidence.
Results
Study selection
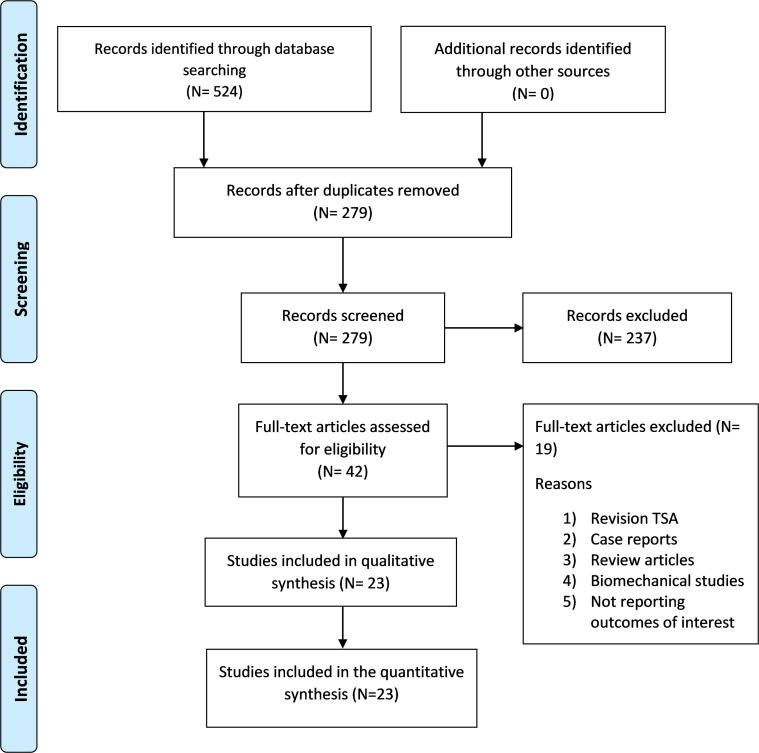
The search strategy resulted in 524 articles, of which 279 articles were duplicated and removed. The records were then screened by titles and abstracts against the eligibility criteria, which resulted in 237 exclusions. Next, 19 of the 42 remaining articles were excluded for either being a case report, review article, biomechanical study, or included revision TSA. A total of 23 studies were eligible for inclusion (Figure 1).
Figure 1.
Search strategy flowchart. TSA: total shoulder arthroplasty.
Study characteristics
Table 1 displays the characteristics of the included studies. Out of the 23 included studies, three were RCTs, seven were cohort studies, and 13 were case series. A total of 1787 patients underwent shoulder arthroplasty, of which 1041 had LTO, 455 underwent ST, and 292 underwent SP. The mean age among studies ranged from 60 to 71.3 years, except for the case series by Gerber et al. 5 where patients had a mean age of 57 years. Most indications were primary osteoarthritis of the shoulder, with minor cases of rheumatoid arthritis and avascular necrosis. The follow-up period ranged between 12 months and 50 months. There were two articles by Lapner et al. published in 2012 8 and 2013 21 with a similar population, however, each article addressed different outcomes. Each article's sample was used in this meta-analysis for the outcome it reported. Armstrong et al. had two publications in 2006 22 and 2016, 23 with different populations in both articles. The preoperative quality of the subscapularis tendon was evaluated differently across studies. Nine studies had only reported that aTSA was performed for primary osteoarthritis without preoperative imaging documenting subscapularis muscle quality, with the exclusion of inflammatory arthritis, osteonecrosis, traumatic or post-traumatic conditions and prior open shoulder surgery.6,22,24–30 One study reported that subscapularis integrity was confirmed with physical examination in addition to applying the aforementioned exclusion criteria. 31 In contrast, aTSA was performed for primary osteoarthritis in addition to rheumatoid arthritis in two studies;8,32 in addition to posttraumatic osteoarthritis and trauma in one study; 33 or in addition to rheumatoid arthritis and avascular necrosis in two studies;34,35 or in addition to inflammatory and instability arthritis or trauma in one study. 5 Four studies performed aTSA in glenohumeral osteoarthritis only and confirmed subscapularis integrity based on preoperative physical examination and advanced imaging in selected cases with an equivocal physical examination.36–39 Three studies did not specify clear eligibility criteria or preoperative subscapularis evaluation.40–42
Table 1.
Baseline characteristics of included studies.
| Study | Design, LoE | Subscapularis management | Mean age | Male % | Diagnosis | TSA | HA | Follow-up |
|---|---|---|---|---|---|---|---|---|
| O’Brien 2020 24 | RCS, III | LTO 28/ST 37 | 68.8/64.8 | 85.7/56.7 | Primary OA | 100% | 0% | 28.4 mo/33.4mo |
| Johnson 2020 40 | CS IV | LTO 142 | 65.2 | 50.80% | NR | 100% | 0% | 12 mo |
| Lapner 2019 25 | RCT, II | ST 37/SP 44 | 69.7 | 48% | Primary OA | 100% | 0% | 24 mo |
| Levine 2019 36 | RCT, I | ST 30/LTO 29 | NR | NR | Primary OA | 100% | 0% | 24 mo |
| Aibinder 2019 26 | RCS, III | ST 68/LTO 55/SP 65 | 64/62/60 | 54%/51.5%/42% | Primary OA | 100% | 0% | 24 mo |
| Levy 2019 41 | CS IV | LTO 189 | 69.5 | 58.20% | NR | 100% | 0% | 50 mo |
| Baumgarten 2018 27 | PPS, I | ST 36 | 70.3 | 55.50% | Primary OA | 100% | 0% | 12 mo |
| Mason 2018 43 | RCS, III | ST 24/LTO 15 | 68.2/70.2 | 71%/60% | Primary OA 37, RA 2 | 100% | 0% | 18.5 mo/20.6 mo |
| Shafritz 2017 44 | RCS, III | SP 46/44 LTO | 61.7/64.6 | 62.20% | Primary OA | 100% | 0% | 48 mo |
| Gobezie 2017 42 | CS IV | SP 60 | 63.9 | 65% | Primary OA | 100% | 0% | 15 mo |
| Armstrong 2016 23 | CS IV | ST 30 | 64 | 50% | Primary OA | 100% | 0% | 24 mo |
| Small 2014 38 | CS IV | LTO 220 | 62.5 | 54.1 | NR | 100% | 0% | Range 6–78 mo |
| Buckley 2014 32 | RCS, III | ST 32/LTO 28 | 68.4/68.3 | 62/54 | OA (94–96%) | 100% | 0% | 31.7 mo/22.1 mo |
| Liem 2012 31 | CS IV | SP 23 | 71.3 | 39 | OA | 61% | 39% | 43 mo |
| Lapner 2012/20138,21 | RCT, I | SP 39/LTO 40 | 65.3/70.4 | 39 | OA (91%/98%) | 80%/83% | 20%/16% | 24 mo |
| De Wilde 2012 39 | CS IV | LTO 36 | 68 | 28 | OA | 100% | 0% | 18 mo |
| Jandhyala 2011 28 | RCS, III | ST 10/LTO 26 | 64/68.4 | 60/53.8 | OA (97.2%) | 100% | 0% | 38 mo |
| Scalise 2010 29 | RCS, III | SP 15/LTO 20 | 67/69 | 46.6%/70% | OA | 100% | 0% | 39 mo/30 mo |
| Jackson 2010 30 | CS IV | ST 15 | 67.1 | NR | OA | 100% | 0% | 31.6 mo |
| Krishnan 2009 6 | CS IV | LTO 100 | 63 | 41 | NR | 100% | 0% | 31 mo |
| Qureshi 2008 34 | CS IV | LTO 30 | 66 | NR | OA (76%)/AVN (16%) | 100% | 0% | 13 mo |
| Armstrong 2006 22 | CS IV | ST 30 | 70.4 | 46 | OA | 100% | 0% | 19 mo |
| Gerber 2005 45 | CS IV | LTO 39 | 57 | 50 | OA (43%)/inflammatory (25%) | 100% | 0% | 39 mo |
LOE: level of evidence; LTO: lesser tuberosity osteotomy; ST: subscapularis tenotomy; SP: subscapularis peel; CS: cohort study; RCS: retrospective cohort study; PPS: prospective prognostic study; RCT: randomized controlled trial; OA; osteoarthritis; NR: not reported. TSA: total shoulder arthroplasty; HA: hemiarthroplasty; mo: months.
Qualitative analysis
The risk of bias assessment demonstrated low risks of bias for all three RCTs (Appendix Figure 1). The MINORS score for the seven non-randomized comparative studies ranged from 18 to 23 (out of 24). The cohort studies by Jandhyala et al., 28 Buckley et al., 32 and Scalise et al. 29 had the highest MINORS score. For case series, the MINORS score ranged between 8 and 14 (out of 16). Armstrong et al. 23 in 2016 had the highest MINORS score for case series (14 out of 16). Most cohort and case series studies had low scores because of the lack of statistical power calculation and/or the lack of outcome assessors blinding. The MINORS scores are summarized in Appendix Table 2.
The ASES score
A total of five studies reported post-operative ASES scores at an average follow-up of 23.3 months.8,24–26,36 The number of patients for the ASES comparison was 250 for LT, 227 for LP and 210 for LTO. The highest P-score was achieved by ST (0.72). The second highest P-score was achieved by SP (0.69), while LTO (0.08) had the lowest P-score (0.08). There was no statistically significant difference in ASES scores between LTO and ST (MD: 3.35; 95% CI: −7.9, 1.23) or SP and ST (MD: −4.2; 95% CI: −4.2, 3.9) (Figure 2).
Figure 2.
Forest plot representing the network meta-analysis comparison of American Shoulder and Elbow Society (ASES) scores between lesser tuberosity osteotomy (LTO), subscapularis peel (SP), and subscapularis tenotomy (ST). MD: mean difference; CI: confidence interval.
WOOS index
A total of four studies reported post-operative WOOS index with an average follow-up of 23.5 months.8,25,32,43 The total number of patients for the WOOS comparison was 97 patients for LP, 103 patients for LT, and 86 patients for LTO. The highest P-score was achieved by LTO (0.84), followed by SP (0.65). There was no statistically significant difference between LTO and SP (MD 1.5; 95% CI: −4.8, 7.8). On the other hand, ST had the lowest P-score (0.01), and it had significantly lower WOOS indices compared to both LTO and SP. The MD was 8.36 (95% CI: 2.8, 13.9) between LTO and SP, and 6.85 (95% CI: 0.33. 13.4) between SP and ST (Figure 3).
Figure 3.
Forest plot representing the network meta-analysis comparison of Western Ontario Osteoarthritis of the Shoulder (WOOS) indices between lesser tuberosity osteotomy (LTO), subscapularis peel (SP), and subscapularis tenotomy (ST). MD: mean difference; CI: confidence interval.
Shoulder forward elevation range of motion
Seven studies reported shoulder forward elevation ROM with an average follow-up of 27.9 months.24–26,28,32,36,44 The total number of patients for the forward elevation comparison was 229 patients for SP, 292 for ST, and 265 patients for LTO. The highest P-score was achieved by LTO (0.81). ST had a P-score of 0.61, and SP had the lowest P-score of 0.07. There was no difference between SP and ST (SMD: −0.19; 95% CI: −0.48, 0.1), and no difference between SP and LTO (SMD: 0.06; 95% CI: −0.19, 0.3) (Figure 4).
Figure 4.
Forest plot representing the network meta-analysis comparison of forward elevation range of motion (ROM) between lesser tuberosity osteotomy (LTO), subscapularis peel (SP), and subscapularis tenotomy (ST). SMD: standardized mean difference; CI: confidence interval.
Shoulder abduction range of motion
Only three studies reported shoulder abduction ROM at an average follow-up of 31.9 months.24,28,32 Only ST and LTO were reported in these studies, therefore, a direct meta-analysis was performed between both treatments only. The total number of patients for the ST group was 79 patients, and 82 patients for the LTO group. There was no significant difference between LTO and ST (SMD: −0.03; 95% CI: −0.35, 0.29) (Figure 5).
Figure 5.
Forest plot representing the network meta-analysis comparison of abduction range of motion (ROM) between lesser tuberosity osteotomy (LTO) and subscapularis tenotomy (ST). SMD: standardized mean difference; CI: confidence interval.
Shoulder external rotation range of motion
Six studies reported external rotation ROM at an average follow-up of 28 months.24–26,28,29,32 The total number of patients was 277 for ST, 183 for SP and 212 for LTO. SP achieved the highest P-score (0.97), whereas both ST and LTO had lower P-scores of 0.45 and 0.07, respectively. SP had a statistically significant increase in external rotation when compared to LTO (SMD: 0.5; 95% CI: 0.11, 0.9) (Figure 6). There was no difference in external rotation between ST and LTO (SMD: 0.17; 95% CI: −0.13, 0.46). Likewise, no difference was found between SP and ST (SMD: 0.34; 95% CI: −0.02, 0.7).
Figure 6.
Forest plot representing the network meta-analysis comparison of external rotation range of motion (ROM) between lesser tuberosity osteotomy (LTO), subscapularis peel (SP), and subscapularis tenotomy (ST). SMD: standardized mean difference; CI: confidence interval.
Shoulder internal rotation strength
Six studies reported internal rotation strength by using a hand-held dynamometer at an average follow-up of 28 months.8,24,25,29,32,36 The total number of patients for the internal rotation strength comparison was 151 patients for ST, 83 for SP, and 145 for LTO. All force units were converted from Newtons or Pounds force to Kilograms force. SP achieved the highest P-score (0.8), followed by LTO (0.68) and ST (0.01). There was no difference in internal rotation strength between SP and LTO (SMD: 0.07; 95% CI: −0.37, 0.5). However, both LTO and SP had statistically significant increases in internal rotation strength when compared to ST (Figure 7). The SMD between SP and ST was 0.47 (95% CI: 0.03, 0.91), and the SMD between LTO and ST was 0.39 (95% CI: 0.08, 0.71).
Figure 7.
Forest plot representing the network meta-analysis comparison of internal rotation strength between – (LTO), subscapularis peel (SP), and subscapularis tenotomy (ST). SMD: standardized mean difference; CI: confidence interval.
Non-comparative outcome: LTO union, subscapularis tendon integrity, and complications
No meta-analytic comparisons were made for the LTO union rates or subscapularis tendon healing rates. The weighted overall average was pooled from both comparative and non-comparative to provide comprehensive rates. Union rates of LTO were reported in 15 studies.6,8,24,26,28,29,32,34,36,38–41,44,45 Union of the LTO was assessed in all studies by plain shoulder radiographs, except in three studies by Gerber et al., 45 Levine et al. 36 and Lapner et al. 21 where the union was assessed by computed tomography. The overall weighted average for LTO complete union was 93.6% (884 unions out of 988 LTOs). Subscapularis integrity was reported in seven studies22,23,25,29,30,32,36 for ST, and in three studies for SP.8,25,42 Integrity of the subscapularis tendon was assessed by ultrasonography except in one study by Lapner et al. 21 in 2013 where computed tomography was used to assess integrity following SP. The overall weighted average for subscapularis tendon healing was 79.4% (151 healed tendons out of 190) for ST, and 87% (131 healed tendon out of 150) for SP. A summary of all complications encountered in the included studies is provided in Appendix Table 2.
Discussion
This meta-analysis shows that although there was no difference in ASES scores, both LTO and SP had significantly higher WOOS scores showing improved quality of life as reported by patients. It also identified a greater internal rotation strength for LTO and SP compared to ST. While patients undergoing LTO had less post-operative external rotation when compared with SP, there was no statistically significant difference between LTO and ST. Additionally, we found that LTO is associated with the greatest union/healing rate compared to both SP and ST. Overall, the results of this meta-analysis suggest that LTO and SP may provide superior clinical outcomes when compared with ST.
Subscapularis dysfunction following shoulder arthroplasty has been shown to lead to poor clinical outcomes, including, but not limited to instability, weakness, pain, and decreased motion.46–48 Despite overall satisfactory outcomes following TSA, rates of subscapularis dysfunction have been reported to be as high as 67%. 36 Therefore, identifying the optimal surgical technique that preserves function is critical in optimizing postoperative function. To date, there remains considerable controversy regarding subscapularis management during TSA. 15
In the early 2000s, there was renewed interest in subscapularis management after studies highlighted subscapularis dysfunction following ST. 35 These studies contributed to a shift in surgical practice to maintain subscapularis function during the surgical approach, popularizing LTO and SP approaches, techniques that would potentially allow for improved healing. Our pooled analysis found that the overall weighted average for LTO complete union was 93.6% compared to subscapularis healing rates of 87% and 79% for SP and ST, respectively. Despite a focus on healing rates, it is important to note that studies have reported mixed findings on the significance of healing. For example, while some studies have shown that subscapularis tendon healing is important for functional outcomes, 32 others have noted that subscapularis integrity may have limited clinical significance.30,31 However, as this meta-analysis demonstrates, there is a clear correlation between increased functional scores and LTO and SP, techniques associated with higher union/healing rates compared to ST.
There is heterogeneity in how subscapularis integrity is assessed. For example, while the belly-press test was originally a validated method of assessing subscapularis muscle healing, ultrasound has recently shown that this physical exam maneuver has poor positive predictive value for detecting rupture. 35 However, ultrasound is operator dependent and may miss small tears of the subscapularis tendon. 15 In our analysis, LTO union was assessed by radiographs or CT, and integrity of the subscapularis tendon was assessed with ultrasound or CT. While CT can show bone-to-bone healing, its ability to assess for subscapularis muscle/tendon healing may be significantly less sensitive. 15 Radiographs have also been shown to have limitations in their ability to assess union. Previous studies have noted up to a 17% incidence of inability to visualize the osteotomy site. Because there is significant variability in assessing subscapularis integrity with limitations of each method, further study is needed to accurately gauge subscapularis healing following shoulder arthroplasty.
Two clinical outcome scores were analyzed in this study as a proxy to assess subscapularis function, ASES and WOOS. While there were no significant differences in ASES scores between all three approaches in subscapularis management, there was a significantly greater WOOS index in both the LTO and SP groups when compared with ST. The WOOS index measures function and quality of life, as reported by patients with glenohumeral osteoarthritis, and WOOS has been shown to be reliable and valid in this population. 13 Previous studies have found the specificity of WOOS to allow for improved ability to detect smaller clinical differences before and after treatment when compared with more generic outcome measures. 49 While we did find a statically significant difference in WOOS indices, it is important to note that the minimum clinically important difference has not been determined for the WOOS. 15 It is plausible that this difference might be clinically relevant given that LTO and SP improved WOOS scores by 8.4 and 6.8 points compared to ST, respectively.
In terms of motion and strength, this meta-analysis showed some advantages of LTO and SP over ST. First, when assessing internal rotation strength, we found that both LTO and SP had improved strength when compared to ST, however, it is important to note that potential confounders for internal rotation strength were unable to be controlled for in this analysis. In terms of motion, our meta-analysis showed that SP had superior external rotation compared to LTO while no difference was observed between SP and ST or between ST and LTO. These findings are corroborated by other reviews suggesting that LTO and SP may confer similar outcomes that are superior to ST; 50 however, there is a limited number of high-quality studies to validate whether one technique is clearly advantageous over another for the preservation of motion and strength. 51 For example, among the six studies that were grouped to analyze external rotation, only one was a randomized control trial while the rest were retrospective cohort trials.
Strengths and limitations
In comparison to prior meta-analyses, this study provided the largest number of studies on subscapularis management in aTSA thus far. A total of 23 studies were included with 10 being comparative and 13 non-comparatives. The latest meta-analysis has not found a statistical difference in ROM between all three subscapularis techniques, and no functional scores were compared due to sample size limitations. 15 The inclusion of 3 additional comparative studies in our network meta-analysis increased the sample size and permitted the comparison of ASES and WOOS scores. Second, our network meta-analytic comparison resulted in statistically significant improvement in WOOS scores and ER ROM for LTO and SP compared to ST. Thus, the main strengths of our network meta-analysis were performing a meta-analytic comparison for functional outcomes and having different results compared to prior meta-analyses. In addition, the inclusion of non-comparative studies allowed the calculation of weighted averages for subscapularis healing and LTO union rates. In turn, this would provide shoulder surgeons with a comprehensive summary of the literature on this topic.
There are limitations to this study. As with all meta-analyses, methodologic heterogeneity between studies can be a potential source of error. There were multiple methods of repairing the subscapularis within each group in our study; for example: different techniques include side-to-side suturing, transosseous suturing, suture incorporation to the humeral stem, and augmentation with a plate or button. 15 Grouping all repairs into three groups may be prone to additional error. Further, additional nuances could not be accounted for, such as LTO size which could potentially affect union rates. Another possible cofounder is the inclusion of some studies analyzing hemiarthroplasty, which has been shown to have less improvement in pain when compared with TSA.52,53 However, these potential limitations are counteracted by the greater statistical rigor as well as external generalizability to the greater population of meta-analyses.
In conclusion, this network meta-analysis demonstrated that LTO and SP may lead to significantly improved shoulder function and quality of life when compared to ST. Moreover, LTO and SP were associated with the high union and subscapularis healing rates compared to ST. These results suggest that LTO and SP demonstrate a trend of superior outcomes compared to ST during aTSA. It is important to highlight that most of the current evidence on subscapularis management in aTSA is low and is derived from level III and IV studies. Therefore, further multicenter randomized studies are warranted to ascertain which subscapularis management technique leads to superior outcomes. This can be performed by focusing on several validated shoulder outcome measures and advanced imaging for investigating subscapularis healing.
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Level of evidence: Therapeutic, Level IV.
ORCID iDs: Abdulaziz F Ahmed https://orcid.org/0000-0002-1902-3291
Jacob Mikula https://orcid.org/0000-0002-5042-8457
Andrew S Miller https://orcid.org/0000-0002-8828-1876
Uma Srikumaran https://orcid.org/0000-0002-2314-8855
References
- 1.Liu EY, Kord D, Horner NS, et al. Stemless anatomic total shoulder arthroplasty: a systematic review and meta-analysis. J Shoulder Elbow Surg 2020; 29: 1928–1937. [DOI] [PubMed] [Google Scholar]
- 2.Simovitch RW, Friedman RJ, Cheung EV, et al. Rate of improvement in clinical outcomes with anatomic and reverse total shoulder arthroplasty. J Bone Joint Surg Am 2017; 99: 1801–1811. [DOI] [PubMed] [Google Scholar]
- 3.Best MJ, Aziz KT, Wilckens JH, et al. Increasing incidence of primary reverse and anatomic total shoulder arthroplasty in the United States. J Shoulder Elbow Surg 2021; 30: 1159–1166. [DOI] [PubMed] [Google Scholar]
- 4.Neer CS, 2nd, Watson KC, Stanton FJ. Recent experience in total shoulder replacement. J Bone Joint Surg Am 1982; 64: 319–337. [PubMed] [Google Scholar]
- 5.Gerber C, Yian EH, Pfirrmann CA, et al. Subscapularis muscle function and structure after total shoulder replacement with lesser tuberosity osteotomy and repair. J Bone Joint Surg Am 2005; 87: 1739–1745. [DOI] [PubMed] [Google Scholar]
- 6.Krishnan SG, Stewart DG, Reineck JR, et al. Subscapularis repair after shoulder arthroplasty: biomechanical and clinical validation of a novel technique. J Shoulder Elbow Surg 2009; 18: 184–192. Discussion 197–198. [DOI] [PubMed] [Google Scholar]
- 7.Ponce BA, Ahluwalia RS, Mazzocca AD, et al. Biomechanical and clinical evaluation of a novel lesser tuberosity repair technique in total shoulder arthroplasty. J Bone Joint Surg Am 2005; 87: 1–8. [DOI] [PubMed] [Google Scholar]
- 8.Lapner PL, Sabri E, Rakhra K, et al. Comparison of lesser tuberosity osteotomy to subscapularis peel in shoulder arthroplasty: a randomized controlled trial. J Bone Joint Surg Am 2012; 94: 2239–2246. [DOI] [PubMed] [Google Scholar]
- 9.Clyde CT, Throckmorton TW, Duquin TR. Subscapularis peel in anatomic total shoulder arthroplasty. J Shoulder Elbow Arthroplasty 2018; 2: 247154921881340. Review. DOI: 10.1177/2471549218813409. [Google Scholar]
- 10.Heckman DS, Hoover SA, Weinhold PS, et al. Repair of lesser tuberosity osteotomy for shoulder arthroplasty: biomechanical evaluation of the Backpack and Dual Row techniques. J Shoulder Elbow Surg 2011; 20: 491–496. [DOI] [PubMed] [Google Scholar]
- 11.Angst F, Schwyzer HK, Aeschlimann A, et al. Measures of adult shoulder function: disabilities of the Arm, Shoulder, and Hand Questionnaire (DASH) and its short version (QuickDASH), Shoulder Pain and Disability index (SPADI), American Shoulder and Elbow Surgeons (ASES) Society standardized shoulder assessment form, Constant (Murley) Score (CS), Simple Shoulder Test (SST), oxford Shoulder Score (OSS), Shoulder Disability Questionnaire (SDQ), and Western Ontario Shoulder Instability Index (WOSI). Arthritis Care Res (Hoboken) 2011; 63: S174–S188. [DOI] [PubMed] [Google Scholar]
- 12.Unger RZ, Burnham JM, Gammon L, et al. The responsiveness of patient-reported outcome tools in shoulder surgery is dependent on the underlying pathological condition. Am J Sports Med 2019; 47: 241–247. [DOI] [PubMed] [Google Scholar]
- 13.Lo IK, Griffin S, Kirkley A. The development of a disease-specific quality of life measurement tool for osteoarthritis of the shoulder: the Western Ontario Osteoarthritis of the Shoulder (WOOS) index. Osteoarthr Cartil 2001; 9: 771–778. [DOI] [PubMed] [Google Scholar]
- 14.Izquierdo R, Voloshin I, Edwards S, et al. American Academy of orthopaedic surgeons clinical practice guideline on the treatment of glenohumeral joint osteoarthritis. J Bone Joint Surg Am 2011; 93: 203–205. [DOI] [PubMed] [Google Scholar]
- 15.Choate WS, Kwapisz A, Momaya AM, et al. Outcomes for subscapularis management techniques in shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg 2018; 27: 363–370. [DOI] [PubMed] [Google Scholar]
- 16.Del Core MA, Cutler HS, Ahn J, et al. Systematic review and network meta-analysis of subscapularis management techniques in anatomic total shoulder arthroplasty. J Shoulder Elbow Surg 2021; 30: 1714–1724. [DOI] [PubMed] [Google Scholar]
- 17.Shields E, Ho A, Wiater JM. Management of the subscapularis tendon during total shoulder arthroplasty. J Shoulder Elbow Surg 2017; 26: 723–731. [DOI] [PubMed] [Google Scholar]
- 18.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009; 62: 1006–1012. [DOI] [PubMed] [Google Scholar]
- 19.Page MJ, McKenzie JE, Higgins JPT. Tools for assessing risk of reporting biases in studies and syntheses of studies: a systematic review. BMJ Open 2018; 8: e019703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg 2003; 73: 712–716. [DOI] [PubMed] [Google Scholar]
- 21.Lapner PL, Sabri E, Rakhra K, et al. Healing rates and subscapularis fatty infiltration after lesser tuberosity osteotomy versus subscapularis peel for exposure during shoulder arthroplasty. J Shoulder Elbow Surg 2013; 22: 396–402. [DOI] [PubMed] [Google Scholar]
- 22.Armstrong A, Lashgari C, Teefey S, et al. Ultrasound evaluation and clinical correlation of subscapularis repair after total shoulder arthroplasty. J Shoulder Elbow Surg 2006; 15: 541–548. [DOI] [PubMed] [Google Scholar]
- 23.Armstrong AD, Southam JD, Horne AH, et al. Subscapularis function after total shoulder arthroplasty: electromyography, ultrasound, and clinical correlation. J Shoulder Elbow Surg 2016; 25: 1674–1680. [DOI] [PubMed] [Google Scholar]
- 24.O’Brien PM, Kazanjian JE, Kelly JD, II, et al. Subscapularis function after total shoulder arthroplasty using lesser tuberosity osteotomy or tenotomy. JAAOS Global Research & Reviews 2020; 4: e20.00032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lapner P, Pollock JW, Zhang T, et al. A randomized controlled trial comparing subscapularis tenotomy with peel in anatomic shoulder arthroplasty. J Shoulder Elbow Surg 2019; 29: 225–234. [DOI] [PubMed] [Google Scholar]
- 26.Aibinder WR, Bicknell RT, Bartsch S, et al. Subscapularis management in stemless total shoulder arthroplasty: tenotomy versus peel versus lesser tuberosity osteotomy. J Shoulder Elbow Surg 2019; 28: 1942–1947. [DOI] [PubMed] [Google Scholar]
- 27.Baumgarten KM, Osborn R, Schweinle WE, Jr, et al. The influence of anatomic total shoulder arthroplasty using a subscapularis tenotomy on shoulder strength. J Shoulder Elbow Surg 2018; 27: 82–89. [DOI] [PubMed] [Google Scholar]
- 28.Jandhyala S, Unnithan A, Hughes S, et al. Subscapularis tenotomy versus lesser tuberosity osteotomy during total shoulder replacement: a comparison of patient outcomes. J Shoulder Elbow Surg 2011; 20: 1102–1107. [DOI] [PubMed] [Google Scholar]
- 29.Scalise JJ, Ciccone J, Iannotti JP. Clinical, radiographic, and ultrasonographic comparison of subscapularis tenotomy and lesser tuberosity osteotomy for total shoulder arthroplasty. J Bone Joint Surg Am 2010; 92: 1627–1634. [DOI] [PubMed] [Google Scholar]
- 30.Jackson JD, Cil A, Smith J, et al. Integrity and function of the subscapularis after total shoulder arthroplasty. J Shoulder Elbow Surg 2010; 19: 1085–1090. [DOI] [PubMed] [Google Scholar]
- 31.Liem D, Kleeschulte K, Dedy N, et al. Subscapularis function after transosseous repair in shoulder arthroplasty: transosseous subscapularis repair in shoulder arthroplasty. J Shoulder Elbow Surg 2012; 21: 1322–1327. [DOI] [PubMed] [Google Scholar]
- 32.Buckley T, Miller R, Nicandri G, et al. Analysis of subscapularis integrity and function after lesser tuberosity osteotomy versus subscapularis tenotomy in total shoulder arthroplasty using ultrasound and validated clinical outcome measures. J Shoulder Elbow Surg 2014; 23: 1309–1317. [DOI] [PubMed] [Google Scholar]
- 33.Caplan JL, Whitfield B, Neviaser RJ. Subscapularis function after primary tendon to tendon repair in patients after replacement arthroplasty of the shoulder. J Shoulder Elbow Surg 2009; 18: 193–196. Discussion 197–198. [DOI] [PubMed] [Google Scholar]
- 34.Qureshi S, Hsiao A, Klug RA, et al. Subscapularis function after total shoulder replacement: results with lesser tuberosity osteotomy. J Shoulder Elbow Surg 2008; 17: 68–72. [DOI] [PubMed] [Google Scholar]
- 35.Miller SL, Hazrati Y, Klepps S, et al. Loss of subscapularis function after total shoulder replacement: a seldom recognized problem. J Shoulder Elbow Surg 2003; 12: 29–34. [DOI] [PubMed] [Google Scholar]
- 36.Levine WN, Munoz J, Hsu S, et al. Subscapularis tenotomy versus lesser tuberosity osteotomy during total shoulder arthroplasty for primary osteoarthritis: a prospective, randomized controlled trial. J Shoulder Elbow Surg 2019; 28: 407–414. [DOI] [PubMed] [Google Scholar]
- 37.Andrews JR, Baumgarten TE. Arthroscopic anatomy of the elbow. Orthop Clin North Am 1995; 26: 671–677. [PubMed] [Google Scholar]
- 38.Small KM, Siegel EJ, Miller LR, et al. Imaging characteristics of lesser tuberosity osteotomy after total shoulder replacement: a study of 220 patients. J Shoulder Elbow Surg 2014; 23: 1318–1326. [DOI] [PubMed] [Google Scholar]
- 39.De Wilde LF, De Coninck T, De Neve F, et al. Subscapularis release in shoulder replacement determines structural muscular changes. Clin Orthop Relat Res 2012; 470: 2193–2201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Johnson NR, Trofa DP, Saltzman BM, et al. Healing rate and clinical outcomes of lesser tuberosity osteotomy for anatomic shoulder arthroplasty. JAAOS Global Res Rev 2020; 4: e19.00119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Levy JC, DeVito P, Berglund D, et al. Lesser tuberosity osteotomy in total shoulder arthroplasty: impact of radiographic healing on outcomes. J Shoulder Elbow Surg 2019; 28: 1082–1090. [DOI] [PubMed] [Google Scholar]
- 42.Gobezie R, Denard PJ, Shishani Y, et al. Healing and functional outcome of a subscapularis peel repair with a stem-based repair after total shoulder arthroplasty. J Shoulder Elbow Surg 2017; 26: 1603–1608. [DOI] [PubMed] [Google Scholar]
- 43.Mason R, Buckley T, Southgate R, et al. Radiographic study of humeral stem in shoulder arthroplasty after lesser tuberosity osteotomy or subscapularis tenotomy. Am J Orthop (Belle Mead NJ) 2018; 47. DOI: 10.12788/ajo.2018.0036. [DOI] [PubMed] [Google Scholar]
- 44.Shafritz AB, Fitzgerald MG, Beynnon BD, et al. Lift-off test results after lesser tuberosity osteotomy versus subscapularis peel in primary total shoulder arthroplasty. J Am Acad Orthop Surg 2017; 25: 304–313. [DOI] [PubMed] [Google Scholar]
- 45.Gerber C, Pennington SD, Yian EH, et al. Lesser tuberosity osteotomy for total shoulder arthroplasty. Surgical technique. J Bone Joint Surg Am 2006; 88: 170–177. [DOI] [PubMed] [Google Scholar]
- 46.Ives EP, Nazarian LN, Parker L, et al. Subscapularis tendon tears: a common sonographic finding in symptomatic postarthroplasty shoulders. J Clin Ultrasound 2013; 41: 129–133. [DOI] [PubMed] [Google Scholar]
- 47.Scheibel M, Tsynman A, Magosch P, et al. Postoperative subscapularis muscle insufficiency after primary and revision open shoulder stabilization. Am J Sports Med 2006; 34: 1586–1593. [DOI] [PubMed] [Google Scholar]
- 48.Miller BS, Joseph TA, Noonan TJ, et al. Rupture of the subscapularis tendon after shoulder arthroplasty: diagnosis, treatment, and outcome. J Shoulder Elbow Surg 2005; 14: 492–496. [DOI] [PubMed] [Google Scholar]
- 49.Moeini S, Rasmussen JV, Klausen TW, et al. Rasch analysis of the Western Ontario Osteoarthritis of the Shoulder index – the Danish version. Patient Relat Outcome Meas 2016; 7: 173–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bornes TD, Rollins MD, Lapner PLC, et al. Subscapularis management in total shoulder arthroplasty: current evidence comparing peel, osteotomy, and tenotomy. J Shoulder Elbow Arthroplasty 2018; 2: 247154921880777. Review. [Google Scholar]
- 51.Dunn R, Joyce CD, Bravman JT. Comparison of subscapularis management and repair techniques. J Shoulder Elbow Arthroplasty 2019; 3: 247154921984815. Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bryant D, Litchfield R, Sandow M, et al. A comparison of pain, strength, range of motion, and functional outcomes after hemiarthroplasty and total shoulder arthroplasty in patients with osteoarthritis of the shoulder. A systematic review and meta-analysis. J Bone Joint Surg Am 2005; 87: 1947–1956. [DOI] [PubMed] [Google Scholar]
- 53.Edwards TB, Kadakia NR, Boulahia A, et al. A comparison of hemiarthroplasty and total shoulder arthroplasty in the treatment of primary glenohumeral osteoarthritis: results of a multicenter study. J Shoulder Elbow Surg 2003; 12: 207–213. [DOI] [PubMed] [Google Scholar]