Abstract
Background
Low self-efficacy (SE) can impact decreasing health status, poor self-care, and quality of life among patients with Coronary Heart Disease (CHD). Many factors can affect SE. However, studies on SE in CHD patients with Rasch Model analysis have not been carried out widely.
Purpose
This study aims to identify the SE in self-care and its related factors that correlate SE among CHD patients.
Patients and Methods
Cross-sectional study was conducted on 104 adult patients (≥18 years) diagnosed with CHD. Selection of the sample using convenience sampling technique with several predetermined criteria. SE was measured using the SEQ-CHDM questionnaire, with high validity and reliability results. Data were analyzed using the Rasch model and chi-square test.
Results
The results showed that most respondents had a moderate SE (51.5%). Care units (p=0.003) and duration of illness (p=0.049) were significantly correlated to SE among patients with CHD. “Maintaining an ideal body weight” is the most challenging thing. On the other hand, stop smoking is the most confident thing to be performed by the respondents.
Conclusion
We conclude that CHD patients in the acute care unit and patients with a duration of illness >6 months have a lower tendency for SE. Health interventions such as raising awareness about the disease, modifying health behavior, and immediately screening can improve patients’ SE. Besides that, proper diagnosis and ongoing treatment are crucial to improving SE and CHD care outcomes.
Keywords: coronary heart disease, self-care, self-efficacy
Introduction
Coronary heart disease (CHD) is the leading cause of death and the most serious health problem globally. Over the past few decades, the CHD mortality rate increased 42.4% from 1990 to 2015.1 On the other hand, CHD caused more than 17 million deaths in 2017 and is expected to increase by 23 million deaths in 2030 worldwide.2 According to the World Health Organization (WHO), more than three-quarters of deaths from CHD occur in low- and middle-income countries.3
The increase in mortality and morbidity in CHD patients aligns with the low level of self-care and participation in cardiac rehabilitation (CR).4,5 Previous reviews said that participation in CR significantly reduces all-cause death from heart disease by 20%-36%.6 Also, the level of self-care and participation in CR will significantly affect the quality of life (QoL) and the prognosis of patients with CHD.7,8 Studies in Indonesia show that many CHD patients still have poor QoL.9,10 Additionally, a study in China also showed the same results, that CHD patients had poor QoL during the Covid-19 pandemic.11 The main factor of poor QoL is the low self-efficacy (SE).5
SE has an important role in the prognosis of patients with CHD. Cardiac SE is essential in managing and controlling health behaviours and adopting healthy lifestyles associated with cardiovascular disease.5,12,13 Previous studies revealed that a low level of SE is closely related to poor self-care, especially in exercise. In contrast, self-care’s ability to carry out health behaviours increases when SE increases among patients with heart disease.5,14 SE is also associated with psychological well-being, improved quality of life, and better rehabilitation adherence.15,16
The importance of SE in determining outcomes in CHD patients encourages the need for continuous SE studies in patients. This can anticipate problems, such as failure to perform self-care. When the Covid-19 pandemic took place, changes in health services, especially for those with chronic illnesses such as heart disease, experienced many changes due to social restrictions, which might impact SE in self-care. Research related to SE in self-care in patients with CHD, to the best of our knowledge, identified before the pandemic occurred,17,18 so that this research can add information related to SE in patients with CHD shortly after the pandemic subsides and social restrictions are lifted.
Many factors can affect SE in patients with CHD. Previous studies reported that knowledge and awareness of the disease are the dominant factors that can affect SE.19 In addition, other factors such as gender, living alone at home, work can also affect the level of SE in patients with CHD.13 Other factors related to demographic background and other medical characteristics have yet to be identified in the research, so other studies are needed to add information regarding these factors, as it is clear that SE, self-care behaviours, and modifiable risk factors play an essential role in improving QoL in CHD patients.20
Several previous studies related to SE in CHD patients both conducted in Indonesia and outside Indonesia identified more levels and predictors of SE.10,13,17,20–25 However, methodologically, there are no studies that analyze SE with the Rasch model approach in a population of patients with CHD. The Rasch model is a statistical method that has advantages in identifying SE, attitudes, perceptions, and other variables.26–28 The advantages of this model include being able to provide linear scales with the same intervals, being able to predict missing data, providing more precise estimates, being able to detect model inaccuracies, and producing measurements that can be replicated or in other words being able to meet valid data measurement requirements.29 In addition, one of the features of Rasch modelling is to produce a wright map that describes the distribution of respondents’ abilities/beliefs and the distribution of problem difficulty levels with the same scale.30,31 Therefore, SE is also evaluated with the wright map to analyse the study’s results comprehensively.
To our knowledge, to date research has identified SE using the Rasch model only in the morbidly obese32 and spinal cord injury populations.33 In addition, the use of the Rasch model in Indonesia is more widely used in the student population.26,27,34–36 Therefore, this study was conducted to investigate SE and factors related to respondents demographic and medical characteristics related to SE in CHD patients using the Rasch model approach. The results of this study are expected to be useful for further research and nursing care for monitoring and evaluation of SE, especially in CHD patients in Indonesia, as part of improving self-care and quality of life for patients.
Methods
Study Design
This study used a cross-sectional design among patients with CHD. The data collection conducted from August to October 2022. This study uses the Rasch model to transform the data and identify the validity and reliability of the instrument and the response of the respondents.
Sample and Setting
The population is CHD patients undergoing treatment at West Java, Indonesia, in a referral hospital. The selection of samples used a convenience sampling technique, and the inclusion criteria were (1) respondents aged at least 18 years, (2) diagnosed with CHD (chronic coronary disease or acute coronary disease), (3) relatively stable condition characterized by being free or having minimal chest pain identified using a numeric rating scale (NRS). In contrast, the exclusion criteria included (1) not understanding Indonesian and (2) having a history of psychological or mental disorders.
The number of samples was determined using the size table for one correlation test.37 It is stated that the smallest minimum sample size is 59 (R0=0.8 and R1=0.9) for 80% statistical power, with an alpha of 0.05, and the largest minimum sample size is between 751. Furthermore, the number of respondents included in this study was 103 patients with CHD.
Research Instrument
The demographic characteristics questionnaire includes age, gender, educational background, care unit, duration of illness, and treatment. Self-Efficacy Questionnaire for Coronary Heart Disease Management (SEQ-CHDM) is an instrument for measuring self-efficacy in self-care among patients with CHD, which was developed based on the study of the learning needs of CHD patients.38 It consists of 26 statements on a Likert scale (ordinal) that measures ten indicators of self-care in CHD patients, including recognizing signs and symptoms of a heart attack; being able to cope with a heart attack; being able to perform safe activities; being able to perform the sexual activity safely; able to choose the right diet; able to set the right diet; able to quit smoking; able to recognize, avoid stress and cope with stress; able to use spiritual beliefs for mental health; and able to comply in taking medication for CHD.
Validity and Reliability of Instruments
The instruments in this study have been tested for validity and reliability in previous studies.38 The results obtained for the validity of the value of r ranged between 0.081 and 0.817 (r table = 0.081), and the results of the reliability test using Cronbach’s alpha was 0.893. This shows that the instrument valid and reliable to use.38 Using a different method, namely the Rasch model, determines instrument validity by unidimensionality. Unidimensionality provides information that the instrument measures what should be measured. It is determined by principal component analysis (PCA) from the residual that measures the extent of the diversity of the instrument (Raw variance).30,31
In this study, the value of the Raw variance explained by measures shows a value of 27%, where the acceptable value is >20%. In addition, Raw variance explained by persons and items offers a value of < 15%, where this value is an acceptable unidimensionality (see Table 1).39 This measure indicates that the instrument can properly measure SE among CHD patients.
Table 1.
Psychometric Attribute of the Instrument (n=103)
| Psychometric Attribute | SEQ-CHDM |
|---|---|
| No of item | 26 |
| Raw explain variance by measure | 27.2% |
| Unexplained variance | <15% |
| Cronbach’s alpha | 0.77 |
| Person reliability | 0.73 |
| Person separation | 1.66 |
| Item reliability | 0.95 |
| Item separation | 4.27 |
| Mean Person | 76.9 |
| Mean Item | 304.7 |
Based on reliability measurement (see Table 1), it shows that the results of the reliability test measurement obtained a Cronbach alpha value of 0.77; this implies that the interaction between the person and the items in the instrument is good. The value of person and item reliability was 0.73 and 0.95, respectively. The instrument quality based on item reliability value (0.95) is in an excellent category. From these results, it can be concluded that the consistency of the answers from the respondents was categorized as good, accompanied by excellent instrument quality. Then, the results of the person and item separation values were 1.66 and 4.27, respectively. This separation value functions for grouping persons and items. This means that the person separation value in the table is 1.66. From the calculations, the result grouping is 2.54 (H=[(4 x separation value)+1)/3]), which means that the data can be divided into two result groups. As for the item separation value, it is 4.27, and if it is entered into the formula (H=[(4 x separation value)+1)/3], the grouping result is 6.02; this means that the items can be grouped into six result groups.
The researcher detects the bias of the measurement results by examining the consistency of the respondents’ answers. This consistency is measured to determine whether certain respondent characteristics influence individual bias, thereby reducing data quality. This measurement is carried out through a differential item functioning test (DIF test).29 The DIFF test results, identified as having no bias, are if the item probability value is less than 5% (0.05).29 The results of the DIF test in this study indicated that there was no individual bias in the measurement results based on p>0.05 for the categories of gender, age, duration of illness, and care unit where the respondents were treated. The results of the DIF test show that the respondents’ answers from the four categories show consistency of answers between items that make sense or do not oppose with each other.
Data Analysis
The data obtained in the form of ordinal data is transformed first into numerical data using the Rasch model (winstep application) before being analyzed further. Numerical data in the form of a Log Odds Unit (logit) score is then used to categorize SE into three categories, including low SE, moderate SE, and high SE, based on the mean logit score cut-off and standard deviation (category: > mean logit score = high SE; < mean logit score – logit 0.0 = moderate SE, and < logit score −0.01 = low SE). In addition, an analysis was also carried out using the Wright map to detect and find items correctly according to the level of difficulty and ability level of the respondent.40,41
To identify the frequency distribution and the relationship between the characteristics of the respondents and the SE category, we analyzed a contingency table and a chi-square test with a significance level of p<0.05. Furthermore, the normality of SE data was identified using the Kolmogorov Smirnov obtained p>0.05, which usually indicates normally distributed data. Apart from using the Winsteps application version 5.4.0.0, data analysis was also carried out using the Jamovi version 2.3.21.
Ethical Consideration
This study has received ethical approval from the Research Ethics Committee of Universitas Padjadjaran (656/UN6.KEP/EC/2022) in compliance with the Declaration of Helsinki. Patients who have the potential to become respondents are given information about the research both verbally and in writing. Furthermore, patients willing to participate in the study signed evidence of consent to become respondents. In addition, researchers assumed that the respondents’ participation was voluntary and that they had the right to leave the process without any consequences. The data from each respondent was analyzed in groups so the participants would not be identified and used for academic purposes only. All information was maintained confidentially. In addition, there were no risks associated with filling out the questionnaire for respondents because we had determined the inclusion and exclusion criteria for respondents, where only patients who were hemodynamically stable and free from chest pain can be taken as respondents.
Results
Characteristic of Study
Based on Table 2 shows that most of the respondents were male (73.8%) and aged > 56 years old (59.2). Most respondents have a senior high school educational background (42.7%). Then, most of the respondents were in the inpatient unit (50.5%) with the duration of illness > 6 months (58.3%) and only received treatment (51.5%).
Table 2.
Characteristics of Respondents (n=103)
| Variable | Frequency (f) | Percentage (%) |
|---|---|---|
| Gender | ||
| Female | 27 | 26.2 |
| Male | 76 | 73.8 |
| Age | ||
| 26–35 years old | 5 | 4.9 |
| 36–45 years old | 11 | 10.7 |
| 46–55 years old | 26 | 25.2 |
| > 56 years old | 61 | 59.2 |
| Educational Background | ||
| Elementary School | 18 | 17.5 |
| Junior High School | 14 | 13.6 |
| Senior High School | 44 | 42.7 |
| Higher Education | 27 | 26.2 |
| Care unit | ||
| Inpatient | 52 | 50.5 |
| Outpatient | 51 | 49.5 |
| Duration ill | ||
| ≤ 6 months | 43 | 41.7 |
| > 6 months | 60 | 58.3 |
| Treatment | ||
| Revascularization and Medications | 50 | 48.5 |
| Medications Only | 53 | 51.5 |
Self-Efficacy Among Coronary Heart Diseases Patients
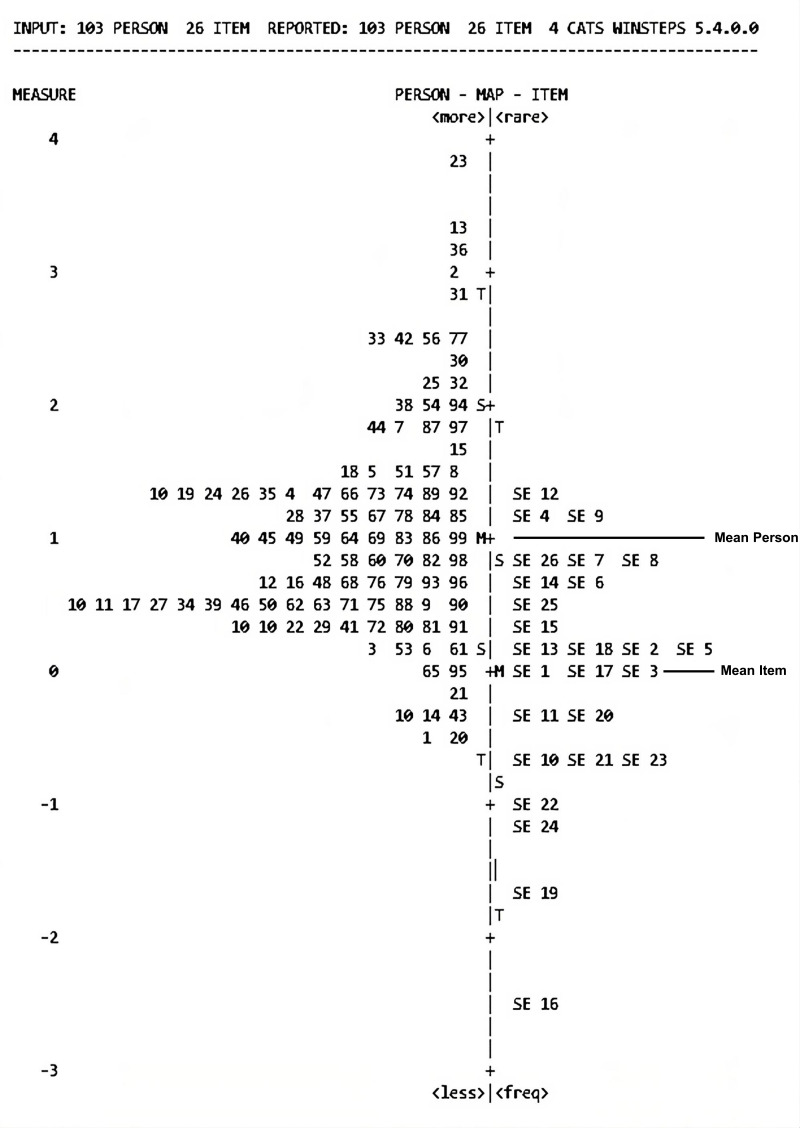
Based on Table 3 shows that most of the respondents have a moderate level of SE (51.5%). However, as many as 5.8% of respondents still have low SE. In addition, based on the results of the distribution of the Wright map (see Figure 1), it shows that there are 44 respondents with abilities or SE above the average (>1.07 logit score). In addition, based on data on the distribution of respondents (left side of the Wright map) and distribution of items (right side of the Wright map), it is identified that respondents tend to have a good SE because the distribution of respondents is more above the distribution of items which are usually considered challenging to agree on. From the Wright map, it was also identified that the statement that is the most difficult for respondents to believe they can do is item number 12 (maintaining an ideal body weight), followed by statement 4 (can drive safely after having a heart attack) and 9 (can handle it if I experience signs and symptoms of a heart attack after engaging in sexual activity). The statement that they feel most capable of doing is item no 16 (stop smoking). For more detail, see Supplementary File 1, which illustrates the self-efficacy based on questionnaire items.
Table 3.
Level of Self-Efficacy (n=103)
| SE Category | SE Logit | SE Scores | Frequency (f) | Percentage (%) |
|---|---|---|---|---|
| Low | <0.00 | ≤66 | 6 | 5.8 |
| Moderate | ≤1.07–0.00 | ≤75–67 | 53 | 51.5 |
| High | >1.07 | >75 | 44 | 42.7 |
| Total | 103 | 100 |
Abbreviation: SE, Self-efficacy.
Figure 1.
Wright Map of Self-efficacy.
Notes: The “Measure” section on the leftmost Wright map shows the logit score. The “person” section on the left of the Wright map describes the serial number of respondents based on SE ability level. While, the “Item” section on the right of the Wright map describes the questionnaire number from the most confident or unconfident thing to be done by respondents. In addition, M is mean for item and person; S means one standard deviation away from mean value; and T means two standard deviation away from mean value.
Abbreviation: SE, Self-efficacy.
Relationship Between Characteristics of Respondent on Self-Efficacy
Based on the results of the Chi-square test (see Table 4) shows that the care unit (p=0.003) and duration of ill (0.049) have a significant relationship with SE in patients with CHD.
Table 4.
Relationship Between Characteristics of Respondent on Self-Efficacy (n=103)
| Variable | Self-Efficacy | n (%) | χ2 | p-value | |||||
|---|---|---|---|---|---|---|---|---|---|
| Low | Moderate | High | |||||||
| n | % | n | % | n | % | ||||
| Gender | |||||||||
| Female | 2 | 1.9 | 17 | 16.5 | 8 | 7.8 | 27 (26.2) | 2.57 | 0.277 |
| Male | 4 | 3.8 | 36 | 35 | 36 | 35 | 76 (73.8) | ||
| Age | |||||||||
| 26–35 years old | 1 | 1 | 3 | 2.9 | 1 | 1 | 5 (4.9) | 6.26 | 0.395 |
| 36–45 years old | 0 | 0 | 5 | 4.9 | 6 | 5.8 | 11 (10.7) | ||
| 46–55 years old | 1 | 1 | 17 | 16.5 | 8 | 7.8 | 26 (25.2) | ||
| > 56 years old | 4 | 3.9 | 28 | 27.2 | 29 | 28.2 | 61 (59.2) | ||
| Educational Background | |||||||||
| Elementary School | 0 | 0 | 13 | 12.6 | 5 | 4.9 | 18 (17.5) | 7.16 | 0.306 |
| Junior High School | 1 | 1 | 9 | 8.7 | 4 | 3.9 | 14 (13.6) | ||
| Senior High School | 3 | 2.9 | 21 | 20.4 | 20 | 19.4 | 44 (42.7) | ||
| Higher Education | 2 | 1.9 | 10 | 9.7 | 15 | 14.6 | 27 (26.2) | ||
| Care Unit | |||||||||
| Inpatient | 0 | 0 | 34 | 33 | 18 | 17.5 | 52 (50.5) | 11.7 | 0.003* |
| Outpatient | 6 | 5.8 | 19 | 18.4 | 26 | 25.2 | 51 (49.5) | ||
| Duration of ill | |||||||||
| ≤ 6 months | 1 | 1 | 28 | 27.2 | 14 | 13.6 | 43 (41.7) | 6.01 | 0.049* |
| > 6 months | 5 | 4.9 | 25 | 24.3 | 30 | 29.1 | 60 (58.3) | ||
| Treatment | |||||||||
| Revascularization and Medications | 2 | 1.9 | 24 | 23.3 | 24 | 23.3 | 50 (48.5) | 1.42 | 0.493 |
| Medications only | 4 | 3.9 | 29 | 28.2 | 20 | 19.4 | 53 (51.5) | ||
Note: *Chi-square test with significant value <0.05.
Abbreviation: SE, Self-efficacy.
Discussion
In this study, we identified the level of SE and its factors related to SE among patients with CHD using the Rasch model approach. SE is an individual’s belief about their ability to organize and perform certain activities.15 This study’s results indicate that most respondents have moderate (51.5%) to high (42.7%) SE ability levels. This condition indicates that respondents believe they can manage CHD, especially concerning smoking cessation (item 16, see Figure 1).
The categorization of SE uses a Log Odds Unit (logit) score in this study so that the analysis results from SE will be more accurate and validated precisely compared to several previous studies, which only used the mean score.17,21,23,42,43 In the Rasch model, the quality of the data answers from respondents can be identified from the value of person reliability, unidimensionality, and DIF measurement. Furthermore, person reliability and Cronbach’s alpha values were at 0.73 and 0.77 (see Table 1). These results indicate that the interaction between the respondents’ answers and the question items in the instrument is in the good category. In addition, there was no individual bias related to the characteristics of the respondents in the categories of gender, age, care unit, educational background, duration of CHD diagnosis, and type of treatment. It shows that the answers or data given by the respondents on these characteristics are consistent.
Several studies conducted in Indonesia also reported similar results.10,17,24,42 Study by Wantiyah et al said most respondents had SE values above the average (71.41 ± 5.45).17 The same study also shows that most respondents (62.8%) have a high level of SE.42 This is also supported by Wistiani et al and Ni Kadek et al, the results showed that as much as 48.8% and 64% of respondents had a moderate level of SE.10,24 Patients with high SE will be able to be more cooperative and consistent in following treatment programs so that they will indirectly maintain optimal health conditions and lead to better QoL.23,44–46
SE in patients with CHD is essential for the attention of health professionals.12,47 SE is important in initiating and maintaining healthy behaviours, leading to decrease cardiac event recurrence.21 CHD patients with a high SE level will have good disease management, increased psychological well-being and QoL, and adherence in rehabilitation.15,44,48 In addition, increased SE was associated with high adherence to physical activity guidelines and a dietary diet.12,21 Conversely, if CHD patients have a low level of SE, they will have poor self-care, especially in the physical exercise aspect, which will impact their physical and psychological health status.5,14 Therefore, it is necessary to pay more attention to the factors related to SE in this population because many factors can relate to the level of SE in CHD patients.13,20,44,47,49
Several factors are associated with the level of SE in CHD patients. The findings in this study indicate that treatment units (p=0.003) and duration of illness (p=0.049) have a significant relationship with SE in CHD patients (see Table 3). In addition, the other findings indicate that respondents with SE in the good category have been diagnosed with CHD for more than six months and are undergoing outpatient care. The duration of being diagnosed with CHD can be associated with a good recovery process and the treatment carried out, especially for those undergoing reperfusion therapy or cardiac rehabilitation.50 Previous studies also stated that patients undergoing treatment at the High Care Unit (HCU) have higher level of helplessness and lower perceived benefits and acceptance than patients undergoing outpatient care.51 This condition shows that the patient’s adaptation to the disease is not yet optimal because the physical condition is still weak after experiencing an acute heart attack.51 This weak physical condition can certainly impact patients’ confidence in managing their disease. Furthermore, other studies reinforce this assumption. In this study, it is stated that helplessness is inversely related to high SE.52
Another factor related to SE among CHD patients is age. Although this study showed no significant relationship between age and SE level (p=0.395), several previous studies reported that age is a predictor of low SE in CHD patients.13,20,53 Previous studies said that increasing age is associated with a decrease in Cardiac SE.20 This could be due to the uneven age distribution of the respondents in this study, where most of the participants (59.2%) were >56 years old (see Table 1), so this would certainly affect the statistical test results. In addition, other factors that were reported to be predictors of low SE were gender (p=0.024), education and knowledge (p<0.001), living conditions (p=0.03), and occupation (p=0.001).13 Possible explanations are that education and employment can increase access to health care by providing health insurance, guaranteeing income, and increasing patient confidence.18 Therefore, many factors are predictors of SE. Hence, health workers need to develop interventions or strategies that increase awareness of cardiac health and promote healthy behaviour is very important to increase SE and overall health outcomes.20
One factor that related to SE is information or knowledge about cardiac care. Consequently, health education is the main strategy to improve SE in CHD patients.20,47 Previous studies in Indonesia reported that health education using workbooks significantly improve SE in CHD patients.38 The same thing was reported in previous studies, which ascertained that increased knowledge about self-care of heart disease patients was associated with an increase in cardiac SE.54,55
Interventions with a health digitalization approach are also reported to have good efficacy in the long-term continuity of care for CHD patients.56 Several previous studies have shown that the effective use of technology can help improve SE in CHD patients.57–59 Studies in Iran show that multimedia-based education is effective in increasing SE and self-esteem in patients with acute coronary syndromes.58 Additionally, the digital cardiac rehabilitation program also positively influences patient knowledge and cardiac SE.56 Then, the Nurse-Led Phone Follow-up Education Program is considered to improve SE and facilitate achieving goals related to risk factors in patients with cardiovascular disease for at least one year.57 Therefore, some of these strategies are expected to increase SE in CHD patients, thus increasing SE will align with increasing patient QoL.
Strengths and Limitations
The limitation of this study is the use of the cross-sectional approach, where the data analyzed came from one measurement time, thus this study could not explain SE at different times. In addition, other limitations of this study emerged from the population aspect, where data collection was performed in one hospital (single setting). Hence the generalizability aspect still needs to be improved. Then, other variables can support the results in the respondents’ unidentified characteristics, such as lifestyle data, such as smoking and body mass index (BMI). However, this study has strengths because it uses the Rasch Model, where in this model, analysis of ordinal data on SE can be measured to be more valid.
Conclusion
Based on the study’s results, most respondents had a moderate to high SE level of CHD management. The wright map results show that “Maintaining an ideal body weight” is the most challenging thing. On the other hand, stop smoking is the easiest thing to agree with the respondents. Unit of care and duration of illness are the most significant factors associated with SE in CHD patients. These results may be related to the patient’s adaptation to the disease. Therefore, health workers, including nurses, have an essential role in this issue, taking this into account in planning effective intervention strategies that nurses can implement to maintain and improve the SE of CHD management in this population.
Acknowledgments
All authors would like to thank Padjadjaran University, Bandung, West Java, Indonesia, which has facilitated the database and funded this research.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Mensah GA, Roth GA, Sampson UKA, et al. Mortality from cardiovascular diseases in sub-Saharan Africa, 1990–2013: a systematic analysis of data from the global burden of disease study 2013. Cardiovasc J Afr. 2015;26(Suppl 1):S6–10. doi: 10.5830/CVJA-2015-036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amini M, Zayeri F, Salehi M. Trend analysis of cardiovascular disease mortality, incidence, and mortality-to-incidence ratio: results from global burden of disease study 2017. BMC Public Health. 2021;21(1):1–12. doi: 10.1186/s12889-021-10429-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roth GA, Abate D, Abate KH, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392(10159):1736–1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fang J, Wang JW, Li J, Li H, Shao C. The correlates of social capital and adherence to healthy lifestyle in patients with coronary heart disease. Patient Prefer Adherence. 2017;11:1701–1707. doi: 10.2147/PPA.S140787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ahn S, Song R, Choi SW. Effects of self-care health behaviors on quality of life mediated by cardiovascular risk factors among individuals with coronary artery disease: a structural equation modeling approach. Asian Nurs Res. 2016;10(2):158–163. doi: 10.1016/j.anr.2016.03.004 [DOI] [PubMed] [Google Scholar]
- 6.Turk-Adawi KI, Grace SL. Narrative review comparing the benefits of and participation in cardiac rehabilitation in high-, middle- and low-income countries. Hear Lung Circ. 2015;24(5):510–520. doi: 10.1016/j.hlc.2014.11.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khadanga S, Savage PD, Gaalema DE, Ades PA. Predictors of cardiac rehabilitation participation. J Cardiopulm Rehabil Prev. 2022;41(5):322–327. doi: 10.1097/HCR.0000000000000573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Biddle MJ, Moser DK, Pelter MM, Robinson S, Dracup K. Predictors of adherence to self-care in rural patients with heart failure. Physiol Behav. 2017;176(3):139–148. doi: 10.1016/j.physbeh.2017.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nurhamsyah D, Trisyani Y, Nur’aeni A. Factors affecting quality of life of post-acute coronary syndrome patients in Indonesia. Open Access Maced J Med Sci. 2022;9(T6):203–206. doi: 10.3889/oamjms.2021.7319 [DOI] [Google Scholar]
- 10.Wistiani NMD, Puspawati NLPD, Pamungkas MA. Self-efficiency and quality of life coronary heart disease patients: a descriptive study. Basic Appl Nurs Res J. 2022;3(2):51–57. doi: 10.11594/banrj.03.02.04 [DOI] [Google Scholar]
- 11.Zhang J, Lyu S, Yin H, et al. Investigation of the quality of life of patients with coronary heart disease during COVID-19 and analysis of influencing factors. Psychol Heal Med. 2022;27(2):409–420. doi: 10.1080/13548506.2021.1930074 [DOI] [PubMed] [Google Scholar]
- 12.Sol BGM, van der Graaf Y, van Petersen R, Visseren FLJ. The effect of self-efficacy on cardiovascular lifestyle. Eur J Cardiovasc Nurs. 2011;10(3):180–186. doi: 10.1016/j.ejcnurse.2010.06.005 [DOI] [PubMed] [Google Scholar]
- 13.Salari A, Rouhi Balasi L, Moaddab F, Zaersabet F, Nouri Saeed A, Habib Nejad S. Patients’ cardiac self-efficacy after coronary artery angioplasty. Jundishapur J Chronic Dis Care. 2016;2016:1–5. [Google Scholar]
- 14.Woodgate J, Brawley LR. Self-efficacy for exercise in cardiac rehabilitation: review and recommendations. J Health Psychol. 2008;13(3):366–387. doi: 10.1177/1359105307088141 [DOI] [PubMed] [Google Scholar]
- 15.Almeida JAB, Florêncio RB, Lemos DA, Leite JC, Monteiro KS, Peroni Gualdi L. Self-efficacy instruments for individuals with coronary artery disease: a systematic review protocol. BMJ Open. 2022;12(7):1–4. doi: 10.1136/bmjopen-2022-062794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Joekes K, Van Elderen T, Schreurs K. Self-efficacy and overprotection are related to quality of life, psychological well-being and self-management in cardiac patients. J Health Psychol. 2007;12(1):4–16. doi: 10.1177/1359105306069096 [DOI] [PubMed] [Google Scholar]
- 17.Wantiyah W, Saputra MR, Deviantony F. Self-efficacy and health status in coronary artery disease patients. J Ners. 2020;15(1):14–18. doi: 10.20473/jn.v15i1.17628 [DOI] [Google Scholar]
- 18.Barham A, Ibraheem R, Zyoud SH. Cardiac self-efficacy and quality of life in patients with coronary heart disease: a cross-sectional study from Palestine. BMC Cardiovasc Disord. 2019;19(1):1–12. doi: 10.1186/s12872-019-01281-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhu Y, Song Y, Wang Y, et al. Relationships among social support, self-efficacy, and patient activation in community-dwelling older adults living with coronary heart disease: a cross-sectional study. Geriatr Nurs. 2022;48:135–140. doi: 10.1016/j.gerinurse.2022.09.008 [DOI] [PubMed] [Google Scholar]
- 20.Shrestha R, Rawal L, Bajracharya R, Ghimire A. Predictors of cardiac self-efficacy among patients diagnosed with coronary artery disease in tertiary hospitals in Nepal. J Public Health Res. 2020;9(4):1787. doi: 10.4081/jphr.2020.1787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kang Y, Yang IS. Cardiac self-efficacy and its predictors in patients with coronary artery diseases. J Clin Nurs. 2013;22(17–18):2465–2473. doi: 10.1111/jocn.12142 [DOI] [PubMed] [Google Scholar]
- 22.Kärner Köhler A, Tingström P, Jaarsma T, Nilsson S. Patient empowerment and general self-efficacy in patients with coronary heart disease: a cross-sectional study. BMC Fam Pract. 2018;19(1):1–10. doi: 10.1186/s12875-018-0749-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ibrahim NM. Self-efficacy, quality of life and coping strategies among patients with coronary artery bypass graft surgery. World J Nurs Sci. 2017;3(3):200–210. [Google Scholar]
- 24.Ni Kadek DPM, Puspawati NLPD, Lisnawati K. The relationship between self-efficacy and physical activity in coronary heart disease patients (Hubungan Efikasi Diri dengan Aktivitas Fisik Pada Pasien Penyakit Jantung Koroner). J Nurs Res Publ Media. 2023;2(1):29–38. Indonesian. [Google Scholar]
- 25.Wahyuni A, Setyowati S. Concept analysis of self efficacy among coronary heart disease patients undergoing percutaneous coronary intervention. J Aisyah J Ilmu Kesehat. 2022;7(4):1051–1058. [Google Scholar]
- 26.Ardiyanti D. Application of the rasch model on the development of the self-efficacy scale in student career decision making. J Psikol. 2017;43(3):248. [Google Scholar]
- 27.Melianasari D. Rasch stacking analysis: Career Decision Making Self-Efficacy (CDMSE) of students based on gender. Psychocentrum Rev. 2022;4(2):210–217. doi: 10.26539/pcr.42996 [DOI] [Google Scholar]
- 28.Boone W, Staver J, Yale M. Rasch Analysis in the Human Sciences. Dordrech: Springer; 2014. [Google Scholar]
- 29.Sumintono B, Widhiarso W. Aplikasi Model Rasch Untuk Penelitian Ilmu-Ilmu Sosial (Edisi Revisi) [Rasch Model Application for Social Research] Revised Edition. Trim Komunikata Publishing House; 2014. [Google Scholar]
- 30.Jimam NS, Ismail NE, Dangiwa DA, et al. Use of Rasch Wright map to understand the quality of Healthcare Workers’ Knowledge, Attitudes, and Practices for Uncomplicated Malaria (HKAPIUM). J Pharm Bioresour. 2021;18(3):237–244. doi: 10.4314/jpb.v18i3.8 [DOI] [Google Scholar]
- 31.Sumintono B Rasch model measurements as tools in assessment for learning. In 1st International Conference on Education Innovation (ICEI 2017); Atlantis Press; 2018:38–42. [Google Scholar]
- 32.Bonsaksen T, Kottorp A, Gay C, Fagermoen MS, Lerdal A. Rasch analysis of the general self-efficacy scale in a sample of persons with morbid obesity. Health Qual Life Outcomes. 2013;11(1):1–11. doi: 10.1186/1477-7525-11-202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Peter C, Cieza A, Geyh S. Rasch analysis of the general self-efficacy scale in spinal cord injury. J Health Psychol. 2014;19(4):544–555. doi: 10.1177/1359105313475897 [DOI] [PubMed] [Google Scholar]
- 34.Afrizal A. Application of the Rasch model in measuring consumer attitudes and word of mouth on student decisions to choose to study at private tertiary institutions. J Ilm Cano Ekon. 2018;7(2):1. [Google Scholar]
- 35.Prasetiyo WH, Sari BI, Sa’diyah H, Naidu NBM, Prasetyo E. Using Rasch model analysis for assessing psychometric properties of digital citizenship in Indonesian students. J E-Learning Knowl Soc. 2022;18(3):96–110. [Google Scholar]
- 36.Asiah N, Rusmana N, Saripah I, Hamdan AH. The development and validation of Indonesian Hope Scale (IHS): a Rasch model analysis. Int J Res Couns Educ. 2022;6(1):69–77. [Google Scholar]
- 37.Bujang MA, Baharum N. Sample size guideline for correlation analysis. World J Soc Sci Res. 2016;3(1):37. doi: 10.22158/wjssr.v3n1p37 [DOI] [Google Scholar]
- 38.Nuraeni A, Mirwanti R, Anna A. Effect of a workbook in health education on self-efficacy and quality of life of patients with coronary heart disease. Belitung Nurs J. 2019;5(6):218–224. doi: 10.33546/bnj.801 [DOI] [Google Scholar]
- 39.Sumintono B, Widhiarso W. Application of the Rasch Model to Research in the Social Sciences. Cimahi: Trim Komunikata Publishing House; 2014. [Google Scholar]
- 40.Abdullah N, Noranee S, Khamis MR. The use of Rasch wright map in assessing conceptual understanding of electricity. Pertanika J Soc Sci Humanit. 2017;25(25):81–92. [Google Scholar]
- 41.Boone WJ, Staver JR, Yale MS, Boone WJ, Staver JR, Yale MS. Person reliability, item reliability, and more. In: Rasch Analysis in the Human Sciences. Springer; 2014:217–234. [Google Scholar]
- 42.Sari EA, Sari SP, Pratiwi SH. Community self-efficacy of coronary heart disease based on characteristic risk factors. NurseLine J. 2018;3(2):65. doi: 10.19184/nlj.v3i2.8341 [DOI] [Google Scholar]
- 43.O’Neil A, Berk M, Davis J, Stafford L. Cardiac-self efficacy predicts adverse outcomes in coronary artery disease (CAD) patients. Health. 2013;05(07):6–14. doi: 10.4236/health.2013.57A3002 [DOI] [Google Scholar]
- 44.Fahmi I, Suryaman A, Ganefianty A. The relationship of psychological well-being with a cardiac diet self efficacy in acute coronary syndrome patients. J Pendidik Keperawatan Indones. 2022;8(2):119–126. [Google Scholar]
- 45.Hasannezhad P, Khanjari S, Nikpajouh A, Hasannezhad Z, Haghani H, Sabeti F. Impact of self-care education on self-efficacy and quality of life of late adolescents with congenital heart disease. J Client Centered Nurs Care. 2023;9(1):69–78. doi: 10.32598/JCCNC.9.1.480.1 [DOI] [Google Scholar]
- 46.Harsono H. The relationship between self care and quality of life among coronary heart disease patients after receiving percutaneous coronary intervention. In: The 4th International Virtual Conference on Nursing; 2021:155–171. [Google Scholar]
- 47.Purnomo A, Herawati T, Yona S. Exploration factors influencing self-efficacy in patients with heart. NurseLine J. 2020;5(2):285–292. doi: 10.19184/nlj.v5i2.17005 [DOI] [Google Scholar]
- 48.Al-Sutari M, Ahmad M. Predictors of adherence to self-care behaviors among patients with coronary heart disease. Nurs Pract Today. 2022;9(2):145–157. [Google Scholar]
- 49.Abdollahzadeh F, Asghari E, Jafarabadi MA, Khangah B, Pourshahbazi E. Predictors of self-management in patients with coronary artery diseases. Int J Med Res Heal Sci. 2016;5(7s):637–643. [Google Scholar]
- 50.Nuraeni A, Praptiwi A, Nurhidayah I. Depression, recurrence, and perceptions of physical fitness among CHD patients: a comparison based on participation in phase II cardiac rehabilitation program. J Keperawatan Padjadjaran. 2020;8(3):241–251. [Google Scholar]
- 51.Nur’aeni A, Nur’aeni A, Mirwanti R. Acceptance, perceived benefits, and helplessness among coronary heart disease patients undergoing treatment in a different ward. Padjadjaran Acute Care Nurs J. 2020;1(2):80–87. [Google Scholar]
- 52.Vergara F, Rosa J, Orozco C, et al. Evaluation of learned helplessness, self-efficacy and disease activity, functional capacity and pain in Argentinian patients with rheumatoid arthritis. Scand J Rheumatol. 2017;46(1):17–21. doi: 10.3109/03009742.2016.1155643 [DOI] [PubMed] [Google Scholar]
- 53.Sarkar U, Ali S, Whooley MA. Self-efficacy as a marker of cardiac function and predictor of heart failure hospitalization and mortality in patients with stable coronary heart disease: findings from the heart and soul study. Health Psychol. 2009;28(2):166–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Polsook R, Aungsuroch Y. A cross-sectional study of factors predicting readmission in Thais with coronary artery disease. J Res Nurs. 2021;26(4):293–304. doi: 10.1177/1744987120946792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yehle KS, Plake KS. Self-efficacy and educational interventions in heart failure: a review of the literature. J Cardiovasc Nurs. 2010;25(3):175–188. doi: 10.1097/JCN.0b013e3181c71e8e [DOI] [PubMed] [Google Scholar]
- 56.Salah Eldin Saad N, El Ashery Ashery Asker R. Effect of digital cardiac rehabilitation program on self efficacy of patients with coronary artery diseases. Egypt J Heal Care. 2020;11(1):400–416. doi: 10.21608/ejhc.2020.177145 [DOI] [Google Scholar]
- 57.Zhou Y, Liao J, Feng F, Ji M, Zhao C, Wang X. Effects of a nurse-led phone follow-up education program based on the self-efficacy among patients with cardiovascular disease. J Cardiovasc Nurs. 2018;33(1):E15–23. doi: 10.1097/JCN.0000000000000414 [DOI] [PubMed] [Google Scholar]
- 58.Ahmadi Z, Abolhassani S, Hasheminia A, Kheiri S. The effects of a multimedia education on self-efficacy and self-esteem among patients with acute coronary syndrome: a clinical randomized trial. Iran J Nurs Midwifery Res. 2022;27(3):181–187. doi: 10.4103/ijnmr.IJNMR_92_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Boroumand S, Moeini M. The effect of a text message and telephone follow-up program on cardiac self-efficacy of patients with coronary artery disease: a randomized controlled trial. Iran J Nurs Midwifery Res. 2016;21(2):171–176. doi: 10.4103/1735-9066.178243 [DOI] [PMC free article] [PubMed] [Google Scholar]