Abstract
The facial artery is the main artery supplying the face occasionally. It gives three branches on the face, the inferior labial, the superior labial, and the lateral nasal, and terminates as the angular artery. Due to congenital vascular variations in the facial artery, it has been considered in the dissection of the head and neck region. During the dissection of a 65-year-old woman to expose this region, we discovered that the left facial artery is terminated by the superior labial artery after giving off the submental and inferior labial branches. At the level of the left oral commissure, the facial artery was attached to the buccinator muscle as connective tissue, with a noticeable decrease in diameter. The purpose of this study is to report a new variation of the facial artery that is particularly important for cadaver dissection, and head and neck surgeries, as well as for facial artery angiography.
Keywords: Arteries, anatomic variation, cadaver, dissection, facial
INTRODUCTION
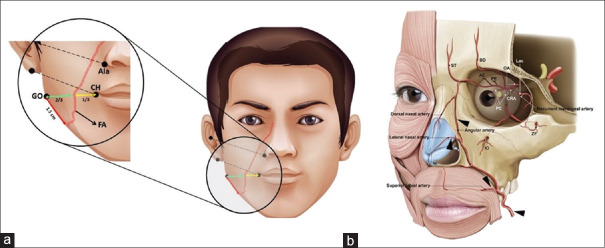
The facial artery is a branch of the external carotid artery, which arises just above the tip of the greater horn of the hyoid bone. The facial artery crosses the inferior mandibular rim just anterior to the masseter muscle insertion, according to surface anatomy. Immediately after the artery grooves the posterior border of the submandibular gland, it forms two loops, first winding down over the submandibular gland, then up over the base of the mandible, and also it is palpated simply at the antro-inferior angle of masseter muscle [Figure 1a].[1]
Figure 1.
(a) Surface anatomy of the facial artery (GO = Gonion CH = Cheilion FA = Facial Artery). (b) Tributaries and direction of the facial artery
After running upwards and forwards, it then ascends to the medial angle of the eye where it terminates by anastomosing with the dorsal nasal branch of the ophthalmic artery. In the face, the facial artery has three main branches including the superior labial, inferior labial, and lateral nasal through its course in this region. As this artery passes through the face, it runs in a lateromedial direction, but since it has been received into the medial canthus of the eye, it continues and ends as an Angular artery [Figure 1b].[2,3] Some studies, however, indicate that in 23% of cases, the angular artery is a branch of the ophthalmic artery.[4] In terms of surgery and dissection, understanding the surface anatomy of this artery is important. Some landmarks such as Manson's point have been used to identify the exact location of this artery.[4,5] Although in many cases these variations do not lead to any diseases or injuries,[6] vascular variants are the most prevalent differences among the arteries and the veins which are extremely crucial related to anatomical education and dissection, surgeries, ultrasound, and angiography.[6,7]
It is possible to see variations in any part of the facial artery. To illustrate, some studies have reported that the facial and lingual arteries have a common trunk called the linguofacial artery which arises from the external carotid.[8,9] Furthermore, this artery may originate within the parotid gland, referred to as the intra-parotid origin.[10] It has been shown that there are some variations related to the course and branches of the right facial artery compared to the left one. As it is mentioned above, this artery can make a loop during its course through the submandibular region, but in some cases not only this loop does not form but Also after passing a short distance, it extends to the lower lip and terminates as the inferior labial artery.[11] In the latest research about facial artery variants, two radiologists retrospectively reviewed 284 cases in angiographies and classified facial arteries into 4 types according to the end branches. This research assessed facial artery variant patterns 36.6% (angular branch), 48.6% (lateral nasal branches), 8.5% (superior labial branches), and, 6.3% (inferior labial branches).[12] In terms of the facial artery development, it is indicated that this artery is prone to agenesis, enlargements, and excessive narrowness, all of which are related to the development of the cardiovascular system in the fetus and how the pharyngeal arches and different branches of each disappear and fuse.[8,13] In addition, this artery may not lead to the medial canthus but goes towards the zygomatic arch or infraorbital which is recognized as a deviated branch.[14,15,16] Due to the wide range of variations of this artery in the way of blood supply to the face and the number of branches separated from it, different categories are made for the variants of this artery.[12]
CASE REPORT
In October 2021, in the Anatomical department of Isfahan University of Medical Sciences, during the dissection of the head and neck of a 65-year-old woman, a case of variation was identified while searching the left facial artery. Further a more accurate search of this area, it is revealed that the facial artery entered the face and after arising the two branches submental and inferior labial, it became extremely narrow and then with the giving off another very small branch that was analogous to the superior labial artery in diameter reached less than one millimeter and disappeared from the naked eye by entering the buccinator muscle. The facial artery ends approximately at the angle of the mouth, and from this region to the medial canthus, this artery does not exist [Figure 2].
Figure 2.
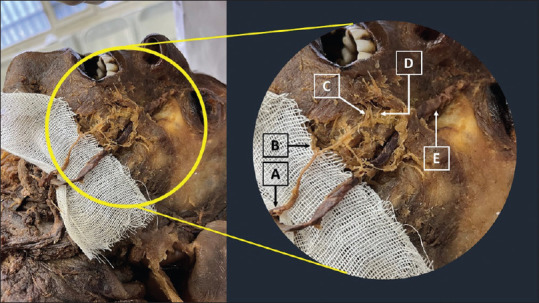
(A) Left facial artery (B) Inferior labial artery (C) Superior labial artery (D) Terminal part of facial artery (E) Facial vein
DISCUSSION
The facial artery is one of three arteries that contribute to the blood supply of the face, originating from the external carotid. There are some variations along its course. As it is mentioned above, it originates from a common trunk with the lingual artery, has unusual loops and deviations in its path, is even shorter than usual, and ends before reaching the medial canthus of the eye.[1,12,17] A study on 40 cadavers has shown that the facial artery terminates as the angular artery in 27 percent of cases, the superior labial artery in 40 percent, and the lateral nasal artery in 30 percent of cases.[9] In examining the variants of the facial artery, the existence of a common trunk with some branches of the external ceratoid artery, the path of movement of this artery in the face, and its terminal branches have always been discussed. However, previous studies have not addressed the issue of conversion of the facial artery to connective tissue and its significant diameter change. In the present study, the facial artery on the right side based on variations was normal and eventually ended in the lateral nasal artery [Figure 3]. Many studies have considered the existence of a common trunk with other branches of the external carotid, the course of the facial artery, and its terminal branches. However, there is no evidence that the artery's diameter decreases or even turns into connective tissue. In the present study, the right facial artery showed normal anatomy through its course, in the left side had a normal course until it reached the angle of the mouth, the diameter then surprisingly showed a significant decrease and it was attached to the buccinator muscle as connective tissue. This artery did not present any tubular structure which is expected to be seen in a normal artery. Therefore, in this case, there is no anastomosis between the facial artery and the ophthalmic artery in the medial canthus, and the blood supply of this region is provided by the angular artery which is raised from the ophthalmic artery in this case. To prove this claim, it has been reported in 23% of cases that the angular artery has been given off from the ophthalmic artery.[4]
Figure 3.

(A) Right facial artery (B) Facial vein (C) Superior labial artery (D) Lateral nasal artery
CONCLUSION
As a result of the complex development of the vascular system, some variations have always been observed. Due to its variations, it has been shown that the facial artery has been considered in the dissection of the head and neck region. A new type of facial artery variation was discussed in this study, which was the conversion of the arterial lumen into connective tissue. These variations can be used to improve facial and mandible surgeries, diagnostic imaging, dissection method, and especially education. It also reduces the possibility of arteries being injured.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Lohn JW, Penn JW, Norton J, Butler PE. The course and variation of the facial artery and vein: Implications for facial transplantation and facial surgery. Ann Plast Surg. 2011;67:184–8. doi: 10.1097/SAP.0b013e31822484ae. [DOI] [PubMed] [Google Scholar]
- 2.Azim NH, Subki A. Abiotic stresses induce total phenolic, total flavonoid and antioxidant properties in Malaysian indigenous microalgae and cyanobacterium. Malays J Microbiol. 2018:25–33. [Google Scholar]
- 3.Moon H-J. Use of fillers in rhinoplasty. Clin Plast Surg. 2016;43:307–17. doi: 10.1016/j.cps.2015.08.003. [DOI] [PubMed] [Google Scholar]
- 4.Lee HJ, Won SY, O J, Hu KS, Mun SY, Yang HM, et al. The facial artery: A comprehensive anatomical review. Clin Anat. 2018;31:99–108. doi: 10.1002/ca.23007. [DOI] [PubMed] [Google Scholar]
- 5.Koziej M, Trybus M, Hołda M, Polak J, Wnuk J, Brzegowy P, et al. Anatomical map of the facial artery for facial reconstruction and aesthetic procedures. Aesthet Surg J. 2019;39:1151–62. doi: 10.1093/asj/sjz028. [DOI] [PubMed] [Google Scholar]
- 6.Kumar A, Elumalai G, Thangamani M, Palayathan N, Singh MK. A rare variation in facial artery and its implications in facial surgery: Case report. J Surg. 2014;2:68–71. [Google Scholar]
- 7.Di Dio LJ. The importance of anatomy. Ann Anat. 1999;181:455–65. doi: 10.1016/s0940-9602(99)80024-7. [DOI] [PubMed] [Google Scholar]
- 8.Mangalgiri A, Namdev LN, Mahore D, Kapre M. The study of higher origin of facial artery and its surgical significance. Indian J Otolaryngol Head Neck Surg. 2015;67:72–4. doi: 10.1007/s12070-014-0786-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Midy D, Mauruc B, Vergnes P, Caliot P. A contribution to the study of the facial artery, its branches and anastomoses; application to the anatomic vascular bases of facial flaps. Surg Radiol Anat. 1986;8:99–107. doi: 10.1007/BF02421376. [DOI] [PubMed] [Google Scholar]
- 10.Nayak S. Abnormal intra-parotid origin of the facial artery. Saudi Med J. 2006;27:1602. [PubMed] [Google Scholar]
- 11.Marx C, Kumar P, Reddy S, Vollala VR. Bilateral variation of facial artery: A case report. Rom J Morphol Embryol. 2008;49:399–401. [PubMed] [Google Scholar]
- 12.Hong SJ, Park SE, Jo JW, Jeong DS, Choi DS, Won JH, et al. Variant facial artery anatomy revisited: Conventional angiography performed in 284 cases. Medicine (Baltimore) 2020;99:e21048. doi: 10.1097/MD.0000000000021048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vijayalakshmi M, Thenmozhi M, Mohanraj KG, Satheesh Kumar C. A study of variations in the origin of facial artery. Drug Invention Today. 2018;10:2400–3. [Google Scholar]
- 14.Furukawa M, Mathes DW, Anzai Y. Evaluation of the facial artery on computed tomographic angiography using 64-slice multidetector computed tomography: Implications for facial reconstruction in plastic surgery. Plast Reconstruct Surg. 2013;131:526–35. doi: 10.1097/PRS.0b013e31827c6f18. [DOI] [PubMed] [Google Scholar]
- 15.Lee J-G, Yang H-M, Choi Y-J, Favero V, Kim Y-S, Hu K-S, et al. Facial arterial depth and relationship with the facial musculature layer. Plast Reconstruct Surg. 2015;135:437–44. doi: 10.1097/PRS.0000000000000991. [DOI] [PubMed] [Google Scholar]
- 16.Yang H-M, Lee J-G, Hu K-S, Gil Y-C, Choi Y-J, Lee H-K, et al. New anatomical insights on the course and branching patterns of the facial artery: Clinical implications of injectable treatments to the nasolabial fold and nasojugal groove. Plast Reconstruct Surg. 2014;133:1077–82. doi: 10.1097/PRS.0000000000000099. [DOI] [PubMed] [Google Scholar]
- 17.Loukas M, Hullett J, Louis RG, Kapos T, Knight J, Nagy R, et al. A detailed observation of variations of the facial artery, with emphasis on the superior labial artery. Surg Radiol Anat. 2006;28:316–24. doi: 10.1007/s00276-006-0093-0. [DOI] [PubMed] [Google Scholar]