Abstract
Background.
Alcohol-related morbidity and mortality have increased substantially in the U.S. Understanding the population health implications of these concerning trends, including by identifying clinical subgroups of alcohol users at increased risk for potentially preventable acute causes of mortality, is of critical importance.
Methods.
This retrospective cohort study used statewide, all-payer, longitudinally-linked ED patient record and mortality data from California. Participants comprised all residents presenting to a licensed ED at least once in 2009–2011 with a diagnosis of alcohol use disorder (AUD). Participants were followed for one year after index ED visit to assess acute injury (unintentional poisoning, suicide, homicide, motor vehicle crash, and fall- or fire-related injury) and all-cause mortality rates per 100,000 person-years. Age-, sex-, race/ethnicity-adjusted standardized mortality rates (SMRs) for acute injury causes of death were determined using statewide mortality data.
Results.
Among 437,855 patients with index non-fatal ED visits for AUD, the 12-month acute injury mortality rate was 608.6 per 100,000 (SMR=8.0; 95% CI=7.7, 8.3), and all-cause mortality was 5,700.7 per 100,000 (SMR=6.5; 95% CI=6.4, 6.6). Unintentional poisoning accounted for 46.5%, and suicide for 19.7%, of acute-injury deaths. Acute injury deaths comprised 71.7% of all-cause mortality among patients aged 10–24 years, but much lower proportions among older patients. Female AUD patients had lower rates for all mortality outcomes.
Conclusions.
Emergency department patients with a recognized AUD comprise a population at persistently elevated risk for mortality. Age-related AUD patient differences in common causes of death, including drug overdose and suicide, can inform the structure of future clinical interventions.
Keywords: Emergency department, alcohol, mortality, injury
1. INTRODUCTION
Alcohol-related morbidity and mortality have increased substantially in the U.S. over the past 20 years (Grucza et al., 2018; Shmulewitz et al., 2021; Spillane et al., 2020; White et al., 2020, 2018). Among the most prominent indicators of growing alcohol morbidity are rates of alcohol-related emergency department (ED) visits and binge drinking, which experienced annual increases of approximately 5% and 1%, respectively, during the first two decades of this century (Grucza et al., 2018; White et al., 2018). For both indicators, the increases appear to be particularly pronounced in females and in middle-aged and older adults. Understanding the population health implications of these concerning trends is of critical importance for informing public health interventions. As part of this goal, identifying subgroups of alcohol users at increased risk for potentially preventable acute causes of mortality can help target clinical interventions.
Patients in clinical samples diagnosed with alcohol-related disorders, hereafter alcohol use disorders (AUD), have all-cause mortality rates that are twice as high as those of individuals without AUD in the general population, and three to four times higher than those of non-AUD comparison groups (Roerecke and Rehm, 2013). Cause-specific mortality ratios among patients with AUD range from two (for cancer and cardiovascular diseases) to nearly 15 (for liver cirrhosis) (Roerecke and Rehm, 2014). Thus, patients with AUD represent a particularly high-risk population that warrants research attention and public health prevention.
ED patients presenting with AUD may face especially high mortality risk, given their increased likelihood of polysubstance use (Fleming et al., 2007; Sanjuan et al., 2014) and comorbid medical and psychiatric conditions (Klein et al., 2018). Furthermore, because alcohol problems are highly prevalent among ED patients (Li et al., 1998; McDonald et al., 2004), mortality information on ED patients with AUD could inform clinical and public health prevention efforts aimed at reducing their mortality risks. Examinations of mortality risks among large general U.S.-based populations of patients presenting with alcohol misuse, however, are currently lacking.
The present study examined 12-month prospective rates of all-cause and selected acute cause-specific mortality among residents of California with ED visits involving AUD diagnoses. The analyses focused primarily on acute injury causes of death that the Centers for Disease Control and Prevention (CDC) includes in its Alcohol-Related Disease Impact application (Centers for Disease Control and Prevention, 2021) to estimate alcohol-related harm, including suicide, homicide, and various unintentional injuries. These deaths differ from chronic alcohol-related natural causes of death (e.g., liver cirrhosis) in that they may offer greater opportunities for prevention through targeted interventions in “boundaried settings” (U.S. Department of Health and Human Services (HHS) Office of the Surgeon General and National Action Alliance for Suicide Prevention, 2012) such as EDs (Betz et al., 2016; Hawk and D’Onofrio, 2018; Houry et al., 2009). ED-based brief interventions among patients with problematic alcohol use have been shown to potentially reduce subsequent acute injury-related morbidity, although this evidence is conflicting and suggests that the greatest benefit is among persons with less severe forms of alcohol misuse (Barata et al., 2017; Landy et al., 2016). Very few studies have assessed mortality as an outcome, and no interventions have been shown to reduce mortality in patient populations with AUD.
As part of our analysis, we examined acute injury causes of death in the period shortly after discharge from the ED or hospital. If the risk of acute causes of death, a fraction of which are likely to be related to alcohol use, is elevated during the weeks immediately after discharge, interventions may need to emphasize components that provide rapid support, such as monitoring and assistance immediately following detoxification (Timko et al., 2019), rather than relying on longer-term programs that can involve months-long delays before intake.
Risk of fatal acute injuries may be concentrated among patients of a particular age or a particular gender. If so, practice guidelines for screening and referral processes should reflect differential risk across the adult lifespan of dying from acute vs. natural causes, even those stemming primarily from alcohol-related harm (Askgaard et al., 2020; Roerecke and Rehm, 2014). To assess risk across age and gender, we examined age and gender variability in the proportion of all deaths among AUD patients that were accounted for by acute injury causes.
2. METHODS
2.1. Data
Discharge data were obtained from the California Office of Statewide Health Planning and Development (OSHPD) on all visits in 2009–2011 to all California-licensed EDs by individuals aged ≥10 years with a California residential zip code. OSPHD also provided information on all individuals in this ED cohort to the California Department of Public Health Vital Records, which assessed vital status in California death records and provided information on date and cause of death for all matching decedents who died in 2009–2012 (excluding those who died out of state, <1% of the total). All data obtained and used by the study team were de-identified, and reflect the most recent year comprehensive death linkages were available. This study was approved by the IRBs of the California Health and Human Services Agency and the University of California, Merced. Data were analyzed June-July 2021.
This cohort was then restricted to all patients with active alcohol dependence, abuse, withdrawal, or related codes, defined as those with at least one ED visit during the 2009–2011 study period that included an International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code in any diagnostic position corresponding to alcohol dependence (codes 303.0–303.02, 303.90–303.92, 790.3, 980.0, or 980.9), alcohol abuse (305.0–305.02), alcohol withdrawal (291.0, 291.4, 298.81) or alcohol poisoning (external cause-of-injury codes [E-codes] E860.0, E860.1, E860.9). Qualifying alcohol visits could not include an ICD-9-CM code corresponding to deliberate self-harm (E950-E958). Since 1990, California has mandated 100% reporting of external cause-of-injury codes (E-codes), which describe the cause and intent of an injury in a single supplementary code (Abellera et al., 2005).
The analyses were limited to index visits, defined as patients’ first ED visit that qualified for study inclusion during the study period. For visits resulting in patient discharge or transfer to another facility, the index date was the date of ED presentation. For visits that resulted in a same-hospital admission, the index date was the date of discharge from the associated hospitalization (Olfson et al., 2017). Patients whose index visit resulted in death were excluded from follow-up analyses.
For calculation of standardized mortality ratios, data on death by manner for California overall in 2009–2012 were obtained from the Center for Disease Control’s WONDER system (Centers for Disease Control and Prevention (National Center for Health Statistics), 2017).
2.2. Measures
The primary outcomes were death within one year of the index date by non-overlapping acute causes of injury that are included in the Centers for Disease Control and Prevention Alcohol-Related Disease Impact Codes (Centers for Disease Control and Prevention, 2021). CDC considers a fraction of these acute injury deaths attributable to alcohol. These mortality outcomes included unintentional poisonings, motor vehicle crashes, fall- or fire-related injuries, suicide, homicide, and an “all other” acute cause category, which comprised various rare causes of injury. To estimate the proportion of all-cause deaths among alcohol patients accounted for by these selected acute injury causes, we also examined deaths from natural causes and deaths from any cause. We defined manners and causes of death based on ICD-10-CM codes (see Table S1), where cause of death refers to the mechanism of the specific injury or disease that led to death and manner of death refers to the determination of how the injury or disease led to death.
Patient demographic characteristics were examined for descriptive purposes and to calculate standardized mortality ratios. These characteristics included gender (male, female), age group (10–24, 25–44, 45–64, ≥65 years at discharge), race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, Asian/Pacific Islander, other), and insurance status (private, Medicaid, Medicare, self-pay, and other).
Primary ICD-9-CM diagnosis at index visit was examined for descriptive purposes, using the diagnoses’ Clinical Classification Software (CCS) groupings. The CCS system aggregates ICD-9-CM diagnoses into discrete, clinically meaningful categories (Elixhauser et al., 2014).
2.3. Analyses
Crude mortality rates per 100,000 person-years of follow-up were calculated, using the survival analysis “st” command suite in Stata 14 (StataCorp LP), for each category of death in the year after the index date. We also calculated age group- and sex-specific mortality rates for each category of death. Individuals who did not link to California mortality records from 365 days after the index date were presumed alive for this period. Decedents were treated as censored on their death date.
Annualized standardized mortality ratios (SMRs), defined as the ratio of the observed numbers of deaths in the ED cohort to expected deaths, were calculated for each category of death. The numbers of expected deaths in California for 2009–2012 were calculated using the WONDER mortality database (based on 5-year age groups), standardized to the distribution of gender, age category, and race/ethnicity category of the ED patient group. We also calculated age- and sex-specific SMRs for all acute injury mortality, natural-cause mortality, and all-cause mortality.
3. RESULTS
During the study period, California patients aged ≥10 years made more than 25.3 million emergency department visits, of which approximately 3.2% had a comorbid AUD diagnosis. A total of 437,855 uniquely-identifiable patients had index non-fatal ED visits for acute alcohol intoxication, dependence, abuse, or withdrawal during the study period, collectively referred to as AUD. Alcohol-related disorder (CCS code 660) was the most common primary diagnosis at index visit (present at 23.9% of all index visits); the next most common primary diagnoses were an open wound to the head, neck, or trunk (3.8%) and superficial injury (3.3%). An additional 5,786 patients had fatal index events and were excluded from follow-up analyses.
The majority of patients in the analytic sample were male (67.8%), and the average age was 44.3 years (SD: 17.2); more than half were non-Hispanic white, with another quarter of Hispanic ethnicity (Table 1). More than two-thirds of the patients had a diagnosis of alcohol abuse without intoxication (69.7%), with most of the rest diagnosed with acute alcohol intoxication or withdrawal (29.6%).
TABLE 1.
Patient characteristics among 437,855 patients receiving emergency department care for acute alcohol intoxication, alcohol dependence, or alcohol abuse, California, 2009-2011.
| Patient characteristics at index visit | N (%) |
|---|---|
|
| |
| Female sex, n (%) | 141,312 (32.2%) |
| Age in years, mean (SD) | 44.5 (17.3) |
| 10–18 years | 20,463 (4.7%) |
| 19–24 years | 51,622 (11.8%) |
| 25–44 years | 141,724 (32.4%) |
| 45–64 years | 169,895 (38.8%) |
| ≥65 years | 54,151 (12.4%) |
| Race/ethnicity, n (%) | |
| Non-Hispanic White | 237,933 (54.3%) |
| Non-Hispanic Black | 50,721 (11.6%) |
| Hispanic | 115,207 (26.3%) |
| Asian/Pac. Islander | 12,797 (2.9%) |
| Non-Hispanic Other | 21,197 (4.8%) |
| Insurance type, n (%) | |
| Private | 120,165 (27.5%) |
| Medicare | 65,969 (15.1%) |
| Medicaid | 104,619 (23.9%) |
| Self-pay | 132,661 (30.3%) |
| Other | 14,081 (3.2%) |
| Alcohol use disorders* | |
| Alcohol dependence | 134,939 (30.4%) |
| Alcohol abuse | 310,580 (70.0%) |
| Alcohol withdrawal | 8,420 (1.9%) |
| Visit disposition | |
| Discharged home | 261,550 (59.7%) |
| Admitted as inpatient | 170,983 (39.1%) |
| Other | 5,322 (1.2%) |
Groups are not mutually exclusive.
A total of 2,671 patients died from one of the selected acute injury causes in the year after index visit, a mortality rate of 608.6 per 100,000. This rate was eight times higher than that of the demographically matched California population (SMR: 8.0 [95% CI: 7.7, 8.3]) (Table 2). Deaths were slightly concentrated in the first part of the follow-up period, with 15.5% (n=413) occurring in the first 30 days, 33.9% (n=904) occurring in the first 90 days, and 58.1% (n=1,554) occurring in the first 6 months, but acute injury mortality risk remained persistently high across the follow-up period (Figure 1).
TABLE 2.
Mortality from selected acute injury causes of death* within one year among California emergency department patients with alcohol dependence, abuse, or withdrawal.
| Manner of death | Deaths, n | Mortality per 100,000 p-y | SMRa (95% CI) | Fraction acute injury deaths |
|---|---|---|---|---|
|
| ||||
| Suicide | 527 | 124.7 | 6.8 (6.2, 7.4) | 19.7% |
| Homicide | 167 | 39.5 | 4.8 (4.1, 5.6) | 6.3% |
| Unintentional injury deaths | ||||
| Poisoning | 1,241 | 293.7 | 15.1 (14.3, 16.0) | 46.5% |
| Motor vehicle crash | 303 | 71.7 | 5.6 (4.9, 6.2) | 11.3% |
| Fall- or fire-related injury | 341 | 80.7 | 9.3 (8.3, 10.3) | 12.8% |
| Other acute injury death | 92 | 21.8 | 1.92 (1.6, 2.4) | 3.4% |
|
| ||||
| All acute injury causes | 2,671 | 608.6 | 8.0 (7.7, 8.3) | 100% |
|
| ||||
| Natural-cause deaths | 21,297 | 5,040.0 | 6.3 (6.2, 6.4) | NA |
|
| ||||
| All-cause mortality | 24,089 | 5,700.7 | 6.5 (6.4, 6.6) | NA |
Centers for Disease Control and Prevention. Alcohol-Related ICD Codes. https://www.cdc.gov/alcohol/ardi/alcohol-related-icd-codes.html.
p-y: person-years.
Standardized Mortality Ratio: mortality by manner of ED group relative to mortality by manner of California population in 2009–2012 matched to the ED group by age, sex, and race/ethnicity. California data come from CDC WONDER detailed mortality tables (https://wonder.cdc.gov/ucd-icd10.html, accessed June 2019).
Figure 1.
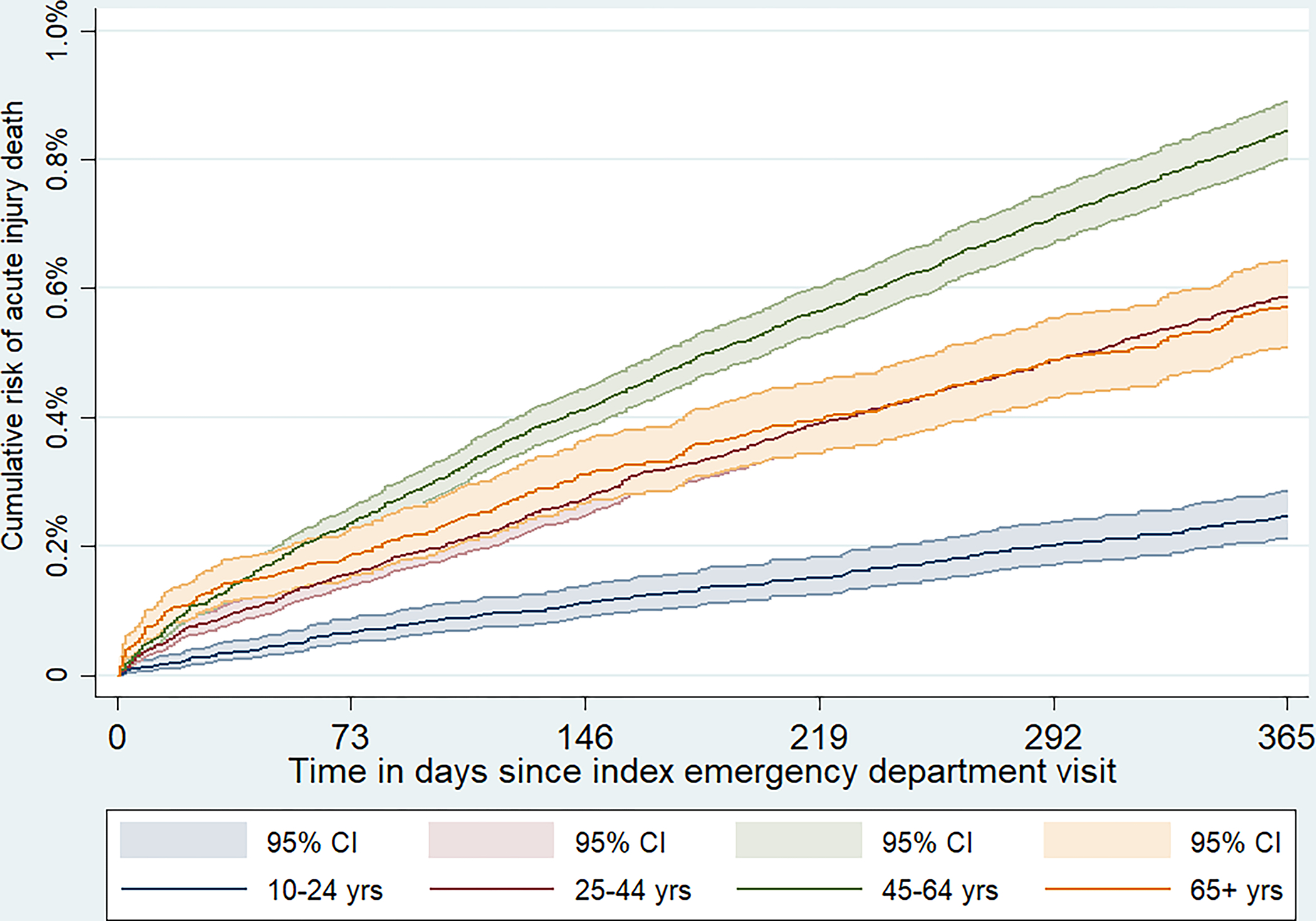
Cumulative incidence of selected acute injury causes of death in the 12 months after index emergency department visit, by age group.
Nearly half of acute injury deaths were due to unintentional poisoning, from which alcohol patients died at approximately 15 times the rate of the demographically matched population (with a rate of 293.7 per 100,000; SMR: 15.1 [14.3, 16.0]). Per the ICD-10 cause-of-death codes, the vast majority of these poisoning deaths were due to “unspecified” drugs (38.9%), narcotics or hallucinogens (30.1%), alcohol poisoning (17.3%), or sedatives/hypnotics (9.8%). Suicide was the second-leading cause of the selected acute injury deaths in the patient cohort (rate of 124.7 per 100,000; SMR: 6.8 [6.2, 7.4]), and was responsible for nearly 20% of these deaths. The primary methods used by suicide decedents comprised hanging or strangulation (28.1%), firearm (18.0%), or self-poisoning (16.3%). Fall- or fire-related injuries and motor vehicle crashes were responsible for most of the remaining acute deaths, with SMRs of 9.3 [8.3, 10.3] and 5.6 [4.9, 6.2], respectively.
Overall, the acute injury deaths accounted for 11.1% of 12-month all-cause mortality among the patient cohort (Table 1). However, this proportion varied substantially by age, and accounted for 71.7% among patients aged 10–24 years, 33.6% among those aged 25–44 years, 11.4% among those aged 45–64 years, and just 3.0% among patients aged ≥65 years (Table 3 and Figure 2). Age-specific SMRs for acute injury mortality, natural-cause mortality, and all-cause mortality tended to be somewhat higher in the age 25–44 (SMRs = 8.1, 15.1, and 12.6, respectively) and age 45–64 groups (SMRs = 9.6, 11.2, and 11.1) than in the age 10–24 (SMRs = 5.5, 6.5, and 6.8) and age ≥65 groups (SMRs = 5.0, 3.9, and 3.9), although direct comparisons of SMRs are not possible because they are standardized to different patient groups (Rothman et al., 2008).
TABLE 3.
Age-specific mortality rates from selected acute injury causes of death* within one year of emergency department patients presenting with alcohol dependence, abuse, or withdrawal.
| Manner of death | Age 10–24 years | Age 25–44 years | Age 45–64 years | Age ≥65 years | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Deaths, n | Mortality per 100,000 p-y | Deaths, n | Mortality per 100,000 p-y | Deaths, n | Mortality per 100,000 p-y | Deaths, n | Mortality per 100,000 p-y | |
|
| ||||||||
| Suicide | 39 | 54.2 | 168 | 119.8 | 269 | 165.7 | 51 | 106.1 |
| Homicide | 37 | 51.5 | 72 | 51.3 | 53 | 32.7 | 5 | 10.4 |
| Unintentional injury deaths | ||||||||
| Poisoning | 68 | 94.6 | 437 | 311.7 | 689 | 424.4 | 47 | 97.7 |
| Motor vehicle crash | 27 | 37.6 | 90 | 64.2 | 149 | 91.8 | 37 | 76.9 |
| Fall- or fire-related injury | 3 | 4.2 | 38 | 27.1 | 170 | 104.7 | 130 | 270.3 |
| Other acute injury death | 3 | 4.2 | 23 | 16.4 | 55 | 33.9 | 11 | 22.9 |
|
| ||||||||
| All selected acute injury causes | 177 | 246.2 | 828 | 590.5 | 1,385 | 853.1 | 281 | 584.4 |
|
| ||||||||
| Natural-cause deaths | 65 | 90.4 | 1,600 | 1,141.1 | 10,654 | 6,562.5 | 8,978 | 18,670.0 |
|
| ||||||||
| All-cause mortality | 247 | 343.5 | 2,464 | 1,757.3 | 12,105 | 7,456.3 | 9,273 | 18,895.0 |
Centers for Disease Control and Prevention. Alcohol-Related ICD Codes. https://www.cdc.gov/alcohol/ardi/alcohol-related-icd-codes.html. p-y: person-years.
Figure 2.
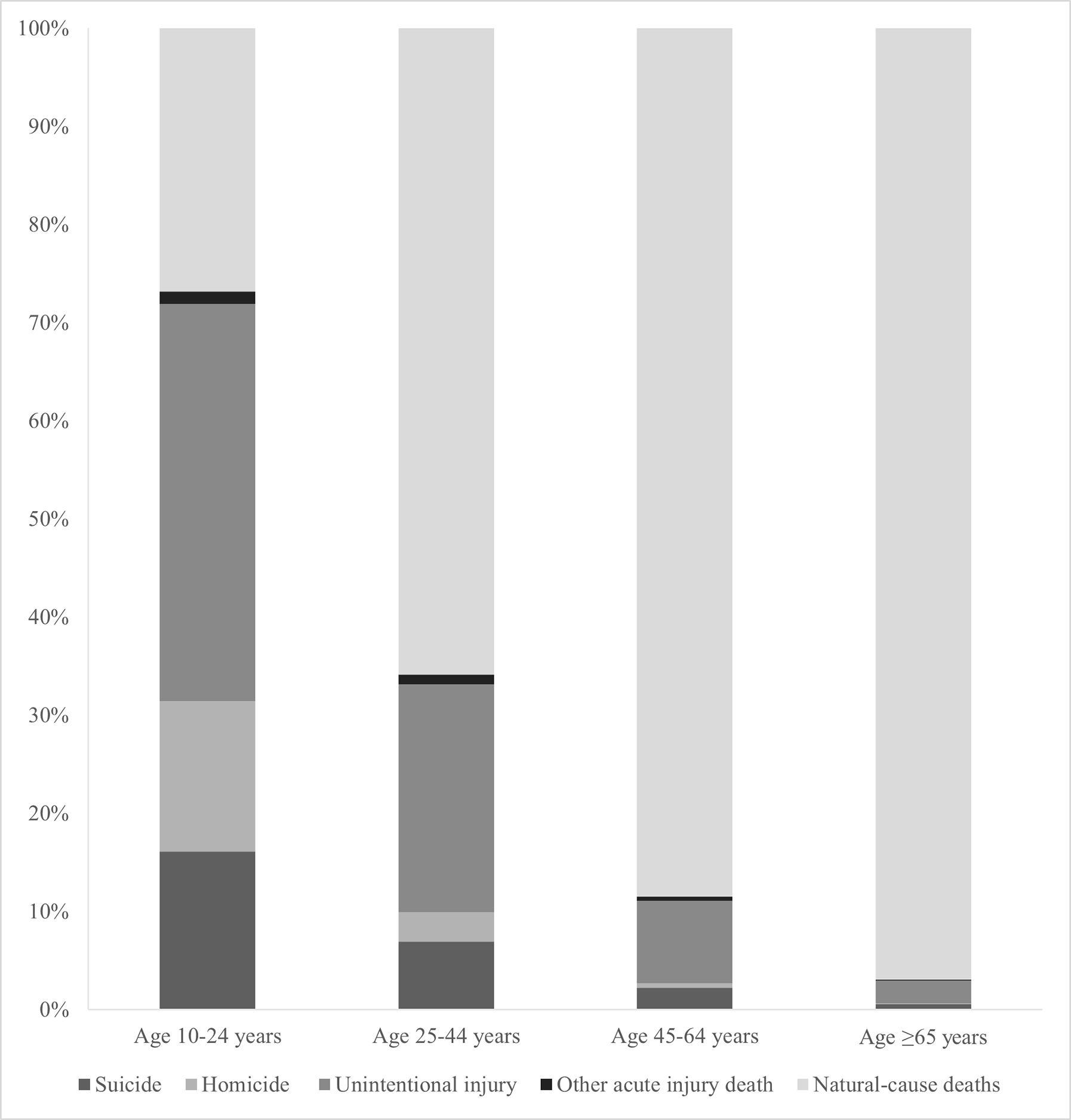
Relative contributions of natural-cause and injury deaths to total mortality among AUD patients, by age group.
The annual rate of any of the acute injury deaths was nearly 50% higher among males than females (708.3 vs. 473.9 per 100,000, respectively), but the relative rankings of each specific cause of death were very similar for both sexes (Table 4). Acute injury deaths accounted for 11.3% and 10.4% of all-cause mortality in males and females, respectively. Male and female patients had relatively similar SMRs for natural-cause and all-cause mortality (male SMRs = 6.4 and 6.5; female SMRs = 6.0 and 6.3, respectively), but the SMR for acute injury mortality among female AUD patients appeared somewhat higher (SMR = 12.2) than that for males (SMR = 7.2).
TABLE 4.
Sex-specific mortality rates from selected acute injury causes of death within one year among emergency department patients presenting with alcohol dependence, abuse, or withdrawal.
| Manner of death | Males | Females | Hazard ratioa | ||
|---|---|---|---|---|---|
|
| |||||
| Deaths, n | Mortality per 100,000 p-y | Deaths, n | Mortality per 100,000 p-y | HR (95% CI) | |
|
| |||||
| Suicide | 395 | 138.5 | 132 | 96.1 | 0.70 (0.57, 0.85) |
| Homicide | 146 | 51.2 | 21 | 15.3 | 0.30 (0.19, 0.47) |
| Unintentional injury deaths | |||||
| Poisoning | 903 | 316.6 | 338 | 246.1 | 0.78 (0.69, 0.88) |
| Motor vehicle crash | 240 | 84.2 | 63 | 45.9 | 0.55 (0.41, 0.72) |
| Fall- or fire-related injury | 264 | 92.6 | 77 | 56.1 | 0.61 (0.47, 0.78) |
| Other acute injury death | 72 | 25.3 | 20 | 14.6 | 0.58 (0.35, 0.95) |
|
| |||||
| All selected acute injury causes | 2,020 | 708.3 | 651 | 473.9 | 0.67 (0.61, 0.73) |
|
| |||||
| Natural-cause death | 15,682 | 5,498.8 | 5,615 | 4,087.5 | 0.75 (0.72, 0.77) |
|
| |||||
| All-cause mortality | 17,803 | 6,242.5 | 6,286 | 4,576.0 | 0.73 (0.71, 0.76) |
Hazard ratio tests are derived from Cox regression models testing the association of being female (males as reference group) with hazard of each cause-specific death. 95% CI = 95% confidence interval.
4. DISCUSSION
This study represents the first population-based examination of acute injury mortality, as well as all-cause mortality, among patients seen in the ED for alcohol use disorders in the U.S. We found that AUD patients had 12-month acute injury mortality rates that were two to 15-fold higher than those in the demographically matched population. Unintentional poisoning and suicide deaths accounted for two-thirds of these acute injury deaths. AUD patients also had substantially elevated risk of natural-cause mortality, leading to an overall mortality rate that was 6.5 times higher than their demographically similar peers. If the excess mortality patterns that we observed in ED patients presenting for care in 2009–2011 extend to more recent cohorts of incident AUD patients, then new clinical interventions and public health planning addressing these risks may be warranted in this patient population.
Our findings build on prior work showing that clinical samples of AUD patients have elevated all-cause and cause-specific mortality compared to non-clinical samples and individuals without AUDs (Askgaard et al., 2020; Hulme et al., 2020; Roerecke and Rehm, 2014, 2013). The all-cause mortality SMR we observed (6.5) was somewhat higher than that estimated in a previous meta-analysis (4.6) (Roerecke and Rehm, 2013), which may reflect changing levels of risk in clinical AUD populations, sample differences, or other factors.
Additional contributions of the current analyses stem from our focus on selected acute injury deaths that have been previously related to AUD and our examination of age and sex differences in AUD patients’ mortality risk. Consistent with estimates from other countries (Britton and McPherson, 2001), we found that these injury deaths contributed particularly strongly to the excess mortality burden in younger patients (those aged 10–24 years), among whom such injury deaths made up nearly three-quarters of total mortality. Acute injury deaths also accounted for one-third of all deaths among AUD patients aged 25–44 years. Although these younger patients’ overall mortality rates were lower than those of other age groups, their very high risk for unintentional poisoning, suicide, and homicide underscores the need for greater use of ED-based, evidence-backed overdose, suicide, and violence prevention approaches (Miller et al., 2017), potentially including assertive interventions (e.g., counselor-initiated home or school-based continuing care) for young patients (Passetti et al., 2016).
In contrast, the acute injury deaths accounted for only 11% of deaths among patients aged 45–64 years (who made up nearly 40% of the cohort), and just 3% among patients aged ≥65 years. In these patients, excess mortality stemmed almost entirely from natural causes of death, especially chronic alcohol-related causes (e.g., alcoholic liver disease, liver and pancreatic cancer, and ischemic heart disease), as other studies have shown (Britton and McPherson, 2001; Roerecke and Rehm, 2014). This distribution underscores the need for post-discharge AUD treatment among midlife and older patients to mitigate their alcohol-related mortality risk. Although we could not examine patients’ access to AUD treatment after discharge, national data suggest that less than 10% of adults aged 50 or over with AUD receive any alcohol treatment, indicating very substantial unmet need (Choi and DiNitto, 2021). Treatment protocols for these patients may also benefit from including integrated management of complex medical conditions, as well as attention to co-morbid psychiatric conditions and occupational, interpersonal, and housing needs (Room et al., 2005; Savic et al., 2017; Wakeman et al., 2019). Among older patients with AUD, fall- and fire-related injuries accounted for nearly half of the injury deaths, calling for greater clinical attention to prevention of these sources of mortality.
Although absolute rates of acute injury mortality, natural-cause mortality, and all-cause mortality were substantially higher among male patients with AUD compared to their female counterparts, the sex-specific SMRs indicated that, relative to their respective general population comparison groups, acute-injury mortality rates might be higher among female than male AUD patients. Male and female SMRs for natural-cause and all-cause mortality were similar. This finding contrasts with results from Roerecke and Rehm’s 2013 meta-analysis, which focused on long-term mortality outcomes and demonstrated higher all-cause SMRs among women compared to men with AUD (Roerecke and Rehm, 2013). The reasons for this difference are not clear, but may be related to our study design, which included patients treated in emergency departments and focused on short-term mortality outcomes — neither of which were included in the Roerecke & Rehm meta-analysis. However, we caution against over-interpretation of these findings, as SMRs in different groups are not directly comparable (Rothman et al., 2008). Within each sex-specific group, the relative contributions of different acute injury mortality causes were approximately the same — e.g., poisoning deaths accounted for approximately 50% of all acute injury deaths in each group, while suicide accounted for 20% and fall/fire injuries for around 12%.
Although we observed a slight disproportionate increase in AUD patients’ mortality risk in the first six months following discharge, rates of mortality remained persistently elevated over the 12-month follow-up. This finding reinforces the conclusion that ED patients with AUD diagnoses comprise a population at persistently elevated risk for mortality, emphasizing the need to connect them with sustained clinical care. However, many patients with alcohol use disorders face challenges, such as long wait times to enter residential treatment facilities, when trying to access addiction specialists (Oleski et al., 2010; Parkman et al., 2017a; Williams et al., 2018). ED patients who report themselves willing to receive post-discharge interventions often do not make it to their first post-discharge appointments (Parkman et al., 2017b; Simioni et al., 2015). Outpatient addiction services with fewer barriers to admission and greater accessibility may facilitate timely entry into treatment and reductions in hazardous drinking (Wiercigroch et al., 2020).
4.1. Limitations
Our study had several important advantages, including a large population-based cohort of ED patients, from the largest and most diverse U.S. state; comprehensive coding of external cause of injury, which is not available in all states; and inclusion of mortality outcomes from validated high-quality registers, which are also not available in all states. However, several limitations should be considered when interpreting the results. The study period and context comprised California in the years 2009–2012; as such, the results may not generalize to other periods, to the entire United States, or outside the US. This is particularly true given the increases in problematic alcohol use observed within the US over the past 10 years; future studies should seek to replicate and extend our analyses. Due to sample size and data use agreement restrictions, we could not examine smaller age groupings (e.g., for adolescents), which limits our findings’ clinical relevance for age-specific patient populations. Mortality data for ED patients who died outside of California were not available for this study; we expect this artifact resulted in a slight downward bias on the absolute mortality rates calculated for the ED patients. We could not assess alcohol involvement at the index visit through breath tests, blood alcohol content, or other means other than diagnostic coding, which may miss many ED patients with alcohol use disorders. The validity of these clinical diagnoses in ED administrative data is uncertain, given that active alcohol intoxication can complicate ED clinical assessments by impairing responses to clinical questions. Furthermore, several other potentially relevant patient characteristics were not examined, including drug use and psychiatric disorder comorbidity, history of repeated ED visits for AUD, and current chronic disease conditions; also, our estimate of injury deaths is conservative, as it does not include undetermined-intent injury deaths, nor does it include some non-drug-related poisoning deaths. Finally, although our mortality analysis focused on selected causes of acute injury that previous research indicates are partially attributable to AUD (Centers for Disease Control and Prevention, 2021), it was not possible to attribute the individual observed deaths directly to alcohol use.
4.2. Conclusion
Emergency department patients with recognized alcohol use disorders comprise a population at persistently elevated risk for mortality. Age-related AUD patient differences in the most common causes of death, including drug overdose and suicide, can inform the structure of future clinical interventions. These findings underscore the potential value of ED-based clinical and public health prevention efforts aimed at reducing mortality risks in this clinical population.
Supplementary Material
Funding sources:
This project was funded through National Institutes of Health grant R15 MH113108–01 to S.G.M. The sponsor had no role in the study design; collection, analysis, or interpretation of data; writing of the report, or decision to submit the article for publication. The views expressed here are those of the authors, and not necessarily those of the National Institute of Mental Health, Department of Health and Human Services, or the federal government. No financial disclosures were reported by the authors of this paper.
Footnotes
Conflicts of interest: The authors report no potential conflicts of interest.
References
- Abellera J, Annest JL, Conn JM, Kohn M, 2005. How states are collecting and using cause of injury data: 2004 update to the 1997 report. Atlanta, GA. [Google Scholar]
- Askgaard G, Leon DA, Deleuran T, Tolstrup JS, 2020. Hospital admissions and mortality in the 15 years after a first-time hospital contact with an alcohol problem: A prospective cohort study using the entire Danish population. Int. J. Epidemiol. 49, 94–102. 10.1093/ije/dyz159 [DOI] [PubMed] [Google Scholar]
- Barata IA, Shandro J, Montgomery M, Polansky R, Sachs CJ, Duber HC, Weaver L, Heins A, Owen HS, Josephson EB, 2017. Effectiveness of SBIRT for alcohol use disorders in the emergency department: A systematic review. West. J. Emerg. Med. 18, 1143–1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betz ME, Wintersteen M, Boudreaux ED, Brown G, Capoccia L, Currier G, Goldstein J, King C, Manton A, Stanley B, Moutier C, Harkavy-Friedman J, 2016. Reducing suicide risk: Challenges and opportunities in the emergency department. Ann. Emerg. Med. 68, 758–765. 10.1016/j.annemergmed.2016.05.030 [DOI] [PubMed] [Google Scholar]
- Britton A, McPherson K, 2001. Mortality in England and Wales attributable to current alcohol consumption. J. Epidemiol. Community Health 55, 383–388. 10.1136/jech.55.6.383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, 2021. Alcohol-Related ICD Codes [WWW Document]. URL https://www.cdc.gov/alcohol/ardi/alcohol-related-icd-codes.html (accessed 8.3.21).
- Centers for Disease Control and Prevention (National Center for Health Statistics), 2017. Compressed Mortality File 1999–2016 on CDC WONDER Online Database [WWW Document]. URL https://wonder.cdc.gov/cmf-icd10.html (accessed 9.20.02). [Google Scholar]
- Choi NG, DiNitto DM, 2021. Alcohol use disorder and treatment receipt among individuals aged 50 years and older: Other substance use and psychiatric correlates. J. Subst. Abuse Treat. 131. 10.1016/j.jsat.2021.108445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elixhauser A, Steiner C, Palmer L, 2014. Clinical classifications software (CCS). Rockville, MD. [Google Scholar]
- Fleming EA, Gmel G, Bady P, Yersin B, Givel J-C, Brown D, Daeppen J-B, 2007. At-risk drinking and drug use among patients seeking care in an emergency department. J. Stud. Alcohol Drugs 68, 28–35. 10.15288/jsad.2007.68.28 [DOI] [PubMed] [Google Scholar]
- Grucza RA, Sher KJ, Kerr WC, Krauss MJ, Lui CK, McDowell YE, Hartz S, Virdi G, Bierut LJ, 2018. Trends in adult alcohol use and binge drinking in the early 21st-century United States: A meta-analysis of 6 national survey series. Alcohol. Clin. Exp. Res. 42, 1939–1950. 10.1111/acer.13859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawk K, D’Onofrio G, 2018. Emergency department screening and interventions for substance use disorders. Addict. Sci. Clin. Pract. 13, 1–6. 10.1186/s13722-018-0117-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houry D, Cunningham RM, Hankin A, James T, Bernstein E, Hargarten S, 2009. Violence prevention in the emergency department: Future research priorities. Acad. Emerg. Med. 16, 1089–1095. 10.1111/j.1553-2712.2009.00544.x [DOI] [PubMed] [Google Scholar]
- Hulme J, Sheikh H, Xie E, Gatov E, Nagamuthu C, Kurdyak P, 2020. Mortality among patients with frequent emergency department use for alcohol-related reasons in Ontario: A population-based cohort study. Can. Med. Assoc. J. 192, E1522–E1531. 10.1503/cmaj.191730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein LR, Martel ML, Driver BE, Reing M, Cole JB, 2018. Emergency department frequent users for acute alcohol intoxication. West. J. Emerg. Med. 19, 398–402. 10.5811/westjem.2017.10.35052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landy MSH, Davey CJ, Quintero D, Pecora A, McShane KE, 2016. A systematic review on the effectiveness of brief interventions for alcohol misuse among adults in emergency departments. J. Subst. Abuse Treat. 61, 1–12. [DOI] [PubMed] [Google Scholar]
- Li G, Keyl PM, Rothman R, Chanmugam A, Kelen GD, 1998. Epidemiology of alcohol-related emergency department visits. Acad. Emerg. Med. 5, 788–795. 10.1111/j.1553-2712.1998.tb02505.x [DOI] [PubMed] [Google Scholar]
- McDonald AJ, Wang N, Camargo CA, 2004. US emergency department visits for alcohol-related diseases and injuries between 1992 and 2000. Arch. Intern. Med. 164, 531–537. [DOI] [PubMed] [Google Scholar]
- Miller IW, Camargo CA, Arias SA, Sullivan AF, Allen MH, Goldstein AB, Manton AP, Espinola JA, Jones R, Hasegawa K, Boudreaux ED, 2017. Suicide prevention in an emergency department population: The ED-SAFE study. JAMA Psychiatry 74, 563–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oleski J, Mota N, Cox BJ, Sareen J, 2010. Perceived need for care, help seeking, and perceived barriers to care for alcohol use disorders in a national sample. Psychiatr. Serv. 61, 1223–1231. 10.1176/ps.2010.61.12.1223 [DOI] [PubMed] [Google Scholar]
- Olfson M, Wall M, Wang S, Crystal S, Gerhard T, Blanco C, 2017. Suicide following deliberate self-harm. Am. J. Psychiatry 174, 765–774. 10.1176/appi.ajp.2017.16111288 [DOI] [PubMed] [Google Scholar]
- Parkman T, Neale J, Day E, Drummond C, 2017a. How do people who frequently attend emergency departments for alcohol-related reasons use, view, and experience specialist addiction services? Subst. Use Misuse 52, 1460–1468. 10.1080/10826084.2017.1285314 [DOI] [PubMed] [Google Scholar]
- Parkman T, Neale J, Day E, Drummond C, 2017b. Qualitative exploration of why people repeatedly attend emergency departments for alcohol-related reasons. BMC Health Serv. Res. 17, 1–9. 10.1186/s12913-017-2091-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passetti LL, Godley MD, Kaminer Y, 2016. Continuing care for adolescents in treatment for substance use disorders. Child Adolesc. Psychiatr. Clin. N. Am. 25, 669–684. 10.1016/j.chc.2016.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roerecke M, Rehm J, 2014. Cause-specific mortality risk in alcohol use disorder treatment patients: A systematic review and meta-analysis. Int. J. Epidemiol. 43, 906–919. 10.1093/ije/dyu018 [DOI] [PubMed] [Google Scholar]
- Roerecke M, Rehm J, 2013. Alcohol use disorders and mortality: A systematic review and meta-analysis. Addiction 108, 1562–1578. 10.1111/add.12231 [DOI] [PubMed] [Google Scholar]
- Room R, Babor T, Rehm J, 2005. Alcohol and public health. Lancet 365, 519–530. 10.1016/s0140-6736(05)66371-4 [DOI] [PubMed] [Google Scholar]
- Rothman KJ, Greenland S, Lash TL, 2008. Modern Epidemiology, 3rd editio. ed. Wolters Kluwer Health/Lippincott Williams & Wilkins, Philadelphia, PA. [Google Scholar]
- Sanjuan PM, Rice SL, Witkiewitz K, Mandler RN, Crandall C, Bogenschutz MP, 2014. Alcohol, tobacco, and drug use among emergency department patients. Drug Alcohol Depend. 138, 32–38. 10.1016/j.drugalcdep.2014.01.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savic M, Best D, Manning V, Lubman DI, 2017. Strategies to facilitate integrated care for people with alcohol and other drug problems: A systematic review. Subst. Abus. Treat. Prev. Policy 12, 1–12. 10.1186/s13011-017-0104-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shmulewitz D, Aharonovich E, Witkiewitz K, Anton RF, Kranzler HR, Scodes J, Mann KF, Wall MM, Hasin D, 2021. The World Health Organization risk drinking levels measure of alcohol consumption: Prevalence and health correlates in nationally representative surveys of U.S. adults, 2001–2002 and 2012–2013. Am. J. Psychiatry. 10.1176/appi.ajp.2020.20050610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simioni N, Rolland B, Cottencin O, 2015. Interventions for increasing alcohol treatment utilization among patients with alcohol use disorders from emergency departments: A systematic review. J. Subst. Abuse Treat. 58, 6–15. 10.1016/j.jsat.2015.06.003 [DOI] [PubMed] [Google Scholar]
- Spillane S, Shiels MS, Best AF, Haozous EA, Withrow DR, Chen Y, Berrington De González A, Freedman ND, 2020. Trends in alcohol-induced deaths in the United States, 2000–2016. JAMA Netw. Open 3, 1–15. 10.1001/jamanetworkopen.2019.21451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timko C, Below M, Vittorio L, Taylor E, Chang G, Lash S, Festin FED, Brief D, 2019. Randomized controlled trial of enhanced telephone monitoring with detoxification patients: 3- and 6-month outcomes. J. Subst. Abuse Treat. 99, 24–31. 10.1016/j.jsat.2018.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (HHS) Office of the Surgeon General, National Action Alliance for Suicide Prevention, 2012. 2012 National Strategy for Suicide Prevention: Goals and Objectives for Action. [PubMed] [Google Scholar]
- Wakeman SE, Rigotti NA, Chang Y, Herman GE, Erwin A, Regan S, Metlay JP, 2019. Effect of integrating substance use disorder treatment into primary care on inpatient and emergency department utilization. J. Gen. Intern. Med. 34, 871–877. 10.1007/s11606-018-4807-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- White AM, Castle IJP, Hingson RW, Powell PA, 2020. Using death certificates to explore changes in alcohol-related mortality in the United States, 1999 to 2017. Alcohol. Clin. Exp. Res. 44, 178–187. 10.1111/acer.14239 [DOI] [PubMed] [Google Scholar]
- White AM, Slater ME, Ng G, Hingson R, Breslow R, 2018. Trends in alcohol-related emergency department visits in the United States: Results from the Nationwide Emergency Department Sample, 2006 to 2014. Alcohol. Clin. Exp. Res. 42, 352–359. 10.1111/acer.13559 [DOI] [PubMed] [Google Scholar]
- Wiercigroch D, Sheikh H, Hulme J, 2020. A rapid access to addiction medicine clinic facilitates treatment of substance use disorder and reduces substance use. Subst. Abuse Treat. Prev. Policy 15, 4. 10.1186/s13011-019-0250-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams EC, Achtmeyer CE, Young JP, Berger D, Curran G, Bradley KA, Richards J, Siegel MB, Ludman EJ, Lapham GT, Forehand M, Harris AHS, 2018. Barriers to and facilitators of alcohol use disorder pharmacotherapy in primary care: A qualitative study in five VA clinics. J. Gen. Intern. Med. 33, 258–267. 10.1007/s11606-017-4202-z [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


