Abstract
Many robotic procedures require active participation by assistants. Most prior work on assistants’ effect on outcomes has been limited in procedural focus and scope, with studies reporting differing results. Knowing how assistant experience affects operating room time could inform operating room case scheduling and provide an impetus for additional assistant training. As such, this retrospective cohort study aimed to determine the association between assistant experience and operating room time for 2291 robotic-assisted operations performed from 2016 to 2022 at our institution. Linear regression showed a significant association between the presence of a junior resident and increased case length differential with an increase of 26.9 min (p = 0.01). There were no significant associations between the presence of a senior resident (p = 0.52), presence of a fellow (p = 0.20), or presence of a physician assistant (p = 0.43) and case length differential. The finding of increased operating room time in the presence of a junior resident during robotic cases supports consideration of the adoption of formal assistant training programs for residents to improve efficiency.
Keywords: Robotic assistance, Bedside assistance, Learning curve, Resident training
Introduction
Educational interventions in robotic surgery often focus on the surgeon at the console. However, many robotic procedures require active participation by additional surgical team members. Assistants can be junior residents, senior residents, fellows, physician assistants (PAs), and other members of the operative team [1]. In some cases, the role of the assistant is minimal and limited to bedside instrument exchange, camera cleaning, and port site closure. In other operations, the assistant must provide adept laparoscopic assistance and understand the flow and sequence of the operation at an advanced level [2]. The assistant’s experience—whether limited as a junior resident or extensive as a fellow—has been posited as important to the success of robotic surgery [3].
Bedside assistance is frequently described as a stepping stone on the path to console surgeon [4–6]. Prior work has acknowledged the multiple skills required as an assistant, and learning curve analysis has suggested that 10–36 cases are required for proficient bedside assistance [2, 7]. However, the actual training of assistants varies [3, 6]. To expedite assistant education, some authors have piloted courses focusing on a combination of didactic and psychomotor training [8, 9]. Another simulation-based report found that an augmented reality intervention with 3D vision decreased the time and errors in performing complex bedside tasks [10]. To provide feedback and assess bedside assistants, one group developed validity evidence for a modified Objective Structured Assessment of Technical Skills (OSATS) [11]. Nonetheless, there is no consensus on a standardized assistant training or assessment program; thus, the experience among assistants differs widely [8].
The effect of operative assistant experience on outcomes has been widely studied in many settings, with different results by procedure, institution, and publication [3, 12–23]. Most of the existing literature on the effect of the assistant in robotic surgery is limited to robotic-assisted prostatectomy and nephrectomy. Given the small samples, limited scopes, and heterogeneous results of prior studies, the importance of experience for assistants remains an unanswered question.
As such, this study aimed to determine the association between assistant experience and operating room time for all robotic-assisted operations performed at our institution. We hypothesized that the presence of more experienced assistants would be associated with shorter operating room time. This information could inform operating room case scheduling and provide an impetus for additional assistant training.
Methods
Design
This was a correlational study assessing predictor variables’ association with the outcome variable of case length differential, which was defined as the difference between the actual operating room (OR) time and the scheduled OR time, including surgical and anesthesia time. Predictor variables were classified as patient related or surgical team related. Patient-related predictor variables comprised patient body mass index (BMI), patient pre-operative opioid use, patient smoking status, and patient American Society of Anesthesiologists (ASA) physical status classification. These patient-related predictor variables were chosen given that prior work has also assessed their possible contribution to peri-operative and OR time [24–27]. Patient-related predictor variable data were not available for all cases. Surgical team-related predictor variables included the number of junior residents, the number of senior residents, the number of fellows, and PA presence. Junior residents were defined as post-graduate year 1 and 2, while senior residents were defined as post-graduate year 3 and greater. Surgical team-related predictor variable data were available for every case. The outcome variable was case length differential. The single outcome variable was pre-specified prior to initiating the analysis.
Setting
This study was conducted at a single tertiary-level academic medical center. At this medical center, the assistant may be a resident, fellow, physician assistant, or there may be no assistant present. Experience among assistants varies significantly with no standardized assistant requirements. Surgical technologists do not dock the robot or exchange instruments at our institution.
Data collection
Data were collected retrospectively from the electronic medical record and operating room archives. All patients who underwent a Da Vinci robotic-assisted operation from January, 2016 to August, 2022 were included (Intuitive Surgical. Sunnyvale, CA, USA). Data included date of surgery, procedure, primary surgeon, all surgeons, PA presence, scheduled start time, scheduled end time, actual start time, actual end time, patient demographics, patient BMI, patient pre-operative opioid use, patient smoking status, and patient ASA physical status classification. All surgeons were subclassified as junior residents, senior residents, fellows, or attendings.
Data analysis
Descriptive data were generated. Two linear regression was performed: one to assess the impact of the patient-related predictor variables on the outcome variable of case length differential and a second to assess the impact of surgical team-related predictor variables on the outcome variable of case length differential. Stata/IC V.16.1 for Mac (StataCorp. College Station, TX, USA) was used for data analysis.
Ethical approval
This study was approved by our Institutional Review Board (IRB22-37360).
Results
During the study period, 2291 robotic-assisted cases were performed and included in the study. Robotic-assisted prostatectomy was the most commonly performed procedure (28.9%; 661 of 2291), followed by robotic-assisted hysterectomy (13.1%; 301 of 2291), and robotic-assisted inguinal hernia repair (9.9%; 227 of 2291).
Of the 2291 cases, 751 contained data on patient-related predictor variables. Among those cases, mean BMI was 26.9 (SD 9.0) and the median ASA physical status classification was 2 (IQR 2–3). Almost all patients (98.1%) were non-smokers and most patients (89.6%) were not using opioids prior to surgery. All 2291 cases contained data on surgical team-related predictor variables. Of these, 1094 cases (47.8%) involved trainees and 126 cases (5.5%) involved PAs (Table 1). One hundred forty-six cases (6.4%) involved more than one trainee. Median actual OR time was 407 min (IQR 324–502). Median scheduled OR time was 400 min (IQR 335–470). The median case length differential was 8 min (IQR − 42 to 81).
Table 1.
Team member involvement in cases
| Case type | Total number of cases n |
Junior resident present n (%) |
Senior resident present n (%) |
Fellow present n (%) |
Physician assistant present n (%) |
Multiple trainees present n (%) |
|---|---|---|---|---|---|---|
| All cases | 2291 | 138 (6) | 336 (15) | 674 (29) | 126 (6) | 146 (6) |
| Prostatectomy | 661 | 1 (0) | 28 (4) | 268 (41) | 21 (3) | 16 (2) |
| Hysterectomy | 301 | 11 (4) | 91 (30) | 79 (26) | 33 (11) | 33 (11) |
| Inguinal hernia repair | 227 | 48 (21) | 42 (19) | 32 (14) | 5 (2) | 16 (7) |
Multiple types of team members were involved in cases, which varied among the three most commonly performed cases
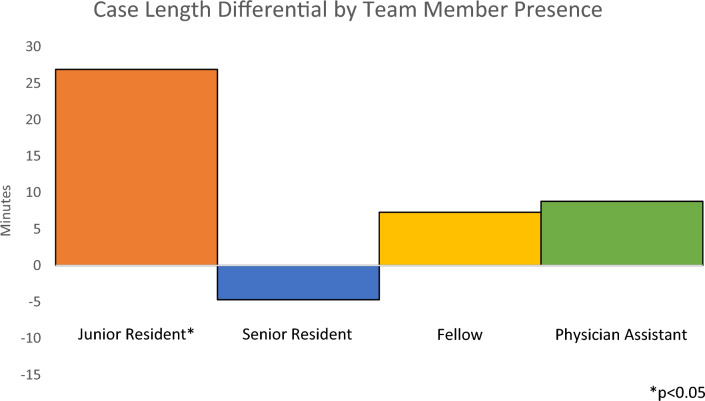
Linear regressions were performed to assess the impact of the patient-related and surgical team-related predictor variables on the outcome variable of case length differential (Table 2). Regression assessing the impact of patient-related predictor variables showed no significant association between BMI (p = 0.98), ASA physical status classification (p = 0.26), smoking (p = 0.34), or pre-operative opioid use (p = 0.29) and case length differential. Regression assessing the impact of surgical team-related predictor variables showed a significant association between the presence of a junior resident and increased case length differential with an increase of 26.9 min (p = 0.01) (Table 3). There was no significant association between the presence of a senior resident (p = 0.52), presence of a fellow (p = 0.20), or presence of a PA (p = 0.43) and case length differential (Fig. 1).
Table 2.
Association between patient-related predictor variables and outcome variable
| Variable | Coefficient | Standard error | t-statistic | p value |
|---|---|---|---|---|
| BMI | − 0.01 | 0.52 | − 0.02 | 0.98 |
| ASA | 8.95 | 7.96 | 1.12 | 0.26 |
| Smoking | 31.99 | 33.49 | 0.96 | 0.34 |
| Pre-operative opioid use | 15.89 | 15.07 | 1.05 | 0.29 |
| R-squared | 0.0052 | |||
| Adjusted R-squared | − 0.0001 | |||
No patient-related predictor variables were significantly associated with the outcome variable of case length differential (actual minus scheduled operating room time) by linear regression
BMI body mass index, ASA American Society of Anesthesiologists physical status classification
Table 3.
Association between surgical team-related predictor variables and outcome variable
| Variable | Coefficient | Standard error | t-statistic | p value |
|---|---|---|---|---|
| Presence of junior resident | 26.94 | 10.64 | 2.53 | 0.01 |
| Presence of senior resident | − 4.65 | 7.27 | − 0.64 | 0.52 |
| Presence of fellow | 7.31 | 5.69 | 1.29 | 0.20 |
| Presence of physician assistant | 8.76 | 11.06 | 0.79 | 0.43 |
| R-squared | 0.0038 | |||
| Adjusted R-squared | 0.0020 | |||
The presence of a junior resident was significantly associated with the outcome variable of case length differential (actual minus scheduled operating room time) by linear regression
Fig. 1.
Case length differential by team member presence. The presence of a junior resident was significantly associated (p = 0.01) with increased case length differential (actual minus scheduled operating room time) during robotic-assisted procedures
Linear regression assessing the impact of surgical team-related predictor variables was repeated for cases without any missing patient-related predictor variables, yielding similar results. This regression was also repeated after removing cases in which more than one trainee was present, given that the role of the bedside assistant was less clear in such cases. This repeated analysis also yielded similar results.
Discussion
In summary, this correlational study demonstrated that the presence of a junior resident during a robotic-assisted procedure was associated with increased OR time by approximately 27 min for 2291 robotic cases at a single institution from 2016 to 2022. The presence of other team members was not significantly associated with changes in OR time.
These findings build on prior work that has also evaluated the experience of the assistant in robotic surgery. Indeed, one previous study assessed the effect of assistant experience in 170 cases of robotic-assisted radical prostatectomy and concluded that an expert assistant (i.e., assistants who had completed formal training) was associated with shorter length of stay, less estimated blood loss, and lower positive margin rate [3]. Another study analyzed case length for 222 assistants in urology by comparing their early and late cases, and found a modest decrease in case length with experience [19]. In contrast, three other studies in prostatectomy and nephrectomy involving a combined 636 patients showed no effect on patient outcomes or case length based on the experience of the assistant [18, 20, 21]. Studies of the impact of assistants in 191 robotic-assisted thyroid operations and 105 robotic-assisted Nissen fundoplications came to conflicting results [22, 23]. Our work adds to this literature with a much larger sample size of real-world, diverse cases in multiple specialties with various types of assistants.
The rapid adoption of robotic surgery has required shifting roles and educational changes, with a consensus assistant training pathway yet to materialize. Unfortunately, assistants frequently lack significant experience and learn in unstructured ways [3, 18, 28]. However, studies repeatedly show that formal training with simulation improves operative performance and efficiency in surgery [29]. As such, our finding of increased OR time in the presence of a junior resident during robotic cases provides additional support for the adoption of formal assistant training programs to improve efficiency. Structured education for junior residents may be a mechanism by which to decrease the OR time discrepancy that we observed. Future studies should assess the impact of such formal training on case length in diverse robotic settings. Additional research could investigate the effect of participant role on more patient-centered outcomes, such as length of hospital stay or complications.
This study has a number of limitations. Most notably, this is a retrospective review and we cannot be certain of the responsibilities of participants in each case. While it is very likely that the non-attending member of the operating team acted as the assistant, it is possible that this did not occur in certain instances. However, repeating the analysis for cases with more role uncertainty (i.e., in which more than one trainee was present and thus one trainee may have been at the console) yielded similar results. It is also possible that attendings might request a dedicated assistant for cases they expect to be complex, thus confounding analysis of the effect of another participant. However, our finding with regard to case length differential was limited to junior resident presence. Furthermore, we evaluated a very diverse collection of procedures, and while this expands on previously reported studies that focused on small numbers of homogenous cases, this may introduce uncontrolled variables into the analysis. Clearly, many other factors play large roles in case length differential. Nonetheless, it was notable that the increased OR time associated with a junior resident of about 27 min was substantially greater than the median case length differential of 8 min. Finally, this is a single institution study at a large academic medical center, and the experiences of participants may differ elsewhere.
Overall, we found that the presence of a junior resident during robotic-assisted procedures was associated with increased OR time. Focused education for robotic assistant skills may be warranted for junior trainees to improve their performance and efficiency during robotic cases.
Acknowledgements
The authors would like to acknowledge the UCSF Robotics Committee for their assistance with data aggregation. The authors would also like to thank Gillian Earnest from the UCSF Clinical & Translational Science Institute for data support.
Author contributions
All authors contributed to the study conception, design, and analysis. The first draft of the manuscript was prepared by Riley Brian. All authors commented on versions of the manuscript and approved the final manuscript.
Funding
This project was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF-CTSI Grant number UL1 TR001872. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. Riley Brian receives funding for his research through the Intuitive-UCSF Simulation-Based Surgical Education Research Fellowship. Daniel Oh is part-time employed by Intuitive Surgical as a medical advisor. Kelli Ifuku receives funding for her research through the National Cancer Institute (NCI), NIH, Grant no. T32CA25107003. Ankit Sarin has consulted for early robotic companies including Johnson & Johnson, Noah Medical, and Neptune Medical.
Data availability
Data are available upon reasonable request.
Declarations
Conflict of interest
Riley Brian receives funding for his research through the Intuitive-UCSF Simulation-Based Surgical Education Research Fellowship. Daniel Oh is part-time employed by Intuitive Surgical as a medical advisor. Kelli Ifuku receives funding for her research through the National Cancer Institute (NCI), NIH, Grant Number T32CA25107003. Ankit Sarin has consulted for early robotic companies including Johnson & Johnson, Noah Medical, and Neptune Medical. Patricia O’Sullivan and Hueylan Chern declare that they have no financial interests.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the University of California, San Francisco Institutional Review Board (IRB22-37360).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Yuh B. The bedside assistant in robotic surgery—keys to success. Urol Nurs. 2013;33(1):29–32. doi: 10.7257/1053-816X.2013.33.1.29. [DOI] [PubMed] [Google Scholar]
- 2.Britton CR, Francis I, Tay LJ, Krishnamoothy B. The role of the bedside assistant in robot-assisted surgery: a critical synthesis. J Perioper Pract. 2022;32(9):208–225. doi: 10.1177/17504589221094136. [DOI] [PubMed] [Google Scholar]
- 3.Garbens A, Lay AH, Steinberg RL, Gahan JC. Experienced bedside-assistants improve operative outcomes for surgeons early in their learning curve for robot assisted laparoscopic radical prostatectomy. J Robot Surg. 2021;15(4):619–626. doi: 10.1007/s11701-020-01146-8. [DOI] [PubMed] [Google Scholar]
- 4.Sridhar AN, Briggs TP, Kelly JD, Nathan S. Training in robotic surgery—an overview. Curr Urol Rep. 2017;18(8):58. doi: 10.1007/s11934-017-0710-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cimen HI, Atik YT, Gul D, Uysal B, Balbay MD. Serving as a bedside surgeon before performing robotic radical prostatectomy improves surgical outcomes. Int Braz J Urol. 2019;45(6):1122–1128. doi: 10.1590/s1677-5538.ibju.2019.0330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lagrange F, Fiard G, Larose C, Eschwege P, Hubert J. Role and training of the bedside surgeon in robotic surgery: a survey among French urologists-in-training. Res Rep Urol. 2022;14:17–22. doi: 10.2147/RRU.S344369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yamada K, Kogure N, Ojima H (2021) Learning curve for robotic bedside assistance for rectal cancer: application of the cumulative sum method. J Robot Surg [DOI] [PubMed]
- 8.Collins JM, Walsh DS, Hudson J, Henderson S, Thompson J, Zychowicz M (2021) Implementation of a standardized robotic assistant surgical training curriculum. J Robot Surg [DOI] [PMC free article] [PubMed]
- 9.Barnes KE, Brian R, Greenberg AL, Watanaskul S, Kim EK, O’Sullivan PS, et al. Beyond watching: harnessing laparoscopy to increase medical students’ engagement with robotic procedures. Am J Surg. 2023;S0002–9610(23):00092–102. doi: 10.1016/j.amjsurg.2023.02.024. [DOI] [PubMed] [Google Scholar]
- 10.Stewart CL, Fong A, Payyavula G, DiMaio S, Lafaro K, Tallmon K et al (2021) Study on augmented reality for robotic surgery bedside assistants. J Robot Surg [DOI] [PubMed]
- 11.Yu N, Saadat H, Finelli A, Lee JY, Singal RK, Grantcharov TP, et al. Quantifying the “Assistant Effect” in robotic-assisted radical prostatectomy (RARP): measures of technical performance. J Surg Res. 2021;260:307–314. doi: 10.1016/j.jss.2020.11.037. [DOI] [PubMed] [Google Scholar]
- 12.Stevens A, Meier J, Balentine C. Resident involvement in inguinal hernia repair is safe but associated with increased operative time. J Surg Res. 2022;276:305–313. doi: 10.1016/j.jss.2022.03.002. [DOI] [PubMed] [Google Scholar]
- 13.Alexander B, Watson JB, Chandler K, Sowers M, McGwin G, Maffulli N, et al. Impact of resident involvement on complication rates in revision total knee arthroplasty. J Taibah Univ Med Sci. 2022;17(6):969–975. doi: 10.1016/j.jtumed.2022.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beaulieu-Jones BR, de Geus SWL, Rasic G, Woods AP, Papageorge MV, Sachs TE. A propensity score matching analysis: impact of senior resident versus fellow participation on outcomes of complex surgical oncology. Surg Oncol. 2023;9(48):101925. doi: 10.1016/j.suronc.2023.101925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gordon AM, Malik AT. Total elbow arthroplasty cases involving orthopaedic residents do not affect short-term postoperative complications. Shoulder Elbow. 2023;15(1):65–73. doi: 10.1177/17585732211034455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Steiger K, Edwards MA, Spaulding A, Borkar S, Evans M, Farres H, et al. Trainee effect on procedural efficiency is limited in vascular surgery operations. Ann Vasc Surg. 2023;90:33–38. doi: 10.1016/j.avsg.2022.10.016. [DOI] [PubMed] [Google Scholar]
- 17.Glass Clark S, Melnyk AI, Bonidie M, Giugale L, Bradley MS. Operative time for minimally invasive sacrocolpopexy: comparison of conventional laparoscopy versus robotic platform. J Minim Invasive Gynecol. 2022;29(9):1063–1067. doi: 10.1016/j.jmig.2022.05.013. [DOI] [PubMed] [Google Scholar]
- 18.Potretzke AM, Knight BA, Brockman JA, Vetter J, Figenshau RS, Bhayani SB, et al. The role of the assistant during robot-assisted partial nephrectomy: does experience matter? J Robot Surg. 2016;10(2):129–134. doi: 10.1007/s11701-016-0582-z. [DOI] [PubMed] [Google Scholar]
- 19.Nayyar R, Yadav S, Singh P, Dogra P. Impact of assistant surgeon on outcomes in robotic surgery. Indian J Urol. 2016;32(3):204. doi: 10.4103/0970-1591.185095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abu-Ghanem Y, Erlich T, Ramon J, Dotan Z, Zilberman DE. Robot assisted laparoscopic radical prostatectomy: assistant’s seniority has no influence on perioperative course. J Robotic Surg. 2017;11(3):305–309. doi: 10.1007/s11701-016-0655-z. [DOI] [PubMed] [Google Scholar]
- 21.Mangano MS, Lamon C, Beniamin F, De Gobbi A, Ciaccia M, Maccatrozzo L. The role of bedside assistant during robot assisted radical prostatectomy: is more experience better? Analysis on perioperative and clinical outcomes. Urologia. 2021;88(1):9–13. doi: 10.1177/0391560320951085. [DOI] [PubMed] [Google Scholar]
- 22.Moore MD, Afaneh C, Gray KD, Panjwani S, Fahey TJ, Pomp A, et al. The impact of the robotic platform on assistant variability in complex gastrointestinal surgery. J Surg Res. 2017;219:98–102. doi: 10.1016/j.jss.2017.05.127. [DOI] [PubMed] [Google Scholar]
- 23.Kwon H. Impact of bedside assistant on outcomes of robotic thyroid surgery: a STROBE-compliant retrospective case–control study. Medicine (Baltimore) 2020;99(36):e22133. doi: 10.1097/MD.0000000000022133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pappada SM, Papadimos TJ, Khuder S, Mack ST, Beachy PZ, Casabianca AB. Contributing factors to operating room delays identified from an electronic health record: a retrospective study. Minervini G, editor. Anesthesiol Res Pract. 2022;2022:1–7. doi: 10.1155/2022/8635454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Miller H, Bush KM, Betances A, Kota R, Wu S, De Leo N, et al. Effect of daily dosage of morphine milligram equivalents on free flap complications: a single-institution retrospective study. J Plast Reconstr Aesth Surg. 2021;74(10):2486–2494. doi: 10.1016/j.bjps.2021.03.028. [DOI] [PubMed] [Google Scholar]
- 26.St Julien JB, Aldrich MC, Sheng S, Deppen SA, Burfeind WR, Putnam JB, et al. Obesity increases operating room time for lobectomy in the society of thoracic surgeons database. Ann Thorac Surg. 2012;94(6):1841–1847. doi: 10.1016/j.athoracsur.2012.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gedaly R, McHugh PP, Johnston TD, Jeon H, Ranjan D, Davenport DL. Obesity, diabetes, and smoking are important determinants of resource utilization in liver resection: a multicenter analysis of 1029 patients. Ann Surg. 2009;249(3):414–419. doi: 10.1097/SLA.0b013e31819a032d. [DOI] [PubMed] [Google Scholar]
- 28.Beane M. Shadow learning: building robotic surgical skill when approved means fail. Adm Sci Q. 2019;64(1):87–123. doi: 10.1177/0001839217751692. [DOI] [Google Scholar]
- 29.Meling TR, Meling TR. The impact of surgical simulation on patient outcomes: a systematic review and meta-analysis. Neurosurg Rev. 2021;44(2):843–854. doi: 10.1007/s10143-020-01314-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request.