Abstract
Background
Hysteroscopic adhesiolysis is the preferred primary method for intrauterine adhesion. However, there is about a 60% of chance of re-adhesion after surgery. The objectives of the study were to evaluate the efficacy and safety of Yangmo decoction as a secondary treatment in preventing intrauterine re-adhesion against those of hyaluronic acid gel.
Methods
Women received oral Yangmo decoction (YD cohort, n = 105) or intrauterine hyaluronic acid gel (HA cohort, n = 125) or did not receive secondary re-adhesion prevention treatments (EP cohort, n = 165) after hysteroscopic adhesiolysis for 6 months. In addition, all women have received 3 mg of oral estrogen and 20 mg oral progesterone combination after hysteroscopic adhesiolysis for 3 months. Intrauterine re-adhesion after hysteroscopic adhesiolysis after 6 months with or without secondary treatment(s) was detected using hysteroscopy. The extent of the cavity, type of adhesion, and the menstrual pattern were included to define the American Fertility Society classification of intrauterine re-adhesions (AFS) score.
Results
Fewer numbers of women suffered from intrauterine re-adhesion after hysteroscopic adhesiolysis in the YD cohort than those of the HA (15(14%) vs. 40(32%), p = 0.0019) and the EP (15(14%) vs. 58(35%). p = 0.0001) cohorts. Among women who developed intrauterine re-adhesion, AFS score was fewer for women of the YD cohort than those of HA (2(2–1) vs. 4(4–3), p < 0.001) and the EP (2(2–1) vs. 4(4–4), p < 0.001) cohorts. AFS score after surgery was fewer for women of the HA cohort than those of the EP cohort (p < 0.05). Higher numbers of women of the YD cohort retained pregnancies after 6-months of treatment than those of the HA (55(52%) vs. 45(36%), p = 0.0161) and EP (55(52%) vs. 35(21%), p < 0.0001) cohorts. Among women who develop re-adhesion, 10(10%) women of the YD cohort only had successful pregnancies.
Conclusions
Yangmo decoction for 6 months after hysteroscopic adhesiolysis can reduce AFS score, prevent intrauterine re-adhesion, and increases the chances of successful pregnancies of women.
Level of evidence
IV.
Technical Efficacy
Stage 5.
Keywords: Amenorrhea, Hormone, Hyaluronic acid, Hysteroscopic adhesiolysis, Hysteroscopy, Yangmo decoction
Background
Intrauterine adhesions (Asherman’s syndrome) have resulted from lesions of the endothelial basement that is caused by various reasons, for example, intrauterine operations and/ or infections [1]. Due to the surgical repair process, the endometrium forms scars and adhesions in the uterine cavity that cause an abnormal uterine morphology [2, 3]. There are several other clinical manifestations of intrauterine adhesion, for example, recurrent miscarriage, menstrual reduction, amenorrhea (abnormal menstrual), infertility, and recurrent lower abdominal pain those are serious issues in women’s health [4]. Hysteroscopic adhesiolysis is the preferred primary method for the treatment of intrauterine adhesion. However, there is about a 60% of chance of intrauterine re-adhesion after surgery (hysteroscopic adhesiolysis) [5]. It is necessary to control intrauterine re-adhesion after surgery [6–8]. Hormones, intrauterine balloons, amniotic membranes, and intrauterine devices have a vital role in preventing intrauterine re-adhesion [9]. However, they have no significant effects on clinical manifestations of intrauterine re-adhesion [6–8]. At present, the intrauterine hyaluronic acid gel is the preferred secondary method of intrauterine re-adhesions after hysteroscopic adhesiolysis [10, 11]. The hyaluronic acid gel is well-established for the prevention of re-adhesion after surgery [1, 12]. Oral estrogen and progesterone combination is the most common treatment for the prevention of intrauterine re-adhesion after hysteroscopic adhesiolysis but it has limitations that this combination cannot increase the rate of fertility of victim women [13]. Yangmo decoction (a traditional Chinese medicine) has better therapeutic action in the treatment of intrauterine re-adhesion after hysteroscopic adhesiolysis than that of estrogen and progesterone combination [13, 14]. Yangmo decoction consists of Sanchi flower, Ginseng flower, Snow lotus, Daidai flower, Licorice, and so on [13]. Yangmo decoction is a common and registered treatment for adhesions prevention in China.
The objectives of the current retrospective study were to evaluate the effectiveness and safety of oral Yangmo decoction in preventing intrauterine re-adhesion after hysteroscopic adhesiolysis (surgery, primary treatment) against those of intrauterine hyaluronic acid gel in Chinese women.
Methods
Inclusion criteria
A total of 20–40 years of women before hysteroscopic adhesiolysis desire to have a pregnancy (according to records of institutes) and who underwent hysteroscopic adhesiolysis (cutting by scissors) for intrauterine adhesion were included in the study.
Exclusion criteria
Women with heart, liver, and/ or kidney disease(s) and women with severe motor disabilities were excluded from the study. Cases of incomplete adhesiolysis were excluded from the analyses. Allergic to one of component of Yangmo decoction and hyaluronic acid were excluded from analyses.
Cohorts
Women who received oral Yangmo decoction after hysteroscopic adhesiolysis for 6 months for secondary treatment of intrauterine re-adhesion [13] were included in the YD cohort (n = 105). The pharmacological bases, dosage, and dose are based on empirical bases. Women who received intrauterine hyaluronic acid gel after hysteroscopic adhesiolysis for 6 months using a 15 cm catheter for secondary treatment of intrauterine re-adhesion [15] were included in the HA cohort (n = 125). Intrauterine hyaluronic acid gel was applied on monthly basis. Women return to the hospital for this treatment. Women who did not receive secondary re-adhesion prevention treatments after hysteroscopic adhesiolysis for 6 months [16] were included in the EP cohort (n = 165). All women have received 20 mg twice a day cefixime for 4 days after hysteroscopic adhesiolysis. In addition, all women have received 3 mg of oral estrogen and 20 mg oral progesterone combination after hysteroscopic adhesiolysis for 3 months [16]. Selection of treatment was the choice of women because Chinese rule provides rights to patients for the selection of Chinese traditional medicine(s) for their treatment(s) of disease(s).
Outcome measures
Hysteroscopy
Intrauterine re-adhesion after hysteroscopic adhesiolysis after 6 months with or without secondary treatment(s) was detected using hysteroscopy. Hysteroscopy was carried out using a hysteroscope, with a light and camera at the end. The hysteroscope had 3–5 mm diameter. Images were sent to a monitor for diagnosis [17].
The american Fertility Society classification of intrauterine adhesions (AFS) score
AFS score was used for classifications of intrauterine re-adhesion severity. The extent of the cavity, type of adhesion, and the menstrual pattern were included to define intrauterine adhesion severity. The extent of the cavity, type of intrauterine adhesion, and the menstrual pattern was graded as per Table 1. A score of 1–4 is considered mild intrauterine re-adhesion, a score of 5–8 is considered intrauterine moderate re-adhesion, and a score of 9 or more is considered severe intrauterine re-adhesion [9]. The extent of the cavity and type of intrauterine adhesion was evaluated using a hysteroscope and the menstrual pattern was self-reported.
Table 1.
Grading of the extent of the cavity, type of intrauterine adhesion, and menstrual pattern
| Score | Extent of cavity | Type of intrauterine adhesion | Menstrual pattern |
|---|---|---|---|
| 1 | < | Filmy | Normal |
| 2 | – | Dense filmy | Hypomenorrhea |
| 4 | > | Dense | Amenorrhea |
1–4: mild re-adhesion, 5–8: moderate re-adhesion, and ≥ 9: severe re-adhesion
The density of endometrial glands
The biopsy performed at the base of the nongravid uterine horn and the other biopsy performed from beneath the conceptus. Computer assisted morphometric analysis was used to evaluate samples to determine the density of endometrial glands.
Statistical analysis
InStat 3.01 GraphPad Software, San Diego, CA, USA was used for statistical analysis purposes. Linear and ordinal variables are depicted as mean ± standard error of the mean (SEM), not linear, and ordinal variables are depicted as median (Q3–Q1), and constant variables are depicted as frequency (percentages). The chi-square test with Yate’s corrections (χ2-test) or Fisher’s exact test was used for the statistical analysis of categorical variables. Kolmogorov and Smirnov test was used to check the linearity of continuous and ordinal variables. One-way analysis of variance (ANOVA) was used for linear continuous and ordinal variables for statistical analysis. Kruskal-Wallis’ test (nonparametric ANOVA) was used for not linear continuous and ordinal variables for statistical analysis. Tukey or Dann’s multiple comparison tests were used for post hoc analysis. Univariate following multivariate analysis was performed for detecting independent parameters for intrauterine re-adhesion. All results were considered significant at a 95% confidence interval (Cl) if the p-value was less than 0.05.
Results
Study population
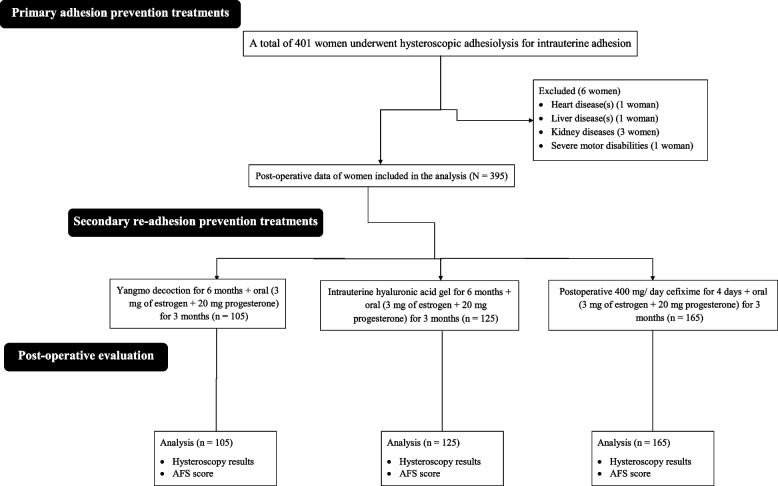
From January 2019 to 15 January 2021, a total of 401 women underwent hysteroscopic adhesiolysis for intrauterine adhesion at the First Affiliated Hospital of Chongqing Medical University, Chongqing, China, and the referring hospitals. Among them, one woman had heart disease(s), one woman had liver disease(s), three women had kidney diseases, and one woman had severe motor disabilities. Therefore, data from these women (n = 6) were excluded from the analysis. Results of hysteroscopy and the AFS score after surgery of a total of 395 women were included in the analysis. The summary chart of the study is presented in Fig. 1.
Fig. 1.
The summary chart of the study. AFS: American Fertility Society classification of intrauterine adhesions
Demographical and clinical characters
All cohorts had a mean AFS score of 4 before hysteroscopic adhesiolysis (Q3–Q1 range: 4–4). Age, body mass index, before surgery location of intrauterine adhesion, AFS score (mild intrauterine re-adhesion), and ethnicity of women were comparable among cohorts (p > 0.05 for all, Table 2). Women were arrived at institute for 2 years in follow-up time for pregnancy outcomes.
Table 2.
Demographical and clinical characters of women before hysteroscopic adhesiolysis
| Characters | Total | Cohorts | Comparisons | ||||
|---|---|---|---|---|---|---|---|
| YD | HA | EP | |||||
| Secondary re-adhesion preventions | Yes/ No | Yangmo decoction | Intrauterine hyaluronic acid gel | None | |||
| Numbers of women | 395 | 105 | 125 | 165 | p-value | Df | |
| Age (years) | 30.14±0.25 | 30.77±0.47 | 29.82±0.48 | 29.98±0.35 | 0.2898 (ANOVA) | N/A | |
| Body mass index (kg/ m2) | 22(23–21) | 22(24–21) | 22(23–21) | 22(23–21) | 0.2861 (Kruskal-Wallis’ test) | N/A | |
| Before surgery location of intrauterine adhesion | Middle cavity | 249(62) | 65(62) | 79(63) | 105(64) | 0.8669 (χ2-test) | 6 |
| Fundus and cornua | 81(21) | 21(20) | 28(23) | 32(19) | |||
| Entire cavity | 43(11) | 11(10) | 14(11) | 18(11) | |||
| Cervico-isthmic | 22(6) | 8(8) | 4(3) | 10(6) | |||
| Before surgery American Fertility Society classification of intrauterine adhesions score | 4(4–4) | 4(4–4) | 4(4–4) | 4(4–4) | 0.161 (Kruskal-Wallis’ test) | N/A | |
| Ethnicity | Han Chinese | 349(88) | 96(91) | 111(88) | 142(86) | 0.854 (χ2-test) | 6 |
| Mongolian | 38(10) | 7(7) | 11(9) | 20(12) | |||
| Tibetan | 5(1) | 1(1) | 2(2) | 2(1) | |||
| Uyghur Muslim | 3(1) | 1(1) | 1(1) | 1(1) | |||
Variables are depicted as mean ± SEM (standard error of the mean) or median (Q3–Q1) or frequency (percentages)
A p-value less than 0.05 was considered significant
Df Degree of freedom, N/A Not applicable
Hysteroscopic adhesiolysis characters
Surgery time, postoperative hysteroscopy observation room, stays, and total hospital stays of women were comparable among cohorts (p > 0.05 for all, Kruskal-Wallis’ test).
Hysteroscopy
Hysteroscopy results after 6 months of treatment(s) revealed that 15 (14%), 40 (32%), and 58 (35%) women of the YD, the HA, and the EP cohorts, respectively suffered from intrauterine re-adhesion after hysteroscopic adhesiolysis. Fewer numbers of women suffered from intrauterine re-adhesion after hysteroscopic adhesiolysis in the YD cohort than those of the HA (p = 0.0019, 95% Cl: 0.3364 to 0.8359 (using the approximation of Katz.), Fisher’s exact test) and the EP (p = 0.0001, 95% Cl: 0.2794 to 0.7241, Fisher’s exact test) cohorts. There was no statistical significance difference between women who suffered from intrauterine re-adhesion after hysteroscopic adhesiolysis between the EP and the HA cohorts (p = 0.6171, Fisher’s exact test). The details of hysteroscopy results are reported in Table 3.
Table 3.
Hysteroscopy results
| Characters | Total | Cohorts | Comparisons among cohorts | |||
|---|---|---|---|---|---|---|
| YD | HA | EP | ||||
| Secondary re-adhesion preventions | Yes/ No | Yangmo decoction | Intrauterine hyaluronic acid gel | None | ||
| Numbers of women | 395 | 105 | 125 | 165 | p-value | Df |
| Intrauterine re-adhesion | 113(29) | 15(14) | 40(32) | 58(35) | 0.0006 | 2 |
Variables are depicted in frequency (percentages)
χ 2-test was used for statistical analysis
A p-value less than 0.05 was considered significant
Df Degree of freedom
Obstetrics parameters
A total of 135 (34%) women with successful pregnancies after 6 months of treatment. Pregnancies were successful in 55 (52%), 45 (36%), and 35 (21%) women of the YD, the HA, and the EP cohorts, respectively. Higher numbers of women in the YD cohort retained pregnancies after 6 months of treatment than those of the HA (p = 0.0161, Fisher exact test) and EP (p < 0.0001, Fisher exact test) cohorts. Higher numbers of women in the HA cohort retained pregnancies after 6 months of treatment than those of the EP cohort (p = 0.0077, Fisher exact test).
Gynecological parameters
Among women who developed intrauterine re-adhesion after hysteroscopic adhesiolysis, AFS score was fewer for women of the YD cohort than those of HA (2 (2–1) vs. 4 (4–3), p < 0.001, Kruskal-Wallis’ test/ Dann test) and the EP (2 (2–1) vs. 4 (4–4), p < 0.001, Kruskal-Wallis’ test/ Dann test) cohorts. AFS score was fewer for women of the HA cohort than those of the EP cohort (p < 0.05, Kruskal-Wallis’ test/ Dann test).
Endometrial thickness was statistically the same among women of all cohorts. Among women who develop intrauterine re-adhesion, only 10 (10%) women of the YD cohort had successful pregnancies after treatment of intrauterine re-adhesion. None of women from the HA and the EP cohorts had successful pregnancies after treatment of intrauterine re-adhesion. The density of endometrial glands was higher in women of the YD cohort than in the HA and the EP cohorts (p < 0.05 for both, Kruskal-Wallis’ test/ Dann test). The details of women after hysteroscopic adhesiolysis Table 4.
Table 4.
The details of women after hysteroscopic adhesiolysis
| Characters | Cohorts | Comparisons between HA and EP | |||||||
|---|---|---|---|---|---|---|---|---|---|
| YD | HA | EP | |||||||
| Secondary re-adhesion preventions | Yangmo decoction | Intrauterine hyaluronic acid gel | Comparisons between YD and HA | None | Comparisons between YD and EP | ||||
| Numbers of women | 105 | 125 | p-value | Cl | 165 | p-value | Cl | p-value | Cl |
| Successful pregnancies | 55(52) | 45(36) | 0.0161 | 1.080 to 1.893 | 35(21) | <0.0001 | 1.650 to 2.933 | 0.0077 | 1.140 to 1.913 |
| Numbers of women who develop re-adhesion | 15(14) | 40(32) | 0.0019 | 0.2794 to 0.7241 | 58(35) | 0.0001 | 0.2794 to 0.7241 | 0.6171 | N/A |
| Postoperative AFS score of women who develop re-adhesion | 2(2–1) | 4(4–3) | <0.001 (Krushal-Wallis’ test) | N/A | 4(4–4) | <0.001 (Krushal-Wallis’ test) | N/A | <0.05 (Krushal-Wallis’ test) | N/A |
| Successful pregnancies after re-adhesion | 10(67) | 0(0) | <0.0001 (Fisher exact test) | 1.990 to 2.695 | 0(0) | <0.0001 (Fisher exact test) | 5.433 to 29.222 | N/A | N/A |
| Endometrial thickness (mm) | 3(3.4–2.8) | 3.45(4.1–2.85) | >0.05 (one-way ANOVA/ Tukey test) | N/A | 3.05(3.5–2.8) | >0.05 (one-way ANOVA/ Tukey test) | N/A | >0.05 (one-way ANOVA/ Tukey test) | N/A |
Variables are depicted in frequency (percentages) or median (Q3–Q1)
AFS American Fertility Society classification of intrauterine adhesions
A p-value less than 0.05 was considered significant
Cl Confidence Interval, N/A Not applicable
Parameters for intrauterine re-adhesion
Before surgery AFS score was > 5 and before surgery, the location of intrauterine adhesion at the fundus and cornua, entire cavity, or cervical-isthmic was the independent parameter of intrauterine re-adhesion. The details of parameters for intrauterine re-adhesion are presented in Table 5.
Table 5.
Parameters for intrauterine re-adhesion
| Parameters | Odd ratio | 95% Cl | p-value |
|---|---|---|---|
| Age (<30 years vs. ≥30 years) | 0.8951 | 0.8621–0.9821 | 0.0821 |
| Before surgery AFS score (>5a vs.<5) | 1.8521 | 1.2451–1.9522 | 0.0412 |
| Before surgery location (other a vs. Middle cavity) | 1.5222 | 0.7541–1.8952 | 0.0221 |
| Body mass index (>23 vs. ≤23) | 0.7421 | 0.6214–0.8241 | 0.0852 |
Multivariate analysis
An odd ratio of more than 1 and a p-value less than 0.05 was considered significant
Cl Confidence Interval
aResponsible parameter for intrauterine re-adhesion
Discussion
The study showed the lowest number of women with intrauterine re-adhesion after hysteroscopic adhesiolysis if they have taken Yangmo decoction. Traditional Chinese medicine Yangmo decoction has a superior effect than 3 months of estrogen and progesterone combinations only [13, 14] because kidney deficiency and blood stasis are the main reasons for women with intrauterine adhesions, and the treatment for that is to nourish the kidney and activate blood circulation [18]. Ingredients of Yangmo decoction nourish the kidney and activate blood circulation [13]. Yangmo decoction for 6 months can prevent intrauterine re-adhesion after hysteroscopic adhesiolysis.
The study showed women had comparatively fewer post-surgery AFS scores if they have taken Yangmo decoction in cases of intrauterine re-adhesion occurrence after hysteroscopic adhesiolysis. The AFS score is evaluated from the scope, type, and menstrual flow of intrauterine adhesions [9]. Yangmo decoction improves menstrual flow and prevents intrauterine re-adhesion after hysteroscopic adhesiolysis. This would lead to improving the AFS score of women. The results of the association of the AFS score of women in the current study are parallel with those of a retrospective analysis [13]. Yangmo decoction reduces the AFS score of women in cases of intrauterine re-adhesion occurrence after hysteroscopic adhesiolysis.
The density of endometrial glands was reported higher in women of the YD cohort. The absence of endometrial glands and increased fibrosis are associated with intrauterine adhesions [19]. The density of endometrial glands is associated with endometrial functions [20, 21]. Yangmo decoction hinders fibrosis and promotes the regeneration of endometrial glands.
Only Yangmo decoction was successful in pregnancies in women with intrauterine re-adhesion that occurred after hysteroscopic adhesiolysis on treatment. A higher density of endometrial glands can promote pregnancies [20, 21]. Yangmo decoction improves the blood supply and uniform blood flow of the endometrium and uterus are beneficial to pregnancy outcomes [22]. Yangmo decoction improves the chances of pregnancies in women with intrauterine re-adhesion after hysteroscopic adhesiolysis.
Before surgery, AFS score > 5 was associated with intrauterine re-adhesion. The results of the association of AFS score with intrauterine re-adhesion are parallel with those of a retrospective analysis [13]. The moderate and severe AFS scores of females have always high intrauterine re-adhesion after surgery [23]. Women with severe or moderate AFS scores (> 5) have difficulties in resolving intrauterine adhesion.
Before surgery, the location of intrauterine adhesion at the fundus and cornua, entire cavity, or cervical-isthmic was the independent parameter of intrauterine re-adhesion. The results of the association of the original location of intrauterine adhesion with occurrences of intrauterine re-adhesion are parallel with those of a retrospective observational study [24]. Besides the extent, the original location of intrauterine adhesion is also associated with intrauterine re-adhesion.
Only 34% women reported successful pregnancies after 6 months of treatment. The results of successful pregnancies are inconsistent with domestic research [25] and foreign research [26]. The clinical, demographical, and operational parameters also affect successful pregnancies [25]. It is difficult for women for intrauterine adhesion to return to normal reproductive function.
The study showed that intrauterine hyaluronic acid gel was not successful to prevent intrauterine re-adhesion, to decrease AFS scores, and to establish fortunate pregnancies. The obstetrics and gynecological results of the current study are parallel with those of a trial [27]. The intrauterine hyaluronic acid gel does not aberrantly reduce the incidence of secondary intrauterine re-adhesion. In the presence of independent parameters for intrauterine re-adhesion, hyaluronic acid gel would not much successful to prevent intrauterine re-adhesion.
The limitations of the study, for example, retrospective analysis with small sample size. In the current study, hysteroscopy was used instead of hysterosalpingography for the detection of intrauterine re-adhesion after hysteroscopic adhesiolysis. The possible justification for the same is that AFS scores would be vigorous if it would be detected using hysteroscopy. The study is underpowered to detect significant differences for the investigated parameters because the study did not perform any “a priori” sample size calculation based on the primary outcome. Yangmo decocticion is not a registered drug in EU. In the future, well-designed, carefully conducted randomized controlled trial are needed, with a particular focus on the live birth rate after hysteroscopic adhesiolysis followed by Yangmo solution and other safety indexes.
Conclusions
According to current study results Yangmo decoction for 6 months can reduce the American Fertility Society classification of intrauterine adhesions score and prevent intrauterine re-adhesion of women after hysteroscopic adhesiolysis. Yangmo decoction hinders fibrosis and promotes the regeneration of endometrial glands. Yangmo decoction improves the chances of pregnancies in women with intrauterine re-adhesion after hysteroscopic adhesiolysis. Women with severe or moderate (> 5) American Fertility Society classification of intrauterine adhesions score have difficulties in resolving intrauterine adhesion.
Acknowledgements
The authors are thankful for the medical and non-medical staff of the First Affiliated Hospital of Chongqing Medical University, Chongqing, China.
Abbreviations
- SEM
Standard error of the mean
- χ2-test
Chi-square test
- ANOVA
Analysis of variance
- Cl
Confidence Interval
- Q3
Third Quartile
- Q1
First Quartile
- AFS
American Fertility Society classification of intrauterine adhesions
- YD cohort
Women received oral Yangmo decoction after hysteroscopic adhesiolysis for 6 months
- HA cohort
Women received intrauterine hyaluronic acid gel after hysteroscopic adhesiolysis for 6 months using a 15 cm catheter
- EP cohort
Women did not receive secondary re-adhesion prevention treatments after hysteroscopic adhesiolysis
Authors' contributions
Both authors have read and approved the manuscript for publication. JD was the project administrator and contributed to the conceptualization, investigation, supervision, resources, methodology, and literature review of the study. YC contributed to the literature review, validation, methodology, formal analysis, and data curation of the study, and drafted, and edited the manuscript for intellectual content. Both authors agree to be accountable for all aspects of work ensuring integrity and accuracy.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Availability of data and materials
The datasets were used and analyzed during the current study available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study was approved by the ethics committee of Chongqing Medical University (approval No. fhCMU dated 17 January 2023) and the gynecological society of China. The study follows the law of China and the v2008 Declaration of Helsinki. Informed consent of all subjects and/ or their legal guardian(s) waived by the ethics committee of the Chongqing Medical University (because of retrospective analysis).
Consent to participate
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Fei Z, Bin Z, Xin X, Fei H, Yuechong C. Meta-analysis on the use of hyaluronic acid gel to prevent recurrence of intrauterine adhesion after hysteroscopic adhesiolysis. Taiwan J Obstet Gynecol. 2019;58(6):731–6. doi: 10.1016/j.tjog.2019.09.002. [DOI] [PubMed] [Google Scholar]
- 2.Yamamoto N, Takeuchi R, Izuchi D, Yuge N, Miyazaki M, Yasunaga M, et al. Hysteroscopic adhesiolysis for patients with Asherman’s syndrome: menstrual and fertility outcomes. Reprod Med Biol. 2013;12(4):159–66. doi: 10.1007/s12522-013-0149-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Conforti A, Alviggi C, Mollo A, De Placido G, Magos A. The management of Asherman syndrome: a review of literature. Reprod Biol Endocrinol. 2013;11:118. doi: 10.1186/1477-7827-11-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vancaillie TG, Garad R. Asherman’s syndrome. Aust Nurs J. 2013;20(8):34–6. [PubMed] [Google Scholar]
- 5.Bosteels J, Weyers S, D’Hooghe TM, Torrance H, Broekmans FJ, Chua SJ, et al. Anti-adhesion therapy following operative hysteroscopy for treatment of female subfertility. Cochrane Database Syst Rev. 2017;11(11):CD011110. doi: 10.1002/14651858.CD011110.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gupta S, Talaulikar VS, Onwude J, Manyonda I. A pilot study of Foley’s catheter balloon for prevention of intrauterine adhesions following breach of uterine cavity in complex myoma surgery. Arch Gynecol Obstet. 2013;88(4):829–32. doi: 10.1007/s00404-013-2838-4. [DOI] [PubMed] [Google Scholar]
- 7.Liu AZ, Zhao HG, Gao Y, Liu M, Guo BZ. Effectiveness of estrogen treatment before transcervical resection of adhesions on moderate and severe uterine adhesion patients. Gynecol Endocrinol. 2016;32(9):737–40. doi: 10.3109/09513590.2016.1160375. [DOI] [PubMed] [Google Scholar]
- 8.Salma U, Xue M, Md Sayed AS, Xu D. Efficacy of intrauterine device in the treatment of intrauterine adhesions. Biomed Res Int. 2014;2014:589296. 10.1155/2014/589296. [DOI] [PMC free article] [PubMed]
- 9.Lee WL, Liu CH, Cheng M, Chang WH, Liu WM, Wang PH. Focus on the primary prevention of intrauterine adhesions: current concept and vision. Int J Mol Sci. 2021;22(10):5175. doi: 10.3390/ijms22105175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li X, Wu L, Zhou Y, Fan X, Huang J, Wu J, et al. New crosslinked hyaluronan gel for the prevention of intrauterine adhesions after dilation and curettage in patients with delayed miscarriage: a prospective, multicenter, randomized, controlled trial. J Minim Invasive Gynecol. 2019;26(1):94–9. doi: 10.1016/j.jmig.2018.03.032. [DOI] [PubMed] [Google Scholar]
- 11.Hooker AB, de Leeuw R, van de Ven PM, Bakkum EA, Thurkow AL, Vogel NEA, et al. Prevalence of intrauterine adhesions after the application of hyaluronic acid gel after dilatation and curettage in women with at least one previous curettage: short-term outcomes of a multicenter, prospective randomized controlled trial. Fertil Steril. 2017;107(5):1223e3–313. doi: 10.1016/j.fertnstert.2017.02.113. [DOI] [PubMed] [Google Scholar]
- 12.Unanyan A, Pivazyan L, Krylova E, Obosyan L, Ishchenko A. Comparison of effectiveness of hyaluronan gel, intrauterine device and their combination for prevention adhesions in patients after intrauterine surgery: systematic review and meta-analysis. J Gynecol Obstet Hum Reprod. 2022;51(4):102334. doi: 10.1016/j.jogoh.2022.102334. [DOI] [PubMed] [Google Scholar]
- 13.Zhao X, He S, You Z, Wang H, Xu D, Zhang A. Chinese medicine Yangmo decoction ameliorates intrauterine adhesion prognosis following hysteroscopic adhesiolysis. J Cent South Univ. 2022;47(11):1540–9. doi: 10.11817/j.issn.1672-7347.2022.220519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhao X, Deng J, You Z, Gan X, Xu D, Zhang A. Value of transvaginal three-dimensional ultrasound in evaluating the curative effect of Yangmo decoction in the treatment of uterine adhesion. J Cent South Univ. 2022;47(11):1550–8. doi: 10.11817/j.issn.1672-7347.2022.220512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Trinh TT, Nguyen KD, Pham HV, Ho TV, Nguyen HT, O’Leary S, et al. Effectiveness of hyaluronic acid gel and intrauterine devices in prevention of intrauterine adhesions after hysteroscopic adhesiolysis in infertile women. J Minim Invasive Gynecol. 2022;29(2):284–90. doi: 10.1016/j.jmig.2021.08.010. [DOI] [PubMed] [Google Scholar]
- 16.Krajčovičová R, Hudečk R, Ventruba P, Surgentová K. The role of hyaluronan in Asherman’s syndrome therapy. J Gynecologic Surg. 2015;31(5):254–8. doi: 10.1089/gyn.2014.0129. [DOI] [Google Scholar]
- 17.Parry JP. St. elsewhere and hysteroscopy. Fertil Steril. 2022;18(4):804. doi: 10.1016/j.fertnstert.2022.08.855. [DOI] [PubMed] [Google Scholar]
- 18.Qiu L, Tan Z. Experience of YOU zhaoling in repairing endometrium from the theory of “kidney master reproduction. Clin J Traditional Chin Med. 2021;33(5):859–61. [Google Scholar]
- 19.Hu X, Dai Z, Pan R, Zhang Y, Liu L, Wang Y, et al. Long-term transplantation human menstrual blood mesenchymal stem cell loaded collagen scaffolds repair endometrium histological injury. Reprod Toxicol. 2022;109:53–60. doi: 10.1016/j.reprotox.2022.03.001. [DOI] [PubMed] [Google Scholar]
- 20.Zhao X, Gao B, Yang X, Zhang A, Jamail G, Li Y, et al. The density of endometrial glandular openings: a novel variable to predict the live birth rate in patients with intrauterine adhesions following hysteroscopic adhesiolysis. Hum Reprod. 2021;36(4):965–75. doi: 10.1093/humrep/deaa377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hua P, Yang Y, Hu J. A meta-analysis of endometrial thickness in predicting pregnancy outcome of IVF-ET. J Reprod Med. 2022;31(8):1119–26. [Google Scholar]
- 22.Kagami K, Ono M, Iizuka T, Matsumoto T, Hosono T, Sekizuka-Kagami N, et al. A novel third mesh-like myometrial layer connects the longitudinal and circular muscle fibers -A potential stratum to coordinate uterine contractions. Sci Rep. 2020;10(1):8274. doi: 10.1038/s41598-020-65299-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu Z, Kong Y, Gao Y, Ren Y, Zheng C, Deng X, et al. Revealing the interaction between intrauterine adhesion and vaginal microbiota using high–throughput sequencing. Mol Med Rep. 2019;19(5):4167–74. doi: 10.3892/mmr.2019.10092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang JH, Chen CD, Chen SU, Yang YS, Chen MJ. The influence of the location and extent of intrauterine adhesions on recurrence after hysteroscopic adhesiolysis. BJOG. 2016;123(4):618–23. doi: 10.1111/1471-0528.13353. [DOI] [PubMed] [Google Scholar]
- 25.Zhang X, Liu W, Zhou Y, Qiu J, Sun Y, Li M, et al. Comparison of therapeutic efficacy of three methods to prevent re-adhesion after hysteroscopic intrauterine adhesion separation: a parallel, randomized and single-center trial. Ann Palliat Med. 2021;10(6):6804–23. doi: 10.21037/apm-21-1296. [DOI] [PubMed] [Google Scholar]
- 26.Capmas P, Mihalache A, Duminil L, Hor LS, Pourcelot AG, Fernandez H. Intrauterine adhesions: what is the pregnancy rate after hysteroscopic management? J Gynecol Obstet Hum Reprod. 2020;49(7):101797. doi: 10.1016/j.jogoh.2020.101797. [DOI] [PubMed] [Google Scholar]
- 27.Guo Y, Shi X, Song D, Liu Y, Huang X, Xiao Y, et al. The efficacy of auto-cross-linked hyaluronic acid gel in addition to oestradiol and intrauterine balloon insertion in the prevention of adhesion reformation after hysteroscopic adhesiolysis. Reprod Biomed Online. 2022;45(3):501–7. doi: 10.1016/j.rbmo.2022.04.017. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets were used and analyzed during the current study available from the corresponding author on reasonable request.