Abstract
Background:
Hip osteoarthritis (HOA) is a growing burden and one of the leading causes of hip pain. The relationship between the HOA and the alignment of the spinopelvic region has been intensively studied, however the issue remains controversial. Spinopelvic imbalance, HOA, and dysplasia were investigated in relation to sagittal spinopelvic parameters in this study.
Methods:
We collected computerized tomography (CT) topograms of the pelvis or abdomen from 380 patients. In antero-posterior (AP) topograms, Tonnis grading, center-edge angle (CEA) and Sharp’s acetabular angle (AA) measurements were performed on each patient. Lateral topograms were used to evaluate the following spinopelvic parameters for each patient: pelvic incidence (PI), pelvic tilt (PT), sacral slope (SS), sacral table angle (STA), lumbar lordosis (LL), proximal lumbar lordosis (PLL), distal lumbar lordosis (DLL), and PI-LL difference. Initially, the cohort was divided into two subgroups based on whether or not they had HOA. Then, they were divided into two subgroups based on whether or not they had dysplasia. Ultimately, it was divided in half based on the PI-LL imbalance. Statistical analyses were conducted to determine the likely correlations between the spinopelvic parameters of these subgroups. In addition, the correlations between spinopelvic parameters were investigated.
Results:
There were 380 patients evaluated. We found no association between HOA or dysplasia and spinopelvic parameters. In addition, there was no association between PI-LL imbalance and HOA or dysplasia.
Conclusion:
There was no difference in constant PI and STA angle, besides other variable parameters, between groups having HOA and dysplasia or not. PI-LL imbalance has no effect on HOA and dysplasia.
Keywords: Hip osteoarthritis, sagittal spinopelvic parameters, hip dysplasia, PI-LL imbalance, correlation analyses
Introduction
Hip osteoarthritis has become a growing burden for both patients and health care providers over the past two decades. It is estimated that 25% of individuals over the age of 45 will develop HOA. 1 Etiological factors for HOA have been investigated for many years, but are still not completely clear. It is considered multifactorial as a mixture of biological and mechanical factors. 2 The role of spinopelvic morphology in the outcome of spinal surgery has been demonstrated in many studies but its possible role on HOA is not yet well understood. While pelvic incidence (PI) and sacral table angle (STA) is considered as constant pelvic parameters, sacral slope (SS), pelvic tilt (PT), and lumbar lordosis (LL) are compensatory dynamic parameters. Especially, the effect of PI and PT in HOA development was researched by some authors and controversial results have been reported.3-9 We therefore examined other constant and dynamic spinopelvic parameters and PI-LL imbalance 10 and the biomechanic adaptations that result would be associated with HOA and dysplasia. The purpose of this study is to assess these probable relationships.
Methods
Study subjects
The study was carried out in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines. 380 patients (220 men, 160 women) aged between 40 and 82 were included in this retrospective study. Patients with previous hip or spine surgical interventions, secondary arthritis (ankylosing spondylitis or rheumatoid), pelvis or vertebral fracture, or other spinal deformities including spondylolisthesis were excluded. Hospital records between February 2021 and May 2022 scanned and patients who had pelvic or abdominal computerized tomography (CT) because of urologic/general surgery complaints were recruited. CT Topograms (10 ma, 120 kV, GE Bright Spears; AP and Lat) were evaluated. Radiographic HOA was graded by unanimous decision of 2 orthopedists according to Tonnis grading in the AP Topograms. Tonnis grade 0 and 1 accepted as non-HOA, grades 2 and 3 accepted as HOA. Center-edge Angle (CEA) and Sharps’ Acetabular Angle (AA) were measured in the same AP Topograms by another orthopedist. CEA < 25° or AA > 42° was accepted as dysplasia. Spinopelvic parameters describing the sagittal profile of the spine, pelvis and hip were quantified by 2 experienced spinal surgeons in the Lat Topogram using Surgimap Spine (Nemaris Inc. Ver. 2.3.2.1, NY, USA). Average value of each parameter was calculated as the final result. Interobserver variability was evaluated. Intraclass correlation coefficient (ICC > .94) was excellent. Each patient’s PI-LL difference was calculated and the patients with PI-LL > 10° accepted as PI-LL imbalance.
Sagittal spinopelvic parameters and hip angles
Lumbar lordosis is the angle between the lines drawn parallel to the lower endplate of the T12 vertebrae and the upper-end plate of the S1 vertebrae. Proximal lumbar lordosis is the angle between the lines drawn parallel to the lower endplate of the T12 vertebra and the lower endplate of the L3 vertebra. Distal lumbar lordosis is the angle between the lines drawn parallel to the upper endplate of the L4 vertebra and the upper endplate of the S1 vertebra. So, the sum of proximal lumbar lordosis (PLL) and distal lumbar lordosis (DLL) is equal to LL. Pelvic incidence is the angle between the line perpendicular to the midpoint of the sacral plate and the line drawn from this point to the bicoxofemoral line. Pelvic tilt is the angle between the vertical plane and the line joining the midpoint of the sacral plate and the bicoxofemoral axis. Sacral slope is the angle between the sacral endplate and the horizontal axis. Sacral table angle is the angle between a line parallel to the sacral endplate and a line drawn to parallel the posterior aspect of the S1 vertebral body (Figure 1).
Figure 1.
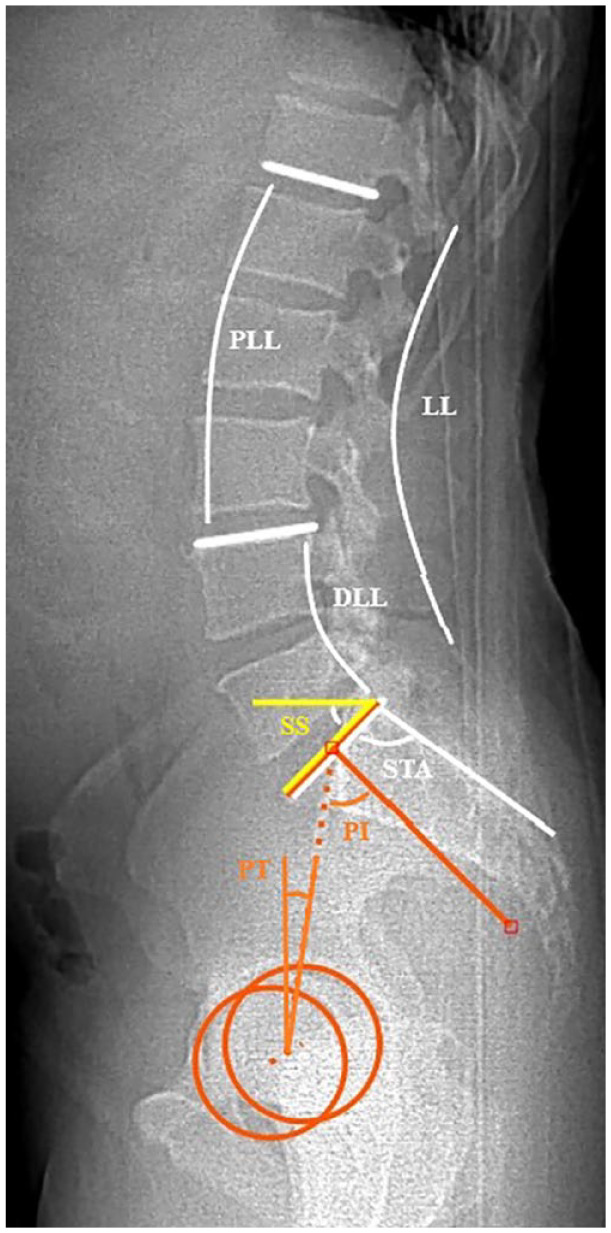
Measurement of spinopelvic parameters. DLL indicates distal lumbar lordosis; LL, lumbar lordosis; PI, pelvic incidence; PLL, proximal lumbar lordosis; SS, sacral slope; STA, sacral table angle.
The CEA was defined as the angle between the line joining the center of the femoral head to the lateral margin of the acetabular roof and the line perpendicular to the line joining the centers of the femoral heads. The AA was defined as the angle between lateral sourcil and horizontal line between the inferior aspect of both pelvic teardrops (Figure 2).
Figure 2.

Measurement of CEA and AA. AA indicates acetabular angle; CEA, center-edge angle.
At first, the cohort stratified into two subgroups, in terms of HOA (66/314). Statistical analysis was performed to compare the spinopelvic parameters of these two subgroups. Second, the cohort was divided into two subgroups, with and without dysplasia (45/335). Finally, cohort was divided into two subgroups according to have PI-LL imbalance (106/274). Statistical comparisons were made between these subgroups. Then, it was investigated whether there was a relationship between dysplasia, HOA, and PI-LL imbalance. Correlation analysis was used to measure the relationships between them.
Statistical analyses
Data were analyzed in IBM SPSS Statistics 22.0 package program. Kolmogorov-Smirnov test was used for the conformity of the data to the normal distribution. Independent samples t test was used between the 2 groups for the mean differences of the variables with normal distribution between the groups, and the chi-square test was used to look at the distribution of the categorical variables between the groups. Pearson correlation coefficient was used for the relations of continuous variables with each other. Mean, standard deviation, r (correlation coefficient), frequency (frequency), and percentage (%) values are given as descriptive statistics. Statistically significant limit of P < .05 was accepted. A post-hoc power analysis was performed to determine the power of the results obtained from the research.
Results
380 patients assessed. There were 160 women and 220 men (average age 51.43 ± 9.29). Demographics and the mean values and standard deviations of the spinopelvic parameters of groups are given in Table 1. When the cohort was divided into 2 groups in terms of OA, there were 66 patients in the HOA group and 314 patients were in the non-HOA group. There were no statistically significant differences between these 2 groups in terms of spinopelvic parameters (P = .16-.96). Then, the cohort was divided into 2 groups in terms of dysplasia. There were 45 patients in the dysplastic group and 335 patients were in the nondysplastic group. It was determined that the power analyses for the difference analyses for 2 different conditions (osteoarthritis and dysplasia) were 0.96 and 0.88 (First power analysis conditions: α = 0.05, effect size = 0.50; sample size group 1 = 66, sample size group 1 = 314; second power analysis conditions: α = 0.05, effect size = 0.50; sample size group 1 = 45, sample size group 1 = 335). There was no statistically significant difference between these two groups in terms of spinopelvic parameters (P = .07-.721). Finally, the cohort was divided into 2 groups in terms of PI-LL imbalance. There were 106 patients in PI-LL imbalanced group, while there were 274 patients in PI-LL balanced group. There were significant difference between these 2 groups only in terms of LL and PLL (<.001). Lumbar lordosis was significantly higher in those with imbalance group (56.03° ± 12.19° vs 50.99° ± 10.52°) and it was seen that this difference appeared to be due to proximal lordosis (17.59° ± 8.85° vs 13.52° ± 7.19°) (P < .001). Then, the group with PI-LL imbalance were compared with the OA group and dysplasia group separately and we observed no statistically significant difference between these groups in terms of spinopelvic parameters. It was observed that PI-LL imbalance was neither associated with the development of HOA (P = .434) nor with dysplasia (P = .209). Correlative relationships of spinopelvic parameters with each other were also investigated and given in Table 2. Strong correlations were observed between PI-SS, LL-SS, and DLL-SS. Moderate correlation was observed between PI-PT, PI-LL, PI-DLL, PI-STA, LL-PLL and LL-DLL. Weak correlation was observed between PT-STA. Scatter plots is given in Figure 3.
Table 1.
Demographic and radiographic evaluation of each parameter.
| Total | Osteoarthritis | P value | Dysplasia | P value | PI-LL mismatch | P value | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Average ± SD | Average ± SD | PI-LL > 10 | ||||||||
| Yes | No | Yes | No | Yes | No | |||||
| Number of patients | 380 | 66 | 314 | 45 | 335 | 106 | 274 | |||
| Age | 51.43 ± 9.29 | 61.57 ± 10.32 | 49.30 ± 7.49 | <.001 | 49.24 ± 7.95 | 51.73 ± 9.43 | .059 | 52.09 ± 9.72 | 51.18 ± 9.13 | .392 |
| Sex (F/M) | 160/220 | 26 /44 | 134/ 180 | .624 | 24/21 | 136/199 | .104 | 53/23 | 107 /274 | .053 |
| CEA | 18/362 | 8/58 | 10/304 | .002 | 18/27 | 0/335 | <.001 | 4/102 | 14/260 | .582 |
| AA | 35/345 | 5/61 | 30/284 | .613 | 35/10 | 0/335 | <.001 | 7/99 | 28/246 | .274 |
| CEA(R + L) | 34.95 ± 5.31 | 34.58 ± 6.5 | 35.3 ± 5.03 | .525 | 27.24 ± 3.91 | 35.99 ± 4.57 | <.001 | 35.37 ± 5.84 | 34.79 ± 5.09 | .345 |
| AA(R + L) | 37.29 ± 2.95 | 36.55 ± 3.24 | 34.45 ± 2.86 | .038 | 42.13 ± 1.8 | 36.64 ± 2.42 | <.001 | 36.86 ± 3.04 | 37.46 ± 2.9 | .077 |
| Mean PI (◦) | 49.85 ± 10.67 | 49.04 ± 11.15 | 50.02 ± 10.58 | .5 | 50.8 ± 10.23 | 49.72 ± 10.74 | .524 | 49.15 ± 11.81 | 50.12 ± 10.21 | .428 |
| Mean PT (◦) | 10.96 ± 5.66 | 10.92 ± 6.08 | 10.96 ± 5.57 | .961 | 12.35 ± 6.06 | 10.77 ± 5.58 | .077 | 9.31 ± 7.92 | 11.59 ± 4.34 | .006 |
| Mean SS (◦) | 38.89 ± 8.13 | 38.12 ± 8.65 | 39.06 ± 8.02 | .394 | 38.45 ± 6.48 | 38.95 ± 8.33 | .638 | 39.84 ± 8.37 | 38.53 ± 8.02 | .158 |
| Mean STA (◦) | 105.33 ± 6.05 | 104.37 ± 6.15 | 105.53 ± 6.01 | .16 | 105.78 ± 6.13 | 105.27 ± 6.04 | .596 | 105.81 ± 6.94 | 105.14 ± 5.66 | .381 |
| Mean LL (◦) | 52.4 ± 11.22 | 52.67 ± 12.16 | 52.34 ± 11.04 | .832 | 51.13 ± 8.81 | 52.57 ± 11.51 | .421 | 56.03 ± 12.19 | 50.99 ± 10.52 | <.001 |
| Mean PLL (◦) | 14.66 ± 7.89 | 15.59 ± 8.50 | 14.46 ± 7.76 | .292 | 13.79 ± 7.41 | 14.77 ± 7.96 | .721 | 17.59 ± 8.85 | 13.52 ± 7.19 | <.001 |
| Mean DLL (◦) | 37.74 ± 7.94 | 37.08 ± 8.37 | 37.88 ± 7.85 | .455 | 37.35 ± 6.32 | 37.8 ± 8.13 | .432 | 38.44 ± 8.62 | 37.48 ± 7.65 | .29 |
Abbreviations: AA, acetabular angle; CEA, center-edge angle; DLL, distal lumbar lordosis; LL, lumbar lordosis; PI, pelvic incidence; PLL, proximal lumbar lordosis; PT, pelvic tilt; SD, standard deviation; SS, sacral slope; STA, sacral table angle.
Table 2.
Correlation table among the spinopelvic parameters.
| PI | SS | STA | LL | DLL | PLL | PI-LL imbalance | |
|---|---|---|---|---|---|---|---|
| Age | −0.011/0.829 | −0.09/0.86 | −0.03/0.544 | 0.069/0.182 | −0.03/0.502 | 0.126/0.014 | 0.043/0.402 |
| PT | 0.648/<0.001 | 0.198/<0.001 | −0.341/<0.001 | 0.027/0.59 | 0.093/0.07 | 0.132/0.01 | −0.257/0.001 |
| PI | 0.852/<0.001 | −0.511/<0.001 | 0.672/<0.001 | 0.487/<0.001 | 0.466/<0.001 | −0.021/0.686 | |
| SS | −0.429/<0.001 | 0.869/<0.001 | 0.708/<0.001 | 0.504/<0.001 | 0.115/0.025 | ||
| STA | −0.326/<0.001 | −0.253/<0.001 | −0.207/<0.001 | −0.01/0.845 | |||
| LL | 0.698/<0.001 | 0.686/<0.001 | 0.227/<0.001 | ||||
| DLL | 0.01/0.841 | 0.107/0.036 | |||||
| PLL | 0.244/<0.001 |
Abbreviations: DLL, distal lumbar lordosis; LL, lumbar lordosis; PI, pelvic incidence; PLL, proximal lumbar lordosis; PT, pelvic tilt; SS, sacral slope; STA, sacral table angle.
Definitive statistics is given as r/p. P < .001 is significant. r = 0.2-0.39 weak; 0.4-0.69 moderate; and 0.7-0.89 strong correlations.
Figure 3.
Scatter plots of spinopelvic parameters. LL indicates lumbar lordosis; PI, pelvic incidence; PT, pelvic tilt; SS, sacral slope; STA, sacral table angle.
Discussion
In recent studies, increased hip joint loading due to spinopelvic sagittal balance changes, along with decreased femoral head coverage due to femoroacetabular impingement and posterior pelvic tilt, has been reported as a risk factor for HOA.11-13 It was reported that larger anterior inclination of the spine was associated with the HOA. 11 The increase in PT associated with decreased LL has been reported to cause decreased coverage of the anterior portion of the acetabulum especially in standing position.12,13
In their study of sagittal alignment of axial skeleton in reference to gravity lines, Hasegawa et al 14 showed that the hip axis (HA) was 1.4 cm anterior to the gravity line in normal population and never posterior to the gravity line. With aging, PT and knee flexion increases compensatory for spinopelvic alignment and gravity line shifts more anterior. This shift is associated with inefficient standing posture and increased hip joint loading. 15 Increased contact stress of hip joint plays an important role in the progression of HOA. 16 It has been shown that an increase in PT causes an increase in contact stress on the anterosuperior acetabulum hip joint. 17
Inai et al 18 found that hip joint contact force increased with the increase in hip extensor muscle strength accompanying hip joint flexion contracture. Association between increase of hip moment and hip joint loading was revealed. 19 Miura et al 15 studied the relationship between spinopelvic alignment and hip joint load and reported that hip joint contact force (HCF) and flexion moment of hip were strongly correlated with sagittal vertical axis but not correlated with other spinopelvic parameters. Although decrease of LL associates with high SVA, PT, and other pelvic parameters were not correlated with it. It was concluded that higher SVA was correlated with increased hip joint contact force which may contributed HOA development. In addition, no association between PI-LL imbalance and SVA or HCF was observed. In our study, we could not find a significant difference in PT and LL values as well as other spinopelvic parameters in terms of both HOA development and dysplasia. Spinopelvic imbalance is demonstrated as a potential cause of instability after primary total hip replacement,20,21 but relation of PI-LL imbalance and HOA is not well known. Prevalence of PI-LL mismatch in HOA patients was recently studied and values appear to vary widely. Some authors analyzed it by stratifying it into two groups as hyperlordotic (HL) and flatback (FB) type. Hip osteoarthritis patients in Japanese population reported to have 12% hyperlordotic type and 29% have flat back type PI-LL imbalance. 22 It was reported 24.8% and 16% respectively for HOA patients in United States. 23 We found these values as 25.7% and 6.1% respectively in our study. Some authors also studied it without stratifying. While Carender et al 24 reported prevalence of as 62.3%, Stefl et al 25 reported as 26.2% in their primary HOA series. We found it to be 31.8% in individuals with HOA. Although relatively high prevalence rates suggest that there may be a correlation between PI-LL imbalance and HOA, our results did not support this. We could not find any correlation between them in our study.
While Takemitsu et al 26 pointing out that an increase in PT values in the sagittal plane may lead to the insufficient covering in the anterior part of the femoral head and thus to the development of HOA even in patients with a normal AA, Yoshimoto et al 5 associated this increase in PT with high PI and low LL values and stated that high PI and high AA values may play a role in the development of HOA in older ages. In their study, there were significant but weak correlation between AA and LL-SS-PT. In contrast, Weng et al 27 stated that HOA patients have significantly lower PT and higher SS and more anteverted pelvis than normal group in their study. PI and LL values had no significant difference. Therefore, there is no clear consensus on the effect of PI and PT on HOA development. When comparing the spinopelvic parameters of HOA patients and age- and sex-matched control group, Okuda et al 28 concluded that LL and SS were similar in early stage HOA group with normal group but significantly greater in advanced HOA group. But Sariali et al 29 found patients with HOA had significantly low SS and comparable PI values than asymptomatic healthy group. Day et al 4 compared the some spinopelvic parameters between limited HOA and severe HOA groups. They reported less PT in severe HOA group in their study. PI-LL and LL were similar. Some authors regarded the hip joint to be an adjacent segment of the spine and reported the occurrence of HOA following spinal surgery.
It is reported that sacroiliac fixation was predictive for HOA development.30-32 In another study, the same authors even found that S2 alar-iliac (SI) screw loosening had a protective effect on HOA. High PI, SS, and PI-LL values were also found to be associated with the development of HOA, particularly after spinal fusion of four or more levels. Increased spinal fusion procedures appear to influence the development of HOA with adjacent segment effects. Patients with elevated PI, SS, and PI-LL imbalances are predicted to be significantly affected.
Although there were many studies investigating the relationship between PI, which is accepted as a fixed parameter, and PT, which is a compensatory variable parameter, and HOA, as far as we know, there is no study investigating the relationship between STA, which is also a fixed anatomical pelvic parameter, and HOA, dysplasia and PI-LL imbalance. It was concluded that STA can serve as good alternative index of PI. 33 Moreover, its measurement is easier and precise than PI measurement. We found no correlation between STA and them.
There are some limitations to our study. At first, the retrospective nature of the analysis and lacks longitudinal data. The confounders which may predispose HOA, such as genetic factors, history of trauma, alcohol or steroid use or high body mass index (BMI) were not known. Therefore, correlational analyses were conducted as rather than cause-and-effect analyses. Prospective longitudinal studies needed. Second, this study conducted with the cohort of subjects from our country which may not be generalizable to other populations because of the differences of mentioned parameters among ethnicities.
Conclusion
We observed that both constant and variable spinopelvic parameters had no effect on HOA development and hip dysplasia. PI-LL imbalance is also not associated with HOA and hip dysplasia. We did not find any evidence that PI and STA, as fixed morphological parameters, are a risk factor for HOA and dysplasia on their own.
Acknowledgments
None.
Footnotes
ORCID iD: Zafer Soydan  https://orcid.org/0000-0001-6387-8628
https://orcid.org/0000-0001-6387-8628
Declarations
Ethics Approval and Consent to Participate: All procedures performed on human participants in studies conformed to the ethical standards of the institutional and/or national research committee and to the 1964 Helsinki Declaration and its subsequent amendments or other comparable ethical standards. The Nisantasi University Faculty of Medicine Clinical Research Ethics Committee (date and number: 02.04.2022, 2022/10) approved the study. For publication of this article, patients’ verbal and written informed consent was obtained for the use of their medical data in this research study.
Author Contributions: Zafer Soydan: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing—original draft; Writing—review.
Emru Bayramoglu: Data curation; Investigation; Methodology; Project administration; Supervision; Validation; Writing—original draft.
Okyar Altas: Conceptualization; Data curation; Formal analysis; Investigation; Resources; Supervision; Validation; Visualization; Writing—original draft.
Cengiz Sen: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Resources; Supervision; Validation; Visualization; Writing—original draft.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of Data and Materials: The data used during the current study are available from the corresponding author on reasonable request.
References
- 1. Courties A, Berenbaum F. Is hip osteoarthritis preventable? Joint Bone Spine. 2020;87:371-375. doi: 10.1016/j.jbspin.2019.11.010 [DOI] [PubMed] [Google Scholar]
- 2. Neogi T, Zhang Y. Epidemiology of osteoarthritis. Rheum Dis Clin North Am. 2013;39:1-19. doi: 10.1016/j.rdc.2012.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gebhart JJ, Weinberg DS, Bohl MS, Liu RW. Relationship between pelvic incidence and osteoarthritis of the hip. Bone Joint Res. 2016;5:66-72. doi: 10.1302/2046-3758.52.2000552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Day LM, DelSole EM, Beaubrun BM, et al. Radiological severity of hip osteoarthritis in patients with adult spinal deformity: the effect on spinopelvic and lower extremity compensatory mechanisms. Eur Spine J. 2018;27:2294-2302. doi: 10.1007/s00586-018-5509-0 [DOI] [PubMed] [Google Scholar]
- 5. Yoshimoto H, Sato S, Masuda T, et al. Spinopelvic alignment in patients with osteoarthrosis of the hip: a radiographic comparison to patients with low back pain. Spine (Phila Pa 1976). 2005;30:1650-1657. doi: 10.1097/01.brs.0000169446.69758.fa [DOI] [PubMed] [Google Scholar]
- 6. Raphael IJ, Rasouli MR, Kepler CK, Restrepo S, Albert TJ, Radcliff KE. Pelvic incidence in patients with hip osteoarthritis. Arch Bone Jt Surg. 2016;4:132-136 [PMC free article] [PubMed] [Google Scholar]
- 7. Iwasa M, Ando W, Uemura K, Hamada H, Takao M, Sugano N. Pelvic incidence is not associated with the development of hip osteoarthritis. Bone Joint J. 2021;103-B:1656-1661. doi: 10.1302/0301-620X.103B11.BJJ-2021-0472.R1 [DOI] [PubMed] [Google Scholar]
- 8. Saltychev M, Pernaa K, Seppänen M, Mäkelä K, Laimi K. Pelvic incidence and hip disorders. Acta Orthop. 2018;89:66-70. doi: 10.1080/17453674.2017.1377017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. van Erp JHJ, Gielis WP, Arbabi V, et al. Unravelling the knee-hip-spine trilemma from the CHECK study. Bone Joint J. 2020;102-B:1261-1267. doi: 10.1302/0301-620X.102B9.BJJ-2019-1315.R2 [DOI] [PubMed] [Google Scholar]
- 10. Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976). 2010;35:2224-2231. doi: 10.1097/BRS.0b013e3181ee6bd4 [DOI] [PubMed] [Google Scholar]
- 11. Tateuchi H, Akiyama H, Goto K, So K, Kuroda Y, Ichihashi N. Sagittal alignment and mobility of the thoracolumbar spine are associated with radiographic progression of secondary hip osteoarthritis. Osteoarthritis Cartilage. 2018;26:397-404. doi: 10.1016/j.joca.2017.12.005 [DOI] [PubMed] [Google Scholar]
- 12. Watanabe W, Sato K, Itoi E, Yang K, Watanabe H. Posterior pelvic tilt in patients with decreased lumbar lordosis decreases acetabular femoral head covering. Orthopedics. 2002;25:321-324. doi: 10.3928/0147-7447-20020301-16 [DOI] [PubMed] [Google Scholar]
- 13. Mekhael M, Kawkabani G, Saliby RM, et al. Toward understanding the underlying mechanisms of pelvic tilt reserve in adult spinal deformity: the role of the 3D hip orientation. Eur Spine J. 2021;30:2495-2503. doi: 10.1007/s00586-021-06778-4 [DOI] [PubMed] [Google Scholar]
- 14. Hasegawa K, Okamoto M, Hatsushikano S, et al. Standing sagittal alignment of the whole axial skeleton with reference to the gravity line in humans. J Anat. 2017;230:619-630. doi: 10.1111/joa.12586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Miura T, Miyakoshi N, Saito K, et al. Association between global sagittal malalignment and increasing hip joint contact force, analyzed by a novel musculoskeletal modeling system. PLoS ONE. 2021;16:e0259049. doi: 10.1371/journal.pone.0259049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Recnik G, Kralj-Iglic V, Iglic A, et al. The role of obesity, biomechanical constitution of the pelvis and contact joint stress in progression of hip osteoarthritis. Osteoarthritis Cartilage. 2009;17:879-882. doi: 10.1016/j.joca.2008.12.006 [DOI] [PubMed] [Google Scholar]
- 17. Kitamura K, Fujii M, Utsunomiya T, et al. Effect of sagittal pelvic tilt on joint stress distribution in hip dysplasia: a finite element analysis. Clin Biomech (Bristol, Avon). 2020;74:34-41. doi: 10.1016/j.clinbiomech.2020.02.011 [DOI] [PubMed] [Google Scholar]
- 18. Inai T, Edama M, Takabayashi T, Kubo M. Relationship between hip flexion contracture and hip-joint contact force in standing posture: a computer simulation study. J Ergonomics. 2017;7:1000194. doi: 10.4172/2165-7556.1000194 [DOI] [Google Scholar]
- 19. Bergmann G, Bender A, Dymke J, Duda GN, Damm P. Physical activities that cause high friction moments at the cup in hip implants. J Bone Joint Surg Am. 2018;100:1637-1644. doi: 10.2106/JBJS.17.01298 [DOI] [PubMed] [Google Scholar]
- 20. Esposito CI, Carroll KM, Sculco PK, Padgett DE, Jerabek SA, Mayman DJ. Total hip arthroplasty patients with fixed spinopelvic alignment are at higher risk of hip dislocation. J Arthroplasty. 2018;33:1449-1454. doi: 10.1016/j.arth.2017.12.005 [DOI] [PubMed] [Google Scholar]
- 21. Heckmann N, McKnight B, Stefl M, Trasolini NA, Ike H, Dorr LD. Late dislocation following total hip arthroplasty: spinopelvic imbalance as a causative factor. J Bone Joint Surg Am. 2018;100:1845-1853. doi: 10.2106/JBJS.18.00078 [DOI] [PubMed] [Google Scholar]
- 22. Kobayashi T, Morimoto T, Yoshihara T, Sonohata M, Rivière C, Mawatari M. The significant relationship among the factors of pelvic incidence, standing lumbar lordosis, and lumbar flexibility in Japanese patients with hip osteoarthritis: a descriptive radiographic study. Orthop Traumatol Surg Res. 2022;108:103123. doi: 10.1016/j.otsr.2021.103123 [DOI] [PubMed] [Google Scholar]
- 23. Buckland AJ, Ayres EW, Shimmin AJ, Bare JV, McMahon SJ, Vigdorchik JM. Prevalence of sagittal spinal deformity among patients undergoing total hip arthroplasty. J Arthroplasty. 2020;35:160-165. doi: 10.1016/j.arth.2019.08.020 [DOI] [PubMed] [Google Scholar]
- 24. Carender CN, Meyer MD, Wynn MS, Bedard NA, Otero JE, Brown TS. The prevalence of abnormal spinopelvic relationships in patients presenting for primary total hip arthroplasty. Arthroplast Today. 2020;6:381-385. doi: 10.1016/j.artd.2020.05.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Stefl M, Lundergan W, Heckmann N, et al. Spinopelvic mobility and acetabular component position for total hip arthroplasty. Bone Joint J. 2017;99-B:37-45. doi: 10.1302/0301-620X.99B1.BJJ-2016-0415.R1 [DOI] [PubMed] [Google Scholar]
- 26. Takemitsu Y, Harada Y, Iwahara T, Miyamoto M, Miyatake Y. Lumbar degenerative kyphosis: Clinical, radiological and epidemiological studies. Spine (Phila Pa 1976). 1988;13:1317-1326. [PubMed] [Google Scholar]
- 27. Weng WJ, Wang WJ, Wu MD, Xu ZH, Xu LL, Qiu Y. Characteristics of sagittal spine-pelvis-leg alignment in patients with severe hip osteoarthritis. Eur Spine J. 2015;24:1228-1236. doi: 10.1007/s00586-014-3700-5 [DOI] [PubMed] [Google Scholar]
- 28. Okuda T, Fujita T, Kaneuji A, Miaki K, Yasuda Y, Matsumoto T. Stage-specific sagittal spinopelvic alignment changes in osteoarthritis of the hip secondary to developmental hip dysplasia. Spine (Phila Pa 1976). 2007;32:E816-E819. doi: 10.1097/BRS.0b013e31815ce695 [DOI] [PubMed] [Google Scholar]
- 29. Sariali E, Lazennec JY, Khiami F, Gorin M, Catonne Y. Modification of pelvic orientation after total hip replacement in primary osteoarthritis. Hip Int. 2009;19:257-263. doi: 10.1177/112070000901900312 [DOI] [PubMed] [Google Scholar]
- 30. Kozaki T, Hashizume H, Nishiyama D, et al. Adjacent segment disease on hip joint as a complication of spinal fusion surgery including sacroiliac joint fixation. Eur Spine J. 2021;30:1314-1319. doi: 10.1007/s00586-020-06700-4 [DOI] [PubMed] [Google Scholar]
- 31. Kawai T, Shimizu T, Goto K, et al. The impact of spinopelvic parameters on hip degeneration after spinal fusion. Spine (Phila Pa 1976). 2022;47:1093-1102. doi: 10.1097/BRS.0000000000004340 [DOI] [PubMed] [Google Scholar]
- 32. Kozaki T, Hashizume H, Taniguchi T, et al. S2 alar-iliac screw loosening as a preventive factor for hip joint osteoarthritis after adult spinal deformity surgery: a case-control study. Eur Spine J. 2022;31:3081-3088. doi: 10.1007/s00586-022-07344-2 [DOI] [PubMed] [Google Scholar]
- 33. Ru N, Li J, Li Y, Sun J, Wang G, Cui X. Sacral anatomical parameters varies in different Roussouly sagittal shapes as well as their relations to lumbopelvic parameters. JOR Spine. 2021;4:e1180. doi: 10.1002/jsp2.1180 [DOI] [PMC free article] [PubMed] [Google Scholar]



