Abstract
Background
Inpatients commonly experience problems with elimination due to incontinence, urinary retentions, and complications with indwelling catheters. Although elimination care (EC) is an important nursing area, few studies explore the burden of EC on nurses.
Aim
To identify the burden on EC by analyzing nurses’ opinions using sequential explanatory mixed method.
Methods
This research was conducted using a sequential explanatory mixed-methods design. A total of 59 nurses at a tertiary hospital in South Korea participated in the study from January 1 to March 31, 2022. For quantitative analysis, information about number of delays of work due to EC, required time for serving bedpan or diaper changes, percentage of EC per shift, and percentage of patients who need EC was collected through a survey. For qualitative analysis, focus group interviews were conducted to identify factors that put a burden on EC. Important themes were derived by analyzing nurses’ opinions on EC.
Results
For nurses in intensive care units, general wards, and integrated nursing care wards, the number of work delays due to EC was 3.6 ± 1.5, 2.3 ± 1.2, and 4.8 ± 2.4 (p<0.01), respectively. The mean percentage of EC work out of total nursing tasks per shift was 36.2 ± 19.0, 29.3 ± 14.4, and 43.8 ± 14.1 (p=0.02), respectively. The mean percentage of patients requiring EC out of patients a nurse cares was 85.4 ± 16.6, 41.3 ± 26.1, and 58.8 ± 21.9 (p<0.01), respectively. Following qualitative analysis, four themes related to nurses’ EC burden were derived: physical burden, frequent care needs, delay of other jobs due to EC, and complications. Among them, frequent care needs were found to be the primary factor requiring consideration to reduce nurses’ burden.
Conclusion
This research found that EC is one of the most burdensome tasks that nurses want to avoid. To alleviate their burden, effective EC protocol or smart medical devices assisting with EC should be developed.
Keywords: nursing, elimination care, mixed-methods approach
Background
Inpatients commonly experience problems with elimination.1 According to a systematic review exploring the effectiveness of nursing interventions for eliminations, approximately 40% of 7361 patients experienced incontinence, 34% had urinary retention, and 31% had indwelling catheters.2 According to a previous study by Johnson et al, more than 85% and 77% of elderly patients in long-term care facilities depend on diapers and urinary catheterization, respectively.3 These problems are also related to other complications including urinary tract infections.4 Diapers used to manage fecal or urinary incontinence are a major aggravating factor for pressure sores or incontinence associated dermatitis (IAD).5 In addition, the elderly are particularly susceptible to the risk of falling when they frequently visit restrooms due to elimination.6 Therefore, elimination care (EC) by nurses is an important nursing task and has a significant effect on the patient’s safety and quality of life.7,8
The EC consists of addressing individuals’ toileting needs and assisting them in eliminating urine and feces through conventional means or catheterization,2 which includes clean intermittent catheterization, Foley catheterization, perineal care, and enema.9,10 EC is usually required frequently during the day, and a significant duration of time is required to complete the task. Therefore, nurses may be delayed in their primary nursing tasks because of frequent EC, resulting in an increased workload. Increased workload and the required intensity of care contribute to job dissatisfaction and intentions to leave the job. A previous study conducted in Nordic countries, including Finland, Norway and Sweden, have reported that an increase in the number of patients requiring assistance with activities of daily living is associated with nurses’ job dissatisfaction and intention to turnover.11 However, few studies reported on how an increased workload by EC places burdens on nurses and affects their job dissatisfaction.
As the Internet of Things related systems and Health Information technologies (HIT) develop, intelligent devices that reduce nurses’ increased workload and support EC are introduced. For example, there are wireless systems that monitor diaper wetness,12–16 a carebidet robot that detects and sucks urine and feces and cleans and dries the skin,17 and a robot that transfers patients between a wheelchair/bed and a toilet.18,19 However, these devices remain limitedly adopted in nursing since they have not been as helpful as expected in reducing the EC burden on nurses and their effectiveness has not been thoroughly verified.
To resolve ineffective EC, the first step should be analyzing and clarifying the nurses’ opinions on EC. However, there have been few studies or investigations on the burdensome factors of EC and which factors could be supported by devices. Several studies investigated musculoskeletal disorders in nurses due to EC, in which the incidence of musculoskeletal disorders or back pain due to EC’s physical work, such as diaper replacement, were high at 49–84%.20–23 According to a study by Saga et al, which examined registered nurses’ (RN) management for nursing home residents’ bowel problems, the RNs felt that they spent a great deal of time toileting residents, and they reported bowel care management as a challenge due to limited time, resources, and organizational conditions.24 However, the results of that singular study do not allow us to understand nurses’ actual struggles with EC.
Therefore, this study aims to identify the burden on EC by analyzing nurses’ opinion with a sequential explanatory mixed-methods design to help researchers develop new nursing protocols or medical devices based on HIT assisting EC.
Materials and Methods
Setting
This study was conducted in a tertiary hospital with 1335 beds in South Korea. The wards in the hospital are divided into general wards (GWs), integrated nursing care wards (INCWs), and intensive care units (ICUs) according to the type of nursing care and patient acuity. A nurse in GWs is usually in charge of 16 (interquartile range: 12–24) patients.25 Fundamental nursing care in GWs, such as EC, bathing, and feeding, are usually supported by family members or caregivers. In terms of EC, nurses support changing diapers or primarily recording the amount of intake and output. The INCWs were first nationally promoted in 2016 to reduce the economic burdens of nursing care for the public, while improving the quality of hospitalization services.26 The INCWs provide 24-hours of comprehensive inpatient care by professionally trained nurses without informal caregivers, as also applied in ICUs.27 All fundamental nursing care in INCWs and ICUs, including EC, are provided by professionally trained nurses. However, the number of patients per nurse in the INCWs is normally five to six, which is higher than that of ICUs, which is two to three.
Study Design
Implementing a sequential explanatory mixed-methods design, this study seeks to analyze nurses’ perspectives on EC. The method incorporates a two-phase procedure, beginning with a quantitative survey, followed by qualitative focus group interviews (FGIs) to form a comprehensive understanding of the subject matter. This design was selected to take advantage of the strength of both methods, to cross-validate, complement, and expand the findings, creating a holistic understanding of the EC burden from the perspective of nurses. In the first phase, quantitative data is collected and analyzed to provide a broad overview of nurses’ opinions on EC. Subsequently, these results form the basis for the qualitative FGIs conducted in the second phase. The amalgamation of these two types of data enables a detailed exploration of nurses’ viewpoints on EC and allows researchers to develop a robust and nuanced understanding of the topic. This, in turn, aims to contribute to the development of new nursing protocols or medical devices, particularly those leveraging Health Information Technology (HIT) to assist EC, thereby aligning with the study’s initial objective.28
Data Collection
Study participants were solicited from all departments across the hospital without any exclusions. This approach was taken to ensure the acquisition of diverse opinions and perspectives pertaining to work environments, thereby enhancing the breadth of data. In terms of sampling method, a purposive sampling technique was utilized. Purposive sampling is a non-probability sampling method where researchers select participants based on their judgement of who would be most beneficial or representative for the study. This approach allows for a more focused and relevant data collection, as it ensures that participants have specific characteristics or experiences relevant to the study’s subject matter. In this case, participants were selected based on their diverse experiences across the various hospital departments, thereby ensuring a wide range of perspectives on EC in different work environments.29 By using the sampling method, this study could include nurses evenly from GWs, INCWs, and ICUs. Following recruitment, the researchers surveyed the participants to quantify the nurses’ EC burden, gathering data on the frequency of work delays due to EC, time required for serving bedpan or diaper changes, proportion of EC tasks per shift, and the percentage of patients needing EC. FGIs were conducted after the survey allowing nurses to provide thorough reasons for their EC burden. The researchers gathered the participants into seven groups; the FGIs were conducted by a researcher with a master’s degree in nursing and a researcher with a bachelor’s degree in natural sciences. Participants from the same ward were placed into a single group to encourage them to speak more freely to one another in an open atmosphere. The interviews were voice-recorded with the participants’ consent, lasting between 30 to 40 minutes. The recorded material was independently transcribed by two researchers, and the transcriptions were then cross-verified by three independent researchers. All individuals participated and signed the consent document voluntarily and were informed of their right to withdraw from the study at any time. During the FGIs, the researchers referred to the predefined semi-structured interview questionnaire that covered all topics related to their experiences and opinions regarding patient care. Important factors were derived that place a burden on nurses’ work when conducting EC. The qualitative analysis followed the COREQ-36 guidelines.30
Data Analysis
For the quantitative analysis, data were described as mean ± standardized deviation and percentage (%). Analysis of Variance and the Kruskal–Wallis test were conducted to compare each group. All statistical analyses were performed using R version 4.0.4 (R Foundation for Statistical Computing, Vienna, Austria), and P<0.05 was considered to be statistically significant.
The qualitative data was analyzed using a thematic analysis approach. Initially, two independent researchers reviewed the content from the interviews and derived initial themes. In instances where there was disagreement on a particular theme, a discussion was initiated among all the researchers until consensus was reached. Following this, the derived themes were analyzed for similarities and differences and subsequently grouped into higher-order abstracted themes. This approach allowed for a comprehensive exploration of the data and ensured that the insights gathered were reflective of the participants’ experiences and opinions.
Data Integration
The data integration process was conducted in the methods, and interpretation (discussion) stage of this study. Through the sequential explanatory mixed-methods approach, the researchers integrated quantitative and qualitative data. Results from the survey were used to gather participants’ in-depth opinions on EC. In discussion, the quantitative and qualitative data were analyzed together to provide comprehensive insights, called the “merging” process.31 For instance, the survey results on the percentage of EC work per shift and percentage of patients requiring EC were compared to the FGI results on nurses’ opinions as to why they have an increased workload or EC burden.
Results
A total of 59 nurses completed the questionnaire and participated in the FGIs (Table 1). Majority of the participants were women, aged between 20 and 39 years. A total of 13 participants were from GWs, 30 from INCWs, and 16 from ICUs, and over 86% of participants had three or more years of nursing experience.
Table 1.
Survey and Focus Group Participants’ Characteristics (n = 59)
| Characteristics | n (%) |
|---|---|
| Gender | |
| Man | 2 (3) |
| Woman | 57 (97) |
| Age (years) | |
| 20–29 | 29 (49) |
| 30–39 | 22 (37) |
| 40–49 | 7 (12) |
| 50–59 | 1 (2) |
| Career (years) | |
| 1–2 | 9 (14) |
| 3–5 | 31 (53) |
| 6–9 | 9 (16) |
| ≥10 | 10 (17) |
| Department | |
| Intensive care unit | 13 (22) |
| General ward | 30 (51) |
| Integrated nursing care ward | 16 (27) |
Quantitative Analysis
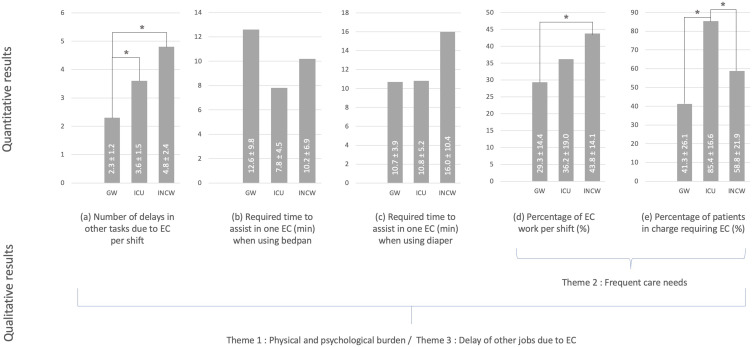
The nurses’ EC burden was measured in four components (Figure 1). Number of delays in other tasks due to EC were 2.3 ± 1.2, 3.6 ± 1.5, and 4.8 ± 2.4, respectively for GWs, ICUs, and INCWs. The delays due to EC were more frequent in ICUs and INCWs than that in GWs with statistical significance (Figure 1a). No statistical differences were found in the required time to assist with one EC task when using bedpans and diapers. (Figure 1b and c). The required time to complete one EC task ranged from 7.8 to 16.0 minutes. In addition, no difference was found in the percentage of EC work per shift between GWs and ICUs; however, the percentage was higher in INCWs than in GWs (43.8 ± 14.1 in INCW vs 29.3 ± 14.4 in GWs) (Figure 1d). The percentage of patients requiring EC in ICUs was higher than that in GWs or INCWs with statistical significance (85.4 ± 16.6 in ICUs vs 41.3 ± 26.1 in GWs or 58.8 ± 21.9 in INCW) (Figure 1e).
Figure 1.
Burden of elimination care. The subparts (a–e) in the figure are indicators of quantifying the nurses’ EC burden. (* p<0.05).
Abbreviations: GW, General ward; ICU, Intensive care unit; INCW, Integrated nursing care ward; EC, Elimination care.
Qualitative Analysis
A total of four themes related to EC were derived from qualitative analysis (Table 2).
Table 2.
Themes and Categories of Results from Qualitative Analysis
| Themes | Categories | Frequency of Extracts |
|---|---|---|
| Physical/psychological burden | Burden of musculoskeletal pain due to patients’ weight | 36 |
| Burden due to odor or form of excrement | 11 | |
| Frequent care needs | Burden due to incontinence | 10 |
| Burden due to urinary retention | 6 | |
| Delay of other jobs | Delay of other jobs or tasks due to bed contamination | 6 |
| Delay of other jobs or tasks due to irregular or unexpected elimination care | 17 | |
| Complications | Skin problems from inadequate elimination care | 29 |
| Disconnection of medical devices during elimination care | 5 |
Theme 1: Physical / Psychological Burden
This theme reflects the direct impact of providing EC on the physical and psychological wellbeing of nurses. The physical strain often leads to musculoskeletal pain, especially when the nurse needs to lift or change the position of heavier patients. Moreover, the unpleasant odor and form of excrement add to the psychological stress of the care providers.
Burden of Musculoskeletal Pain Due to Patients’ Weight
Musculoskeletal pain due to EC was mentioned frequently as one of the most common ailments among nurses because they often lifted patients during EC.
P15: Suffer from back and wrist pain when the patients weigh more.
P49: I am sure that changing the patient’s position or providing patients’ EC is among the top three most difficult parts of a nurse’s role regardless of the severity of the disease.
Burden Due to Odor or Form of Excrement
Hematochezia and unpleasant odor were other reasons nurses found EC to be their most difficult task.
P06: The smell of hematochezia makes me mentally tired.
P29: When nursing a patient who continues to have diarrhea, the smell and shape of the bowel are burdensome every time.
Theme 2: Frequent Care Needs
This theme emphasizes the repetitive and time-consuming nature of providing EC. Particularly, the need for frequent diaper changes due to incontinence or bowel irregularities, and the necessity of clean intermittent catheterization for patients with urinary retention, place an additional burden on the nursing staff.
Burden Due to Incontinence
Participants responded that bowel irregularities were one of the most burdensome aspects of EC. Diaper replacement and changing the patient’s position should be done once every eight hours and once every two hours, respectively; however, EC should be done more frequently if the patient has bowel irregularities, such as severe diarrhea.
P07: I should change diapers multiple times a day if the patient has severe diarrhea.
Burden Due to Urinary Retention
Clean intermittent catheterization should be applied frequently to patients who cannot urinate independently. Participants mentioned this as one burdensome factor of EC.
P27: We regularly urinate patients who can’t urinate themselves. If there are many such patients, it can be a burden.
Theme 3: Delay of Other Jobs
This theme highlights the interruptions caused by unexpected or irregular EC tasks, which impact the flow of nurses’ regular tasks and consequently increase the nursing burden.
This theme was closely related to unexpected or irregular EC. Participants repeatedly mentioned the unexpectedness of EC as the most difficult aspect, increasing the nursing burden.
Delay of Other Jobs or Tasks Due to Bed Contamination
P47: Bed contamination is common when EC is performed on patients with continuous diarrhea. In this case, it will interfere with other tasks.
P03: If bed contamination occurs due to feces, it is often difficult to do other tasks.
Delay of Other Jobs or Tasks Due to Irregular or Unexpected EC
P46: Usually, if it is difficult for the caregiver to do alone, the nurse sometimes helps; but honestly, it is not the nurse’s job in the GWs, but helping often hinders other tasks.
P43: When working in a INCW, EC accounts for a large portion of work, and every time EC is performed, important work is often delayed.
P10: It is most difficult to manage irregular urination or defecation, such as diarrhea or defecation immediately after elimination care.
Theme 4: Complications
This theme encapsulates the complications that arise due to inadequate EC, emphasizing their significance for effective EC. Participants responded that complications caused by inadequate EC are important considerations for effective EC.
Skin Problems from Inadequate EC
The occurrence of skin damage due to excretion and sustained enema caused by constipation were found to be difficult factors of EC. Many participants stated that conscious patients are unwilling to inform nurses about needing EC due to humiliation. However, as the skin is exposed to excretion waste, IAD can develop, which not only increases the patients’ hospitalization period but may also lead to death in worst-case scenarios. Moreover, if the patient experiences skin damage, more care must be performed, which further increases nurses’ workload.
P50: Patients who wear diapers tend to develop incontinence-related dermatitis if they are not taken care of well. It’s important to take care of it so that it doesn’t happen, but I think it’s hard. Furthermore, inadequate EC can exacerbate pressure sores.
Disconnection of Medical Devices During EC
In addition, participants worried about unexpected disconnection of medical devices during EC. In particular, ICUs use various patient monitoring medical devices, and changing a patient’s position is often necessary during a diaper change, increasing nurses’ EC burden.
P13: Since everyone is using medical devices, the most common accident is that they often fall into their intubation while cleaning up their bowel movements. That’s hard. Of the things that I do not want to do, I hate it the most.
Discussion
This study analyzed the opinions of 59 nurses and the factors for effective EC using a sequential explanatory mixed-methods design. Based on the mixed-methods approach, this research provides a comprehensive understanding of the burden of EC on nurses, combining both quantitative and qualitative insights.
The quantitative results suggested that delays due to EC were more prevalent in ICUs and INCWs compared to GWs. Interestingly, there was no significant difference found in the time required for one EC task across all wards, showing a general consistency in the time commitment for EC. Meanwhile, the proportion of EC work per shift was significantly higher in INCWs, and the percentage of patients requiring EC was markedly higher in ICUs. This is likely due to the fact that a nurse typically cares for a larger number of patients in INCWs compared to ICUs. However, ICUs often care for more severely injured patients. These findings suggest that customized protocols or medical devices may be necessary, taking into account the distinct characteristics of nursing services and patient acuity in each ward.
The qualitative analysis provided further insights into the nature of the EC burden, shedding light on four critical themes: physical/psychological burden, frequent care needs, delay of other tasks, and complications. Nurses reported musculoskeletal pain, discomfort due to the odor and form of excrement, and psychological stress as part of their EC-related burden. The need for frequent care, such as diaper changes and catheterizations, was highlighted as a significant issue. EC also led to delays in other tasks, especially when unexpected or irregular EC occurred. Furthermore, complications from inadequate EC, such as skin problems or disconnection of medical devices, added to the workload and stress of the nurses.
In synthesizing these findings, it is clear that while time requirements for individual EC tasks may be consistent, the overall burden of EC is multi-dimensional and significantly influenced by the ward type, patient condition, and unexpected EC needs. The integration of these quantitative and qualitative results illuminates the complexity of the EC burden on nurses, suggesting that strategies to mitigate this burden must consider both operational efficiency and the lived experiences of nurses.
This study’s novelty is that it identified nurses’ difficulties and burdens when performing EC, which was not known previously. First, the findings of this study suggest that EC increases nurses’ physical burden and, consequently, is highly likely to cause physical symptoms, such as musculoskeletal pain or musculoskeletal disorders. In the quantitative analyses, the percentage of patients requiring EC (41.3~85.4%) and the percentage of EC work per shift (29.3~43.8%) were higher than expected. In addition, through FGIs, participants mentioned musculoskeletal pain as one of the most common ailments among nurses since EC requires lifting or moving patients. According to a previous study by Choi et al, nurses’ and nursing assistants’ work-related musculoskeletal risks increase when they lift or move patients manually.22 In particular, the prevalence of lower back pain was measured as high at 63% (95% Confidence Interval (CI): 57.4–68.5) and 61.2% (95% CI: 55.7–66.7) during the nurses’ work life and within the last year, respectively.21 Although EC is not the only reason for the high prevalence of lower back pain, improved protocol or special medical devices for effective EC should be developed to reduce the nurses’ physical burden.
Second, frequent care needs associated with the unexpectedness and irregularity of EC was an important factor contributing to EC burden. In particular, in the INCWs and ICUs, where nurses are responsible for all processes of EC, the EC burden was greater than in GWs. In the previous study,27 nurses in INCWs commented positively on the prospects for robotic care to reduce stress and somatic symptoms caused by increased workload. Although “measuring/monitoring”, “mobility/activity”, and “safety care” were selected as the top-three desired roles for care robots, the nurses expected that the workload related to “urination/excretion” and “hygiene care” would also decrease by using the care robots. According to a study by Han et al32 which explored the nursing workflow of ICU RNs in China, nurses spent most of their time in direct nursing care (51.27%). Among direct nursing care, the frequency of and time spent in basic nursing and basic operations including EC, such as excretion assistance, enema, and perineal irrigation care, were higher than other activities. As nurses organize work to accommodate their shift time, frequent and unexpected EC can interrupt their organization and planned work. Thus, if EC efficiency is achieved using care robots or effective protocols, the time and frequency for nursing processes, such as problem assessment or nursing evaluation, can be increased.
Furthermore, this study found that complications occurring during EC or due to incorrect EC are important aspects to consider for improving EC. Complications that can occur due to elimination include the spread of hospital-acquired infections (eg, Clostridium difficile), delirium, and urinary tract infections. Participants mentioned that IAD aggravated by inadequate EC and the disconnection of medical devices during EC should be considered to perform effective EC. Effective EC may reduce risk for skin disorder and improve biological markers as shown in a previous study using a carebidet robot in an ICU.17 Shin, Kim, Jang, and Kim (2021)17 investigated the effects of carebidet robot-assisted EC on the risk of IAD and pressure ulcer in patients admitted to an ICU. The carebidet robot had functions of sensing diaper wetness, inhaling urine or feces, washing, and drying the skin. The study demonstrated that carebidet robot was more effective than the usual EC in reducing IAD, pressure ulcer risk, and improving biological markers, such as serum albumin and lymphocyte, in ICU. Therefore, smart medical devices such as a carebidet robot, can be used to improve basic nursing care including EC in the hospital setting and nursing home by supporting patient safety and the quality of care.33
Limitations
There are several limitations in this research. First, the research data were only from one tertiary hospital. To generalize the results of the study, multi-center studies are needed in the future. Second, the researcher’s personal perspective may have affected the interpretation of qualitative analysis. However, the researchers adhered to the guidance of COREQ-36 and cross-validated deducted themes from multiple researchers to minimize the potential biases. Third, nursing environments experiences with EC can vary from hospital to hospital or country to country. Therefore, the results in this research may not be transferrable to other situations. However, the researchers wanted to address nurses’ EC burden, and the innate characteristics of patients’ elimination and EC are generalizable; thus, researchers in different environments can learn from this study. Fourth, working time spent on EC, number of work delays due to EC, the percentage of EC per shift, and the percentage of patients requiring EC were values estimated by nurses, not values calculated using scientific tools or time-motion study. Therefore, in the near future, it is necessary to conduct research that identifies the nursing tasks delayed due to frequent EC by analyzing nursing records and measuring the actual time spent performing EC.
Conclusions
This study explored the EC burden placed on nurses and the factors necessary for effective EC. This research found that EC is one of the most burdensome tasks that nurses want to avoid, and nurses’ EC burdens include physical/psychological burden, frequent care needs, delay of other jobs due to bed contamination or irregular and unexpected EC, and complications due to EC. To develop effective protocols or medical devices that reduce nurses’ burdens and minimize delays in other nursing tasks and complication caused by EC, researchers should understand nurses’ opinions concerning the current status of EC.
Acknowledgments
The authors would like to acknowledge the participants of this study for their time and honest responses. The authors also thank staff members at the CR center for their assistance with participant recruitment.
Funding Statement
This work was supported by the Korea Medical Device Development Fund grant funded by the South Korean government (Ministry of Science and ICT, Ministry of Trade, Industry and Energy, Ministry of Health & Welfare, Ministry of Food and Drug Safety; Project Number: 202016B03, KMDF_PR_20200901_0157).
Data Sharing Statement
The datasets generated and/or analyzed in this study are not publicly available due to confidentiality but are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
This research had been performed in accordance with the Declaration of Helsinki and had been approved by the Institutional Review Board of Human Research of SNUBH, Republic of Korea. (Protocol No. B-2102-667-308) Written informed consent to participate in the study was obtained from the participants. Participants informed consent included publication of anonymized responses.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Choi E-J, Lee Y-S, Yang E-J, Kim J-H, Kim Y-H, Park H-A. Characteristics and risk factors for falls in tertiary hospital inpatients. J Korean Acad Nurs. 2017;47(3):420–430. doi: 10.4040/jkan.2017.47.3.420 [DOI] [PubMed] [Google Scholar]
- 2.Richards DA, Hilli A, Pentecost C, Goodwin VA, Frost J. Fundamental nursing care: a systematic review of the evidence on the effect of nursing care interventions for nutrition, elimination, mobility and hygiene. J Clin Nurs. 2018;27(11–12):2179–2188. doi: 10.1111/jocn.14150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Johnson TM, Ouslander JG, Uman GC, Schnelle JF. Urinary incontinence treatment preferences in long‐term care. J Am Geriatr Soc. 2001;49(6):710–718. doi: 10.1046/j.1532-5415.2001.49146.x [DOI] [PubMed] [Google Scholar]
- 4.Lukacz ES, Santiago-Lastra Y, Albo ME, Brubaker L. Urinary incontinence in women: a review. JAMA. 2017;318(16):1592–1604. doi: 10.1001/jama.2017.12137 [DOI] [PubMed] [Google Scholar]
- 5.Bender JK, Faergemann J, Sköld M. Skin health connected to the use of absorbent hygiene products: a review. Dermatol Ther. 2017;7(3):319–330. doi: 10.1007/s13555-017-0189-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pahwa AK, Andy UU, Newman DK, Stambakio H, Schmitz KH, Arya LA. Noctural enuresis as a risk factor for falls in older community dwelling women with urinary incontinence. J Urol. 2016;195(5):1512–1516. doi: 10.1016/j.juro.2015.11.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coggrave M. Neurogenic continence. Part 3: bowel management strategies. Br J Nurs. 2008;17(15):962–968. doi: 10.12968/bjon.2008.17.15.30698 [DOI] [PubMed] [Google Scholar]
- 8.Sharma P, Bhutta BS. Assisting Patients With Elimination. In: StatPearls. StatPearls Publishing; 2022. [PubMed] [Google Scholar]
- 9.Yu S-M, Choi D, Jeong HS, Sohng K-Y. Critical review iii to standardize the textbooks of fundamentals of nursing: nutrition, urinary and bowel elimination needs. J Korean Acad Fundam Nurs. 2021;28(1):105–120. doi: 10.7739/jkafn.2021.28.1.105 [DOI] [Google Scholar]
- 10.Kim S, Lee K-H, Hwang H, Yoo S. Analysis of the factors influencing healthcare professionals’ adoption of mobile electronic medical record (EMR) using the unified theory of acceptance and use of technology (UTAUT) in a tertiary hospital. BMC Med Inform Decis Mak. 2016;16:12. doi: 10.1186/s12911-016-0249-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lindqvist R, Smeds Alenius L, Runesdotter S, et al. Organization of nursing care in three Nordic countries: relationships between nurses’ workload, level of involvement in direct patient care, job satisfaction, and intention to leave. BMC Nurs. 2014;13(1):1–13. doi: 10.1186/1472-6955-13-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ang L, Ow S, Seng K, et al. Wireless Intelligent Incontinence Management System Using Smart Diapers. IEEE; 2008:69–72. [Google Scholar]
- 13.Wai AAP, Foo SF, Jayachandran M, et al. Towards Developing Effective Continence Management Through Wetness Alert Diaper: Experiences, Lessons Learned, Challenges and Future Directions. IEEE; 2010:1–8. [Google Scholar]
- 14.Fuketa H, Yoshioka K, Yokota T, et al. 30.3 Organic-Transistor-Based 2kV ESD-Tolerant Flexible Wet Sensor Sheet for Biomedical Applications with Wireless Power and Data Transmission Using 13.56 MHz Magnetic Resonance. IEEE; 2014:490–491. [Google Scholar]
- 15.Nilsson H-E, Sidén J, Gulliksson M. An Incontinence Alarm Solution Utilizing RFID Based Sensor Technology. IEEE; 2011:359–363. [Google Scholar]
- 16.Yamada K, Toshiaki N, Ishihara K, et al. Development of New Type Incontinence Sensor Using RFID Tag. IEEE; 2010:2695–2700. [Google Scholar]
- 17.Shin NY, Kim TG, Jang JY, Kim MY. The effects of carebidet robot during defecation on incontinence associated dermatitis, pressure ulcer risk, and biological markers in critical care patients. J Digit Converg. 2021;19(12):649–660. [Google Scholar]
- 18.Homma K, Yamada Y, Matsumoto O, et al. A Proposal of a Method to Reduce Burden of Excretion Care Using Robot Technology. IEEE; 2009:621–625. [Google Scholar]
- 19.Wang Y, Wang S. Development of an Excretion Care Support Robot with Human Cooperative Characteristics. IEEE; 2015:6868–6871. [DOI] [PubMed] [Google Scholar]
- 20.Soylar P, Ozer A. Evaluation of the prevalence of musculoskeletal disorders in nurses: a systematic review. Med Sci. 2018;2018:1. doi: 10.5455/medscience.2017.06.8747 [DOI] [Google Scholar]
- 21.Azizpour Y, Delpisheh A, Montazeri Z, Sayehmiri K. Prevalence of low back pain in Iranian nurses: a systematic review and meta-analysis. BMC Nurs. 2017;16:50. doi: 10.1186/s12912-017-0243-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Choi SD, Brings K. Work-related musculoskeletal risks associated with nurses and nursing assistants handling overweight and obese patients: a literature review. Work. 2016;53(2):439–448. doi: 10.3233/WOR-152222 [DOI] [PubMed] [Google Scholar]
- 23.Sezgin D, Esin MN. Predisposing factors for musculoskeletal symptoms in intensive care unit nurses. Int Nurs Rev. 2015;62(1):92–101. doi: 10.1111/inr.12157 [DOI] [PubMed] [Google Scholar]
- 24.Saga S, Seim A, Mørkved S, Norton C, Vinsnes AG. Bowel problem management among nursing home residents: a mixed methods study. BMC Nurs. 2014;13(1):1–12. doi: 10.1186/s12912-014-0035-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cho S-H, Lee J-Y, June K-J, Hong KJ, Kim Y. Nurse staffing levels and proportion of hospitals and clinics meeting the legal standard for nurse staffing for 1996~ 2013. J Korean Acad Nurs Acronym. 2016;22(3):209–219. doi: 10.11111/jkana.2016.22.3.209 [DOI] [Google Scholar]
- 26.Kim J, Kim S, Park E, Jeong S, Lee E. Policy issues and new direction for comprehensive nursing service in the national health insurance. J Korean Acad Nurs Acronym. 2017;23(3):312–322. doi: 10.11111/jkana.2017.23.3.312 [DOI] [Google Scholar]
- 27.Lee JY, Song YA, Jung JY, et al. Nurses’ needs for care robots in integrated nursing care services. J Adv Nurs. 2018;74(9):2094–2105. doi: 10.1111/jan.13711 [DOI] [PubMed] [Google Scholar]
- 28.Ivankova NV, Creswell JW, Stick SL. Using mixed-methods sequential explanatory design: from theory to practice. Field Methods. 2006;18(1):3–20. doi: 10.1177/1525822X05282260 [DOI] [Google Scholar]
- 29.Gentles SJ, Charles C, Ploeg J, McKibbon KA. Sampling in qualitative research: insights from an overview of the methods literature. Qual Rep. 2015;20(11):1772–1789. [Google Scholar]
- 30.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. doi: 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 31.Fetters MD, Curry LA, Creswell JW. Achieving integration in mixed methods designs—principles and practices. Health Serv Res. 2013;48(6pt2):2134–2156. doi: 10.1111/1475-6773.12117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Han B, Li Q, Chen X, Zhao G. Workflow for intensive care unit nurses: a time and motion study. SAGE Open. 2020;10(3):2158244020947433. doi: 10.1177/2158244020947433 [DOI] [Google Scholar]
- 33.Mieronkoski R, Azimi I, Rahmani AM, et al. The Internet of Things for basic nursing care-A scoping review. Int J Nurs Stud. 2017;69:78–90. doi: 10.1016/j.ijnurstu.2017.01.009 [DOI] [PubMed] [Google Scholar]