Abstract
Objectives
To compare intrauterine adhesion (IUA) formation after hysteroscopic removal (HR) of retained products of conception (RPOC) with IUA formation after ultrasound-guided electric vacuum aspiration (EVA) and externally validate the outcomes of an RCT.
Study design
This prospective cohort study was conducted from April 2015 until June 2022 in 2 Dutch teaching hospitals and one Belgian university hospital. Women opting for EVA underwent the procedure as soon as possible. In the HR group, the therapeutic hysteroscopy was performed at least eight weeks after the end of pregnancy. Postoperatively, an office second-look hysteroscopy was offered to all patients. Women were included if they had been diagnosed with RPOC ranging from 1 to 4 cm on ultrasound and did not want to participate in the RCT. EVA was performed using a Karman cannula. Operative hysteroscopy consisted either of hysteroscopic morcellation with the TruClear™ System or the Intrauterine BIGATTI Shaver or cold loop resection with a bipolar resectoscope.
Results
Of 178 included women, 124 were treated with HR and 28 with EVA. Outcomes of HR and EVA did not differ significantly in terms of complications (5.6 % vs 3.6 %; p = 1.00). Second-look hysteroscopy showed IUAs in 14 of 91 women (15.4 %) after HR and in 1 of 16 (6.3 %) after EVA (p = .461). Completeness of removal was significantly higher (90.1 %) after HR than after EVA (68.8 %) (p = .035). Additional operative hysteroscopy was required in 14.3 % of the HR group versus 37.5 % in the EVA group (p = .036).
Conclusion
In our cohort study, no significant differences in IUAs or complications were found. RPOC removal with HR was more often complete than removal with EVA, and additional therapeutic hysteroscopy was less frequently required after HR. These findings need to be correlated with those of RCTs.
Clinical trial registration
The study was registered in de Dutch Trial Register (NTR4923). Date of registration 23-11-2014. Date of first enrollment 01-01-2015. https://trialsearch.who.int/Trial2.aspx?TrialID=NTR4923
Keywords: Dilation and Curettage, Hysteroscopy, Intrauterine adhesions, Placental remnants, Retained products of conception
Highlights
-
•
Hysteroscopic RPOC removal achieves more complete one-step removal, reducing the need for further surgery.
-
•
Hysteroscopic removal of RPOC and curettage do not differ in intrauterine adhesion formation or complication rate.
-
•
Both an RCT and observational study have found these results, strengthening the generalizability to clinical practice.
Introduction
Retained products of conception (RPOC) occur after up to 6 % of all pregnancies [1]. RPOC can be managed expectantly or medically treated in mildly or asymptomatic patients. Surgical removal is indicated if these approaches are unsuccessful. The most widely performed procedure for removing RPOC, dilation and curettage (D&C), may lead to intrauterine adhesions (IUAs) and subsequent infertility [1]. The incidence of IUAs after miscarriage and curettage varies between 7 % and 38 % [1], [2], [3], [4], [5], [6]. After repeated curettage for incomplete miscarriage, the risk of IUAs increases to40 to 48 % [5], [6], [7], [8].
D&C can be performed with a metal curette or by vacuum aspiration, which is potentially less harmful [3], [4], [5]. The safety and completeness of removal may be optimized by ultrasound guidance [9], [10], [11], [12]. Recent studies indicated that a good alternative for curettage is hysteroscopic removal (HR) [2], [13], [14], [15], [16], [17]. The potential advantages of HR are removal under direct vision, reduction of uterine trauma and subsequent IUA formation, and more complete removal [2], [16], [17]. A systematic review of 5 small cohort studies concluded that cold loop HR might be superior to curettage, with fewer IUAs (13 % vs 30 %) and fewer incomplete evacuations (1 % vs 29 %) [2].
Since patients included in RCTs might poorly represent the general population, we ran an observational study concurrently with an RCT to evaluate the external validation [18], [19], [20], [21], [22], [23]. Both studies aimed to assess the prevalence of intrauterine adhesions (IUA), effectivity and safety of HR of the removal of RPOC and compare it with ultrasound-guided EVA.
Materials and methods
This multicenter, prospective cohort study was conducted from April 2015 until June 2022 alongside an RCT in two teaching hospitals, the Catharina Hospital (Eindhoven) and OLVG (Amsterdam), and in the Ghent University Hospital (Ghent). The study was approved by the Medical Research Ethics Committees United (MEC-U) in Nieuwegein, and by the Ethical Committee of the Ghent University Hospital. The study was registered in de Dutch Trial Register (NTR4923). Written informed consent was obtained from all patients.
Adult women were eligible to participate in this study if the ultrasonographic image was suggestive for RPOC with a diameter of 1–4 cm. Women who met the inclusion criteria were first invited to participate in the RCT. If they did not want to participate in the RCT due to a preference for a specific treatment option after counseling, they were asked to take part in the observational arm of the study. Patients consented to follow-up and received the treatment of their choice. Patients were excluded if they presented with fever, showed evidence of a malignancy, had untreated cervical stenosis or a contra-indication for surgery.
The end of pregnancy was in all cases defined as the moment of expulsion or removal of the pregnancy. If a patient opted for EVA, she underwent the procedure as soon as possible. If a patient desired hysteroscopic treatment, the therapeutic hysteroscopy was performed at least eight weeks after the end of pregnancy. A diagnostic hysteroscopy took place before the therapeutic hysteroscopy according to hospital protocol (Catharina hospital and UZ Gent) because of logistical reasons. The minimum interval of 8 weeks after pregnancy was chosen because early hysteroscopic interventions may be related to more adverse events [1], [24].
The choice between hysteroscopic morcellation (HM) or cold loop removal depended on the center. In the OLVG and the Catharina Hospital, only HM was performed. In the Ghent University hospital, both cold loop resection and HM were performed. The choice of instruments depended on RPOC characteristics (size, vascularization, location) and system availability. The procedures were performed either by staff members or residents in training under direct supervision. The operations were performed under conscious sedation or under general or spinal anesthesia in an outpatient setting.
EVA was performed with an 8 or 10 mm flexible plastic Karman cannula with two lateral openings. After dilating the uterine cervix with dilators (up to Hegar 8–10), the cannula was inserted under transabdominal ultrasound guidance. Ultrasonographic visualization was maintained throughout the whole procedure. The tissue was aspirated using a vacuum source with a maximum suction power of 0.8 bar.
HM was performed with the TruClear™ 8.0 System or Elite Hysteroscope Plus, using the Soft Tissue Shaver Plus (currently: Medtronic, Minneapolis, USA) or the Intrauterine BIGATTI Shaver (Karl Storz GmbH, Tuttlingen, Germany). Cold loop resection was performed with a rigid 8.5-mm bipolar rectoscope (Karl Storz GmbH, Tuttlingen, Germany). The techniques have been previously described [24], [25], [26], [27]. Hysteroscopes were inserted under direct vision after dilating the uterine cervix with dilators (up to Hegar 9–10). Fluid balance was closely monitored using the HysteroLux™ (previously: Hysteroscopic Fluid Management System Smith & Nephew, Andover, USA; currently: Medtronic, Minneapolis, USA) with a maximum pressure setting of 120 mmHg and a maximum flow setting of 700 mL/min for hysteroscopic morcellation or loop resection, or the Hysteropump (Richard Wolf GmbH, Knittlingen, Germany) with a maximum pressure setting of 150 mmHg and a maximum flow setting of 450 mL/min for loop resection. Specifically, for the BIGATTI shaver, the ENDOMAT LC SCB unit (Karl Storz GmbH, Tuttlingen, Germany) was used as a suction pump.
The primary outcome was the presence of IUAs diagnosed with office second-look hysteroscopy after at least 1 menstruation or a minimum of 8 weeks after removal of the RPOC. Intrauterine adhesions were classified as mild, moderate, or severe according to the classification of Valle and Sciarra [28].
Secondary outcomes included installation time (time to set up the hysteroscope or EVA cannula ready for use, including cervical dilation) and operating time (time from cannula or hysteroscope introduction until removal of the instrument at the procedure end), conversion rates, intra- and postoperative complications (including fluid deficit ≥2500 mL with clinical consequences, hemorrhage (>500 mL), uterine perforation, and infection), pathology results, completeness of removal at second-look hysteroscopy, and the need for additional treatment. Complications were graded according to the Clavien-Dindo classification [29].
The two treatment groups were compared on the following variables: baseline characteristics, surgical data, and clinical outcome data. For normally distributed continuous variables, standard deviations and mean differences were calculated with the one-way ANOVA test. For non-normally distributed continuous variables, median and inter-quartile ranges were computed and analyzed using the Kruskal-Wallis test or the Mann-Whitney U test. Skewed time variables were log-transformed and analyzed with the Student’s t-test to compare geometrical means. Categorical data are presented as frequency and percentage per study group and were analyzed using the Chi-square Test or Fisher’s Exact Test. Data were collected and analyzed using the statistical software SPSS (IBM SPSS Statistics 25.0, IBM Corp., Armonk, NY, USA).
Results
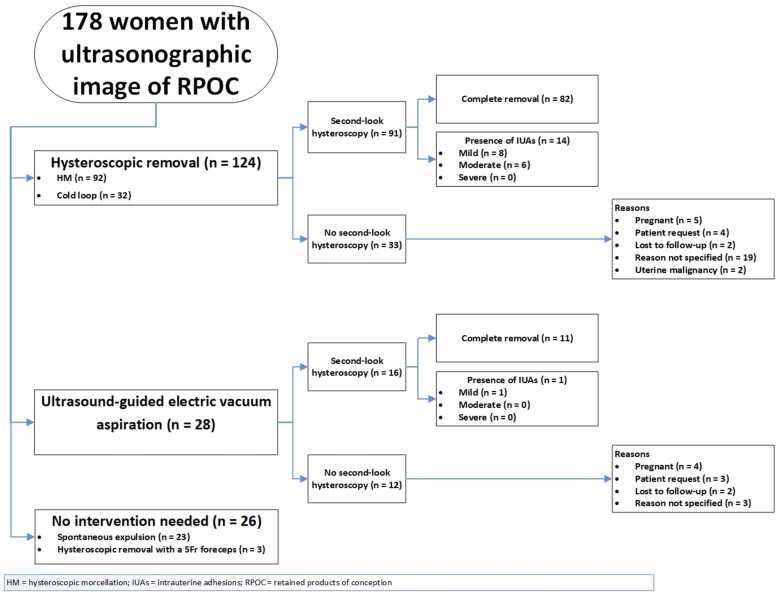
In total, 178 women were included, 6 of whom participated in the OLVG East Hospital, 70 in the Ghent University Hospital, and 102 in the Catharina Hospital. Hysteroscopic removal was chosen by 124 women, 92 of whom underwent HM and 32 cold loop resection. Ultrasound-guided EVA was chosen by 28 women. The remaining 26 women did not undergo the procedure, 23 because of spontaneous expulsion while waiting for surgical treatment, and 3 because the RPOC had become so small that it was possible to remove them during office hysteroscopy with a 5Fr forceps (Fig. 1).
Fig. 1.
Flow chart describing patients participation in the study.
The baseline characteristics of the HR group, the EVA group and the group that received no surgery did not differ except for the number of congenital uterine anomalies (Table 1). However, the number of these anomalies did not differ between the HR group and the EVA group (p = 1.00). There were no statistically significant differences in history of uterine surgery.
Table 1.
Baseline characteristicsa.
| Hysteroscopy# (124) | EVA (28) | No surgery (26) | P value | |
|---|---|---|---|---|
| Age (y) | 32 ( ± 4.0) | 32 ( ± 3.9) | 32 ( ± 5.4) | .776b |
| BMI (kg/m2) | 21.0 (21.0 – 26.4) | 24.0 (22.4 – 26.0) | 22.1 (20.7 – 27.8) | .381c |
| Obstetric history | ||||
| Gravidity | 2 (1 – 3) | 2 (1 – 3) | 2 (1 – 3) | .500c |
| Parity | 1 (0 – 2) | 1 (0 – 2) | 1 (1 – 2) | .830c |
| Previous cesarean section | 13 (10.5) | 1 (3.6) | 2 (7.7) | .497 |
| Previous manual placenta removal | 7 (5.6) | 3 (10.7) | 1 (3.8) | .522 |
| Previous curettage | 22 (17.7) | 6 (21.4) | 2 (7.7) | .360 |
| Previous operative hysteroscopy | 11 (8.9) | 0 (0) | 0 (0) | .200 |
| Previous hysteroscopic RPOC removal | 7 (5.6) | 0 (0) | 0 (0) | .202 |
| Previously diagnosed congenital uterine malformation * | 1 (0.8) | 0 (0) | 3 (11.5) | .002 |
| Previously diagnosed IUAs | .644 | |||
| Mild | 1 (0.8) | 0 (0) | 0 (0) | |
| Moderate | 1 (0.8) | 0 (0) | 0 (0) | |
| Smoker | 9 (7.3) | 3 (11.1) | 4 (15.4) | .397 |
| ASA classification | 1 (1 – 1) | 1 (1 – 1) | 1 (1 – 1) | .890c |
ASA = American Society of Anesthesiologists; BMI = body mass index; EVA = electric vacuum aspiration; IUAs = intrauterine adhesions; RPOC = retained products of conception a Data are mean ± standard deviation, median (interquartile range [25–75 %], or n (%) unless otherwise specified. Percentage excludes patients with missing values. All P values are from Chi-Square test unless otherwise specified. b P value from one-way ANOVA test. c P value from Kruskal-Wallis test. # Hysteroscopy = hysteroscopic morcellation or cold loop resection. * In the HR group, one patient had a bicorporal uterus. In the no-surgery group, two patients had a bicorporal uterus and one a hemi uterus.
Data on the pregnancies immediately preceding the RPOC diagnosis are summarized in Table 2. Participants in the three groups did not differ significantly in the way their pregnancy had ended, in the expulsion or delivery mode, nor in the percentage that underwent manual placenta removal (MPR) or curettage or both. Per the protocol, the interval between the end of pregnancy and the RPOC removal differed between the two treatment groups, with a median of 12 weeks in the HR group versus six weeks in the EVA group.
Table 2.
Pregnancy dataa.
| Hysteroscopy# (124) | EVA (28) | No surgery (26) | P value | |
|---|---|---|---|---|
| First trimester | 50 (40.3) | 15 (53.6) | 14 (53.8) | .356 |
| Incomplete miscarriage | 20 (40) | 6 (40) | 3 (21.4) | |
| Empty amniotic sac | 3 (6) | 3 (20) | 1 (7.1) | |
| Embryo without cardiac activity | 17 (34) | 5 (33.3) | 8 (57.1) | |
| Abortion | 10 (20) | 1 (6.7) | 2 (14.3) | |
| Second trimester | 14 (11.3) | 3 (10.7) | 3 (11.5) | .361 |
| Abortion | 4 (28.6) | 1 (33.3) | 0 (0) | |
| Intrauterine fetal demise | 7 (50) | 0 (0) | 2 (66.7) | |
| Immature birth | 3 (21.4) | 2 (66.7) | 1 (33.3) | |
| Third trimester | 60 (48.4) | 10 (35.7) | 9 (34.6) | .554 |
| Premature birth | 6 (10) | 1 (10) | 2 (22.2) | |
| Term delivery | 54 (90) | 9 (90) | 7 (77.8) | |
| Expulsion mode first trimester | 50 (40.3) | 15 (53.6) | 14 (53.8) | .279 |
| Spontaneous | 11 (22) | 4 (26.7) | 4 (28.6) | |
| Medical treatment | 25 (50) | 10 (66.7) | 9 (64.3) | |
| Electric vacuum aspiration | 14 (28) | 1 (6.7) | 1 (7.1) | |
| Expulsion mode second trimester | 14 (11.3) | 3 (10.7) | 3 (11.5) | .110 |
| Spontaneous | 4 (28.6) | 1 (33.3) | 0 (0) | |
| Medical treatment | 10 (71.4) | 1 (33.3) | 3 (100) | |
| Electric vacuum aspiration | 0 (0) | 1 (33.3) | 0 (0) | |
| Delivery mode third trimester | 60 (48.4) | 10 (35.7) | 9 (34.6) | .481 |
| Spontaneous | 39 (65) | 8 (80) | 7 (77.8) | |
| Medical treatment | 6 (10) | 0 (0) | 0 (0) | |
| Vacuum extraction | 1 (1.7) | 1 (10) | 1 (11.1) | |
| Primary cesarean section | 7 (11.7) | 0 (0) | 1 (11.1) | |
| Secondary cesarean section | 7 (11.7) | 1 (10) | 0 (0) | |
| Manual placenta removal | 18 (24.3) | 3 (23.1) | 3 (27.3) | .970 |
| Curettage | 5 (6.8) | 2 (15.4) | 0 (0) | .334 |
| Manual placenta removal + curettage | 11 (14.9) | 2 (15.4) | 0 (0) | .387 |
| Interval end of pregnancy - RPOC intervention (weeks) | 12 (10 – 14) | 6 (4 – 8) | <.001d |
EVA = electric vacuum aspiration; RPOC = retained products of conception a Data are mean ± standard deviation, median (interquartile range [25–75 %], or n (%) unless otherwise specified. Percentage excludes patients with missing values. All P values are from Chi-Square test unless otherwise specified. d P value from Mann-Whitney U test. # Hysteroscopy = hysteroscopic morcellation or cold loop resection.
Table 3 shows the clinical presentation and characteristics of the RPOC. Most women suffer from abnormal uterine bleeding, with or without pain symptoms. The diameter of the RPOC differed significantly between the EVA group, the HR group, and the no surgery group.
Table 3.
Clinical presentation and RPOC characteristicsa.
| Hysteroscopy# (124) | EVA (28) | No surgery (26) | P value | |
|---|---|---|---|---|
| Clinical presentation - Asymptomatic | 39 (31.5) | 6 (21.4) | 9 (34.6) | .509 |
| Clinical presentation - Symptomatic | 85 (68.5) | 22 (78.6) | 17 (65.4) | .509 |
| AUB | 78 (91.8) | 20 (90.9) | 15 (88.2) | .561 |
| Pain | 26 (30.6) | 6 (27.3) | 4 (23.5) | .800 |
| Type of imaging | ||||
| US | 12 (9.8) | 24 (85.7) | 3 (11.5) | <.001 |
| US and SIS | 1 (0.8) | 2 (7.1) | 1 (3.8) | .106 |
| US and hysteroscopy | 91 (74) | 1 (3.6) | 20 (76.9) | <.001 |
| Hysteroscopy | 6 (4.8) | 1 (3.6) | 1 (3.8) | .944 |
| US, SIS and hysteroscopy | 13 (10.6) | 0 (0) | 1 (3.8) | .123 |
| Largest diameter (mm) of RPOC | 20 ( ± 8) | 27 ( ± 8) | 17 ( ± 6) | <.001b |
| Vascularization of RPOC present¥ | 23 (40.4) | 7 (46.7) | 3 (27.3) | .764 |
| Vascularization of RPOC absent¥ | 34 (59.6) | 8 (53.3) | 8 (72.7) | .764 |
| Location during imaging* | ||||
| Fundal | 44 (37.3) | 15 (62.5) | 6 (40.0) | .073 |
| Other° | 68 (57.6) | 7 (29.2) | 7 (46.7) | .035 |
| Not specified | 6 (5.1) | 2 (8.3) | 2 (13.3) | .427 |
| Spontaneous expulsion | 23 (88.5) | |||
| Outpatient removal | 3 (11.5) |
AUB = abnormal uterine bleeding; EVA = electric vacuum aspiration; SIS = saline infusion sonography; RPOC = retained products of conception; US = ultrasound a Data are mean ± standard deviation, median (interquartile range [25–75 %]), or n (%) unless otherwise specified. Percentage excludes patients with missing values. All P values are from Chi-Square test unless otherwise specified. b P value from one-way ANOVA test # Hysteroscopy = hysteroscopic morcellation or cold loop resection. ¥ Vascularization is measured during ultrasound as either flow or no flow in or around the RPOC. If no ultrasound has been performed, the data will be noticed as missing. * Location as seen during hysteroscopy (golden standard). If no hysteroscopy was performed, the data from the ultrasound or saline infusion sonography were used. ° Location specified as being other than fundal.
The installation time was significantly longer in the HR group (median 4.40 min) than in the EVA group (median 1.04 min (p = <.001). The median operating time did not differ significantly between the HR group (7.50 min) and the EVA group (5.50 min (p = .077). Consequently, the procedure time, i.e., the sum of the installation and operating time, reached a statistically significant difference (median 12.45 min) versus 7.59 min (p = <.001) in favor of the EVA group.
The number of insertions of the hysteroscope was significantly smaller than the number of insertions of the curettage cannula (median 1 (IQR 1–1) versus 3 (IQR 2–6), p = <.001). Furthermore, for HM, the median number of insertions was one time (IQR 1–1), with a maximum of two times, and for cold loop resection the median was one time (IQR 1–3) with a maximum of five times (p = .991).
Surgery data are presented in Table 4. 4 % of the women in the HR group had a grade 1 %, and 0.8 % had a grade 3a intraoperative complication (addendum). Conversion to EVA took place in 2 of 124 patients (1.6 %) of the HR group (once because of hemorrhage (patient 5 in the addendum)), and once because of bad visibility ± poor distention/rapid fluid loss). One woman in the EVA group (3.6 %) had an intraoperative complication (addendum). One of the 124 (0.8 %) women in the HR group had a postoperative complication (addendum).
Table 4.
Surgery dataa.
| Hysteroscopy# (124) | EVA (28) | P value | |
|---|---|---|---|
| Installation time (min) | 4.40 (3.55 – 5.22) | 1.04 (0.55 – 2.46) | <.001e |
| Operating time (min) | 7.50 (4.43 – 12.83) | 5.50 (3.65 – 8.97) | .077e |
| Procedure time (min) | 12.45 (8.72 – 17.84) | 7.59 (4.56 – 11.14) | <.001e |
| Total number of insertions of the hysteroscope/ cannula | <.001 | ||
| 1 | 92 (80.7) | 4 (14.3) | |
| 2 | 14 (12.2) | 1 (5.9) | |
| ≥3 | 8 (7.0) | 12 (70.6) | |
| Conversion rates | 2 (1.6) | 0 (0) | 1.00f |
| HM to EVA | 2 (1.6) | 0 (0) | |
| Intraoperative complications | 6 (4.8) | 1 (3.6) | 1.00f |
| Hemorrhage (>500 mL) | 1 (0.8) | 1 (3.6) | .335f |
| Perforation during dilation | 2 (1.6) | 0 (0) | 1.00f |
| Perforation during surgery | 1 (0.8) | 0 (0) | 1.00f |
| Fluid deficit ≥2500 mL | 2 (1.6) | 0 (0) | 1.00f |
| Hospitalized >1 day | 0 (0) | 1 (3.7) | .180f |
EVA = electric vacuum aspiration; HM = hysteroscopic morcellation
a Data are mean ± standard deviation, median (interquartile range [25–75 %]), or n (%) unless otherwise specified. Percentage excludes patients with missing values. All P values are from Chi-Square test unless otherwise specified.
e P value from Independent-Samples t-test on log-transformed data.
f P value from Fisher’s Exact Test.
# Hysteroscopy = hysteroscopic morcellation or cold loop resection.
Table 5 presents the postoperative course of the groups. Second-look hysteroscopy was performed in 73.4 % in the HR group and 57.1 % in the EVA group (Fig. 1). The second-look hysteroscopy took place after a median of seven weeks (IQR 6–8 weeks) in both HR and EVA group. In the HR group the RPOC was more often completely removed compared to the EVA group (90 % versus 69 %; p = .035).
Table 5.
Postoperative coursea.
| Hysteroscopy# (124) | EVA (28) | P value | |
|---|---|---|---|
| Postoperative complication (hemorrhaghe) | 1 (0.8) | 0 (0) | 1.00f |
| Rehospitalization | 1 (0.9) | 0 (0) | 1.00f |
| Blood loss duration in weeks | |||
| ˂2 | 71 (74.0) | 11 (73.3) | 1.00f |
| ≥2 | 25 (26.0) | 4 (26.7) | 1.00f |
| Second look hysteroscopy performed | 91 (73.4) | 16 (57.1) | .089 |
| Completeness of removal at second look hysteroscopy^ | 82 (90.1) | 11 (68.8) | .035f |
| Presence of IUAs* | 14 (15.4) | 1 (6.3) | .461f |
| Mild | 8 (57.1) | 1 (100) | 1.00f |
| Moderate | 6 (42.9) | 0 (0) | .588f |
| Pathology result- malignant | |||
| Endometrial cancer | 1 (0.9) | 0 (0) | 1.00f |
| Choriocarcinoma | 1 (0.9) | 0 (0) | 1.00f |
| Additional hysteroscopic treatment | 13 (14.3) | 6 (37.5) | .036f |
| For RPOC | 6 (6.6) | 5 (31.3) | .011f |
| For IUAs | 8 (8.8) | 1 (6.3) | 1.00f |
EVA = electric vacuum aspiration; IUAs = intrauterine adhesions; RPOC = retained products of conception f P value from Fisher’s Exact Test. # Hysteroscopy = hysteroscopic morcellation or cold loop resection. ^ Of the 9 patients with incomplete removals in the hysteroscopy group, 6 had been appointed as incomplete immediately after the procedure. In the EVA group, 2 of the 5 cases of incomplete removal were suspected to be incomplete after the procedure.
* Presence of IUAs as diagnosed with second-look hysteroscopy after at least 1 menstruation or after a minimum period of 4 weeks after removal of the placental remnants.
There were no statically significant differences in IUAs between the two groups (p = .461). The HR group showed de novo IUAs in 15.4 %. In the HR group, two patients had a history of IUAs, but IUAs did not recur after RPOC treatment. The one patient in the EVA- group (6.3 %) had de novo IUAs, graded as mild. Additional hysteroscopic treatment was less often needed in the HR group than in the EVA group (14.3 % versus 37.5 %, p = 0.036). In the HR group, persistent RPOC were removed hysteroscopically in six patients, and eight underwent adhesiolysis. In the EVA group, persistent RPOC were removed hysteroscopically in five patients, and one patient underwent adhesiolysis.
Discussion
In this cohort, the percentage of complete RPOC removal was significantly higher after HR than after EVA. As a result, fewer patients in the HR group required additional hysteroscopic treatment compared to the EVA group. No differences in complication rates or IUAs were observed between the two groups. These outcomes are in concordance with our RCT, which provides evidence for the external validity of the RCT and supports its generalizability.
The percentage of IUAs after HR (15.4 %) found in our study is similar to the percentage of 12.8 % described in the systematic review by Hooker et al. [2]. However, IUAs percentage was higher than the 3 % in an RCT comparing hysteroscopic morcellation with loop resection of RPOC [26]. In contrast to our finding of IUAs in 6.3 % of the patients treated with EVA, a review by Hooker et al. described 29.6 % IUAs in the curettage group. This might be explained by the curettage technique. In the review the technique was often not specified. Our study used ultrasound-guided vacuum aspiration, which may ensure a more accurate and safe procedure with less trauma.
Our finding that HR results in a higher percentage of complete removal also follows the existing literature. We observed a difference in complete removal of 21 % (90.1 % vs 68.8 %) between HR and EVA. Hooker et al. reported complete removal in 99 % of patients treated with hysteroscopy and in 71 % treated with curettage. The explanation may be that HR is performed under direct vision instead of ultrasound guidance so it is possible to observe whether the RPOC has been completely evacuated [2], [13], [14], [15], [16], [17]. Another explanation could be the timing of the interventions. The interval until hysteroscopic removal was 12 weeks, compared to an interval of six weeks for EVA. This difference in timing may also explain the larger diameters of the RPOC in the EVA group, as the RPOC size may diminish over time.
Spontaneous expulsion of RPOC occurred in 13 % during the waiting period of surgery. To our knowledge, the percentage of spontaneous expulsion has not been previously described. Spontaneous expulsion occurred on average between 7.5 and 13 weeks after the end of pregnancy. Both the possibility of spontaneous expulsion and the higher complete removal rate in the HR group would justify a longer interval between the end of pregnancy and any intervention.
The primary outcome of our trial appears to be in line with the recently published RCT of Huchon et al., which reports equal pregnancy rates in both groups [30]. Nevertheless, it is important to address the differences between our study and that of Huchon et al. in terms of the study population. Huchon et al. included women who were planned for surgical removal of an incomplete spontaneous abortion, encompassing cases of embryonic death, anembryonic gestation, as well as RPOC, all with subsequent pregnancy desire. In our study, we enrolled women with ultrasonographic evidence of RPOC measuring 1–4 cm in diameter after all types of pregnancy (after miscarriage, termination of pregnancy (TOP) or delivery), and even after initial surgical treatment (manual placental removal and/or curettage). This said, Huchon et al. studied surgical treatment of early post-miscarriage retentions and RPOC, whereas our trial focused on post-pregnancy RPOC at a later stage. In contrast to the findings of Huchon et al., who found no benefit of hysteroscopy over vacuum aspiration in women with incomplete spontaneous abortion of the first trimester, we found that in our study population of patients with RPOC, hysteroscopic resection resulted in a reduced need for re-interventions compared to EVA.
The number of complications was small and did not differ between the treatment groups (5.6 % for the HR group and 3.6 % for the EVA group). In the review by Hooker et al., the rates of intraoperative complications were similarly low (0 % vs 1.4 % for HR and EVA, respectively) [2]. Due to the longer installation time, HR was longer than EVA. However, the difference in operation time was small (7.50 min vs 5.50 min), and one might debate whether this difference in total procedure time is clinically relevant. Also, the installation time might be reduced by simplifying the process.
A strength of this study is that this is the largest prospective study to date comparing HR with EVA for RPOC removal. The study ran alongside an RCT with the aim to strengthen the external validity and assess the generalizability of the RCT. Further, no other studies have described the course prior to the intervention, including spontaneous expulsion. Thirdly, the present study comprehensively describes the completeness of removal and additional treatments. A limitation of the study is its prospective cohort design. We observed that physicians and patients strongly prefer HR, so the EVA group was small. Secondly, not all patients underwent a second-look hysteroscopy, which may have introduced bias into our data on IUAs. Another limitation is that we assessed the incidence of adhesions and not the live birth rate. Adhesions are a surrogate outcome, and the primary outcome should preferably be the impact on reproductive outcome.
In conclusion, our study indicates that HR resulted in a higher rate of completely removed RPOC than EVA, resulting in fewer additional hysteroscopic treatments for persistent RPOC in the HR group. We did not find a difference between complication rates or the IUA formation. This cohort study strengthens the external validity and transferability to the clinical practice of the alongside running RCT since both studies observed similar outcomes. We noted a 13 % spontaneous RPOC expulsion prior to HR, which justifies a wait-and-see policy. Therefore, HR is a viable alternative for EVA, as it displays the advantages of ‘visual control‘, leading to a higher rate of complete removal with a single procedure.
Funding
H.v.V received an unrestricted grant from the External Research Program from Medtronic. The Ghent University Hospital Research Center receives unrestricted external research support from Medtronic for the ongoing RIGHT trial.
Disclosure statement
H.v.V. and B.S. received fees from Medtronic on an hourly basis for lectures on hysteroscopic morcellation. All the fees were donated to a foundation which promotes research in obstetrics and gynecology. Ghent University Hospital received a fee from Medtronic for a lecture on RPOC by T.H
Declaration of Competing Interest
None.
Acknowledgments
We thank all of our patients for their participation in this study and our colleague gynecologists for referral of their patients.
Footnotes
This work was presented as an oral presentation at the European Society for Gynecological Endoscopy’s 31st Annual Congress, Lisbon, Portugal, October 2–5, 2022.
Appendix A
Addendum.
Intraoperative complications EVA group.
Grade 2.
-
1.
Patient 1: Hemorrhage requiring longer hospitalization.
Intraoperative complications HR group.
Grade 1.
-
1.
Patient 1: Fluid deficit of 2500 mL or more with no clinical consequences;
-
2.
Patient 2: Fluid deficit of 2500 mL or more with no clinical consequences;
-
3.
Patient 3: Perforation during cervical dilation, but the procedure was not stopped prematurely and the RPOC was completely removed;
-
4.
patient 4: Perforation during cervical dilation, but the procedure was not stopped prematurely and the RPOC was completely removed;
-
5.
Patient 5: Hemorrhage resulting in conversion to EVA due to blood loss and minimal RPOC visible at the second look.
Grade 3a
-
6.
Patient 1: Perforation during RPOC removal at the level of the cesarean scar (with minimal residual myometrium overlying the RPOC), resulting in a small bladder perforation confirmed by cystoscopy and treated by a bladder catheter for 10 days.
Postoperative complication HR group.
Grade 3b.
-
1.
Patient 1: Consisting of hemorrhage, for which she was rehospitalized and treated with curettage.
References
- 1.Golan A., Dishi M., Shalev A., Keidar R., Ginath S., Sagiv R. Operative hysteroscopy to remove retained products of conception: novel treatment of an old problem. J Minim Invasive Gynaecol. 2011;1:100–103. doi: 10.1016/j.jmig.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 2.Hooker A., Aydin H., Brölmann H.A.M., Huirne J.A.F. Long-term complications and reproductive outcome after the management of retained products of conception: a systematic review. Fertil Steril. 2016;105(1):156–164. doi: 10.1016/j.fertnstert.2015.09.021. [DOI] [PubMed] [Google Scholar]
- 3.Salzani A., Yela D., Gabiatti J.R., Bedone A.J., Monteiro I.M. Prevalence of uterine synechia after abortion evacuation curettage. Sao Paula Med J. 2007;125:261–264. doi: 10.1590/S1516-31802007000500002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuzel D., Horak P., Hrazdirova L., Kubinova K., Sosna O., Mara M. “See and treat” hysteroscopy after missed abortion. Minim Invasive Ther Allied Technol. 2011;20(1):14–17. doi: 10.3109/13645706.2010.496999. [DOI] [PubMed] [Google Scholar]
- 5.Römer Post-abortion-hysteroscopy–a method for early diagnosis of congenital and acquired intrauterine causes of abortions. Eur J Obstet Gynecol Reprod Biol. 1994;57:171–173. doi: 10.1016/0028-2243(94)90295-x. [DOI] [PubMed] [Google Scholar]
- 6.Friedler S., Margalioth E., Kafka I., Yaffe H. Incidence of post-abortion intra-uterine adhesions evaluated by hysteroscopyda prospective study. Hum Reprod. 1993;8:442–444. doi: 10.1093/oxfordjournals.humrep.a138068. [DOI] [PubMed] [Google Scholar]
- 7.Hooker A., Muller L., Thurkow A., Heymans M., Opmeer B., Brolmann H., et al. Systematic review and meta-analysis of intrauterine adhesions after miscarriage: prevalence, risk factors and long-term reproductive outcome. Hum Reprod. 2014;20(20):262–278. doi: 10.1093/humupd/dmt045. [DOI] [PubMed] [Google Scholar]
- 8.Westendorp I., Ankum W., Mol B.W., Vonk J. Prevalence of Asherman’s syndrome after secondary removal of placental remnants or a repeat curettage for incomplete abortion. Hum Reprod. 1998;13(12):3347–3350. doi: 10.1093/humrep/13.12.3347. [DOI] [PubMed] [Google Scholar]
- 9.Meshaal H., Salah E., Fawzy E., Abdel-Rasheed M., Maged A., Saad H. Hysteroscopic managment versus ultrasound-guided evacuation for women with first-trimester pregnancy loss, a randomised controlled trial. BMC Women's Health. 2022:22. doi: 10.1186/s12905-022-01774-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chaikof M., Lazer T., Gat I., Quach K., Alkudmani B., Zohni K., et al. Lower complication rates with office-based D&C under ultrasound guidance for missed abortion. Minerva Ginecol. 2017;69(1):23–28. doi: 10.23736/S0026-4784.16.03935-6. [DOI] [PubMed] [Google Scholar]
- 11.Acharya G., Morgan H., Paramanantham L., Fernando R. A randomized controlled trial comparing surgical termination of pregnancy with and without continuous ultrasound guidance. Eur J Obstet Gynecol Reprod Biol. 2004;114(1):69–74. doi: 10.1016/j.ejogrb.2003.09.042. [DOI] [PubMed] [Google Scholar]
- 12.Criniti A., Lin P. Applications of intraoperative ultrasound in gynecological surgery. Curr Opin Obstet Gynecol. 2005;17(4):339–342. doi: 10.1097/01.gco.0000175349.10684.e8. [DOI] [PubMed] [Google Scholar]
- 13.Capmas P., Lobersztajn A., Duminil L., Barral T., Pourcelot A.G., Fernandez H. Operative hysteroscopy for retained products of conception: Efficacy and subsequent fertility. J Gynecol Obstet Hum Reprod. 2018;48:151–154. doi: 10.1016/j.jogoh.2018.12.005. [DOI] [PubMed] [Google Scholar]
- 14.Smorgick N., Barel O., Fuchs N., Ben-Ami I., Pansky M., Vaknin Z. Hysteroscopic management of retained products of conception: meta-analysis and literature review. Eur J Obstet Gynecol Reprod Biol. 2014;173:19–22. doi: 10.1016/j.ejogrb.2013.11.020. [DOI] [PubMed] [Google Scholar]
- 15.Foreste V., Gallo A., Manzi A., Riccardi C., Carugno J., di Spiezio Sardo A. Hysteroscopy and retained products of conception: an update. Gynecol Minim Invasive Ther. 2021;10:203–209. doi: 10.4103/GMIT.GMIT_125_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cohen S., Kalter-Ferber A., Weisz B., Zalel Y., Seidman D., Mashiach S., et al. Hysteroscopy may be the method of choice for management of residual trophoblastic tissue. J Am Assoc Gynecol Laparosc. 2001;8(2):199–202. doi: 10.1016/s1074-3804(05)60577-4. [DOI] [PubMed] [Google Scholar]
- 17.Rein D., Schmidt T., Hess A., Volkmer A., Schondorf T., Breidenbach M. Hysteroscopic management of residual trophoblastic tissue is superior to ultrasound-guided curettage. J Minim Invasive Gynaecol. 2011;18:774–778. doi: 10.1016/j.jmig.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 18.Averitt A., Ryan P., Weng C., Perotte A. A conceptual framework for external validity. J Biomed Inform. 2021:121. doi: 10.1016/j.jbi.2021.103870. [DOI] [PubMed] [Google Scholar]
- 19.Kennedy-Martin T., Curtis S., Faries D., Robinson S., Johnston J. A literature review on the representativeness of randomized controlled trial samples and implications for the external validity of trial results. Trials. 2015;16(1) doi: 10.1186/s13063-015-1023-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dekkers O., Elm von E., Romijn J., Vandenbroucke J. How to assess the external validity of therapeutic trials: a conceptual approach. Int J Epidemiol. 2009;39(1):89–94. doi: 10.1093/ije/dyp174. [DOI] [PubMed] [Google Scholar]
- 21.Steckler A., McLeroy M. The importance of external validity. Am J Public Health. 2008;98(1):9–10. doi: 10.2105/AJPH.2007.126847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sniderman A., LaChapelle K., Rachon N., Furberg C. The necessity for clinical reasoning in the era of evidence-based medicine. Mayo Clin Proc. 2013;88(10):1108–1114. doi: 10.1016/j.mayocp.2013.07.012. [DOI] [PubMed] [Google Scholar]
- 23.Rothwell P. Factors that can affect the external validity of randomised controlled trials. PLoS Clin Trials. 2006;1(1) doi: 10.1371/journal.pctr.0010009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hamerlynck T., Blikkendaal M., Schoot B., Hanstede M., Jansen F. An alternative approach for removal of placental remnants: hysteroscopic morcellation. J Minim Invasive Gynaecol. 2013;20:796–802. doi: 10.1016/j.jmig.2013.04.024. [DOI] [PubMed] [Google Scholar]
- 25.Emanuel M., Wamsteker K. The intra uterine morcellator: a new hysteroscopic operating technique to remove intrauterine polyps and myomas. J Minim Invasive Gynecol. 2005;12(1):62–66. doi: 10.1016/j.jmig.2004.12.011. [DOI] [PubMed] [Google Scholar]
- 26.Hamerlynck T., van Vliet H., Beerens A., Weyers S., Schoot B. Hysteroscopic morcellation versus loop resection for removal of placental remnants: a randomized trial. J Minim invasice Gynaecol. 2016;23(7):1172–1180. doi: 10.1016/j.jmig.2016.08.828. [DOI] [PubMed] [Google Scholar]
- 27.Bigatti G., Ferrario C., Rosales M., Baglioni A., Bianchi S. IBS Integrated Bigatti Shaver versus conventional bipolar resectoscopy: a randomised comparative study. Gynecol Surg. 2012;9:63–72. doi: 10.1007/s10397-012-0737-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Deans R., Abbot J. Review of intrauterine adhesions. J Minim Invasive Gynaecol. 2010;17:555–569. doi: 10.1016/j.jmig.2010.04.016. [DOI] [PubMed] [Google Scholar]
- 29.Dindo D., Demartines N., Clavien P. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huchon C., Drioueche H., Koskas M., Agostini A., Bauville E., Bourdel N., et al. Operative Hysteroscopy vs Vacuum aspiration for incomplete Spontaneous Abortion a randomized clinical trial. JAMA. 2023;329(14):1197–1205. doi: 10.1001/jama.2023.3415. [DOI] [PMC free article] [PubMed] [Google Scholar]