ABSTRACT
The biomedical research infrastructure of our academic medical centers elucidates disease mechanisms and develops diagnostic tests and treatments with scientific rigor, but the mechanism for reliably moving these findings into clinical settings lacks careful design. Hence, there is a wide gap between medical discoveries and the health benefit realized by the U.S. population. Performance improvement (PI) is a discipline that focuses on intentional redesign of core processes in our health system to close these gaps. The application of PI science is more consequential to health outcomes as is traditional biomedical research. This article describes why application and recognition of PI science as a discipline is imperative and why we should require training with similar intensity in undergraduate medical education (UME) and graduate medical education (GME). It also proposes investment in infrastructure (developing faculty expertise) and rigorous fellowships, which are, perhaps, more likely to thrive in teaching hospitals with a strong clinical mission.
INTRODUCTION
In the world of business, advances in knowledge have rapidly brought a wide range of new products, services, and better experience to benefit consumers. Businesses have achieved this by reengineering their core processes as technology, consumer needs, and expectations evolve (1). Core processes are those essential activities that a business or department must perform effectively in order to maintain the quality of its product or service. For any human resources department, core processes would include hiring, onboarding, and annual reviews. In automobile manufacturing, core processes would include stamping, welding, painting, and assembly. In the world of medicine, advancement in knowledge has not been nearly as successful. Since the formation of the National Institutes of Health (NIH) in 1938, society has funded medical research with the expectation that research findings would translate into improved health care delivery and outcomes for individuals and populations. This research investment has contributed substantially to the 34 million citations in PubMed. However, the benefit of this immense accumulation of medical knowledge has not been fully realized in terms of health outcomes for the U.S. population. Indeed, despite established know-how and best practices in medicine, medical practice lags behind medical knowledge. Multiple factors account for this situation, including lack of awareness and diffusion, but the ability to continually reengineer the delivery systems and processes to safely and efficiently incorporate the growing body of medical knowledge at the front line of medical care is a major barrier and gap that needs to be narrowed. The comparison of outcomes in medicine with outcomes in businesses such as manufacturing is often criticized, but validity of this comparison is sound when one considers that all organizations (e.g., manufacturing, banks, hospitals, outpatient practices) are the sum total of their processes. Optimizing the admission, rounding, insertion of central lines, consulting, image ordering, or discharge process would be similar to optimizing core processes in other industries. This article emphasizes the value of developing physicians as “health systems scientists” through training and incentives in order to narrow the gap between already immense medical knowledge and poorer health outcomes due to suboptimal processes or medical errors. Although the application of improvement science is needed broadly across the health care system, the focus of this paper will be on the hospital side, which is responsible for the largest portion of spending in health care.
THE GAP BETWEEN MEDICAL KNOWLEDGE AND HEALTH OUTCOMES
The gap between progress in medical knowledge and progress in health outcomes is substantial and widening.
Medical Knowledge Accumulation
One measure of progress in medical knowledge is the accumulation of citations in the PubMed database. Since 1938, the accumulated growth in NIH spending has been exponential, amounting to $1.8 trillion in today's dollars (not including investment in medical training and the health care system) (2). This expenditure has fueled research and allowed us to gain insights into disease pathogenesis leading to diagnostics, therapeutics, and technology for disease management. As of November 2022, there were 34 million citations in the PubMed database (3). This volume of medical knowledge has, no doubt, led to 3,500 to 5,000 laboratory tests, 13,000 drugs, and 26,000 medical devices (4-6). Just 100 years ago, a patient presenting with pneumonia or congestive heart failure (CHF) would almost certainly die. Then, the treatment for pneumonia was rotating pillows to optimally aerate normal lung tissue and improve oxygenation (7). Likewise, treatment for congestive heart failure was rotating tourniquets to decrease congestion of the heart (8). Today, we have therapeutic options with demonstrated efficacy, in randomized clinical trials, for preventing, diagnosing, and treating these and many other diseases.
Health Outcomes
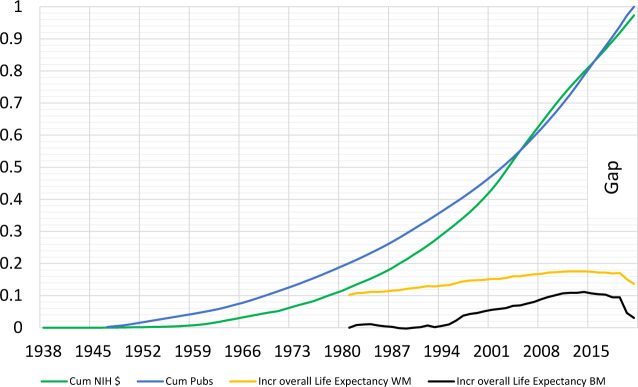
Sadly, despite the enormous investment and exponential accumulation of medical knowledge and know-how, the rate of improvement in health outcomes and overall life expectancy, health disparities, and health-care-associated conditions has been slow. One measure of progress, life expectancy, a known indicator of population health, has many determinants, but advances in medical knowledge and application in the clinical setting is an important one. Since 1845, there has been a slow, steady rise in life expectancy, but this increase has not been proportional to the increase in medical knowledge (see Figure 1) (9). Importantly, the improvement in life expectancy has been uneven across the population. About 40 years ago (1980), the difference between life expectancy for White men and Black men was 5.2 years. In the setting of rapid advances in medical knowledge, this disparity narrowed slightly, to 4.2 years in 2014, but has widened to 7 years since the COVID-19 pandemic. This trend points to multiple factors including health care access and social and structural determinants of health, but also failures in our health care delivery systems and processes.
Fig. 1.
Accumulated NIH expenditure, publications, and relative increase in overall life expectancy by race. The blue line shows the rate of accumulation of PubMed citations. The green line shows the rate of accumulation of NIH expenditures (adjusted for inflation) from 1938. The yellow line shows the increase in overall life expectancy for White males. The black line shows the increase in life expectancy for Black males. Despite an exponential increase in NIH spending and knowledge (as measured by PubMed citations), life expectancy and disparity in life expectancy have not improved.
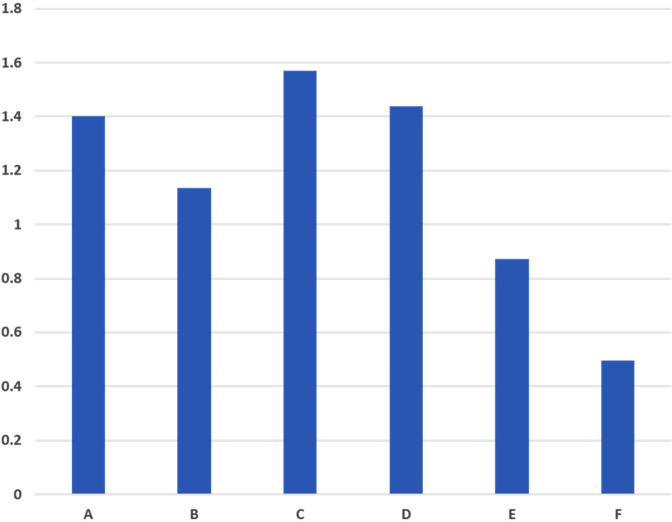
Among the common diseases contributing to premature mortality and morbidity are hypertension, hyperlipidemia, diabetes mellitus, and congestive heart failure. Progress in understanding the pathogenesis and management of these diseases has been similar to the overall advancement in scientific knowledge. Figure 2 shows both the exponential rate of accumulation of PubMed citations on the management of hypertension and changes in blood pressure control over the same period of time (10). Figure 3 shows both the exponential rate of accumulation of PubMed citations on the management of congestive heart failure and the hospital readmission rate for this disease over the same period of time (11). A similar pattern of divergence between accumulated knowledge and health outcomes exists for other diseases such as diabetes and hyperlipidemia.
Fig. 2.
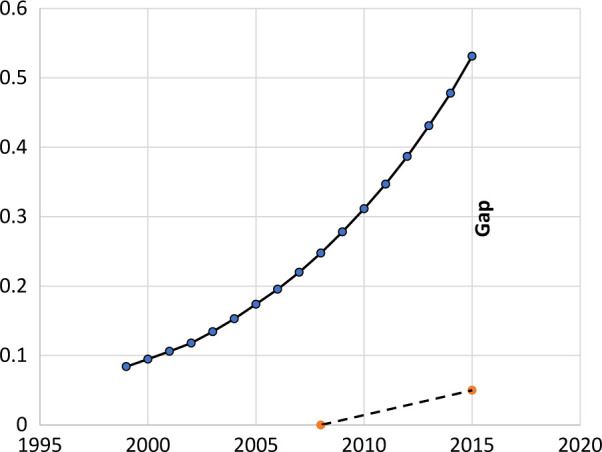
CHF management citations versus readmissions rate. The solid line shows the rate of accumulation of PubMed citations on management of congestive heart failure. The dashed line shows the change in 30-day hospital admission rates at two points (2008 and 2015). There is a wide gap between knowledge accumulation (as measured by PubMed citations) and improvement in readmission rates for congestive heart failure.
Fig. 3.
Hypertension management citations versus control. The beaded line shows the rate of accumulation of PubMed citations on management of hypertension. The solid line shows the percent of patients with controlled blood pressure from 1999 to 2017. There is a wide gap between knowledge accumulation (as measured by PubMed citations) and improvement in blood pressure control.
The number of health care acquired conditions (HAC)—preventable infections or other complications that a patient develops in the hospital while undergoing treatment for a different condition—is one reflection of hospital safety and quality of care. Many HACs are tracked by the Center for Medicare and Medicaid Services (CMS) and reported as measures of hospital safety and quality, and health care reimbursement is often linked to these outcomes. Figure 4 shows the standard infection ratios for catheter associated urinary tract infections across six hospitals in Maryland (12). Figure 5 shows the standard infection ratios for central line associated blood stream infections (CLABSIs) for six hospitals in Maryland (12). Despite established best practices for preventing HACs, they still occur at significant rates. Shannon et al demonstrated that CLABSIs could be eliminated by consistent application of standard practice in placement and maintenance. Within one year, CLABSIs decreased from 10.5 to 1.2 infections per 1,000 line-days in the ICU setting and sustained this for a 34-month period (13). This study suggests that HACs are not inevitable, even in a complex care setting, but they are due to lack of systems that reduce variability in application of medical knowledge.
Fig. 4.
Variability in catheter associated urinary tract infection (CAUTI) standard infection ratios (SIR) for six hospitals in Maryland.
Fig. 5.
Variability in central line associated blood stream infections (CLABSI) standard infection ratios (SIR) for six hospitals in Maryland.
Why the Gap Between Medical Knowledge and Health Outcomes Exists
There are many reasons for the significant and growing gap between medical knowledge and health outcomes. One is the increased complexity of the health care delivery system brought about by the combined effect of advances in medical science and the benefits thereof. In 1922, the life expectancy was 58.8 years. Since then, life expectancy has grown to 79 years (2022) (9). With longer life expectancy, patients accumulate comorbidities. The need for intense care coupled with the availability of a plethora of diagnostic, therapeutic, and technological advances has fueled a health system that is incredibly complex. Another reason for the gap between medical knowledge and health outcomes is the lack of powerful incentives for improving systems and processes in health care in order to narrow the gap between knowledge and health outcomes. Finally, health outcomes are driven by social and structural determinants that limit access to preventive care and disease management for a segment of the population. This latter cause of gaps, which are not in the direct control of health system leaders, is outside the scope of this paper.
COMPLEXITY IN A HEALTH CARE SYSTEM
Even at the microsystem level, health care delivery occurs in a complex system. Caring for patients with multiple comorbidities requires coordinated activities among a large and highly specialized workforce. In such a structure, no single person is responsible for the patient's outcome. Rather, the health outcome is dependent on medical knowledge and skills on the one hand and, equally important, a highly functioning system allowing effective coordination and application of that knowledge.
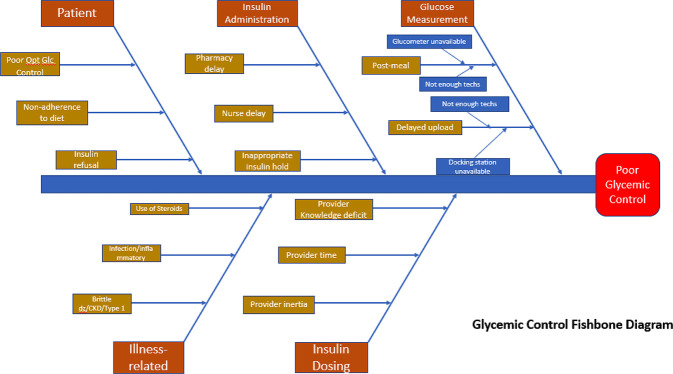
Complexity in health care is easier to describe than to measure. As an example of the complex system in hospitals, the typical patient admitted to the author's hospital encounters 35 different individuals directly or indirectly in the first 24 hours. This would not be atypical for most hospitals. Another example of complexity is apparent when one considers the infrastructure for management of glycemia, a substantial problem in hospitals. Hyperglycemia is important because it may contribute to increased risk of hospital acquired infections, morbidity, and mortality. Twenty-five percent of patients on general medicine services have diabetes, usually as a comorbidity rather than reason for admission, and 30% of these individuals have hyperglycemia. Keeping blood glucose within a range of 70 mg/dl and 180 mg/dl minimizes risk. Figure 6 is a fishbone diagram showing the causes of poorly controlled diabetes in hospitals. Controlling blood sugar requires consistently measuring blood glucose before the patient eats each major meal, uploading the measurement into the electronic medical record system, timely interpretation of the blood glucose measure, determination of insulin dose, request of insulin from the pharmacy, preparation and delivery of insulin to the hospital unit, and administration of the insulin. With this degree of complexity, there are numerous points where failure could lead to a poor outcome for the patient and, at most of these points, the physician has no direct role. As such, the outcomes for the patient (glycemic control) depend more on the effectiveness of processes and systems in place for care delivery than on the people providing the care. A good doctor or allied practitioner is always required, but not nearly sufficient to ensure safe and high-quality medical care and health outcomes.
Fig. 6.
A fishbone diagram showing the factors contributing to poor glycemic control in hospitals.
ACADEMIC INCENTIVES
Based on the Agency for Healthcare Research and Quality (AHRQ) budget, about 1% of NIH expenditures is directed to health systems improvement (14). Charlie Munger, a successful investor, once said, “Show me the incentives and I'll show you the outcome.” One of the major incentives in academic medical centers (AMCs) has traditionally been medical research dollars (15). The research dollar is a currency for national reputation and ranking of the AMC (16). Within the AMC, the research dollar is currency for faculty publications, reputation and recognition, and criterion for promotion and tenure (15). The research dollar also stimulates development through training of successive cohorts of researchers. This entire system of training and incentives has driven fulfilment of the strongest of the AMC's three missions (excellence in research) and has propelled exponential advances in medical knowledge, development of diagnostic tests, therapeutics, and technology. A similarly powerful incentive that promotes advancement in design and improvement of systems to safely deliver medical care would foster narrowing the “know-do gap” and fulfil the mission of excellence in patients, but this incentive does not exist to a comparable degree.
How We Close the Gap Between Medical Knowledge and Health Outcomes
AMCs have successfully contributed to excellence in research and medical knowledge, but this knowledge is of no value without systems and processes that facilitate application to the patients who need it. In other words, the degree of benefit from medical knowledge is dependent on the degree to which our systems and processes permit us to harness that knowledge for our patients.
Closing the gap between medical knowledge and health outcomes requires quality improvement (QI)—a systematic approach to constantly improve processes and systems. The importance of this is underscored by the competency requirements set by accrediting, certifying, and other bodies in the medical education and practice space. The American Association of Medical Colleges (AAMC) has proposed a roadmap for curricular and professional competencies across the educational continuum from UME to GME (17); the Accreditation Council for Graduate Medical Education (ACGME) has requirements for education in quality improvement at the GME level (18); and the American Board of Internal Medicine (ABIM) maintenance of certification (MOC) program includes options for earning MOC points for quality improvement activities (19). In addition, other organizations support training and produce evidence to improve quality and safety in health care. The Institute for Healthcare Improvement (IHI) helps health care organizations build capability to apply quality improvement science through education and training (20). The AHRQ is a government agency that produces evidence to improve patient safety and quality (21).
It is important to understand the concept of quality and quality improvement. To use a business analogy, quality is “conformance to specifications” (22). Assume that a customer orders 1 million pencils. The customer specifies the pencils’ dimensions (length, width, and hardness of the body; angle and length of the point; length of the ferrule and eraser). If the vendor delivers pencils that meet these specifications, the standard of quality is met. If the customer orders a second set of pencils with different specifications, the manufacturer must re-tool machinery to meet the new specifications. Patients (customers of health care) also have specifications for the health care they seek. Their specifications are usually defined by (1) what they need, (2) when they need it, and (3) the manner in which they want it delivered. What patients need will continually change as knowledge advances but also depends on disease, comorbidities, and social determinants. This means that health systems must continually reengineer systems and processes as knowledge, standard of care, or patient expectations evolve.
Systems and process design and improvement are rigorous. The methods of improvement are well defined in business and have already been adopted, though not universally, in health care. Some notable health care institutions that have adopted whole system improvement approaches are Virginia Mason, Thedda Care, and Greater Baltimore Medical Center. While medicine is not often considered a “business” per se, we can learn much from business approaches. Three quality improvement frameworks already adopted successfully in health care are Six Sigma, LEAN, and the IHI model for improvement. Six Sigma is a methodology developed by Motorola in the 1980s, designed to identify, monitor, and reduce variability in a process. LEAN was developed by Toyota in the 1940s to identify and eliminate waste in a process. In this framework, waste is considered as anything for which the customer (patient) is not willing to pay (23). Examples of waste are overproduction (ordering unnecessary diagnostic tests), transportation (moving patients to a distant imaging site due to poor layout), and defects (procedure tray with missing supplies). LEAN is an effective approach for improving flow and efficiency in patient care. The IHI's model for improvement involves setting specific improvement aims and a metric of success and testing new ideas using the Plan-Do-Study-Act (PDSA) cycle. This is ideal for problems with a clear cause. All three of these QI frameworks operate within the local care environment of a specific health care system, where patient care is delivered: the QI activity leads to reengineering that improves a specific problem in that local environment. Dissemination and implementation (D&I) science is often conflated with QI, but they are different. D&I science is an area of research that describes how evidenced-based interventions can be disseminated, implemented, and maintained broadly in health care delivery systems (24). Since each health care delivery system is different in infrastructure, staffing, and available technology, local efforts are always required to implement new evidence. D&I and QI are therefore different but complementary.
Training clinicians and clinical leaders in improvement science and providing incentives to further develop and apply the science is a prerequisite to improving the systems and processes in health care that could narrow the gap between medical knowledge and health outcomes. This training and incentive approach has been a highly effective medical education approach for teaching the basic sciences and research methodology, but we have not used it to teach methodology for improving health delivery systems. With this in mind, the author makes the following recommendations:
- Training
- Further develop QI as a scientific discipline to advance systems improvement methodology.
- Implement robust curriculum in QI at the UME and GME levels sufficient to equip graduates with skills to diagnose and treat health system problems at the microsystem level.
- Develop fellowship programs to produce “master health system scientists” and train all faculty in QI so they can be role models and coaches.
- Establish partnerships between university- and community-based academic health systems to foster these goals. The very strong clinical mission in community-based academic systems along with their small size and agility is fertile ground for QI training.
- Incentives
- Award and fund protected time for clinical leaders to lead QI in their divisions.
- Require impactful QI activities for promotion of clinical faculty; teaching QI cannot be sufficient.
- Nationally fund the QI training infrastructure proposed.
- Develop a national ranking of QI culture for medical centers.
CONCLUSION
Physicians are part of a profession that the public holds responsible for the quality of care in medicine. Indeed, caring (and quality care) for the patient has always been the soul and essence of the practice of medicine. In earlier years, patients saw the physician as ever present in health care delivery. Today's patients experience medicine as a “complex system” that provides care. Notwithstanding this, physicians and the medical profession at large must retain responsibility for care quality, which, in today's context, means caring for the patient and tending to the delivery system. It means having robust skills to diagnose and treat the patient as well as the delivery system. Unfortunately, in the current state, insurers, government, accreditors, and technology startup companies are taking the lead in defining quality and physicians are in a reactive posture. The author's proposal provides an opportunity for the profession to retake the lead in health care quality, an issue that matters most to our patients, by building infrastructure that develops and sustains a physician workforce with the knowledge and skills to lead reengineering of systems and processes in health care delivery. By so doing, our population will benefit fully from our medical knowledge as it advances.
ACKNOWLEDGMENTS
The inspiration to write this manuscript came from comparing three health systems in which I have had the privilege to work. One is a large academic medical center (Washington University in St. Louis), one is an affiliate (The John J. Cochran Veterans Affairs Hospital in St. Louis), and the third is my current employer [Greater Baltimore Medical Center (GBMC) Healthcare]. GBMC is a small, agile, fully integrated health system that has successfully deployed LEAN across its whole system—from environmental services to the ICU. There is a constant focus on learning and transforming based on learning and application of evidence. The 10 + years of effort and success in this area led to a Malcolm Baldrige National Quality Award.
I am indebted to and grateful for information, advice, and review provided by: John Chessare, MD, President and CEO, Greater Baltimore Medical Center, Baltimore, MD; Richard Barron, MD, President, American Board of Internal Medicine; Kedar Matte, MD, President and CEO, Institute for Healthcare Improvement; Kenneth Ludmerer, MD, Professor of Medicine, Washington University School of Medicine; Erica Johnson, MD, wife, and Assistant Professor of Medicine, Johns Hopkins School of Medicine; Rhonda Wyskiel, MD, Former Director of Performance Improvement and Innovation, GBMC Healthcare; and Darcie Cote-Rumsey, Medical Librarian, GBMC Healthcare.
DISCUSSION
Ludmerer, St. Louis: Thank you, Melvin, for that terrific talk. We're delighted to have you and Erica with us at this organization. Two questions if I may: I think your attention to the system is highly appropriate and I agree with everything you said. Where does the individual in medical education fit into it, specifically physicians who are decades rather than years out of residency and trying to stay up to date? How does that fit into your scheme of translating knowledge to patients? I know you used in your presentation publications as a proxy for knowledge. How accurate do you think that is given the enormous redundancy and triviality in medical literature? Abraham Flexner whom you cited had a motto, “Think much publish little.”
Blanchard, Baltimore: Yes, I think it's probably the best surrogate (of the volume of medical knowledge) that we have presently. In terms of your first question about older physicians keeping up to date with advancing medical knowledge, lifelong learning is one of the competencies in medicine required of a physician. We have to continuously learn and acquire the new skills necessary to ensure that our patients receive the excellent care they deserve. If we go back to the early 1900s, a patient with a severe illness only needed a good doctor. Today, a patient with a severe illness still needs a good doctor, but a good doctor is not sufficient. We need someone with current knowledge who can take care of the patient and a system that delivers care as well. So, there must be continuous learning with medical advances.
Weinstein, Boston: Thank you again for a wonderful overview. I also have a question about life expectancy which is used in public media all the time for lambasting U.S. health care. So much of life expectancy relates to social and political issues in the country. We reduce mortality from cholera not by treating individual patients with cholera but by building sewer systems. What is really the best metric— one newborn infant who dies because of the absence of prenatal care for the mother? Or to make 70- to 75-year-olds live a year longer to make up for that one infant death? I wonder about your thoughts on that.
Blanchard, Baltimore: Yes, I agree with you that life expectancy is not the best measure for assessing the quality of health care, but it's the broadest measure. It may be better to use disease-specific outcomes that eliminate the effect of social and structural determinants. But these do not measure the overall system performance. So, I agree that mortality is not the best measure.
Desir, New Haven: Good morning, Dr. Blanchard, and thank you for your very eloquent call to action. You focus primarily on the inpatient side. Do you think the quality improvement measures would also apply to the outpatient setting? Many patients who are admitted to the hospital for severe hypertension could have been treated better or earlier, as outpatients.
Blanchard, Baltimore: Absolutely. Just to use another example. We've known for decades that if we reduce LDL by 10%, we can reduce coronary events by 20%. If reduced it by 25%, we can reduce events by 50%. However, in the outpatient setting, the proportion of patients who are on statins that are prescribed at the appropriate dose is less than 50%. Quality improvement must happen in the outpatient setting. If we don't improve care upstream from the hospital, then downstream we'll be caring for the same patients in the cardiac catheterization lab and hospital.
Humphrey, New York City: Melvin, I think that was a wonderful talk, and it's important for the audience to know that this is not a new interest of yours. Many years ago (I can't remember how many) when you were the residency program director at Washington University in St. Louis, I remember you showing me your spreadsheet of every resident in your program and their individual outcomes for the patients under their care related to hypertension and a variety of things so you've been at work on this for a very long time. I recall Elizabeth McGlynn and her colleagues publishing that paper in the New England Journal of Medicine in 2003 around the quality of care that adults were receiving in the United States. About half the time, they were receiving what was recommended, with a low of 10% of the time for alcohol dependence and 78% of the time for cataracts. So, in response to the prior question, you gave a little insight into one element. Do you know how we are doing, now from 2003 to almost 2023, compared to what the RAND group demonstrated? Are we doing any better? It's not the life expectancy outcome alone.
Blanchard, Baltimore: I haven't seen a follow-up from the 2003 RAND study that you referenced, but we are not where we need to be with implementation of evidenced-based guidelines for chronic disease management and preventive care. Since 2003, we have certainly advanced medical knowledge, but, as I have demonstrated for chronic conditions (like hypertension and congestive heart failure), there is a wide gap between knowledge and outcomes. The reason for this is complex. Yes, there are individual preferences on the part of patients as well as structural issues in the health system that affect affordability of care. But, on the provider and systems side, we see challenges as well. Physicians in practice are spending much more time doing production work [time with the Electronic Medical Record (EMR)] and relatively less time doing solution work (thinking through what the patient needs) today compared with the early 2000s. This concept was well described in the New England Journal of Medicine by Sinsky and Panzer earlier this year. Every provider goes to practice every day with their best selves, their best intentions, and a desire for the best outcome for their patients. So, when evidenced-based recommendations are not implemented, we need to focus on improving or building systems—systems that will narrow the gap between what we know will improve patient outcomes and what is actually done.
Rathmell, Nashville: Really beautiful talk. In addition to improving outcomes, your suggestions probably would increase physician satisfaction as well, if the system works around them. My question is about partnering groups. Specifically, can you say anything about how you engage nursing leadership and nurses in this process? You have a really interesting background from the business operations side which most of us don't. How can we make that fit better into what we want to do as physicians?
Blanchard, Baltimore: Yes, nurses are critical to improving systems. The organizational structure at our health system is dyadic at every level. So, at my level (chairman), I partner with the director of nursing on all inpatient medicine service line initiatives. Similarly, at the front line of care, we have unit medical directors (physicians) who lead geolocalized units in conjunction with a nurse manager as a local (unit level) dyad. There is a job description that defines how this dyad partners. Together, they choose improvement initiatives, track key performance indicators, and plan the improvement process. These relationships are modeled on the dyadic relationship between the chief nursing officer and the chief medical officer. Nurses and physicians collaborate on all improvements in patient flow, care processes, and improvement.
Schwartz, Denver: Thank you for your very interesting perspective. Could you comment on how the absence of a health care system in the United States contributes to the gap, and how it compares to other countries that truly have a health care system?
Blanchard, Baltimore: Absolutely. The absence of a “health care system” in the United States contributes to the gap. The reason for the knowledge-practice gap is complex. While some of the gap is due to systems and processes, the contribution of social and structural factors is substantial, and health systems do not have control over this latter issue. The best systems in hospitals and practices will not overcome the challenge that not everyone is insured and can afford preventive services, evaluation, and treatment. Compared with other Organization for Economic Cooperation and Development (OECD) countries with “health care systems,” the United States performs poorly, with a low life expectancy and a high prevalence of chronic conditions compared with other countries. But the health system is not within the sphere of control of the local hospital or physician practice. You are correct that other countries with a true health system may have a lower gap. My focus has been on improving outcomes for those who have access, by making our processes function better.
Schwartz, Denver: I think that part of the problem though is that we're inventing these approaches in each one of our systems and not applying them across the health care delivery system in the United States.
Blanchard, Baltimore: I completely agree with you, but, as you know, every hospital and practice is so dissimilar that we need local experts who can make the delivery of care effective locally. Each hospital and practice has different resources, a workforce with different skills, and capacity so quality improvement has to be a local issue. Dissemination and implementation focus on uptake more broadly, but different health systems are so unique that we need expertise within the local care setting.
Wilson, Durham: Thank you for your awesome comments. Our health system within the inpatient sector has been modeled in this fashion. As a practitioner, I believe the major way of defining a good outcome is to have the right question and answer in the beginning. In other words, I didn't see a focus on the physician or provider really formulating the correct question. That happens so frequently as people come in from the outpatient area. There's been a failure—not because of system failure but the right question wasn't asked or answered. Do you have a metric for that as well in the initial intake of the patient?
Blanchard, Baltimore: Can you please clarify the question?
Wilson, Durham: Suppose a patient comes in with a condition that you define as congestive heart failure, but that is not really their true problem. A whole system of quality and outcomes and so forth is formulated, but that patient will not have a good outcome because the initial premise was flawed.
Blanchard, Baltimore: Yes, the outcome for any patient does depend on making the correct diagnosis early in the course of a patient's presentation. We need good physicians to be able to make that diagnosis initially. But it's not sufficient just to have that good doctor. A good doctor is required, but good systems and processes are incredibly important for outcomes.
Wilson, Durham: How are you measuring that in addition to all of your other metrics?
Blanchard, Baltimore: We're actually beginning to look at that issue. We have patients admitted who don't need to be admitted, which is not uncommon in hospitals. This is partly due to the clinician's knowledge and skill but also to the pressured workflow. As an example, our stroke pathway from ED to inpatient is very efficient. Recently, one of our patients with unilateral facial symptoms was admitted with stroke-like symptoms, and an astute neurologist realized that these facial symptoms were really due to salivary duct stones! We will be looking at cases such as this one to learn from and improve our processes and systems.
Footnotes
Potential Conflicts of Interest: None Disclosed.
REFERENCES
- 1.Zamzow, C. Business Process—Reengineering: 7 Critical Success Factors for a Smooth Transition of Your Organizational Processes. Second. SpacePublisher Independent Publishing Platform; 2010. [Google Scholar]
- 2. National Institutes of Health. Office of Budget. Available at: https://officeofbudget.od.nih.gov/index.htm.
- 3. Pubmed.gov. Bethesda (MD): National Library of Medicine (US), National Center for Biotechnology Information. 2004. Available at: https://www.ncbi.nlm.nih.gov/gene/. Accessed on November 27, 2022.
- 4. Quest Diagnostics. Lab Logistics. Available at: https://www.questdiagnostics.com/laboratory-managers/lab-management/operations.
- 5. Labcorp. More than Diagnostic Testing for Hospitals and Physician Organizations. Available at: https://www.labcorp.com/organizations/hospitals.
- 6. FDA at a Glance. Over 20,000 Prescription Drug Products Approved for Marketing and FDA Oversees over 6,700 Different Medical Device Products. Available at: https://www.fda.gov/media/154548/download.
- 7.Singer M, Nambiar S, Valappil T, et al. Historical and regulatory perspectives on the treatment effect of antibacterial drugs. Clin Infect Dis. 2008;47:S216–24. doi: 10.1086/591407. [DOI] [PubMed] [Google Scholar]
- 8.Habak P, Mark A, Kioschos J, et al. Effectiveness of congesting cuffs (“rotating tourniquets”) in patients with left heart failure. Circulation. 1974;50:366–71. doi: 10.1161/01.cir.50.2.366. [DOI] [PubMed] [Google Scholar]
- 9. CDC. National Center for Health Statistics—Life Tables. Available at: https://www.cdc.gov/nchs/products/life_tables.htm.
- 10.Muntner P, Hardy S, Fine L, et al. Trends in blood pressure control among US adults with hypertension, 1999–2000 to 2017–2018. JAMA. 2020;324(12):1–12. doi: 10.1001/jama.2020.14545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. CHF Readmissions Maryland MHACs. Available at: https://www.medicare.gov/care-compare/results?searchType=Hospital&page=1&city=Baltimore&state=MD&zipcode=21224&radius=25&sort=closest&tealiumEventAction=Landing%20Page%20-%20Search&tealiumSearchLocation=search%20bar.
- 12. Maryland MHACS. Available at: https://www.medicare.gov/care-compare/results?searchType=Hospital&page=1&city=Baltimore&state=MD&zipcode=21224&radius=25&sort=closest&tealiumEventAction=Landing%20Page%20-%20Search&tealiumSearchLocation=search%20bar.
- 13.Shannon R, Frndak D, Grunden N, et al. Using real-time problem solving to eliminate central line infections. J Quality and Patient Safety. 2006;32(9):479–87. doi: 10.1016/s1553-7250(06)32063-6. [DOI] [PubMed] [Google Scholar]
- 14. Agency for Healthcare Research and Quality. Operating Plan for Fiscal Year 2022. Available at: ahrq.gov.
- 15.Mullangi S, Blutt M, Ibrahim S. Is it time to reimagine academic promotion and tenure? JAMA Health Forum. 2020;1(2):e200164:1–3. doi: 10.1001/jamahealthforum.2020.0164. [DOI] [PubMed] [Google Scholar]
- 16. Morse R, Brooks E, Hines K, Wellington S. Methodology: 2023–2024 Best Medical Schools Rankings. 2023. Available at: https://www.usnews.com/education/best-graduate-schools/articles/medical-schools-methodology.
- 17.AAMC. New and Emerging Areas in Medicine Series: Quality Improvement and Patient Safety Competencies Across the Learning Continuum. 2019. Available at: https://store.aamc.org/downloadable/download/sample/sample_id/302/.
- 18. ACGME. ACGME's New Requirements for Patient Safety, Physician Well-Being and Clinical Excellence, and Education Hours. 2017. Available at: https://www.medschool.lsuhsc.edu/medical_education/omen/2017/03/16/acgmes-new-requirements-for-patient-safety-physician-well-being-and-clinical-experience-and-education-hours/#:∼:text=Patient%20Safety%20and%20Quality%20Improvement%20The%20proposed%20requirements,of%20care%20being%20delivered%20by%20residents%20and%20faculty.
- 19. ABIM. QI/PO Activities. Available at: https://www.abim.org/maintenance-of-certification/ earning-points/qi-pi-activities.
- 20.Sampath B, Rakover J, Baldoza K, Mate K, Lenoci-Edwards J, Barker P. Whole System Quality: A Unified Approach to Building Responsive, Resilient Health Care Systems. IHI White Paper. Boston: Institute for Healthcare Improvement; 2021. [Google Scholar]
- 21. Agency for Healthcare Research and Quality. A Profile. Available at: ahrq.gov. [DOI] [PubMed]
- 22.Crosby, P. Quality Is Free—The Art of Making Quality Certain. First. Signet Book; 1980. [Google Scholar]
- 23.Silver SA, Harel Z, McQuillan R, Weizman AV, Thomas A, Chertow GM, Nesrallah G, Bell CM, Chan CT. How to begin a quality improvement project. Clin J Am Soc Nephrol. 2016;11(5):893–900. doi: 10.2215/CJN.11491015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bauer M, Damschroder L, Hagedorn H, et al. An introduction to implementation science for the non-specialist. BMC Psych. 2015;3:32. doi: 10.1186/s40359-015-0089-9. [DOI] [PMC free article] [PubMed] [Google Scholar]