Abstract
Open reduction and internal fixation of distal radius fractures is one of the most common operations for orthopaedic surgeons. A vital step of the operation is restoring radial height, which can be challenging if the surgeon is operating alone. To address this, we present a novel surgical technique called the distal radius mini distractor. The technique utilizes a compression / distraction device in tandem with a volar locking plate to aid in the reduction of impacted distal radius fractures. The written technique guide is presented alongside intra-operative surgical pictures and fluoroscopy. The objective of this article is to introduce the mini distractor technique, which can be of particular use for the surgeon operating without assistance.
Keywords: Upper extremity, Trauma, Technique, Distal radius
Introduction
Surgical treatment of distal radius fractures has become more common since the advent of volar locked plating [1]. Restoring radial height, radial inclination, and volar tilt can typically be restored with axial traction and ligamentotaxis, however, this can be a challenge when the surgeon is operating alone. Although the use of physician extenders is becoming more common, many surgeons in community-based trauma centers perform operations without a surgical assistant [2]. Moreover, as surgeons are faced with mounting pressures brought forth by cost-containment principles, it is likely that more surgeons in the future will have to operate without surgical assistant [3]. There is a need to develop surgical techniques that can be performed with one person.
In this article we describe a surgical technique for reducing distal radius fractures without the use of a surgical assistant. We use a compression/distraction device in conjunction with a locked volar plate to reduce and stabilize impacted distal radius fractures with significant shortening.
Methods
The effected extremity is prepped and draped according to the surgeon's preference in the standard sterile way. With the surgeon sitting in the patient's axillae and the C-arm coming in from the patient's head, the planned incision is marked, and the extremity is exsanguinated. The authors' preferred approach is the Flexor Carpi Radialis Approach as described by Orbay et al. [4] The fascia over the FCR tendon is opened distally to the scaphoid tubercle taking care not to injure the superficial radial artery. The tendon is then retracted ulnarly, and the subsheath is opened distally to the scaphoid tuberosity. The fat and flexor pollicis longus in the space of Parona are swept ulnarly and a self-retaining retractor is inserted. The watershed line (volar rim of the distal radius) is identified. The transitional fibrous zone over the watershed line is elevated in a radial to ulnar direction. Pronator muscle belly is then elevated in a radial to ulnar direction. Next, the radial septum is released, the tendons of the first dorsal compartment are protected, and the brachioradialis tendon is tenotomized with a step cut. Grasping the radial metaphysis with a bone-holding forceps from the radial direction, the wrist is extended and radial shaft is pronated out of the wound. This gives the surgeon access to the fracture to debride hematoma or callus if present. Importantly, it also gives access to the dorsal periosteum, which can be very stout if there is any callus present. In the authors' clinical experience, the release of both the brachioradialis tendon and the dorsal periosteum can assist in maintain reduction in fractures 2–4 weeks old. The shaft is then reduced back into the wound.
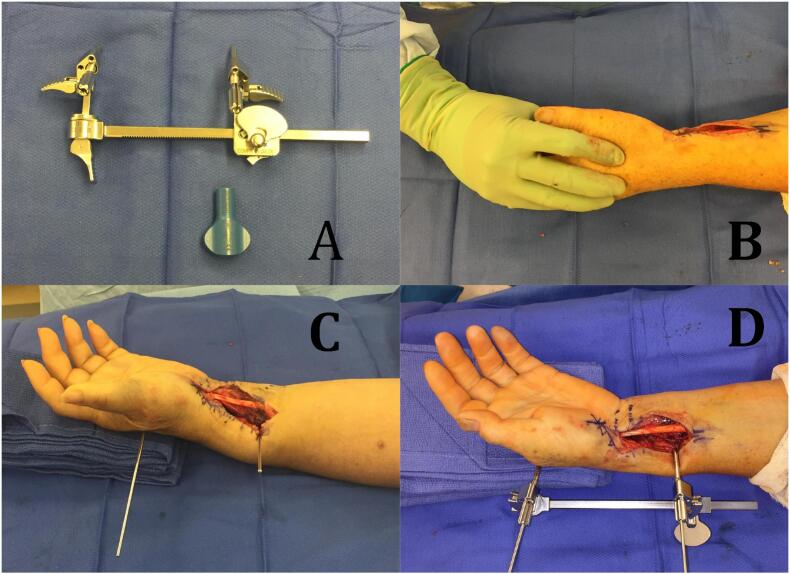
The Compression/Distraction Device (Depuy Synthes, Raynham, MA, USA), or “mini-distractor,” is then prepared (Fig. 1A). There are 3 locking clamps on the device and all three are initially released. There are 2.0 mm, 2.5 mm, and 3.0 mm pin sizes available. The authors prefer 2.5 mm threaded tip pins because they do not bend when traction is applied. The 2.5 mm holding sleeves are then partially threaded into the fixation holes on the holding arms. Next, a 2.5 mm threaded tip pin is inserted in a radial to ulnar direction in the radial shaft roughly 4 fingerbreadths from the radial styloid. The radial surface of the center of the index metacarpal is palpated, a small skin incision is made, the tissue is spread, and a 2.5 mm threaded tip pin is inserted into the index metacarpal shaft (B). The supinated wrist is then placed on a stack of 4 towels longitudinally oriented starting at the wrist joint and supporting the hand distally (C). The stack of towels helps to restore volar tilt while providing space for the distractor. To space the holding arms appropriately for application, the switch is rocked into either the “DISTR” or “COMP” position and the wing bolt is turned. The sleeves are slid down to bone and tightened over the K wires using a holding sleeve handle. Gently, downward pressure is applied to the radial shaft to approximate some volar tilt and the three locking clamps are tightened (D). Finally, C arm is brought in. Under fluoroscopic guidance, the device is used to “dial” the wrist into correct radial height using ligamentotaxis (Fig. 2). When radial height has been confirmed, the surgeon has the option to fill any metaphyseal bone void with crushed cancellous allograft.
Fig. 1.
Assembly of the distal radius mini distractor. Compression/Distraction Device (Depuy Synthes) displayed (A). Palpation of radial surface of index metacarpal (B). 4 folded towels are placed under the hand to assist in restoring volar tilt (C). The device is applied with the long arm hanging toward the table and all hinges are locked (D).
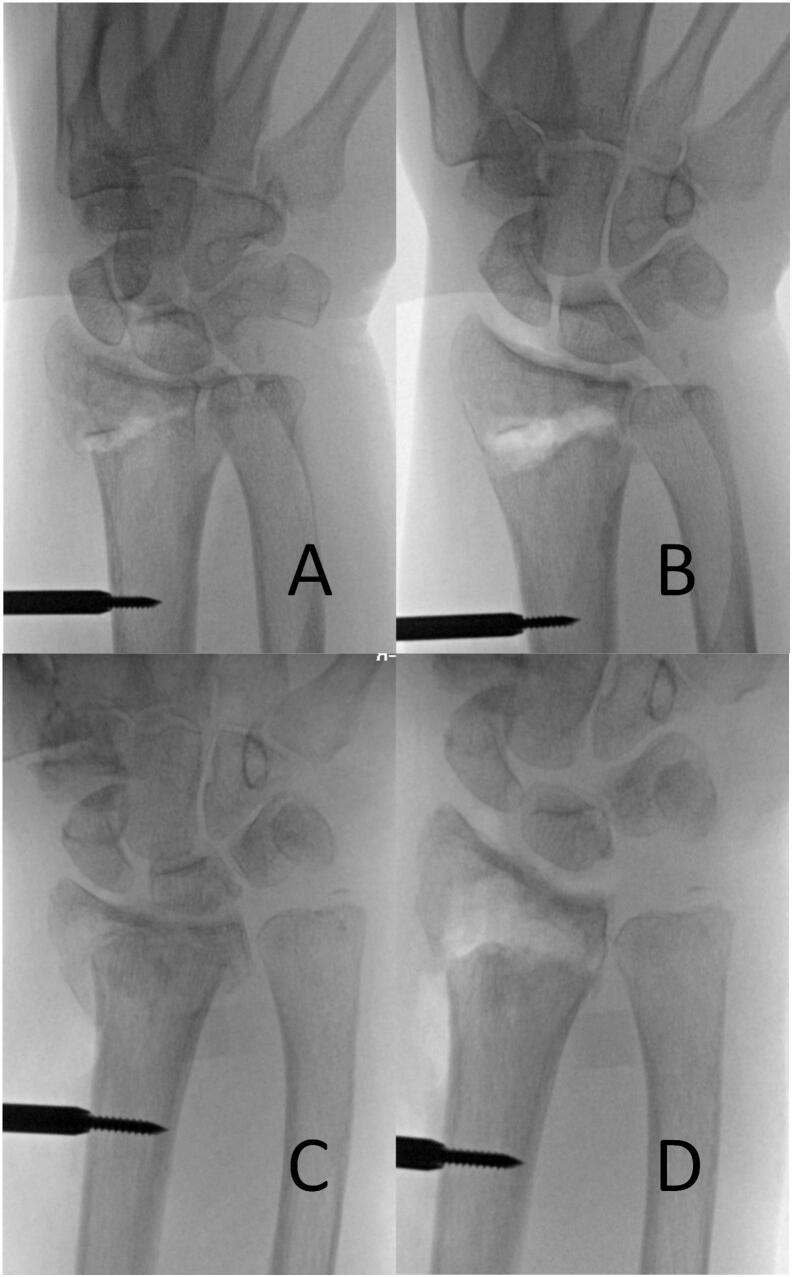
Fig. 2.
Pre-distraction (A and C) and Post-distraction (B and D) fluoroscopic examples using the device to “dial in” radial height and inclination.
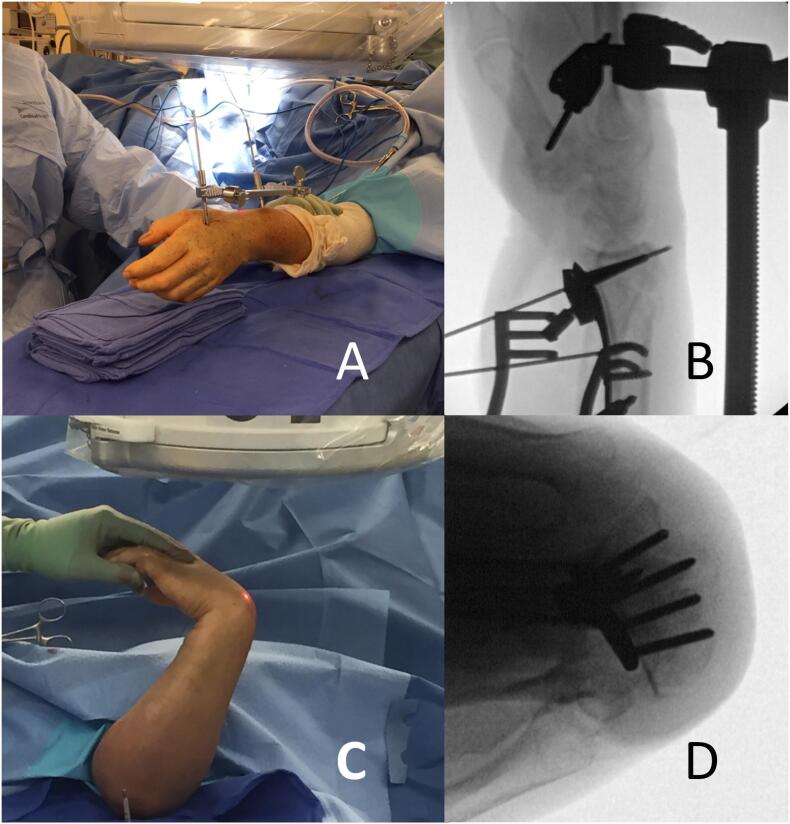
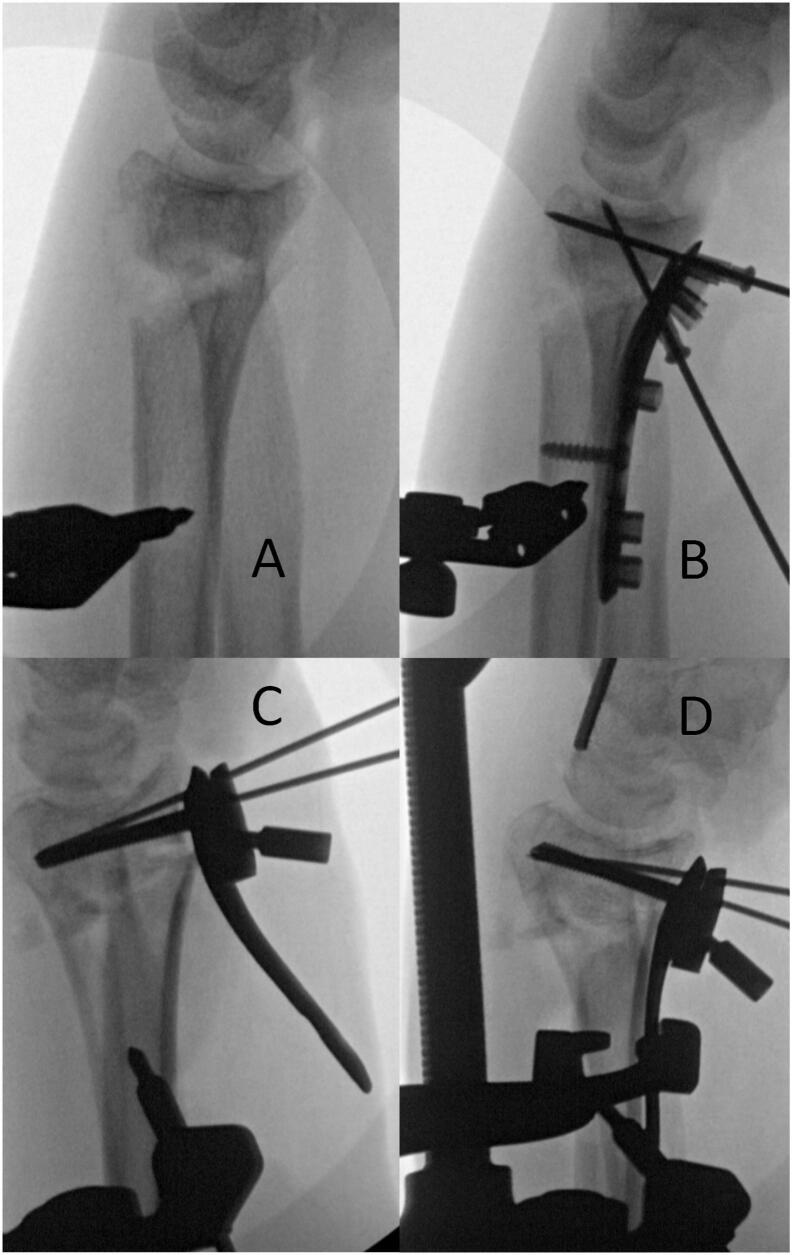
Next, a radial inclination lateral view is obtained elevating the wrist 20 degrees off the table. Using the mini-distractor as a handle is a reliable way to get orthogonal imaging without losing reduction (Fig. 4A). Frequently volar tilt is not completely restored using the distractor alone. With radial height and inclination locked in using the distractor, volar tilt can reliable be restored with the plate. There are two techniques for restoring volar tilt that the authors prefer; one way is to fix the plate to the shaft first followed by using the plate as a template and reducing the fracture to the plate. Another method is to first fix the plate to the distal fragment followed by reducing the plate to the diaphysis with a Verbrugge clamp (Fig. 3). The mini-distractor reduces and provisionally stabilizes the fracture in the coronal plane, thereby liberating the surgeon to focus on getting correct sagittal plane alignment. An important final step after all hardware has been inserted is to confirm that there are no screws protruding through the dorsal cortex using the Hoya view [5]. The Hoya view is obtained by flexing the elbow to 90°, flexing the wrist, externally rotating the shoulder 20°, and shooting an X ray down the dorsal surface of the wrist. Long screws are identified and swapped out (Fig. 4B).
Fig. 4.
A radial inclination view is performed but elevating the wrist 20 degrees off of the table (A and B). A Hoya view is obtained but flexing the elbow and wrist and shooting the beam down the back of the wrist (C and D).
Fig. 3.
Restoring volar tilt using a volar plate as a reduction template (A and B.) Restoring volar tilt by fixing the plate to the distal fragment (C) and reducing the plate to the shaft using a Verbrugge clamp (D).
Finally, brachioradialis, pronator, and transitional fibrous zone fibers are repaired to each other covering the plate. The skin is closed, and the wrist is placed into a sterile splint. Sutures and splint are removed 2 weeks postoperatively and a Velcro brace is given to the patient so range of motion work can begin with a hand therapist. Final x-rays are obtained at 6 weeks postoperatively and full weight bearing is initiated if appropriate.
Although we have not encountered any complications when using this technique, a possible complication could include subsequent fracture through the pin site placed at the second metacarpal due to the induced stress riser. When placing the radial pin, the surgeon must be cautious to avoid the radial artery and superficial radial nerve to avoid vascular damage.
Discussion
The distal radius mini-distractor is a useful technical tool for the orthopaedic surgeon operating without assistance on distal radius fractures. The best indication is assistance in restoring radial height when an assistant is unavailable. With restoration of radial height and ligamentotaxis, the surgeon can then be more free to appropriately see and reduce the articular surface. Anatomic restoration of the articular surface is paramount, and no surgeon should accept a poor reduction due to lack of assistance [[6], [7], [8], [9]]. With the ligamentotaxis provided by the distractor, the volar plate can be more powerful in restoring volar tilt. While it is the surgeon that is ultimately reducing the fracture, the mini distractor is a useful adjunct to allow the surgeon to focus on appropriate reduction. In the authors' experience, this has improved surgical efficiency and reduction. We hope the technique can be of use throughout the orthopaedic community.
Declaration of competing interest
The authors have no conflicts of interest to disclose.
Acknowledgements
The authors' have no acknowledgments to report.
References
- 1.Chung K.C., Shauver M.J., Birkmeyer J.D. Trends in the United States in the treatment of distal radial fractures in the elderly. J. Bone Joint Surg. Am. 2009;91(8):1868–1873. doi: 10.2106/JBJS.H.01297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Althausen P.L., Shannon S., Owens B., Coll D., Cvitash M., Lu M., et al. Impact of hospital-employed physician assistants on a level II community-based orthopaedic trauma system. J. Orthop. Trauma. 2013;27(4):e87–e91. doi: 10.1097/BOT.0b013e3182647f29. [DOI] [PubMed] [Google Scholar]
- 3.Althausen P.L., Kauk J.R., Shannon S., Lu M., O’Mara T., Bray T.J. Operating room efficiency: benefits of an orthopaedic traumatologist at a level II trauma center. J. Orthop. Trauma. 2016;30(Suppl. 5):S15–S20. doi: 10.1097/01.bot.0000510720.85008.87. [DOI] [PubMed] [Google Scholar]
- 4.Orbay J.L., Badia A., Indriago I.R., Infante A., Khouri R.K., Gonzalez E., et al. The extended flexor carpi radialis approach: a new perspective for the distal radius fracture. Tech. Hand Up. Extrem. Surg. 2001;5(4):204–211. doi: 10.1097/00130911-200112000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Dolce D., Goodwin D., Ludwig L., Edwards S. Intraoperative evaluation of dorsal screw prominence after polyaxial volar plate fixation of distal radius fractures utilizing the Hoya view: a cadaveric study. Hand (N Y) 2014;9(4):511–515. doi: 10.1007/s11552-014-9616-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alluri R.K., Hill J.R., Ghiassi A. Distal radius fractures: approaches, indications, and techniques. J. Hand Surg. (Am. Ed.) 2016;41(8):845–854. doi: 10.1016/j.jhsa.2016.05.015. [DOI] [PubMed] [Google Scholar]
- 7.Trumble T.E., Schmitt S.R., Vedder N.B. Factors affecting functional outcome of displaced intra-articular distal radius fractures. J. Hand. Surg. [Am.] 1994;19(2):325–340. doi: 10.1016/0363-5023(94)90028-0. [DOI] [PubMed] [Google Scholar]
- 8.Chung K.C., Kotsis S.V., Kim H.M. Predictors of functional outcomes after surgical treatment of distal radius fractures. J. Hand. Surg. [Am.] 2007;32(1):76–83. doi: 10.1016/j.jhsa.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 9.Bobby C.A., Baris Y. Adult distal radius fracture management. JAAOS. 2021;29(22):e1105–e1116. doi: 10.5435/JAAOS-D-20-01335. [DOI] [PubMed] [Google Scholar]