Abstract
Purpose
Technological developments and implants newer generation allowed to expand the indications for total ankle arthroplasty (TAA) with aim to maintain active lifestyles. This systematic review and meta-analysis examined chance of return to sport, achievable activity level, the type of patients and the sport type after TAA.
Methods
A literature search of PubMed, Scopus, and Cochrane databases was performed. Meta-analysis was performed if the same outcomes scores were reported at least by 4 studies. PRISMA guidelines were used. Risk of bias was assessed through the MINORS criteria. Included studies reported data and outcomes related to sport in patients undergoing TAA.
Result
Initial search results yielded 483 articles; 11 articles were included in the review process. The chance to return to sport increases after TAA, achieving a mean sport participation rate of 61.9% postoperatively. Until to 92% of patients was able to return to their preoperative level of activity. Meta-analysis showed a significant postoperative improvement in the most represented outcomes scores. Especially, young, male, with lower BMI, and affected by non-inflammatory osteoarthritis were those who returned to sport reporting significantly better outcomes scores. The most frequent postoperative sports included cycling, swimming, hiking and gymnastic. Only few patients practiced impact sport.
Conclusions
Current literature does not allow to advise TAA for young and active patient who want to play sports after surgery. Selected patients undergoing TAA can return to sport after surgery, and the most approachable activities are low demanding sport. However, no strong evidence is available to support these findings. Further prospective randomized studies are necessary to establish more accurate expectations concerning sport activity after TAA implantation.
Level of evidence
Level II, systematic review.
Keywords: Total ankle arthroplasty, Total ankle replacement, Ankle arthritis, Sport
1. Introduction
Decades ago, joint replacement was restricted to the inactive elderly, but thanks to technological developments which seek to maximize the durability and longevity of the new generation of implants by maintaining an active lifestyle, surgeons were able to offer total joint replacement to a wider array of person. Thus, in the recent decades the indications for total ankle arthroplasty (TAA) have expanded from the very young active patients suffering posttraumatic osteoarthritis (PTA) to older patients who have a rising mean life expectancy and try to remain active.1 Moreover, the ankle osteoarthritis, unlike hip or knee, occurs commonly as a result of trauma, and patients whose underwent TAA are notoriously younger and with a higher baseline level of routine physical activity than those who have undergone total hip or knee replacement.2,3
Sports activity represents a significant part of social life, hence most patients after TAA inquire about postoperative expectations. Despite this consideration, there is a paucity of studies dealing with sports participation in patients who have undergone TAA.
Aim of this systematic review was to examine the current literature to assess the return to sport, the sport related outcomes, and the type of sport tolerated in patients after TAA to understand the chance of return to sport, the achievable activity level, who returns to sport and what type of sports could be played.
2. Materials and methods
2.1. Search strategy and selection criteria
This study focused on literature pertaining return to sports, sport related outcomes, and type of sports tolerated in patients following TAA. The PRISMA (Preferred Reporting Item for Systematic Reviews and Meta-Analyses) guidelines were followed, incorporating a flow chart to summarise the selection process of the revised studies.4
A comprehensive search on the PubMed, Scopus databases and Cochrane Library was conducted on First December 2022. The search terms were combined as (ankle replacement) AND (sport). All keywords were thoroughly scrutinized both individually and combined with their Medical Subject Headings (MeSH) terms. A comprehensive search was conducted among the reference lists of all included publications to identify potential studies. The literature search was independently carried out by two authors (AA and AM). A protocol was not prepared.
This paper included original studies reporting data and outcomes related to sport in patients undergoing TAA implantation. Non-English publications, review and cadaveric studies and the articles without clinical outcome measures not specifically address to sports or sport participation examination after TAA implantation were excluded.
In particular we assessed the following topics:
-
1.
Chance of return to sport;
-
2.
Achievable activity level;
-
3.
Type of patients who are able to play sport;
-
4.
Type of sports activities.
2.2. Study selection and data collection
After duplicates removal, title and abstract of all papers identified was independently screened for eligibility based on the inclusion and exclusion criteria by two authors (AA and AM). At the end of screening process, pertinent full-text articles were retrieved for eligibility. In cases of disagreements concerning the inclusion of an article, the senior author acted as the final arbiter to resolve such discrepancies (C·F.).
Study characteristics extracted included key information including author and year of publication, study design and level of evidence (LOE). Data from included studies were extracted according to PICO question (participants, intervention, comparisons, and outcomes) and includes:
-
-
Participants: number of ankles, patients demographic characteristics (age, gender, body mass index (BMI)) and mean of follow-up;
-
-
Intervention: ankle arthritis etiology, TAA implant used and additional procedures, post-operative protocol;
-
-
Comparisons: number of patients who take sport before and after surgery, differences in outcomes, activity level and sport type;
-
-
Outcomes: clinical outcomes through the PROMs (Patient Reported Outcomes Measures) regarding physical activity and sport, such as Foot and Ankle Ability Measure (FAAM) sport,5 8 items subscale ranging from 0 to 4, with 0 indicating “impossible” and 4 “no difficulty”, which assesses more difficult tasks that are essential to sport; and University of California at Los Angeles (UCLA),6 a basic scale grading from 1 to 10, whereby a score of 1 denoted “no engagement in physical activity,” while a score of 10 was defined as “regular participation in impact sports”.
Data collection was carried out utilizing Microsoft Excel (Microsoft Corporation, Redmond, Washington, USA) for Windows 11.
2.3. Quality assessment
The quality assessment (risk of bias) of included studies was performed independently by two reviewers (AA and AM) using the Methodological index for non-randomized studies (MINORS) score.7 MINORS is a validated index designed to assess methodological quality of non-randomised studies and includes 8 items for non-comparative studies. The items are scored 0 (not reported), 1 (reported but inadequate) or 2 (reported and adequate). The ideal global score for non-comparative studies is 16.
2.4. Data analysis
A meta-analysis was carried out using the software Jamovi project (2022) version 2.3, retrieved from https://www.jamovi.org. The studies sharing the same PROMS and reporting mean and standard deviation of the pre- and post-operative score values were considered eligible for meta-analysis. The analysis was performed if applicable to 4 or more studies.
Information retrieved from all studies were reported using descriptive statistics. Data are reported as ranges of absolute values in the results part. Continuous variables were reported as mean value and standard deviation or range.
3. Results
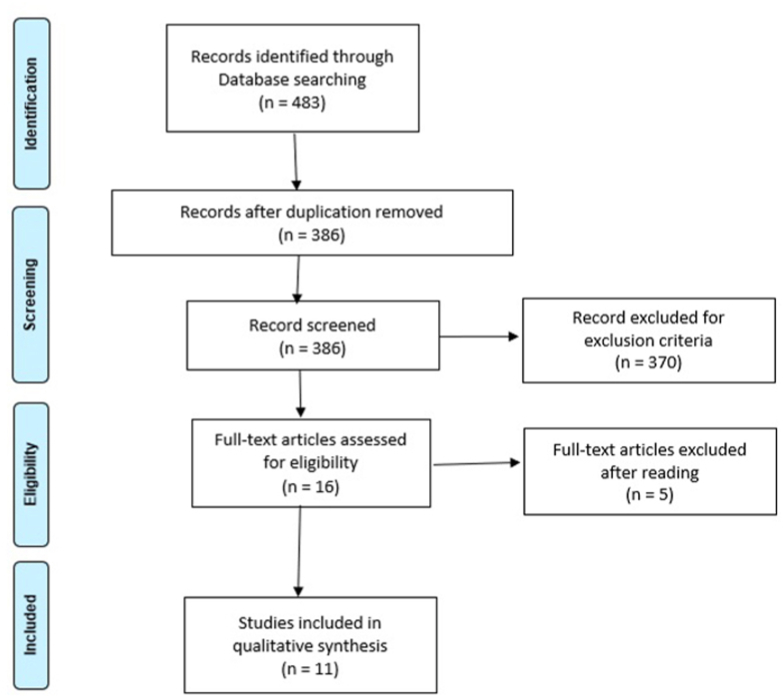
The search process initially yielded 483 articles on PubMed, Scopus databases and Cochrane Library databases search engine. After duplicates removal, titles and abstracts were screened against the inclusion and exclusion criteria. Then 16 full-text articles were select for eligibility. At the end, a total of 11 articles met the inclusion criteria and were included in the qualitative synthesis. The selection process is shown in Fig. 1.
Fig. 1.
Flowchart of review process by PRISMA.
Details of the selected studies including study design and LOE are shown in Table 1. The identified articles spanned from 2006 to 2022 (Table 1).
Table 1.
Studies design and patients’ characteristics.
| AUTHOR/YEAR | STUDY TYPE | LOE | N° ANKLE | GENDER | MEAN AGE | BMI | MEAN FU (MONTHS) |
|---|---|---|---|---|---|---|---|
| B. FRAM ET AL. -202238 | Retrospective | IV | 58 | 30 M/28 F | 63.3 | 31.9 | 27.4 |
| B. CHO ET AL - 202113 | Retrospective | III | 64 | 19 M/45 F | 64.8 | 24.7 | >36 |
| B.J. SANGEORZAN ET AL - 202127 | Prospective | II | 414 | 237 M/177 F | 63.2 | 29.9 | 48 |
| B.A. HENDY ET AL -201836 | Retrospective | IV | 109 | 53 M/54 F | 65 | 28.2 | 24 |
| S.M. RAIKIN ET AL -201714 | Retrospective | IV | 115 | 61 M/54 F | 63.2 | 28.8 | 109 |
| F.G. USUELLI ET AL - 20178 | Retrospective | IV | 76 | 44 M/32F | 56 | / | 12 |
| F. DALAT ET AL - 201415 | Retrospective | III | 32 | 13 M/19F | 51.4 | 27.7 | 59.9 |
| R. SCHUH ET AL - 20129 | Retrospective | III | 20 | 11 M/10F | 56.2 | 27.3 | 39.0 |
| F.D. NAAL ET AL - 200910 | Prospective | IV | 101 | 50 M/51F | 59.4 | 26.3 | 44.3 |
| M.P. BONNIN ET AL - 200912 | Retrospective | III | 140 | 50 M/90F | 60.9 | 25.6 | 53.8 |
|
V. VALDERRABANO ET AL - 200611 |
Prospective |
IV |
152 |
/ |
59.6 |
/ |
33.6 |
|
TOTAL |
1281 |
568 M/560 F |
|||||
| AVERAGE | 56 | 27.8 | 44.3 |
Abbreviations:LOE Level of evidence; FU Follow-up; M male; F female; m months.
3.1. Quality assessment
The methodological quality assessment of 11 nonrandomized studies, as measured by MINORS score, is summarized in Table 2.
Table 2.
Quality assessment for included studies.
| AUTHOR/YEAR | Clearly Stated Aim | Inclusion of Consecutive Patients | Prospective Collection of data | Endpoint Appropriate to the Study aim | Unbiased Evaluation of Endpoints | Follow-up Period Appropriate to the study aim | Loss to Follow-up less than 5% | Prospective Calculation of the study Size | Total |
|---|---|---|---|---|---|---|---|---|---|
| B. FRAM ET AL. -202238 | 2 | 2 | 1 | 2 | 0 | 2 | 1 | 0 | 10 |
| B. CHO ET AL - 202113 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 15 |
| B.J. SANGEORZAN ET AL - 202127 | 2 | 2 | 2 | 2 | 1 | 2 | 1 | 1 | 13 |
| B.A. HENDY ET AL -201836 | 2 | 2 | 1 | 2 | 1 | 2 | 0 | 0 | 10 |
| S.M. RAIKIN ET AL -201714 | 2 | 1 | 2 | 2 | 0 | 2 | 1 | 0 | 10 |
| F.G. USUELLI ET AL - 20178 | 2 | 1 | 0 | 2 | 0 | 1 | 2 | 0 | 8 |
| F. DALAT ET AL - 201415 | 2 | 2 | 0 | 2 | 0 | 2 | 1 | 0 | 9 |
| R. SCHUH ET AL - 20129 | 2 | 2 | 1 | 2 | 0 | 2 | 1 | 0 | 10 |
| F.D. NAAL ET AL - 200910 | 2 | 2 | 2 | 2 | 0 | 2 | 1 | 0 | 11 |
| M.P. BONNIN ET AL - 200912 | 2 | 2 | 0 | 2 | 0 | 2 | 1 | 0 | 9 |
| V. VALDERRABANO ET AL - 200611 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 0 | 12 |
Note: The items are scored 0 (not reported), 1 (reported but inadequate) or 2 (reported and adequate), thus the ideal global score for non-comparative studies is 16.
We considered the 8 items of MINORS score because the presence of non-comparative study design of the eligible papers. The mean MINORS score was 10.6 and the most frequent score resulted to be 10/16 in four manuscripts, while only one study reached 15/16 (Table 2).
3.2. Population
The total number of included ankles was 1281. All but one the articles reported the gender distribution: in total 568 males (50.4%) and 560 females (49.6%) were included. Mean age at time of surgery was 56 years (range 51.4–65) and BMI, when reported, resulted on average 27.8 (range, 24.7–31.9). Mean follow-up was of 44.3 months (range 12–109).
Patients’ characteristics are reported in Table 1.
3.3. Chance to return to sport
Out of the 11 studies selected, only four studies8, 9, 10, 11 reported sport participation in pre- and postoperative period (Table 3). Overall, 49% of patients were active in sports before surgery but improved achieving an average of sport participation rate of 61.9% postoperatively. Only one study9 recorded a decrease of patients participating in sports from 86% to 76% but it wasn't statistically significant. Another study10 reported no differences in pre- and postoperative participation in sports, but recorded besides that only 10% of patients had a cessation of sport activities, while 14% of inactive ones before surgery resumed sport postoperatively.
Table 3.
Sport participation, activity level after surgery and sport type.
| AUTHOR/YEAR | Sport partecipation pre-op | Sport partecipation post-op | Activity level post-op | Sport type |
|---|---|---|---|---|
| B. FRAM ET AL. -202238 | / | / | / | / |
| B. CHO ET AL - 202113 | / | / | / | / |
| B.J. SANGEORZAN ET AL - 202127 | / | / | / | / |
| B.A. HENDY ET AL -201836 | / | / | / | / |
| S.M. RAIKIN ET AL -201714 | / | / | / | / |
| F.G. USUELLI ET AL - 20178 | 9 (11.7%) | 38 (49.4%) | / | Jogging, dancing, biking, skiing Impact sports: jogging (13), martial arts (1) |
| F. DALAT ET AL - 201415 | / | / | / | Cycling 15 (47%), swimming 16 (49%) |
| R. SCHUH ET AL - 20129 | 18 (86%) | 16 (76%) | / | Cycling (48%), hiking (43%), skiing and swimming (both 38%), gymnastics (19%) |
| F.D. NAAL ET AL - 200910 | 62 (62.4%) | 66 (66.3%) | 8 (7.9%) sports ability worse after surgery, 27 (26.7%) no change in sports ability, 66 (65.4%) surgery improved sports ability. | Cycling, swimming, fitness-/weight training, hiking, downhill skiing, gymnastics |
| M.P. BONNIN ET AL - 200912 | / | / | 4% of cases return to initial sport level |
Of 100 OA patients: 38 cycling, 21 recreational gymnastics, 58 swimming, 50 home gardening, 27 dancing, 43 hiking. Impact sports: 7 tennis, 9 cross-country skiing (3 regularly), 17 downhill skiing (11 regularly), 6 running (1 regularly) |
| V. VALDERRABANO ET AL - 200611 | 55 (36%) | 85 (56%) (p < .001) RA group did not contribute to the sports participation rate increase (P = 1). | 42 (76%) maintained their sports activity after TAA (P = .01), 13 (24%) sports-active arthritis patients lost their sports activity after TAA, 43 (44%) sport- inactive patients preoperatively regained a sports activity after TAA implantation (P < .001) | Hiking 45 (52.8%), biking 39 (45.9%), swimming 29 (34.1%), aerobics 10 (11.8%), golfing 5 (5.9%), bowling 1 (1.2%). Impact sport: downhill skiing 7 (8.2%), horseback riding 2 (2.4%), tennis 1, jogging 1, and water-skiing 1 (1.2%). |
3.4. Achievable activity level
Only three10, 11, 12 of 11 studies particularly focused the activity level of sports participation after surgery (Table 3). Although none of patients performed sports at competitive level in pre- and post-operative, almost all patients expressed overall satisfaction with TAA and successfully returned to their pre-operative activity levels. Patients affected by osteoarthritis demonstrated a significantly higher rate of returning to their preoperative activity level compared to those with rheumatoid arthritis.
Valderrabano et al.11 reported that 76% of patients maintained their sports activity after TAA implantation (P = .01) and 44% of sport-inactive patients preoperatively regained a sports activity postoperatively (P < .001). Moreover, there was a significant improvement in sports-active intensity and duration (P < .001). As well as the study by Naal et al.10 shown that 92.1% of cases return at least to their sport level and in 61.3% of them, surgery even improved sports ability. However, 7.9% of TAA patients declared that their sports ability was worse after surgery. One study12 reported that only 4% of cases return to initial sport level.
3.5. Type of patients who are able to play sport
One study10 showed a significant correlation between sports activity and younger age among patients (P = .04), with a higher representation of male (P = .04). The highest FAAM sport subscale were recorded in patients with a low mean of BMI (24.713 and 28.814) and an average age of 64 years old. The best values for UCLA scale belonged to one study9 of 20 cases, whose mean age was 56.2 years and mean BMI was 27.3. The same study assessed the clinical outcomes through another score: the Ankle Activity Score, which assesses and quantifies the number of sports and recreational activities in patients with ankle-related condition, recording a significant worsening between pre- and postoperative situations (Table 1, Table 5).
Table 5.
Surgery data and outcomes.
| AUTHOR/YEAR | Ankle arthritis etiology | Implant | Outcomes MEASURE | Significance pre & post-op | Outcome pre-op | Outcome post-op |
|---|---|---|---|---|---|---|
| B. FRAM ET AL. -202238 | Primary OA, PTA, AA or TAA revision with bone stock | Semiconstrained prosthesis Cadence (Integra LifeScience, Plainsboro,NJ) | FAAM, VAS, SF-12 score | FAAM (p < .001) VAS (p < .001) SF-12 (NS) |
FAAM sport: 23.7 (18.2) | FAAM sport: 53.5 (32.5) |
| B. CHO ET AL - 202113 | OA (45), RA (19) | 3-component mobile-bearing prosthesis Zenith (Corin, Cirencester, UK) | AOFAS, FAOS, FAAM score | AOFAS (p < .001) FAOS (p < .001) FAAM (p < .001) |
FAAM sport: 26.7 (7.5) [OA] 28.9 (8.1) [RA] |
FAAM sport: 62.5 (13.6) [OA] 56.4 (13.2) [RA] |
| B.J. SANGEORZAN ET AL - 202127 | PTA (213), OA (71), Instability (103), other (26) | 211 (51.0%) Salto Talaris Ankle (Integra LifeSciences); 174 (42.0%) INBONE Total Ankle System (Wright Medical); 23 (5.6%) STAA (Stryker); 5 (1.2%) Trabecular Metal Total Ankle (Zimmer Biomet) and 1 other. | FAAM, SF-36, CPG score | FAAM (p < .001) SF-36 physical (p < .001) SF-36 mental (NS) CPG (p < .001) |
FAAM sport: 19.8 (2.0) | FAAM sport: 37.4 (1.4) |
| B.A. HENDY ET AL -201836 | PTA (53), OA (47), RA (9) | Fixed-bearing prosthesis Salto Talaris ankle implant (Integra LifeSciences) | VAS, FAAM, SF-12 score | VAS (p < .001) FAAM (p < .001) SF-12 (p < .001) |
FAAM sport: 18.8 | FAAM sport: 50.0 |
| S.M. RAIKIN ET AL -201714 | PTA (72), OA (36), RA (7) | Semiconstrained prosthesis Agility (DePuy, Warsaw, IN) | VAS, FAAM, SF-12 score | / | / | FAAM sport: 55.3 |
| F.G. USUELLI ET AL - 20178 | PTA (70), RA (3), other (3) | 3-component mobile-bearing Hintegra (Newdeal SA, Lyon, France) | UCLA, SF-12, AOFAS, VAS, sports participation | UCLA (P < .001) SF-12 (p < .001) AOFAS (p < .001) VAS (p < .001) |
UCLA: 2.4 (0.8) | UCLA: 6.3 (2.3) |
| F. DALAT ET AL - 201415 | OA (29), RA (3) | 3-component mobile-bearing AES Biomet (BiometInc., Valence, France) | AOFAS, FAAM, FFI, SF-36, sports participation | / | / | FAAM sport: 49.5 (24.4) |
| R. SCHUH ET AL - 20129 | OA | 3-component mobile-bearing Hintegra (Newdeal SA, Lyon, France) | UCLA, AOFAS, sports participation, Ankle Activity score | Ankle Activity score (p < .05) worsening | Ankle activity score: 4.7 (2.3) |
Ankle activity score: 3.3 (2.7) UCLA: 6.8 (1.8) |
| F.D. NAAL ET AL - 200910 | Primary OA (35), PTA (47), RA (19) | 3-component uncemented Buechel-Pappas implant (Endotec Inc, South Orange, New Jersey) in 47, 3-component uncemented Mobility prosthesis DePuy Orthopaedics (Warsaw, Indiana) in 54 |
UCLA, AOFAS, IPAQ | UCLA (P < .001) AOFAS (p < .001) |
UCLA: 4.3 (2.2) | UCLA: 6.2 (1.6) |
| M.P. BONNIN ET AL - 200912 | Primary OA (30), PTA (70), RA (40) | Mobile-bearing cementeless Salto total ankle prostheses (Tornier SA, Montbonnot, France) |
AOFAS, FFI, FAAM, VAS, sports participation | / | / | FAAM sport: 48.9 (28) VAS sport [0–100] (100 was level before ankle patology: 53.7 (28) |
| V. VALDERRABANO ET AL - 200611 | Primary OA (21), PTA (115), RA (16) | 3-component mobile-bearing Hintegra (Newdeal SA, Lyon, France) | VAS, AOFAS, ROM, sports participation | VAS (p < .001) AOFAS (p < .001) ROM (p = .04) |
/ | / |
Abbreviations:PTA post traumatic arthritis; RA rheumatoid arthritis; OA osteoarthritis; AA Ankle Artrodesis; FAAM Foot and Ankle Ability Measure; AOFAS American Orthopaedic Foot & Ankle Society; FAOS Foot and Ankle Outcome Score; AOS Ankle Osteoarthritis Scale; SF-# Short Form - #; FFI Foot Function Index; CPG Chronic Pain Grade; VR-12Veterans RAND 12 Item Health Survey; UCLA University of California at Los Angeles; FADI Foot & Ankle Disability Index; SMFA Short Musculoskeletal Function Assessment; SPPB Short Physical Performance Battery; FSST Four-Square Step Test; ROM Range of motion; IPAQ International Physical Activity Questionnaire.
Two studies10,12,13 demonstrated that the osteoarthritis group demonstrated significantly higher scores in the FAOS sports and leisure, FAAM sports activity subscales and VAS score, as well as in sport participation than the rheumatic arthritis group.
No specific TAA implant seemed to correlate with better outcomes scores (Table 5).
3.6. Type of sport activities
Six papers8, 9, 10, 11, 12,15 of 11 have dealt with sport type following TAA (Table 3). The most frequent postoperative activities included cycling, swimming, hiking and gymnastic. Although participation in impact sport was less frequently after TAA implantation, in three distinct studies jogging and downhill skiing were practiced, followed by tennis and skiing reported in two different studies (Table 4).
Table 4.
Sport participation frequency after ankle arthroplasty.
| Authors |
Non impact sport |
Impact sport |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sports | Cycling | Swimming | Dancing | Hiking | Golf | Bowling | Gymnastics | Home gardening | Jogging | Tennis | Skiing | Cross-country skiing | Downhill skiing | Martial arts | Horseback riding | Water-skiing |
| R. SCHUH ET AL - 20129 | x | x | x | x | x | |||||||||||
| F.G. USUELLI ET AL - 20178 | x | x | x | x | x | |||||||||||
| F. DALAT ET AL - 201415 | x | x | ||||||||||||||
| F.D. NAAL ET AL - 200910 | x | x | x | x | x | |||||||||||
| M.P. BONNIN ET AL - 200912 | x | x | x | x | x | x | x | x | x | x | ||||||
|
V. VALDERRABANO ET AL - 200611 |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
x |
|||||
| Frequency | 6 | 5 | 2 | 4 | 1 | 1 | 4 | 1 | 3 | 2 | 2 | 1 | 3 | 1 | 1 | 1 |
One study11 showed a significant higher participation rate between pre- and postoperative situations for hiking (P < .001) and biking (P = .02). While two papers reported significantly fewer patients were involved in high-demanding activities, such as tennis and jogging (P < .05)10 and none practiced soccer, handball, ice-skating and rowing after TAA.9
3.7. Statistical analysis
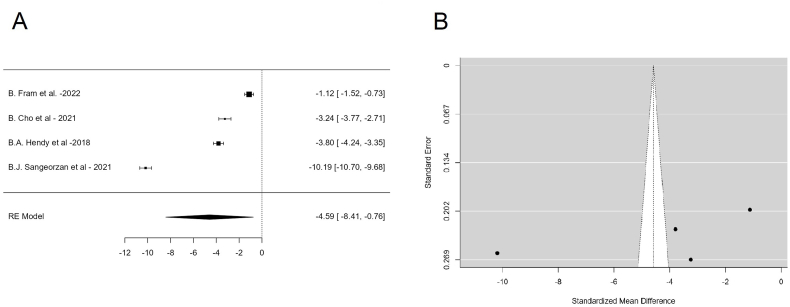
Four studies were included in the FAAM meta-analysis. The average outcome differed significantly from zero (z = 2.341, p = .0189). An examination of the studentized residuals revealed that one study (REF) had a value larger than ± 2.4977 and may be a potential outlier in the context of this model (Fig. 2).
Fig. 2.
Forest Plot (A) and Funnel Plot (B) of the FAAM sport outcomes Meta-analysis performed on 4 Studies.
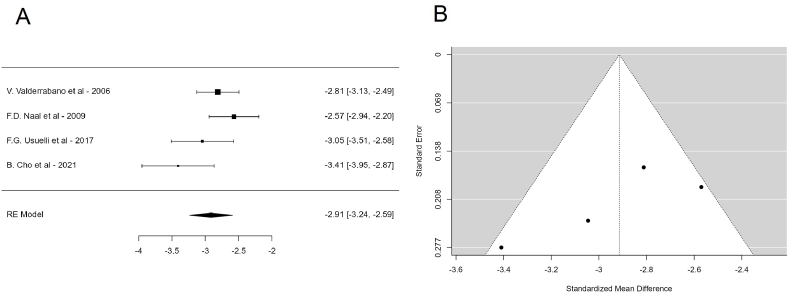
Four studies were included in the AOFAS meta-analysis analysis. The average outcome differed significantly from zero (z = 17.7424, p < .0001) (Fig. 3).
Fig. 3.
Forest Plot (A) and Funnel Plot (B) of the AOFAS outcomes Meta-analysis performed on 4 Studies.
4. Discussion
Historically, Ankle fusion has traditionally been considered the gold standard treatment for end-stage ankle OA. Despite the good results reported,16 ankle fusion affects lower limb kinematics, restricting gait patterns and may lead to OA of adjacent joints overtime. TAA was proposed in order to restore a normal kinematics, to improve gait patterns and to protect adjacent joints from OA.17,18 For this reason, TAA may represent a better solution also in active patients who wish to optimize joint function.
Nevertheless, in the past, ankle fusion was preferred for young and active people, while TAA was more advisable in patients with low functional demands.16,19 This tendency was probably due to the higher complication and revision rates reported for TAA,20 and high-impact activity were hypothesized to lead to earlier implant failure.21, 22, 23
More than twenty years after these indications,24 this trend seems to be gradually changing,26 thanks to the evolution of implant designs, materials, and surgical techniques.25
Two of the selected studies compared TAA with ankle fusion and reported a better functional improvement in the TAA group,27 and a decrease in sports participation in the ankle fusion group.9 Despite this evidence, nowadays the sport activity level recommended after both TAA and ankle fusion is similar.28, 29, 30
This review assessed the chance of returning to sport, the achievable activity level, the type of patients who can play sport and the type of sports activities that can be done after TAA.
4.1. Chance to return to sport
The results suggest that the prevalence of sports-active patients raises after TAA.
Most articles in the literature reported that the rate of sports participation varies between 29% and 56% after total hip arthroplasty (THA), and between 34% and 77% after total knee arthroplasty (TKA).31, 32, 33, 34 The mean rate of sports participation after TAA in this systematic review was of 61.9% (range 49.4–76%), thus in line with other joint arthroplasties. However, it would be necessary to consider the large inhomogeneity in sample size of the studies and that only 4 of 11 studies reported pre- and postoperative sports participation, which may have biased the mean sport participation rate reported in this review.
Patients were more likely to limit their sporting activity for reasons unrelated to their ankle, and the proportion of patients who did not play sport because of their operated ankle was lower than those who returned to sport.12
4.2. Achievable activity level
A large proportion of patients were able to return to their preoperative activity level, although only three studies addressed the sport activity level after surgery and the preoperative activity level is unclear.
Some studies in the literature suggest that the increased activity levels and participation in joint-bearing sports might also be associated with increased rates of aseptic loosening, polyethylene wear and fracture, and earlier implant failure.21, 22, 23 Nevertheless, during 44 months of follow-up Naal et al.10 reported no relationship between highly active patients and the onset of radiographic periprosthetic radiolucency, as well as Hörterer et al.35 conducting a systematic review didn't establish evidence that engaging in sports activities could potentially be linked to a higher risk of TAA failure. Similarly, Raikin et al.14 demonstrated a TAA survival rate of 80% at nine years with no association between failure rate and sports participation, but rather reported that patients with their original implant were still functioning also in sports activities.
However, long-term follow-ups and randomized trials would be needed to evaluate whether those actually participate in sports are at a greater risk of polyethylene wear and implant failure.
4.3. Type of patients who are able to play sport
The active younger patient with a low BMI and non-inflammatory osteoarthritis can reasonably expect to return to sport. None of the trials found a specific age range that correlated better with sports participation and a higher level of activity. Though, the mean age of the studies showing a high percentage of sport participation was 57.8 years old.8, 9, 10, 11
Significant relationships were reported between sport participation and functional outcome measures after TAA, such as FAAM sport subscale and UCLA scores,10,11 which signifies their activity level improvement. Furthermore, sports-active TAA patients reported higher AOFAS score than did inactive ones (P < .001).11 Similarly, better postoperative range of motion correlated with less pain as measured by the VAS and better function as measured by the FAAM.36 Patients who obtained the best outcomes, even those not directly related to sport, were the most active and those who returned to the preoperative sport level. The single score used in one study9 that reported the worsening of the outcomes between pre- and post-operative situations was the Ankle Activity Score, which was originally presented as an outcome measure for patients with ankle ligament injuries. The Ankle Activity Score reduction was attributed by the authors to patients’ selection of less demanding sports activities on the ankle joint after surgery, which does not indicate a general deterioration in sports performance, but most likely point a change in sport type practiced.
Despite a few studies reporting inconsistent outcomes, a significant post-operative improvement in different PROMs, confirmed by the FAAM sport and AOFAS outcomes meta-analysis, was reported by almost all authors.
Although significant improvement in return to sports and functional activity scores was already recorded at 12 months after surgery,8 the current literature has not yet clearly identified the ideal timing for return to sports.
4.4. Type of sport activities
Generally, patients who underwent total joint arthroplasty are advised to engage in low-impact sports while avoiding high-impact activities.29,30
In this review, low-impact sports are preferred following TAA, with cycling, swimming, hiking, and gymnastic among the most frequent practiced. Nevertheless, some patients also enjoyed in high-impact sports, such as jogging, tennis and skiing. Bonnin et al.12 revealed that a limited proportion of patients were able to realize their desired sports activities. Specifically, only 20% of individuals who aspired to play tennis, 40% of those interested in downhill skiing, and merely 15% of those who wished to engage in running were able to actively participate in these sports. The ability to practice high-impact sports is likely to be highly dependent on the level of preoperative physical training and significance prior experience in that sport. This should be considered as the satisfaction of preoperative expectations is a key factor in determining the subjective outcome of intervention, hence it is imperative to thoroughly assess and understand the patient's desires prior to the surgery.37
4.5. Limitations
An important limitation is the retrospective nature of most of the selected studies, with no randomization or control group. Other limitations include the large inhomogeneity in sample size across studies and the outcomes related to sports determined by questionnaire answers, making interviewer bias likely. The presence of conflicts of interest between authors involved in designing a prosthesis may introduce bias into certain trials.
In addition, sports-related total joint replacement is a sensitive issue because most orthopedic surgeons believe that the goal of total joint replacement for their patients is not to play sports. This may explain why few studies reported on sports participation after TAA, and there may be some bias because these authors may have performed TAA in more active patients, and this is why they used sports participation as an outcome measure, whereas other studies performed in more sedentary populations would probably report lower rates of sports participation, if this parameter were evaluated.
Considering the abovementioned limitations, and the lack of strong evidence, the current literature does not allow to advise TAA for young active patients who want to play sports after surgery. A customized approach should always be adopted, considering the patients’ needs, and pre-operative clinical and athletic condition, also weighting the possible complications of the surgical procedure. Informed consent plays a fundamental role in establishing realistic postoperative expectations.
6. Conclusions
Some studies show that patients undergoing TAA, especially if young, with low BMI and affected by non-inflammatory osteoarthritis, have a 62% chance to play sports after surgery and in most cases can return to preoperative activity level. Despite that, nowadays no strong evidence supports these data.
For TAA patients who can play sports, the most approachable activities are swimming, cycling, hiking, and gymnastics. High impact sports seem to be allowed for only few and selected patients.
Further prospective randomized trials are needed to validate these initial findings and to establish more precise expectations regarding sports activity after TAA.
Ethical approval
Ethical Approval was not required for this systematic review.
Informed consent and patient details
It was not required for this systematic review.
Declarations of interest
None.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author's contribution
All authors contributed to the study conception, drafting and editing. All authors read and approved the final manuscript.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jor.2023.09.001.
Contributor Information
Alberto Arceri, Email: alberto.arceri@ior.it.
Antonio Mazzotti, Email: antonio.mazzotti@ior.it.
Simone Zielli, Email: simoneottavio.zielli@ior.it.
Simone Bonelli, Email: simone.bonelli@ior.it.
Elena Artioli, Email: elena.artioli@ior.it.
Pejman Abdi, Email: pejman.abdi@ior.it.
Laura Langone, Email: laura.langone@ior.it.
Cesare Faldini, Email: cesare.faldini@ior.it.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Clifford P.E., Mallon W.J. Sports after total joint replacement. Clin Sports Med. 2005;24(1):175–186. doi: 10.1016/j.csm.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 2.Horisberger M., Valderrabano V., Hintermann B. Posttraumatic ankle osteoarthritis after ankle-related fractures. J Orthop Trauma. 2009;23(1):60–67. doi: 10.1097/BOT.0b013e31818915d9. [DOI] [PubMed] [Google Scholar]
- 3.Saltzman C.L., Salamon M.L., Blanchard G.M., et al. Epidemiology of ankle arthritis: report of a consecutive series of 639 patients from a tertiary orthopaedic center. Iowa Orthop J. 2005;25:44–46. [PMC free article] [PubMed] [Google Scholar]
- 4.M D., L A., T J., A Dg. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4) doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 5.Martin R.L., Irrgang J.J., Burdett R.G., Conti S.F., Van Swearingen J.M. Evidence of validity for the foot and ankle ability measure (FAAM) Foot Ankle Int. 2005;26(11):968–983. doi: 10.1177/107110070502601113. [DOI] [PubMed] [Google Scholar]
- 6.Zahiri C.A., Schmalzried T.P., Szuszczewicz E.S., Amstutz H.C. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13(8):890–895. doi: 10.1016/s0883-5403(98)90195-4. [DOI] [PubMed] [Google Scholar]
- 7.Slim K., Nini E., Forestier D., Kwiatkowski F., Panis Y., Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 8.Usuelli F.G., Pantalone A., Maccario C., Guelfi M., Salini V. Sports and recreational activities following total ankle replacement. Joints. 2017;5(1):12–16. doi: 10.1055/s-0037-1601408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schuh R., Hofstaetter J., Krismer M., Bevoni R., Windhager R., Trnka H.J. Total ankle arthroplasty versus ankle arthrodesis. Comparison of sports, recreational activities and functional outcome. Int Orthop. 2012;36(6):1207–1214. doi: 10.1007/s00264-011-1455-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Naal F.D., Impellizzeri F.M., Loibl M., Huber M., Rippstein P.F. Habitual physical activity and sports participation after total ankle arthroplasty. Am J Sports Med. 2009;37(1):95–102. doi: 10.1177/0363546508323253. [DOI] [PubMed] [Google Scholar]
- 11.Valderrabano V., Pagenstert G., Horisberger M., Knupp M., Hintermann B. Sports and recreation activity of ankle arthritis patients before and after total ankle replacement. Am J Sports Med. 2006;34(6):993–999. doi: 10.1177/0363546505284189. [DOI] [PubMed] [Google Scholar]
- 12.Bonnin M.P., Laurent J.R., Casillas M. Ankle function and sports activity after total ankle arthroplasty. Foot Ankle Int. 2009;30(10):933–944. doi: 10.3113/FAI.2009.0933. [DOI] [PubMed] [Google Scholar]
- 13.Cho B.K., An M.Y., Ahn B.H. Comparison of clinical outcomes after total ankle arthroplasty between end-stage osteoarthritis and rheumatoid arthritis. Foot Ankle Int. 2021;42(5):589–597. doi: 10.1177/1071100720979923. [DOI] [PubMed] [Google Scholar]
- 14.Raikin S.M., Sandrowski K., Kane J.M., Beck D., Winters B.S. Midterm outcome of the agility total ankle arthroplasty. Foot Ankle Int. 2017;38(6):662–670. doi: 10.1177/1071100717701232. [DOI] [PubMed] [Google Scholar]
- 15.Dalat F., Trouillet F., Fessy M.H., Bourdin M., Besse J.L. Comparison of quality of life following total ankle arthroplasty and ankle arthrodesis: retrospective study of 54 cases. Orthop Traumatol Surg Res. 2014;100(7):761–766. doi: 10.1016/j.otsr.2014.07.018. [DOI] [PubMed] [Google Scholar]
- 16.Hanna M., Whicker E.A., Traub B., Allam E., Labib S.A. Sport activity levels following ankle fusion. Int Orthop. 2021;45(9):2347–2354. doi: 10.1007/s00264-021-05100-7. [DOI] [PubMed] [Google Scholar]
- 17.Beyaert C., Sirveaux F., Paysant J., Molé D., André J.M. The effect of tibio-talar arthrodesis on foot kinematics and ground reaction force progression during walking. Gait Posture. 2004;20(1):84–91. doi: 10.1016/j.gaitpost.2003.07.006. [DOI] [PubMed] [Google Scholar]
- 18.Haddad S.L., Coetzee J.C., Estok R., Fahrbach K., Banel D., Nalysnyk L. Intermediate and long-term outcomes of total ankle arthroplasty and ankle arthrodesis. A systematic review of the literature. J Bone Joint Surg Am. 2007;89(9):1899–1905. doi: 10.2106/JBJS.F.01149. [DOI] [PubMed] [Google Scholar]
- 19.Thordarson D.B. Fusion in posttraumatic foot and ankle reconstruction. J Am Acad Orthop Surg. 2004;12(5):322–333. doi: 10.5435/00124635-200409000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Liu S., Wang Y., Zhang M., et al. A comparative study of modern total ankle replacement and ankle arthrodesis for ankle osteoarthritis at different follow-up times: a systematic review and meta-analysis. Int Orthop. March 10, 2023 doi: 10.1007/s00264-023-05753-6. Published online. [DOI] [PubMed] [Google Scholar]
- 21.Schmalzried T.P., Shepherd E.F., Dorey F.J., et al. The John Charnley Award. Wear is a function of use, not time. Clin Orthop Relat Res. 2000;381:36–46. doi: 10.1097/00003086-200012000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Harris N.J., Brooke B.T., Sturdee S. A wear debris cyst following S.T.A.R. Total Ankle Replacement--surgical management. Foot Ankle Surg. 2009;15(1):43–45. doi: 10.1016/j.fas.2008.06.002. [DOI] [PubMed] [Google Scholar]
- 23.Scott A.T., Nunley J.A. Polyethylene fracture following STAR ankle arthroplasty: a report of three cases. Foot Ankle Int. 2009;30(4):375–379. doi: 10.3113/FAI.2009.0375. [DOI] [PubMed] [Google Scholar]
- 24.Neufeld S.K., Lee T.H. Total ankle arthroplasty: indications, results, and biomechanical rationale. Am J Orthoped. 2000;29(8):593–602. [PubMed] [Google Scholar]
- 25.Mazzotti A., Arceri A., Zielli S., Bonelli S., Viglione V., Faldini C. Patient-specific instrumentation in total ankle arthroplasty. World J Orthoped. 2022;13(3):230–237. doi: 10.5312/wjo.v13.i3.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cody E.A., Scott D.J., Easley M.E. Total ankle arthroplasty: a critical analysis review. JBJS Rev. 2018;6(8):e8. doi: 10.2106/JBJS.RVW.17.00182. e8. [DOI] [PubMed] [Google Scholar]
- 27.Sangeorzan B.J., Ledoux W.R., Shofer J.B., et al. Comparing 4-year changes in patient-reported outcomes following ankle arthroplasty and arthrodesis. J Bone Joint Surg Am. 2021;103(10):869–878. doi: 10.2106/JBJS.20.01357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vertullo C.J., Nunley J.A. Participation in sports after arthrodesis of the foot or ankle. Foot Ankle Int. 2002;23(7):625–628. doi: 10.1177/107110070202300707. [DOI] [PubMed] [Google Scholar]
- 29.Healy W.L., Iorio R., Lemos M.J. Athletic activity after joint replacement. Am J Sports Med. 2001;29(3):377–388. doi: 10.1177/03635465010290032301. [DOI] [PubMed] [Google Scholar]
- 30.Macaulay A.A., VanValkenburg S.M., DiGiovanni C.W. Sport and activity restrictions following total ankle replacement: a survey of orthopaedic foot and ankle specialists. Foot Ankle Surg. 2015;21(4):260–265. doi: 10.1016/j.fas.2015.01.014. [DOI] [PubMed] [Google Scholar]
- 31.Mallon W.J., Callaghan J.J. Total hip arthroplasty in active golfers. J Arthroplasty. 1992;7(Suppl):339–346. doi: 10.1016/s0883-5403(07)80022-2. [DOI] [PubMed] [Google Scholar]
- 32.Ritter M.A., Meding J.B. Total hip arthroplasty. Can the patient play sports again? Orthopedics. 1987;10(10):1447–1452. doi: 10.3928/0147-7447-19871001-15. [DOI] [PubMed] [Google Scholar]
- 33.Huch K., Muller K., Sturmer T., Brenner H., Puhl W., Gunther K. Sports activities 5 years after total knee or hip arthroplasty: the Ulm Osteoarthritis Study. Ann Rheum Dis. 2005;64(12):1715–1720. doi: 10.1136/ard.2004.033266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bradbury N., Borton D., Spoo G., Cross M.J. Participation in sports after total knee replacement. Am J Sports Med. 1998;26(4):530–535. doi: 10.1177/03635465980260041001. [DOI] [PubMed] [Google Scholar]
- 35.Hörterer H., Miltner O., Müller-Rath R., Phisitkul P., Barg A. Sports activity in patients with total ankle replacement. Sports Orthopaedics and Traumatology Sport-Orthopädie - Sport-Traumatologie. 2015;31(1):34–40. doi: 10.1016/j.orthtr.2014.12.011. [DOI] [Google Scholar]
- 36.Ba H., El M., N K., et al. Improvement of outcomes during the First two years following total ankle arthroplasty. J Bone Jt Surg Am Vol. 2018;100(17) doi: 10.2106/JBJS.17.01021. [DOI] [PubMed] [Google Scholar]
- 37.Noble P.C., Conditt M.A., Cook K.F., Mathis K.B. The John Insall Award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. 2006;452:35–43. doi: 10.1097/01.blo.0000238825.63648.1e. [DOI] [PubMed] [Google Scholar]
- 38.Fram B., Corr D.O., Rogero R.G., Pedowitz D.I., Tsai J. Short-term complications and outcomes of the cadence total ankle arthroplasty. Foot Ankle Int. 2022;43(3):371–377. doi: 10.1177/10711007211043853. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.