Abstract
A 63-year-old man was analyzed for platypnea-orthodeoxia syndrome (POS). A complete obstruction due to bronchial carcinoma was found in the left main bronchus with bronchoscopy. After left sided pneumonectomy POS resolved completely. Historical reports suggest increased shunting through the left lung could occur in the upright position caused by decreased compression of the left pulmonary artery due to the central bronchial carcinoma. Partially absent hypoxic vasoconstriction was confirmed in this case and suggests (without a relevant shunt through a patent foramen ovale) this ‘historical’ hypothesis could explain the POS due to increased shunting in the upright position in this patient.
Keywords: Platypnea-orthodeoxia syndrome, Left main bronchus carcinoma, Lung carcinoma
1. Introduction
Platypnea-orthodeoxia syndrome (POS) is a rare syndrome characterized by position dependent dyspnea. The characteristic findings are dyspnea (platypnea) and (arterial) desaturation (orthodeoxia) in the upright position and improving in the recumbent position. Multiple causes for POS have been described and divided in cardiac, pulmonary and miscellaneous causes [1]. The most common cause is a patent foramen ovale (PFO) or atrial septal defect with right-to-left shunting in the upright position. Most patients with an intracardiac shunt causing POS demonstrate a secondary anatomic or a functional defect that redirects preferential flow causing right-to-left shunting in the upright position [[2], [3], [4]]. Other causes are rare and underlying pathophysiologic mechanisms are not completely understood. This case illustrates a rare cause of POS in a patient with a left sided main bronchus carcinoma and considerations about the probable pathophysiology.
2. Case report
A 63-year-old man presented at the emergency department with a 2 week history of shortness of breath worsening in the upright position. The patient had no relevant medical history. Physical examination showed absent breathing sounds on the left hemithorax and no signs of orthostatic hypotension. The patient showed signs of POS with an oxygen saturation of 68% in the upright position and 93% in the supine position with 5 L of oxygen suppletion through nasal cannula. The arterial blood gas in the supine position showed a hypoxemia (pH 7,44; pO2 8.1 kPa; pCO2 4,3 kPa; bicarbonate 22 mmol/L) and chest x-ray (Fig. 1) showed a complete atelectasis of the left lung. Bronchoscopy revealed a complete obstruction caused by adenosquamous bronchial carcinoma (Fig. 2) in the left main bronchus. Lung perfusion scintigraphy in recumbent position(Fig. 3) showed clues for absent hypoxic vasoconstriction, because the left lung still showed a perfusion contribution of 30%. Transthoracic echocardiography with agitated salt showed a small PFO with only subtle right-to-left shunting in the upright position. After left sided pneumonectomy the platypnea-orthodeoxia syndrome (POS) resolved completely. Echocardiography was repeated 6 months after pneumonectomy and still showed signs for subtle right-to-left shunting through the PFO. Only symptoms of a gentle shortness of breath with exertion were reported by the patient. Because the persistent subtle right-to-left shunting through the PFO and gentle shortness of breath with exertion cardiopulmonary exercise testing (CPET) was performed in the upright position with arterial blood sampling. CPET showed no signs of hypoxemia at rest (pO2 12.2kPa) nor with maximum exercise (pO2 13.7kPa). Maximum VO2 was reached 1842ml/min and 120% of predicted.
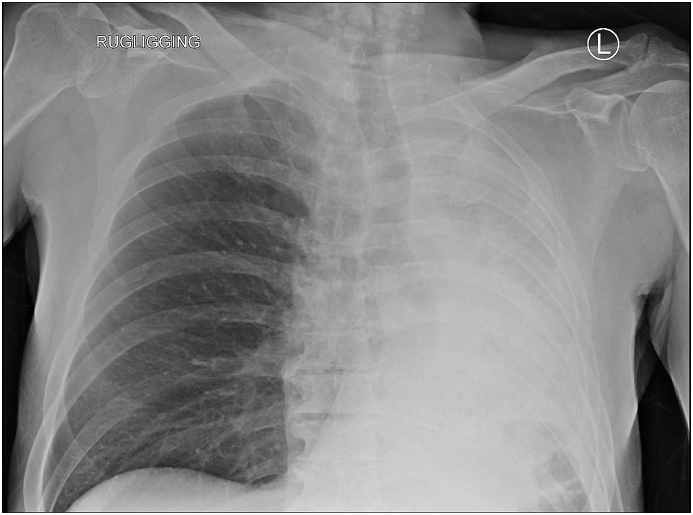
Fig. 1.
Chest x -ray in the supine position showing a complete atelectasis of the left lung.
Fig. 2.
Complete obstruction of the left main bronchus due to adenosquamous carcinoma.
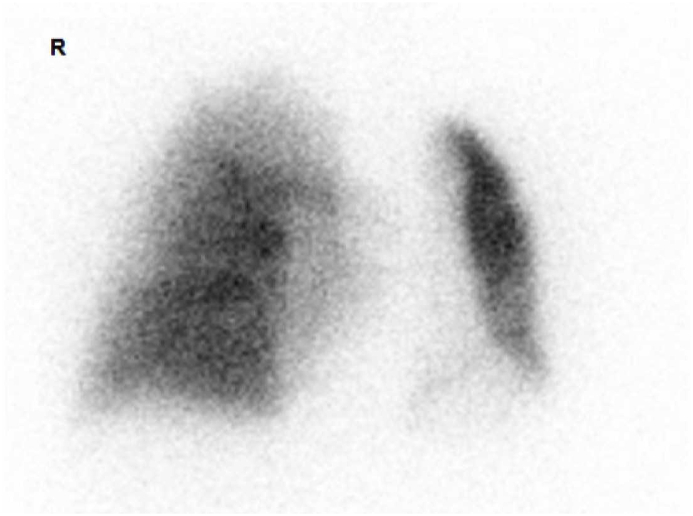
Fig. 3.
Lung perfusion scintigraphy revealed the left lung still showing a perfusion contribution of 30% in recumbent position.
After the pneumonectomy the patient was treated with adjuvant chemotherapy. Multiple suspected lymph nodes and right femur metastasis were found 1.5 year after the pneumonectomy. The femur metastasis was treated with radiotherapy whereafter immunotherapy (pembrolizumab) was started because of PDL1 of 70% and no activating mutation. Nine months after the first treatment with immunotherapy a complete response was found with follow-up CT scan.
3. Discussion
Left main bronchus carcinoma is described in literature to cause POS. It is not completely clear which mechanism induces this syndrome. Increased pulmonary shunting through the not ventilated lung is described as the most likely pathophysiology. Probably the pulmonary shunt increases in the upright position because the left pulmonary artery is upright less compressed due to the central bronchogenic carcinoma [5,6]. Contrast-enhanced chest CT showed a narrow relation between the central tumour and left main pulmonary artery (Fig. 4) in this patient suggesting this narrow relation could support this hypothesis. Moreover hypoxic vasoconstriction did not fully occur in this patient. There are some clues hypoxic vasoconstriction does not always occur in patients with liver cirrosis [7]. In this patient there was already a two-week history of platypnea and the left lung still contributed to 30% of the total lung perfusion. Also there was no history of liver cirrhosis, known liver disease or abundant alcohol consumption in this patient. A PFO persist in 15–35% of adults [8]. Probably the subtle right-to-left shunting through the PFO played only a minor role in the POS since after pneumonectomy it was still recognized by echocardiography while the POS resolved completely. Moreover a right-to-left shunt through a patent PFO causing POS is frequently described after and not before lobectomy or pneumonectomy [9,10].
Fig. 4.
Contrast-enhanced CT showing a narrow relation between the central tumour and left main pulmonary artery.
4. Conclusion
A left main bronchus carcinoma luxated platypnea-orthodeoxia syndrome in this case. We conclude this case illustrates partially absent hypoxic vasoconstriction can occur in patients without known liver disease and contributed to the platypnea-orthodeoxia syndrome in this patient with central bronchial carcinoma. Last but not least; ‘It is not always a patent foramen ovale that counts the most in POS’.
Declaration of competing interest
There is no conflict of interest.
Handling Editor: DR AC Amit Chopra
References
- 1.Agrawal A., Arunabh Talwar A.P. The multiple dimensions of Platypnea-Orthodeoxia syndrome: a review. Respir. Med. 2017;129:31–38. doi: 10.1016/j.rmed.2017.05.016. [DOI] [PubMed] [Google Scholar]
- 2.Mima H., Sakamoto J., Mikaye M., Enomoto S., Kondo H., Tamura T. Posture-related change in intracardiac blood flow detected by transoesophageal echocardiography in platypnea-orthodeoxia-syndrome. Cardiovascul. Imag. Case Rep. 2022;6(5):218–222. doi: 10.1016/j.case.2022.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schmid S., John G., Mossaz L., Choutko V. An uncommon cause of hypoxemia: platypnea orthodeoxia syndrome. J. Geriatric Cardiol. 2015;12(5):584–587. doi: 10.11909/j.issn.1671-5411.2015.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nassif M., Lu H., Konings T.C., Bouma B.J., Vonk Noordegraaf A., Straver B., Blom N.A., Clur S.A., Backx A.P.C.M., Groenink M., Boekholdt S.M., Koolbergen D.R., Hazekamp M.G., Mulder B.J.M., de Winter R.J. Neth. Heart J. 2015;23(11):539–545. doi: 10.1007/s12471-015-0714-5. Platypnoea-orthodeoxia syndrome, an underdiagnosed cause of hypoxaemia: four cases and the possible underlying mechanisms. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gacad G., Akhtar N., Cohn J.N. Orthostatic Hypoxemia in a patient with bronchogenic carcinoma. Arch. Intern. Med. 1974;184:1113–1115. [PubMed] [Google Scholar]
- 6.Awan A.N., Ashraf R., Meyerson M.B., Dunn T.L. Radiation-induced bronchial stenosis: a new cause of platypnea-orthodeoxia. South. Med. J. 1999;92(7):720–724. doi: 10.1097/00007611-199907000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Daoud F., Reeves J.T., Schaeffer J.W. Failure of hypoxic pulmonary vasoconstriction in patients with liver cirrhosis. J. Clin. Invest. 1972;51(5):1076–1080. doi: 10.1172/JCI106899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Teshome M.K., Najib K., Nwagbara C.C., Akinseye O.A., Ibebuogu U.N. Patient foramen ovale: a comprehensive review. Curr. Probl. Cardiol. 2020;45(2) doi: 10.1016/j.cpcardiol.2018.08.004. [DOI] [PubMed] [Google Scholar]
- 9.D'Mello A.C., Haji K., Moir S., Leong P. Platypnea–orthodeoxia syndrome after right lower lobectomy for lung cancer. Oxford Med. Case Rep. 2019;1:1–4. doi: 10.1093/omcr/omy049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smeenk F.W., Twisk S.P., Berreklouw E., Gooszen H.C., Postmus P.E. Dyspnea after pneumonectomy. Eur. Respir. J. 1991;4:243–245. [PubMed] [Google Scholar]