Abstract
BACKGROUND
The immunosuppressive capacity of mesenchymal stem cells (MSCs) is dependent on the “license” of several proinflammatory factors to express immunosuppressive factors such as programmed cell death 1 ligand 1 (PD-L1), which determines the clinical therapeutic efficacy of MSCs for inflammatory or immune diseases. In MSCs, interferon-gamma (IFN-γ) is a key inducer of PD-L1 expression, which is synergistically enhanced by tumor necrosis factor-alpha (TNF-α); however, the underlying mechanism is unclear.
AIM
To reveal the mechanism of pretreated MSCs express high PD-L1 and explore the application of pretreated MSCs in ulcerative colitis.
METHODS
We assessed PD-L1 expression in human umbilical-cord-derived MSCs (hUC-MSCs) induced by IFN-γ and TNF-α, alone or in combination. Additionally, we performed signal pathway inhibitor experiments as well as RNA interference experiments to elucidate the molecular mechanism by which IFN-γ alone or in combination with TNF-α induces PD-L1 expression. Moreover, we used luciferase reporter gene experiments to verify the binding sites of the transcription factors of each signal transduction pathway to the targeted gene promoters. Finally, we evaluated the immunosuppressive capacity of hUC-MSCs treated with IFN-γ and TNF-α in both an in vitro mixed lymphocyte culture assay, and in vivo in mice with dextran sulfate sodium-induced acute colitis.
RESULTS
Our results suggest that IFN-γ induction alone upregulates PD-L1 expression in hUC-MSCs while TNF-α alone does not, and that the co-induction of IFN-γ and TNF-α promotes higher expression of PD-L1. IFN-γ induces hUC-MSCs to express PD-L1, in which IFN-γ activates the JAK/STAT1 signaling pathway, up-regulates the expression of the interferon regulatory factor 1 (IRF1) transcription factor, promotes the binding of IRF1 and the PD-L1 gene promoter, and finally promotes PD-L1 mRNA. Although TNF-α alone did not induce PD-L1 expression in hUC-MSCs, the addition of TNF-α significantly enhanced IFN-γ-induced JAK/STAT1/IRF1 activation. TNF-α up-regulated IFN-γ receptor expression through activation of the nuclear factor kappa-B signaling pathway, which significantly enhanced IFN-γ signaling. Finally, co-induced hUC-MSCs have a stronger inhibitory effect on lymphocyte proliferation, and significantly ameliorate weight loss, mucosal damage, inflammatory cell infiltration, and up-regulation of inflammatory factors in colitis mice.
CONCLUSION
Overall, our results suggest that IFN-γ and TNF-α enhance both the immunosuppressive ability of hUC-MSCs and their efficacy in ulcerative colitis by synergistically inducing high expression of PD-L1.
Keywords: Human umbilical-cord-derived mesenchymal stem cells, Programmed cell death 1 ligand 1, Immunomodulation, Interferon-gamma, Tumor necrosis factor-alpha, Ulcerative colitis
Core Tip: Our study showed that interferon-gamma (IFN-γ) and tumor necrosis factor-alpha (TNF-α) significantly induced programmed cell death protein 1 ligand 1 (PD-L1) expression in human umbilical-cord-mesenchymal stem cells (hUC-MSCs), and pretreated hUC-MSCs exhibited stronger immunomodulatory capacity. Signaling pathway analysis showed that TNF-α up-regulated IFN-γ receptor expression in hUC-MSCs through nuclear factor kappa-B pathway, and then promoted IFN-γ -mediated activation of JAK/STAT1/interferon regulatory factor 1 pathway and PD-L1 expression. In ulcerative colitis mice, hUC-MSCs pretreated with IFN-γ and TNF-α exhibited stronger immunosuppressive ability through high expression of PD-L1, effectively inhibited the inflammation in the colon of mice.
INTRODUCTION
Mesenchymal stem cells (MSCs) are multipotent adult stem cells present in multiple tissues, including the umbilical cord, bone marrow, and fat tissue. MSCs can self-renew by dividing and differentiating into multiple tissues, including bone, cartilage, muscle, fat cells, and connective tissue[1]. In addition, MSCs have a strong immunomodulatory capacity, exerting both anti-inflammatory and pro-inflammatory effects[2]. Owing to their immunosuppressive function, MSCs are widely used to treat various inflammatory and autoimmune diseases, including inflammatory bowel disease, rheumatoid arthritis, pulmonary fibrosis, and systemic sclerosis[3-6]. However, the current clinical efficacy of MSCs transplantation (MSCT) is highly variable among individuals, even for the same autoimmune disease[7]. In general, the immunosuppressive function of MSCs depends on the licensing of the proinflammatory factor-mediated immunological microenvironment[8,9]. The individual differences in the clinical efficacy of MSCT might be explained by the substantial individual variations in the pro-inflammatory factor-mediated immunological microenvironment at different stages of disease development in patients with inflammatory or autoimmune diseases. Therefore, to improve the therapeutic efficacy of MSCT in these diseases, there is an urgent need to explore the licensing mechanism of the immunosuppressive function of MSCs and to establish an optimal strategy for inducing and maintaining immunosuppressive MSCs.
It is currently believed that immunosuppressive MSCs induced by pro-inflammatory factors inhibit the activity of various immune cells by secreting many soluble immunosuppressive factors, such as indoleamine 2,3-dioxygenase (IDO). They also express many immunosuppressive receptors, such as programmed cell death 1 ligand 1 (PD-L1), which functions in a cell-to-cell contact manner[10,11]. Programmed cell death 1 (PD-1) is an immune-inhibitory receptor expressed in activated T cells, which binds to PD-L1 and can inhibit proliferation, induce apoptosis, and restore the subgroup balance of T cells[12]. PD-1/PD-L1 are important immune checkpoint molecules that play a pivotal role in tumor immune escape[13]. Emerging evidence suggests that PD-1/PD-L1 dysfunction is also involved in the immune hyperactivity observed in multiple autoimmune and inflammatory diseases[14,15]. Additionally, PD-L1 plays an important role in the immunosuppressive capacity of MSCs, inhibiting the activation of the immune response in a variety of ways. This includes reducing the release of inflammatory factors, the proliferation and activation of T cells, and the Th17-mediated autoimmune response, as well as augmenting the generation of regulatory T cells (Tregs)[15-17]. Therefore, to improve the therapeutic efficacy of MSCs for inflammatory or autoimmune related diseases, there is an urgent need to clarify the regulatory mechanism of PD-L1 expression in MSCs and to establish an optimal strategy for inducing and maintaining this expression.
Interferon-gamma (IFN-γ) alone has been suggested to upregulate PD-L1 expression in MSCs at low levels, although the specific mechanism remains unclear[18]. It is also unclear whether a combination of proinflammatory factors can synergistically enhance PD-L1 expression in MSCs and their immunosuppressive function. Notably, researchers have recently demonstrated that the immunosuppressive capacity of MSCs depends on stimulation by IFN-γ, and the effect can be amplified further by cytokines, such as tumor necrosis factor-α (TNF-α)[4,19]. In addition, Li et al[20] recently reported that TNF-α can enhance the IFN-γ-induced PD-L1 expression in hepatocellular carcinoma cells. Such findings suggest that TNF-α could also enhance IFN-γ-induced PD-L1 expression in MSCs. In the present study, we first confirmed that IFN-γ induced human-umbilical-cord-MSCs (hUC-MSCs) express PD-L1 through the JAK/STAT1/IRF1 pathway. Second, we observed that TNF-α synergistically enhanced PD-L1 expression induced by IFN-γ in hUC-MSCs. TNF-α also upregulated IFN-γ receptor 1 (IFNGR1) expression through the nuclear factor kappa-B (NF-κB) signaling pathway to promote IFN-γ/IFNGR/STAT1/ interferon regulatory factor 1 (IRF1)/PD-L1 signaling axis activation. Finally, based on an in vitro lymphocyte mixing experiment and an in vivo dextran sulfate sodium (DSS)-induced acute colitis mouse model, we found an optimal strategy of enhancing the immunosuppressive capacity of hUC-MSCs by licensing with IFN-γ and TNF-α. The results not only elucidate the specific molecular mechanism by which the IFN-γ and TNF-α combination enhances the immunosuppressive function of MSCs, but also provide a theoretical basis for improving the therapeutic efficacy of MSCT in future clinical applications.
MATERIALS AND METHODS
Culture and treatment of hUC-MSCs
All hUC-MSCs were provided by the FuMei Stem Cell Biotechnology Company (Chongqing, China). The hUC-MSCs used in the present study were identified by flow cytometry and three-lineage differentiation culture. The results showed that the hUC-MSCs had the correct molecular phenotype and three-lineage differentiation potential (Supplementary Figure 1). All hUC-MSCs used in the experiment were derived from passages 3 to 7. hUC-MSCs were cultured and stimulated in serum-free medium (LONZA). To measure the induction of PD-L1 expression, hUC-MSCs were incubated with human IFN-γ, TNF-α or both (Peprotech, United States). After 4 h of culture, the cells were harvested for mRNA expression analysis using quantitative real-time PCR (qRT-PCR). After 24 h of culture, they were harvested for protein expression analysis by western blot or flow cytometry.
Quantitative Real-time PCR
Total RNA was extracted from hUC-MSCs using Trizol (Sigma, T9424), and reverse transcribed into cDNA using HiScript® II Q RT SuperMix for qRT-PCR (+gDNA wiper) (Vazyme, China). The qRT-PCR assay was performed using ChamQ Universal SYBR qRT-PCR Master Mix (Vazyme, China). All qRT-PCR experiments were independently repeated three times. All primer sequences used for qRT-PCR are listed in Supplementary Table 1.
Flow cytometry
The hUC-MSCs were prepared as single-cell suspensions and stained for 30 min at room temperature. PD-L1-FITC antibody (BD Pharmingen, 558065), IFNGR1-PE antibody (BD Pharmingen, 558937), FITC isotype control antibody (BD Pharmingen, 555742), or PE isotype control antibody (BD Pharmingen, 555749) were used to quantify the expression of PD-L1 or IFNGR1 in hUC-MSCs. CD29-PE antibody (BD Pharmingen, 555443), CD34-PE antibody (BD Pharmingen, 555822), CD44-PE antibody (BD Pharmingen, 555479), CD45-PE antibody (BD Pharmingen, 555483), CD73-PE antibody (BD Pharmingen, 550257), CD90-PE antibody (BD Pharmingen, 555596), and CD105-PE antibody (BD Pharmingen, 560839) were used to identify hUC-MSCs. Our gating strategy was to select active hUC-MSCs groups. Flow cytometry was performed using a NovoCyte flow cytometer (ACEA Biosciences).
Western blot analysis
Western blot assay was performed to observe changes in relative protein content. Whole cell proteins were extracted from cells using radioimmunoprecipitation assay strong lysate (Beyotime Biotechnology, P0013). The cell lysates from each sample were separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis and transferred onto polyvinylidene fluoride (PVDF) membranes. The PVDF membranes were blocked with 5% skim milk in TBST for 60 min, incubated with primary antibodies and then with secondary antibodies conjugated with horseradish peroxidase (HRP), and developed using a chemiluminescence HRP substrate (Millipore, WBKLS0100). The primary antibodies used were PD-L1, IFNGR1, JAK1, p-JAK1, JAK2, p-JAK2, STAT1, p-STAT1, IRF1, IKKα, IKKβ, p-IKKα/β, IKBα, p-IKBα, p65, p-p65, and β-tubulin (1:1000, CST). The secondary antibodies were goat anti-rabbit IgG and goat anti-mouse IgG (1:10000, CST).
Signaling inhibition assay
To investigate the signaling pathways activated by IFN-γ or TNF-α in hUC-MSCs, we used the reagents: Ruxolitinib (10 μM) and BAY11-7082 (10 μM) (Selleckchem). After 30 min of pretreatment with the inhibitors, hUC-MSCs were co-cultured with IFN-γ, TNF-α, or IFN-γ plus TNF-α for 4 h or 24 h. The cells were collected for further investigation. The control cells were treated with these cytokines and DMSO.
Small interfering RNA assay
To identify the key pathway molecules involved in the inducible expression of PD-L1 or IFNGR1, a specific Small interfering RNA (siRNA) assay was performed. The siRNA synthesized by RiboBio Company (Guangzhou, China) have proven effective and were thus used in the siRNA assay (Supplementary Figure 2). The siRNAs were transfected into hUC-MSCs using Lipofectamine RNAiMAX transfection reagent (Life Technologies, United States) according to the manufacturer’s protocol. After 24 h of transfection, the hUC-MSCs were treated with cytokines for 4 h or 24 h. They were then harvested and subjected to qRT-PCR analysis or western blot.
Gene promoter activity assay
Vector plasmids, IRF1 promoter plasmids, p65 promoter plasmids, PD-L1 promoter plasmids, IFNGR1 promoter plasmids, PD-L1 promoter point mutation plasmids, and IFNGR1 promoter point mutation plasmids were purchased from OBiO Technology (Shanghai). 293T cells were cultured in plates and transfected with the plasmids by DNA transfection reagent (NEOFECT, China) according to the manufacturers’ instructions. Fluorescence intensity was determined using a Dual Luciferase Reporter Gene Assay Kit (Beyotime) according to the manufacturer’s instructions.
Cell proliferation assay
Cell proliferation was analyzed using the Cell Counting Kit-8 (CCK-8) assay. The hUC-MSCs were plated in six-well plates (1 × 105 cells per well) and cultured for 24 h. Subsequently, the CCK-8 reagent (Beyotime Biotechnology, China) was added to each well, according to the manufacturer’s instructions. The absorbance of each well at 450 nm was measured using an ELX808 microplate reader (Biotek, United States).
Cell apoptosis assay
Apoptotic hUC-MSCs were detected using the Annexin V-FITC/PI Apoptosis Detection Kit and Annexin V-APC/PI Apoptosis Detection Kit (KeyGEN BioTECH, China). The hUC-MSCs were plated in six-well plates (1 × 105 cells per well) and cultured for the indicated time. After TNF-α stimulation for 24 h, all hUC-MSCs were stained by Annexin V and PI, according to the manufacturer’s instructions. Afterward, the cells were evaluated using the NovoCyte flow cytometer. The percentage of apoptotic hUC-MSCs was determined by the sum of Annexin V positive cells.
IFNGR1 overexpression assay
IFNGR1-overexpressing lentiviruses were purchased from Shanghai OBiO Technology. The lentivirus infection procedures were modified from a previously published protocol[21]. After IFNGR1-overexpressed hUC-MSCs were successfully constructed using IFNGR1-overexpressing lentivirus, we used small interfering RNA (siRNA) to interfere with the p65 expression in cells. PD-L1 mRNA expression was detected by qRT-PCR assays after induction by IFN-γ or TNF-α for 4 h.
PBMCs isolation and proliferation assays
Peripheral blood samples were obtained from healthy donors. Peripheral blood mononuclear cells (PBMCs) were isolated using a human peripheral blood lymphocyte separation tube (Dakewe, China), activated by monoclonal anti-human CD3 antibody (Acro, United States), and stained with 10 mmol/L 5-(and-6)-carboxyfluorescein diacetate succinimidyl ester (CFSE, Beyotime, China). CFSE-labeled PBMCs (1 × 106 cells/well) were co-incubated with hUC-MSCs at a ratio of 10:1 in the presence of 100 IU/mL IL2. After co-culturing for 3 d, the proliferation of PBMCs was analyzed using flow cytometry.
DSS-induced colitis and treatment
C57BL/6J mice were purchased from the Weitong Lihua Experimental Animal Technology Company (China). The animal protocol was designed to minimize pain or discomfort to the animals. The animals were acclimatized to laboratory conditions (23 °C, 12 h/12 h light/dark, 50% humidity, ad libitum access to food and water) for 2 wk prior to experimentation. Mice were randomly assigned to six experimental groups: WT, DSS, DSS + MSCs, DSS + IT-MSCs (IT-MSCs: hUC-MSCs treated with IFN-γ and TNF-α), DSS + IT-MSCs + iso antibody, and IT-MSCs + PD-L1 antibody (atezolizumab, Selleck). In the DSS, DSS + MSCs, DSS + IT-MSCs, DSS + IT-MSCs + iso antibody, and IT-MSCs + PD-L1 antibody groups, acute colitis was induced in mice by the addition of 4% (w/v) DSS (40 kDa, MP Biomedicals) to the drinking water for 7 d, until euthanasia. The WT group received drinking water only. All mice were weighed daily. On day 3, mice from the DSS + MSCs, DSS + IT-MSCs, DSS + IT-MSCs + iso antibody, and IT-MSCs + PD-L1 antibody groups were transfused with 1 × 106 hUC-MSCs via the tail vein, and the other mice were transfused with equal amounts of saline via the tail vein. Mice in the IT-MSCs group were transfused via the tail vein with 1 × 106 hUC-MSCs previously treated with IFN-γ and TNF-α for 24 h. The hUC-MSCs of the DSS + IT-MSCs + iso antibody group and the DSS + IT-MSCs+PD-L1 antibody group were treated with IFN-γ, TNF-α, isotype antibody or PD-L1 antibody for 24 h. After seven days of induction, the mice were sacrificed by cervical dislocation, and their colons were collected.
Colon histopathology analysis
For histological analysis, colon samples were fixed with 4% paraformaldehyde (Beyotime, P0099) for 24 h and embedded in paraffin for hematoxylin and eosin staining, as previously described[22]. We evaluated the histopathological scores of colon tissue using a combination of inflammatory cell infiltration and epithelial damage to the colon[22].
Colon immunohistochemistry analysis
Immunohistochemistry was performed on paraffin embedded sections of colon samples. The sections were incubated with anti-CD4 (Abcam, 1:1000) or anti-CD11b (Abcam, 1:4000) at 4 °C overnight and with anti-rabbit IgG and HRP-linked antibody (CST, 1:50) for 60 min. Immunoreactivity was analyzed with a microscope (Olympus CKX31). The total number of CD4 or CD11b positive cells in each of four nonadjacent fields of view was counted per colon sample.
Myeloperoxidase activity assay
We performed a myeloperoxidase (MPO) activity assay to determine the number of neutrophils in the colon tissue. The MPO activity kit was purchased from Jiancheng (Nanjing, China, A044-1-1). We determined the level of MPO activity in the colon tissue following the protocol recommended by the manufacturer. The absorbance of each well was evaluated using an ELX808 microplate reader.
Enzyme linked immunosorbent assay
The concentrations of TNF-α, IFN-γ, and IL-6 secreted by mice with acute colitis were determined by enzyme linked immunosorbent assay (ELISA). The TNF-α, IFN-γ, and IL-6 ELISA kits were purchased from Boster (Wuhan, Hubei Province, China), and were used according to the manufacturer’s instructions. The absorbance of each well was evaluated using an ELX808 microplate reader.
Statistical analysis
The results are shown as mean ± SD. Statistical analyses were performed using GraphPad Prism v8.4.2 (GraphPad Software Inc., San Diego, CA, United States). Student’s unpaired t-test and one-way analysis of Variance were used to determine significant differences between groups. Statistical significance was set at P < 0.05.
RESULTS
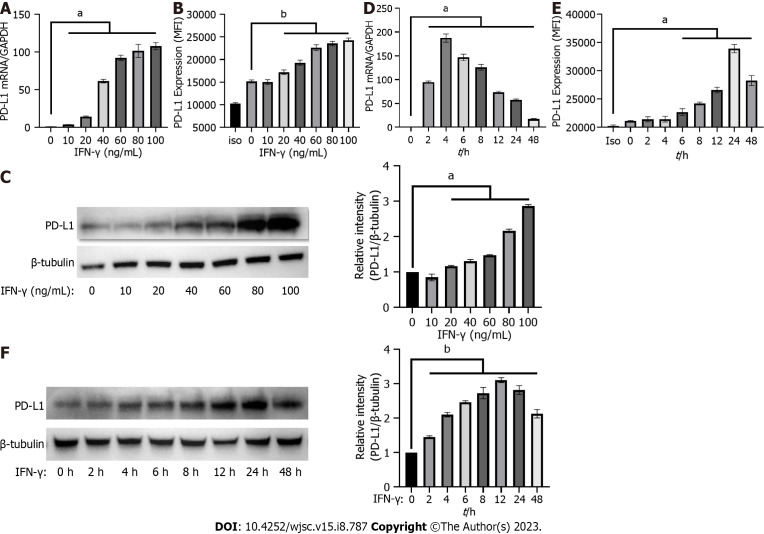
IFN-γ induced the expression of PD-L1 in the hUC-MSCs
IFN-γ induces MSCs to express PD-L1, which exerts an immunosuppressive effect. In the present study, we further investigated the effect of IFN-γ on PD-L1 expression in hUC-MSCs. And hUC-MSCs were treated with either different concentrations of IFN-γ or fixed concentrations of IFN-γ for different time periods. PD-L1 expression in hUC-MSCs was detected using qRT-PCR, western blot, and flow cytometry. After treating hUC-MSCs with variable concentrations of IFN-γ for 24 h, the results showed that when the concentration of IFN-γ was 20 ng/mL, PD-L1 expression increased significantly; it was the highest under 100 ng/mL IFN-γ (Figure 1A-C). Moreover, PD-L1 mRNA expression induced by 20 ng/mL IFN-γ began to increase 2 h after stimulation, and was the highest at 4 h (Figure 1D). The total and membrane protein levels of PD-L1 in hUC-MSCs peaked at 24 h (Figure 1E and F). Based on the results above, we used 20 ng/mL IFN-γ stimulation for 4 h for follow-up qRT-PCR experiments, and 20 ng/mL IFN-γ stimulation for 24 h for western blot or flow cytometry experiments. The results confirmed that IFN-γ induced PD-L1 expression in hUC-MSCs.
Figure 1.
Interferon-gamma induced the expression of programmed cell death protein 1 ligand 1 in human umbilical-cord-mesenchymal stem cells. A-C: Programmed cell death protein 1 ligand 1 (PD-L1) expression was measured by quantitative real-time PCR (qRT-PCR), flow cytometry, and western blot in human umbilical-cord-mesenchymal stem cells (hUC-MSCs) treated with 0, 10, 20, 40, 60, 80 or 100 ng/mL interferon-gamma (IFN-γ) for 24 h; D-F: PD-L1 expression was measured by qRT-PCR, flow cytometry, and western blot in hUC-MSCs treated with 20 ng/mL IFN-γ for 0, 2, 4, 6, 8, 12, 24 or 48 h. Data were represented as mean ± SEM of n = 3. Iso: Isotype; C: Control; aP < 0.01; bP < 0.001. IFN-γ: Interferon-gamma; PD-L1: Programmed cell death protein 1 ligand 1.
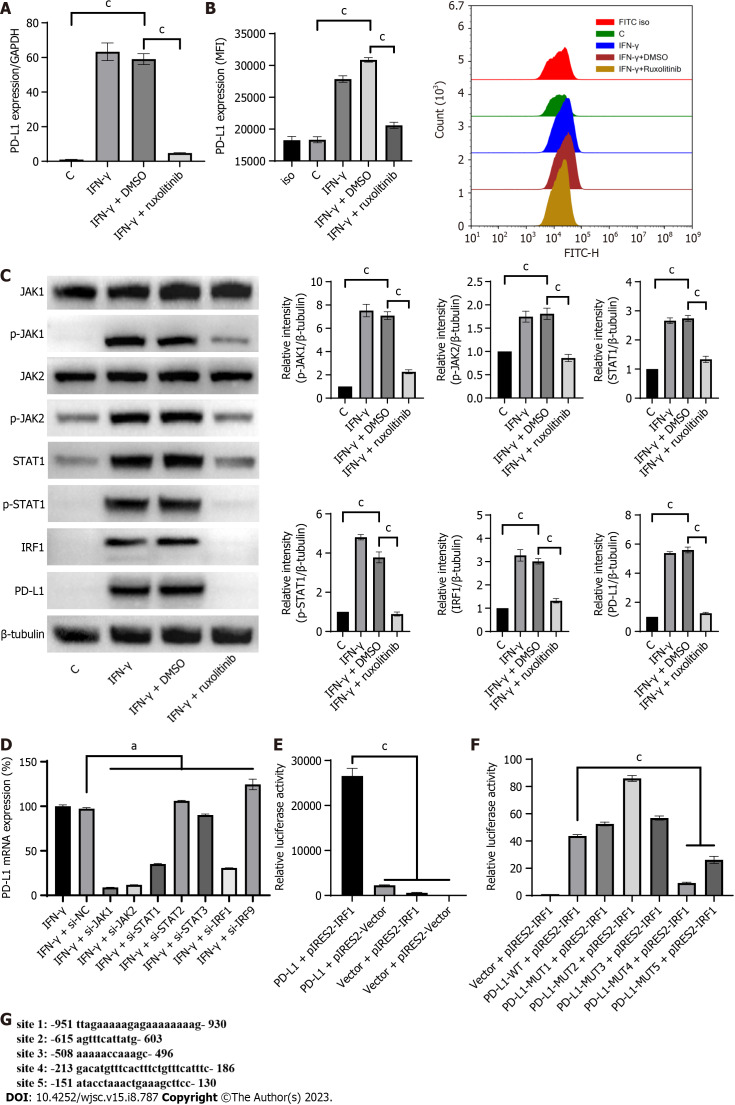
IFN-γ upregulated PD-L1 expression through the JAK/STAT1/IRF1 pathway in hUC-MSCs
A previous study showed that IFN-γ increased PD-L1 expression in tumor cells by activating the JAK/STAT/IRF1 pathway[23]. To confirm this finding, we performed signaling inhibition and siRNA interference experiments. We found that ruxolitinib (10 μM), a JAK/STAT signaling pathway inhibitor, significantly reduced IFN-γ-induced PD-L1 mRNA expression (Figure 2A; Supplementary Figure 3A). The results of western blot and flow cytometry showed that ruxolitinib also significantly reduced the levels of IFN-γ-induced PD-L1 membrane protein and total protein (Figure 2B and C). The results suggest that IFN-γ could induce PD-L1 expression through the JAK/STAT pathway in hUC-MSCs.
Figure 2.
Interferon-gamma upregulated programmed cell death protein 1 ligand 1 expression via the JAK/STAT1/ interferon regulatory factor 1 pathway in human umbilical-cord-mesenchymal stem cells. A: Programmed cell death protein 1 ligand 1 (PD-L1) expression was quantified by quantitative real-time PCR (qRT-PCR) in human umbilical-cord-mesenchymal stem cells (hUC-MSCs) treated with a combination of IFN-γ with or without the JAK inhibitor ruxolitinib (10 µM) for 4 h; B: PD-L1 expression was quantified by flow cytometry in hUC-MSCs treated with a combination of IFN-γ with or without ruxolitinib (10 M) for 24 h; C: Activation of the JAK/STAT/interferon regulatory factor 1 (IRF1) pathway and PD-L1 expression were analyzed by western blot in hUC-MSCs treated with IFN-γ (20 ng/mL) with or without ruxolitinib (10 M) for 24 h; D: The PD-L1 expression was quantified by qRT-PCR in hUC-MSCs transfected with siRNA against JAK1, JAK2, STAT1, STAT2, STAT3, IRF1, or IRF9 and subsequently treated with IFN-γ for 4 h. The expression of PD-L1 in hUC-MSCs of the IFN-γ + si-NC (negative control) group was used as the standard (100%); E: PGL4.10-PD-L1 promoter, pIRES2-IRF1, and Renilla luciferase plasmids were transfected together or separately into 293T cells. Cells were lysed 24 h after transfection and luciferase activity was measured; F: pIRES2-IRF1 plasmid and Renilla luciferase plasmid were transfected into 293T cells with the PGL4.10-PD-L1 promoter plasmid or IRF1 binding site mutant PGL4.10-PD-L1 promoter plasmids. Cells were lysed 24 h after transfection and luciferase activity was measured; G: Predicted binding sites of IRF1 on the PD-L1 promoter. Data were represented as mean ± SEM of n = 3. C: Control; Iso: Isotype; aP < 0.01; cP < 0.0001. IFN-γ: Interferon-gamma; PD-L1: Programmed cell death protein 1 ligand 1.
To further confirm that the JAK/STAT pathway mediates the IFN-γ-induced effect on hUC-MSCs expressing PD-L1, we analyzed the total protein and the phosphorylation levels of key proteins in the JAK/STAT signaling pathway in hUC-MSCs. Western blot results showed that IFN-γ promoted JAK1/2 phosphorylation, STAT1 phosphorylation, IRF1 expression, and PD-L1 expression, while ruxolitinib reversed all these effects (Figure 2C). To confirm the findings, we performed an siRNA interference assay using the effective siRNAs for JAK1/2, STAT1/2/3, and IRF1/9, and observed that the siRNAs remarkably inhibited the PD-L1 expression induced by IFN-γ (Figure 2D). The results indicate that IFN-γ induced PD-L1 expression in hUC-MSCs via the JAK/STAT1/IRF1 pathway.
IRF1 is a key transcription factor in the JAK/STAT pathway. We constructed a dual-luciferase reporter system to confirm that IRF1 binds to the PD-L1 promoter to promote PD-L1 mRNA expression. In 293T cells, relative luciferase activity was weak when transfected with IRF1 or the PD-L1 promoter plasmid; it was the strongest when the two were co-transfected (Figure 2E). We then predicted the potential binding sites of the proximal part of the PD-L1 gene to IRF1 and identified the five most likely binding sites. Point mutant plasmids were constructed at the five binding sites to assess luciferase reporter activity. We co-transfected a WT-PD-L1 promoter plasmid and five IRF1 binding site mutant PD-L1 promoter plasmids into 293T cells with an IRF1 promoter plasmid and a Renilla luciferase plasmid. We measured the relative luciferase activity 24 h after transfection (Figure 2F). The locations of the binding sites in the PD-L1 promoter are shown in Figure 2G. According to the results, mutations at sites 4 or 5 reduced IFN-γ-induced PD-L1 promoter activity, with site 4 having the greatest effect (Figure 2F). These findings indicate that IFN-γ activated the JAK/STAT pathway in hUC-MSCs and induced IRF1 expression; IRF1, in turn, bound to the PD-L1 promoter, thereby promoting PD-L1 transcription.
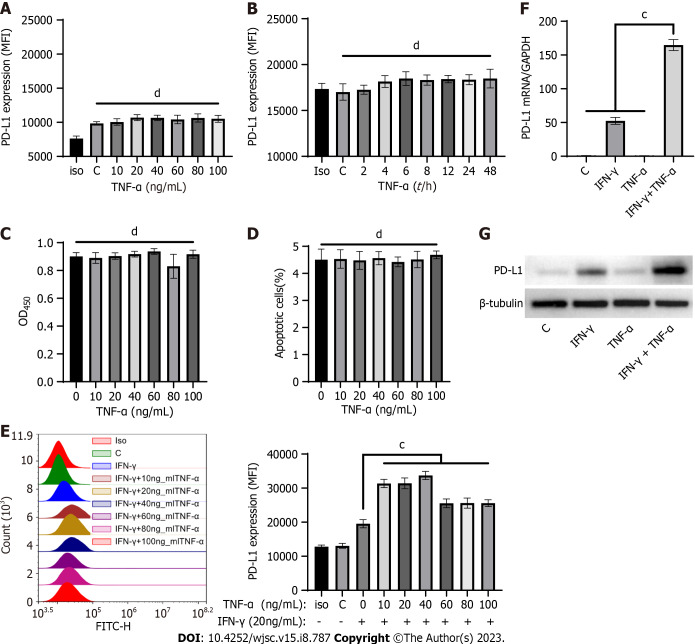
TNF-α synergistically enhanced IFN-γ-induced PD-L1 expression in hUC-MSCs
As mentioned above, the mechanism by which TNF-α synergistically enhances IFN-γ-induced PD-L1 expression has not been elucidated. To study the effect of TNF-α alone or in combination with IFN-γ on PD-L1 expression in hUC-MSCs, we performed the following experiments. First, hUC-MSCs were stimulated with seven different concentrations of TNF-α (0 ng/mL, 10 ng/mL, 20 ng/mL, 40 ng/mL, 60 ng/mL, 80 ng/mL, and 100 ng/mL) for 24 h, or with the experimentally designed highest concentration (100 ng/mL) of TNF-α for different time periods (0 h, 2 h, 4 h, 6 h, 12 h, 24 h, and 48 h). Subsequently, the membrane expression of PD-L1 was detected by flow cytometry. Our results demonstrated that TNF-α stimulation alone did not affect PD-L1 expression in hUC-MSCs (Figure 3A and B).
Figure 3.
Tumor necrosis factor-alpha synergistically enhanced interferon-gamma-induced programmed cell death protein 1 ligand 1 expression in human umbilical-cord-mesenchymal stem cells. A: Programmed cell death protein 1 ligand 1 (PD-L1) expression was measured by flow cytometry in human umbilical-cord-mesenchymal stem cells (hUC-MSCs) treated with 0, 10, 20, 40, 60, 80 or 100 ng/mL tumor necrosis factor-alpha (TNF-α) for 24 h; B: PD-L1 expression was measured by flow cytometry in hUC-MSCs treated with 100 ng/mL TNF-α for 0, 2, 4, 6, 8, 12, 24, or 48 h; C: Proliferation was measured by CCK8 in hUC-MSCs treated with 0, 10, 20, 40, 60, 80 or 100 ng/mL of TNF-α for 24 h; D: Apoptotic hUC-MSCs were measured by flow cytometry in hUC-MSCs treated with 0, 10, 20, 40, 60, 80 or 100 ng/mL TNF-α for 24 h. The histogram shows the quantification results pertaining to the percentage of apoptotic cells (Annexin V+ cells) in each group; E: PD-L1 expression was quantified by flow cytometry in hUC-MSCs after 24 h of incubation with IFN-γ (20 ng/mL) and 0, 10, 20, 40, 60, 80 or 100 ng/mL TNF-α; F: PD-L1 expression was measured by quantitative real-time PCR in hUC-MSCs treated with IFN-γ (20 ng/mL), TNF-α (10 ng/mL), or a combination of IFN-γ (20 ng/mL) and TNF-α (10 ng/mL) for 4 h; G: PD-L1 expression was analyzed by western blot in hUC-MSCs treated with IFN-γ (20 ng/mL), TNF-α (10 ng/mL), or a combination of IFN-γ (20 ng/mL) and TNF-α (10 ng/mL) for 24 h. Data were represented as mean ± SEM of n = 3. C: Control; Iso: Isotype; bP < 0.001; cP < 0.0001; dP > 0.05. IFN-γ: Interferon-gamma; PD-L1: Programmed cell death protein 1 ligand 1; TNF-α: Tumor necrosis factor-alpha.
Subsequently, to analyze the effect of TNF-α on hUC-MSCs viability, the proliferation and apoptosis of hUC-MSCs treated with TNF-α was tested using cell proliferation and apoptosis assays. We found that TNF-α had no effect on the proliferation or apoptosis of hUC-MSCs (Figure 3C and D). We then studied the effect of combined treatment with IFN-γ and TNF-α on PD-L1 expression in hUC-MSCs. We stimulated hUC-MSCs with 20 ng/mL IFN-γ and different concentrations of TNF-α (0 ng/mL, 10 ng/mL, 20 ng/mL, 40 ng/mL, 60 ng/mL, 80 ng/mL, and 100 ng/mL) and detected PD-L1 expression using flow cytometry. The results showed that 10 ng/mL TNF-α enhanced IFN-γ-induced PD-L1 expression significantly; however, the enhanced effect of TNF-α did not appear to be concentration-dependent (Figure 3E). Furthermore, qRT-PCR and western blot results showed that the mRNA and total protein levels of PD-L1 increased significantly when hUC-MSCs were simultaneously stimulated with 20 ng/mL IFN-γ and 10 ng/mL TNF-α when compared with IFN-γ or TNF-α alone (Figure 3F and G). Based on the results, 10 ng/mL TNF-α was used in follow-up experiments. In addition, we investigated the effects of IFN-γ (20 ng/mL) or TNF-α (10 ng/mL) stimulation individually or in combination on the proliferation or apoptosis of hUC-MSCs. Our results showed that the stimuli were unable to exert any effect on apoptosis or proliferation of hUC-MSCs at the current concentrations (Supplementary Figure 3B and C). The findings suggest that TNF-α alone had no effect on PD-L1 expression; however, TNF-α could synergistically increase IFN-γ-induced PD-L1 expression in hUC-MSCs.
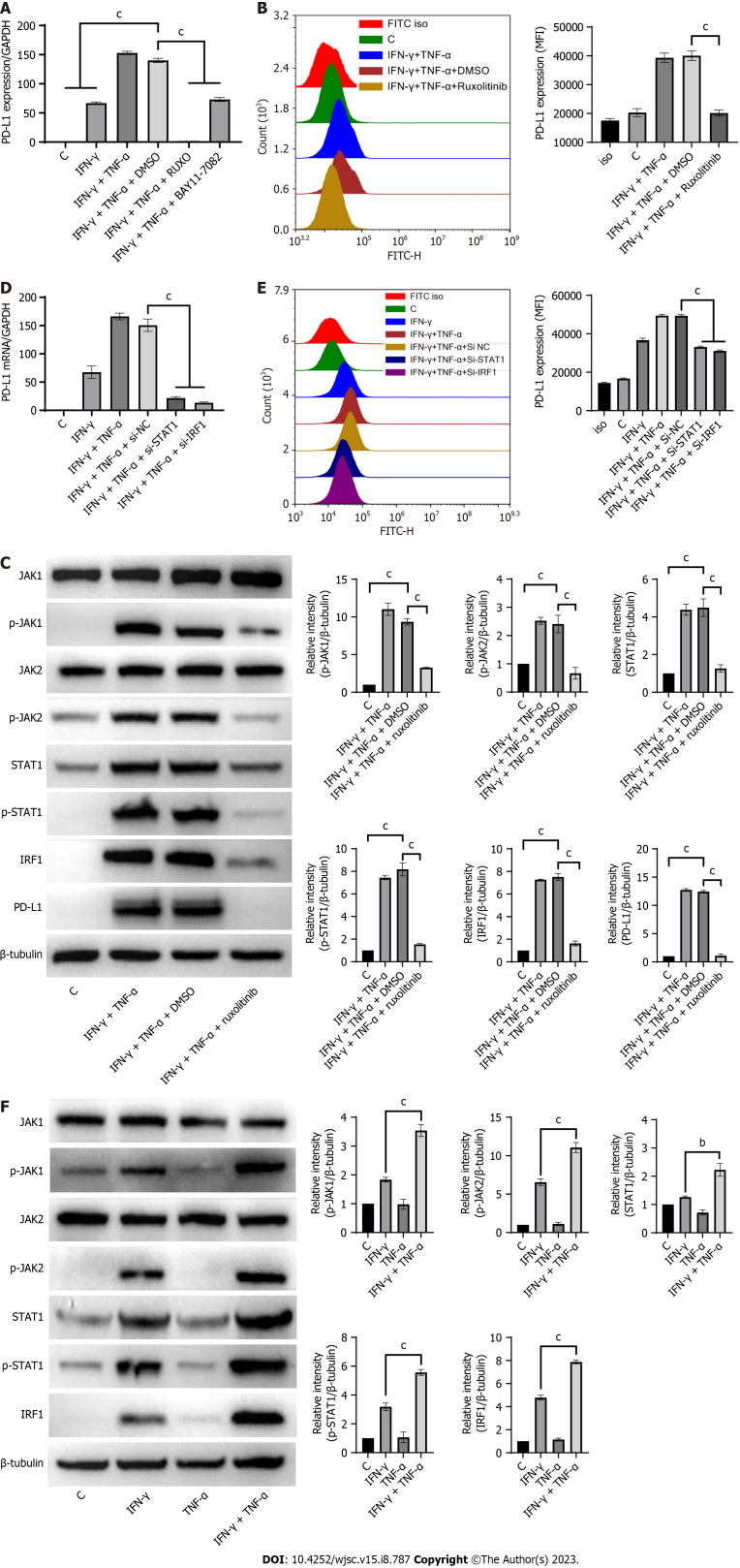
TNF-α improved PD-L1 expression by promoting the activation of JAK/STAT1/IRF1 pathway induced by IFN-γ
As previous studies have demonstrated that IFN-γ induces hUC-MSCs to express PD-L1 through the JAK/STAT1/IRF1 pathway and TNF-α induces various downstream biological effects through activation of the NF-κB pathway[24], we explored the molecular mechanism by which TNF-α enhances IFN-γ-induced PD-L1 expression using signaling inhibition experiments. We treated hUC-MSCs with ruxolitinib and the NF-κB inhibitor BAY11-7082, and then detected PD-L1 mRNA levels after combined treatment with IFN-γ and TNF-α for 4 h. Our results showed that both BAY11-7082 and ruxolitinib inhibited PD-L1 expression induced by a combination of IFN-γ and TNF-α (Figure 4A). Ruxolitinib displayed a stronger inhibitory effect, almost completely inhibiting the induction of PD-L1 mRNA expression, while BAY11-7082 only partially inhibited the expression (Figure 4A). Flow cytometry and western blot assays also showed that ruxolitinib completely inhibited PD-L1 protein expression in hUC-MSCs treated with IFN-γ and TNF-α (Figure 4B and C). Furthermore, we performed an siRNA interference assay using STAT1 siRNA and IRF1 siRNA. The siRNA against STAT1 and IRF1 decreased PD-L1 expression induced by IFN-γ or TNF-α in hUC-MSCs (Figure 4D and E). The results indicated that PD-L1 gene transcription is also induced through the JAK/STAT1/IRF1 pathway when stimulated by IFN-γ and TNF-α.
Figure 4.
Tumor necrosis factor-alpha increased programmed cell death protein 1 ligand expression by promoting interferon-gamma-induced activation of the JAK/STAT1/interferon regulatory factor 1 pathway. A: Programmed cell death protein 1 ligand (PD-L1) expression was quantified by quantitative real-time PCR (qRT-PCR) in human umbilical-cord-mesenchymal stem cells (hUC-MSCs) after 4 h of incubation with IFN-γ and tumor necrosis factor-alpha (TNF-α) in the presence or absence of ruxolitinib (10 μM) or the NF-κB inhibitor BAY11-7082 (10 μM); B: PD-L1 expression in hUC-MSCs was quantified by flow cytometry after 24 h of incubation with IFN-γ and TNF-α in the presence or absence of ruxolitinib (10 μM); C: Activation of the JAK/STAT1/interferon regulatory factor 1 (IRF1) pathway and the expression of PD-L1 were analyzed by western blot in hUC-MSCs after 24 h of incubation with IFN-γ and TNF-α in the presence or absence of ruxolitinib (10 μM); D and E: PD-L1 expression was quantified by quantitative real-time PCR and flow cytometry in hUC-MSCs transfected with siRNA of NC, STAT1, or IRF1 and subsequently treated with IFN-γ and TNF-α for 4 h or 24 h; F: Activation of the JAK/STAT1/IRF1 pathway was analyzed by western blot in hUC-MSCs treated with IFN-γ (20 ng/mL), TNF-α (10 ng/mL), or a combination of IFN-γ (20 ng/mL) and TNF-α (10 ng/mL) for 24 h. Data were represented as mean ± SEM of n = 3. C: Control; Iso: Isotype; cP < 0.0001. IFN-γ: Interferon-gamma; PD-L1: Programmed cell death protein 1 ligand 1; TNF-α: Tumor necrosis factor-alpha.
To investigate whether TNF-α affects the activation of the JAK/STAT1/IRF1 pathway, we analyzed the activation of the JAK/STAT1/IRF1 pathway in hUC-MSCs treated with IFN-γ and TNF-α. The results showed that the activation level of the JAK/STAT1/IRF1 pathway was significantly higher following stimulation with IFN-γ and TNF-α (Figure 4F). Additionally, ruxolitinib significantly reduced the phosphorylation levels of JAK1/2 and STAT1, as well as the expression levels of IRF1 and PD-L1, in hUC-MSCs induced by IFN-γ and TNF-α (Figure 4C). The results revealed that the activation of the JAK/STAT1/IRF1 pathway was significantly stronger when co-stimulated with IFN-γ and TNF-α, thus leading to higher PD-L1 expression.
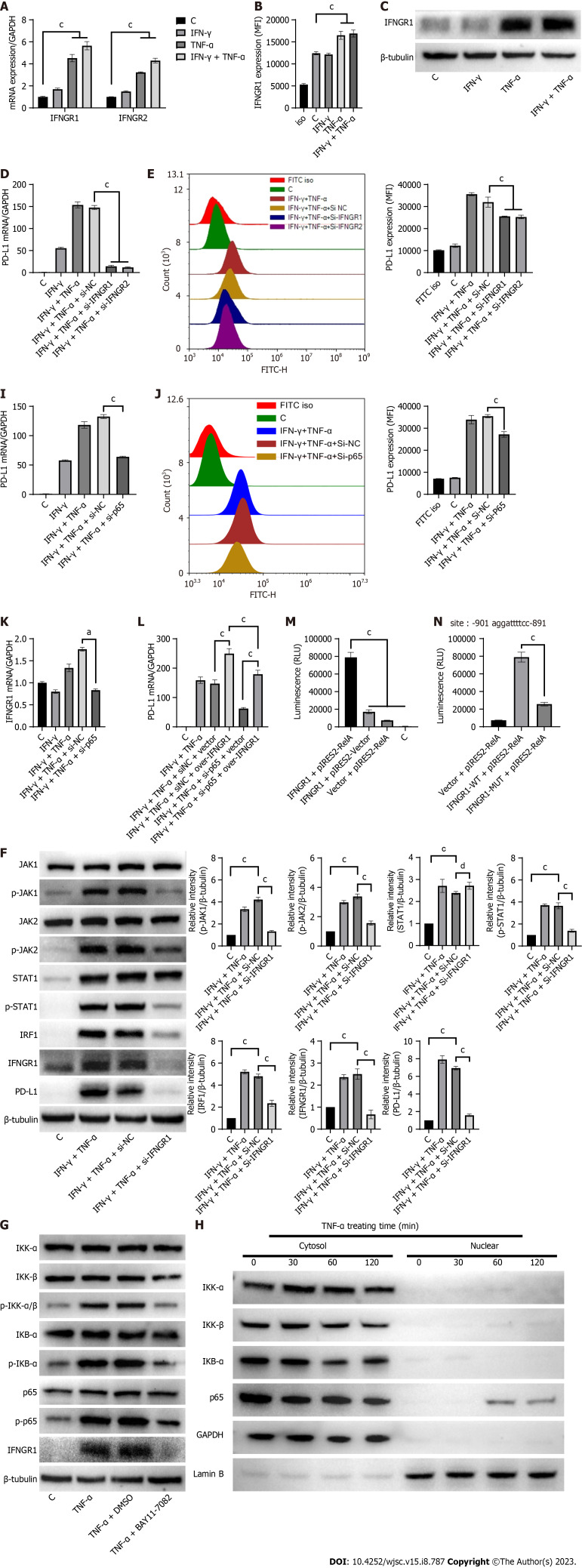
TNF-α synergistically amplified IFN-γ-induced JAK/STAT1/IRF1 signaling activation by upregulating NF-κB-mediated IFNGR1 expression
IFNGR1/2 acts as the membrane receptor of IFN-γ and transmits an activation initiation signal to the JAK/STAT1/IRF1 pathway, which is the key player in PD-L1 expression[23]. We speculated that the higher activation level of the JAK/STAT1/IRF1 pathway might be caused by TNF-α induced IFNGR1/2 expression. As predicted, TNF-α upregulated the expression of IFNGR1 mRNA and protein and the expression of IFNGR2 mRNA (Figure 5A-C). Notably, since no effective anti-IFNGR2 antibody is available, only IFNGR1 expression was detected in western blot experiments. Additionally, the siRNA for IFNGR1/2 decreased PD-L1 mRNA and protein expression in hUC-MSCs induced by IFN-γ and TNF-α (Figure 5D-F). Furthermore, western blot results showed that IFNGR1 siRNA reduced JAK1/2 and STAT1 phosphorylation, as well as IRF1 expression (Figure 5F). The results suggest that TNF-α amplifies the IFN-γ-induced activation of the JAK/STAT1/IRF1 pathway by upregulating IFNGR1/2 expression.
Figure 5.
Tumor necrosis factor-alpha synergistically amplified interferon-gamma-induced JAK/STAT1/interferon regulatory factor 1 signaling activation by upregulating NF-κB-mediated interferon-gamma receptor 1/2 expression. A: The expression of NF-κB-mediated interferon-gamma receptor 1/2 (IFNGR1/2) were quantified by quantitative real-time PCR (qRT-PCR) in human umbilical-cord-mesenchymal stem cells (hUC-MSCs) treated with IFN-γ and tumor necrosis factor-alpha (TNF-α) alone or in combination for 4 h; B and C: IFNGR1 expression was quantified by flow cytometry or WB in hUC-MSCs treated with IFN-γ and TNF-α alone or in combination for 24 h; D and E: PD-L1 expression was quantified by qRT-PCR or flow cytometry in hUC-MSCs transfected with siRNA against NC, IFNGR1, or IFNGR2, and subsequently treated with IFN-γ and TNF-α for 4 h or 24 h; F: Activation of the JAK/STAT1/interferon regulatory factor 1 pathway and the expressions of PD-L1 and IFNGR1 were analyzed by western blot in hUC-MSCs after 24 h of incubation with IFN-γ and TNF-α in the presence or absence of IFNGR1 siRNA; G: Activation of the NF-κB pathway and expression of IFNGR1 were analyzed by western blot in hUC-MSCs after 24 h of incubation with TNF-α in the presence or absence of the NF-KB inhibitor BAY11-7082 (10 μM); H: IKKα, IKKβ, p65 and IκBα protein levels in the cytoplasm and nucleus of hUC-MSCs after TNF-α stimulation were measured through western blot; I: IFNGR1 expression was quantified by qRT-PCR in hUC-MSCs transfected with p65 siRNA and subsequently treated with IFN-γ and TNF-α for 4 h; J and K: PD-L1 expression was quantified by qRT-PCR or flow cytometry in hUC-MSCs transfected with p65 siRNA and subsequently treated with IFN-γ and TNF-α for 4 h or 24 h; L: hUC-MSCs were infected with IFNGR1 overexpressed lentivirus and transfected with siRNA of p65, and induced with IFN-γ and TNF-α for 4 h, and then PD-L1 expression was quantified by qRT-PCR; M: PGL4.10-IFNGR1 promoter plasmid, pIRES2-p65 plasmid, and Renilla luciferase plasmid were transfected together or separately into 293T cells. Cells were lysed 24 h after transfection and luciferase activity was measured; N: pIRES2-p65 plasmid and Renilla luciferase plasmid were transfected into 293T cells with the PGL4.10-IFNGR1 promoter plasmid or the p65 binding site mutant PGL4.10-IFNGR1 promoter plasmid. Cells were lysed 24 h after transfection and luciferase activity was measured. The predicted binding sites of p65 to the IFNGR1 promoter are above the graph. Data were represented as mean ± SEM of n = 3. C: Control; Iso: Isotype; bP < 0.001; cP < 0.0001; dP > 0.05. IFN-γ: Interferon-gamma; PD-L1: Programmed cell death protein 1 ligand 1; TNF-α: Tumor necrosis factor-alpha.
The NF-κB pathway inhibitor BAY11-7082 partially impaired the expression of PD-L1 induced by the combination of IFN-γ and TNF-α (Figure 4A; Supplementary 3D). This suggests that the NF-κB pathway is involved in the regulation of PD-L1 expression induced by IFN-γ and TNF-α. Therefore, we examined the expression of IFNGR1 and the activation of the NF-κB pathway in hUC-MSCs induced by TNF-α. As predicted, TNF-α upregulated IFNGR1 expression by activating the NF-κB pathway, while BAY11-7082 decreased the phosphorylation levels of IKK-α/β, IKB-α, and p65, as well as the expression of IFNGR1 (Figure 5G; Supplementary Figure 4A). To explore NF-κB pathway activation by TNF-α in hUC-MSCs, we assessed nuclear and cytoplasmic p65 and IκB expression after TNF-α treatment. The expression of IκB in the cytoplasm was reduced at 60 min and then restored, while the expression of p65 in the nucleus was significantly increased at 60 min (Figure 5H; Supplementary Figure 4B). These findings indicate that TNF-α can promote NF-κB pathway activation in hUC-MSCs, in addition to enhancing p65 translocation to the nuclei. Moreover, when the expression of p65 was downregulated by siRNA, the effect of TNF-α on the expression of IFNGR1 and PD-L1 induced by IFN-γ was significantly reduced (Figure 5I-K). Importantly, we found that IFNGR1-overexpressing lentivirus restored PD-L1 expression that was reduced by p65 siRNA (Figure 5L). Furthermore, TNF-α upregulated IFNGR1 expression through the NF-κB pathway, and synergistically amplified the activation of JAK/STAT1/IRF1 induced by IFN-γ, finally resulting in an increase in PD-L1 expression in hUC-MSCs.
To confirm that p65 binds to the IFNGR1 promoter to activate IFNGR1 expression, we constructed a luciferase reporter system with NF-κB-driven activity. In 293T cells, higher luciferase activity was observed when p65 and IFNGR1 promoter plasmids were co-transfected into the cells than when these were transfected separately (Figure 5M). As the proximal part of the IFNGR1 gene contained only one p65 binding site, we constructed an IFNGR1 promoter plasmid with a point mutation at this binding site. We found that this p65 binding site mutant plasmid displayed weaker luciferase activity in response to TNF-α stimulation compared to the WT-type IFNGR1 promoter plasmid (Figure 5N). The results indicate that TNF-α induces NF-κB p65 activation of the IFNGR1 promoter.
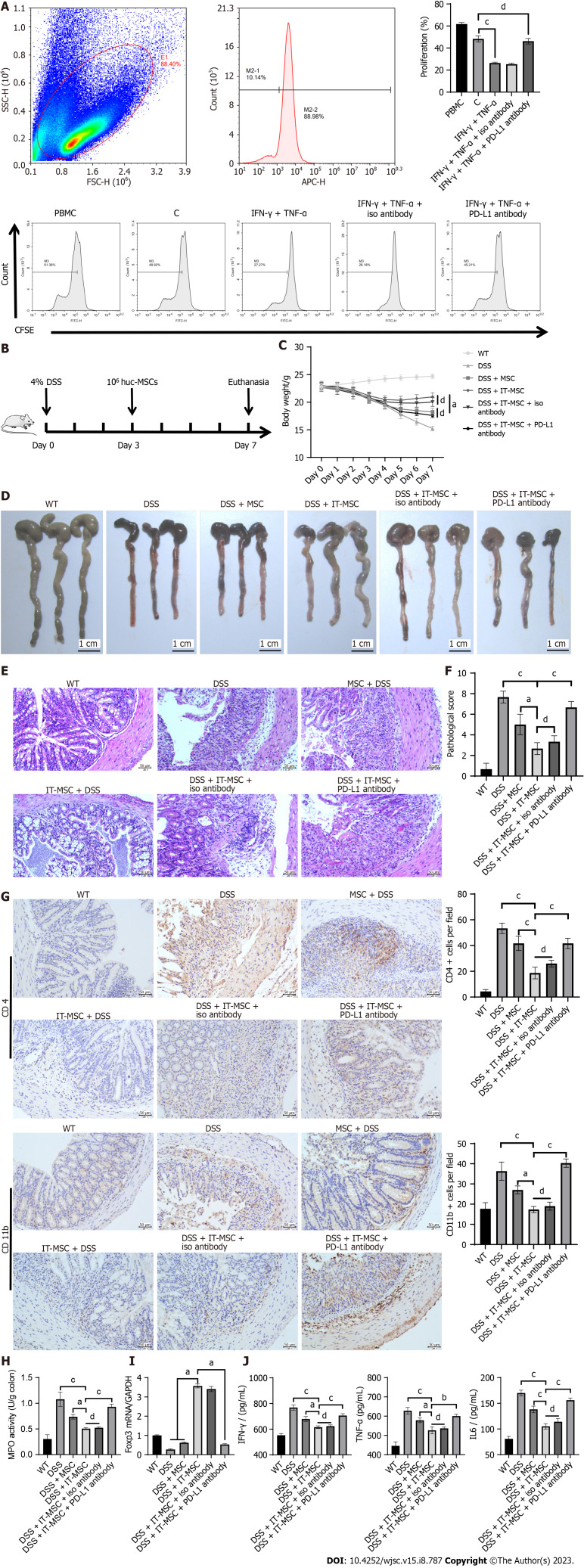
Synergy of IFN-γ and TNF-α enhanced the immunosuppressive capacity of hUC-MSCs by inducing PD-L1 expression
To explore whether the high expression of PD-L1 in hUC-MSCs induced by a combination of IFN-γ and TNF-α could enhance their immunosuppressive function, we first conducted a T lymphocyte proliferation inhibition experiment in vitro. The results showed that PBMCs co-cultured with hUC-MSCs that were pre-treated with IFN-γ and TNF-α had higher CFSE fluorescence intensity than that in other groups, which indicated that IFN-γ- and TNF-α-pretreated hUC-MSCs showed a stronger inhibitory effect on PBMCs proliferation (Figure 6A). Meanwhile, the PD-L1 antibody eliminated the inhibitory effect of hUC-MSCs pre-treated with IFN-γ and TNF-α on PBMCs proliferation (Figure 6A). The results suggest that IFN-γ and TNF-α-pretreated hUC-MSCs, with high PD-L1 expression, exhibited a stronger inhibitory effect on T cell proliferation.
Figure 6.
Synergy by IFN-γ and tumor necrosis factor-alpha enhanced the immunosuppressive capacity of human umbilical-cord-mesenchymal stem cells by inducing programmed cell death protein 1 ligand expression. A: The CFSE fluorescence intensity of CFSE-labeled peripheral blood mononuclear cells (PBMCs) was detected after co-culture with human umbilical-cord-mesenchymal stem cells (hUC-MSCs) with different treatments for 3 d. The CFSE fluorescence intensity of CD3-positive PBMCs on day 0 was used as the reference (1.29%). The histogram shows the quantification results pertaining to the mean fluorescent intensity of CFSE in each group; B: Schematic diagram of dextran sulfate sodium-induced colitis and MSCs transplantation therapy in mice; C: Bodyweight of mice in each group during the disease process (n = 6); D: Macroscopic appearance of the colon in each group; E: Colon sections embedded in paraffin were stained with hematoxylin and eosin for light microscopy assessment. Scale bar, 50 μm; F: Histopathological score of colons from each group was assessed for disease severity (n = 3); G: Infiltration cells expressing CD4 or CD11b in colon tissue sections from each group were analyzed by immunohistochemical staining (n = 3). Scale bar, 50 μm; H: Myeloperoxidase activity in the colon was determined (n = 3); I: The colonic mRNA expression of Treg (Foxp3) from each group were analyzed by quantitative real-time PCR (n = 3); J: Levels of inflammatory factors in colon tissue homogenates from each group were determined using ELISA (n = 3). IT-MSCs refer to hUC-MSCs pretreated with IFN-γ and tumor necrosis factor-alpha for 24 h. C: Control; aP < 0.01; bP < 0.001; cP < 0.0001; dP > 0.05.
We further explored the therapeutic efficacy of hUC-MSCs pre-treated with a combination of IFN-γ and TNF-α in mice with DSS-induced colitis. Colitis was induced in mice by feeding them DSS added to drinking water, and hUC-MSCs were transplanted according to the schematic diagram shown in Figure 6B. Compared with the wild-type hUC-MSCs treatment group, hUC-MSCs pretreated with a combination of IFN-γ and TNF-α displayed a better therapeutic efficacy in DSS-induced mice, including mitigated bodyweight loss (Figure 6C); improved colonic morphology (Figure 6D); relieved colonic ulcer, mucosal edema, epithelial cell injury, and inflammatory cell infiltration (Figure 6E); lower histopathological scoring of colon tissue (Figure 6F); inhibited infiltration of immune cells including CD4+ T cells, CD11b+ macrophages, and neutrophils (lower MPO activity) in colon tissue (Figure 6G and 6H); more Treg (Foxp3+) cells in colon tissue (Figure 6I), and significantly decreased levels of inflammatory factors such as TNF-α, IFN-γ, and IL-6 in colon tissue (Figure 6J). However, PD-L1 antibody treatment significantly inhibited such effects. In addition, no adverse reactions related to hUC-MSCs transplantation were observed. The results suggest that the combination of IFN-γ and TNF-α synergistically enhanced the immunosuppressive capacity of hUC-MSCs by upregulating the expression of PD-L1, yielding a better therapeutic efficacy in DSS-induced mice.
DISCUSSION
MSCs are usually derived from the umbilical cord, bone marrow, and adipose tissue. In the present study, hUC-MSCs were selected based on multiple considerations. First, as a type of medical waste, umbilical cord tissue is easier to obtain with less ethical controversy. A large number of MSCs are easily obtained from umbilical cord tissue by mature isolation methods. Second, hUC-MSCs have greater proliferative capacity and immunomodulatory ability than other types of MSCs[25,26]. Third, the major histocompatibility complex I (MHC-I) expression level and the immunogenicity of hUC-MSCs is lower. Hence, although the biosafety of MSCs has been a matter of great concern, hUC-MSCs have become the main source of cells for mesenchymal stem cell transplantation therapy[27]. Therefore, as hUC-MSCs have greater clinical application potential, they were selected for use in the study. In DSS-induced colitis mice, MSCs not only significantly improved the colonic lesions of mice but also ameliorated the tumorigenesis of colitis[28]. In a clinical trial, researchers followed up 34 patients with ulcerative colitis who received hUC-MSCs for up to two years, and no long-term complications such as malignant tumors and immune rejection were observed during follow-up[29]. Similarly, except for the therapeutic effect of hUC-MSCs on colitis mice, no MSC-related side effects or toxicities were observed in the present study. Overall, MSCs have a high safety profile in the treatment of ulcerative colitis.
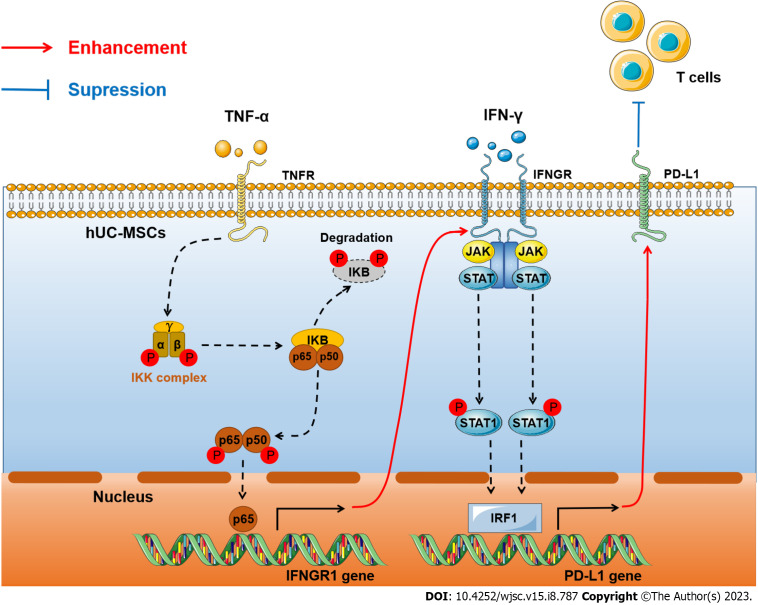
PD-L1 plays an important role in the immunosuppressive capacity of hUC-MSCs. Although the mechanism of PD-L1 expression has been thoroughly elucidated in tumors[30], it remains to be explored in MSCs. The cytokines that induce MSCs to express PD-L1 include IFN-γ, IL25, and IL27, and the relevant pathways are STAT1, JNK/STAT3, and JAK/STAT1[31-33]. We performed this study to investigate the mechanism of PD-L1 expression in MSCs under IFN-γ and TNF-α stimulation and to find a way to enhance the immunosuppressive capacity of MSCs. In the present study, we confirmed that IFN-γ induces PD-L1 expression through the JAK/STAT1/IRF1 pathway in hUC-MSCs. TNF-α upregulates the expression of IFNGR1/2 via the NF-κB pathway, which promotes the activation of the JAK/STAT1/IRF1 pathway induced by IFN-γ, significantly increasing PD-L1 expression. Furthermore, synergistic IFN-γ and TNF-α induction of high PD-L1 expression in hUC-MSCs strongly inhibited T-cell proliferation[33]. In mice with DSS-induced colitis, tail vein infusion of pretreated hUC-MSCs reduced disease activity, colonic tissue damage, cytokine levels, and inflammatory cell infiltration. Thus, combined treatment with IFN-γ and TNF-α synergistically induces high PD-L1 expression in hUC-MSCs, which strengthens the immunosuppressive capacity of hUC-MSCs (Figure 7).
Figure 7.
Molecular mechanism of interferon-gamma and tumor necrosis factor-alpha synergistically upregulated expression of programmed cell death protein 1 ligand in human umbilical-cord-mesenchymal stem cells to inhibit T cells. IFN-γ: Interferon-gamma; PD-L1: Programmed cell death protein 1 ligand 1; TNF-α: Tumor necrosis factor-alpha; hUC-MSCs: Human umbilical-cord-mesenchymal stem cells; IRF1: Interferon regulatory factor 1.
PD-L1 expression has been extensively studied in inflammatory diseases and tumors. In tumor cells, various pathways are involved in IFN-γ-induced PD-L1 expression[30]. For instance, IFN-γ induces PD-L1 expression via the JAK/STAT/IRF1 pathway in tumor cells[34,35]. Similarly, studies have shown that PD-L1 expression in MSCs can be induced by IFN-γ mediated by STAT1. Based on these studies, we speculated that these signals are similar, and that PD-L1 expression induced by IFN-γ in hUC-MSCs might have occurred through the JAK/STAT1/IRF1 pathway. To verify our hypothesis, we conducted signaling pathway inhibitor, RNA interference, and luciferase reporter gene experiments. Our results showed that IFN-γ activates the JAK/STAT1 pathway and promotes IRF1 binding to the PD-L1 promoter, increasing PD-L1 mRNA expression. The results reveal the molecular mechanism by which IFN-γ induces the expression of PD-L1 in hUC-MSCs in detail.
In tumor cells, TNF-α co-stimulation with IL4 or IFN-γ increased PD-L1 expression, and the effect was associated with the NF-κB pathway[20,36]. HCC cells induced by IFN-γ and TNF-α had higher PD-L1 expression than those induced by IFN-γ alone, and had stronger resistance to adaptive immunity[20]. Such findings suggest that TNF-α enhances PD-L1 expression induced by IFN-γ and NF-κB signaling might be involved. In our results, we found that TNF-α significantly increased IFN-γ-induced PD-L1 expression in hUC-MSCs. Importantly, we demonstrated that TNF-α upregulated IFNGR1 expression through the NF-κB pathway, which enhanced IFN-γ/IFNGR/JAK/STAT1/IRF1 signaling axis activation, significantly upregulating PD-L1 expression. In addition, we found that trends of PD-L1 expression in two others common MSCs pretreated with IFN-γ and TNF-α were similar to those of hUC-MSCs (Supplementary Figure 4C). The results suggest that IFN-γ and TNF-α synergistically induce high PD-L1 expression, which may be universally present in MSCs from different sources. Another issue to consider is that IFN-γ or TNF-α may affect cell survival. Therefore, the effect of such cytokines on the proliferation and apoptosis of hUC-MSCs was evaluated. Additionally, the results showed that IFN-γ and TNF-α stimulation alone or in combination had no effect on the proliferation and apoptosis of hUC-MSCs (Figure 3C and D; Supplementary Figure 3B and C).
Ulcerative colitis is an autoimmune disease with complex mechanisms[37]. PD-L1 is involved in the pathogenesis of colitis by targeting T cells[38]. The high PD-L1 expression in colitis regulates cytokine production in colonic dendritic cells, inhibits Th1/Th17 cell activity, and promotes Treg cell proliferation[38-40]. Therefore, DSS-induced colitis models are often used to evaluate the efficacy of drugs and the immunomodulatory ability of MSCs[22,41,42]. We used T-cell proliferation inhibition experiments in vitro to confirm that hUC-MSCs treated with IFN-γ and TNF-α have a stronger immunosuppressive capacity than untreated hUC-MSCs. Furthermore, we evaluated the immunosuppressive capacity of hUC-MSCs treated with IFN-γ and TNF-α in a DSS-induced mouse colitis model and found that they exhibited fewer disease symptoms and less tissue damage, as well as lower inflammatory cell infiltration, lower inflammatory factors, and greater Treg cells recruitment than untreated hUC-MSCs. Moreover, we performed RNA-seq analysis on hUC-MSCs treated with IFN-γ and TNF-α. We found that with a combination of IFN-γ and TNF-α treatment, hUC-MSCs also expressed IDO, TSG-6, and other immunosuppressive molecules (data not shown). The results suggest that hUC-MSCs treated with IFN-γ and TNF-α have a stronger immunomodulatory capacity than untreated hUC-MSCs, perhaps because hUC-MSCs can express PD-L1 as well as other immunosuppressive molecules. This idea is worthy of further investigation.
In recent years, MSCT therapy has been rising in popularity for the treatment of various inflammatory diseases due to the immunosuppressive ability of MSCs. However, due to differences in both the sources of MSCs and the techniques of cell extraction and culture, the efficacy of MSCT in patients is not stable. Based on the present study, it is likely that the abundance of immunosuppressive molecules expressed by MSCs plays an important role. Therefore, this study provides two possible solutions to improve the efficacy of MSCT in diseases. On the one hand, MSCs can express more immunosuppressive molecules (PD-L1) after co-induction with lower concentrations of inflammatory factors (IFN-γ and TNF-α) without impairing cell viability. On the other hand, the efficacy of MSCT can be improved by detecting and screening for MSCs with high expression levels of immunosuppressive molecules before transplantation. In future studies, to compensate for some of the limitations of this study in a translational application, it is necessary to investigate the effect of more combinations of inflammatory factors on PD-L1 expression in MSCs, and also investigate the immunosuppressive molecules induced by other inflammatory factors. More research in this area will contribute to the translational application of MSCT in clinical practice.
CONCLUSION
In the present study, we found that IFN-γ and TNF-α synergistically induce a high level of PD-L1 expression in hUC-MSCs, and we elucidated the molecular mechanism involved. More importantly, both in vitro and in vivo experiments confirmed that INF-γ- and TNF-α-pretreated hUC-MSCs with these high PD-L1 expression levels have strong immunosuppressive capacity and, therefore, have great potential for clinical application in the treatment of autoimmune diseases.
ARTICLE HIGHLIGHTS
Research background
The immunosuppressive capacity of Mesenchymal stem cells (MSCs) is dependent on the “license” of several proinflammatory factors to express immunosuppressive factors such as programmed cell death 1 ligand 1 (PD-L1), which determines the clinical therapeutic efficacy of MSCs for inflammatory or immune diseases. In MSCs, interferon-gamma (IFN-γ) is a key inducer of PD-L1 expression, which is synergistically enhanced by tumor necrosis factor-alpha (TNF-α), but this; however, the mechanism is unclear.
Research motivation
The efficacy of MSCs transplantation (MSCT) is limited by the expression of immunosuppressive molecules of MSCs, including PD-L1. However, the mechanism of IFN-γ alone or in combination with TNF-α inducing MSCs high expression of PD-L1 remains unclear.
Research objectives
To reveal the mechanism of high PD-L1 expression in MSCs pretreated with IFN-γ and TNF-α and explore the application prospects of MSCs with high PD-L1 expression in ulcerative colitis.
Research methods
We assessed PD-L1 expression in human umbilical cord-MSCs (hUC-MSCs) induced by IFN-γ and TNF-α, alone or in combination. Additionally, we performed signaling inhibition and RNA interference experiments to elucidate the specific cross-talk signaling pathways between IFN-γ and TNF-α. Finally, we evaluated the immunosuppressive capacity of hUC-MSCs treated with IFN-γ and TNF-α in an in vitro mixed lymphocyte culture assay, and in vivo in mice with dextran sulfate sodium (DSS)-induced acute colitis.
Research results
Our results showed that IFN-γ upregulated PD-L1 expression in hUC-MSCs to enhance their immunosuppressive activities through the JAK/STAT1/interferon regulatory factor 1 (IRF1) pathway. TNF-α synergistically enhanced IFN-γ-induced PD-L1 expression in hUC-MSCs by upregulating nuclear factor kappa-B (NF-κB)-mediated expression of IFN-γ receptor 1 to activate JAK/STAT1/IRF1 signaling. Furthermore, high PD-L1 expression in hUC-MSCs induced by IFN-γ and TNF-α significantly attenuated DSS-induced acute colitis in mice.
Research conclusions
Our study revealed that IFN-γ and TNF-α synergistically induce the high PD-L1 expression of hUC-MSCs through the JAK/STAT1/IRF1 pathway and the NF-κB pathway, which effectively improves the immunosuppressive capacity of hUC-MSCs.
Research perspectives
The results of the present study could facilitate the optimization of clinical application strategies of MSCT.
Footnotes
Institutional animal care and use committee statement: All procedures involving animals were reviewed and approved by the Institutional Animal Care and Use Committee of the Army Medical University (SYXK2022-0018).
Conflict-of-interest statement: The authors confirm that this article has no conflict of interest to report.
ARRIVE guidelines statement: The authors have read the ARRIVE Guidelines, and the manuscript was prepared and revised according to the ARRIVE Guidelines.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: March 13, 2023
First decision: June 6, 2023
Article in press: July 24, 2023
Specialty type: Cell biology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gallone A, Italy; Maurya DK, India S-Editor: Chen YL L-Editor: A P-Editor: Zhao S
Contributor Information
Zhuo Chen, Department of Stem Cell & Regenerative Medicine, State Key Laboratory of Trauma, Burn and Combined Injury, Daping Hospital, Army Medical University, Chongqing 400042, China; College of Basic Medical Sciences, Army Medical University, Chongqing 400038, China.
Meng-Wei Yao, Department of Stem Cell & Regenerative Medicine, State Key Laboratory of Trauma, Burn and Combined Injury, Daping Hospital, Army Medical University, Chongqing 400042, China.
Zhi-Lin Shen, Department of Stem Cell & Regenerative Medicine, State Key Laboratory of Trauma, Burn and Combined Injury, Daping Hospital, Army Medical University, Chongqing 400042, China.
Shi-Dan Li, Department of Orthopedics, Daping Hospital, Army Medical University, Chongqing 400042, China.
Wei Xing, Department of Stem Cell & Regenerative Medicine, State Key Laboratory of Trauma, Burn and Combined Injury, Daping Hospital, Army Medical University, Chongqing 400042, China.
Wei Guo, Department of Stem Cell & Regenerative Medicine, State Key Laboratory of Trauma, Burn and Combined Injury, Daping Hospital, Army Medical University, Chongqing 400042, China.
Zhan Li, Department of Stem Cell & Regenerative Medicine, State Key Laboratory of Trauma, Burn and Combined Injury, Daping Hospital, Army Medical University, Chongqing 400042, China.
Xiao-Feng Wu, Department of Stem Cell & Regenerative Medicine, State Key Laboratory of Trauma, Burn and Combined Injury, Daping Hospital, Army Medical University, Chongqing 400042, China.
Luo-Quan Ao, Department of Stem Cell & Regenerative Medicine, State Key Laboratory of Trauma, Burn and Combined Injury, Daping Hospital, Army Medical University, Chongqing 400042, China.
Wen-Yong Lu, Department of Hepatobiliary Surgery, The First Affiliated Hospital of Wenzhou Medical University, The South of Shangcai Village, Wenzhou 325005, Zhejiang Province, China.
Qi-Zhou Lian, Department of Medicine, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong 999077, China.
Xiang Xu, Department of Stem Cell & Regenerative Medicine, State Key Laboratory of Trauma, Burn and Combined Injury, Daping Hospital, Army Medical University, Chongqing 400042, China.
Xiang Ao, Department of Stem Cell & Regenerative Medicine, State Key Laboratory of Trauma, Burn and Combined Injury, Daping Hospital, Army Medical University, Chongqing 400042, China; Department of Orthopedics, 953 Hospital of PLA Army, Shigatse Branch of Xinqiao Hospital, Army Medical University, Shigatse 857000, Tibet Autonomous Region, China. ax_syd@163.com.
Data sharing statement
Data sets used or analyzed during the current study can be obtained reasonably request of the corresponding authors.
References
- 1.Lv FJ, Tuan RS, Cheung KM, Leung VY. Concise review: the surface markers and identity of human mesenchymal stem cells. Stem Cells. 2014;32:1408–1419. doi: 10.1002/stem.1681. [DOI] [PubMed] [Google Scholar]
- 2.Nauta AJ, Fibbe WE. Immunomodulatory properties of mesenchymal stromal cells. Blood. 2007;110:3499–3506. doi: 10.1182/blood-2007-02-069716. [DOI] [PubMed] [Google Scholar]
- 3.Ni K, Liu M, Zheng J, Wen L, Chen Q, Xiang Z, Lam KT, Liu Y, Chan GC, Lau YL, Tu W. PD-1/PD-L1 Pathway Mediates the Alleviation of Pulmonary Fibrosis by Human Mesenchymal Stem Cells in Humanized Mice. Am J Respir Cell Mol Biol. 2018;58:684–695. doi: 10.1165/rcmb.2017-0326OC. [DOI] [PubMed] [Google Scholar]
- 4.He X, Yang Y, Yao M, Yang L, Ao L, Hu X, Li Z, Wu X, Tan Y, Xing W, Guo W, Bellanti JA, Zheng SG, Xu X. Combination of human umbilical cord mesenchymal stem (stromal) cell transplantation with IFN-γ treatment synergistically improves the clinical outcomes of patients with rheumatoid arthritis. Ann Rheum Dis. 2020;79:1298–1304. doi: 10.1136/annrheumdis-2020-217798. [DOI] [PubMed] [Google Scholar]
- 5.Taki Z, Gostjeva E, Thilly W, Yaseen B, Lopez H, Mirza M, Hassuji Z, Vigneswaran S, Ahmed Abdi B, Hart A, Arumalla N, Thomas G, Denton CP, Suleman Y, Liu H, Venturini C, O'Reilly S, Xu S, Stratton R. Pathogenic Activation of Mesenchymal Stem Cells Is Induced by the Disease Microenvironment in Systemic Sclerosis. Arthritis Rheumatol. 2020;72:1361–1374. doi: 10.1002/art.41267. [DOI] [PubMed] [Google Scholar]
- 6.Regmi S, Seo Y, Ahn JS, Pathak S, Acharya S, Nguyen TT, Yook S, Sung JH, Park JB, Kim JO, Young CS, Kim HS, Jeong JH. Heterospheroid formation improves therapeutic efficacy of mesenchymal stem cells in murine colitis through immunomodulation and epithelial regeneration. Biomaterials. 2021;271:120752. doi: 10.1016/j.biomaterials.2021.120752. [DOI] [PubMed] [Google Scholar]
- 7.Yang Y, He X, Zhao R, Guo W, Zhu M, Xing W, Jiang D, Liu C, Xu X. Serum IFN-γ levels predict the therapeutic effect of mesenchymal stem cell transplantation in active rheumatoid arthritis. J Transl Med. 2018;16:165. doi: 10.1186/s12967-018-1541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yao M, Chen Z, He X, Long J, Xia X, Li Z, Yang Y, Ao L, Xing W, Lian Q, Liang H, Xu X. Cross talk between glucose metabolism and immunosuppression in IFN-γ-primed mesenchymal stem cells. Life Sci Alliance. 2022;5 doi: 10.26508/lsa.202201493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carvalho AÉS, Sousa MRR, Alencar-Silva T, Carvalho JL, Saldanha-Araujo F. Mesenchymal stem cells immunomodulation: The road to IFN-γ licensing and the path ahead. Cytokine Growth Factor Rev. 2019;47:32–42. doi: 10.1016/j.cytogfr.2019.05.006. [DOI] [PubMed] [Google Scholar]
- 10.Li M, Soder R, Abhyankar S, Abdelhakim H, Braun MW, Trinidad CV, Pathak HB, Pessetto Z, Deighan C, Ganguly S, Dawn B, McGuirk J, Dunavin N, Godwin AK. WJMSC-derived small extracellular vesicle enhance T cell suppression through PD-L1. J Extracell Vesicles. 2021;10:e12067. doi: 10.1002/jev2.12067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu S, Liu F, Zhou Y, Jin B, Sun Q, Guo S. Immunosuppressive Property of MSCs Mediated by Cell Surface Receptors. Front Immunol. 2020;11:1076. doi: 10.3389/fimmu.2020.01076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hudson K, Cross N, Jordan-Mahy N, Leyland R. The Extrinsic and Intrinsic Roles of PD-L1 and Its Receptor PD-1: Implications for Immunotherapy Treatment. Front Immunol. 2020;11:568931. doi: 10.3389/fimmu.2020.568931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sun C, Mezzadra R, Schumacher TN. Regulation and Function of the PD-L1 Checkpoint. Immunity. 2018;48:434–452. doi: 10.1016/j.immuni.2018.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dai S, Jia R, Zhang X, Fang Q, Huang L. The PD-1/PD-Ls pathway and autoimmune diseases. Cell Immunol. 2014;290:72–79. doi: 10.1016/j.cellimm.2014.05.006. [DOI] [PubMed] [Google Scholar]
- 15.Nakamori Y, Park EJ, Shimaoka M. Immune Deregulation in Sepsis and Septic Shock: Reversing Immune Paralysis by Targeting PD-1/PD-L1 Pathway. Front Immunol. 2020;11:624279. doi: 10.3389/fimmu.2020.624279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim JY, Park M, Kim YH, Ryu KH, Lee KH, Cho KA, Woo SY. Tonsil-derived mesenchymal stem cells (T-MSCs) prevent Th17-mediated autoimmune response via regulation of the programmed death-1/programmed death ligand-1 (PD-1/PD-L1) pathway. J Tissue Eng Regen Med. 2018;12:e1022–e1033. doi: 10.1002/term.2423. [DOI] [PubMed] [Google Scholar]
- 17.Mrahleh MA, Matar S, Jafar H, Wehaibi S, Aslam N, Awidi A. Human Wharton's Jelly-Derived Mesenchymal Stromal Cells Primed by Tumor Necrosis Factor-α and Interferon-γ Modulate the Innate and Adaptive Immune Cells of Type 1 Diabetic Patients. Front Immunol. 2021;12:732549. doi: 10.3389/fimmu.2021.732549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guan Q, Li Y, Shpiruk T, Bhagwat S, Wall DA. Inducible indoleamine 2,3-dioxygenase 1 and programmed death ligand 1 expression as the potency marker for mesenchymal stromal cells. Cytotherapy. 2018;20:639–649. doi: 10.1016/j.jcyt.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 19.Su W, Wan Q, Huang J, Han L, Chen X, Chen G, Olsen N, Zheng SG, Liang D. Culture medium from TNF-α-stimulated mesenchymal stem cells attenuates allergic conjunctivitis through multiple antiallergic mechanisms. J Allergy Clin Immunol. 2015;136:423–32.e8. doi: 10.1016/j.jaci.2014.12.1926. [DOI] [PubMed] [Google Scholar]
- 20.Li N, Wang J, Zhang N, Zhuang M, Zong Z, Zou J, Li G, Wang X, Zhou H, Zhang L, Shi Y. Cross-talk between TNF-α and IFN-γ signaling in induction of B7-H1 expression in hepatocellular carcinoma cells. Cancer Immunol Immunother. 2018;67:271–283. doi: 10.1007/s00262-017-2086-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ao X, Yang Y, Li W, Tan Y, Guo W, Ao L, He X, Wu X, Xia J, Xu X, Guo J. Anti-αFR CAR-engineered NK-92 Cells Display Potent Cytotoxicity Against αFR-positive Ovarian Cancer. J Immunother. 2019;42:284–296. doi: 10.1097/CJI.0000000000000286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xu F, Fei Z, Dai H, Xu J, Fan Q, Shen S, Zhang Y, Ma Q, Chu J, Peng F, Zhou F, Liu Z, Wang C. Mesenchymal Stem Cell-Derived Extracellular Vesicles with High PD-L1 Expression for Autoimmune Diseases Treatment. Adv Mater. 2022;34:e2106265. doi: 10.1002/adma.202106265. [DOI] [PubMed] [Google Scholar]
- 23.Garcia-Diaz A, Shin DS, Moreno BH, Saco J, Escuin-Ordinas H, Rodriguez GA, Zaretsky JM, Sun L, Hugo W, Wang X, Parisi G, Saus CP, Torrejon DY, Graeber TG, Comin-Anduix B, Hu-Lieskovan S, Damoiseaux R, Lo RS, Ribas A. Interferon Receptor Signaling Pathways Regulating PD-L1 and PD-L2 Expression. Cell Rep. 2017;19:1189–1201. doi: 10.1016/j.celrep.2017.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hayden MS, Ghosh S. Regulation of NF-κB by TNF family cytokines. Semin Immunol. 2014;26:253–266. doi: 10.1016/j.smim.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shin S, Lee J, Kwon Y, Park KS, Jeong JH, Choi SJ, Bang SI, Chang JW, Lee C. Comparative Proteomic Analysis of the Mesenchymal Stem Cells Secretome from Adipose, Bone Marrow, Placenta and Wharton's Jelly. Int J Mol Sci. 2021;22 doi: 10.3390/ijms22020845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Abbaszadeh H, Ghorbani F, Derakhshani M, Movassaghpour AA, Yousefi M, Talebi M, Shamsasenjan K. Regenerative potential of Wharton's jelly-derived mesenchymal stem cells: A new horizon of stem cell therapy. J Cell Physiol. 2020;235:9230–9240. doi: 10.1002/jcp.29810. [DOI] [PubMed] [Google Scholar]
- 27.Liau LL, Ruszymah BHI, Ng MH, Law JX. Characteristics and clinical applications of Wharton's jelly-derived mesenchymal stromal cells. Curr Res Transl Med. 2020;68:5–16. doi: 10.1016/j.retram.2019.09.001. [DOI] [PubMed] [Google Scholar]
- 28.Kim HS, Shin TH, Lee BC, Yu KR, Seo Y, Lee S, Seo MS, Hong IS, Choi SW, Seo KW, Núñez G, Park JH, Kang KS. Human umbilical cord blood mesenchymal stem cells reduce colitis in mice by activating NOD2 signaling to COX2. Gastroenterology. 2013;145:1392–403.e1. doi: 10.1053/j.gastro.2013.08.033. [DOI] [PubMed] [Google Scholar]
- 29.Hu J, Zhao G, Zhang L, Qiao C, Di A, Gao H, Xu H. Safety and therapeutic effect of mesenchymal stem cell infusion on moderate to severe ulcerative colitis. Exp Ther Med. 2016;12:2983–2989. doi: 10.3892/etm.2016.3724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cha JH, Chan LC, Li CW, Hsu JL, Hung MC. Mechanisms Controlling PD-L1 Expression in Cancer. Mol Cell. 2019;76:359–370. doi: 10.1016/j.molcel.2019.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang WB, Yen ML, Liu KJ, Hsu PJ, Lin MH, Chen PM, Sudhir PR, Chen CH, Sytwu HK, Yen BL. Interleukin-25 Mediates Transcriptional Control of PD-L1 via STAT3 in Multipotent Human Mesenchymal Stromal Cells (hMSCs) to Suppress Th17 Responses. Stem Cell Reports. 2015;5:392–404. doi: 10.1016/j.stemcr.2015.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Xu F, Yi J, Wang Z, Hu Y, Han C, Xue Q, Zhang X, Luan X. IL-27 regulates the adherence, proliferation, and migration of MSCs and enhances their regulatory effects on Th1 and Th2 subset generations. Immunol Res. 2017;65:903–912. doi: 10.1007/s12026-017-8929-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jang IK, Jung HJ, Noh OK, Lee DH, Lee KC, Park JE. B7H1mediated immunosuppressive properties in human mesenchymal stem cells are mediated by STAT1 and not PI3K/Akt signaling. Mol Med Rep. 2018;18:1842–1848. doi: 10.3892/mmr.2018.9102. [DOI] [PubMed] [Google Scholar]
- 34.Bellucci R, Martin A, Bommarito D, Wang K, Hansen SH, Freeman GJ, Ritz J. Interferon-γ-induced activation of JAK1 and JAK2 suppresses tumor cell susceptibility to NK cells through upregulation of PD-L1 expression. Oncoimmunology. 2015;4:e1008824. doi: 10.1080/2162402X.2015.1008824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mimura K, Teh JL, Okayama H, Shiraishi K, Kua LF, Koh V, Smoot DT, Ashktorab H, Oike T, Suzuki Y, Fazreen Z, Asuncion BR, Shabbir A, Yong WP, So J, Soong R, Kono K. PD-L1 expression is mainly regulated by interferon gamma associated with JAK-STAT pathway in gastric cancer. Cancer Sci. 2018;109:43–53. doi: 10.1111/cas.13424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Quandt D, Jasinski-Bergner S, Müller U, Schulze B, Seliger B. Synergistic effects of IL-4 and TNFα on the induction of B7-H1 in renal cell carcinoma cells inhibiting allogeneic T cell proliferation. J Transl Med. 2014;12:151. doi: 10.1186/1479-5876-12-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kobayashi T, Siegmund B, Le Berre C, Wei SC, Ferrante M, Shen B, Bernstein CN, Danese S, Peyrin-Biroulet L, Hibi T. Ulcerative colitis. Nat Rev Dis Primers. 2020;6:74. doi: 10.1038/s41572-020-0205-x. [DOI] [PubMed] [Google Scholar]
- 38.Song MY, Hong CP, Park SJ, Kim JH, Yang BG, Park Y, Kim SW, Kim KS, Lee JY, Lee SW, Jang MH, Sung YC. Protective effects of Fc-fused PD-L1 on two different animal models of colitis. Gut. 2015;64:260–271. doi: 10.1136/gutjnl-2014-307311. [DOI] [PubMed] [Google Scholar]
- 39.Beswick EJ, Grim C, Singh A, Aguirre JE, Tafoya M, Qiu S, Rogler G, McKee R, Samedi V, Ma TY, Reyes VE, Powell DW, Pinchuk IV. Expression of Programmed Death-Ligand 1 by Human Colonic CD90(+) Stromal Cells Differs Between Ulcerative Colitis and Crohn's Disease and Determines Their Capacity to Suppress Th1 Cells. Front Immunol. 2018;9:1125. doi: 10.3389/fimmu.2018.01125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moreira TG, Mangani D, Cox LM, Leibowitz J, Lobo ELC, Oliveira MA, Gauthier CD, Nakagaki BN, Willocq V, Song A, Guo L, Lima DCA, Murugaiyan G, Butovsky O, Gabriely G, Anderson AC, Rezende RM, Faria AMC, Weiner HL. PD-L1(+) and XCR1(+) dendritic cells are region-specific regulators of gut homeostasis. Nat Commun. 2021;12:4907. doi: 10.1038/s41467-021-25115-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.DA Costa Gonçalves F, Serafini MA, Mello HF, Pfaffenseller B, Araújo AB, Visioli F, Paz AH. Bioactive factors secreted from mesenchymal stromal cells protect the intestines from experimental colitis in a three-dimensional culture. Cytotherapy. 2018;20:1459–1471. doi: 10.1016/j.jcyt.2018.06.007. [DOI] [PubMed] [Google Scholar]
- 42.Bilsborough J, Fiorino MF, Henkle BW. Select animal models of colitis and their value in predicting clinical efficacy of biological therapies in ulcerative colitis. Expert Opin Drug Discov. 2021;16:567–577. doi: 10.1080/17460441.2021.1851185. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sets used or analyzed during the current study can be obtained reasonably request of the corresponding authors.