Abstract
Background:
Approximately 8% of elementary school-aged children in the United States have food allergies, a complicated health management situation that requires parents to use many types of health literacy, empowerment, and advocacy skills to work with school staff to protect their children.
Objective:
This cross-sectional study examined (a) whether the highest versus lowest levels of functional, communicative, and critical health literacy are associated with higher perceived effectiveness of parental advocacy behaviors for safe food allergy management in schools [parental advocacy]; and (b) whether communicative and critical health literacy are more strongly associated with parental advocacy than functional health literacy.
Methods:
A sample of parents of elementary school-aged children was recruited through 26 food allergy organizations and a research patient registry. Participants completed an anonymous online survey. Self-reported measurements of parental health literacy, empowerment, and advocacy were adapted and refined through pre-testing and pilot-testing. General linear model analyses were conducted to predict parental advocacy.
Key Results:
Participants (N = 313) were predominantly White, college-educated mothers with moderately high levels of food allergy knowledge, health literacy, empowerment, and parental advocacy skills. Parents who scored at the highest levels in the three dimensions of health literacy reported they engaged in more effective advocacy behaviors than parents who scored at the lowest levels. Parental advocacy was predicted largely by parental empowerment and the quality of the relationship with the school (B = .41 and B = .40, respectively). Functional health literacy and the child's diagnosis of asthma were smaller predictors. While accounting for covariates, functional health literacy was significantly associated with parental advocacy whereas communicative and critical health literacy were not.
Conclusions:
Interventions to impact parental empowerment and parent-school relationships, including a health-literate universal precautions approach of communicating food allergy school policies, may influence parental advocacy for food allergy safety in schools. Further research could use a performance-based multidimensional measure of health literacy. [HLRP: Health Literacy Research and Practice. 2023;7(3):e165–e175.]
Plain Language Summary:
This online survey of parents of school-aged children in the U.S. examined health literacy predictors of effective parental advocacy behaviors for safe food allergy management in elementary schools. The results suggest that the parents' quality of their relationship with the school, parental empowerment, functional health literacy, and the child's diagnosis of asthma were associated with parents' reports of effective advocacy for food allergy safety, but communicative and critical health literacy were not.
Parents of elementary school-aged children with food allergies need a sufficient level and variety of health literacy skills to work with school staff to safely manage food allergies. Parental health literacy is the degree to which people can obtain, communicate, appraise, and understand health information and services to make informed and shared health decisions for themselves and others (an adapted definition) (Patient Protection and Affordable Care Act, 2010; Koo, 2021; von Wagner et al., 2009). The range of health literacy skills is grouped into three dimensions: functional, communicative (interactive), and critical health literacy (Nutbeam, 2000). Functional health literacy skills (reading, writing, numeracy) are important contributors toward parental knowledge to manage a child's health condition (DeWalt & Hink, 2009; Riemann et al., 2021). Evidence is inconclusive related to the association between parental health literacy and parental health behaviors or child health outcomes (DeWalt & Hink, 2009; Riemann et al., 2021). Furthermore, there is mixed evidence about the role of communicative health literacy skills (speaking, listening, interpersonal skills) and critical health literacy (synthesis and appraisal of health information for situational application) in chronic disease management (Lai et al., 2013; Londoño & Schulz, 2015; Náfrádi et al., 2016; Qiu et al., 2020; Wang et al., 2016). Limited evidence supports a paradox that high parental communicative and critical health literacy is associated with lower childhood vaccination compliance (Amit Aharon et al., 2017) and worse asthma symptoms (Ogasawara & Hashimoto, 2020). Specific to food allergies, caregivers' low health literacy, as measured by the Newest Vital Sign, may be associated with treatment knowledge gaps, failure to carry and correctly use an epinephrine autoinjector, and an increased number of allergic reactions (Egan et al., 2019).
In addition to health literacy, some psychosocial variables, such as empowerment and self-efficacy, are considered important factors in the relationships between health literacy and health behaviors or health outcomes in several health literacy frameworks (Cudjoe et al., 2020; Paasche-Orlow & Wolf, 2007; Sørensen et al., 2012; von Wagner et al., 2009). An important parental health behavior to consider in the context of food allergy management in schools is their advocacy to prevent allergen exposure and to recognize and treat an allergic reaction quickly. In some districts, parents are the champions who promote implementation of food allergy guidelines in local schools (Lawlis et al., 2017).
Food allergies in schools are a useful topic to examine parental health literacy because of the health literacy challenges posed by understanding and implementing complex school management guidelines (Centers for Disease Control and Prevention [CDC], 2013; Waserman et al., 2021). The complexity of recommendations is challenging because of numerous methods to prevent exposures (CDC, 2013); difficulties with identifying an anaphylactic reaction (Lieberman et al., 2015); and barriers to rapid emergency response with epinephrine (Kao et al., 2018; Szychlinski et al., 2015). Emergency response must be quick because anaphylaxis poses a risk of severe impairment or death (Lieberman et al., 2015). Approximately 8% of children have the potential for food-related anaphylaxis (Gupta et al., 2018).
This cross-sectional study informs the gap in our understanding about parental functional, communicative, and critical health literacy in a specific context: food allergy management in elementary schools (Koo, 2021). The study tested the following hypotheses (a) three parallel hypotheses that parents who score at the highest levels on measures of functional, communicative, and critical health literacy report higher perceived effectiveness of advocacy behaviors for food allergy safety in schools [parental advocacy] than parents who score at the lowest levels and (b) communicative and critical health literacy are more strongly associated with parental advocacy than functional health literacy. The results highlight the importance of functional health literacy, empowerment, and the quality of primary caregivers' relationships with schools as potential areas for intervention.
Methods
Participants
Parents of children with food allergies were recruited through 26 food allergy organizations and one patient registry from November 2020 through February 2021 to participate in an online survey hosted on Qualtrics (version November 2020) (Koo, 2021). Through the groups, recruitment ads were emailed, posted in closed private social media groups, a blog, and a print magazine. Participants were included if they self-reported that they were parents, guardians, or primary caregivers of elementary school-aged children with life-threatening food allergies whose diagnosis was confirmed by a health care provider. The child must have attended kindergarten through 6th grade in-person in the United States at any time during the prior 12 months. The parent had to speak English, be older than age 18 years, and have internet access with any device. Exclusion criteria included prior participation in this or the pilot study. A small electronic gift card incentive was offered to every participant. Data were anonymized. Missing data were minimized through reminder pop-ups. Survey responses were evaluated for exclusion from analyses according to pre-set quality control criteria for highly suspicious, low-quality data (Kramer et al., 2014).
Measures
Development of measures. Measures of parental health literacy, empowerment, and advocacy were adapted for the context of parental perspectives about food allergy management in elementary school (Koo, 2021). Measures were revised after cognitive interviewing with six experts (with content validity index = 1.0 in three iterative rounds of revisions). Next, a pilot test with a convenience sample (N = 33) provided feedback about survey feasibility and scales' test/re-test reliability, criterion-related validity, and convergent validity. This led to further refinement of survey flow, items, and measures. Scale scores were the average of item responses, with possible ranges from 1 to 5. Higher scores indicated higher levels of self-reported parental health literacy, parental empowerment, and parental advocacy.
Parental health literacy. The parental health literacy scale measures the degree of self-reported difficulty with health literacy tasks, adapted from the Functional, Communicative and Critical Health Literacy Scale (FCCHLS) with permission (Ishikawa et al., 2008). The FCCHLS was selected because some evidence suggests that communicative and critical health literacy may be more strongly associated with adult chronic disease management behaviors and outcomes than functional health literacy (Heijmans et al., 2015; Lai et al., 2013). The adapted scale consists of 12 items with five response options (from very difficult to very easy). In this study sample, the parental health literacy scale and three subscales demonstrated good internal consistency (Cronbach's alpha range = .85 to .92). The continuous forms of the health literacy variable and subscales were used for correlations and the two-step regression. To test three parallel hypotheses about highest versus lowest scorers, cut points for dichotomous health literacy variables were created by examining their distributions and Receiver Operating Characteristics to predict a correlated variable according to methods in the literature (Chou et al., 2020). In this highly educated sample, the lowest scores do not imply low or inadequate health literacy, but rather are distinguished from highest scores by dichotomizing.
Parental empowerment. The parental empowerment scale measures the self-reported degree of agreement with empowered statements related to food allergy management. It was adapted from the Health Empowerment Scale with permission (Londoño & Schulz, 2015) to include food allergy ideas from Warren et al. (2015). The scale contains nine items, with five response options (from strongly disagree to strongly agree), comprising three subconstructs (meaning, competence, and impact). Internal consistency was adequate (α = .77).
Parental advocacy. Based on the literature (Burke et al., 2016; Burke & Sandman, 2017; Cawthon & Caemmerer, 2014; Malec et al., 2010; Wright & Taylor, 2014), the parental advocacy scale is new and measures the parents' perceived effectiveness of advocacy behaviors for safe food allergy management at school. It is composed of 13 items with five response options (from not successful to completely successful) that contain three subconstructs (educating others, requesting safety practices, and communicating with school staff). Reliability was very good (α = .93).
Covariates included participant demographics, characteristics of the youngest child in elementary school with food allergies, child's diagnosis of asthma (0 = no, 1 = yes), school characteristics, and quality of the relationship with the school (rating of their relationship with the elementary school with five response options from poor to excellent). Lastly, the food allergies quality of life – parental burden (FAQOL-PB) (Cohen, 2004) was adapted to include five response options instead of seven with permission from the current owner (FARE [Food Allergy Research and Education]). Data from four essay items about experiences related to advocating for food allergy safety in schools will be reported separately.
Statistical Analyses and Power
Statistical analyses were conducted using SPSS (version 27). Pearson's r correlations and independent t-tests examined bivariate associations. Based on the hypotheses, three analysis of covariance tests (ANCOVA) were conducted to predict mean differences in parental advocacy for lowest versus highest scorers on the three health literacy measures while controlling for covariates, ‘quality of the relationship with the school’ and FAQOL-PB. A two-step hierarchical linear regression to predict parental advocacy was conducted with three health literacy subscale measures (in continuous form) while controlling for parental empowerment, quality of the relationship with the school, and asthma. Statistical significance was set to alpha less than .05. Post-hoc power analyses conducted with SPSS and GPower 3.1.9.4 (Faul et al., 2009) demonstrated acceptable power achieved (range 83% to 99%, N = 306–311).
Ethical Considerations
The University of Maryland College Park granted primary Institutional Review Board (IRB) approval and the University of Maryland Baltimore granted secondary IRB approval for human participants research (Koo, 2021).
Results
Participant Recruitment and Participation
Three hundred forty participants consented and started the survey (Koo, 2021). Twenty-four responses were excluded due to completing less than 50% of the survey. Of the remaining 317 responses, four responses were excluded according to pre-set quality criteria. Median survey completion time was 20 minutes. The estimated ad viewership was 8,200 persons, based on a subset of food allergy organizations' private social media groups' viewership and email open rates.
Participant Characteristics
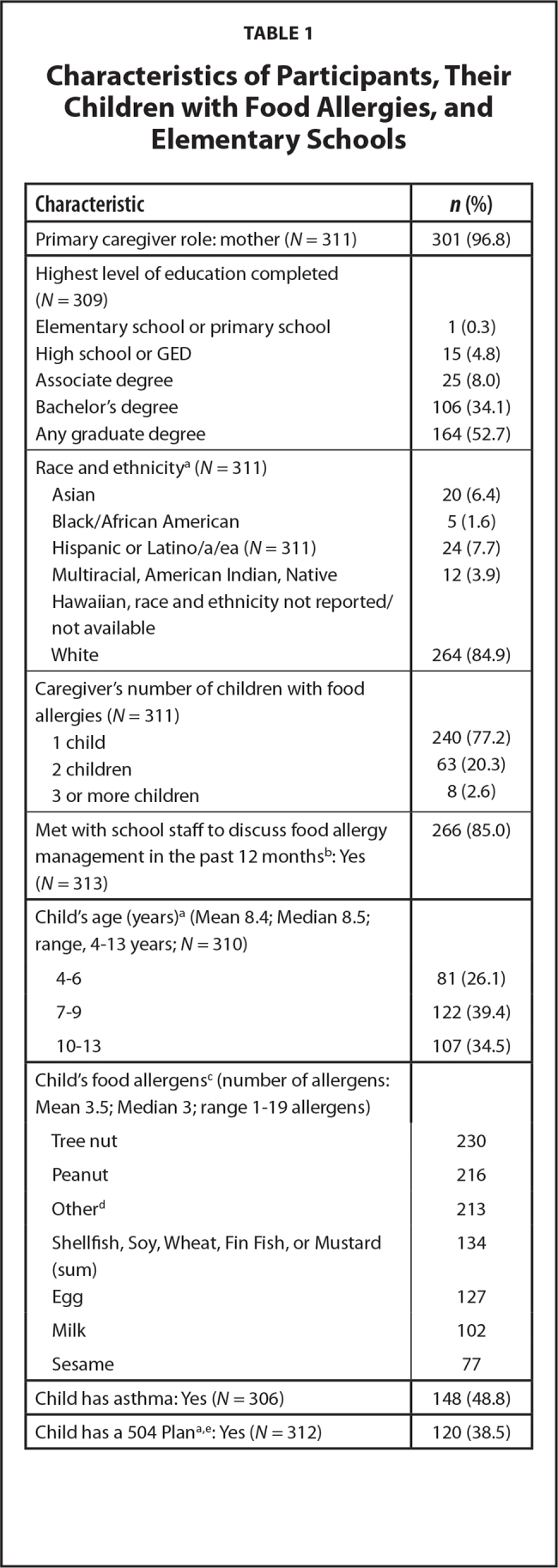
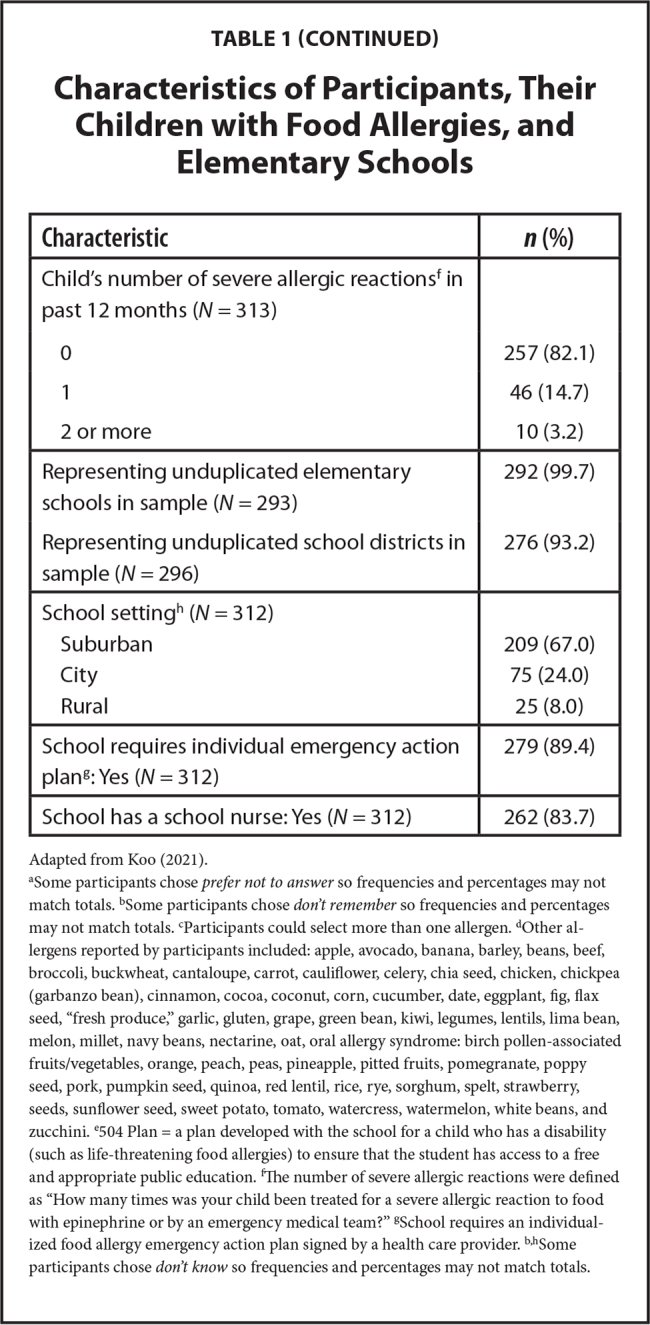
The participants were predominantly White, college-educated mothers (N = 313; Table 1). The participants reported that their youngest child in elementary school with food allergies was allergic to a median of three allergens (range, 1–19). The most frequently reported allergens were tree nuts, peanuts, and others not listed among the top 10 allergens. Nearly one-half of the children had asthma (48.8%). Participants represented 292 different schools and 276 different school districts in the U.S. Nearly 90% of schools required an emergency action plan for their child and 84% had a school nurse.
Table 1.
Characteristics of Participants, Their Children with Food Allergies, and Elementary Schools
| Characteristic | n (%) |
|---|---|
|
| |
| Primary caregiver role: mother (N = 311) | 301 (96.8) |
|
| |
| Highest level of education completed (N = 309) | |
| Elementary school or primary school | 1 (0.3) |
| High school or GED | 15 (4.8) |
| Associate degree | 25 (8.0) |
| Bachelor's degree | 106 (34.1) |
| Any graduate degree | 164 (52.7) |
|
| |
| Race and ethnicitya (N = 311) | |
| Asian | 20 (6.4) |
| Black/African American | 5 (1.6) |
| Hispanic or Latino/a/ea (N = 311) | 24 (7.7) |
| Multiracial, American Indian, Native | 12 (3.9) |
| Hawaiian, race and ethnicity not reported/not available | |
| White | 264 (84.9) |
|
| |
| Caregiver's number of children with food allergies (N = 311) | |
| 1 child | 240 (77.2) |
| 2 children | 63 (20.3) |
| 3 or more children | 8 (2.6) |
|
| |
| Met with school staff to discuss food allergy management in the past 12 monthsb: Yes (N = 313) | 266 (85.0) |
|
| |
| Child's age (years)a (Mean 8.4; Median 8.5; range, 4–13 years; N = 310) | |
| 4–6 | 81 (26.1) |
| 7–9 | 122 (39.4) |
| 10–13 | 107 (34.5) |
|
| |
| Child's food allergensc (number of allergens: Mean 3.5; Median 3; range 1–19 allergens) | |
| Tree nut | 230 |
| Peanut | 216 |
| Otherd | 213 |
| Shellfish, Soy, Wheat, Fin Fish, or Mustard (sum) | 134 |
| Egg | 127 |
| Milk | 102 |
| Sesame | 77 |
|
| |
| Child has asthma: Yes (N = 306) | 148 (48.8) |
|
| |
| Child has a 504 Plana,e: Yes (N = 312) | 120 (38.5) |
| Characteristic | n (%) |
|---|---|
|
| |
| Child's number of severe allergic reactionsf in past 12 months (N = 313) | |
| 0 | 257 (82.1) |
| 1 | 46 (14.7) |
| 2 or more | 10 (3.2) |
|
| |
| Representing unduplicated elementary schools in sample (N = 293) | 292 (99.7) |
| Representing unduplicated school districts in sample (N = 296) | 276 (93.2) |
|
| |
| School settingh (N = 312) | |
| Suburban | 209 (67.0) |
| City | 75 (24.0) |
| Rural | 25 (8.0) |
|
| |
| School requires individual emergency action plang: Yes (N = 312) | 279 (89.4) |
|
| |
| School has a school nurse: Yes (N = 312) | 262 (83.7) |
Adapted from Koo (2021).
Some participants chose prefer not to answer so frequencies and percentages may not match totals.
Some participants chose don't remember so frequencies and percentages may not match totals.
Participants could select more than one allergen.
Other allergens reported by participants included: apple, avocado, banana, barley, beans, beef, broccoli, buckwheat, cantaloupe, carrot, cauliflower, celery, chia seed, chicken, chickpea (garbanzo bean), cinnamon, cocoa, coconut, corn, cucumber, date, eggplant, fig, flax seed, “fresh produce,” garlic, gluten, grape, green bean, kiwi, legumes, lentils, lima bean, melon, millet, navy beans, nectarine, oat, oral allergy syndrome: birch pollen-associated fruits/vegetables, orange, peach, peas, pineapple, pitted fruits, pomegranate, poppy seed, pork, pumpkin seed, quinoa, red lentil, rice, rye, sorghum, spelt, strawberry, seeds, sunflower seed, sweet potato, tomato, watercress, watermelon, white beans, and zucchini.
504 Plan = a plan developed with the school for a child who has a disability (such as life-threatening food allergies) to ensure that the student has access to a free and appropriate public education.
The number of severe allergic reactions were defined as “How many times was your child been treated for a severe allergic reaction to food with epinephrine or by an emergency medical team?”
School requires an individualized food allergy emergency action plan signed by a health care provider.
Some participants chose don't know so frequencies and percentages may not match totals.
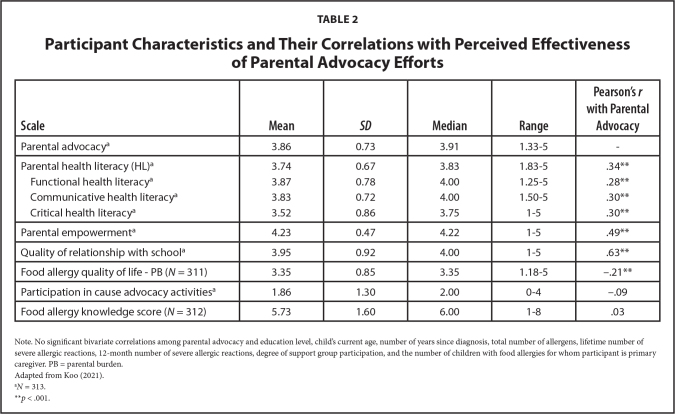
Participants reported moderately high levels of parental health literacy, parental empowerment, and parental advocacy (Table 2). Ceiling effects were noted for the functional health literacy measure but not for the other major variables. Most participants (71.8%) reported above average or excellent relationships with their schools. Parents had moderately high levels of food allergy knowledge and their FAQOL-PB was somewhat low.
Table 2.
Participant Characteristics and Their Correlations with Perceived Effectiveness of Parental Advocacy Efforts
| Scale | Mean | SD | Median | Range | Pearson's r with Parental Advocacy |
|---|---|---|---|---|---|
|
| |||||
| Parental advocacya | 3.86 | 0.73 | 3.91 | 1.33–5 | - |
|
| |||||
| Parental health literacy (HL)a | 3.74 | 0.67 | 3.83 | 1.83–5 | .34** |
| Functional health literacya | 3.87 | 0.78 | 4.00 | 1.25–5 | .28** |
| Communicative health literacya | 3.83 | 0.72 | 4.00 | 1.50–5 | .30** |
| Critical health literacya | 3.52 | 0.86 | 3.75 | 1–5 | .30** |
|
| |||||
| Parental empowermenta | 4.23 | 0.47 | 4.22 | 1–5 | .49** |
|
| |||||
| Quality of relationship with schoola | 3.95 | 0.92 | 4.00 | 1–5 | .63** |
|
| |||||
| Food allergy quality of life - PB (N = 311) | 3.35 | 0.85 | 3.35 | 1.18–5 | −.21** |
|
| |||||
| Participation in cause advocacy activitiesa | 1.86 | 1.30 | 2.00 | 0–4 | −.09 |
|
| |||||
| Food allergy knowledge score (N = 312) | 5.73 | 1.60 | 6.00 | 1–8 | .03 |
Note. No significant bivariate correlations among parental advocacy and education level, child's current age, number of years since diagnosis, total number of allergens, lifetime number of severe allergic reactions, 12-month number of severe allergic reactions, degree of support group participation, and the number of children with food allergies for whom participant is primary caregiver. PB = parental burden.
Adapted from Koo (2021).
N = 313.
p < .001.
Bivariate Analyses
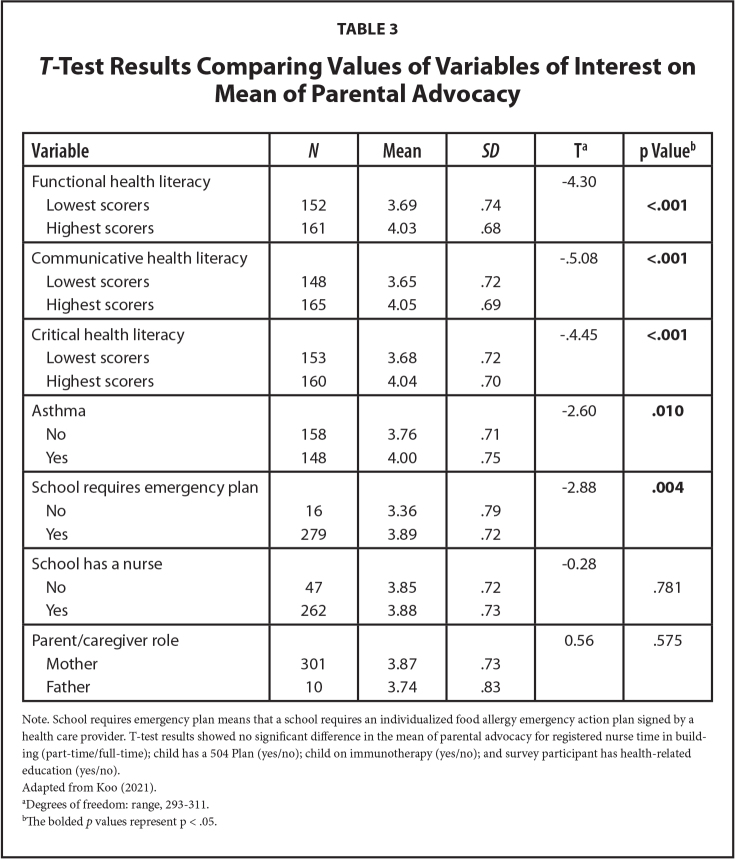
In the bivariate analyses, the perceived effectiveness of parental advocacy behaviors for food allergy management in schools [parental advocacy] was significantly and positively associated with functional, communicative, and critical health literacy; parental empowerment; and the quality of the relationship with the school (p < .001; Table 2). Lower FAQOL-PB was associated with higher parental advocacy scores. Highest versus lowest scorers on the measures of functional, communicative, and critical health literacy also demonstrated significant favorable differences in mean parental advocacy scores (p < .001; Table 3). A child with asthma versus one without, and a school that required an emergency action plan versus one that did not, were significantly associated with differences in mean parental advocacy scores.
Table 3.
T-Test Results Comparing Values of Variables of Interest on Mean of Parental Advocacy
| Variable | N | Mean | SD | Ta | p Valueb |
|---|---|---|---|---|---|
|
| |||||
| Functional health literacy | −4.30 | ||||
| Lowest scorers | 152 | 3.69 | .74 | <.001 | |
| Highest scorers | 161 | 4.03 | .68 | ||
|
| |||||
| Communicative health literacy | −.5.08 | <.001 | |||
| Lowest scorers | 148 | 3.65 | .72 | ||
| Highest scorers | 165 | 4.05 | .69 | ||
|
| |||||
| Critical health literacy | −.4.45 | <.001 | |||
| Lowest scorers | 153 | 3.68 | .72 | ||
| Highest scorers | 160 | 4.04 | .70 | ||
|
| |||||
| Asthma | −2.60 | .010 | |||
| No | 158 | 3.76 | .71 | ||
| Yes | 148 | 4.00 | .75 | ||
|
| |||||
| School requires emergency plan | −2.88 | .004 | |||
| No | 16 | 3.36 | .79 | ||
| Yes | 279 | 3.89 | .72 | ||
|
| |||||
| School has a nurse | −0.28 | ||||
| No | 47 | 3.85 | .72 | .781 | |
| Yes | 262 | 3.88 | .73 | ||
|
| |||||
| Parent/caregiver role | 0.56 | .575 | |||
| Mother | 301 | 3.87 | .73 | ||
| Father | 10 | 3.74 | .83 | ||
Note. School requires emergency plan means that a school requires an individualized food allergy emergency action plan signed by a health care provider. T-test results showed no significant difference in the mean of parental advocacy for registered nurse time in building (part-time/full-time); child has a 504 Plan (yes/no); child on immunotherapy (yes/no); and survey participant has health-related education (yes/no).
Adapted from Koo (2021).
Degrees of freedom: range, 293–311.
The bolded p values represent p < .05.
Health Literacy and Parental Advocacy
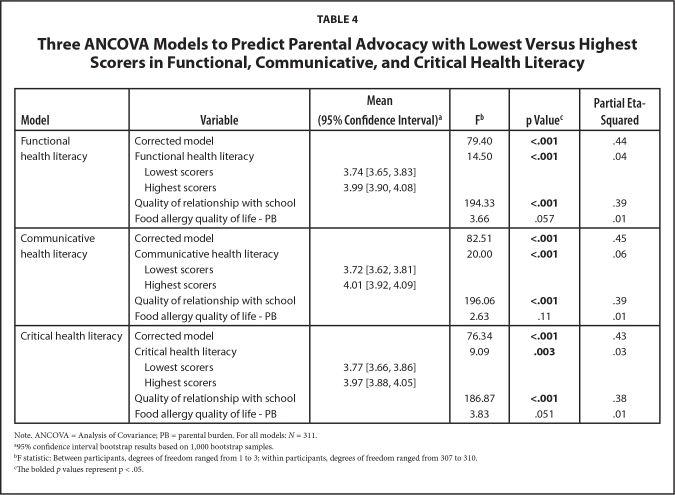
Three parallel hypotheses were tested with ANCOVA to determine if lowest versus highest scorers on self-reported measures of functional, communicative, and critical health literacy were associated with a difference in mean parental advocacy scores while accounting for the quality of the relationship with the school and FAQOL-PB (Table 4). Parents who scored at the highest levels in the three dimensions of health literacy reported that they engaged in advocacy behaviors for food allergy management in schools perceived to be more effective than parents who scored at the lowest levels (hypotheses accepted, p < .05). The models accounted for about 44% of the variance of parental advocacy (range, R2 = .43 to .45 [adjusted R2 = .42 to .45]). Partial eta-squared [partial η^2] is the proportion of total variance, or the effect size, of one predictor variable while accounting for the variance contributed by other variables. In all three models, the quality of the relationship with the school accounted for most of the variance in mean parental advocacy scores (range, partial η2 = .38 to .39).
Table 4.
Three ANCOVA Models to Predict Parental Advocacy with Lowest Versus Highest Scorers in Functional, Communicative, and Critical Health Literacy
| Model | Variable | Mean (95% Confidence Interval)a | Fb | p Valuec | Partial Eta-Squared |
|---|---|---|---|---|---|
|
| |||||
| Functional health literacy | Corrected model | 79.40 | <.001 | .44 | |
| Functional health literacy | 14.50 | <.001 | .04 | ||
| Lowest scorers | 3.74 [3.65, 3.83] | ||||
| Highest scorers | 3.99 [3.90, 4.08] | ||||
| Quality of relationship with school | 194.33 | <.001 | .39 | ||
| Food allergy quality of life - PB | 3.66 | .057 | .01 | ||
|
| |||||
| Communicative health literacy | Corrected model | 82.51 | <.001 | .45 | |
| Communicative health literacy | 20.00 | <.001 | .06 | ||
| Lowest scorers | 3.72 [3.62, 3.81] | ||||
| Highest scorers | 4.01 [3.92, 4.09] | ||||
| Quality of relationship with school | 196.06 | <.001 | .39 | ||
| Food allergy quality of life - PB | 2.63 | .11 | .01 | ||
|
| |||||
| Critical health literacy | Corrected model | 76.34 | <.001 | .43 | |
| Critical health literacy | 9.09 | .003 | .03 | ||
| Lowest scorers | 3.77 [3.66, 3.86] | ||||
| Highest scorers | 3.97 [3.88, 4.05] | ||||
| Quality of relationship with school | 186.87 | <.001 | .38 | ||
| Food allergy quality of life - PB | 3.83 | .051 | .01 | ||
Note. ANCOVA = Analysis of Covariance; PB = parental burden. For all models: N = 311.
95% confidence interval bootstrap results based on 1,000 bootstrap samples.
F statistic: Between participants, degrees of freedom ranged from 1 to 3; within participants, degrees of freedom ranged from 307 to 310.
The bolded p values represent p < .05.
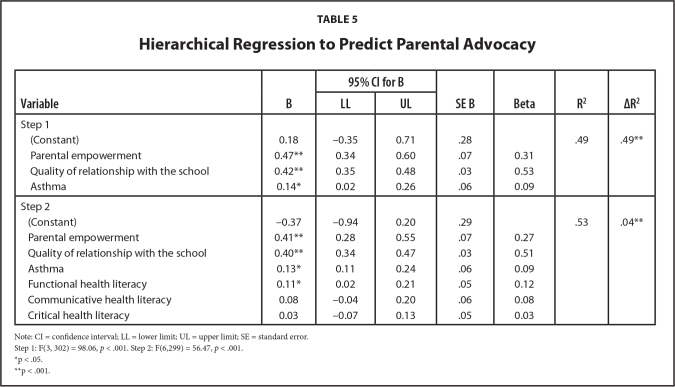
A two-step hierarchical linear regression was conducted to predict parental advocacy while controlling for covariates (Table 5). In step one, the covariates parental empowerment, quality of the relationship with the school, and the child's diagnosis of asthma accounted for 49% of the variance in parental advocacy (Model 1 R2 = .49. In step two, the largest predictors of parental advocacy were parental empowerment and the quality of the relationship with the school (B = .41 and B = .40, respectively). In this second step, functional health literacy was significantly associated with parental advocacy (p = .018) whereas communicative and critical health literacy were not (p > .05). Thus, the hypothesis that communicative and critical health literacy are more strongly associated with parental advocacy than functional health literacy was rejected. Functional health literacy accounted for 4% of the variance in parental advocacy (Model 2 R2 = .53 (ΔR2 = .04). Asthma also was a significant small predictor (p = .032).
Table 5.
Hierarchical Regression to Predict Parental Advocacy
| Variable | B | 95% CI for B | SE B | Beta | R2 | ΔR2 | |
|---|---|---|---|---|---|---|---|
|
| |||||||
| LL | UL | ||||||
|
| |||||||
| Step 1 | |||||||
| (Constant) | 0.18 | −0.35 | 0.71 | .28 | .49 | .49** | |
| Parental empowerment | 0.47** | 0.34 | 0.60 | .07 | 0.31 | ||
| Quality of relationship with the school | 0.42** | 0.35 | 0.48 | .03 | 0.53 | ||
| Asthma | 0.14* | 0.02 | 0.26 | .06 | 0.09 | ||
|
| |||||||
| Step 2 | |||||||
| (Constant) | −0.37 | −0.94 | 0.20 | .29 | .53 | .04** | |
| Parental empowerment | 0.41** | 0.28 | 0.55 | .07 | 0.27 | ||
| Quality of relationship with the school | 0.40** | 0.34 | 0.47 | .03 | 0.51 | ||
| Asthma | 0.13* | 0.11 | 0.24 | .06 | 0.09 | ||
| Functional health literacy | 0.11* | 0.02 | 0.21 | .05 | 0.12 | ||
| Communicative health literacy | 0.08 | −0.04 | 0.20 | .06 | 0.08 | ||
| Critical health literacy | 0.03 | −0.07 | 0.13 | .05 | 0.03 | ||
Note: CI = confidence interval; LL = lower limit; UL = upper limit; SE = standard error.
Step 1: F(3, 302) = 98.06, p < .001. Step 2: F(6,299) = 56.47, p < .001.
p < .05.
p < .001.
Discussion
In this cross-sectional study, the findings highlight the importance of parental empowerment and the quality of the relationship with the school as the strongest predictors of parental advocacy (Koo, 2021). These findings are consistent with the literature (Burke et al., 2019; Burke & Hodapp, 2016; Cudjoe et al., 2020; Mackey et al., 2016). Secondly, the unexpected finding that functional health literacy may be more important than communicative and critical health literacy adds to the mixed evidence regarding the role of communicative and critical health literacy in health management (Amit Aharon et al., 2017; Lai et al., 2013; Londoño & Schulz, 2015; Náfrádi et al., 2016; Ogasawara & Hashimoto, 2020; Qiu et al., 2020; Wang et al., 2016).
Empowerment and Quality of the Relationship with the School
The salience of parental empowerment in this study is congruent with systematic reviews that show some evidence that self-efficacy, a component of empowerment, is associated with chronic disease management behaviors and health outcomes (Cudjoe et al., 2020; Mackey et al., 2016). Psychological empowerment is related to asthma self-management behaviors (Londoño & Schulz, 2015) and medical decision-making (Sak et al., 2017).
This study's finding that the quality of the relationship with the school is an important factor in parental advocacy is supported by studies demonstrating the significant role of the parent-professional partnership on intermediate outcomes related to parental advocacy for children's special education services (Burke et al., 2019; Burke & Hodapp, 2016). Building relationships is considered foundational to interpersonal advocacy efforts (Crawford & Arnold, 2016; Wright & Taylor, 2014). Promoting school-family partnerships that address power dynamics through shared responsibilities, trust, and two-way communication is essential for optimal outcomes in students with disabilities (Haines et al., 2017).
Functional Health Literacy as a Predictor of Parental Advocacy
Functional health literacy was a significant predictor of parental advocacy, whereas communicative and critical health literacy were not significant. This surprising finding may be due to the high ceiling effect of the functional health literacy variable, likely related to the sample's high education level (Koo, 2021). Limited evidence supports the association between functional health literacy and chronic disease management behaviors of parents on behalf of their children (DeWalt & Hink, 2009; Riemann et al., 2021), including correct epinephrine autoinjector technique (Egan et al., 2019). The unexpected finding may be explained by the self-reported nature of the health literacy measure, and future studies could consider a performance-based measure of health literacy (Ayre et al., 2020; Schulz et al., 2021).
Highest Versus Lowest Scorers on Measures of Health Literacy
A practical difference in a research measurement means a real-world difference that impacts patients (Wright et al., 2012). In this study, the statistically significant differences are interpreted as borderline differences for real-world implications for highest versus lowest scorers in the three dimensions of health literacy to predict parental advocacy (0.2–0.3 on 5-point scales; less than one-half of the standard deviation of the outcome measure, using accepted criteria for a minimal clinically important difference) (Chan, 2013; Wright et al., 2012). These results add to the mixed evidence about the associations between communicative and critical health literacy and chronic disease management behaviors in diabetes (Lai et al., 2013; Wang et al., 2016), hypertension (Náfrádi et al., 2016; Qiu et al., 2020), asthma (Amit Aharon et al., 2017; Londoño & Schulz, 2015), and childhood vaccinations (Ogasawara & Hashimoto, 2020).
Strengths and Limitations
This study is valuable in the field of health literacy because it addresses a gap in our understanding about the relationship between three dimensions of health literacy and parental behaviors for a child's food allergy management. This under-studied issue (Ditzler & Greenhawt, 2016; Egan et al., 2019) is examined with carefully constructed multidimensional measures. Study strengths include rigorous methods for disease-specific adaptations of measures; pilot-testing; and robust statistical methods (Koo, 2021). The sample represents many distinct schools and districts in the U.S. without significant duplication. Assessing health literacy outside of the context of the health care encounter has good potential for understanding how to impact disease-management health behaviors (Guzys et al., 2015).
Limitations of this study are related to the cross-sectional design that cannot infer causality in relationships among variables; biases of self-selection, self-report, and history; and generalizability of the sample of predominantly college-educated, White mothers (Koo, 2021). Temporal causality cannot be inferred, for example, in that the quality of the relationship with the school may not be a predictor of parental advocacy but rather a reaction to the school culture and practices (Burke et al., 2019; Burke & Hodapp, 2016). All variables were survey measures of participants' perceptions, and thus are subject to self-report bias. Self-selection and historical biases are probable due to recruitment efforts through a research patient registry and many online food allergy organizations, as well as due to COVID-19-related restrictions to virtual recruitment methods. Findings are not generalizable to populations with low educational attainment or diverse races and ethnicities; yet, future analysis of essay responses from the larger study may provide insights regarding health-literate and empowered strategies to advocate for food allergy safety in schools.
Research Implications
The unexpected finding regarding the salience of functional health literacy, but not communicative nor critical health literacy, has a few possible explanations. Health literacy is a complex multidimensional construct that is difficult to measure. Self-reported health literacy measures, compared to testable measures, may not accurately capture health literacy (Ayre et al., 2020; Schulz et al., 2021). Yet, the most used testable measure of health literacy, the Newest Vital Sign (NVS), involves reading a food label and thus may not be an appropriate measure for parents of children with food allergies due to high ceiling effects (Ditzler & Greenhawt, 2016; Egan et al., 2019). A different objective measure of health literacy may be necessary in food allergy research. The covariate ‘quality of the relationship with the school’ was measured with a single item, yet this construct may benefit from a multidimensional assessment similar to the measure of family-school partnership (Burke et al., 2019; Burke & Hodapp, 2016). Furthermore, other variables not captured in this study may explain the variance in parental advocacy. Recruitment methods beyond virtual means and specialized online groups are necessary to reach a more heterogeneous sample with diverse educational attainment.
Practice Implications
The quality of the relationship with the school and parental empowerment are important factors associated with the parental advocacy for food allergy safety behaviors in schools. School personnel and parents can improve the quality of their relationship and through open communication styles that emphasize listening, trust-building methods, and consistent implementation of systemic policies (Burke & Hodapp, 2016; Haines et al., 2017). In the related context of advocating for special education services, the parents' perceived quality of the relationship with the school was not equivalent to their satisfaction with services nor the school's response to advocacy efforts (Burke, et al., 2019). A school's response to advocacy efforts for food allergy safety may influence the quality of the parent-school relationship, or vice versa, but causality cannot be inferred from this study. To improve parental empowerment, practitioners can encourage building on small successes to improve self-efficacy and adjusting outcome expectations (Bandura, 2004). This could be accomplished through a role-play in which a parent successfully talks about how to avoid food allergen exposures before conversing with a classroom teacher. The important role of functional health literacy found in this study underscores the fundamental necessity of childhood education and adult literacy programs, as well as a health-literate universal precautions approach (Agency for Healthcare Quality and Research, 2015) to communicate school safety management policies.
In conclusion, functional health literacy seems to be the salient dimension of health literacy when measured by a three-dimensional self-report scale to predict effective advocacy behaviors for food allergy safety in schools among highly educated mothers. Health literacy appears to be one of many factors that impact parental chronic disease management strategies and impact everyday life encounters outside of healthcare services. Areas for intervention may target enhancing parental empowerment and the quality of their relationship between parents and schools through open communication and building trust regarding food allergy management.
Acknowledgments
The authors thank Erin R. Hager and Boris D. Lushniak who provided valuable input during the dissertation process; the leaders of food allergy organizations who allowed or facilitated participant recruitment through their organizations, including the FARE (Food Allergy Research and Education) Patient Registry; and the parent volunteers.
References
- Agency for Healthcare Quality and Research . ( 2015. ). Health Literacy Universal Precautions Toolkit , 2nd Edition . https://www.ahrq.gov/health-literacy/improve/precautions/toolkit.html
- Amit Aharon , A. , Nehama , H. , Rishpon , S. , & Baron-Epel , O. ( 2017. ). Parents with high levels of communicative and critical health literacy are less likely to vaccinate their children . Patient Education and Counseling , 100 ( 4 ), 768 – 775 . 10.1016/j.pec.2016.11.016 PMID: [DOI] [PubMed] [Google Scholar]
- Ayre , J. , Costa , D. S. J. , McCaffery , K. J. , Nutbeam , D. , & Muscat , D. M. ( 2020. ). Validation of an Australian parenting health literacy skills instrument: The parenting plus skills index . Patient Education and Counseling , 103 ( 6 ), 1245 – 1251 . 10.1016/j.pec.2020.01.012 PMID: [DOI] [PubMed] [Google Scholar]
- Bandura , A. ( 2004. ). Health promotion by social cognitive means . Health Education & Behavior , 31 ( 2 ), 143 – 164 . 10.1177/1090198104263660 PMID: [DOI] [PubMed] [Google Scholar]
- Burke , M. M. , Goldman , S. E. , Hart , M. S. , & Hodapp , R. M. ( 2016. ). Evaluating the efficacy of a special education advocacy training program . Journal of Policy and Practice in Intellectual Disabilities , 13 ( 4 ), 269 – 276 . 10.1111/jppi.12183 [DOI] [Google Scholar]
- Burke , M. M. , & Hodapp , R. M. ( 2016. ). The nature, correlates, and conditions of parental advocacy in special education . Exceptionality , 24 ( 3 ), 137 – 150 . 10.1080/09362835.2015.1064412 [DOI] [Google Scholar]
- Burke , M. M. , Lee , C. E. , & Rios , K. ( 2019. ). A pilot evaluation of an advocacy programme on knowledge, empowerment, family-school partnership and parent well-being . Journal of Intellectual Disability Research , 63 ( 8 ), 969 – 980 . 10.1111/jir.12613 PMID: [DOI] [PubMed] [Google Scholar]
- Burke , M. M. , & Sandman , L. ( 2017. ). The effectiveness of a parent legislative advocacy program . Journal of Policy and Practice in Intellectual Disabilities , 14 ( 2 ), 138 – 145 . 10.1111/jppi.12173 [DOI] [Google Scholar]
- Cawthon , S. W. , Caemmerer , J. M. , & the PEPNET 2 Research and Evidence Synthesis Team . ( 2014. ). Parents' perspectives on transition and postsecondary outcomes for their children who are d/Deaf or hard of hearing . American Annals of the Deaf , 159 ( 1 ), 7 – 21 . 10.1353/aad.2014.0013 PMID: [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . ( 2013. ). Voluntary guidelines for managing food allergies in schools and early care and education programs . U.S. Department of Health and Human Services; . https://www.cdc.gov/healthyschools/foodallergies/pdf/20_316712-A_FA_guide_508tag.pdf [Google Scholar]
- Chan , L. S. ( 2013. ). Minimal clinically important difference (MCID)—Adding meaning to statistical inference . American Journal of Public Health , 103 ( 11 ), e24 – e25 . 10.2105/AJPH.2013.301580 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chou , H.-L. , Lo , Y.-L. , Liu , C.-Y. , Lin , S.-C. , & Chen , Y.-C. ( 2020. ). Development and psychometric evaluation of the cancer health literacy scale in newly diagnosed cancer patients . Cancer Nursing , 43 ( 5 ), E291 – E303 . 10.1097/NCC.0000000000000711 PMID: [DOI] [PubMed] [Google Scholar]
- Cohen , B. L. , Noone , S. , Muñoz-Furlong , A. , & Sicherer , S. H. ( 2004. ). Development of a questionnaire to measure quality of life in families with a child with food allergy . The Journal of Allergy and Clinical Immunology , 114 ( 5 ), 1159 – 1163 . 10.1016/j.jaci.2004.08.007 PMID: [DOI] [PubMed] [Google Scholar]
- Crawford , E. R. , & Arnold , N. W. ( 2016. ). Exploring the meaning and paths of advocacy for undocumented students' access to education . Journal of Latinos and Education , 15 ( 3 ), 197 – 213 . 10.1080/15348431.2015.1131691 [DOI] [Google Scholar]
- Cudjoe , J. , Delva , S. , Cajita , M. , & Han , H.-R. ( 2020. ). Empirically tested health literacy frameworks . HLRP: Health Literacy Research and Practice , 4 ( 1 ), e22 – e44 . 10.3928/24748307-20191025-01 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeWalt , D. A. , & Hink , A. ( 2009. ). Health literacy and child health outcomes: A systematic review of the literature . Pediatrics , 124 ( Suppl. 3 ), S265 – S274 . 10.1542/peds.2009-1162B PMID: [DOI] [PubMed] [Google Scholar]
- Ditzler , N. , & Greenhawt , M. ( 2016. ). Influence of health literacy and trust in online information on food allergy quality of life and self-efficacy . Annals of Allergy, Asthma & Immunology , 117 ( 3 ), 258 – 263.e1 . 10.1016/j.anai.2016.07.011 PMID: [DOI] [PubMed] [Google Scholar]
- Egan , M. , Yin , H. S. , Greenhawt , M. , & Wang , J. ( 2019. ). Low caregiver health literacy among pediatric food-allergic patients is associated with poorer food allergy management knowledge. The Journal of Allergy and Clinical Immunology . In Practice , 7 ( 2 ), 655 – 658 . 10.1016/j.jaip.2018.05.021 PMID: [DOI] [PubMed] [Google Scholar]
- Faul , F. , Erdfelder , E. , Buchner , A. , & Lang , A.-G. ( 2009. ). Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses . Behavior Research Methods , 41 ( 4 ), 1149 – 1160 . 10.3758/BRM.41.4.1149 PMID: [DOI] [PubMed] [Google Scholar]
- Gupta , R. S. , Warren , C. M. , Smith , B. M. , Blumenstock , J. A. , Jiang , J. , Davis , M. M. , & Nadeau , K. C. ( 2018. ). The public health impact of parent-reported childhood food allergies in the United States . Pediatrics , 142 ( 6 ), e20181235 Advance online publication. 10.1542/peds.2018-1235 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guzys , D. , Kenny , A. , Dickson-Swift , V. , & Threlkeld , G. ( 2015. ). A critical review of population health literacy assessment . BMC Public Health , 15 , 215 . 10.1186/s12889-015-1551-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haines , S. J. , Francis , G. L. , Mueller , T. G. , Chiu , C.-Y. , Burke , M. M. , Kyzar , K. , Shepherd , K. G. , Holdren , N. , Aldersey , H. M. , & Turnbull , A. P. ( 2017. ). Reconceptualizing Family-Professional Partnership for Inclusive Schools: A Call to Action. Reconceptualización de La Colaboración Entre La Familia y El Profesional Para Las Escuelas Inclusivas [Academic Search Ultimate.] . Un Llamado a La Acción . , 5 ( 4 ), 234 – 247 . [Google Scholar]
- Heijmans , M. , Waverijn , G. , Rademakers , J. , van der Vaart , R. , & Rijken , M. ( 2015. ). Functional, communicative and critical health literacy of chronic disease patients and their importance for self-management . Patient Education and Counseling , 98 ( 1 ), 41 – 48 . 10.1016/j.pec.2014.10.006 PMID: [DOI] [PubMed] [Google Scholar]
- Ishikawa , H. , Takeuchi , T. , & Yano , E. ( 2008. ). Measuring functional, communicative, and critical health literacy among diabetic patients . Diabetes Care , 31 ( 5 ), 874 – 879 . 10.2337/dc07-1932 PMID: [DOI] [PubMed] [Google Scholar]
- Kao , L. M. , Wang , J. , Kagan , O. , Russell , A. , Mustafa , S. S. , Houdek , D. , Smith , B. , & Gupta , R. ( 2018. ). School nurse perspectives on school policies for food allergy and anaphylaxis . Annals of Allergy, Asthma & Immunology , 120 ( 3 ), 304 – 309 . 10.1016/j.anai.2017.12.019 PMID: [DOI] [PubMed] [Google Scholar]
- Koo , L. W. ( 2021. ). Parental health literacy, empowerment, and advocacy in the context of food allergies management in schools (Publication No. 2634813333) [Doctoral dissertation , University of Maryland, College Park; ]. ProQuest Dissertations & Theses Global. http://www.proquest.com/dissertations/docview/2634813333/abstract/2DBAD1F1E88D4E6BPQ/1 [Google Scholar]
- Kramer , J. , Rubin , A. , Coster , W. , Helmuth , E. , Hermos , J. , Rosenbloom , D. , Moed , R. , Dooley , M. , Kao , Y. C. , Liljenquist , K. , Brief , D. , Eng-gasser , J. , Keane , T. , Roy , M. , & Lachowicz , M. ( 2014. ). Strategies to address participant misrepresentation for eligibility in Web-based research . International Journal of Methods in Psychiatric Research , 23 ( 1 ), 120 – 129 . 10.1002/mpr.1415 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai , A. Y. , Ishikawa , H. , Kiuchi , T. , Mooppil , N. , & Griva , K. ( 2013. ). Communicative and critical health literacy, and self-management behaviors in end-stage renal disease patients with diabetes on hemo-dialysis . Patient Education and Counseling , 91 ( 2 ), 221 – 227 . 10.1016/j.pec.2012.12.018 PMID: [DOI] [PubMed] [Google Scholar]
- Lawlis , T. , Bakonyi , S. , & Williams , L. T. ( 2017. ). Food allergy in schools: The importance of government involvement . Nutrition & Dietetics: The Journal of the Dietitians Association of Australia , 74 ( 1 ), 82 – 87 . 10.1111/1747-0080.12225 PMID: [DOI] [PubMed] [Google Scholar]
- Lieberman , P. , Nicklas , R. A. , Randolph , C. , Oppenheimer , J. , Bernstein , D. , Bernstein , J. , Ellis , A. , Golden , D. B. K. , Greenberger , P. , Kemp , S. , Khan , D. , Ledford , D. , Lieberman , J. , Metcalfe , D. , Nowak-Wegrzyn , A. , Sicherer , S. , Wallace , D. , Blessing-Moore , J. , Lang , D. , Tilles , S. A. ( 2015. ). Anaphylaxis—A practice parameter update 2015 . Annals of Allergy, Asthma & Immunology , 115 ( 5 ), 341 – 384 . 10.1016/j.anai.2015.07.019 PMID: [DOI] [PubMed] [Google Scholar]
- Londoño , A. M. M. , & Schulz , P. J. ( 2015. ). Influences of health literacy, judgment skills, and empowerment on asthma self-management practices . Patient Education and Counseling , 98 ( 7 ), 908 – 917 . 10.1016/j.pec.2015.03.003 PMID: [DOI] [PubMed] [Google Scholar]
- Mackey , L. M. , Doody , C. , Werner , E. L. , & Fullen , B. ( 2016. ). Self-management skills in chronic disease management: What role does health literacy have? Medical Decision Making , 36 ( 6 ), 741 – 759 . 10.1177/0272989X16638330 PMID: [DOI] [PubMed] [Google Scholar]
- Malec , J. F. , Brown , A. W. , & Moessner , A. M. ( 2010. ). Two new measures for assessing advocacy activities and perceived control after acquired brain injury . Disability and Rehabilitation , 32 ( 1 ), 33 – 40 . 10.3109/09638280902980936 PMID: [DOI] [PubMed] [Google Scholar]
- Náfrádi , L. , Galimberti , E. , Nakamoto , K. , & Schulz , P. ( 2016. ). Intentional and unintentional medication non-adherence in hypertension: The role of health literacy, empowerment and medication beliefs . Journal of Public Health Research , 5 ( 3 ), 3/21/18 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nutbeam , D. ( 2000. ). Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century . Health Promotion International , 15 ( 3 ), 259 – 267 . 10.1093/heapro/15.3.259 [DOI] [Google Scholar]
- Ogasawara , H. , & Hashimoto , H. ( 2020. ). Relationship between maternal communicative/critical health literacy and child's asthma symptoms: Results from a population-based survey in metropolitan Japan . Patient Education and Counseling , 103 ( 5 ), 999 – 1004 . 10.1016/j.pec.2019.11.026 PMID: [DOI] [PubMed] [Google Scholar]
- Paasche-Orlow , M. K. , & Wolf , M. S. ( 2007. ). The causal pathways linking health literacy to health outcomes . American Journal of Health Behavior , 31 ( Suppl. 1 ), S19 – S26 . 10.5993/AJHB.31.s1.4 PMID: [DOI] [PubMed] [Google Scholar]
- Qiu , C. , Zhang , X. , Zang , X. , & Zhao , Y. ( 2020. ). Acceptance of illness mediate the effects of health literacy on self-management behaviour . European Journal of Cardiovascular Nursing , 19 ( 5 ), 411 – 420 . 10.1177/1474515119885240 PMID: [DOI] [PubMed] [Google Scholar]
- Riemann , L. , Lubasch , J. S. , Heep , A. , & Ansmann , L. ( 2021. ). The role of health literacy in health behavior, health service use, health outcomes, and empowerment in pediatric patients with chronic disease: a systematic review . International Journal of Environmental Research and Public Health , 18 ( 23 ), 12464 . 10.3390/ijerph182312464 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sak , G. , Rothenfluh , F. , & Schulz , P. J. ( 2017. ). Assessing the predictive power of psychological empowerment and health literacy for older patients' participation in health care: A cross-sectional population-based study . BMC Geriatrics , 17 ( 1 ), 59 . 10.1186/s12877-017-0448-x PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz , P. J. , Pessina , A. , Hartung , U. , & Petrocchi , S. ( 2021. ). Effects of objective and subjective health literacy on patients' accurate judgment of health information and decision-making ability: Survey study . Journal of Medical Internet Research , 23 ( 1 ), e20457 . 10.2196/20457 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sørensen , K. , Van den Broucke , S. , Fullam , J. , Doyle , G. , Pelikan , J. , Slonska , Z. , Brand , H. , & the (HLS-EU) Consortium Health Literacy Project European . ( 2012. ). Health literacy and public health: A systematic review and integration of definitions and models . BMC Public Health , 12 ( 1 ), 80 . 10.1186/1471-2458-12-80 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szychlinski , C. , Schmeissing , K. A. , Fuleihan , Z. , Qamar , N. , Syed , M. , Pongracic , J. A. , & Singh , A. M. ( 2015. ). Food allergy emergency preparedness in Illinois schools: Rural disparity in guideline implementation. The Journal of Allergy and Clinical Immunology . In Practice , 3 ( 5 ), 805 – 7.e8 . 10.1016/j.jaip.2015.04.017 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patient Protection and Affordable Care Act . ( 2010. ). Pub. L. No. 111–148, 1252. https://www.hhs.gov/sites/default/files/v-healthcareworkforce.pdf [Google Scholar]
- von Wagner , C. , Steptoe , A. , Wolf , M. S. , & Wardle , J. ( 2009. ). Health literacy and health actions: A review and a framework from health psychology . Health Education & Behavior , 36 ( 5 ), 860 – 877 . 10.1177/1090198108322819 PMID: [DOI] [PubMed] [Google Scholar]
- Wang , R.-H. , Hsu , H.-C. , Lee , Y.-J. , Shin , S.-J. , Lin , K.-D. , & An , L.-W. ( 2016. ). Patient empowerment interacts with health literacy to associate with subsequent self-management behaviors in patients with type 2 diabetes: A prospective study in Taiwan . Patient Education and Counseling , 99 ( 10 ), 1626 – 1631 . 10.1016/j.pec.2016.04.001 PMID: [DOI] [PubMed] [Google Scholar]
- Warren , C. M. , Gupta , R. S. , Sohn , M.-W. , Oh , E. H. , Lal , N. , Garfield , C. F. , Caruso , D. , Wang , X. , & Pongracic , J. A. ( 2015. ). Differences in empowerment and quality of life among parents of children with food allergy . Annals of Allergy, Asthma & Immunology , 114 ( 2 ), 117 – 125 . 10.1016/j.anai.2014.10.025 PMID: [DOI] [PubMed] [Google Scholar]
- Waserman , S. , Cruickshank , H. , Hildebrand , K. J. , Mack , D. , Bantock , L. , Bingemann , T. , Chu , D. K. , Cuello-Garcia , C. , Ebisawa , M. , Fahmy , D. , Fleischer , D. M. , Galloway , L. , Gartrell , G. , Greenhawt , M. , Hamilton , N. , Hourihane , J. , Langlois , M. , Loh , R. , Muraro , A. , Brozek , J. L. ( 2021. ). Prevention and management of allergic reactions to food in child care centers and schools: Practice guidelines . The Journal of Allergy and Clinical Immunology , 147 ( 5 ), 1561 – 1578 . 10.1016/j.jaci.2021.01.034 PMID: [DOI] [PubMed] [Google Scholar]
- Wright , A. C. , & Taylor , S. ( 2014. ). Advocacy by parents of young children with special needs: Activities, processes, and perceived effectiveness . Journal of Social Service Research , 40 ( 5 ), 591 – 605 . 10.1080/01488376.2014.896850 [DOI] [Google Scholar]
- Wright , A. , Hannon , J. , Hegedus , E. J. , & Kavchak , A. E. ( 2012. ). Clinimetrics corner: A closer look at the minimal clinically important difference (MCID) . The Journal of Manual & Manipulative Therapy , 20 ( 3 ), 160 – 166 . 10.1179/2042618612Y.0000000001 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]