Abstract
Background Spastic joint contractures remain a complex and challenging condition. For patients with upper extremity spastic dysfunction, improving the muscle balance is essential to maximize their hand function. Multiple procedures, including proximal row carpectomy (PRC) and wrist arthrodesis (WA), are considered among the different surgical alternatives. However, the biomechanical consequences of these two procedures have not been well described in current literature. Hence, the objective of our study is to assess the change in the extrinsic digit flexor tendon resting length after proximal row carpectomy and wrist arthrodesis.
Methods Six fresh-frozen cadaver upper extremities (four females and two males) with no obvious deformity underwent dissection, PRC, and WA. All the flexor digitorum profundus (FDP), flexor digitorum superficialis (FDS), and flexor pollicis longus (FPL) tendons were marked proximally 1-cm distal to their respective myotendinous junction and cut distally at the marked point. The overlapping segment of each distal flexor tendon from its proximal mark was considered the amount of flexor tendon resting length change after PRC and WA. A descriptive evaluation was performed to assess the increment in tendon resting length. Additionally, a regression analysis was performed to evaluate the relation between the tendon resting length and the proximal carpal row height.
Results Following PRC and WA, the mean digit flexor tendon resting length increment achieved across all tendons was 1.88 cm (standard deviation [SD] = 0.45; range: 1.00–3.00 cm). A weak direct relationship ( R = 0.0334) between the increment in tendon resting length and proximal carpal row height was initially suggested, although no statistical significance was demonstrated ( p = 0.811).
Conclusion This study provides an anatomic description of the increased extrinsic digit flexor tendon resting length after PRC and WA in cadaveric specimens. Findings provide a useful framework to estimate the amount of extrinsic digit flexor resting length increment achieved after wrist fusion and the proximal carpal row removal.
Keywords: proximal row carpectomy, flexor tendon resting length, wrist arthrodesis, proximal carpal row height, cadaveric study
Introduction
The management of patients with spastic joint contractures is complex and challenging. 1 Patients typically present with a flexion contracture of the wrist and digits secondary to spasticity of the flexor-pronator mass. This condition deteriorates functionality, hygiene, and esthetics. 2 3 It may occur as a sequela of an insult to the upper motor neuron system as seen in patients with a traumatic brain injury, stroke, or cerebral palsy. 1 4 5 The severity of the spasticity will dictate the amount of flexion contracture present in the digits and wrist. One method to evaluate spasticity is through the Volkmann angle which is described as the position of the wrist in which the digits start flexing into a fist on wrist extension. The greater the severity of the contracture of digit flexors, the greater the Volkmann angle. 6
Treatment of the upper extremity spastic dysfunction is focused on improving muscle balance to maximize hand function. 7 Surgical options for managing wrist flexion deformity and digital flexor contracture consist of soft tissue procedures such as tendon transfers, flexor-pronator slide, and tendon lengthening. 1 In cases of severe static wrist flexion deformity (grade-3 Zancolli's classification) with little to no voluntary control, soft tissue procedures alone would not provide an adequate correction. 8 Thus, to allow for passive wrist extension into the neutral position, WA is the recommended surgical option. 1 3 In skeletally mature individuals, adding a proximal row carpectomy (PRC) has been recommended due to the benefits of reducing the fusion sites, obtaining bone graft from the proximal carpal row, and shortening the skeletal level arm of the wrist to relax the digit flexor tendons. 1 3 8 9 10 It also provides an equal relative lengthening of all the flexor muscle–tendon units crossing the wrist. 3 8 Whenever additional flexor lengthening is necessary, flexor lengthening procedures like fractional lengthening or Z-lengthening are performed concomitantly. 9 Following these procedures, it is expected that resting length and digits' position would improve. In the latter of the benefits, no previous study has indicated the digit flexor tendon resting length increment achieved after PRC and WA. This information may prove valuable during the preoperative planning if a concomitant flexor tendon fractional lengthening or Z-lengthening is needed.
Therefore, the primary objective of our cadaveric study was to quantify the flexor tendon resting length increment after PRC and WA. It is particularly imperative to estimate the amount of tendon lengthening needed for an adequate correction since overcorrection can lead to decreased grip strength and undercorrection can lead to a persistent clenched fist after WA. 3 11 Our secondary objective was to evaluate the relationship between the proximal carpal row height with the amount of flexor tendon resting length increment obtained after PRC and WA. We hypothesize that these procedures will provide an increment in resting length that correlates with the amount of proximal carpal row height.
Materials and Methods
Six fresh-frozen cadaver upper extremities (four females and two males), with no obvious deformity and an average age of 63 years (range: 51–72 years), were obtained from the Board of Anatomic Donations of the Medical Sciences Campus at the University of Puerto Rico to be used in this study. All specimens were previously stored at freezing temperature, then thawed at room temperature for 24 hours before conducting the study at room temperature. Transhumeral amputations were performed to preserve flexor-pronator mass insertions. Before the procedure, a standard true posteroanterior radiograph of all wrists in neutral position was taken with a scanogram radiology ruler and analyzed by the primary investigator. In every radiograph, the proximal carpal row height was measured as the distance from the lunate fossa to the base of the capitate. Dissection of all volar forearm and hand subcutaneous tissue was performed. All tendons of the flexor digitorum profundus (FDP), flexor digitorum superficialis (FDS), and flexor pollicis longus (FPL) were marked proximally 1-cm distal to their respective myotendinous junction. An 18-gauge needle was inserted at this point for each tendon to fix the proximal end into the surrounding tissues and avoid tendon recoil, as suggested by a previous study. 12
All digits were fixed in extension using 2.0-mm Kirschner wires (K-wires) by intramedullary drilling that traveled from each digit distal phalanx tip ending at the middle third of each metacarpal bone. Distally, all tendons' insertions were left intact at their bony attachments. The forearm was then placed in a prone position. A medial longitudinal incision of 10 cm was performed on the dorsal aspect of the wrist aligned with the third metacarpal to expose the carpal bones. The extensor pollicis longus tendon was released from the third-extensor compartment and retracted radially. The periosteum on the dorsal aspect of the radius and dorsal wrist capsule was divided longitudinally between the second and fourth compartments. Also, the periosteum along the dorsal aspect of the third metacarpal was split. The radial and ulnar wrist capsular flaps were reflected to expose the wrist joint. Then, the scaphoid, lunate, and triquetrum were excised. The articular cartilage and subchondral bone were carefully removed from the lunate fossa and the proximal pole of the capitate. After dissection, all wrists were fixed with a 2.4-mm K-wire in an anterograde configuration. The wrists were placed in 10 degrees of dorsiflexion with 5 degrees of ulnar deviation in all cadaver specimens. The degrees of joint angulation were assessed and confirmed with a goniometer.
After PRC and WA, the extremity was placed in the supine position. The tendons were then cut perpendicularly with a surgical scalpel blade distally to the previously inserted needle at the marked point in all cadaver specimens. Afterward, the change in resting length of all FDP, FDS, and FPL tendons was quantified using the ruler method as described by Chang et al that consisted of a length measure with a ruler between the proximal and distal borders of the desire tendon. 13 We measure each distal flexor tendon overlapping segment from its proximal mark using a flexible ruler (Flexi-Ruler, Devon, Kendall, Massachusetts, United States). 12 13 This overlapping measure was considered the amount of flexor tendon resting length increment after PRC and WA ( Fig. 1 ).
Fig. 1.
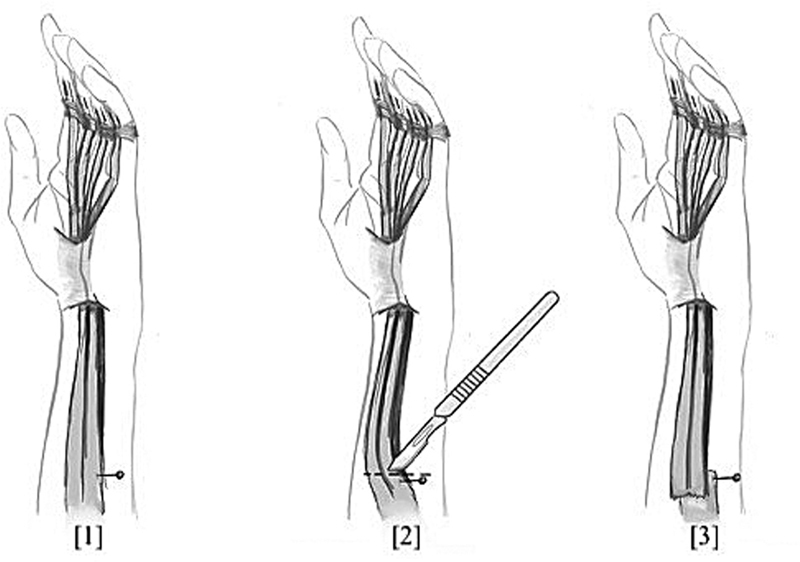
Method for tendon measurement. (1) Flexor digitorum superficialis, flexor digitorum profundus, and flexor pollicis longus were marked proximally 1-cm distal to their respective myotendinous junction with an 18-gauge needle. (2) After proximal row carpectomy and wrist arthrodesis, the extremity was placed in supine position and the tendons were cut perpendicular distally at the previously marked point. (3) Each distal flexor tendon overlapping of its proximal mark was measured, and the overlapping was considered as the amount of flexor tendon resting length increment.
The mean and standard deviation were calculated for our quantitative variables. The change in tendon resting length and the proximal carpal row height were measured. An analysis of variance (ANOVA) was performed to evaluate the variation in the repeated measures of the proximal carpal row height.
A linear regression analysis described the relationship between the proximal carpal row height and the increment in resting length after PRC and WA. The correlation between proximal carpal row height and tendon resting length increment was visualized using a scatter plot ( Fig. 2 ). A value of p less than 0.05 was set for statistical significance.
Fig. 2.

Graph showing the relation between the proximal carpal row height and the Increment in tendon resting length achieved after a proximal row carpectomy and wrist arthrodesis.
Results
The mean flexor tendon resting length increment achieved across all tendons was 1.88 cm (SD = 0.45; range: 1.00–3.00 cm). Among the 24 FDS tendons, the mean flexor tendon resting length increment achieved was 1.93 cm (SD = 0.39; range: 1.40–3.00 cm). The 24 FDP tendons showed a mean tendon resting length increment of 1.94 cm (SD = 0.47; range: 1.00–2.70 cm). The six FPL tendons showed a mean of tendon excursion of 1.43 cm (SD = 0.31; range: 1.00–1.80 cm). In addition, the mean flexor tendon resting length increment achieved for the 24 FDS and the 24 FDP was evaluated as a group obtaining a value of 1.94 cm (SD = 0.44; range: 1.00–3.00 cm). The distribution of average tendon resting length measurements by individual digits is seen in Table 1 .
Table 1. Tendon resting length effect by digit of all FDP, FDS, and FPL after proximal row carpectomy and wrist arthrodesis.
| Variables | n | Change in flexor tendon resting length (cm) |
|---|---|---|
| All flexor by digit (cm) | Mean (SD) [range] | |
| 1st (FPL) | 6 | 1.43 (0.31) [1.00–1.80 cm] |
| 2nd (FDS and FDP) | 12 | 1.77 (0.60) [1.20–3.00 cm] |
| 3rd (FDS and FDP) | 12 | 2.08 (0.22) [1.60–2.30 cm] |
| 4th (FDS and FDP) | 12 | 2.07 (0.38) [1.60–2.70 cm] |
| 5th (FDS and FDP) | 12 | 1.83 (0.41) [1.00–2.60 cm] |
| All FDP by digit | ||
| 2nd (FDP) | 6 | 1.47 (0.21) [1.20–1.80 cm] |
| 3rd (FDP) | 6 | 2.13 (0.12) [2.00–2.30 cm] |
| 4th (FDP) | 6 | 2.24 (0.45) [1.60–2.70 cm] |
| 5th (FDP) | 6 | 1.95 (0.58) [1.00–2.60 cm] |
| All FDS by digit | ||
| 2nd (FDS) | 6 | 2.07 (0.74) [1.40–3.00 cm] |
| 3rd (FDS) | 6 | 2.02 (0.29) [1.60–2.30 cm] |
| 4th (FDS) | 6 | 1.92 (0.24) [1.70–2.30 cm] |
| 5th (FDS) | 6 | 1.72 (0.06) [1.70–1.80 cm] |
Abbreviations: FDP, flexor digitorum profundus; FDS, flexor digitorum superficialis; FPL, flexor pollicis longus; SD, standard deviation.
An average proximal carpal row height of 1.33 cm (SD = 0.19 cm; range: 1.10–1.50 cm) was observed on all X-rays. No statistically significant difference was observed after evaluation of the variation in repeated measurements ( p = 0.065).
The association between the proximal carpal row height and the increment in tendon resting length suggests a weak direct relationship ( R = 0.0334), although no statistical significance was demonstrated ( p = 0.811).
Discussion
The biomechanical consequences of a PRC and WA have not been well described in current literature. Further studies are required to evaluate their effect on the mechanic of the digits. 14
The results of our study provide surgeons a valuable tool for estimation of the amount of flexor tendon resting length increment that can be achieved after wrist fusion and removal of the proximal carpal row. Our study found an average digit flexor tendon resting length increment of 1.88 cm after performing a PRC and WA in six cadaveric arms.
Flexor tendon lengthening procedures include fractional lengthening and Z-lengthening. Through fractional lengthening of each tendon flexor, 1 to 3 cm of length can be achieved, while 2 to 5 cm of length can be achieved through Z-lengthening of each tendon flexor. 15 Our findings suggest that a similar value of tendon resting length increment after a fractional length can be achieved through the PRC and WA alone. Therefore, in cases where proximal flexor-pronator origin release is being considered for digit deformity correction, the bone procedures coupled with fractional lengthening may suffice in providing the necessary lengthening. Further flexor lengthening procedures require an additional incision, escalate the complexity of the surgery, and have been related to a greater risk of neurovascular complications. 3 9 It is noteworthy to recognize the potential 1 to 3 cm of tendon resting length increment already achieved after a PRC and WA.
After our descriptive analysis, we evaluated the statistical association between the increments in resting length with the amount of proximal carpal row height. We found a weak direct relationship in our regression analysis that revealed that it was not significant after a rigorous statistical evaluation.
This cadaveric study holds several limitations. Due to its in vitro nature, its results may not be able to be extrapolated to living subjects. The indications to perform a PRC and WA include a wrist with a severe flexion deformity. This was not the case with our cadaveric patients in which no obvious deformities were evident. A significant consideration in our study is that cadavers may have altered tissue turgor due to postmortem fluid shifts. This turgor loss affects tissue elasticity, potentially causing a discrepancy between quantifiable lengths in cadavers versus living subjects.
Moreover, differences in tissue behavior between cadavers could be considerable depending on their conservation process and unique postmortem deterioration state during the study. Therefore, the descriptive approach seems more relevant for hand surgeons since pursuing a statistical relation may not be predictable or achievable due to the limitations previously mentioned. Ideally, higher volume clinical studies with more rigorous control are necessary to investigate whether these results have statistical correlation and significance that can be translated into live subjects. On the other hand, to better evaluate these patients' proximal carpal row height, we recognize that a true posteroanterior wrist X-ray would not be a realistic alternative.
In these cases, we recommend obtaining a contralateral posteroanterior wrist X-ray. If this is not possible, physicians could consider an ipsilateral lateral view wrist X-ray or a three-dimensional computed tomography scan.
Acknowledgment
We would like to thank Paola A. Richiez-Nieves, MD, for the help provided in the artwork of this study.
Footnotes
Conflict of Interest None declared.
References
- 1.Duquette S P, Adkinson J M. Surgical management of spasticity of the forearm and wrist. Hand Clin. 2018;34(04):487–502. doi: 10.1016/j.hcl.2018.06.006. [DOI] [PubMed] [Google Scholar]
- 2.Carlson M G, Athwal G S, Bueno R A. Treatment of the wrist and hand in cerebral palsy. J Hand Surg Am. 2006;31(03):483–490. doi: 10.1016/j.jhsa.2005.12.013. [DOI] [PubMed] [Google Scholar]
- 3.Omer G E, Capen D A. Proximal row carpectomy with muscle transfers for spastic paralysis. J Hand Surg Am. 1976;1(03):197–204. doi: 10.1016/s0363-5023(76)80038-x. [DOI] [PubMed] [Google Scholar]
- 4.Gharbaoui I, Kania K, Cole P. Spastic paralysis of the elbow and forearm. Semin Plast Surg. 2016;30(01):39–44. doi: 10.1055/s-0035-1571255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trompetto C, Marinelli L, Mori L et al. Pathophysiology of spasticity: implications for neurorehabilitation. BioMed Res Int. 2014;2014:354906. doi: 10.1155/2014/354906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zancolli E A, Zancolli E R., Jr Surgical management of the hemiplegic spastic hand in cerebral palsy. Surg Clin North Am. 1981;61(02):395–406. doi: 10.1016/s0039-6109(16)42389-3. [DOI] [PubMed] [Google Scholar]
- 7.Van Heest A E, House J H, Cariello C. Upper extremity surgical treatment of cerebral palsy. J Hand Surg Am. 1999;24(02):323–330. doi: 10.1053/jhsu.1999.0323. [DOI] [PubMed] [Google Scholar]
- 8.Rayan G M, Young B T. Arthrodesis of the spastic wrist. J Hand Surg Am. 1999;24(05):944–952. doi: 10.1053/jhsu.1999.0944. [DOI] [PubMed] [Google Scholar]
- 9.Lomita C, Ezaki M, Oishi S. Upper extremity surgery in children with cerebral palsy. J Am Acad Orthop Surg. 2010;18(03):160–168. doi: 10.5435/00124635-201003000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Pinzur M S. Carpectomy and fusion in adult-acquired hand spasticity. Orthopedics. 1996;19(08):675–677. doi: 10.3928/0147-7447-19960801-12. [DOI] [PubMed] [Google Scholar]
- 11.Keenan M A, Abrams R A, Garland D E, Waters R L. Results of fractional lengthening of the finger flexors in adults with upper extremity spasticity. J Hand Surg Am. 1987;12(04):575–581. doi: 10.1016/s0363-5023(87)80211-3. [DOI] [PubMed] [Google Scholar]
- 12.Wu C H, Shoap S, Strauch R J. Subcutaneous transposition of the flexor pollicis longus: does it provide increased length for tendon repair? A cadaveric study. Hand (N Y) 2020;15(06):828–830. doi: 10.1177/1558944719837014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chang C B, Seong S C, Kim T K. Preoperative magnetic resonance assessment of patellar tendon dimensions for graft selection in anterior cruciate ligament reconstruction. Am J Sports Med. 2009;37(02):376–382. doi: 10.1177/0363546508324971. [DOI] [PubMed] [Google Scholar]
- 14.Sobczak S, Rotsaert P, Vancabeke M, Van Sint Jan S, Salvia P, Feipel V. Effects of proximal row carpectomy on wrist biomechanics: a cadaveric study. Clin Biomech (Bristol, Avon) 2011;26(07):718–724. doi: 10.1016/j.clinbiomech.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 15.Matsuo T, Lai T, Tayama N. Combined flexor and extensor release for activation of voluntary movement of the fingers in patients with cerebral palsy. Clin Orthop Relat Res. 1990;(250):185–193. [PubMed] [Google Scholar]


