Abstract
The advent of hand surgery in India reads like a fortuitous saga, a continuum of the hand deformity correction on leprosy patients pioneered by Dr. Paul Wilson Brand at the Christian Medical College (CMC) Vellore, Madras State (Tamil Nadu [TN]), in 1948. The “Hand Research Unit,” established in 1951, became the largest repository for hand reconstructive surgeries and with its head-start drew in most hand dysfunctions in the country. Early industrialization and disorderly road traffic generated hand injuries that threatened workforce in India. Propitiously, a hand injury service was opened in 1971 at the Government Stanley Medical College Hospital, Chennai. The inexorable growth of hand surgery continued and incorporated the gamut of conditions that required hand care and rehabilitation, including brachial plexus injuries. Continuing Medical Education programs, Hand Surgery workshops, Indian Society for Surgery of the Hand meetings, Hand Fellowships, etc., increased the number of “hand surgery” practitioners, which drew the attention of the Medical Council of India to commence a postgraduate Hand Surgery program that it eventually gazetted. The sagacity of the members of the Board of Studies of TN Medical University honored the historical role of CMC Vellore in hand surgery and allowed it to commence the first Master of Chirurgiae Hand Surgery course in India in 2015. An intuitive understanding of 70 years of hand surgery accomplishments that redesigned and restored deformed and injured hands and protected livelihoods have made young surgeons increasingly take hand surgery as a career.
Keywords: advent, hand surgery, Paul Brand, leprosy hand reconstruction, Hand Research unit, hand injury service, Govt SMCH, TN Medical University, MCh Hand Surgery, career
Introduction
A tidy thatched roof construct within the Bagayam campus of Christian Medical College (CMC) Vellore, India, referred to as “a two room shack” 1 was where Dr. Paul Brand performed the first claw hand corrective surgery on a leprosy patient in 1948. 2 From that momentous event, leprosy deformity corrections in nascent India began transforming the lives of the neglected. 3 With hindsight we realize that hands disabled by any etiology need to be respected and its functionality restored; more so in developing countries where hands are prized as the most basic units of productivity. Dr. Paul Brand was given a challenge forthwith on joining CMC Vellore in 1946 by Dr. Robert G. Cochrane, 4 the Principal of CMC Vellore at the time. He told young Dr. Brand, “Do something to ease the burden of deformities and plantar ulcerations in Leprosy.” Dr. Brand, born in the Kozhimalai Hills of the present Salem District of Tamil Nadu, India, probably grew up observing the suffering of many and resolved to improve the lives of some at a young age.
Dr. Brand ( Fig. 1 ) started his crusade treating plantar ulcerations and launched into correcting hand deformities of leprosy individuals, despite the disease not being under a control regime and its healing potential not so well understood then. He sowed the seeds of scientific hand surgery and contrived the art through meticulous evaluation, accurate record keeping, optimal surgical choice and technique with supervised after-care, and regular follow-up.
Fig. 1.
Dr. Paul W. Brand (July 17, 1914–July 8, 2003). Pioneered hand reconstructive surgery, 1948, Christian Medical College (CMC) Vellore. Founder of first Hand Surgery unit in India (Hand Research unit, CMC Vellore), 1951. Inducted as Hand Surgery Pioneer, 1986.
Hand reconstruction was a successful program at the Hand Research unit (HR unit), CMC Vellore, the first-hand surgery center in India that he founded in 1951. The program was replicated at hospitals across the country, and mission hospitals led the way. Central and state government's leprosy centers—JALMA at Agra, Uttar Pradesh; Chingleput's Leprosy Research and Training Center, Tamil Nadu (TN); Gandhi Memorial Leprosy Foundation Wardha, Maharashtra; etc.—started later and provided additional benefits that accrue from government-associated programs. Reconstructive Surgery workshops were held biannually at the HR unit, CMC Vellore, from the late 1950s (the earliest known hand surgery workshops in India). The Schieffelin Leprosy Research & Training Centre, Karigiri; The Leprosy Mission centers; and central government institutions began workshops a decade later. Steady stream of medical graduates was attracted to this hand surgery training within the country. Brand's extensor four tail transfer procedure using the extensor carpi radialis longus muscle as motor and lengthened with the palmaris longus tendon or fascial lata from the thigh became the workhorse procedure of the time. Subsequently several procedures found their place in claw correction. 5 6
Skilled orthopedic surgeons were the early ones to take up these hand reconstruction programs and enlarged their inventory correcting other hand deformities. Rehabilitation followed every form of care to leprosy patients with vocational rehabilitation being the metaphorical “hill to climb.” Dr. Paul Brand set up the world's first leprosy rehabilitation center in 1954 at the Bagayam Campus, CMC Vellore, India, and named it Nava Jeeva Nilayam or New Life Center. Similar rehabilitation centers came up in other states in the country with the admirable objective of reintegrating the leprosy afflicted into society. The World Health Organization deputed trainees from South Asian, South East Asian, African, and South American nations to the HR unit, CMC Vellore, and then to central government leprosy centers. Dr. Brand's vision was realized over the decades in reducing the incidence of leprosy deformities. 5
The magnitude of programs started and set up to control leprosy and rehabilitate tens of thousands of individuals was largely due to the benevolence of international and national nongovernmental organizations. India is greatly indebted to all of them. The central and state governments played their part in supporting institutions that were initiated through the Directorate General of Health Services (Leprosy) India and World Health Organization support.
Hand injuries increased from the late 1950s disabling hundreds of individuals. Farm-related injuries were humungous. Lesser number of injuries occurred at heavy industries since qualified applicants were screened and provided in-service training, whereas larger numbers of hand injuries occurred in workers of “small and medium scale industries” presumably due to poor qualifications or training. Accidents on single track roads and streets were due to most users being unaware of the rules of the road or ignoring them altogether.
In early times, government clinics and hospitals had the onus to care for hand injuries. But it was not long before patients were noticed receiving inadequate fracture stabilization, poor skin coverage, and left with persisting infections. Physical therapy was not given when needed, although hand therapy with leprosy physiotherapy at the technical level was introduced in 1951 by Dr. Brand and also promoted through a Physiotherapy Technicians Course at HR unit CMC Vellore from 1958. Government hospitals were not programmed that far ahead to assimilate this essential service. Slapdash care and the plight of hand injury patients stirred up concerned surgeons who began instilling scientific approaches to hand injury care to graduating medical students and surgical trainees. Those that led the way were Dr. B.B. Joshi, Mahatma Gandhi Memorial (MGM) Hospital, Parel, Bombay (Mumbai) from the mid-1960s; Dr. R. Venkataswamy, Government Stanley Medical College Hospital (Govt SMCH), Chennai, from 1971; and Prof. A.J. Selvapandian, the HR unit, CMC Vellore, from the late 1950s. Institutions such as Grant Medical College Hospital, Sion Municipal General Hospital, King Edward Memorial Hospital, all in Bombay (Mumbai), Maulana Azad Medical College Hospital, All India Institute of Medical Sciences, and St. Stephens Hospital, all in Delhi, to name a few treated hand injuries guided by the advice of aforementioned stalwarts. Operative Microsurgery launched in late 1970s at the hand injury service of Govt SMCH, Chennai, produced successes in reimplantations and good outcomes in severe hand injuries management.
Setbacks in Early Hand Care
Primary health centers were set up late in post-Independence India in spite of 80% of the population living in villages and over 90% of the citizens accessing government hospital care. The few MBBS—Bachelor of Medicine and Bachelor of Surgery—graduates (referred to as “modern medical graduates” even now) that were selected then, were put off by the frugalities in villages and preferred practice in town and city locales. The “health needs” in Indian villages were taken over by quacks. Bone-setters became the go-to-guys for closed forearm/hand injuries. With temerity, rough-tough straightening of presumed or actual fractured limbs of the hapless or innocent was done followed by wrapping the limb firmly with muslin cloth soaked in white of eggs or green leaf pastes. Consent was nonexistent. Complications were rife. Compartment syndromes and Volkmann's ischemic contracture (VIC) of the hands were commonplace. VIC was their trademark. 7 These miscreants got off unscathed. Such nefarious practices audaciously continued for decades in the country; and thank God, they have dwindled.
Varieties of Hand Problems Treated in Early Times
Hand problems treated in comparatively smaller numbers were: neglected deformities of past injuries and infections, residual paralytic deformities of poliomyelitis, VIC of the forearm and hand, cerebral palsied upper extremity in children, neglected nerve injuries with deformities, and large numbers of pyogenic and granulomatous hand infections. Occasional hand swellings and tumors interrupted the customariness of above conditions.
Congenital hand deficiency and deformities frequented the Departments of Plastic Surgery (DPS) more or less after the mid-1970s at Govt General Hospital, Madras (Chennai); Govt SMCH, Chennai; established Hospitals in Bombay; and All India Institute of Medical Sciences, Delhi. At CMC Vellore, the DPS transferred its responsibility of all hand care to the upgraded HR unit—the Hand and Leprosy Reconstructive Surgery Unitary Department (HLRS)—in 1986. This name change to HLRS in 1984 was at the request of this author owing to the diversity of hand problems being cared for at the time while he was designated the Surgeon-in-Charge of the HR unit.
Gradually better equipment and implants replaced the use of the ubiquitous K-wires with Bunnell's hand drill. Fracture reorganization and carpal fracture management improved around the country and image intensification could not have come at a better time in India. Imaging studies facilitated hand diagnoses from the early 1990s and the cost of care began shooting up. Clinical evaluation got to be partially relegated, but lead clinicians in university hospitals continued their emphasis on Apley's—look, touch, feel, and move sequence of examination—for hand and wrist symptomatology.
From around mid-1960s, neglected peripheral nerve injuries that were becoming fairly common in the country arrived for treatment from distant villages and towns, with the ever-reliable Indian Railways transporting hordes of patients wherever they wished to travel. Centers like HR unit, CMC Vellore, began doing large numbers of muscle transfers/joint stabilizations. To this was added late arrival of brachial plexus injuries (BPIs) for secondary reconstruction.
In 1990, the author introduced and regularized BPIs primary neural surgery in India at the HLRS, CMC Vellore, disseminating the science through integrated course lectures of the Indian Orthopaedic Association and at invited meetings on hand surgery. Neurolysis, fascicular nerve repair, nerve grafting, and nerve transfers were safely done with the operative microscope.
It was in the early 1990s that private hospitals and private clinics made the scene and began to provide good hand injury care. Some centers were even attracted to doing brachial plexus surgery from the mid-1990s in Chennai, Cochin, Coimbatore, Delhi, Hyderabad, Mumbai, Pune, etc. A brachial plexus group was inaugurated in 2002 by Dr. R. Venkataswamy for trainees and colleagues keen to take on and do brachial plexus surgery.
Other Conditions and Procedures
Carpal Trauma
Scaphoid fractures, mostly nonunions (NUs), were not uncommon in the 1980s. The accepted “3-weeks postinjury reimaging-to-confirm #” routine to continue with casting or advising ORIF—open reduction and internal fixation—was ignored. Negligence and missed diagnosis brought in NUs and few centers did internal fixation with bone grafting. 8
In 1991, the author introduced the vascularized bone grafting—VBG (Zaidemberg's 1, 2 intercompartmental supraretinacular artery [ICSRA] or 2, 3 ICSRA vessel choice)—for scaphoid NUs at the HLRS, CMC Vellore. With a good follow-up, it was presented at the Goa Conference of Indian Society for Surgery of the Hand (ISSHCON) in 1998 by Dr. Binu Thomas. This became a worthy take-home message and Indian Society for Surgery of the Hand (ISSH) members began doing them pro re nata . From 1993, the author selectively did the VBG for Lichtman's Stage-2 Kienböck's disease. Carpal dissociations and management were new to most practitioners even up to the early 2000s and selective reconstructions were done. Compression screw fixation for acute and delayed acute scaphoid fractures was started by Dr. Vikas Gupta in Delhi, and few others in India.
Wrist Arthroscopy
Dr. Vikas Gupta in New Delhi, Dr. Abhijeet Wahegaonkar at Pune, Prof. Binu P. Thomas at the HLRS, to name a few, have taken to wrist arthroscopy. It remains in its infancy as an assist for distal radius intra-articular fracture management, repair of scapholunate interosseous ligament tear, or mini-carpal fusions. More hands-on workshops on wrist arthroscopy are expected.
Distal Radioulnar Joint (DRUJ) Arthroscopy and Repair of Triangular Fibrocartilage (TFC)
Although the open triangular fibrocartilage (TFC) complex repair gives good outcomes with insignificant numbers requiring reexploration and TFC ligament reconstruction, arthroscopic repair of TFC is gaining traction. Their outcomes are awaited.
Hand Transplantation
This is the big one with hand surgeons drawing on multispecialty cooperative endeavors. It was first successfully done in Kerala, and much later in few other states, and not so far back at the Institute for Research and Rehabilitation of Hand (IRRH), Chennai. Several factors impact the program: from ideal recipient and a suitable donor limb to overcoming financial constraints, handling psychological problems in the posttransplant period, and prolonged postoperative rehabilitation besides compulsory immunosuppressive therapy intake. India, without a national health system, is hard pressed in advancing hand specialty where exceptional procedures are required but expenses are prohibitive.
Training Abroad
Young postgraduate (PG) surgeons train abroad, to improve their approach and skills in hand surgery. Lots of conditions seen there exist here as well, like basal joint arthritis of thumb for which first CMC joint replacement or ligament reconstruction and tendon interposition or fusions are done as appropriate in centers. Experience can be garnered from consultants and their associates abroad, sometimes even getting to train under master surgeons. The UK is the most favored destination for hand surgery training among Indians. The invited surgeons are given clinical and surgical responsibilities, find accommodation, get a remunerative position (paid Fellowship or by filling up a regular post for a fixed period), etc. Switzerland, Germany, France, Austria, and Italy allow observational training but the courtesies/conveniences come rarely. A good number go to the famous Christine Kleinert Centre for Hand and Microsurgery, Kentucky, USA. Dr. Harold E. Kleinert, a doyen of hand surgery, facilitated this hand training with foresight years ago. Our graduates immensely benefit taking up the 1-year training in this nonprofit education and research organization dedicated to excellence in hand and microsurgery. The support that our surgeons get from Dr. Amit Gupta, MD (an Overseas Citizen of India), a hand surgeon of repute in the USA, serves them well. Few others train in other states of the USA, Canada, Australia, and in the Far East countries: Japan, South Korea, and Taiwan.
A kind of fallibility shadows some of our hand surgery aspirants when they realize that they are not familiar with some basic procedures/techniques. Poor exposure to clinical material, problem solving, being caught up in unmotivating environments with absence of research opportunities, etc. are to blame at home. They return from abroad with greater understanding, better perspective, and determination.
Hand Surgery Education in India
Clinical postings for PG orthopedic diploma and later degree trainees in units where there are orthopedic surgeons with a penchant for hand reconstruction or hand injury care were the earliest known hand surgery education. This was from the mid-1960s. At CMC Vellore, it was a lot easier for the orthopedic PG trainees to be fitted into a 4-week assignment in the HR unit. They handled outpatient departments, did clinical evaluation, provided inpatient care, attended operation theaters (OTs), and took regular on-call duties, besides presenting scientific topics on a regular basis. Master of Chirurgiae (MCh) Plastic Surgery PG trainees had 6 months of posting and Physical Medicine and Rehabilitation PGs 2 months from the early 1990s, and Neurosurgery PGs were given an option to train at the HLRS unitary department.
Postgraduate Fellowship Training in Hand Surgery
In 1999, the author introduced a nouveau academic program in India—the Postgraduate Fellowship in Hand Surgery. There could not have been a more ideal situation than in having widespread hand dysfunctions to care for, and varieties of surgeries to assist in or do: reconstructions, hand trauma management, tumors, peripheral nerve lacerations, compressive neuropathies, carpal dysfunctions, hand-centered plastic surgery, microsurgery complementing hand surgery, brachial plexus surgery, endoscopic carpal tunnel release sporadically, and several miscellaneous conditions, with support of the full-fledged hand therapy section (since 1951 in HR unit, CMC Vellore). The Senatus of CMC Vellore deliberated over the new academic initiative and curriculum. With the approval of the Academic Council, the Dr Paul Brand Postgraduate Fellowship in Hand Surgery was started in 1999. Suitability of MS Orthopedic and MCh Plastic Surgery PGs (and even Diplomate of National Board Orthopedic PGs) was gauged after they were found eligible by clearing an entrance test. This was the “first Fellowship” not just for hand surgery, but for all branches of medical sciences in India. Dr Paul Brand, the legend and founder, formally inaugurated the program on September 1, 2000 ( Figs. 2 and 3 ). The National Board of Examinations (NBE), New Delhi, started a Hand Fellowship 2 years later in 2001 to benefit private hospitals. But the NBE also opened the floodgate to a legion of other Fellowships from then on.
Fig. 2.
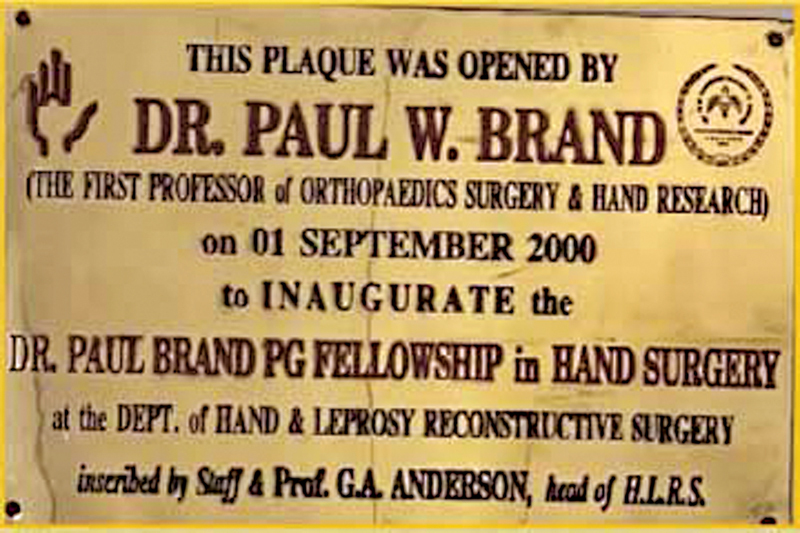
Inauguration of Dr. Paul Brand postgraduate Fellowship in Hand Surgery, Hand and Leprosy Reconstructive Surgery Unitary Department unit aka Hand Research unit, Christian Medical College Vellore, by Dr. Paul W. Brand in September 2000.
Fig. 3.

The Author with Dr. Paul Brand and his wife Dr. Margaret Brand at the front of the plaque of Dr Paul Brand PG Fellowship in Hand Surgery after the inaugural function in September 2000.
MCh Hand Surgery, 3-Year Degree Course
Well-wishers within the country and abroad, several that visited or had done hand training in the HR unit/HLRS unit, CMC Vellore, hoped that a degree course in Hand Surgery could be started. This was in the early years of the new millennium. The Medical Council of India (MCI) studied the need for a PG degree in the hand surgery specialty. The author superannuated in 2010 after 31 years of service and this brought Dr. Binu P. Thomas to the Headship of Dr. Paul Brand Centre for Hand Surgery and Peripheral Nerve Surgery (the name change from HLRS was to honor Dr. Paul Brand after his demise in 2003). Prof. Binu Thomas together with the Principal and Academic Council of CMC Vellore presented the voluminous data in the area of hand surgery at CMC Vellore, since 1951, to the nation's leading scientific and highest medical education authorities for the objective of having a PG degree in Hand Surgery degree program in the country. A positive decision was received with gratitude coming as immense relief to hand surgery academics. The MCI had placed a gazette notification for the MCh Hand Surgery degree to go ahead, provided all the stipulated conditions are met. The Members of the Board of Studies at the TN Medical University with sagacity recognized CMC Vellore's historical role in hand surgery and honored and endorsed the institution commence the first Master of Hand Surgery (MCh Hand Surgery) 3-year degree course in India, which started from September 2015. The author as former Lead Clinician and Head of HR unit/HLRS unitary department and Dr Paul Brand Centre for Hand Surgery and Peripheral Nerve Surgery, in that sequence, inaugurated the course in September 2019 ( Fig. 4 )
Fig. 4.
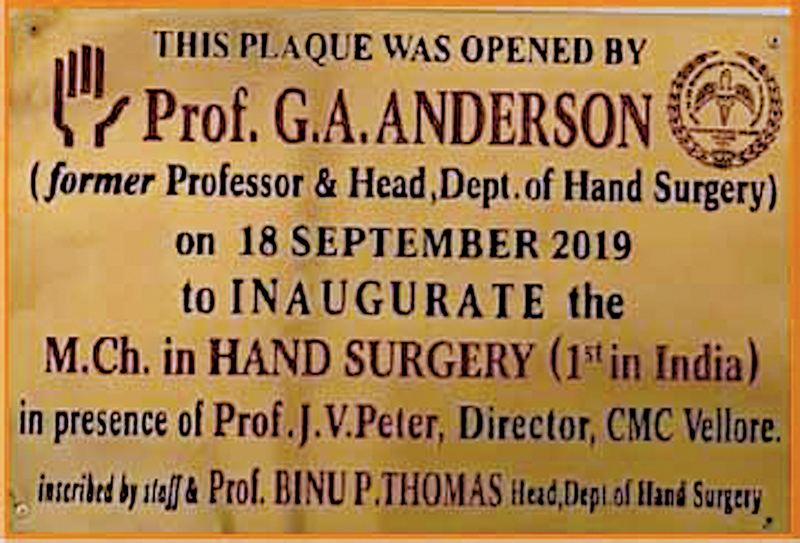
The first MCh Hand Surgery Course in India started in Christian Medical College (CMC) Vellore, September 2015. Inaugurated in September 2019 by Prof. G.A. Anderson, Former Head of Department, Dr. Paul Brand Centre for Hand Surgery and Peripheral Nerve Surgery, CMC Vellore, India.
Hand Surgery Units in Medical Universities
There is need for medical universities in the country to introduce hand surgery units/departments with faculty positions as is done for other surgical specialties that the MCI had endorsed. That the Vice Chancellors of medical universities will be glad to see this through if they are enlightened with the origins and metamorphosis of hand surgery in India as an optimistic thought nurtured by many. The ISSH should now play a big role in seeing this through to benefit the number of eager hand surgeons wishing to serve needy areas and states.
Pioneers of Hand Surgery in India
Dr. Paul W. Brand
Dr. Brand was one in the first List of Pioneers in Hand Surgery. The program of honoring pioneers at the International Federation of Societies for Surgery of the Hand (IFSSH) triennial conferences was only started from 1986 (at the 3rd IFSSH Congress, Tokyo, Japan). The reader is advised to surf the net and open several websites providing information on Dr. Brand's distinguished career, achievements, and honors bestowed on him, and his publications and books written on his vision and life.
Dr. Brij Bushan Joshi
He was inducted as Pioneer in Hand Surgery at the 8th IFSSH Congress, Istanbul, Turkey, 2001.
B.B. Joshi, as he was referred to, was an orthopedic consultant who worked at the MGM Hospital, Parel, Bombay (Mumbai) from about the mid-1960s. Workers from numerous mills and factories in the metropolis with hand injuries were some of his clients. His techniques though simple as they may seem today were innovative, doable, and appropriate for sticky problems he highlighted. Those that trained under him or visited him, like this author in 1985, can vouch for his inventiveness. Some of his pertinent publications were: “The problem of sensory loss in finger-tip injuries in the blind,” 9 “the need for sensory flaps for the degloved mutilated hand,” 10 and “the percutaneous internal fixation of fractures of the proximal phalanges.” 11 He used reusable material to fabricate hand splints, capitalizing on Dr. Paul Brand's method of hand rehabilitation, i.e., in motivating patients treated earlier to make splints under supervision. He brought out his versatile external fixation set JESS—Joshi's external stabilization system—in his postretirement period. B.B. Joshi took every opportunity to demonstrate his passion in caring for injured hands. ( Fig. 5 )
Fig. 5.
Dr. Brij Bushan Joshi (1928–2009). Consultant Orthopedic Surgeon, Mahatma Gandhi Memorial Hospital, Parel, Mumbai, India. Pioneer in Hand Surgery, 2001.
Dr. R. Venkataswamy
He was inducted as Pioneer in Hand Surgery at the 9th IFSSH Congress, Budapest, Hungary, 2004. ( Fig. 6 )
Fig. 6.

Prof. R. Venkataswamy. Former Head, Department of Plastic Surgery, Government Stanley Medical College Hospital, Chennai, Tamil Nadu, India. Started the Institute for Research and Rehabilitation of Hand, Chennai. Served from 1971 to 1991. Pioneer in Hand Surgery, 2004.
Prof. V as he was referred to had been transferred to the Govt SMCH, Chennai, in 1971 to Head the DPS. Burgeoning industrialization in the city and suburbs produced a surfeit of hand injuries. He started an innovative hand injury service, initially admitting patients even on a veranda to tide over the large numbers needing inpatient care. Hand injuries came in 24 × 7 with referrals even from the two other large medical college hospitals in the metropolis at the time. Rotation duty cover was provided by the DPS surgical staff and plastic surgery trainees guaranteeing prompt care. Operative microsurgery in the late 1970s took hand injury management to new heights. 12 Prior to his retirement in 1991, the hand injury service was upgraded to the Institute for Research and Rehabilitation of Hand (IRRH). It remains a boon to all workers within the city, neighboring districts, and even for patients from afar. IRRH Chennai was undoubtedly a trendsetter in the country.
Other Pioneers of Hand Surgery in India are:
Dr. H. Srinivasan, inducted as Pioneer in Hand Surgery, at Sidney, Australia, 2007.
Dr. D.D. Palande, inducted as Pioneer in Hand Surgery, at New Delhi, India, 2013.
Dr. G. Balakrishnan, inducted as Pioneer in Hand Surgery, at Berlin, Germany, 2019.
Achievements of ISSH Members Worthy to be on Record
Prof. Ambrose J. Selvapandian, CMC Vellore, a trusted colleague of Dr. Paul Brand between 1951 and 1965 and Head of the Department (HOD) of Orthopaedics and HR unit, CMC Vellore, from 1966 to 1981, pioneered the Mobile Surgical Program in India largely to do with hand surgery reconstructions. He was the first President of Indian Society of Surgery of the Hand in 1973, and recipient of the BC Roy Award. 13 (The Bidhan Chandra Roy Award was instituted in 1962 in memory of Dr. B.C. Roy by the MCI.)
Dr. Santosh Rath of Odisha obtained his Doctorate (PhD) in 2010 for his research “Early Active Mobilization of Tendon Transfers” 14 from the Erasmus University, Rotterdam, Netherlands. This was in contrast to time honored Paul Brand-E.P. Fritschi-Anderson postoperative hand therapy regime for claw hand correction. 6 15
Indian Society for Surgery of the Hand
The Indian Orthopaedic Association (IOA) started the first Hand Club in India in 1967. Orthopedic surgeons presented hand injuries, VIC, leprosy hand deformity correction, and other hand problems of the time at the Hand Club (Hand Section) sessions of IOA conferences.
Plastic surgeons came into the fold bringing excellent solutions for hand injuries, in particular with Dr. R. Venkataswamy as their “envoy” leading the path in 1971. Senior orthopedic surgeons and plastic surgeons doing hand surgery met (the twain had met) and mooted a hand surgery society in India. Both streams of surgeons at that time in India were either “ in service ” at government hospitals or “ for service ” at multidenominational unaided institutions like CMC Vellore; and enquiring where someone served was more respectful than if they were asked where they “practiced.” But Bob Dylan had already sung “The Times they are a-changin” as early as 1964 and reminded us all what was to come. The former are now practitioners and the latter still “for service.”
On the August 15, 1973, the Indian Society for Surgery of the Hand was inaugurated. Prof. Ambrose J. Selvapandian, HOD Orthopaedics and In-Charge HR unit, CMC Vellore, was the first President of ISSH and Prof. R. Venkataswamy, HOD Plastic Surgery and Hand Injury service at Govt SMCH, Chennai, became the Secretary. Mr. Guy Pulvertaft, Senior Consultant Orthopaedic and Hand Surgeon at the Derby Hand Unit (currently the Pulvertaft Hand Centre, Royal Derby Hospital), England, a Doyen of Hand surgery, presided and did the honors. Prominent ISSH Executive Council members were Drs. Brij Bushan Joshi, A. Sengupta, S.D. Pandey, P.V. Joshi, M.M. Desai, R. Thangaraj, E.P. Fritschi, and H. Srinivasan. The ISSH had its first meeting 6 years later. Its membership numbers have appreciated to almost 1,500 and it holds Continuing Medical Education programs, Workshops, and other academic activities during the year. Two orations in the names of Dr. Venkataswamy and Dr. Brij Bushan Joshi are delivered at the ISSHCONs by surgeons from abroad, some known for excellent work in hand surgery. These orations are a great source of learning for delegates.
12th IFSSH Congress, 2013, New Delhi, India: This was a well-organized and successfully held Congress. Dr. S. Raja Sabapathy, Chief Executive Officer and Consultant Plastic Surgeon at the Ganga Pvt. Hospital Ltd, Coimbatore, TN, took the initiative as a past president of ISSH having announced his decision at the ISSHCON 2010. He set the ball rolling with an energized team. The ISSH members as registered delegates took different responsibilities and probably all were assigned a role as Chair or Co-Chair for scientific sessions.
Aspect of ISSH Membership
Positive developments characterized hand surgery as private hospitals took to doing hand surgery from the early 1990s in India. Private hospital consultants probably make up over 90% of ISSH membership, while university-regulated hospital hand surgery consultants were few to begin with and remain much the same now. The strength in numbers of the former has provided them the opportunity to hold on to and steer the ISSH continuously as office bearers and even otherwise. The constitution of ISSH holds out on university hospital hand surgery department consultants becoming ISSH senior office bearers, despite the several years of membership they hold in the ISSH. The constitution of the ISSH has to be revisited to consider reversing the archaic practice that holds sway. It is hoped that the ISSH will be futuristic and get ahead of the times as do other IFSSH members in their respective societies.
Present-Day Scenario of Hand Surgery in India
The principal driver of hand surgery in India continues to be hand injuries, and the present practice is in dealing with the great many varieties. The endemicity of hand injuries in India, the causation, and the varieties remain sketchy. 16 The ISSH would do well in assigning this as a research project for the ardent young hand surgeon.
University hospitals with hand unit/department continue with fairly adequate clientele; voluntary consultations equal to or greater than referrals. The opposite is probably true for the legion of privately run hospitals that do hand surgery.
Other spread of surgery is for late arriving complicated hand injuries, multiple tendon injuries, nerve lacerations, entrapment neuropathies, adult BPI, obstetrical brachial plexus palsy (OBPP), scaphoid fractures and NUs, and miscellaneous conditions; and relatively smaller number of polyarthritis, scaphoid avascular necrosis, scapholunate dissociation, scaphoid nonunion advanced collapse and scapholunate advanced collapse wrist, Kienböck's disease, DRUJ instability, etc.
A large percentage of road traffic accidents and vehicular impact hand injuries are avoidable. The Union Ministry of Transport put out statistics for the year 2019, where 451,360 were injured on our roads and deaths occurred in about a third of them. 17 The irony is that India had only 1% of the world's vehicle numbers but accounted for 11% of all road accident deaths. It would not be naive in asking whether this carnage will end.
Inner city hospitals scarcely receive severe hand injuries directly because industries have relocated to suburbs. The suburban clinics/hospitals get such cases from villages or small towns and tide over associated crisis and provide primary treatment for the hand injury and then pass them on to the city hospitals. Kharif crop harvesting in the last quarter of the year and Rabi crop harvesting between March and May are the period when workers' hands are more vulnerable. Majority of hand injuries are from threshers, crushers, and other agricultural implements and machinery. Injuries in Deepavali/Diwali—the annual festival of Lights, once associated with hand injuries and burns especially in children due to sparklers, chakkars, flower pots, and even cracker blasts—have reduced considerably through government restrictions in timing of play and use, and regulations imposed on pyrotechniques manufacturers.
Funeral procession cracker blast injury is a whole different animal, an out-and-out heinous accident. As the deceased is taken by a hearse from the house to the pyre, crackers are frequently set off. Thunderous sounds rend the air as though they were packed incendiary devices and momentarily drown the accompanying “death-beat rhythm” of drummers, whistlers, and raucous dancers. So much for customs that become a liability for the innocent. These are some of the worst hand mutilations surgeons may get summoned to treat.
Hand trauma care, delivered through fixed low-tariff rates for the injured arriving within the golden hour, is the brainchild of the Department of Hand Surgery, CMC Vellore. This has really done a world of good for beneficiaries whose livelihood depends on the use of those very hands.
In the Person-to-Person scheme of CMC Vellore, donors help cover the monetary deficits of individuals who receive inpatient care. The beneficiaries remain anonymous to the donor with only the former's social conditions revealed if requested. This is akin to the giver's “left hand not knowing what the right hand is doing.” 18 Many centers have their own ways of handling the cost of care for deserving patients.
External fixation of the hand was popular in the 1990s and only an ardent few get to use it given half a chance. ExFixes prolong duration to recovery, add one or more surgeries to the initial one, bring on joint stiffness with hand therapy requirements lasting weeks, and it is not cost effective. The Graham Lister 19 principle of caring for hand injuries is well practiced in India. Thorough primary care, stabilization and well-vascularized flap cover, and early hand therapy promote the new mantra : “return the hand injured individual as soon as possible to remunerative work.” This is ensconced in responsible hand centers. Excellent work has been done, on mangled hand injuries and the “polytraumatized individuals” with hands that are also injured, by Dr. S. Raja Sabapathy at the Ganga Pvt. Hospital, Coimbatore, TN, besides his success with major reimplantations. 20 21 Major reconstructions are arduous surgical exercises requiring a great deal of effort and team work, and many others adopt the practice around the country. Hand injury care by Dr. Pankaj Jindal, Pune, Dr Shailesh Gupta, Indore, and Dr Sudhir Warrier, Mumbai, to name a few, concentrates on a wide mix of hand injury problems. There is reason to believe that several senior hand surgeons continue efficiently, and maintain competency and high standards in providing the acme of hand injury care.
Unfortunately, there are several “fly by night clinics” (FBNCs) in city fringes and towns purporting to provide statum care. These are young PG surgeons searching for suitable turf to set up camps. Individuals making trips on roads between work/service destinations on two-wheelers may sustain hand injuries due to any one of several reasons; and they make a bee line to the nearest FBNCs and receive quick-fix care. The next day reveals an injured swollen hand, hurting awfully and the patient gets to an “as advertised” hand center, courtesy a Google search. Here the must-pay rule applies with the default regime of charging for just about anything. The insured injured takes this nonchalantly but the uninsured worker is in dire straits. India spent just 1.8% of its gross domestic product on health in 2020 to 2021; it was 1 to 1.5% in the previous years. This is among the lowest any government spends on health in the world. As a result, India is among the top 10 nations with the highest out-of-pocket expenditure. 22 India currently ranks 145 out of 180 countries in quality of and access to healthcare, and 179 of 189 countries in prioritization of health in government budgets. 23 Most hand injuries are sustained by the no-, low-, and middle-income individuals. The need for state governments to run hospitals like the IRRH, Chennai, in each state to provide good hand injury service is very real but grossly wanting.
Brachial plexus surgery has caught the imagination of hand surgeons in many centers for the last 20+ years. Brachial plexus surgical works of Dr. Anil Bhatia, Dr. P.S. Bhandari, 24 Dr. Mukund Thatte, 25 Dr. G. Balakrishnan, Dr. Hari Venkataramani, Prof. Binu Thomas in the DHS, CMC Vellore, to name a few, are impressive. Depending on the level and nature of the plexus injury, explorations, microneurolysis, intercalary fascicular nerve grafting, and selective nerve transfers may be required even on one patient. The author believes in doing it by a well-planned combination of procedures, even if it were to take an hour or two longer. Repeated forays of primary neural surgery are inadvisable. Good team work and planned change in roles for the stages of surgery reduces the fatigue factor. Secondary surgeries for brachial plexus paralysis have been well honed at CMC Vellore from early 1970s, and are done in other centers recently.
Common carpal trauma is handled by hand surgeons who work or visit centers. Equipment and implants may be up to date, and if deficient they summon the instrumentation and implants from vendors, and delivery is done to the OT on the previous evening or even just a few hours before surgery. Hospitals must eschew this practice of using the ad hoc vendor-supplied equipment and implants.
Many hand swellings/tumors are received by hand surgeons provided they escape the man Friday round the corner. Of the essential contingencies there ought to be good support from the Departments of Pathology (tumor division) and Radio Imaging.
As for hand therapy, only few centers have this service. Patients get referred to a “therapist” picked out from a list of names the hospital/clinic has with them. Patients tend to pay more for this service. Few “mobile” therapists have adopted a stratagem of collecting a whole week's charges in advance (supposedly convenient to them and the patient because of dysfunctional point-of-sale machines). That done, the patient goes on a leather hunt trying to pin down this roving therapist for a session! Schadenfreude at miseries befalling hand patients in their vulnerable state is so undesirable.
Employing a social welfare officer in large hand units helps in liaising on behalf of the patient to facilitate smooth return to the former vocation or in adjusting to an alternate job. They also help patients that are uninsured with ways of settling components of the final bill to be paid. Hand centers that are rapacious in their dealing with less affordable individuals could sully the reputation of hand surgery services in the country.
Conclusion
Covering the Hand Surgery India subject narrative of 70 years' duration in a brief or blandly ingratiating way is to do injustice. The readers ought to be cognizant of the vicissitudes of the hand surgery specialty in the largest developing country. There was such strength and courage in the face of adversity in surgeons that combined a vision with passion to make hand surgical science succeed. Dr. Paul Brand's pioneering triple achievement of correcting hand deformities, restoring function, and providing dignity for the leprosy afflicted with hand deformities from 1948 went on to act as a service cue. The surgical skills of Dr. B.B. Joshi, Dr. R. Venkataswamy, and several contemporaries and immediate juniors of the author who find mention here gave their devotion and expertise for managing increasingly difficult conditions. Others who are not mentioned in the write up, to keep down the word count, can be rest assured that they are very much appreciated by the author.
The HR unit, CMC Vellore, was the bellwether for hand surgery in India from 1951, and has stood the test of time. The IRRH, which had begun as a hand injury service at the DPS, Govt SMCH, Chennai, in 1971, has in a way propagated a vital aspect of hand surgery—hand injury management and is the driver of most hand surgery practice. As the ISSH nears its Golden Jubilee celebration on August 23, 2023, it would be ideal if the IRRH Chennai model of hand injury is replicated in other states. This can be best taken up by the ISSH and an exclusive committee be created to see it through. It would be seen as ISSH's most notable achievement in the country since 1973. There is no better way to care for the injured hands of hard-working resident and migrant agrarians and those that toil in MSMEs throughout the country.
It is gratifying to know that OBPP primary neural surgery is done only by a few expert surgeons in India who are doing a commendable job. It is wiser for those who are keen, to become consistently successful doing adult BPI primary surgery.
ISSHCON proceedings are required to be brought out after every annual meet. Together with that, a white paper can be drawn up on the contemporary management of common hand conditions for the benefit of the junior colleagues.
Young colleagues must follow a failsafe and trouble-free practice at the outset, since some have (inadvertently) displayed elements of incomplete care, letting down the Fellowship apprenticeship they had gone through. It is good to remember that a hand surgeon's skill is under the scanner every time he treats another hand, whatever the problem.
Higher education in hand surgery has reached a high point with conferring of the MCh Hand Surgery degree after a 3-year period of intense training. The starting of hand surgery units/departments at every medical university in the country is reiterated as a worthy pursuit to build up a faculty proficient in spreading care and efficient in treating patients, besides research. The ISSH office bearers, past and present, with the good offices of hand surgery pioneers could devote their time to getting this “done” by the ISSH Golden Jubilee year 2023.
Senior members need to add to the body of hand surgery knowledge of India in international journals, especially since India has for well over a decade a journal that it can be proud of, the Journal of Hand and Microsurgery (JHAM), which has a good spread of excellent contributions from the Far East, South East Asia, South Asia, and the Middle East.
Most senior hand surgeons have all the scientific material they need, but the bulk of them run private hospitals or clinics in India, with the pecuniary angle of practice dominating their career. And probably for the same reason, clinical and basic sciences research in hand surgery lags behind.
The author with 40 years of hand surgery experience in the country holds firmly to the belief that whatever the circumstances, the ascendency to greater heights in hand science with a perennially better quality of hand care is ensured for now and the future.
Footnotes
Conflict of Interest None declared.
References
- 1.Hunter J M, Schneider L H, MaCkin E J, Bell J A. St. Louis: The CV Mosby Company; 1978. Rehabilitation of the Hand. Dedicated to Dr Paul W. Brand, p. ix. [Google Scholar]
- 2.Brand P W. The reconstruction of the hand in leprosy. Ann R Coll Surg Engl. 1952;11(06):350–361. [PMC free article] [PubMed] [Google Scholar]
- 3.Brand P W. Treatment of leprosy. II. The role of surgery. N Engl J Med. 1956;254(02):64–67. doi: 10.1056/NEJM195601122540205. [DOI] [PubMed] [Google Scholar]
- 4.Cochrane R G, Davey T F. Bristol: John Wright and Sons Ltd; 1964. Leprosy in theory and practice; pp. 447–467. [Google Scholar]
- 5.Anderson G A. The surgical management of deformities of the hand in leprosy. J Bone Joint Surg Br. 2006;88(03):290–294. doi: 10.1302/0301-620X.88B3.17100. [DOI] [PubMed] [Google Scholar]
- 6.Anderson G A.Ulnar Nerve Palsy. Green's Operative Hand Surgery, 5th edition London: Elsevier; 2005. Chapter 33, 1167-93 [Google Scholar]
- 7.Anderson G A.Child's hand in the developing world London: Mosby-Wolfe; 2000. Section 20, Chapter 114, 1097-1114 [Google Scholar]
- 8.Anderson G A, Thomas B P. Non-union of Scaphoid Fractures: Treatment by the Fisk-Fernandez Technique. Ind Jl Orth. 2000;34(04):275–279. [Google Scholar]
- 9.Joshi B B. Problem of sensory loss in finger-tip injuries in the blind. Br J Plast Surg. 1970;23(03):283–284. doi: 10.1016/s0007-1226(70)80056-x. [DOI] [PubMed] [Google Scholar]
- 10.Joshi B B. Sensory flaps for the degloved mutilated hand. Hand. 1974;6(03):247–254. doi: 10.1016/0072-968x(74)90035-7. [DOI] [PubMed] [Google Scholar]
- 11.Joshi B B. Percutaneous internal fixation of fractures of the proximal phalanges. Hand. 1976;8(01):86–92. doi: 10.1016/0072-968x(76)90069-3. [DOI] [PubMed] [Google Scholar]
- 12.Venkataswamy R.Staged neurovascular island flap from the middle finger to the thumb tipBoston: Little Brown & Co.1990892–894. [Google Scholar]
- 13.Anderson G A.Ambrose J Selvapandian: ObituaryInd Jl Ortho2011
- 14.Rath S. Immediate postoperative active mobilization versus immobilization following tendon transfer for claw deformity correction in the hand. J Hand Surg Am. 2008;33(02):232–240. doi: 10.1016/j.jhsa.2007.10.012. [DOI] [PubMed] [Google Scholar]
- 15.Fritschi E P. Bristol: John Wright; 1971. Reconstructive Surgery in Leprosy. [Google Scholar]
- 16.Panse N, Sahasrabudhe P. Hand injury prevention in India: are we doing enough? Indian J Plast Surg. 2011;44(03):532. doi: 10.4103/0970-0358.90861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Government of India, Ministry of Road Transport & Highways; Annual Report 2018–2019. [Google Scholar]
- 18.Gospel according to St. Matthew; chapter 6, verse 3New KJV
- 19.Rockwell W B, Lister G D. Soft tissue reconstruction. Coverage of hand injuries. Orthop Clin North Am. 1993;24(03):411–424. [PubMed] [Google Scholar]
- 20.Sabapathy S R, Venkatramani H, Bharathi R R, Dheenadhayalan J, Bhat V R, Rajasekaran S. Technical considerations and functional outcome of 22 major replantations (The BSSH Douglas Lamb Lecture, 2005. J Hand Surg Eur Vol. 2007;32(05):488–501. doi: 10.1016/J.JHSE.2007.06.013. [DOI] [PubMed] [Google Scholar]
- 21.Sabapathy S R, Venkatramani H, Bharathi R R, Bhardwaj P. Replantation surgery. J Hand Surg Am. 2011;36(06):1104–1110. doi: 10.1016/j.jhsa.2011.03.039. [DOI] [PubMed] [Google Scholar]
- 22.Kaur B.Union Budget 2021–22: how good is the hike in allocation for health? InDown to Earth01/02/2021
- 23.Sinha D.Economy, Government, Heath. Explained: Despite Govt Claims, India's Health Budget Only Around 0.34% of GDP, In The WIRE01/02/2021
- 24.Bhandari P S, Sadhotra L P, Bhargava P et al. Surgical outcomes following nerve transfers in upper brachial plexus injuries. Indian J Plast Surg. 2009;42(02):150–160. doi: 10.4103/0970-0358.59272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thatte M R, Agashe M V, Rao A, Rathod C M, Mehta R. Clinical outcome of shoulder muscle transfer for shoulder deformities in obstetric brachial plexus palsy: a study of 150 cases. Indian J Plast Surg. 2011;44(01):21–28. doi: 10.4103/0970-0358.81441. [DOI] [PMC free article] [PubMed] [Google Scholar]


