Key Clinical Message
In this case report, total knee arthroplasty was performed in a patient with pigmented villonodular synovitis. During surgery, severe black discoloration of the articular cartilage and menisci was observed in the patient. According to literatures, this is the first case report of severe articular cartilage pigmentation in a patient with pigmented villonodular synovitis.
Keywords: black cartilage, black menisci, case report, PVNS, total knee arthroplasty
1. INTRODUCTION
Mild discoloration of the articular cartilage is widely accepted to occur with age. However, pathological pigmentation of the articular cartilage and meniscus can occur in certain conditions in patients, such as alkaptonuria (ochronosis), 1 , 2 chronic phenol poisoning, 3 artifacts, 3 burns, 3 hemosiderosis, 4 Parkinson's disease medications, 5 some antibiotics, 6 , 7 and hydroquinone.
In the present case report, total knee arthroplasty (TKA) was performed in a patient with pigmented villonodular synovitis (PVNS). During the surgery, severe black discoloration of the articular cartilage and menisci was observed. To our knowledge, this is the first report of black pigmentation of the articular cartilage and menisci in a patient with PVNS.
2. CASE REPORT
The patient was a 64‐year‐old woman with a 2‐year history of right knee pain and swelling without any traumatic injury. Physical examination revealed joint line tenderness and limited range of motion; however, despite conservative treatment, knee pain and swelling persisted. Clinical evaluation revealed acceptable hip‐knee‐ankle alignment. The patient had diabetes mellitus and received metformin.
Radiographic evaluation revealed joint space narrowing, subchondral sclerosis, and osteophyte formation (Figure 1). Furthermore, complete blood count values; erythrocyte sedimentation rates; C‐reactive protein, alanine transaminase, and aspartate transaminase levels; and activated partial thromboplastin and prothrombin times were all within the normal range. Physical examination revealed that a part of the patient's knee was swollen and had a rubbery consistency; therefore, knee magnetic resonance imaging (MRI) was performed to detect a possible lesion.
FIGURE 1.

Hip‐knee‐ankle radiographic with joint space narrowing, subchondral sclerosis, and osteophyte formation.
MRI showed knee joint effusion with a popliteal cyst and internal debris located posteriorly, suggesting the possibility of PVNS (Figure 2).
FIGURE 2.
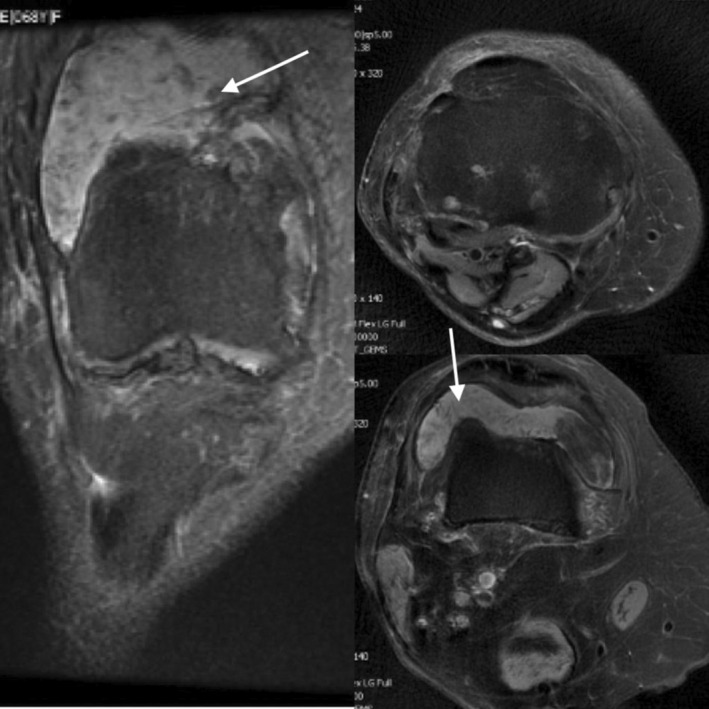
Knee joint effusion and popliteal cyst with internal debris which located posteriorly, suggesting the possibility of pigmented villonodular synovitis (PVNS).
Although there are different treatment options for PVNS, TKA with total synovectomy was selected owing to the patient's age and presence of cartilage destruction on radiography and MRI.
Cemented right TKA was performed under spinal anesthesia by using a cemented posterior‐stabilized prosthesis (Stryker Triathlon® Total Knee System). The right knee articular cartilage was exposed using the medial parapatellar approach, which revealed severe black pigmentation of the synovial membrane and menisci, and pigmentation of the articular surface (Figure 3). The articular surface was eroded, and a small part of the subchondral bone of the medial femoral condyle was visible. After the femoral condyle was cut, pigmentation was found to be localized in the cartilage layer. Total synovectomy was performed, and the synovial and popliteal fossa mass biopsy specimens were analyzed.
FIGURE 3.

Severe black pigmentation of the synovial membrane and menisci and pigmentation of the articular surface.
Postsurgical radiographic and clinical examination results were acceptable, and there were no intraoperative or perioperative complications (Figure 4).
FIGURE 4.

Postsurgical radiographic with acceptable alignment.
Diagnosis was confirmed by histopathologic evaluation, which revealed a tenosynovial giant cell tumor (PVNS; Figure 5).
FIGURE 5.

The lesion is composed of papillary, villous, nodular, and pseudoglandular or cleft like spaces with a synovial lining. Osteoclast‐like multinucleated giant cells and hemosiderin‐laden macrophages are seen. Histopathologic evaluation is compatible with pigmented villonodular synovitis (PVNS).
According to the literatures, this is the first report of severe articular cartilage pigmentation in a patient with PVNS.
The patient was followed up for 14 months, during which time she was free of complications.
3. DISCUSSION
Pigmented villonodular synovitis is a proliferative disorder of the synovium with locally aggressive nature, and its etiology is unclear, although neoplasm, recurrent hemorrhage, and trauma have been reported as possible causes. 8 , 9 To our knowledge, there are no reports of severe articular surface, synovial, and meniscal pigmentation in patients with PVNS; however, certain conditions have been reported to cause severe articular cartilage and meniscal pigmentation abnormalities in patients, such as alkaptonuria (ochronosis) and use of antibiotics and drugs such as levodopa and methyldopa. 1 , 2 , 3 , 4 , 5 , 6 , 7
In 2016, Matsumoto et al. reported black discoloration of the knee articular cartilage after spontaneous recurrent hemarthrosis in a patient and concluded that hemosiderin and lipofuscin accumulation due to recurrent hemarthrosis might increase black pigmentation of joint cartilage. 9 They roll outed specific condition by histopathological examination. 9
Patients with PVNS commonly present with hemarthrosis 10 ; therefore, it is reasonable that recurrent hemarthrosis in patients with PVNS could cause articular surface and meniscal pigmentation owing to hemosiderin and lipofuscin accumulation and combination.
4. CONCLUSION
To our knowledge and according to the literatures, this is the first report of severe black pigmentation of the articular cartilage and menisci in a patient with PVNS. Based on report of black discoloration of the knee articular surface by Matsumoto et al, 9 we hypothesize that recurrent hemarthrosis in patients with PVNS could result in severe articular and meniscal pigmentation owing to hemosiderin and lipofuscin accumulation.
AUTHOR CONTRIBUTIONS
Mohammad Ayati Firoozabadi: Conceptualization; project administration; writing – review and editing. S. M. Javad Mortazavi: Supervision. Hesam Toofan: Data curation. Marzieh khalili: Data curation; visualization. Mohammad Javad Shariyate: Writing – original draft.
FUNDING INFORMATION
This study had no financial support.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflict of interests.
CONSENT STATEMENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Firoozabadi MA, Mortazavi SMJ, Toofan H, Khalili M, Shariyate MJ. Black discoloration of the knee articular cartilage in a patient with pigmented villonodular synovitis: A case report. Clin Case Rep. 2023;11:e7894. doi: 10.1002/ccr3.7894
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request. More detailed data are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Kara A, Celik H, Seker A, Sezer HB, Kilinc E, Uzun M. Ochronosis diagnosed after knee arthroscopy. Int J Surg Case Rep. 2014;5(8):497‐499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Raaijmaakers M, Steenbrugge F, Dierickx C. Ochronosis, arthroscopy of a black knee: a case report and review of the literature. Knee Surg Sports Traumatol Arthrosc. 2008;16(2):182‐184. [DOI] [PubMed] [Google Scholar]
- 3. Sudesh G. Pigmentation of articular surfaces of bones as an identification factor: a unique case report. Am J Forensic Med Pathol. 2006;27:161‐162. [DOI] [PubMed] [Google Scholar]
- 4. Lee CA, Kessler CM, Varon D, et al. Synovium in haemophilic arthropathy. Haemophilia. 1998;4(4):502‐505. [DOI] [PubMed] [Google Scholar]
- 5. Connolly CE, O'Reilly U, Donlon J. Black cartilage associated with levodopa. The Lancet. 1986;327(8482):690. [DOI] [PubMed] [Google Scholar]
- 6. Reed DN, Gregg FO, Corpe RS. Minocycline‐induced black bone disease encountered during total knee arthroplasty. Orthopedics. 2012;35(5):e737‐e739. [DOI] [PubMed] [Google Scholar]
- 7. Middleton SD, Anakwe RE, McKinley JC. Black bone disease of the foot. Minocycline related pigmentation. Foot Ankle Surg. 2011;17:e34‐e36. [DOI] [PubMed] [Google Scholar]
- 8. Miller WE. Villonodular synovitis: pigmented and nonpigmented variations. South Med J. 1982;75:1084‐1086. [PubMed] [Google Scholar]
- 9. Matsumoto K, Ishimaru D, Ogawa H, Akiyama H. Black colouration of the knee articular cartilage after spontaneously recurrent haemarthrosis. Case Rep Orthop. 2016;2016:12‐14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nagai K, Matsumoto T, Matsushita T, et al. Spontaneous recurrent hemarthrosis of the knee joint in the elderly: a report of two cases. J Orthop Sci. 2012;17:649‐653. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request. More detailed data are available from the corresponding author upon reasonable request.


