Abstract
Objective:
The purpose of this systematic review is to broaden our knowledge of colorectal cancer (CRC) screening in South Asian immigrants living in Canada, Hong Kong, the United Kingdom, the United States, and Australia by determining the barriers and facilitators and examining interventions for CRC screening.
Methods:
A literature search of PubMed, Ovid Medline, and Google was conducted using South Asian, Asian Indians, cancer screening, colorectal neoplasm, early detection of cancer, and mass screening as search terms. The review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Only research articles written in English from 2000 to July 2022 were collected. Inclusion criteria included all English-language articles, the South Asian population, and either reporting barriers, facilitators, interventions, or recommendations for CRC screening. Exclusion criteria included all articles that did not meet inclusion criteria or were duplicates. A total of 32 articles were deemed eligible for inclusion and were retrieved for further analysis. The countries of origin in the articles reviewed included Canada, Hong Kong, the United Kingdom, the United States, and Australia.
Results:
In general, the studies indicated that South Asians have low CRC screening rates. The most common barriers reported were poor knowledge/awareness of CRC and CRC screening, lack of physician recommendation, psychological factors (e.g., fear, anxiety, and shame), cultural/religious factors, and sociodemographic factors (language barrier, lower income, and female gender). The most important facilitator reported was the physician’s recommendation. Six intervention studies of either education or organized screening programs were shown to have a positive influence by increasing knowledge and improving attitudes toward CRC screening.
Conclusion:
Of the limited number of studies identified, the population categorized as South Asians was largely heterogeneous, including a diversity of ethnicities. Although the rates of CRC among South Asians were relatively low, there remain many cultural barriers to the awareness of and screening for CRC in this population. Further research in this population is needed to better identify the factors related to CRC in individuals of South Asian ethnicity. Recommending CRC screening by physicians and mid-level providers and educating patients with culturally sensitive programs and materials are important to increase knowledge and awareness of CRC and CRC screening.
Key Words: Colorectal cancer, screening, South Asians, review
Introduction
Colorectal cancer (CRC) is the third most common cancer (1.93 million annual cases) and the second most common cause of cancer death (935,000 annual deaths) worldwide (National Cancer Institute, 2021). Early detection through screening is crucial in reducing mortality, morbidity, and treatment costs associated with CRC (Schreuders et al., 2015; Simon, 2016). Since CRC is a preventable cancer that meets the criteria for appropriate screening, it is essential to increase screening rates, particularly in high-risk groups (Beck, 2015). The United States Preventive Task Services Force (USPSTF) recommends screening for CRC in all adults aged 50 to 75 years, either annually by stool-based tests with high sensitivity (fecal occult blood testing [FOBT]/fecal immunochemical testing [FIT]), every 5 years by flexible sigmoidoscopy (FSIG), or every 10 years by colonoscopy (USPSTF, 2021).
The South Asian immigrant population is one of the fastest-growing racial and ethnic groups in the United States and Canada (Statistics Canada, 2018; Jones et al., 2021). A recent survey reported an estimated 4.6 million Asian Indians living in the United States, the second largest Asian population after those of Chinese origin (Pew Research Center, 2021). In Canada, South Asians are the largest minority group, estimated to represent 28% of the visible minority population by 2031 (Statistics Canada, 2018). South Asians also comprise the largest ethnic group in the United Kingdom (Glenn et al., 2009). While CRC rates are generally low among South Asians, studies indicate that CRC incidence rates increase with time spent in the settlement country and approach rates of natives in the settlement country (Jain et al., 2005; Hislop et al., 2007; Rastogi et al., 2008). However, studies have documented disparities in CRC screening for South Asian immigrants (Wong et al., 2005; Lee et al., 2011). Moreover, health information related to CRC screening for the South Asian population is limited because of the paucity of studies on this population and the aggregation of South Asian with other Asian groups in population-based health statistics (Menon et al., 2014). For example, the term “Asian” commonly encompasses Chinese, Filipino, Vietnamese, Korean, and Japanese. Furthermore, research on preventive health interventions in South Asians (including those with origins in India, Pakistan, Bangladesh, Bhutan, Nepal, or other countries in the diaspora) is lacking (Crawford et al., 2015; Kazi et al., 2021).
The aim of this clinical review is to broaden the knowledge of CRC screening in South Asian immigrants. This clinical review, therefore, identifies barriers (i.e., factors that decrease the likelihood of screening) and facilitators (i.e., factors that increase the likelihood of screening) to CRC screening among South Asian immigrants. The review also reviews interventions and recommendations to increase screening rates. Findings from this review would improve screening rates and reduce disparities in CRC outcomes among this population.
Materials and Methods
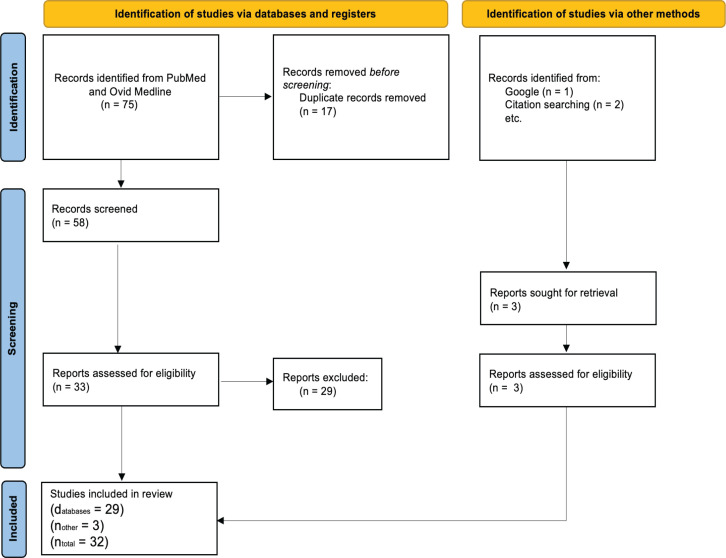
The systematic review was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses as a guide. The identification of relevant studies began with systematic searches using PubMed and Ovid Medline. The search covered the period up to July 2022 and employed keywords such as “colorectal cancer screening,” “South Asian,” and “Asian Indians.” The following MeSH terms were used: “colorectal neoplasm,” “early detection of cancer,” and “mass screening.” The search yielded 75 articles: 33 from PubMed and 42 from Ovid Medline.
Inclusion criteria included English-language articles published between 2000 and 2022, focusing on the South Asian population, and reporting barriers, facilitators, or interventions for CRC screening. Exclusion criteria included duplicate articles and those that did not meet the inclusion criteria. After removing duplicates, 49 articles were included for further screening for eligibility. Three more articles were identified through other methods as follows: One abstract (Khokhar et al., 2009) was found through a Google search on “Barriers to Colorectal Cancer Screening in South Asians,” and two articles were identified from citation (Figure 1).
Figure 1.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses Flow Diagram
Two investigators initially screened the articles to determine their relevance to the study question and purpose. Each article was subsequently presented to the other reviewer for further assessment of appropriateness for inclusion or exclusion. The principal investigator remained available to address any disagreements that might arise between the reviewers. After evaluation, 32 articles were deemed eligible for inclusion in the study. The data collected included participant demographics, screening rates, barriers, facilitators, and interventions.
Results
CRC Screening
The findings of several studies (Thompson et al., 2014; Blanks et al., 2015; Choi et al., 2015; Sy et al., 2018; Rastogi et al., 2019; Campbell et al., 2020; Wyatt et al., 2022) revealed that South Asians had lower CRC screening rates than other populations. However, in Wong et al.’s (2005) study, South Asians did not have the lowest CRC screening rate (Ever screened: FOBT 32%, endoscopy 41%, and any screening: 53%; Up to date: FOBT 21%, endoscopy 39%, and any screening 48%) compared with other ethnic groups. Koreans had the lowest CRC screening rates (Ever screened: FOBT 23%, endoscopy 38%, and any screening: 49%; Up to date: FOBT 12%, endoscopy 34%, and any screening 41%). Another study by Glenn et al. (2009) reported heterogeneity among CRC screening rates in South Asian subgroups: Indian (25%), Pakistani (37%), Bangladeshi (17%), and Sri Lankan (68%).
Knowledge of CRC and CRC Screening/Awareness
Poor knowledge of CRC and CRC screening/awareness was commonly associated with lower CRC screening rates among South Asians (Khokhar et al., 2009; Choi et al., 2015; Crawford et al., 2015; Manne et al., 2015; Palmer et al., 2015; Ivey et al., 2018; Kazi et al., 2021; Patel et al., 2021). Recently, Patel et al. (2021) reported that a lack of information and knowledge regarding CRC and CRC screening is the most frequently cited cultural challenge factor. In another study by Manne et al. (2015), the level of awareness of CRC screening among individuals in the South Asian population was relatively low: 54.6% had never heard of FOBT, 73.9% had never heard of FSIG, 31% had never heard of colonoscopy, and 29.5% had never heard of any of these tests. Compared with white British adults, South Asians in the United Kingdom showed a pronounced lack of knowledge about CRC screening (Robb et al., 2008).
Health Care Factors
Health care factors that can influence CRC screening include physician recommendations, frequency of physician visits, and insurance coverage. A lack of physician recommendation was reported as a barrier to CRC screening in three studies (Choi et al., 2015; Kazi et al., 2021; Patel et al., 2021) and one abstract (Khokhar et al., 2009). In Kazi et al.’s (2021) study, the participants’ top reason for not receiving CRC screenings was a lack of communication from physicians regarding the necessity of screening (7 out of 31 participants). In contrast, five studies (Choi et al., 2015; Crawford et al., 2015; Ivey et al., 2018; Kazi et al., 2021; Patel et al., 2021) identified physician recommendations as a facilitator for CRC screening. Patel et al. (2021) revealed that physician referrals were the most significant facilitator for CRC screening. Participants of both genders mentioned that physicians play a key role in encouraging CRC screening uptake (Kazi et al., 2021). Furthermore, Choi et al. (2015) found that health professionals’ recommendations were the only factor that significantly interacted with ethnicity in relation to facilitating CRC screening. Lofters et al. (2015) identified physician characteristics that acted as barriers to CRC screening, such as trained South Asian physicians, Caribbean/Latin American-trained physicians, and shorter time in independent practice. However, in the same study, physicians who were Canadian graduates, Eastern European trained, or had more experience contributed to higher CRC screening rates (Lofters et al., 2015).
In addition, the frequency of physician visits was positively associated with CRC screening (13%–22% increase in CRC screening per visit in the last 2 years; Wong et al., 2005; Thompson et al., 2014). A lack of insurance coverage was cited as a barrier to CRC screening in four studies (Ivey et al., 2018; Kazi et al., 2021; Patel et al., 2021; Mukherjea et al., 2022). Conversely, having insurance was identified as a facilitator for CRC screening in six studies (Wong et al., 2005; Glenn et al., 2009; Sy et al., 2018; Kazi et al., 2021; Mukherjea et al., 2022; Wyatt et al., 2022).
Cultural and Psychological Factors
Four studies (Robb et al., 2008; Crawford et al., 2015; Kazi et al., 2021; Patel et al., 2021) cited psychological factors as barriers to CRC screening. These psychological barriers include anxiety, fear, embarrassment, and the perceived shame associated with CRC screening and diagnosis. Almost half of the participants in one study (Patel et al., 2021) reported shame/discomfort and embarrassment associated with CRC and CRC screening in their communities. One participant in the study thought the cause of CRC “may be dirty things, dirty people,” and another participant stated, “a lot of people feel ashamed…for this reason they don’t do it.” However, despite these barriers, the benefits of CRC screening are widely acknowledged (Manne et al., 2015).
Cultural and religious aspects have also been identified as factors influencing CRC screening (Campbell et al., 2020; Ivey et al., 2018; Kazi et al., 2021; Patel et al., 2021; Khokhar et al., 2009). For example, fatalism was cited in three studies (Ivey et al., 2018; Kazi et al., 2021; Patel et al., 2021) as a barrier to CRC screening, with participants stating that they had no control over cancer or when they were going to die. In Kazi et al.’s (2021) study, female participants expressed concerns about the cultural and religious stigma of stool tests, emphasizing that stool is unclean and dirty. Kazi et al. (2021) also reported that immigrants who do not have a culture of annual exams in their native countries hold the same attitudes in the USA. Ivey et al. (2018) found that some female participants hold cultural preconceptions that chronic diseases are more prevalent in men.
Sociodemographic Factors
The most common sociodemographic factors identified as barriers to CRC screening included gender, length of stay, education, language barrier, and socioeconomic status.
Gender
Three studies (Glenn et al., 2009; Campbell et al., 2020; Kazi et al., 2021) showed that South Asian women are less likely than men to undergo CRC screening. This was attributed in one study to modesty and feelings of shyness regarding the exposure of private body parts to a male physician (Kazi et al., 2021). However, Wong et al. (2005) found that males were significantly less likely to ever receive FOBT CRC screenings (OR, 0.90; 95% CI, 0.83–0.97) but were more likely to be up to date on colonoscopies. Negative attitudes toward CRC screening were also found to be more prevalent among men (OR: 1.66; CI 1.47-1.88). The odds of undergoing CRC screening were shown to be higher among females in one study (Sy et al., 2018), but were higher among males in another (Lofters et al., 2015).
Length of Stay
The length of stay in the United States for South Asian immigrants affects their likelihood of undergoing CRC screening. Shorter lengths of stay were associated with lower CRC screening rates among South Asian immigrants in the United States (US). Rastogi et al. (2019) found that those who had lived in the US for less than 5 years had an odds ratio of 0.44 (95%, CI 0.22–0.87) of up-to-date colonoscopy. Wong et al. (2005) showed that South Asian immigrants who had lived in the US for less than 15 years had an odds ratio of 0.56 (95%, CI 0.38-0.83) of ever having FOBT screening for CRC. Manne et al. (2015) also reported that living in the US for less than 5 years was connected to decreased CRC uptake. Mukherjea et al. (2022) showed non-adherence (not being up to date) to CRC screening to be higher in immigrants with less than 40% of their life spent in the US. Living in the United States for at least 5 years was linked to a ninefold increase in the likelihood of having an endoscopic screening test compared with living in the US for less than 5 years (Menon et al., 2014). An explanation suggested that it takes at least 5 years to obtain a permanent resident (“green”) card, which allows eligibility for free or subsidized healthcare. Finally, non-adherence to CRC screening guidelines was lower among South Asians who had lived in the US for > 60% of their life (Mukherjea et al., 2022).
Education
Higher education was identified as a facilitator of CRC screening (Wong et al., 2005; Wyatt et al., 2022). Menon et al. (2014) also found that individuals who received sigmoidoscopy were more likely to have at least a high school education (X22 = 8.72, P G = .05).
Language Barrier
Language is a key factor associated with CRC screening, especially in English-speaking countries (Menon et al., 2014; Thompson et al., 2014; Manne et al., 2015; Mukherjea et al., 2022, Palmer et al., 2015; Rastogi et al., 2019). Thompson et al. (2014) found that patient-physician language discordance significantly decreased the odds of CRC screening (concordant: OR, 0.94; CI, 0.77-1.15; discordant: OR, 0.79; CI, 0.72-0.87). Non-adherence (not being up to date) to CRC screening by USPSTF guidelines was lower among South Asians who spoke English at home (Mukherjea et al., 2022).
Socioeconomic Status
Poverty level and employment status were identified as factors commonly associated with CRC screening rates. Unemployed or retired Asian Indians were less likely to get screened for CRC compared with their employed counterparts (OR: 0.65; Sy et al., 2018). Low income was described as a barrier to CRC screening in six studies (Wong et al., 2005; Blanks et al., 2015; Lofters et al., 2015; Manne et al., 2015; Orbell et al., 2017; Rastogi et al., 2019). Menon et al. (2014) found that income was a predisposing predictor of endoscopic cancer screening (AOR, 2.7; CI, 1.0-7.1). Moreover, Orbell et al. (2017) discussed that nonparticipation in FOBT uptake showed a linear association across the distribution of SES, with rates across five quintiles (most deprived to least deprived) of 29.8%, 24.4%, 21.3%, 23%, and 18%.
Interventions
In this review, ten articles related to interventions were examined (Table 2). Six of the intervention studies were based on education (Wu et al., 2010; Cullerton et al., 2016; Lofters et al., 2017; Mukherjea et al., 2020; Manne et al., 2021; So et al., 2022). The implementation of various interventions for increasing CRC screening has been shown to have positive effects on screening behavior. Cullerton et al. (2016) stressed that culturally tailored educational programs improve attitudes and increase knowledge of CRC and intent toward CRC screening. In the study, prior to the session, only 25% of participants reported an intent to undergo FOBT screening, whereas after the session, this number increased to 49% (Cullerton et al., 2016). Manne et al.’s (2021) study included one-on-one sessions that were highly rated by participants. The intent-to-treat analysis showed a 30% uptake in CRC screening at the four-month follow-up, along with an increase in knowledge and a reduction in barriers to screening, such as worry about the screening process. Physician-led presentations on CRC screening (Mukherjea et al., 2020) were shown to have a positive impact on those who had not previously been screened, with 87% of participants expressing a high intent to get screened after the presentation (103 participants, 48% never screened). The distribution of culturally sensitive brochures (Mukherjea et al., 2020) has been shown to increase awareness of CRC screenings among family and friends. So et al. (2022) showed that a multifaceted intervention consisting of a CRC screening presentation by a trained instructor, distribution of booklet information translated into different languages, and targeting younger family members in encouraging their older family members to undergo CRC screening resulted in higher FIT rates among participants in the intervention group compared to the control group (71.8% vs. 6.8%, p<0.001). Community-based education events have also been effective in increasing knowledge and improving attitudes toward CRC screening. A follow-up conducted 6-12 months after the intervention showed that 78% of those who received the intervention had been screened in the last 12 months, whereas only 37% were screened for CRC with any tests prior to the intervention (Wu et al., 2010). In another study by Lofters et al. (2017), health ambassadors (HA) making phone calls to patients who were overdue for CRC screening at Physicians 1, 2, and 3 offices showed greater success in reaching a larger population compared to having HA provide education at physician’s offices. However, at Physician 4 office, one-on-one education by HA showed that 65.2% of the patients spoken to were willing to be screened.
Table 2.
Intervention Studies
| Reference | Location | Study design | Population/screening rate | Intervention | Finding |
|---|---|---|---|---|---|
| Cullerton et al. (2016) | Australia - Queensland | Pre- and post-education evaluation sessions | 159 | Culturally tailored cancer education pilot program | Knowledge increased, attitude toward participation became more positive, intent to screen increased |
| Crawford et al. (2017) | UK, US, and Canada | Mixed methods study | N/A | Identifying best survey metrics that may predict colorectal cancer screening outcomes utilizing data from prior scoping and focus group studies | Optimal survey metrics were the following: Perceived severity, Perceived self-efficacy, CRC screening practices, and subjective norm (familial influences) |
| Crawford et al. (2020) | Canada - Ontario | Cross-sectional design | 328 | Pilot test English and Urdu version of Colon Cancer Screening Behaviors Survey; Objective 1) evaluate the feasibility of administration, data collection, and response burden Objective; and 2) examine the prevalence of CRC screening among SA and evaluate the psychometric properties of sub-scales in the survey | The feasibility identified were 1) successful recruitment despite reasons for refusal; 2) problematic items and response categories; and 3) computer/tablet limitations. Principle component analysis identified 14 components that explained 68.7 % of total variance; 34 items were retained after factor analysis. The internal consistency of 4 scales ranged from 0.79-0.91. There was significant differences in perceived barriers scale scores (− 12.21; 95% CI, − 17.13 to - 7.28; p < 0.0001) between those who participated and those who did not participate in screening. |
| Lofters et al. (2013) | Canada - Ontario | Ecological study | 76, 314 | Utilizing a geographic information system, including Local Indicators of Spatial Association using GeoDa software to identify regions with a high population of South Asians and low level of CRC screening | The approach allowed investigators to quickly target areas that would most benefit from CRC screening initiatives |
| Lofters et al. (2017) | Canada - Ontario | Participating physicians were selected for a quality improvement initiative within their offices that they feel could increase willingness to screen and cancer screening uptake | 4 primary care physicians, 60% of their patients were SA | One-on-one cancer screening education by Health Ambassadors (HA) at physician office waiting rooms, educational videos in the waiting room, pamphlets, telephone patients overdue for CRC screening | Physicians 1, 2, and 3 offices intervention by one-to-one education by HA, handed out pamphlets, and/or educational videos were not able to reach many patients. Phone calls by HA to patients who are overdue for CRC screening in Physicians 1,2, and 3 offices were able to reach a bigger population. At Physician 4 office, one-on-one education approached by HA, a total of 65.2% of SA patients spoken were willing to be screened |
| Thompson et al. (2014) | Canada - Ontario |
20,793 Asian Indian 4693 |
Electronic Health Record reminders for physicians and patients | 30% increase in odds for cervical and breast cancer screening, but no impact on CRC screening | |
| So et al. (2022) | Hong Kong | cluster-randomized control trial with a waitlist control group | 320 | a multimedia health talk, conveying the importance of colorectal cancer screening and support from younger family members in encouraging their older relatives to undergo screening | The proportion of older adults participating in FIT testing was significantly higher among intervention compared with controls (71% vs 6.8% p<.001) |
| Ghai et al. (2018) | US - California | Cross-sectional study | 1,746,714 | Organized colorectal cancer screening program, FIT kits | Post-intervention, almost all subgroups met the 80% screening target: Chinese (83.3%), Vietnamese (82.4%), Korean (82.1%), other Asian (80.3%), Filipino (78.7%), Asian Indian (79.6%), and Japanese (79%) |
| Mukherjea et al. (2020) | US - California | Survey on post-presentation of screening history, the likelihood of getting screened, and acceptance of brochure | 103; screening rate prior to presentation, 52% | South Asian physician-led presentations about CRC screening and culturally sensitive brochures | Intent to get screened after the presentation, 87%; those who took culturally sensitive brochures are willing to share information with family (95%) and friends (39%). 86% (n=37) of those who had not screened agreed with a state that they would be screened |
| Manne et al. (2021) | US - New Jersey | Baseline survey followed by post session survey 4 months after baseline | 93 | 1:1 sessions with community educator | An increase in knowledge, reduction in perceived barriers to screening, and worry about CRC screening tests declined significantly. Intent to treat analyses 30% 4-month follow-up to CRC screening uptake |
| Wu et al. (2010) | US- Michigan | Healthy Asian Americans Project expanded to include community-based CRC screening in the years 2005-2006 | 304 | Community-based education at local community/cultural centers | Post-educational events showed improvement in CRC screening |
Organized CRC screening programs have also been effective in increasing screening rates. Ghai et al. (2018) showed that almost all subgroups met an 80% target of being screened, including Asian Indian, Chinese, Vietnamese, Korean, Filipino, and Japanese populations. The program included mailed FIT kits to eligible health plan members aged 51-75 who were not up to date with CRC screening by colonoscopy or FSIG. These individuals were reminded through office/preventive health visits, mailed letters, and telephone messages.
However, using Electronic Health Record Reminders (Thompson et al., 2014) was not shown to have an impact on CRC screening, although there was a 30% increase in odds for cervical and breast cancer screening. Lofters et al. (2013) explored the use of Geographic Information System, including Local Indicators of Spatial Association using GeoDa software to identify regions with a high population of South Asian individuals and low levels of CRC screening. This method was able to identify high-risk areas consisting of multiple neighboring censuses with low screening rates and large SA populations.
Table 1.
Barriers and Facilitators of CRC in South Asian Immigrants in the US, UK, Canada, and Hong Kong
| Reference | Location | Study Design | Sample Size/Screening Rate | Age (yrs) | Ethnicity | Barriers | Facilitators |
|---|---|---|---|---|---|---|---|
| Crawford et al. (2015) | Canada - Ontario | Qualitative study: A cross-sectional study | 42 | 50–74 | Country of origin: India (69%); Pakistan and Bangladesh (14%); and Mauritius, Uganda, Kenya, or Africa (14%) | The belief that screening is not necessary, fear of invasive test/results, bowel practices, and poor knowledge and awareness of CRC and CRC screening | Family physician support/recommendations and physicians with same ethnicity and gender as patients |
| Crawford et al. (2017) | Canada - Ontario | Mixed methods study | N/A | N/A | N/A | Factors that affect CRC screening: Perceived susceptibility, perceived severity, perceived benefits, perceived barriers (language and cost), perceived self-efficacy (low confidence w/ completing test), and subjective norm (influence of family members and physicians to have screening) | |
| Lofters et al. (2015) | Canada - Ontario | Ecological study | 6303 primary care physicians The CRC screening cohort consisted of 2,260,569 patients |
Male: 52.85 + 10.95 Female: 48.8 + 9.64 |
Demographic: Caribbean/Latin America, East Asia, Eastern Europe, Middle East/North Africa, USA/Australia, New Zealand, and Western Europe | Physician-based barriers: International Medical Graduates Country of origin (Caribbean, Latin America, Western and Eastern Europe), not in patient enrollment model, and shorter time in independent practice Patient-based barriers: Male and lower income |
Physician-based facilitators: Canadian graduates, Eastern European trained, and more experience Patient-based facilitator: Female |
| Choi et al. (2015) | Hong Kong | Cross-sectional telephone survey | General public:2,004 Ethnic minority: 323 | Ethnic Minority group: Indian, Nepalese, and Pakistani | Lower education attainment, participants without any chronic illness, those who do not use complementary therapy, those who do not believe in visiting a doctor regularly was good, lack of health professional’s recommendation, and lower perceived susceptibility to cancer | Perception that visiting a regular doctor is good for health, use of complementary therapy, perceived susceptibility to cancer, and health professional’s recommendations | |
| Robb et al. (2008) | United Kingdom (UK) | Survey | 875 | 16–55+ | Indian, Pakistani, Bangladeshi, Caribbean, African, Chinese, white British | Shame/embarrassment | |
| Orbell et al. (2017) | UK | Questionnaire | 1678 (final sample size used in analysis) | 50-67 | British white European, British Minority Ethnic, and South Asian (Hindu, Muslim, and Sikh) | Nonparticipation of FOBT uptake showed a linear association across the distribution of SES of five quintiles (most deprived to least deprived; 29.8%, 24.4%, 21.3%, 23%, and 18%). Self-efficacy and response cost were statistically significant direct predictors of participation. There were significant negative effects of age on self-efficacy and gender on response cost and a significant positive effect of gender on severity. | |
| Palmer et al. (2015) | UK - England | Qualitative study: interviewed key informants of communities | 16 | N/A | Hindu, Sikh, and (Bangladeshi) Muslim communities | Limitations posed by English, any written language, reliance on younger family members, low awareness of cancer and screening, the difficulty associated with feces | N/A |
| Blanks et al. (2015) | UK - England | National Health Service Bowel Cancer Screening Programme in England (NHSBCSP) | N/A | N/A | White, Black, and South Asian | Current smokers, obese women, women from deprived tertile, South Asians and Blacks exhibited lower acceptance | Parous women, more frequent activity, drinking more alcohol, using Hormone Therapy for menopause |
| Reference | Location | Study Design | Sample Size/Screening Rate | Age (yrs) | Ethnicity | Barriers | Facilitators |
| Campbell et al. (2020) | UK - Scotland | Two rounds of the Scottish Bowel Cancer Screening Programme (2007-2013) linked to the 2021 Census; retrospective cohort study | 1.7 million Screening relative risk (95%CI): Other white British, 109.6 (108.8–110.3); Chinese, 107.2 (102.8–111.8); Indian, 80.5 (76.1–85.1); Pakistani, 65.9 (62.7–69.3); Bangladeshi, 76.6 (63.9–91.9); Other South Asian, 88.6 (81.8-96.1) |
50–74 | White Scottish, Other White British, White Irish, Other White, any mixed background, Indian, Pakistani, Bangladeshi, Other South Asian, Caribbean, African, Black Scottish or Other Black, and Chinese | Gender (female) and Religion (Hindu, Muslim, and Sikh) | N/A |
| Taskila et al. (2009) | UK - West Midlands | 11,355 | 50-69 | White, Indian, Pakistani/Bangladesh, Black Caribbean, Black African, Chinese, and mixed | Men, older people, and ethnicity (Indian ethnic background) | Ethnicity (Black Caribbean background), people w/ multiple symptoms, and those reporting abdominal pain, bleeding, and tiredness more likely to have a positive attitude | |
| Sy et al. (2018) | The US | Medical Expenditure Panel Survey data for the years 2009–2014 data used | Total, 30,740; Asian Indian, 456 CRC screening rate: White, 62.3%: Filipino, 55%; Chinese, 50.9%; Asian Indian, 48.6% |
50–75 | White, 93.8%; Asian Indian, 1%; Chinese, 2.1%; Filipino, 2.6% |
Asian Indian: unemployed or retired | Asian Indian: sex (men), employment, English fluency, and general health All groups: older age, health insurance, and having a usual source o provider |
| Mukherjea et al. (2022) | US - California | Data from the 2001–2009 California Health Interview Study Survey and multivariable logistic regression were used to examine determinants of non-adherent CRC screening | 459 | 50-70+ | Uninsured, immigrants <40% of life in the US, only speaking a language other than English at home, and having not had a flu shot in the past year | Non-adherence was lower among older South Asian Americans, private or Medicare insurance, those who lived in the US for more than 60% of their life, those who speak English at home, obese individuals, those who have other health conditions (high blood pressure and heart disease), and those who received flu shot in the past year | |
| Glenn et al. (2009) | US - Southern California | Interviews and self-administered questionnaire | 344; Any CRC screening rate: Indian, 25%; Pakistani, 37%; Bangladeshi, 17%; Sri Lankan, 68% |
20–65+ | Indian, 41%; Pakistani, 25%; Bangladeshi, 20%; Sri Lankan, 11%; Nepali, 2%; Other, 1% |
Gender (women were significantly less likely to receive colorectal cancer screening) | Insurance |
| Reference | Location | Study Design | Sample Size/Screening Rate | Age (yrs) | Ethnicity | Barriers | Facilitators |
| Ivey et al. (2018) | US -California | Survey; cross sectional | 53 CRC screening rate: 52.8% |
40–82 | Asian Indian and Bangladeshi | Low perception of risk, medical mistrust, cost concerns/health insurance, lower acculturation, lack of knowledge, and cultural milieu | Role and recommendation of physicians and Organizational strategies/program |
| Kazi et al. (2021) | US - California | Brief demographic survey and focus group Interviews | 32; CRC screening rate: 53% |
40–71 | Bangladesh, 47%; Pakistan, 44%; India, 9% |
Poor knowledge of CRC and CRC screening, lack of awareness of CRC, prioritizing preventive health is not as common in their native countries, fatalism, gender (female), cultural and religious stigma, lack of physician recommendation, having not had any problems, afraid, and cost/insurance | Physicians, families, social groups, and insurance |
| Thompson et al. (2014) | US -California | Cross-sectional analysis | Total, 20,793; Asian Indian, 4,693 CRC screening rate: Asian Indian, 45.6%; Japanese, 68.3%; Chinese, 66.7%; Filipino 59%; Korean, 66.2%; Vietnamese 65.8%; Native Hawaiian and Pacific Islander, 53.8% |
50–75 | Asian Indian, 22.5%; Japanese, 8.8%; Chinese, 45.6%; Filipino, 18.4%; Korean, 3.0%; Vietnamese, 2.7% |
Non-English primary language and patient-provider language discordant | Frequency of primary care visits |
| Wong et al. (2005) | US - California | Survey | South Asian, 148; Ever screened, 53%; up to date, 48% |
50+ | FOBT and Colonoscopy (ever screened): male gender, households of >3 individuals, living in the US <15 years, and family income <300%; FOBT (Up to date): households of > 3; Colonoscopy (Up to date): households of > 3 individuals, lived in the US for < 15 years, family income of < 200% of the FPL. |
FOBT and Colonoscopy (ever had screening): older, college graduates, family history of colon cancer, insurance (private or public), usual source of care, greater physician visits, and better health status; FOBT (Up to date): married, family history of colon cancer, insurance (public or private), more physician visits, and usual source of care; Colonoscopy (Up to date): male gender and greater education attainment. |
|
| Reference | Location | Study Design | Sample Size/Screening Rate | Age (yrs) | Ethnicity | Barriers | Facilitators |
| Menon et al. (2014) | US - Chicago (Illinois) | Subsample data from South Asian Health Descriptor Study; Cross-sectional | 275 | 50+ | Asian Indian, 86.9%; Pakistan, 10.9%; other South Asian countries, 2.2% | Decreased English-language proficiency, length of stay in the US, and education level (less than high school education); SBT: language acculturation and medical mistrust; Endoscopy: language acculturation, perception of CRC risk, completed SBT, income, and living in the US >5 years. |
|
| Manne et al. (2015) | US - New York and New Jersey | Survey | 208; Approx. 69% of the sample was not on schedule concerning CRC screening, 65% of the sample have undergone colonoscopy | 50–70 | Country of origin: India, 88.9%; Bangladesh, 3.4%; Pakistan, 17.8%; other, 0.04% |
Poor awareness of CRC screening, lower level of education, lower levels of income, fewer number of years in the US, less fluency in English, and perceived benefits and barriers to screening | Living in the US for a longer time |
| Patel et al. (2021) | US - New York (New York) | Semi-structured interviews and questionnaires | 51 | 50–75 | Indian, 14%; Pakistani, 16%; Bangladeshi, 17%; Nepali, 4% |
Poor knowledge of CRC and CRC screening, shame/discomfort and embarrassment regarding CRC and CRC screening in their community, fear of test and impact of diagnosis, fatalism, financial challenges, lack of physician recommendation, lack of insurance, and language barrier | Physician referral |
| Rastogi et al. (2019) | US - New York (New York) | Cross-sectional analysis using 2014 NYCCHS | Total, 4,190; Asian Indians, 50; CRC screening: total, 69.3%; Asian Indian, 45.1% |
50–65+ | Asian Indian, 1.2% | Colonoscopy: lived in the US <5 years, Asian Indian language spoken at home, lower income, and location (outside of Manhattan) | Colonoscopy: age >65 years and not being in the labor force |
| Patel et al., 2021 | US - New York (New York) | Semi-structured interviews and questionnaires | 51 | 50–75 | Indian, 14%; Pakistani, 16%; Bangladeshi, 17%; Nepali, 4% |
Poor knowledge on CRC and CRC screening, shame/discomfort and embarrassment regarding CRC and CRC screening in their community, fear of test and impact of diagnosis, fatalism, financial challenges, lack of physician recommendation, lack of insurance, language barrier | Physician referral |
| Reference | Location | Study Design | Sample Size/Screening Rate | Age (yrs) | Ethnicity | Barriers | Facilitators |
| Rastogi et al., 2019 | US - New York (New York) | Cross sectional analysis using 2014 NYCCHS | Total, 4,190; Asian Indians, 50; CRC screening: total, 69.3%; Asian Indian, 45.1% |
50–65+ | Asian Indian, 1.2% | Colonoscopy: lived in US <5 years, Asian Indian language spoken at home, lower income, location (outside of Manhattan) | Colonoscopy: age >65 years, not being in the labor force |
| Wyatt et al., 2021 | US - New York (New York) | Retrospective cross-sectional analysis of combined 2014-2018 NYC Community Health Survey data | Total, 24,288; NH South Asian, 359; CRC screening rate (colonoscopy last 10 years): NH white, 68.6%; NH black, 70.2%; Hispanic, 71.3%; NH East Asian, 65.9%; NH South Asian, 61.2% |
50+ | South Asian ethnic group consists of Indian, Bangladeshi, Pakistani, and Nepali ancestry | Age ≥65 years more likely than age 50-64 (p<0.001); Any type of health insurance were more likely than uninsured (p<0.001); lower poverty, education (high school vs less than high school) | |
| Khokhar et al., 2009 | US -Washington, DC | Survey | 112 | 40–78 | Poor knowledge on CRC and CRC screening, lack of physician recommendation, Cultural and/or religious sensitivities |
Discussion
This systematic review examines the barriers and facilitators to CRC screening among South Asian immigrants. While overall CRC screening has increased in recent years, ranging from 64.7% in 2016 to 68.6% in 2018 for ages 50-75 years (Centers for Disease Control and Prevention, 2021), South Asians have notably lower rates, ranging from 52% to 61.2% (Ivey et al., 2018; Mukherjea et al., 2020; Wyatt et al., 2022). These rates are the lowest among other ethnic groups, such as non-Hispanic white, non-Hispanic black, Hispanic, and other Asian groups (Sy et al., 2018; Rastogi et al., 2019; Wyatt et al., 2022).
According to the literature, the major barriers to CRC screening among South Asian immigrants include poor knowledge/awareness of CRC and CRC screening (Khokhar et al., 2009; Choi et al., 2015; Crawford et al., 2015; Manne et al., 2015; Palmer et al., 2015; Ivey et al., 2018; Kazi et al., 2021; Patel et al., 2021), lack of physician recommendation, psychological factors (e.g., fear, anxiety, shame), cultural/religious factors, and sociodemographic factors (language barrier, lower income, and female gender). In contrast, the greatest facilitators for increased screening are physician recommendation, frequency of physician visits, and having health insurance that covers CRC screening.
A key aspect of interpreting the above data is recognizing that Asians, including Asian Americans, do not represent a homogenous group (Hwang, 2013; Kim, 2017). Predictors of CRC, therefore, differ among Asian subgroups as follows (Fedewa et al., 2016): Filipinos (sex, income, attitude toward health, and general health); Chinese (education, English fluency, and attitude toward health); and Asian Indians (sex, employment, English fluency, and general health). The heterogeneity among Asian subgroups is also reflected in the disparities in CRC screening rates, where South Asians often have the lowest rates. Moreover, the South Asian population comprises heterogeneous subgroups, and subgroup screening rates differ by religion (Campbell et al., 2020). Therefore, further research is necessary to better understand the screening patterns of the Asian population, including cultural and structural barriers to receiving care. In light of the significant gap in CRC screening rates in the South Asian population, the review recommends three areas of improvement: increased education, increased frequency of recommendations, and strategic planning of interventions.
Targeting Underserved Regions Most at Risk
Identifying underserved regions most at risk to target for increasing CRC screening rates is critical to intervention success. The greater the intervention uptake in a low-prevalence screening area, the greater the opportunity is for uptake. Although many studies examined CRC screening rates in South Asians, a few employed innovative approaches (Lofters et al., 2013; Sy et al., 2013). For example, Sy et al. (2013) examined CRC screening prevalence utilizing Medical Expenditure Panel Survey National Data, and Lofters et al. (2013) used population-level data to identify underserved areas. Lofters et al. (2013) also highlighted the need to focus on both patients and physicians, as physicians of certain demographics and educational backgrounds tend to screen their own patients at lower rates. However, their analysis was limited to a particular region (Lofters et al., 2013).
Increased Education About CRC Screening
A lack of knowledge is a major barrier to CRC screening in SA communities (Choi et al., 2015; Crawford et al., 2015; Manne et al., 2015; Palmer et al., 2015; Ivey et al., 2018; Kazi et al., 2021; Patel et al., 2021). This lack of knowledge stems from various factors, such as a belief that screening is unnecessary or a lack of awareness about the disease (Crawford et al., 2015; Manne et al., 2015). Furthermore, this is exacerbated by the fact that preventative health is not emphasized in the South Asian community, which is critical for a disease like CRC that often presents in later stages (Kazi et al., 2021).
Addressing this core issue remains incredibly challenging. Moreover, there is no clear consensus on the best educational medium. Passive and active approaches can be successful (Taskila et al., 2009; Lee et al., 2011; Choi et al., 2015; Ivey et al., 2018; Wyatt et al., 2022). For example, resources such as brochures tailored to South Asian culture have been shown to be beneficial (Mukherjea et al., 2020). These resources ultimately enable patients to learn on their own time without fear of judgment. Active engagement, such as support groups, religious activities, or community events, can also have a positive impact on education (Kazi et al., 2018; Wyatt et al., 2022; Ivey et al., 2018; Lee et al., 2011). South Asian women, in particular, found that open group discussions were essential for discussing CRC screening (Wu et al., 2010), possibly because of the stigma surrounding the topic (Robb et al., 2008; Crawford et al., 2015; Kazi et al., 2021; Patel et al., 2021).
Emphasis on Cultural Sensitivity
The literature indicates that community/religious leaders should be involved in the process of promoting CRC screening, regardless of the medium used. Several articles emphasized the importance of utilizing a culturally sensitive approach (Kazi et al., 2021; Lee et al., 2011). The reasoning behind this appears to be that community/religious leaders are often in tune with the interworking of their constituents at the population level (Kazi et al., 2021), and their respect and influence can significantly sway their constituents to undergo screening. As previously noted, understanding the gender composition of groups is also critical. Gender-specific focus groups or matching patients with physicians based on gender can increase patients’ receptiveness to hearing about CRC screening (Kazi et al., 2021; Mukherjea et al., 2020). The effectiveness of patient resources is contingent on patients’ willingness to receive information, and their level of comfort with the medium used.
Limitations
A limitation of this review is the small number of studies (31) on CRC screening among South Asian immigrants that met the inclusion criteria. Additionally, several studies included South Asians in a homogenous study group, which may obscure the heterogeneity of this population. Caution should be exercised when interpreting the generalized results of Asian groups. Furthermore, Asian Indian participants were overrepresented in most studies, which could disproportionately influence the data of other South Asian groups, such as Pakistani, Bangladeshi, and Nepalese. Further research is required to identify differences in barriers among subgroups of the South Asian population and to evaluate the efficacy of interventions. Another limitation is that the majority of studies on CRC screening are US-based, which makes generalizing barriers and facilitators to CRC screening for South Asian immigrants worldwide challenging.
In conclusion, the prevalence of CRC among South Asian immigrants in the United States is comparable to that of the general US population, and this holds true for South Asian immigrants in Canada and the United Kingdom compared to the general populations of those countries. However, South Asians have among the lowest CRC screening rates across all ethnicities in the US. Given that screening is critical for the early detection and treatment of CRC, healthcare providers and community leaders must assist South Asian immigrants in overcoming screening barriers. Poor understanding of CRC and CRC screening, lack of physician recommendation, cultural/religious factors, psychological factors, language barriers, lower income, and female gender are the barriers identified in this review. Physician recommendation, regular physician visits, and having health insurance are facilitators to getting screened. To increase CRC screening among South Asian immigrants, it is essential to help them obtain health insurance. Furthermore, healthcare providers, educators, and community leaders must offer culturally sensitive education to South Asian immigrants on CRC and strongly encourage them to undergo screening.
Author Contribution Statement
All the authors contributed to the preparation of the final manuscript.
Acknowledgements
This manuscript has not been approved by any scientific body nor is it part of an approved student thesis. This manuscript is not registered in any registering dataset (e.g., clinical trials, guidelines, and meta-analyses).
Conflict of Interest
The authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter discussed in this manuscript.
References
- Beck DE. The importance of colorectal cancer screening. Ochsner J. 2015;15:11–2. [PMC free article] [PubMed] [Google Scholar]
- Blanks RG, Benson VS, Alison R, et al. Nationwide bowel cancer screening programme in England: cohort study of lifestyle factors affecting participation and outcomes in women. Br J Cancer. 2015;112:1562–7. doi: 10.1038/bjc.2015.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell C, Douglas A, Williams L, et al. Are there ethnic and religious variations in uptake of bowel cancer screening? A retrospective cohort study among 1 7 million people in Scotland. BMJ Open. 2020;10:e037011. doi: 10.1136/bmjopen-2020-037011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi KC, So WK, Chen JM, et al. Comparison Study of Uptake of Colorectal Cancer Testing between Ethnic Minorities and the General Population in Hong Kong. Asian Pac J Cancer Prev. 2015;16:7713–20. doi: 10.7314/apjcp.2015.16.17.7713. [DOI] [PubMed] [Google Scholar]
- Crawford J, Ahmad F, Beaton DE, Bierman AS. Colorectal cancer screening behaviors among South Asian immigrants in Canada: a qualitative study. Int J Migr Health Soc Care. 2015;11:130–46. doi: 10.1111/hsc.12208. [DOI] [PubMed] [Google Scholar]
- Crawford J, Beaton D, Ahmad F, et al. Cross-cultural survey development: The Colon Cancer Screening Behaviors Survey for South Asian populations. BMC Res Notes. 2017;10:770. doi: 10.1186/s13104-017-3098-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford J, Morfaw F, Ahmad F, et al. The colon cancer screening behaviours survey for South Asians: a pilot study of feasibility and psychometric evaluation. J Patient Rep Outcomes. 2020;4:12. doi: 10.1186/s41687-019-0160-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cullerton K, Gallegos D, Ashley E, et al. Cancer screening education: can it change knowledge and attitudes among culturally and linguistically diverse communities in Queensland, Australia? Health Promot J Austr. 2016;27:140–7. doi: 10.1071/HE15116. [DOI] [PubMed] [Google Scholar]
- Ghai NR, Jensen CD, Corley DA, et al. Colorectal Cancer Screening Participation Among Asian Americans Overall and Subgroups in an Integrated Health Care Setting with Organized Screening. Clin Transl Gastroenterol. 2018;9:186. doi: 10.1038/s41424-018-0051-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenn BA, Chawla N, Surani Z, et al. Rates and sociodemographic correlates of cancer screening among South Asians. J Community Health. 2009;34:113–21. doi: 10.1007/s10900-008-9129-1. [DOI] [PubMed] [Google Scholar]
- Hwang H. Colorectal cancer screening among Asian Americans. Asian Pac J Cancer Prev. 2013;14:4025–32. doi: 10.7314/apjcp.2013.14.7.4025. [DOI] [PubMed] [Google Scholar]
- Ivey SL, Mukherjea A, Patel A, et al. Colorectal Cancer Screening Among South Asians: Focus Group Findings on Attitudes, Knowledge, Barriers and Facilitators. J Health Care Poor Underserved. 2018;29:1416–37. doi: 10.1353/hpu.2018.0104. [DOI] [PubMed] [Google Scholar]
- Jain RV, Mills PK, Parikh-Patel A. Cancer incidence in the south Asian population of California, 1988-2000. J Carcinog. 2005;4:21. doi: 10.1186/1477-3163-4-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazi E, Sareshwala S, Ansari Z, et al. Promoting Colorectal Cancer Screening in South Asian Muslims Living in the USA. J Cancer Educ. 2021;36:865–73. doi: 10.1007/s13187-020-01715-3. [DOI] [PubMed] [Google Scholar]
- Khokhar O, Khatri N, Lewis J. Colon Cancer Screening Rates and Knowledge Among South Asians in the U S When Culture Clashes with Recommendations: 1520. Official journal of the American College of Gastroenterology. ACG. 2009;104:S572. [Google Scholar]
- Kim SB. Unraveling the Determinants to Colorectal Cancer Screening Among Asian Americans: a Systematic Literature Review. J Racial Ethn Health Disparities. 2018;5:683–99. doi: 10.1007/s40615-017-0413-6. [DOI] [PubMed] [Google Scholar]
- Lee HY, Lundquist M, Ju E, et al. Colorectal cancer screening disparities in Asian Americans and Pacific Islanders: which groups are most vulnerable? Ethn Health. 2011;16:501–18. doi: 10.1080/13557858.2011.575219. [DOI] [PubMed] [Google Scholar]
- Lofters AK, Gozdyra P, Lobb R. Using geographic methods to inform cancer screening interventions for South Asians in Ontario, Canada. BMC Public Health. 2013;13:395. doi: 10.1186/1471-2458-13-395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lofters AK, Ng R, Lobb R. Primary care physician characteristics associated with cancer screening: a retrospective cohort study in Ontario, Canada. Cancer Med. 2015;4:212–23. doi: 10.1002/cam4.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lofters AK, Vahabi M, Prakash V, et al. Lay health educators within primary care practices to improve cancer screening uptake for South Asian patients: challenges in quality improvement. Patient Prefer Adherence. 2017;11:495–503. doi: 10.2147/PPA.S127147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manne S, Steinberg MB, Delnevo C, et al. Colorectal Cancer Screening Among Foreign-born South Asians in the Metropolitan New York/New Jersey Region. J Community Health. 2015;40:1075–83. doi: 10.1007/s10900-015-0053-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manne SL, Islam N, Frederick S, et al. Culturally-adapted behavioral intervention to improve colorectal cancer screening uptake among foreign-born South Asians in New Jersey: the Desi Sehat trial. Ethn Health. 2021;26:554–70. doi: 10.1080/13557858.2018.1539219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menon U, Szalacha L, Prabhughate A, et al. Correlates of colorectal cancer screening among South Asian immigrants in the United States. Cancer Nurs. 2014;37:19–27. doi: 10.1097/NCC.0b013e31828db95e. [DOI] [PubMed] [Google Scholar]
- Mukherjea A, Ansari ZK, Senthil Kumar S, et al. Preliminary Evaluation of Educational Outreach to Promote Colorectal Cancer Screening Among South Asians in the San Francisco Bay Area. J Immigr Minor Health. 2020;22:873–7. doi: 10.1007/s10903-019-00965-8. [DOI] [PubMed] [Google Scholar]
- Mukherjea A, Shariff-Marco S, Yang J, et al. Determinants of Colorectal Cancer Screening among South Asian Americans. J Asian Health. 2022;10:1–12. [PMC free article] [PubMed] [Google Scholar]
- Orbell S, Szczepura A, Weller D, et al. South Asian ethnicity, socioeconomic status, and psychological mediators of faecal occult blood colorectal screening participation: A prospective test of a process model. Health Psychol. 2017;36:1161–72. doi: 10.1037/hea0000525. [DOI] [PubMed] [Google Scholar]
- Palmer CK, Thomas MC, McGregor LM, et al. Understanding low colorectal cancer screening uptake in South Asian faith communities in England – a qualitative study. BMC Public Health. 2015;15:998. doi: 10.1186/s12889-015-2334-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel S, Kranick J, Manne S, et al. A Population Health Equity Approach Reveals Persisting Disparities in Colorectal Cancer Screening in New York City South Asian Communities. J Cancer Educ. 2021;36:804–10. doi: 10.1007/s13187-020-01707-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rastogi N, Xia Y, Inadomi JM, et al. Disparities in colorectal cancer screening in New York City: An analysis of the 2014 NYC Community Health Survey. Cancer Med. 2019;8:2572–9. doi: 10.1002/cam4.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rastogi T, Devesa S, Mangtani P, et al. Cancer incidence rates among South Asians in four geographic regions: India, Singapore, UK and US. Int J Epidemiol. 2008;37:147–60. doi: 10.1093/ije/dym219. [DOI] [PubMed] [Google Scholar]
- Robb KA, Solarin I, Power E, et al. Attitudes to colorectal cancer screening among ethnic minority groups in the UK. BMC Public Health. 2008;8:34. doi: 10.1186/1471-2458-8-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreuders EH, Ruco A, Rabeneck L, et al. Colorectal cancer screening: a global overview of existing programmes. Gut. 2015;64:1637–49. doi: 10.1136/gutjnl-2014-309086. [DOI] [PubMed] [Google Scholar]
- Simon K. Colorectal cancer development and advances in screening. Clin Interv Aging. 2016;11:967–76. doi: 10.2147/CIA.S109285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- So WKW, Chan DNS, Law BMH, et al. Effect of a family-based multimedia intervention on the uptake of faecal immunohistochemical test among South Asian older adults: A cluster-randomised controlled trial. Int J Nurs Stud. 2022;132:104254. doi: 10.1016/j.ijnurstu.2022.104254. [DOI] [PubMed] [Google Scholar]
- Sy AU, Lim E, Ka’opua LS, et al. Colorectal cancer screening prevalence and predictors among Asian American subgroups using Medical Expenditure Panel Survey National Data. Cancer. 2018;124:1543–51. doi: 10.1002/cncr.31098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taskila T, Wilson S, Damery S, et al. Factors affecting attitudes toward colorectal cancer screening in the primary care population. Br J Cancer. 2009;101:250–5. doi: 10.1038/sj.bjc.6605130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson CA, Gomez SL, Chan A, et al. Patient and Provider Characteristics Associated with Colorectal, Breast, and Cervical Cancer Screening among Asian Americans. Cancer Epidemiol Biomarkers Prev. 2014;23:2208–17. doi: 10.1158/1055-9965.EPI-14-0487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong ST, Gildengorin G, Nguyen T, et al. Disparities in colorectal cancer screening rates among Asian Americans and non-Latino whites. Cancer. 2005;104:2940–7. doi: 10.1002/cncr.21521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu TY, Kao JY, Hsieh HF, et al. Effective colorectal cancer education for Asian Americans: a Michigan program. J Cancer Educ. 2010;25:146–52. doi: 10.1007/s13187-009-0009-x. [DOI] [PubMed] [Google Scholar]
- Wyatt LC, Patel S, Kranick JA, et al. Disparities in colorectal cancer screening among South Asians in New York City: a cross-sectional study. J Cancer Educ. 2022;37:1510–8. doi: 10.1007/s13187-021-01991-7. [DOI] [PMC free article] [PubMed] [Google Scholar]