Abstract
Aims
As a chronic inflammatory disease, endometriosis (EMS) is often associated with pain affecting different aspects of women's lives. Up to now, a wide variety of interventions have been implemented to alleviate pain in patients with this condition, including pharmacological, surgical, and rarely non‐pharmacological ones. Against this background, this review aimed to investigate pain‐focused psychological interventions among EMS women.
Methods
A systematic review of the articles published in this field was conducted through a comprehensive search on the databases of Scopus, PubMed, MEDLINE, Web of Science, ScienceDirect, the Cochrane Library, PsycINFO, Google Scholar, and Scientific Information Database (SID). The quality of studies was then assessed by the Jadad Scale.
Results
In total, 10 articles were entered into this systematic review. The findings further revealed that the pain‐focused psychological interventions in patients with EMS were cognitive‐behavioral therapy (CBT) (n = 2), mindfulness therapy (n = 4), yoga (n = 2), psychoeducation (n = 1), and progressive muscle relaxation (PMR) training (n = 1). Besides, the findings established that all the given interventions had improved and reduced pain in women living with this condition. Moreover, five articles were of good quality based on the Jadad Scale.
Conclusion
The study results demonstrated that all the listed psychological interventions had affected pain relief and improvement in women suffering from EMS. Considering the limited number of studies in this field and the fact that there were only five articles endowed with good quality, more high‐quality studies could provide stronger evidence to support the implementation of the mentioned interventions influencing pain in patients.
Keywords: chronic pelvic pain, endometriosis, pain, psychological intervention
This systematic review aimed to investigate pain‐focused psychological interventions among Women with endometriosis. In total, 10 articles were entered into this review. The study results demonstrated that all the listed psychological interventions had affected pain relief and improvement in women suffering from endometriosis.

1. INTRODUCTION
As a painful, chronic inflammatory disease, endometriosis (EMS) is characterized by the proliferation of endometrial glands and stroma outside the uterine cavity. 1 , 2 , 3 The prevalence rate of this health condition has been also reported by 10%–15% 1 , 4 , 5 and its incidence rate has been estimated as 8–12 individuals per 1000 population. It is noteworthy that EMS is most commonly observed among women in their 30–40s, and may make it harder to get pregnant, i.e., the most prevalent age is between 35 and 44. 6 , 7 The symptoms of this condition are abundant, including pain and chronic pelvic pain, painful intercourse (viz., dyspareunia), menstrual cramps (or dysmenorrhea), fertility decline, constipation, diarrhea, anxiety, mood swings, and depression 5 , 8 , 9 , 10 Besides, EMS is often associated with pain, particularly chronic pelvic ones, affecting different aspects of women's lives, 11 , 12 and leading to negative impacts on their abilities in terms of performing their own daily activities, taking on maternal roles, fulfilling their marital relationships, and losing jobs. 9 , 10 EMS can further have biopsychosocial effects, giving rise to psychosomatic disorders. 13
The pharmacological treatments adopted for symptomatic EMS include clinical interventions and surgeries, 14 , 15 such as prescribing non‐steroidal anti‐inflammatory drugs (NSAIDs), gonadotropin‐releasing hormone (GnRH) and its analogues (GnRH‐a), androgen derivatives, oral contraceptives, and progestogens. 13 , 16 , 17 , 18 However, numerous studies have so far shown the high possibility of increased pain and relapse upon discontinuing such medications. Current medical treatments do not often provide sufficient pain relief, or bring intolerable side effects caused by the androgenic and hypoestrogenic properties (namely, weight gain, hirsutism, acne, vaginal atrophy, breast atrophy, hot flashes, decreased libido, fatigue, nausea, and vomiting), along with high costs of medical and surgical practices, resulting in patients' tendency toward opting for non‐pharmacological techniques to lower EMS‐associated pain. 9 , 11 For this reason, 25–50% of women choose to stop medical treatments, 13 but pursue psychological interventions, such as cognitive‐behavioral therapy (CBT), mindfulness therapy, 9 , 12 yoga, 6 psychoeducation, or psychotherapy techniques, 11 and progressive muscle relaxation (PMR) training. 19 Therefore, the use of non‐pharmacological therapies together with other treatments has been advocated to alleviate pain in patients living with EMS. Exploiting non‐pharmacological treatments, such as complementary therapies and psychological interventions, including mindfulness therapy, can also sometimes boost the immune system, diminish stress, enhance mental health status, augment pain tolerance, relieve pain, and ultimately improve quality of life among EMS women. 6 Some studies have already confirmed the effectiveness of mindfulness therapy in reducing pain in women suffering from this condition. 9 , 12 As well, CBT has minimized pain in such patients. 20 Other studies have further evidenced that physiotherapy, CBT, and mindfulness practices have decreased pain in such women, but the results have not been significant, 21 , 22 due to the use of different measurement tools and small sample sizes. Since the results of the studies regarding the effects of psychological interventions on pain in women with EMS are contradictory, a systematic review can be helpful. The nature of this type of study is to reconcile a series of related studies and allow readers to apply the results of multiple ones on the same topic simultaneously. 23 , 24 , 25
With regard to the available resources and the comprehensive overview of the related literature as well as the lack of a systematic review of the articles examining psychological interventions for pain relief in women living with EMS, this review aimed to investigate pain‐focused psychological interventions in such individuals.
2. METHODS
A systematic review was conducted based on the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses (PRISMA) checklist. 26
2.1. Data sources and search strategies
A systematic review of the published articles, with no time limits, was conducted through a comprehensive search on the databases of Scopus, PubMed, MEDLINE, Web of Science, ScienceDirect, the Cochrane Library, PsycINFO, Google Scholar, Scientific Information Database (SID). Moreover, the list of the retrieved articles was manually in the related journals to extract the ones reflecting on this topic. The databases were searched from January 10 to March 5, 2023. The Medical Subject Headings (MeSH) w also employed with the following keywords:
“Endometriosis” OR “Pelvic Pain” OR “Chronic Pelvic Pain” AND “Pain” AND “Intervention” OR “Psychological Intervention” OR “Supportive Intervention” OR “Support Group” OR “Cognitive Behavioral Therapy” OR “Cognitive Behavioral Treatment” OR “Cognitive Therapy” OR “Cognitive Psychotherapy” OR “Cognitive Behavioral Intervention” OR “Mindfulness” OR “Yoga” OR “Psychotherapy” OR “Behavior Therapy” OR “Relaxation” OR “Relaxation Therapy” OR “Muscle Relaxation” OR “Progressive Muscle Relaxation Training” OR “Hypnosis”.
2.2. Study selection
All the articles recruited in this systematic review met the following inclusion criteria. That is, the study involved a clinical or quasi‐experimental research design, examining the effects of pain‐focused psychological interventions in women with EMS, as well as reporting the sample size and the results of the interventions. The articles that did not meet these criteria along with the abstracts of the articles presented in conferences, and the ones with no full texts, were excluded.
2.3. Data extraction
All the relevant studies were extracted during systematic and advanced searches. The duplicated articles were further removed. The irrelevant articles, identified by their titles, abstracts, or full texts, were also excluded. Two independent researchers further selected the final articles. In the event of a disagreement, the third researcher made the final decision.
Upon reading the abstracts and full texts of the articles meeting the inclusion criteria in this review, the data, namely, author/year/country, objectives, age, sample size, tool, as well as type/duration/follow‐up of interventions, and results were, extracted to develop the present review. Ultimately, the data were classified and reported (Table 1).
TABLE 1.
Description of studies.
| No. | Author /year/country | Objectives | Age (years.) | Sample size | Tools | Intervention: 1. Type. 2. Duration. 3. Follow‐up | Results: S: Significant. NS: Non‐significant |
|---|---|---|---|---|---|---|---|
| 1 | Hansen et al./2023/Denmark | Psychological interventions to improve quality of life despite persistent pain in EMS based on three‐armed RCT results | 18–47 |
58 MY‐ENDO: 20 Non‐Specific: 19 Control: 19 |
NRS CPAQ WAI VPPDT ER‐QOL |
|
Specific mindfulness and ACT psychological interventions (viz., MY‐ENDO) reduced pain intensity and unpleasantness, but not significantly (p = 0.310, Cohen's d = 0.42). (NS) Non‐Specific psychological interventions alleviated pain intensity and unpleasantness, but not significantly (p = 0.087, Cohen's d = 0.71). (NS) The MY‐ENDO intervention was not superior to the Non‐Specific one. |
| 2 | Ravins et al./2022/Israel | Investigating the effect of practicing yoga on stress and quality of life for women with EMS | 18–50 | 52 |
PNRS EHP‐36 |
|
Yoga reduced pain in patients with EMS (p = 0.001). (S) |
| 3 | Marcelo de França Moreira et al./2022/Brazil | The effects of a brief mindfulness‐based intervention in women with deep EMS |
Mean age IG: 37.67 CG: 34.68 |
63 IG: 31 CG: 32 |
PNRS PSS SF‐36 |
|
A brief mindfulness‐based intervention decreased pelvic and unpleasantness pain after intervention and follow‐up. After intervention: pelvic pain (p = 0.013, Effect size: 0.16) and pain unpleasantness (p = 0.001, effect size: 0.68). Follow‐up: pelvic pain (p = 0.007, Effect size: 0.25) and pain unpleasantness (p = 0.001, effect size: 0.40). (S) |
| 4 | Hansen et al./2017/Denmark | Long‐term effects of mindfulness‐based psychological intervention for coping with pain in EMS: A 6‐year follow‐up in a pilot study | 14–37 | 10 |
EHP GHS |
|
Mindfulness psychological intervention alleviated pain in patients with EMS and the results in follow‐ups showed significant differences the data from 12 months after intervention to 6 years after it. Therefore, the results confirmed the stability of improvement and the effect of the intervention p < 0.001 (S) There was a difference between 12 months and 6 years after the intervention p = 0.0583 |
| 5 | Goncalves et al./2017/Brazil | The practice of Hatha yoga for the treatment of pain associated with EMS | 18–50 |
40 IG:28 CG:12 |
EHP |
|
Yoga intervention reduced pain in patients with EMS. (S) p = 0.0007 |
| 6 | Meissner et al./2016/Germany | Using psychotherapy with somatosensory stimulation for EMS‐associated pain | 18–40 |
67 IG:35 CG:32 |
STAI, HADS, SF‐12, FW‐7 Pain Questionnaire of the German Society‐NRS |
|
Psychotherapy along with somatosensory stimulation (viz., various techniques of acupuncture‐point stimulation), moderated pain in patients with EMS, especially after 3 months. (S) p = 0.002 |
| 7 | Kold et al./2012/Denmark | The effect of mindfulness‐based psychological intervention for coping with pain in EMS | 14–37 | 10 |
EHP GHS |
|
Mindfulness‐based psychological intervention reduced pain in patients with EMS and the results were consistent in the follow‐up. (S) After intervention: p = 0.005 After 6‐month follow‐up: p = 0.001 After 12‐month follow‐up: p = 0.003 |
| 8 | Friggi et al./2012/Brazil | Use of physical therapy and psychological intervention normalizing cortisol levels and improving vitality in women with EMS |
Mean age 32.2 |
26 |
VAS PSQ SF‐36 |
|
Physical therapy intervention and CBT reduced pain in women with EMS, but the results were not significant. (NS) p > 0.05 |
| 9 | Zhao et al./2012/China | The effect of PMR training on anxiety, depression, and quality of life of EMS patients | 48–18 |
100 IG: 50 CG:50 |
STAI HADS SF‐36 |
|
PMR Training reduced pain in women with EMS. (S) p < 0.001 |
| 10 | Lorencatto et al./2007/Brazil | Evaluation of pain and depression in women with EMS after a multi‐professional group intervention |
Mean age IG: 34.7 CG: 32.8 |
128 IG: 64 CG: 64 |
VAS BDI |
|
CBT reduced pain in women with EMS. (S) p < 0.0001 |
Abbreviations: ACT, Acceptance and Commitment; BDI, Beck Depression Inventory; CBT, Cognitive Behavioral Therapy; CG, Control Group; CPAQ, Chronic Pain Acceptance Questionnaire; EHP, Endometriosis Health Profile; ER‐QOL, Endometriosis‐Related Quality of Life; FW‐7, 7‐Item Functional Well‐Being; GHS, General Health Questionnaire; HADS, Hospital Anxiety Depression Scale; IG, Intervention Group; NRS, Numeric Rating Scale; PMR, Progressive Muscular Relaxation; PNRS, Pain Numeric Rating Scale; PSQ, Perceived Stress Questionnaire; PSS, Perceived Stress Scale; SF‐12, 12‐Item Short‐Form Health Survey; SF‐36, Short‐Form Health Survey‐36; STAI, State–Trait Anxiety Inventory; VAS, Visual Analogue Scale; VPPDT, Vaginal Pressure Pain Detection Threshold; WAI, Work Ability Index.
2.4. Quality assessment of articles
Following the search on different databases, the required data were extracted and the quality of the included articles was assessed using the Jadad Scale. 27 Of note, the Jadad Scale is utilized to evaluate the methodological quality of clinical trials, via direct and indirect sections, to shed light on their bias control, and includes three original items, viz., random allocation, double‐blindness, and dropout rate that are often associated with bias control in clinical trials. 27 , 28 The three direct statements in the Jadad Scale are general and can be employed in all fields of medical science. Several studies have thus far incorporated only the three direct items, although others have applied both direct and indirect ones. 24 , 29 , 30 In this systematic review, three direct items were evaluated using the Jadad Scale with the application for all fields in medical science. The scoring system in the direct statements was as follows. The first statement was associated with the randomization of the samples, in which the word randomization was scored 1, and the description of the study stages and randomization procedure were awarded 2 (at a 0–2 score range). The second statement was also related to being a double‐blind study. A score of 1 was thus given if the term double‐blind was mentioned in the study, while a score of 2 was assigned if the study stages and an appropriate blindness method were described (at a 0–2 score range). The third item referred to the dropout rate and causes. A score of 1 was further given if the dropout rate and the cases were reported in the study (at a 0–1 score range). 27 The overall Jadad Scale score was 5, so a score of less than 3 showed that the study was of poor quality, while a score greater than 3 considered it of good quality. 27 , 28 , 31 , 32
3. RESULTS
3.1. Description of studies
Initially, a total number of 2813 articles were retrieved using the search strategies. As well, eight studies were found during a manual search. Subsequently, the duplicated and irrelevant articles were excluded, and 119 cases remained. Then, 96 and 13 articles were removed after reading their abstracts and full texts, respectively. Finally, 10 articles were selected for this systematic review (Figure 1).
FIGURE 1.
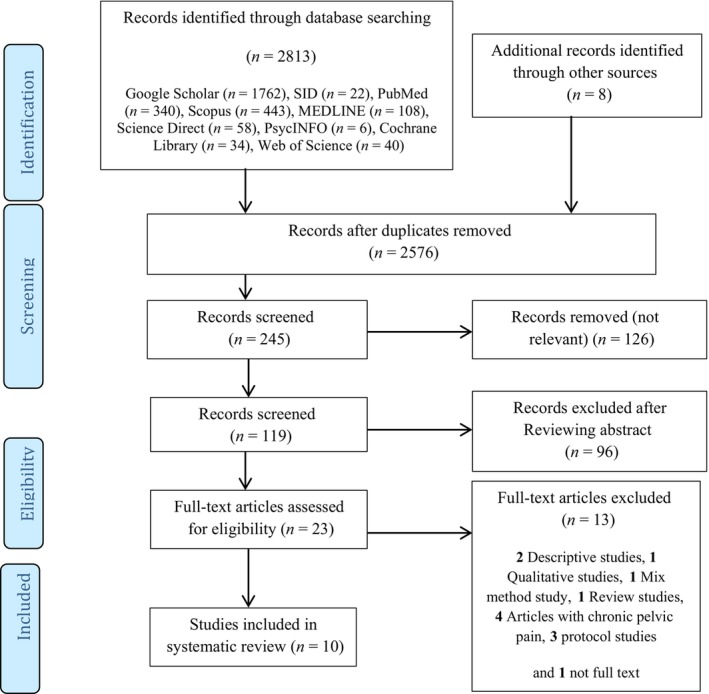
Flow chart of study selection according to PRISMA guidelines is presented.
The clinical or quasi‐experimental articles that included examining the effects of pain‐focused psychological interventions in women with EMS, the number of sample size was mentioned, and the study results were stated were included in this systematic review.
3.2. Article review
3.2.1. Study participants
The participants recruited in all the selected articles were women affected by EMS. These individuals are aged 14–50 years. Moreover, the inclusion and exclusion criteria had been mentioned in all studies.
3.3. Classification of interventions
3.3.1. Cognitive‐behavioral therapy (CBT)
Two articles evaluated the effects of CBT on pain in EMS women. 20 , 21 In this respect, one study examined the impacts of physical therapy and CBT‐based psychological interventions to improve cortisol levels and quality of life in women with this condition. As well, one article had assessed the effectiveness of 10 CBT sessions, arranged once per week for 150 min. In the first hour of each session, the patients received physical therapy including body awareness training (BAT), breathing exercises, relaxation techniques, stretching, pineal muscle strength exercises, massage therapy, self‐massage, special pain relief workouts, as well as transcutaneous electrical nerve stimulation (TANS) therapy. After that, the CBT‐based psychological interventions and some topics, such as awareness‐raising about EMS, stress management, CBT techniques for coping with the illness and its associated pain, patients' feelings and thoughts regarding EMS and its symptoms, as well as social, familial, and sexual relationships had been discussed. It should be noted that the intervention sessions had been conducted by an experienced psychologist and a physiotherapist in a safe and comfortable environment, accompanied by relaxing music. 21 In another study, 20 pain and depression had been measured in women living with EMS after receiving CBT‐based group interventions. The intervention sessions had been designed for 10 CBT sessions, once per week for 2.5 h. Within the first hour of each session, the patients received physiotherapy and breathing exercises. Then, the CBT‐based psychological intervention had been implemented, addressing issues such as giving information about EMS, mind–body relationships, coping skills, stress management, cognitive techniques, problem‐solving strategies, coping with pain, management of EMS symptoms, familial relationships, as well as sexuality. Moreover, the intervention sessions had been conducted by a trained psychologist and instructor. 20
3.3.2. Mindfulness therapy
In total, four articles examined the effects of mindfulness therapy on pain in patients suffering from EMS. 9 , 12 In one study, the effectiveness of mindfulness‐based psychological interventions to cope with pain in EMS patients had been further evaluated. As well, there were 10 intervention sessions once per week for 2 h. The intervention sessions had been held as five individual and five group sessions. Mindfulness training, body scanning, breathing techniques, music therapy, along with biofeedback support, group counseling, and psychotherapy, encompassing psychological challenges, grief processes, adaptation to chronic pain, stress and pain, health habits, such as eating and exercising, as well as mind–body interactions, had been among the issues raised in the group sessions. In the individual sessions, some issues, such as mindfulness techniques, counseling, and supportive therapies corresponding patients' goals and challenges as well as much focus on pain had been further deliberated. It should be noted that one of the individual intervention sessions had been attended by the patients' husbands. The individual and group intervention sessions had been also directed by a psychologist. 12 In another study, the long‐term impacts of mindfulness‐based psychological interventions on pain in EMS patients had been similarly investigated. This study was in line with the previous one in which the effect and stability of mindfulness interventions on pain in 10 patients living with EMS had been assessed over six years. 9 In one study, the results revealed that psychological interventions had improved quality of life despite persistent pain in women living with EMS. 22 The MY‐ENDO intervention also consisted of a manual 10‐week program, including 3‐h weekly group sessions with patient education about themes related to EMS, with a variety of mindfulness, acceptance and commitment, yoga, and group therapy techniques, focused on patients' experiences and coping mechanisms in relation to these themes. The participants had been further encouraged to practice 30–45 min of yoga and mindfulness meditation at home, 5–7 days a week. In the other group, the Non‐Specific intervention had been developed by removing all aspects specific to mindfulness meditation, acceptance and commitment, and yoga from the MY‐ENDO manual. This intervention comprised relaxation, while listening to soft and relaxing music, and guided physical training (namely, warm‐up, muscle training, and stretching) for women with chronic pelvic pain. The participants in this group had also practiced 30–45 min of physical training and relaxation at home, 5–7 days a week. The control group had merely received medical treatment. This intervention had been implemented by two private clinical psychologists. 22 In another study, the effects of a brief mindfulness‐based intervention in women with deep endometriosis had evaluated. There were four intervention sessions, once per week for 1.5 h. The intervention session contained mindfulness meditation practices, psychoeducation, mindfulness attitudes, reconceptualization, and pain modulation from tissue damage to general risk perception, emotions, body sensations, and their role in stress, stress response, as well as interactions between thoughts and pain and well‐being. Formal meditation practices had been additionally trained, including mindful movement, meditation, and mindfulness of the body scan, mindfulness of the breath, walking, breath, and thoughts. The participants had been then supported to do mindfulness of the breath, mindfulness of the movement, and 3‐min brief breath space for 20–30 min at home. In the control group, women had simply received standard medical care services. 33
3.3.3. Yoga
Two studies evaluated the effect of yoga on pain in patients with EMS. There were also eight intervention sessions, held twice per week for 2 h. Each session included talking and interacting with each other (30 min), muscle relaxation techniques (10 min), yoga training with 5–10 breathing exercises (60 min), muscle relaxation techniques with meditation and breathing exercises (10 min), as well as questions and answers (10 min). Moreover, the intervention sessions had been conducted by a yoga instructor. 6 In another study, the impact of practicing yoga on stress and quality of life in EMS had been further assessed. 13 The program included 8 weeks of conventional therapy, and then eight sessions of yoga classes, twice per week for 90 min. At first, the women had been divided into seven groups, and each group included 5–9 women and their yoga teacher. The yoga session consisted of conversations, including discussions about breathing techniques, emotional support, and sources of pain (15 min), physical and psychological relaxation breathing exercises (10 min), warm‐up exercises for joints (10 min), Hatha yoga poses with accessories, such as blocks and bolsters, to relieve pain in the pelvis or lower back (40 min), resting in a pose or physical and psychological relaxation (20 min), intuitive writing (5 min), and reflection (5 min). 13
3.3.4. Psychoeducation
One study evaluated the impact of psychotherapy along with somatosensory stimulations on pain in patients suffering from EMS. This intervention had been based on mindfulness, hypnosis, problem‐solving, CBT, and acupuncture techniques. During the intervention sessions, the therapist further raised questions about patients' concerns as well as sense of pain in various parts of the body and had utilized psychoeducation practices as well as somatosensory stimulation as acupuncture‐point stimulation to deal with such problems. Eventually, the patients ended up suffering from endometrial stress and negative emotions induced by pain and illness. It should be noted that the intervention sessions had been conducted by a psychiatrist and an acupuncturist. Each session also lasted 30–60 min. 11
3.3.5. Progressive muscular relaxation (PMR)
Only one article examined the effect of PMR training on pain in patients living with EMS. 19 There were eight intervention sessions, twice per week for 40 min. Of note, PMR was based on a classic muscle relaxation program, developed by Jacobson, and systematically involved relaxing the major muscle groups of the body with the goal of physical and mental relaxation. PMR training had been further discussed as an introductory group discussion of anxiety and depression in EMS patients, as well as a rationale and a general description of the purpose of relaxation, how to relax and contract the muscles of the right hand and the forearm, the right biceps, the left hand and the forearm, the left biceps, the forearm, the upper section of the cheeks and the nose, the lower section of the cheeks and the nose, the neck and the throat, the chest, the shoulders and the upper part of the back, the abdominal region and the stomach, the right thigh, the right calf, the right foot, the left thigh, the left calf and the left foot (16 muscle groups). The intervention group had also been given a brochure describing the mechanisms and benefits of relaxation and a relaxation audio CD providing a helpful guide for at‐home PMR practices. 19
3.4. Tools
The outcomes measured in all the articles included in this review were associated with pain in patients with EMS. In the meantime, four studies had assessed pain based on patients' self‐reports, using the Pain Numeric Rating Scale (PNRS). 11 , 13 , 22 , 33 Four articles had also measured pain in such patients via the Endometriosis Health Profile (EHP) 6 , 9 , 12 , 13 and two other studies had utilized the Visual Analogue Scale (VAS). 20 , 21 Two articles had further evaluated pain in women with EMS with the 36‐item Short‐Form Health Survey (SF‐36), 19 , 33 and one study had reflected on pain by the Chronic Pain Acceptance Questionnaire (CPAQ) and the Vaginal Pressure Pain Detection Threshold (VPPDT). 22 In addition to measuring pain, patients' general health status had been also assessed in two articles, using the General Health Questionnaire (GHQ). 9 , 12 In two studies, other parameters in addition to pain, such as anxiety, hospital‐related depression, and quality of life had been measured employing the State–Trait Anxiety Inventory (STAI), the Hospital Anxiety and Depression Scale (HADS), the SF‐12‐item Short‐Form Health Survey (SF‐12), and the Functional Well‐Being (FW‐7), respectively. 11 , 19 In one article, depression together with pain had been also assessed, using the Beck Depression Inventory (BDI), 20 and quality of life in EMS women had been evaluated in one study by the Endometriosis‐Related Quality Of Life (ER‐QOL). 22 Moreover, pain and perceived stress had been simultaneously measured in one study, through the Perceived Stress Questionnaire (PSQ). In another study, it had been assessed with the Perceived Stress Scale (PSS) 33 and patients' general health status had been evaluated via the 36‐item Short‐Form Health Survey (SF‐36). It should be noted that cortisol levels had been correspondingly measured in this study. 19 , 21
3.5. Quality assessment of articles
According to the scoring system of the Jadad Scale, five articles completely explained random allocation within three direct items. 6 , 11 , 19 , 22 , 33 One study had just mentioned randomization 20 and four articles had no trace of randomization at all. 9 , 12 , 13 , 21 In addition, all studies had completely described frequency and reasons for sample attrition. Among the articles reviewed with regard to the three direct items, only five cases were endowed with good quality, 6 , 11 , 19 , 22 , 33 and the other five studies had poor quality, 9 , 12 , 13 , 20 , 21 so that the final score for three articles was 3, 6 , 11 , 19 , 22 , 33 one was awarded with 2, 20 and four studies were assigned with 1 9 , 12 , 13 , 21 (Table 2).
TABLE 2.
Quality assessment of articles using the Jadad scale.
| No. | Authors/year | Jadad scale items (direct) | Total score | Quality | ||
|---|---|---|---|---|---|---|
| Was the study described as randomized? | Was the study described as double‐blinded? | Was there a description of withdrawals and dropouts? | ||||
| 1 | Hansen et al./2023 | 2 | 0 | 1 | 3 | Good |
| 2 | Ravins et al./2022 | 0 | 0 | 1 | 1 | Poor |
| 3 | Marcelo de França Moreira et al./2022 | 2 | 0 | 1 | 3 | Good |
| 4 | Hansen et al./2017 | 0 | 0 | 1 | 1 | Poor |
| 5 | Goncalves et al./2017 | 2 | 0 | 1 | 3 | Good |
| 6 | Meissner et al./2016 | 2 | 0 | 1 | 3 | Good |
| 7 | Kold et al./2012 | 0 | 0 | 1 | 1 | Poor |
| 8 | Friggi et al./2012 | 0 | 0 | 1 | 1 | Poor |
| 9 | Zhao et al./2012 | 2 | 0 | 1 | 3 | Good |
| 10 | Lorencatto et al./2007 | 1 | 0 | 1 | 2 | Poor |
4. DISCUSSION
In this systematic review, a total number of 10 articles evaluating the effects of psychological interventions on pain in women with EMS were examined, whose results could be submitted to healthcare providers to develop and implement effective psychological practices for pain relief in patients living with this condition and improve their quality of life.
CBT was one of the psychological interventions affecting pain in EMS women. In this line, Lorencatto et al. (2007), examining the effect of group‐based CBT on pain in women with EMS, stated that interventions with much focus on coping skills, stress management, as well as problem‐solving and cognitive techniques, had improved pain in women suffering from EMS (p < 0.0001). 20 The results of this study were not consistent with the reports of Friggi et al. However, Friggi et al. (2012), measuring the combined effects of physical therapy and CBT on pain in women with EMS, had shown that the results were not statistically significant, although the intervention had reduced pain (p > 0.05). Low sample size and lack of a control group were the main reasons for the non‐significant results of the given study. 21
One other psychological intervention relieving pain in EMS women was mindfulness. In Kold et al. (2012), the mindfulness‐based psychological intervention had thus mitigated pain in such patients, and the results had also remained stable during three (p = 0.005), six (p = 0.001), and 12 months after the intervention (p = 0.003). 12 The results of this study were consistent with those in Hansen et al. (2017) (p < 0.001), 9 and Moreira et al. (2022) (p = 0.001). 33 According to these studies, mindfulness minimized pain in women with EMS through reconceptualizing pain modulation from tissue, damage to general risk perception, movement mindfulness, discussions about unpleasant events, mental habits and behaviors, pleasant events, concentration on breathing techniques, body scanning, expression of feelings and emotions, stress management, and relaxation. 9 , 12 , 33 The results of these studies were not consistent with the reports by Hansen et al. (2022). In this study, although Specific mindfulness and ACT psychological interventions (namely, MY‐ENDO) reduced pain intensity and unpleasantness, not significantly. Low sample size, long‐time intervention sessions (3 h), and participants' fatigue were the reasons for the non‐significance of this study. 22
Yoga was also among other interventions affecting pain in women with EMS. In the word of Goncalves et al. (2015), yoga decreased pain in such patients (p = 0.0007). 6 The results of this study were consistent with the study by Rains et al. (2022) (p = 0.001). 13 As well, the pain pathway could be regulated by Gamma‐aminobutyric acid (GABA) as an inhibitory neurotransmitter in the brain. Practicing yoga on a regular basis could thus elevate the levels of GABA, which could facilitate the inhibitory action on the transmission of pain signaling. Yoga could further reduce the stress response with much focus on breathing techniques, meditation, and pain cascade by the downregulation of the hypothalamus‐pituitary–adrenal (HPA) axis and vague nerve stimulation (VNS). 6 , 13 , 34
Another intervention affecting pain in women with EMS was psychoeducation. In this regard, Meissner et al. (2016), exploring the effect of psychoeducation via somatosensory stimulation on pain in EMS patients reported that it had significantly reduced pain, especially after 3 months (p = 0.002). 11 In fact, this intervention had led to a decline in the levels of stress and negative emotions and had consequently induced relaxation in patients, thus alleviating pain in women with EMS, through much focus on psychological techniques, such as mindfulness, CBT, problem‐solving, hypnosis, as well as acupuncture techniques.
Besides, PMR training was another intervention to ease pain in women with EMS. Zhao et al. (2012) accordingly evaluated the effect of PMR training on pain in such women. This intervention reduced pain based on a classic muscle relaxation program developed by Jacobson (p < 0.001). 19
A general overview of the articles showed that psychological interventions, such as CBT, mindfulness therapy, yoga, and psychoeducation could be employed as effective practices to improve and reduce pain in women with EMS. In all the studies evaluated, the interventions had been also implemented by specialists, such as psychiatrists, 11 psychologists, 9 , 12 , 21 physiotherapists, 21 acupuncturists, yoga instructors, 6 , 13 as well as trained instructors in CBT and PMR. 20 In addition, long‐term follow‐ups in most articles (namely, 3, 6, 12, 24 months, and 6 years) as well as the consistency of the results in the follow‐ups could be one of the main reasons for employing such interventions as the effective ones to alleviate pain in women living with EMS. 6 , 9 , 11 , 12 Nevertheless, some of the most important factors had been overlooked. For example, there was no homogeneity between the intervention and control groups since the individuals in the intervention group had a higher level of education, which was significant. 6 In some articles, self‐report and the NRS had been used to measure pain in patients with EMS 11 , 13 , 22 ; however, it was better to utilize a standardized questionnaire to do so, like other studies. Furthermore, the study by Friggi et al. (2012) lacked a control group for better comparisons, which could decrease the generalizability and validity. 21
It should be noted that one of the limitations of this study was no access to the full texts of some articles.
5. CONCLUSION
The study results demonstrated that all the listed psychological interventions had affected pain relief and improvement in women with EMS. Considering the limited number of studies in this field and the fact that there were only five articles endowed with good quality, more high‐quality studies could provide stronger evidence to support the implementation of the mentioned psychological interventions influencing pain relief in EMS.
AUTHOR CONTRIBUTIONS
Elahe Samami: Writing the primary manuscript, manuscript preparation. Forouzan Elyasi: Contribution in the conception of the work, definition of intellectual content and intellectual and language editing of the manuscript. Zohreh Shahhosseini and Soghra Khani: Contribution in conceptual and language editing of the manuscript. The final manuscript was reviewed and approved by all the authors.
FUNDING INFORMATION
This study was funded by Mazandaran University of Medical Sciences (Grant number: 5563).
CONFLICT OF INTEREST STATEMENT
The authors declared no conflict of interest in this study.
ETHICS STATEMENT
Approval of the Research Protocol by an Institutional Reviewer Board: N/A.
Informed Consent: N/A.
Registry and the Registration No of the Study: The research proposal was also approved by the Ethics Committee affiliated to Mazandaran University of Medical Sciences, Sari, Iran (Code: IR.MUZUMS.REC.1398.1143).
Animal Studies: N/A.
ACKNOWLEDGMENTS
The authors are grateful to the Student Research Committee of Mazandaran University of Medical Sciences for supporting this research project.
Samami E, Shahhosseini Z, Khani S, Elyasi F. Pain‐focused psychological interventions in women with endometriosis: A systematic review. Neuropsychopharmacol Rep. 2023;43:311–320. 10.1002/npr2.12348
DATA AVAILABILITY STATEMENT
All data provided during this study are included in this article.
REFERENCES
- 1. Morotti M, Vincent K, Becker CM. Mechanisms of pain in endometriosis. Eur J Obstet Gynecol Reprod Biol. 2017;209:8–13. [DOI] [PubMed] [Google Scholar]
- 2. Greene AD, Lang SA, Kendziorski JA, Sroga‐Rios JM, Herzog TJ, Burns KA. Endometriosis: where are we and where are we going? Reproduction. 2016;152(3):R63–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Buggio L, Barbara G, Facchin F, Frattaruolo MP, Aimi G, Berlanda N. Self‐management and psychological‐sexological interventions in patients with endometriosis: strategies, outcomes, and integration into clinical care. Int J Womens Health. 2017;9:281–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Barnett R, Banks N, Decherney AH. Endometriosis and fertility preservation. Clin Obstet Gynecol. 2017;60(3):517–23. [DOI] [PubMed] [Google Scholar]
- 5. Mendes N, Figueiredo B. Psychological approach to endometriosis: women's pain experience and quality of life improvement. Psicologia Saúde e Doenças. 2012;13(1):36–48. [Google Scholar]
- 6. Goncalves AV, Barros NF, Bahamondes L. The practice of hatha yoga for the treatment of pain associated with endometriosis. J Altern Complement Med. 2017;23(1):45–52. [DOI] [PubMed] [Google Scholar]
- 7. Abbas S, Ihle P, Köster I, Schubert I. Prevalence and incidence of diagnosed endometriosis and risk of endometriosis in patients with endometriosis‐related symptoms: findings from a statutory health insurance‐based cohort in Germany. Eur J Obstet Gynecol Reprod Biol. 2012;160(1):79–83. [DOI] [PubMed] [Google Scholar]
- 8. Vercellini P, Vigano P, Somigliana E, Fedele L. Endometriosis: pathogenesis and treatment. Nat Rev Endocrinol. 2014;10(5):261–75. [DOI] [PubMed] [Google Scholar]
- 9. Hansen KE, Kesmodel US, Kold M, Forman A. Long‐term effects of mindfulness‐based psychological intervention for coping with pain in endometriosis: a six‐year follow‐up on a pilot study. Nord Psychol. 2017;69(2):100–9. [Google Scholar]
- 10. Aredo JV, Heyrana KJ, Karp BI, Shah JP, Stratton P. Relating chronic pelvic pain and endometriosis to signs of sensitization and myofascial pain and dysfunction. Semin Reprod Med. 2017;35(1):88–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Meissner K, Schweizer‐Arau A, Limmer A, Preibisch C, Popovici RM, Lange I, et al. Psychotherapy with somatosensory stimulation for endometriosis‐associated pain. Obstet Gynecol. 2016;128(5):1134–42. [DOI] [PubMed] [Google Scholar]
- 12. Kold M, Hansen T, Vedsted‐Hansen H, Forman A. Mindfulness‐based psychological intervention for coping with pain in endometriosis. Nord Psychol. 2012;64(1):2–16. [Google Scholar]
- 13. Ravins I, Joseph G, Tene L. The effect of practicing "endometriosis yoga" on stress and quality of life for women with endometriosis: AB design pilot study. Altern Ther Health Med. 2023;29:AT7514. [PubMed] [Google Scholar]
- 14. Flyckt R, Kim S, Falcone T. Surgical management of endometriosis in patients with chronic pelvic pain. Semin Reprod Med. 2017;35(1):54–64. [DOI] [PubMed] [Google Scholar]
- 15. Gallicchio L, Helzlsouer KJ, Audlin KM, Miller C, MacDonald R, Johnston M, et al. Change in pain and quality of life among women enrolled in a trial examining the use of narrow band imaging during laparoscopic surgery for suspected endometriosis. J Minim Invasive Gynecol. 2015;22(7):1208–14. [DOI] [PubMed] [Google Scholar]
- 16. Grand TS, Basarir H, Jackson LJ. The cost‐effectiveness of oral contraceptives compared to 'no hormonal treatment' for endometriosis‐related pain: an economic evaluation. PLoS One. 2019;14(1):e0210089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Taylor HS, Giudice LC, Lessey BA, Abrao MS, Kotarski J, Archer DF, et al. Treatment of endometriosis‐associated pain with Elagolix, an oral GnRH antagonist. N Engl J Med. 2017;377(1):28–40. [DOI] [PubMed] [Google Scholar]
- 18. Almassinokiani F, Khodaverdi S, Solaymani‐Dodaran M, Akbari P, Pazouki A. Effects of vitamin D on endometriosis‐related pain: a double‐blind clinical trial. Med Sci Monit. 2016;22:4960–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Zhao L, Wu H, Zhou X, Wang Q, Zhu W, Chen J. Effects of progressive muscular relaxation training on anxiety, depression and quality of life of endometriosis patients under gonadotrophin‐releasing hormone agonist therapy. Eur J Obstet Gynecol Reprod Biol. 2012;162(2):211–5. [DOI] [PubMed] [Google Scholar]
- 20. Lorençatto C, Vieira MJN, Marques A, Benetti‐Pinto CL, Petta CA. Evaluation of pain and depression in women with endometriosis after a multi‐professional group intervention. Rev Assoc Med Bras. 2007;53(5):433–8. [DOI] [PubMed] [Google Scholar]
- 21. Friggi Sebe Petrelluzzi K, Garcia MC, Petta CA, Ribeiro DA, de Oliveira Monteiro NR, Céspedes IC, et al. Physical therapy and psychological intervention normalize cortisol levels and improve vitality in women with endometriosis. J Psychosom Obstet Gynecol. 2012;33(4):191–8. [DOI] [PubMed] [Google Scholar]
- 22. Hansen K, Brandsborg B, Kesmodel U, Forman A, Kold M, Pristed R, et al. Psychological interventions improve quality of life despite persistent pain in endometriosis: results of a 3‐armed randomized controlled trial. Qual Life Res. 2023;32(6):1–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Samami E, Elyasi F, Mousavi Nasab N, Shojaee L, Zaboli E, Shahhosseini Z. Coping strategies‐oriented interventions in breast cancer women: a systematic scoping review of the quantitative evidence. Iran J Psychiatry Behav Sci. 2020;14(2):e99884. [Google Scholar]
- 24. Samami E, Elyasi F, Mousavinasab SN, Shojaee L, Zaboli E, Shahhosseini Z. Effect of non‐pharmacological interventions on stress of women with breast cancer undergoing chemotherapy: a systematic review. JMUMS. 2019;29(178):167–80. [Google Scholar]
- 25. Moosazadeh M, Hamzehgardeshi Z, Elyasi F, Janbabai G, Rezaei M. The effect of therapeutic‐supportive interventions on body image in women with breast cancer: a systematic review. J Health Field. 2017;5(1):32–42. [Google Scholar]
- 26. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. Int J Surg. 2010;8(5):336–41. [DOI] [PubMed] [Google Scholar]
- 27. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17(1):1–12. [DOI] [PubMed] [Google Scholar]
- 28. Li J, Liu Z, Chen R, Hu D, Li W, Li X, et al. The quality of reports of randomized clinical trials on traditional Chinese medicine treatments: a systematic review of articles indexed in the China National Knowledge Infrastructure database from 2005 to 2012. BMC Complement Altern Med. 2014;14(1):362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bridoux V, Moutel G, Roman H, Kianifard B, Michot F, Herve C, et al. Methodological and ethical quality of randomized controlled clinical trials in gastrointestinal surgery. J Gastrointest Surg. 2012;16(9):1758–67. [DOI] [PubMed] [Google Scholar]
- 30. Emami‐Sahebi A, Elyasi F, Yazdani‐Charati J, Shahhosseini Z. Psychological interventions for nausea and vomiting of pregnancy: a systematic review. Taiwan J Obstet Gynecol. 2018;57(5):644–9. [DOI] [PubMed] [Google Scholar]
- 31. Moosavi S, Rohani C. Critical appraisal of the randomized controlled trial studies reports in nursing journals. Iran J Nurs Res. 2016;11(3):37–47. [Google Scholar]
- 32. Wang G, Mao B, Xiong Z‐Y, Fan T, Chen X‐D, Wang L, et al. The quality of reporting of randomized controlled trials of traditional Chinese medicine: a survey of 13 randomly selected journals from mainland China. Clin Ther. 2007;29(7):1456–67. [DOI] [PubMed] [Google Scholar]
- 33. Moreira MF, Gamboa OL, Pinho Oliveira MA. A single‐blind, randomized, pilot study of a brief mindfulness‐based intervention for the endometriosis‐related pain management. Eur J Pain. 2022;26(5):1147–62. [DOI] [PubMed] [Google Scholar]
- 34. Gupta S, Gautam S, Kumar U, Arora T, Dada R. Potential role of yoga intervention in the management of chronic non‐malignant pain. Evid Based Complement Alternat Med. 2022;2022:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data provided during this study are included in this article.


