Abstract
Background
. Low back pain is one of the major causes of morbidity worldwide. Studies on low back pain quality of care are limited. This study aimed to evaluate the quality of care of low back pain worldwide and compare gender, age, and socioeconomic groups.
Methods
. This study used GBD data from 1990 to 2017 from the Institute for Health Metrics and Evaluation (IHME) website. Extracted data included low back pain incidence, prevalence, disability-adjusted life years (DALYs), and years lived with disability (YLDs). DALYs to prevalence ratio and prevalence to incidence ratio were calculated and used in the principal component analysis (PCA) to make a proxy of the quality-of-care index (QCI). Age groups, genders, and countries with different socioeconomic statuses regarding low back pain care quality from 1990 to 2017 were compared.
Results
The proxy of QCI showed a slight decrease from 36.44 in 1990 to 35.20 in 2017. High- and upper-middle-income countries showed a decrease in the quality of care from 43.17 to 41.57 and from 36.37 to 36.00, respectively, from 1990 to 2017. On the other hand, low and low-middle-income countries improved, from a proxy of QCI of 20.99 to 27.89 and 27.74 to 29.36, respectively.
Conclusion
. Despite improvements in the quality of care for low back pain in low and lower-middle-income countries between 1990 and 2017, there is still a large gap between these countries and higher-income countries. Continued steps must be taken to reduce healthcare barriers in these countries.
Keywords: Low back pain, Epidemiology, Burden, DALY, YLD
Introduction
Low back pain is one of the common causes of morbidity worldwide, with a one-month prevalence of 23.2% [1]. The point prevalence of low back pain has decreased in recent years from 8.2% in 1990 to 7.5% in 2017; however, the number of people with low back pain worldwide has increased from 377.5 million in 1990 to 577 million in 2020 [2]. Low back pain has been the leading cause of years lived with disability (YLDs) from 1990 (42.5 million YLD, 95% Uncertainty Interval (UI) 30.2 to 57.2) to 2017 (64.95 million YLDs, 95% UI 46.5 to 87.4) [2, 3]. The highest incidence of low back pain is in people in their third decade of age [4], and the prevalence of low back pain increases with age, with the highest prevalence in adults aged 80–89 years [2]. There are discrepancies in studies regarding the prevalence of low back pain in males and females. In a systematic review, Fatoye et al. found that in most studies, the prevalence of low back pain has been higher among males [5]; however, based on the global burden of diseases (GBD) project’s data, the point prevalence of low back pain has been higher in females throughout the years [2].
Although low back pain is a major public health issue for people with different demographic characteristics, disparities exist regarding people’s care for low back pain. Taylor et al. reported differences exist between the care people receive for low back pain based on gender and ethnicity [6]. For example, they found that physicians are more likely to suggest surgical treatment or order imaging evaluations for white subjects than black subjects. There were also differences between genders regarding the recommendation of surgical treatment and imaging evaluations [6]. As all patients need appropriate care and services for the treatment of pain, such disparities in the care they receive, which are partly due to their gender and ethnicity, may lead to major health problems globally.
Many health system quality studies consider access to medical services as an indicator of the quality of care. On the other hand, there is a consensus that over-treatment of low back pain has led to worse care [7–9]. In light of the over-treatment paradox, it is clear that access to high-end medical facilities and services cannot be the only index in assessing low back pain care. Quality of care metrics based on public health metrics like prevalence, incidence, and disease burden can help assess the quality of care based on a condition’s actual status instead of merely access indices. GBD health metrics can be incorporated into one score through a principal component analysis, named the Quality of Care Index (QCI), which can help determine care quality and inequality among age and gender subgroups [10–12]. QCI has been used to evaluate the quality of care for several chronic and potentially fatal diseases, including thyroid cancers, brain cancers, and hematological cancers [10–12].
While there are many studies on the consequences and cost-effectiveness of each treatment option for low back pain [8], there is a scarce number of studies on the quality and equality of care for low back pain in geographical, gender, and age categories. In addition, while the quality of care studies are feasible in developed countries because of registries [13–15], the need for registries in developing countries prevents comparing different health systems in low back pain care. Therefore, in our sight of view defining an Index that could demonstrate the disparity of low back pain care across different locations and genders would be extremely valuable in setting future goals. To the best of our knowledge, although there were recent studies about the burden of low back pain in GBD [16, 17], this is the first study aimed to determine the global quality and equality of low back pain care in various geographical, gender, and age categories using GBD data and the newly designed QCI.
Methods
Overview and data resources
This study used GBD data from 1990 to 2017 from the Institute for Health Metrics and Evaluation (IHME) website, which employs estimation models for input data from a wide range of resources. IHME provides GBD data using a systematic strategy to explain epidemiologic data on various diseases and risk factors stratified by sex, age, and geographic areas in different categories of nations and regions [3, 18]. The low back pain data is available on the GBD-compare webpage under the GBD code “B.11.3” in the “Causes” section. IHME defines low back pain as “pain in the area on the posterior aspect of the body from the lower margin of the twelfth ribs to the lower gluteal folds (with or without pain referred into one or both lower limbs) that lasts for at least one day. “ GBD is fully aligned with the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) Statement, which aims to improve the accuracy and quality of population health research [19]. A review of the methodological design behind the GBD results is outside the scope of our work and has been reported previously and is accessible on the website [18].
A Proxy of quality of care index
This descriptive study uses GBD metrics to report the current status of low back pain and assess the quality and equality of low back pain care across geographic, gender, and age categories.
Disability-adjusted life years (DALYs) is defined as the sum of years of life lost to early death (YLLs) and YLDs. As no mortality has been reported for low back pain, YLL is negligible, and DALYs and YLD can be used interchangeably in the case of low back pain [20]. YLD = P*DW, where P = prevalence, DW = disability weight of specific disease. So YLD/prevalence = DW is independent of prevalence, and so is DALYs/prevalence. Therefore, DALYs/prevalence shows the burden of low back pain regardless of its prevalence.
Two secondary indices were generated to assess the quality-of-care parameters in this study.
DALYs to Prevalence Ratio = DALYs/prevalence.
Prevalence to Incidence Ratio = prevalence/incidence.
It was assumed that increases in both measures might show deterioration in care for low back pain. It can be argued that in an episodic and self-limiting condition such as low back pain, the success of care can be defined as shortening episodes, preventing the disease from becoming chronic, and reducing recurrence. The prevalence/incidence would show how long a new low back pain episode will likely last cumulatively until the next year.
These two metrics (prevalence/incidence and DALYs/prevalence) were then combined in a principal component analysis (PCA) to obtain a single score for quality of care, named a proxy of QCI. It should also be noted that we used age-standardized values to calculate the metrics prior to calculating the proxy of QCI. The QCI was calculated beforehand and used in some GBD studies to show care quality and equality [10–12]. As QCI for low back pain due to zero death rate lacked one secondary index in calculations, it was called a proxy of QCI instead of the QCI.
Low back pain care in high-income, high middle income, lower middle income, and low-income countries (based on world bank classifications) [21] and in the age categories of 15–59 years and over 60 years were compared. The classification of countries was based on the World Bank country reports on income levels. Based on previous studies showing that the prevalence of low back pain gradually increases from the teenage years to 60 years of age and then decreases, we chose the categories 15–59 and over 60 years old to assess the impact of age on the index of care [22].
Gender disparity ratio
To yield insight into the disparity of quality of care services between males and females with LBP, the gender disparity ratio (GDR) was used. It was calculated by dividing males’ proxy of QCI by females’ QCI across countries. A GDR equal to 1 indicates no gender disparity. However, values lower or higher than one was indicative of disparity against males and females, respectively.
Validation of the Proxy of QCI
To validate the proxy of QCI, a mixed model was used to compare it to the Healthcare Access and Quality Index (HAQI) [23]. In this model, proxy of QCI was set as the dependent variable, and inpatient and outpatient health care utilization, DALY, and prevalence of LBP were set as independent parameters, with different nations considered as random effects parameters of the model. The Pearson’s correlation coefficient between the predicted values with the HAQI was 0.77, indicating an acceptable correlation [24].
Statistical analysis
Based on the GBD study, primary index values were reported with a 95% uncertainty interval (UI) of all age numbers and age-standardized rates per 100,000 population, and if the UIs of two strata did not overlap, shifting trends were regarded as significant [25]. For the analysis, age-standardized indices were used to compare countries with different age structures. Six-sigma tests were used to investigate the distribution of outliers in GBD metrics.
The secondary indices were combined in a PCA model to obtain a single score for quality of care measurement. PCA is a multivariable statistical technique that results in uncorrelated components through a linear combination of variables [26]. The first emerged component of PCA carries the most information about input variables. This component was termed a proxy of QCI and created a scale from 0 to 100, with 0 representing low quality and 100 representing the optimal quality of care. The calculated score was then used to compare the proxy of quality of care across geographic, gender, and age categories. Gender equality was assessed by dividing the score of males of each country to the scores of females, any deviation from 1 would indicate gender inequality.
All statistical analyses and plots were performed by R statistical packages v3.6.1 (http://www.r-project.org/, RRID: SCR _001905) [27]. Additional details of the calculation and codes are available in a previously published protocol about the QCI [28].
Results
Incidence, prevalence, DALYs, and other epidemiologic indices
The age-standardized point prevalence, incidence, and YLD of LBP in the world by sex in 1990 and 2017 are summarized in Table 1. The results show that in 2017 about 552 (95% UI 491 to 621) million people suffered from LBP worldwide, and the prevalence of LBP was 7013.7 (6247.9 to 7891.9) per 100,000 people in the world. Compared to 1990, 43% more people were affected by low back pain in 2017, but the prevalence rate of low back pain decreased by 16%. There were higher crude incidence and YLD in 2017 than in 1990, but the incidence and YLD rate per 100,000 people decreased by 13.7% and 15.9%, respectively. Furthermore, the prevalence, incidence, and YLD age-standardized rates of LBP in females were higher than in males in both years.
Table 1.
Global prevalence, incidence, and YLD across countries and age-standardized rates for both sexes, females, and males, in 1990 and 2017 (with 95% uncertainty interval (UI))
| Prevalence | Incidence | DALYs (YLD) | ||||
|---|---|---|---|---|---|---|
| Cases (million) | Rate (per 100,000) | Cases (million) | Rate (per 100,000) | YLD (million) | Rate (per 100,000) | |
| 1990 | ||||||
| Both | 386 (343 to 434) | 8341.1 (7389.8 to 9370.1) | 149 (131 to169) | 3168.9 (2799.7 to 3572.9) | 43 (31 to 58) | 932.5 (658.5 to 1248.3) |
| Female | 224 (199 to 253) | 9528.3 (8455.2 to 10736.5) | 85 (75 to 96) | 3550.6 (3141.5 to 4008.1) | 25 (33 to 18) | 1059 (748.5 to 1414.0) |
| Male | 161 (143 to 181) | 7085.9 (6299.5 to 7939.4) | 64 (56 to 73) | 2770.2 (2447.1 to 3131.8) | 18 (13 to 24) | 799.3 (562.0 to 1069.5) |
| 2017 | ||||||
| Both | 552 (491 to 621) | 7013.7 (6247.9 to 7891.9) | 216 (191 to 244) | 2748.9 (2428.7 to 3101.6) | 62 (43 to 83) | 785.1 (554.3 to 1051.5) |
| Female | 320 (285 to 360) | 7949.9 (7084 to 8961.1) | 124 (110 to 139) | 3086.9 (2735.7 to 3476.8) | 35(25 to 48) | 884.4 (626.1 to 1184.2) |
| Male | 232 (206 to 260) | 6022.4 (5362.9 to 6727.9) | 92 (81 to 105) | 2392.94 (2109.3 to 2703.9) | 26 (18 to 35) | 680.3 (478.9 to 909.9) |
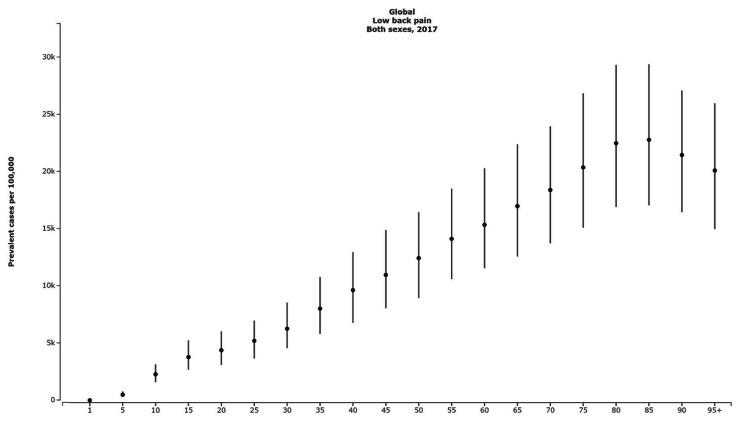
When comparing different age groups, the result showed that after a steady increase, the prevalence cases of LBP peaked in the age group of 85–89 years with 22,786.71 (17,047.44 to 29,402.05) cases per 100,000. This pattern was observed in both females and males in 2017. YLD and incidence rates also follow the same pattern, peaking in the 85–89 years age group for both sexes (Fig. 1).
Fig. 1.
The global point prevalence rate with 95% uncertainty intervals in different ages in 2017
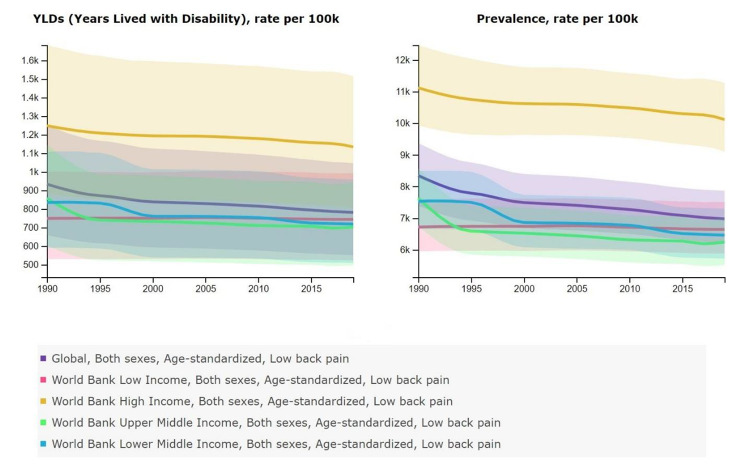
When comparing YLD and the prevalence of LBP between countries with different income levels, the results show the lower YLD and prevalence rate in 2017 compared to 1990 in all income levels. High-income level countries represent the highest YLD and prevalence rate of low back pain in 1990 and 2017. In 2017, The YLD and prevalence rate of high-income countries were 1,151.6 (816.6 to 1,538.5) and 10,261.31 (9,259.0 to 11,408.7) per 100,000 persons, respectively. In addition, upper-middle-income countries had the lowest YLD and prevalence rates in 2017 at 696.24 (491.16 to 930.20) and 6,186.76 (5,478.93 to 6,936.73) per 100,000 persons, respectively (Fig. 2).
Fig. 2.
Age-standardized YLD and Prevalence of low back pain, 1990–2017, in global level, in different income level countries
A proxy of the quality of care index
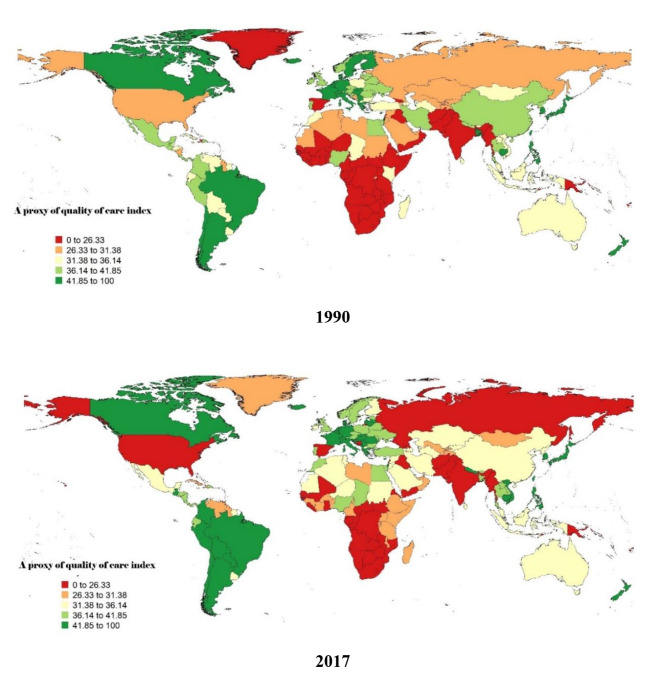
The proxy of QCI for low back pain was calculated to compare the quality and equity of low back pain care across countries (Fig. 3). The index showed a slight decrease from 36.44 in 1990 to 35.20 in 2017. High- and upper-middle-income countries showed a decrease in the quality of care from 43.17 to 41.57 and from 36.37 to 36.00, respectively, from 1990 to 2017. On the other hand, the quality of care in low and low-middle-income countries improved, from a proxy of QCI of 20.99 to 27.89 and 27.74 to 29.36, respectively. While the score for the 15–59 age category is better in high-income and upper-middle-income countries than for the over-60s in 2017, this is not the case in low-income and lower-middle-income countries, where the score for the 15–59 age category is lower than for the over-60s (Table 2).
Fig. 3.
A proxy of quality of care index (QCI) of Low back in 1990 and 2017(age standardized)
Table 2.
A proxy of quality of care index in countries with different income levels and two age categories of 15–59 and over 60 in 1990 and 2017
| Location | Year | Age category | Sex | DALY/Prevalence Ratio | Prevalence/Incidence Ratio | Low back pain care index |
|---|---|---|---|---|---|---|
| Global | 1990 | Age-standardized | Both | 0.11223 | 2.3657 | 36.44 |
| 2017 | 0.11242 | 2.3416 | 35.20 | |||
| High-income | 1990 | Age-standardized | Both | 0.11307 | 2.3745 | 43.17 |
| 2017 | 0.11301 | 2.3635 | 41.57 | |||
| Upper-middle-income | 1990 | Age-standardized | Both | 0.11241 | 2.3534 | 36.37 |
| 2017 | 0.11278 | 2.3249 | 36.00 | |||
| Lower-middle-income | 1990 | Age-standardized | Both | 0.11117 | 2.3526 | 27.74 |
| 2017 | 0.11170 | 2.3330 | 29.36 | |||
| Low-income | 1990 | Age-standardized | Both | 0.11058 | 2.3274 | 20.99 |
| 2017 | 0.11150 | 2.3325 | 27.89 | |||
| High-income | 1990 | 15–59 | Both | 0.11478 | 2.3848 | 44.48 |
| 2017 | 0.11478 | 2.3742 | 43.43 | |||
| Upper-middle-income | 1990 | 15–59 | Both | 0.11485 | 2.3476 | 41.34 |
| 2017 | 0.11507 | 2.3453 | 42.87 | |||
| Lower-middle-income | 1990 | 15–59 | Both | 0.11371 | 2.3399 | 31.51 |
| 2017 | 0.11423 | 2.3286 | 34.53 | |||
| Low-income | 1990 | 15–59 | Both | 0.11309 | 2.3019 | 22.76 |
| 2017 | 0.11392 | 2.3065 | 29.87 | |||
| High-income | 1990 | Over 60 | Both | 0.10342 | 2.6856 | 34.09 |
| 2017 | 0.10342 | 2.6640 | 32.65 | |||
| Upper-middle-income | 1990 | Over 60 | Both | 0.10208 | 2.6888 | 44.07 |
| 2017 | 0.10257 | 2.5895 | 34.04 | |||
| Lower-middle-income | 1990 | Over 60 | Both | 0.10068 | 2.6852 | 54.13 |
| 2017 | 0.10113 | 2.6431 | 48.11 | |||
| Low-income | 1990 | Over 60 | Both | 0.10087 | 2.6504 | 50.44 |
| 2017 | 0.10181 | 2.6711 | 44.91 |
Gender disparity ratio
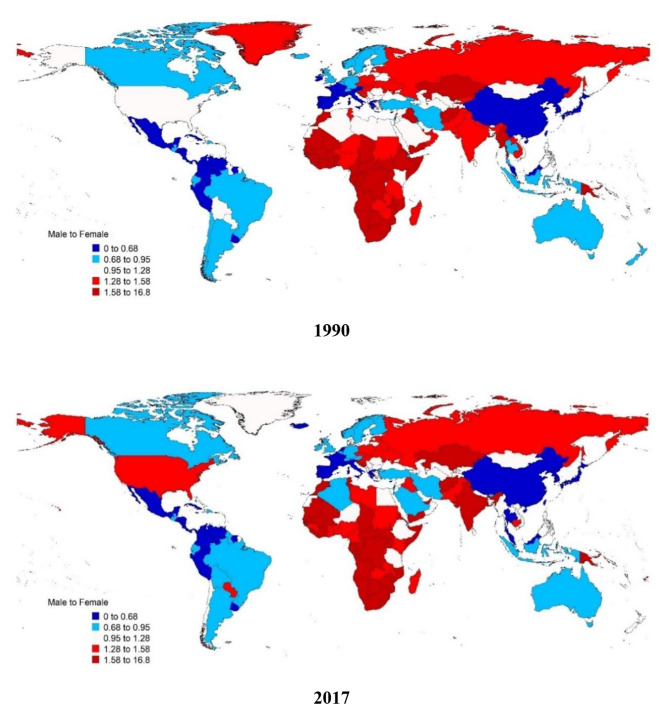
Gender inequality in the quality of care for low back pain is shown in Fig. 4. When comparing gender inequality, GDR decreased from 1.0100 in 1990 to 0.9802 in 2017, indicating that the proxy of QCI for men compared to women was lower in 2017 than in 1990. In addition, GDR in 2017 was lower than 1 in high-income and upper-middle-income countries, which means a higher quality of care for women compared to men, and it was higher than 1 in low-income and lower-middle-income countries, which indicates that a higher quality of care for men compared to women in these countries (Table 3). Furthermore, the scatter plot of QCI based on gender between different regional categories showed no pattern between specific regional categories. (Fig. 5).
Fig. 4.
Gender inequity in a proxy of the quality-of-care index (QCI) of Low back pain, 1990, 2017
Table 3.
Gender Inequality of the proxy of quality of care index for low back pain in different income level countries in both sexes in 1990 and 2017
| Location | Year | Age category | Sex | DALY/Prevalence Ratio | Prevalence/Incidence Ratio | Low back pain care index | Gender disparity ratio |
|---|---|---|---|---|---|---|---|
| Global | 1990 | Age-standardized | Male | 0.11175 | 2.3295 | 37.97 | 1.0100 |
| Female | 0.11288 | 2.3914 | 37.59 | ||||
| Global | 2017 | Age-standardized | Male | 0.11298 | 2.3170 | 35.34 | 0.9802 |
| Female | 0.11197 | 2.3596 | 36.05 | ||||
| World Bank High-Income | 2017 | Age-standardized | Male | 0.11347 | 2.3413 | 34.55 | 0.8195 |
| Female | 0.11262 | 2.3791 | 42.16 | ||||
| World Bank Upper-Middle-Income | 2017 | Age-standardized | Male | 0.11343 | 2.2944 | 28.42 | 0.7653 |
| Female | 0.11231 | 2.3473 | 37.13 | ||||
| World Bank Lower-Middle-Income | 2017 | Age-standardized | Male | 0.11242 | 2.3161 | 40.02 | 1.3692 |
| Female | 0.11114 | 2.3452 | 29.22 | ||||
| World Bank Low-Income | 2017 | Age-standardized | Male | 0.11105 | 2.3178 | 44.46 | 1.5381 |
| Female | 0.11192 | 2.3478 | 28.90 |
Fig. 5.
Countries scatter plots of a proxy of quality of care index (QCI) for female and male in 2017
Discussion
This is the first study to use GBD data with the newly developed proxy of QCI to assess the overall quality and equity of low back pain treatment across different geographic, gender, and age groups. Volinn et al. suggested that improvement in the indices to compare the quality of low back pain care in different countries was needed, as there are disparities regarding the prevalence of low back pain across countries [29]. In this study, we proposed a new method to compare and analyze the quality of care in different regions called the proxy of QCI. The low back pain GBD crude measures, such as prevalence and YLDs, were reported in a similar publication. Still in this study, we used these indicators to calculate secondary indices to highlight quality and equity of care in different areas and genders, making it more practical for policymakers [16, 17].
Despite the increase in the crude prevalence, incidence, and YLD in the results, this study showed that the prevalence, incidence, and YLD rate of low back pain per 100,000 individuals decreased between 1990 and 2017. The growth of the population from 1990 to 2017, from 5.33 to 7.55 billion, can be the main cause of the total rise in prevalence, incidence, and YLD [30]. Furthermore, the global median age has increased in recent decades [31]. Evidence also indicates that a history of low back pain is the single most significant predictor of future low back pain, suggesting that older adults have a greater chance of developing subsequent low back pain [32]. On the other hand, the lower prevalence and YLD rate per 100,000 might show an improvement in the quality of care and medical management through the disease between 1990 and 2017. Also, the lower incidence rate can be due to lowering risk factors. For example, globally, the percentage of the population that smokes every day has decreased, which may play a role in decreasing the incidence and prevalence of low back pain, considering smoking as a risk factor for low back pain [33, 34]. Also, the higher quality of life and education due to globalization in recent decades can play an important role in decreasing the incidence rate of low back pain [35].
Results indicate that the female gender had the higher prevalence, incidence, and YLD age-standardized rate across years. In previous studies, it was shown that females are more prone to low back pain due to their higher pain sensitivity, lower lumber muscle mass, and typical changes in their lifecycle, including pregnancy, childbirth, hormonal imbalances, and menopause, which may all have a role in higher low back pain rates in females compared to males [36, 37].
Results showed that low back pain prevalence peaked at the 85–89 age group in 2017. The same pattern was observed for both sexes and incidence and YLD rates. The results are similar to previous studies, which showed that low back pain becomes more common with advancing age [22]. This may be attributed to low physical activity, osteoarthritis, spinal stenosis, and degeneration of joints in the lumbar spine [38, 39]. However, some evidence declined this relation [40].
Lower global prevalence and YLD rate of low back pain per 100,000 individuals with different socioeconomic statuses in 2017 compared to 1990 were shown in our results. As the proxy of QCI showed, it may be mainly due to the improvement of low-income and lower-middle-income countries in the quality of care for back pain and higher global educational level and lower poverty rates, which both boost health care among people [41]. However, the highest prevalence and YLD were among high-level income countries in 1990 and 2017, possibly due to better patient data registration and higher quality data in these countries. Also, it has been shown that people with worse socioeconomic status might be less sensitive to pain and might not seek care for less severe pain, which can lead to underestimation of the low back pain cases in countries with poor socioeconomic status [42].
Proxy of QCI showed a slight global decrease in the quality of care for low back pain from 36.44 in 1990 to 35.20 in 2017. While the low-income and lower-middle-income countries have improved in terms of quality of care for back pain, the high-income and higher-middle-income countries had lower quality of care in 2017 compared to 1990. Furthermore, it was shown that the highest quality of care in high-income and higher-middle-income countries was dedicated to those aged 15–59 years as opposed to lower and lower-middle-income countries, where people aged 60 years or older had the highest quality of care for low back pain. Older people have the highest prevalence and YLD, so this difference can explain why the quality of care for low back pain has decreased in high and higher-middle-income countries where older adults receive worse care than younger adults. Despite the improvement in low-income and low-middle-income countries in QCI, there is still a considerable difference compared to higher-income countries. It is documented that more healthcare expenditures lead to better healthcare. The low-income countries have the lowest expenditures, which can explain the difference between these countries and high-income countries in QCI [43]. The WHO reports between 2000 and 2017 showed that the health spending of low and middle-income countries increased annually by 6.3 and 7.8%, respectively, which may explain the increase in quality of care in these countries in 2017 compared to 1990 [44].
We also found out that while the global male-to-female quality of care has changed in favor of the female gender since 1990, it is not the case for all countries, and low and lower-middle-income countries show a male-to-female gap in favor of the male gender. Previous studies showed that women in low and lower-middle-income countries have more barriers to healthcare. Also, they have lower access to resources such as education, employment, and money, which are the main reasons for these societies undervalue women and prioritize men’s health [45, 46]. There is a need for interventions to increase awareness of gender norms and empower women to advocate for their health in these countries [47].
Limitations
There were no data regarding ethnicity in the GBD database, which is the main limitation of our study as there may be considerable differences in the quality of low back pain across ethnicities. Also, the heterogeneity and accuracy of data collection and reporting across countries may affect the results.
Conclusion
In this study, we introduced scale to examine the quality of care for low back pain in various regions, as well as the disparities in low back healthcare between men and women. Despite an increase in the quality of care for low back pain in low and lower-middle-income nations between 1990 and 2017, there is still a large gap between these countries and higher-income countries, which must take initiatives to enhance healthcare in these countries.
Authors’ contributions
Results and analysis were done by E.Gh, Ma.R, N.R, M.N, and A.Gh. All authors (M.Gh, E.Gh, Mo.R, Ma.R, N.R, M.N, K.D, A.N.A a, A.Gh, A.B, A.A.A, A.T, J.T, N.M, R.K) contributed in the writing of the manuscript and also read and approved the final manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Data Availability
The data that support the findings of this study are openly available in the Institute for Health Metrics and Evaluation (IHME) website at [https://gbd2017.healthdata.org/gbd-compare/] [48].
Declarations
Ethical approval
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, et al. A systematic review of the global prevalence of low back pain. Arthr Rhuem. 2012;64(6):2028–37. doi: 10.1002/art.34347. [DOI] [PubMed] [Google Scholar]
- 2.Wu A, March L, Zheng X, Huang J, Wang X, Zhao J et al. Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the global burden of Disease Study 2017. Annals of translational medicine. 2020;8(6). [DOI] [PMC free article] [PubMed]
- 3.Global regional. and National incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet (London, England). 2018;392(10159):1789–858. [DOI] [PMC free article] [PubMed]
- 4.Hoy D, Brooks P, Blyth F, Buchbinder R. The epidemiology of low back pain. Best Pract Res Clin Rheumatol. 2010;24(6):769–81. doi: 10.1016/j.berh.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 5.Fatoye F, Gebrye T, Odeyemi I. Real-world incidence and prevalence of low back pain using routinely collected data. Rheumatol Int. 2019;39(4):619–26. doi: 10.1007/s00296-019-04273-0. [DOI] [PubMed] [Google Scholar]
- 6.Taylor BA, Casas-Ganem J, Vaccaro AR, Hilibrand AS, Hanscom BS, Albert TJ. Differences in the work-up and treatment of conditions associated with low back pain by patient gender and ethnic background. Spine. 2005;30(3):359–64. doi: 10.1097/01.brs.0000152115.79236.6e. [DOI] [PubMed] [Google Scholar]
- 7.Buchbinder R, van Tulder M, Öberg B, Costa LM, Woolf A, Schoene M, et al. Low back pain: a call for action. The Lancet. 2018;391(10137):2384–8. doi: 10.1016/S0140-6736(18)30488-4. [DOI] [PubMed] [Google Scholar]
- 8.Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. The Lancet. 2018;391(10137):2368–83. doi: 10.1016/S0140-6736(18)30489-6. [DOI] [PubMed] [Google Scholar]
- 9.Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, et al. What low back pain is and why we need to pay attention. The Lancet. 2018;391(10137):2356–67. doi: 10.1016/S0140-6736(18)30480-X. [DOI] [PubMed] [Google Scholar]
- 10.Azadnajafabad S, Saeedi Moghaddam S, Mohammadi E, Rezaei N, Ghasemi E, Fattahi N, et al. Global, regional, and national burden and quality of care index (QCI) of thyroid cancer: a systematic analysis of the global burden of Disease Study 1990–2017. Cancer Med. 2021;10(7):2496–508. doi: 10.1002/cam4.3823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Keykhaei M, Masinaei M, Mohammadi E, Azadnajafabad S, Rezaei N, Moghaddam SS, et al. A global, regional, and national survey on burden and quality of Care Index (QCI) of hematologic malignancies; global burden of disease systematic analysis 1990–2017. Experimental Hematol Oncol. 2021;10(1):1–15. doi: 10.1186/s40164-021-00198-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mohammadi E, Ghasemi E, Azadnajafabad S, Rezaei N, Saeedi Moghaddam S, Ebrahimi Meimand S, et al. A global, regional, and national survey on burden and quality of Care Index (QCI) of brain and other central nervous system cancers; global burden of disease systematic analysis 1990–2017. PLoS ONE. 2021;16(2):e0247120. doi: 10.1371/journal.pone.0247120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gologorsky Y, Knightly JJ, Chi JH, Groff MW. The Nationwide Inpatient Sample database does not accurately reflect surgical indications for fusion. J Neurosurgery: Spine. 2014;21(6):984–93. doi: 10.3171/2014.8.SPINE131113. [DOI] [PubMed] [Google Scholar]
- 14.Martin BI, Mirza SK, Spina N, Spiker WR, Lawrence B, Brodke DS. Trends in lumbar fusion procedure rates and associated hospital costs for degenerative spinal diseases in the United States, 2004 to 2015. Spine. 2019;44(5):369–76. doi: 10.1097/BRS.0000000000002822. [DOI] [PubMed] [Google Scholar]
- 15.Saifi C, Cazzulino A, Laratta J, Save AV, Shillingford JN, Louie PK, et al. Utilization and economic impact of posterolateral fusion and posterior/transforaminal lumbar interbody fusion surgeries in the United States. Global Spine Journal. 2019;9(2):185–90. doi: 10.1177/2192568218790557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu A, March L, Zheng X, Huang J, Wang X, Zhao J, et al. Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the global burden of Disease Study 2017. Annals of Translational Medicine. 2020;8(6):299. doi: 10.21037/atm.2020.02.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen S, Chen M, Wu X, Lin S, Tao C, Cao H, et al. Global, regional and national burden of low back pain 1990–2019: a systematic analysis of the Global Burden of Disease study 2019. J Orthop Translation. 2022;32:49–58. doi: 10.1016/j.jot.2021.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Collaborators GBDCoD Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the global burden of Disease Study 2017. Lancet. 2018;392(10159):1736–88. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stevens GA, Alkema L, Black RE, Boerma JT, Collins GS, Ezzati M, et al. Guidelines for Accurate and Transparent Health estimates reporting: the GATHER statement. PLoS Med. 2016;13(6):e1002056. doi: 10.1371/journal.pmed.1002056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sarah Cuschieri GMAW, Neville, Calleja. Vanessa Gorasso & Brecht Devleesschauwer Measuring disability-adjusted life years (DALYs) due to low back pain in Malta. Archives of Public Health; 2020. [DOI] [PMC free article] [PubMed]
- 21.group TWB. World Bank Country and Lending Groups 2023 [Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
- 22.Wong AY, Karppinen J, Samartzis D. Low back pain in older adults: risk factors, management options and future directions. Scoliosis Spinal Disord. 2017;12:14. doi: 10.1186/s13013-017-0121-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Access GBDH, Quality C. Measuring performance on the Healthcare Access and Quality Index for 195 countries and territories and selected subnational locations: a systematic analysis from the global burden of Disease Study 2016. Lancet. 2018;391(10136):2236–71. doi: 10.1016/S0140-6736(18)30994-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mukaka MM. Statistics corner: a guide to appropriate use of correlation coefficient in medical research. Malawi Med J. 2012;24(3):69–71. [PMC free article] [PubMed] [Google Scholar]
- 25.AC R. A Review Of “Methods of Multivariate Analysis,Second Edition. IIE Trans. 2005:1083–5.
- 26.Saha R. Principal Component Analysis(PCA). 2020.
- 27.team DCR. A Language and Environment for Statistical ComputingTeam 2013.
- 28.Mohammadi E, Ghasemi E, Moghaddam SS, Yoosefi M, Ghanbari A, Ahmadi N, et al.Quality of care index (QCI). protocolsio. 2020;2021:24.
- 29.Volinn E. The epidemiology of low back pain in the rest of the world. A review of surveys in low- and middle-income countries. Spine (Phila Pa 1976). 1997;22(15):1747-54. [DOI] [PubMed]
- 30.Max Roser HRaEO-O. World Population Growth. Our World in Data. 2013.
- 31.Szmigiera M. World population - median age by fertility variant 1990–2100. Statista.2021.
- 32.Taylor JB, Goode AP, George SZ, Cook CE. Incidence and risk factors for first-time incident low back pain: a systematic review and meta-analysis. Spine J. 2014;14(10):2299 – 319. [DOI] [PubMed]
- 33.Mikkonen P, Leino-Arjas P, Remes J, Zitting P, Taimela S, Karppinen J. Is smoking a risk factor for low back pain in adolescents?: A prospective cohort study. Spine.2008;33(5):527 – 32. [DOI] [PubMed]
- 34.Feldman DE, Rossignol M, Shrier I, Abenhaim L. Smoking: a risk factor for development of low back pain in adolescents. Spine. 1999;24(23):2492. [DOI] [PubMed]
- 35.Stewart R. Despite declines in smoking rates, number of smokers and cigarettes rises. Institute for Health Metrics and Evaluation. 2014. [PubMed]
- 36.Wang YX, Wang JQ, Kaplar Z. Increased low back pain prevalence in females than in males after menopause age: evidences based on synthetic literature review. Quant Imaging Med Surg. 2016;6(2):199–206. [DOI] [PMC free article] [PubMed]
- 37.Hall KR, Stride E. The varying response to pain in psychiatric disorders: a study in abnormal psychology. Br J Med Psychol. 1954;27(1–2):48–60. [DOI] [PubMed]
- 38.Jones LD, Pandit H, Lavy C. Back pain in the elderly: a review. Maturitas. 2014;78(4):258 – 62. [DOI] [PubMed]
- 39.Bento TPF, Genebra CVdS, Maciel NM, Cornelio GP, Simeão SFAP, Vitta Ad. Low back pain and some associated factors: is there any difference between genders? Brazilian Journal of Physical Therapy. 2020;24(1):79–87. [DOI] [PMC free article] [PubMed]
- 40.Fejer R, Leboeuf-Yde C. Does back and neck pain become more common as you get older? A systematic literature review. Chiropractic & Manual Therapies. 2012;20(1):24. [DOI] [PMC free article] [PubMed]
- 41.Mohajerzadeh L, Ebrahimian M, Sarafi M, Ebrahimisaraj G, Tabatabaei SR, Noorbakhsh SM, et al. Effects of COVID-19 Pandemic on the Frequency of Complicated Appendicitis in Pediatric Populations. Archives of Pediatric Infectious Diseases. 2023;11(1).
- 42.Summers KM, Deska JC, Almaraz SM, Hugenberg K, Lloyd EP. Poverty and pain: Low-SES people are believed to be insensitive to pain. Journal of Experimental Social Psychology.2021;95:104116.
- 43.Schieber GJ, Poullier JP. Overview of international comparisons of health care expenditures. Health Care Financ Rev. 1989;Spec No:1–7. [PMC free article] [PubMed]
- 44.Organization WH. Global Spending on Health: A World in Transition. 2019.
- 45.Mariani G, Kasznia-Brown J, Paez D, Mikhail MN, D HS, Bhatla N, et al. Improving women’s health in low-income and middle-income countries. Part I: challenges and priorities.Nucl Med Commun. 2017;38(12):1019-23. [DOI] [PMC free article] [PubMed]
- 46.Shatilwe JT, Kuupiel D, Mashamba-Thompson TP. Evidence on access to healthcare information by women of reproductive age in low- and middle-income countries: Scoping review. PLoS One. 2021;16(6):e0251633. [DOI] [PMC free article] [PubMed]
- 47.Azad AD, Charles AG, Ding Q, Trickey AW, Wren SM. The gender gap and healthcare:associations between gender roles and factors affecting healthcare access in Central Malawi, June-August 2017. Arch Public Health. 2020;78(1):119. [DOI] [PMC free article] [PubMed]
- 48.Zhu Y, Sun A, Meng T, Li H. Protective role of long noncoding RNA CRNDE in myocardial tissues from injury caused by sepsis through the microRNA-29a/SIRT1 axis. Life Sciences. 2020;255:117849. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are openly available in the Institute for Health Metrics and Evaluation (IHME) website at [https://gbd2017.healthdata.org/gbd-compare/] [48].