Abstract
Background
Understanding perceptions of telehealth implementation from patients and providers can improve the utility and sustainability of these programs, particularly in under-resourced rural settings. The purpose of this study was to evaluate both patient and provider perceptions of telehealth visits in a large rural healthcare system during the COVID-19 pandemic. To promote sustainability of telehealth approaches, we also assessed whether the percentage of missed appointments differed between in-person and telehealth visits.
Methods
Using anonymous surveys, we evaluated patient preferences and satisfaction with telehealth visits from November 2020 -March 2021 and assessed perceptions of telehealth efficiency and value among rural providers from September–October 2020. We examined whether telehealth perceptions differed according to patients’ age, educational attainment, insurance status, and distance to clinical site and providers’ age and length of time practicing medicine using ANOVA test. We also examined whether the percentage of missed appointments differed between in-person and telehealth visits at a family practice clinic within the rural healthcare system from April to September 2020 using a Chi-square test.
Results
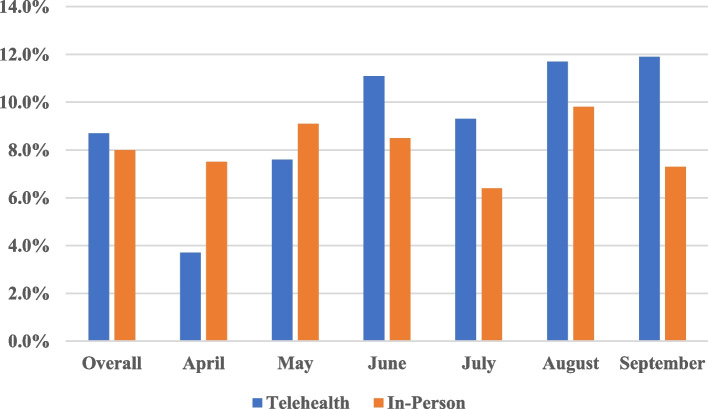
Over 73% of rural patients had favorable perceptions of telehealth visits, and satisfaction was generally higher among younger patients. Patients reported difficulty with scheduling follow-up appointments, lack of personal contact and technology challenges as common barriers. Over 80% of the 219 providers responding to the survey reported that telehealth added value to their practice, while 36.6% agreed that telehealth visits are more efficient than in-person visits. Perception of telehealth value and efficiency did not differ by provider age (p = 0.67 and p = 0.67, respectively) or time in practice (p = 0.53 and p = 0.44, respectively). Technology challenges for the patient (91.3%) and provider (45.1%) were commonly reported. The percentage of missed appointments was slightly higher for telehealth visits compared to in-person visits, but the difference was not statistically significant (8.7% vs. 8.0%; p = 0.39).
Conclusions
Telehealth perceptions were generally favorable among rural patients and providers, although satisfaction was lower among older patients and providers. Our findings suggest that telehealth approaches may add value and efficiency to rural clinical practice. However, technology issues for both patients and providers and gaps in care coordination need to be addressed to promote sustainability of telehealth approaches in rural practice.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-023-09994-4.
Keywords: Telehealth, Telemedicine, COVID-19, Rural, Implementation, Provider, Barriers
Introduction
Telehealth approaches hold tremendous potential to address healthcare access barriers, particularly in geographically disperse rural settings, where patients often travel longer distance to receive care [1–3]. The efficacy of telehealth for provision of clinical care has been demonstrated in multiple settings [4–8]. In a systematic review of the literature, telehealth visits were consistently associated with high patient satisfaction and improved clinical outcomes [9]. Moreover, telehealth visits have been shown to add quality and value to clinical practice by improving efficiency, enhancing convenience for patients and providers alike, [10] and reducing provider stress and burnout [11, 12]. Burgeoning evidence also suggests that telehealth approaches may enable accessible care by reducing missed healthcare appointments [13].
Despite the well-documented benefits of telehealth approaches, numerous barriers have impeded the widespread adoption of telehealth in clinical care. Commonly reported barriers to telehealth include the necessity of physical exams, technological literacy, cost and reimbursement challenges, and privacy and security concerns [14–16]. Nevertheless, the use of telehealth visits in clinical practice has increased in recent years, doubling from 14% of visits in the US in 2016 to 28% in 2019, [10] and expanding rapidly in response to the COVID-19 pandemic [17–19]. The rapid adoption of telehealth in clinical practice has been bolstered by expanded reimbursements for telehealth visits in an effort to promote continued access to care and prevent COVID-19 transmission [19, 20].
Important lessons from this period of deregulation can be used to inform post-pandemic telehealth regulations and maintain the momentum of telehealth approaches moving forward [19]. Indeed, given the substantial investment in telehealth infrastructure and training in response to the COVID-19 pandemic, there is strong impetus for health systems to systematically evaluate telehealth implementation efforts and to characterize perceptions of telehealth from both patient and provider perspectives. This is particularly relevant for rural populations who arguably stand to benefit most from telehealth approaches [1–3]. However, to our knowledge, no prior studies have simultaneously examined rural provider and patient perspectives of telehealth implemented during the COVID-19 pandemic. It is also unclear whether the transition to telemedicine has impacted the likelihood of missed healthcare appointments in rural clinical settings.
Thus, the purpose of this study was to evaluate patient and provider perceptions of telehealth visits implemented at a large rural healthcare system during the COVID-19 pandemic. We sought to identify patient and provider barriers that may limit telehealth’s broader adoption, and assessed whether the percentage of missed appointments differed between in-person and telehealth visits.
Materials and methods
Study setting and procedures
This study was conducted at Munson Healthcare (MHC), a large rural healthcare system serving over 500,000 residents across 30 rural counties in Northwest Michigan. The patient survey was distributed at Munson Family Practice Center (MFPC), a MHC-owned family practice office located directly adjacent to Munson Medical Center, the flagship community hospital of the MHC system.
All patients seen during the study period 11/2/2020 to 3/24/2021 were asked by office staff at telehealth visit check-in to complete the voluntary and anonymous online survey to assess telemedicine perceptions. Those who agreed to participate were sent a secure link to the survey following completion of their visit. With a MFPC patient population of 12,000, we aimed to collect 100 surveys to promote representativeness of the target patient population, using a confidence level of 95% and a 10% margin of error. Providers across the MHC system were sent an emailed link from the MHC digital health team to complete the voluntary and anonymous online provider survey. The online survey was developed using SurveyMonkey and the survey link was distributed via email from the MHC telehealth coordinator to 1,180 MHC providers and MHC-affiliated and independent healthcare providers from September 1, 2020 to October 1, 2020. A retrospective review of electronic health records for all patients with scheduled appointments at Munson Family Practice Center from April 2020 to September 2020 was conducted to assess the number missed visits by visit type (telehealth vs. in-person) as noted in the medical record.
Patient survey
The 12-question survey was based on a survey used in a prior study, [21] and assessed telehealth use, reason for use, and telehealth perceptions and barriers. Participants were asked to rate perceptions of telehealth on a Likert-scale ranging from “Strongly Disagree” to “Strongly Agree”. Perceptions of telehealth were assessed using the following statements; “I like using telehealth visits”, “Telehealth visits are convenient”, “I am likely to request a telehealth visit in the future”, “I received high quality care”, “There was an efficient process for check-in”, “There was an efficient process for check-out/follow up”, “It is important that my healthcare provider be physically in the room”, “I felt comfortable with the plan of care and follow up”, “Telehealth was a reasonable way to maintain social distancing and stay at home orders during the COVID-19 pandemic while receiving health care services”, I am glad that I had the option for telehealth offered to me during the COVID-19 pandemic.” Participants were also asked to select reasons for liking telehealth from the following options: “I feel safer by reducing person-to-person contact during COVID-19″, “Less travel time”, “More convenient for my personal schedule”, “I do not need additional child care services”, “Less waiting time between check-in and seeing provider”. Participants were also asked to select reasons for disliking telehealth visits from the following options: “I did not have personal contact with my healthcare provider”, “I had technology problems or interruptions”, “Follow up was difficult to schedule”, “There was a barrier to communication (example: difficulty in accessing Medical Translation Services)”, “Other (please specify)”. Participants were asked to specify reasons for requesting telehealth visits in the future, and reasons why they would not request a telehealth visit in the future using open-ended text responses. Finally, participants were asked whether they experienced any of the following technical problems or barriers with telehealth visits; “Lack of smart phone, tablet, or computer”, “Internet/WIFI difficulties”, “Software or app problems”, “I have not experienced any technical problems/barriers”. Information on demographic factors (age, educational attainment, health insurance status, and approximate travel time in minutes from home to the clinic) were also ascertained.
Provider survey
We utilized a 14-question survey generated from a prior study conducted by the American Medical Association [10] to assess telehealth preferences and impact on clinical practice. Inclusion criteria included all providers including physicians, nurse practitioners, and physician assistants who had participated in either a video or telephone visit at MHC in the past 3 months. The primary outcome of interest was the perception of quality and value that telehealth visits may have added to rural clinical practice. Secondary outcomes evaluated included barriers to use and provider’s perceptions on the types of visits where telehealth worked well (e.g., acute care, Medicare wellness).
Statistical analyses
Descriptive statistics were used to summarize the patient and provider survey data. We used ANOVA tests to evaluate differences in perception of telehealth visits according to patient age, educational attainment, insurance status, distance to the clinic, and reason for clinic visit. We assessed whether provider telehealth perceptions significantly differed by provider age and length of time practicing medicine using ANOVA tests with p-values < 0.05 considered significant. In secondary exploratory analyses, we compared the percentage of all missed visits across groups defined by visit type (telehealth vs. in-person) using Chi-square tests with p-values < 0.05 considered significant. All analyses were performed with SAS version 9.4 statistical software. The study was approved by the Munson Healthcare Institutional Review Board.
Results
Patient characteristics
Overall, 100 patients responded to the patient survey, with 93 providing information on telehealth perceptions included in this study analysis. As shown in Table 1, 56% of patients surveyed were between 35 and 64 years of age and nearly a quarter of the rural patient population travelled over 30 min to the clinic. Over half of patient participants had high school education or less, and 25% received Medicaid. Study participants were seen virtually for a variety of reasons including for medication review (22.6%), to report a new problem (20.4%), follow-up on health issue (17.2%), new patient visit (17.2%), transition of care (14.0%), behavioral health (12.9%) and other wellness and/or rehabilitation check in (3.3%).
Table 1.
Characteristics of rural patients (n = 93) and providers (n = 219)
|
Patients N (%) |
Providers N (%) |
||
|---|---|---|---|
| Age, years | Age, yearsc | ||
| 18–25 | 6 (6.5%) | 25–30 | 13 (6.9%) |
| 26–34 | 21 (22.2%) | 31–40 | 44 (23.3%) |
| 35–50 | 22 (23.7%) | 41–50 | 57 (30.2%) |
| 51–64 | 30 (32.3%) | 51–65 | 67 (35.5%) |
| > 65 | 14 (15.1%) | > 65 | 8 (4.2%) |
| Educational Attainment | Years Practicing Medicinec | ||
| < High School | 3 (3.2%) | Resident | 14 (7.4%) |
| High School Graduate | 48 (51.6%) | < 5 | 26 (13.8%) |
| Some College | 22 (23.7%) | 5–10 | 24 (12.7%) |
| Bachelor’s Degree | 17 (18.3%) | 11–20 | 50 (26.5%) |
| Graduate School | 3 (3.2% | 21–30 | 55 (29.1%) |
| > 30 | 20 (10.6%) | ||
| Insurance Statusa | |||
| No Insurance | 6 (3.2%) | Type of Practiced | |
| Medicare | 14 (15.2%) | Munson Healthcare owned | 104 (54.7%) |
| Medicaid | 23 (25.0%) | Independent | 86 (45.3%) |
| Commercial | 49 (53.3%) | ||
| Time Spent Travelling to Clinic | |||
| 10 min or less | 3 (3.2%) | ||
| 11–20 min | 24 (25.8%) | ||
| 21–30 min | 44 (47.3%) | ||
| More than 30 min | 22 (23.7%) | ||
| Reason for Visitb | |||
| Transition of care | 13 (14.0%) | ||
| Medication review | 21 (22.6%) | ||
| Behavioral health | 12 (12.9%) | ||
| New patient visit | 16 (17.2%) | ||
| Report new problem | 19 (20.4%) | ||
| Follow-up on health issue | 16 (17.2%) | ||
| Wellness/rehabilitation check | 3 (3.3%) | ||
aMissing information on insurance status for 1 patient
bNumber of patients exceeds the sample size as patients could list multiple reasons
cMissing information on age and years practicing medicine for 30 providers
dMissing information on type of practice for 19 providers
Provider characteristics
For the provider survey, 252 providers (24.8%) completed the survey, with 219 providers (86.9%) reporting telehealth use in the past 3 months included in this analysis. The age range of providers was normally distributed, with nearly 66% of providers between the ages of 41–65 years (Table 1). The majority of providers had been practicing medicine for 11–20 years (26.5%) or between 21–30 years (29.1%) and most were MHC providers (54.7%).
Patient perceptions
Patient participants had favorable perceptions of telehealth visits, with over 73% either agreed or strongly agreed that they liked using telehealth (Table 2). 97 percent of patients strongly agreed/agreed telehealth is convenient and 94% strongly agreed/agreed that telehealth offers a reasonable option to maintain social distancing during the pandemic. Patients’ responses were less favorable with regard to the efficiency of the check-out process with only 28% strongly agreed/agreed that the process was efficient, yet 47% of patients strongly agreed/agreed they were likely to request a telehealth visit in the future. Nearly 50% of patients agreed or strongly agreed that it was important to have their healthcare provider be physically in the room. Interestingly, favorable overall perceptions of telehealth visits differed according to patient age, with generally higher favorability among younger patients. For example, patients ages 18–25 years reported average score of 4.5 on the statement “I like using telehealth visits” (on scale of 1 = strongly disagree to 5 = strongly agree), compared to 3.5 among those 51–64 years and 4.0 among those 65 years and older; p = 0.007). Overall telehealth perception did not vary significantly according to patient’s educational attainment (p = 0.15), insurance status (p = 0.72), distance travelled to the clinic (p = 0.49), or according to the type of telehealth visit (p = 0.10).
Table 2.
Rural patient perceptions of telehealth visits (n = 93)
| Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree | |
|---|---|---|---|---|---|
| I like using telehealth visits | 33.3% | 39.8% | 20.4% | 4.3% | 2.2% |
| Telehealth visits are convenient | 44.1% | 52.7% | 3.2% | 0.0% | 0.0% |
| I am likely to request a telehealth visit in the future | 18.3% | 29.0% | 38.7% | 9.7% | 4.3% |
| I received high quality care | 12.9% | 51.6% | 32.3% | 2.2% | 1.1% |
| There was an efficient process for check-in | 9.7% | 54.8% | 28.0% | 7.5% | 0.0% |
| There was an efficient process for check-out | 4.3% | 14.0% | 38.7% | 40.9% | 2.2% |
| It is important that my healthcare provider be physically in the room | 7.5% | 39.8% | 50.5% | 2.2% | 0.0% |
| I felt comfortable with the plan of care and follow-up | 6.5% | 63.4% | 25.8% | 4.3% | 0.0% |
| Telehealth was a reasonable way to maintain social distancing and stay at home orders during the COVID-19 pandemic while receiving healthcare services | 49.5% | 44.1% | 6.5% | 0.0% | 0.0% |
| I am glad that I had the option for telehealth offered to me during the COVID-19 pandemic | 40.9% | 33.3% | 18.3% | 5.4% | 2.2% |
Provider perceptions
Providers’ perceptions of telehealth visits are shown in Table 3. Over 80% of providers strongly agreed or agreed that telehealth added value to their practice. The perception of telehealth efficiency was slightly lower than perceived value, with 36.6% of providers strongly agreeing (12.9%) or agreeing (23.7%) that a telehealth visit is more efficient than an in-person visit. Perception of telehealth value and efficiency did not differ significantly by providers’ age (p = 0.67 and p = 0.67, respectively) or time in practice (p = 0.53 and p = 0.44, respectively). However, the perception of telehealth’s value was generally lower among older providers, with 84.6% of providers aged 25–30 years and only 57.2% of providers aged 65 years and older agreeing or strongly agreeing that telehealth visits added value to practice. The majority of providers strongly agreed or agreed that telehealth impacted clinical practice by improving access to care (90.1%), timeliness of care (70.4%), the safety of patients (66.4%) and patient and family-centered care (54.4%). The types of medical visits most highly suited for telehealth in this study were anxiety/depression, mental health visits, COVID-19 assessments, and Diabetes. Providers in this study predicted continued use of telehealth, with just over half selecting the range of 1–10% for the amount of their patient visits which would be conducted virtually moving forward.
Table 3.
Rural provider perceptions of telehealth visits (n = 219)
| Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree | |
|---|---|---|---|---|---|
| Adds Value | 33.2% | 47.2% | 10.9% | 7.3% | 1.6% |
| Adds Efficiency | 12.9% | 23.7% | 25.8% | 27.8% | 9.8% |
| Telehealth has impacted my practice by improving: | |||||
| The health of my patients | 11.7% | 35.6% | 39.9% | 12.8% | 0.0% |
| The safety of my patients | 19.2% | 47.2% | 21.8% | 7.8% | 4.2% |
| Timeliness of care of my patients | 16.7% | 53.7% | 21.4% | 5.2% | 3.1% |
| Patient and Family Centered-Care | 12.3% | 42.1% | 29.2% | 12.9% | 3.5% |
| Access to care | 30.9% | 59.2% | 4.2% | 3.7% | 2.1% |
| No-show rate | 11.4% | 22.3% | 45.7% | 17.7% | 2.9% |
| Financial health of my practice | 6.6% | 25.6% | 43.5% | 14.9% | 9.5% |
| Job satisfaction | 10.5% | 22.5% | 38.7% | 19.4% | 8.9% |
| Types of visits where telehealth works well: | |||||
| Diabetes | 19.8% | 53.2% | 15.1% | 11.9% | 0.0% |
| Anxiety/Depression | 44.7% | 42.1% | 8.6% | 3.3% | 1.3% |
| Other Mental Health | 36.7% | 48.3% | 10.9% | 2.0% | 2.0% |
| Hypertension | 9.6% | 30.2% | 29.4% | 26.5% | 4.4% |
| Coronary Artery Disease | 13.0% | 36.6% | 27.5% | 22.9% | 0.0% |
| Asthma/COPD | 7.3% | 22.6% | 27.0% | 38.7% | 4.4% |
| Medicare Wellness | 33.3% | 30.1% | 11.4% | 19.5% | 5.7% |
| Skin Lesion/Rash | 6.5% | 30.7% | 21.6% | 28.8% | 12.4% |
| Acute Care | 9.6% | 37.0% | 19.9% | 27.4% | 6.2% |
| Hospital/ED follow-up | 5.7% | 35.9% | 21.4% | 20.1% | 5.7% |
| COVID-19 Assessment | 35.2% | 38.6% | 17.2% | 7.6% | 1.4% |
Reported challenges with telehealth visits
Challenges were encountered with telehealth visits among both patients and providers in this study (Table 4). Patients commonly cited difficulty with scheduling follow-up (48.3%) and lack of personal contact (46.0%), with only 12.6% reporting technology problems (software issues, lacking smart phone, tablet, computer, and/or broadband internet access) and 2.3% reporting communication barriers. However, 91.3% of providers reported technology challenges for the patient, and 45.1% reported technology challenges for the provider. Moreover, providers also cited barriers related to lack of reimbursement (34.4%) and lack of implementation support (20.0%).
Table 4.
Rural patient and provider reported challenges with telehealth visits
|
Patients N (%) |
|
| Did not have personal contact with provider | 40 (46.0%) |
| Technology problems or interruptions | 11 (12.6%) |
| Follow-up was difficult to schedule | 42 (48.3%) |
| Communication barrier | 2 (2.3%) |
| Other | 24 (27.6.0%) |
| None reported | 9 (10.3%) |
|
Providers N (%) |
|
| Lack of reimbursement | 67 (34.4%) |
| Licensure | 4 (2.1%) |
| Technology challenges for the patient | 178 (91.3%) |
| Technology challenges for the provider/practice | 88 (45.1%) |
| Low patient engagement | 37 (19.0%) |
| Lack of implementation support | 39 (20.0%) |
| No challenges | 2 (1.0%) |
Percentages do not add to 100% as respondents could choose multiple options
Missed appointments
Overall, 6,604 visits were scheduled at Munson Family Practice from April through September 2020. The majority of clinical visits were scheduled in-person (n = 3,832, 58.0%), while 42.0% (n = 2,772), of visits were scheduled via telehealth. A total of 547 visits were missed over the study period (240 telehealth and 307 in-person). As shown in Fig. 1, the percentage of missed appointments out of all scheduled visits was slightly higher for telehealth visits compared to in-person visits, but the difference was not statistically significant (8.7% vs. 8.0%; p = 0.39). For telehealth visits, the percentage of no-shows generally increased from 3.7% in April to 11.9% in September. The percentage of no-shows for in-person visits also increased slightly across study months, ranging from 6.4% in July to 9.8% in August. Among patients with missed appointments, we did not observe any differences in patient age according to visit type (p = 0.35).
Fig. 1.
Percentage of Missed Appointments Overall and by Month According to Visit Type (Telehealth vs. In-Person)
Discussion
In this study, rural patients had generally favorable perceptions of telehealth, and satisfaction was higher among younger patients. Rural providers overwhelmingly reported that telehealth added value to clinical practice, though less than half of providers felt that telehealth improved efficiency. Difficulties with scheduling follow-up appointments, lack of personal contact and technology challenges were commonly reported barriers to telehealth. We did not observe any differences in the percentage of missed appointments according to visit type (telehealth vs. in-person) in this study. Taken together, our findings suggest that telehealth approaches are acceptable to rural patients and providers but that technology issues and gaps in care coordination need to be addressed to promote sustainability.
Our finding that favorability of telehealth was higher among younger compared to older patients were consistent with results from prior studies conducted both before [22], and during the COVID-19 pandemic [23] and may be attributed in part to lower technology access and lower digital literacy among older adults [24]. While results from a prior study conducted in 2019 demonstrated lower satisfaction with telehealth among those with less educational attainment, [23] in this study of rural patients, perceptions of telehealth during the pandemic did not vary according to educational attainment, insurance status, distance travelled to clinic or according to type of visit. The benefits of telehealth approaches for older adults have been well documented and include increased convenience, care partner engagement, and improved understanding of home environments by clinicians [22]. Therefore, additional resources are needed to support older adults and those with limited access to internet and technology to maintain quality care in telehealth settings and to avoid exacerbating existing health disparities among older and underserved populations [18].
The provision of quality clinical care relies on a trusted exchange of information between the patient and provider, traditionally occurring through face-to-face clinic visits. With the rapid adoption of telehealth approaches in recent years, it is still unclear how virtual approaches impact communication and the overall patient-provider relationship. One study reported that the majority of providers felt that the physician–patient relationship was unimpaired using telehealth approaches implemented during the pandemic [24]. However, another recent study of telehealth during the pandemic, which used semi-structured interviews found that the physicians noted concerns about loss of personal connections with patients, difficulty reading people’s body language over videos and loss of connectiveness though physical touch [25]. Understanding patient perspectives is important to ensure that telehealth approaches are not detrimental to the relationship. In our study, nearly 40% of patients who reported disliking telehealth cited the lack of personal contact with their provider as the main reason. These findings suggest the need for future studies to address issues related to developing and maintaining the important physician–patient relationship in a virtual environment.
Most rural providers in this study believed that telehealth added value to clinical practice by improving the health and safety of patients, timeliness and access to care and patient and family-centered care—important goals for any outpatient clinical practice. These results were in accordance with findings from several recent studies conducted during the pandemic [24–28]. While we did not observe significant differences by provider age, the perception of telehealth’s added value generally decreased with increasing provider age in our study, with highest favorability among providers aged 25–30 years. As such, telehealth implementation efforts, particularly for an aging rural physician workforce,[29] may need to better understand and address age-related differences in telehealth perception. Importantly, telehealth implementation has been linked to less provider time spent in the electronic health records (EHR) outside of normal working hours [26]. Given that provider burnout has been correlated with time spent in the EHR outside of work, [30–32] this finding suggests that telehealth approaches could also help improve physician satisfaction and reduce burnout.
In this study, less than half of rural providers felt that telehealth approaches improved efficiency in clinical practice. These findings are discordant with results from several prior studies [24–27]. For example, the majority of providers in a large health system in central Pennsylvania reported that telehealth improved efficiency and cut down on driving time required to travel to other clinics [25]. Moreover, in an EHR-based study of over 600 providers in New York City, Beiser et al. observed increased efficiency in terms of the number of patients seen after implementation of telehealth [26]. Discrepancies in findings related to perceived efficiency could be due to the high level of technological challenges reported by rural providers in this study [24–27] Moreover, our study evaluated the rapid deployment of telehealth during the COVID-19 pandemic, and 20% of providers cited barriers related the lack of implementation support. These factors could also have contributed to the lower perception of telehealth efficiency observed in this study.
Reducing patient and provider barriers to telehealth will improve the overall quality of care with telehealth visits and promote broader telehealth adoption. Commonly reported barriers to telehealth identified in our study included difficulties with scheduling follow-up appointments, lack of personal contact and technology challenges. Telehealth approaches are highly dependent on broadband or cellular internet access, which is not equitably available [33–35]. For example, nearly 20% of the US population resides in rural communities, where access to academic medical centers, reliable internet and other resources is often limited [36, 37]. Given these challenges in rural settings, additional support may be necessary to limit technology challenges for both rural providers and patients. Interestingly, rural patients and providers reported divergent views of technology-related barriers in this study. Specifically, providers were more likely to report technology challenges for both patients and providers, while patient-reported technology challenges were less common. Additional studies are needed to explore potential underlying reasons for this discrepancy.
Reducing missed healthcare appointments is a key component to increasing efficiency in clinical practice [38]. In a prior qualitative study, providers cited more missed appointments in the virtual compared to in-person setting [22]. Missed healthcare appointments have been shown to be associated with multiple factors, including a lack of urgency to receive care, scheduling policy, fear and anxiety surrounding appointments, language barriers, forgetfulness, transportation-related issues, concern over service cost, weather, insurance coverage, long lead times to appointments, and miscommunication with clinic staff [39–41]. Results from our study suggested that telehealth visits did not significantly impact missed healthcare appointments in rural primary care settings during the pandemic. The lack of difference in missed appointments between telehealth and in-person visits in our study suggested that factors other than transportation-related issues may be more strongly associated with missed appointments in our rural setting. Although, preferences for telehealth may vary by geographic region – those living in metropolitan areas were less likely to miss telemedicine appointments but more likely to miss in-person appointments in a prior study, [13] potentially due to higher preference for accessing healthcare through technology and more robust internet access in urban areas. Future studies are needed to assess missed appointments according to visit type after the pandemic-associated social distancing measures were lifted.
One of the main strengths of this study is the focus on perceptions of rural patients and rural physicians across diverse provider settings, whereas most studies of telehealth during the pandemic have focused on urban regions and/or specific clinical subspecialties. Given that access to care can be particularly challenging in rural areas, rural populations arguably stand to benefit most from telehealth approaches. Thus, our study can provide insight to ensure the sustainability of telehealth approaches in rural regions, even after the pandemic. Additionally, findings from this study can be used to implement tailored telehealth approaches in rural health systems to improve quality of care and access. This study had several limitations, including potential survey response bias, given that only providers delivering telehealth and patients using telehealth were eligible for the study. We also lacked data on the volume of telehealth visits conducted by reason for visit, which could have influenced overall provider perceptions. While the patient survey in this study was based on a similar survey from a prior publication, [21] the questions were not specifically validated. We were unable to determine the response rate for the patient survey due to pandemic-related limitations on tracking, although our sample size was calculated to promote broader representation of the target population. Lastly, generalizability of the results to other rural locations may be limited given that this survey study was conducted through a single rural healthcare system in Northwest Michigan.
Conclusion
An improved understanding of patient and provider perceptions of telehealth is critical to widespread telehealth adoption and improved healthcare access. Findings from this study indicate favorable perceptions of telehealth among rural patients and providers and suggest that telehealth approaches may add value to rural clinical practice. However, technology issues for both patients and providers and gaps in care coordination need to be addressed to promote sustainability of telehealth approaches in rural practice. Given that most prior research evaluating telehealth implementation has been conducted in large urban healthcare settings, findings from this study are important and can be used to tailor telehealth approaches in other under-resourced settings. Further research is needed to more comprehensively characterize the underlying barriers and facilitators for telehealth and promote equitable implementation of telehealth programs in rural settings.
Supplementary Information
Acknowledgements
The authors would like to thank all the Munson Healthcare providers and patients who participated in the research study and Chelsea Szafranski who distributed online surveys.
Abbreviations
- ANOVA
Analysis of Variance
- EHR
Electronic Health Records
- MFPC
Munson Family Practice Center
- MHC
Munson HealthCare
- P
P-value
- SAS
Statistical Analysis Software
- US
United States
- WIFI
Wireless Fidelity
Authors’ contributions
DK, DP, JK, JB, WJ and KH conceptualized the study. DK drafted the manuscript and oversaw the research. DP, WJ, JK developed data collection procedures and interpretation of study findings. KH analyzed and interpreted the data and contributed to manuscript writing. All authors contributed to manuscript writing. All authors read and approved the final manuscript.
Funding
No funding was received for this article.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the Institutional Review Board at Munson Healthcare (REF #1651750–2, 1647744–2, 1645803–2) – consent was waived.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gifford Kathleen, et al. States Focus on Quality and Outcomes Amid Waiver Changes. 2018. [Google Scholar]
- 2.Medicaid and CHIP Payment and Access Commission . “Telehealth in Medicaid” in Report to Congress on Medicaid and CHIP. 2018. [Google Scholar]
- 3.Onyi Lam, Brian Broderick adn Skye Toor. How far Americans live from the closest hospital differs by community type. Pew Research Center; 2018. Cited 2022 Apr 25. Available from: https://www.pewresearch.org/fact-tank/2018/12/12/how-far-americans-live-from-the-closest-hospital-differs-by-community-type/.
- 4.Chen YY, Guan BS, Li ZK, Li XY. Effect of telehealth intervention on breast cancer patients’ quality of life and psychological outcomes: a meta-analysis. J Telemed Telecare. 2018;24(3):157–167. doi: 10.1177/1357633X16686777. [DOI] [PubMed] [Google Scholar]
- 5.Dario AB, Moreti Cabral A, Almeida L, Ferreira ML, Refshauge K, Simic M, et al. Effectiveness of telehealth-based interventions in the management of non-specific low back pain: a systematic review with meta-analysis. Spine J. 2017;17(9):1342–1351. doi: 10.1016/j.spinee.2017.04.008. [DOI] [PubMed] [Google Scholar]
- 6.Marx W, Kelly JT, Crichton M, Craven D, Collins J, Mackay H, et al. Is telehealth effective in managing malnutrition in community-dwelling older adults? A systematic review and meta-analysis. Maturitas. 2018;111:31–46. doi: 10.1016/j.maturitas.2018.02.012. [DOI] [PubMed] [Google Scholar]
- 7.Rush KL, Hatt L, Janke R, Burton L, Ferrier M, Tetrault M. The efficacy of telehealth delivered educational approaches for patients with chronic diseases: a systematic review. Patient Educ Couns. 2018;101(8):1310–1321. doi: 10.1016/j.pec.2018.02.006. [DOI] [PubMed] [Google Scholar]
- 8.Shigekawa E, Fix M, Corbett G, Roby DH, Coffman J. The current state of telehealth evidence: a rapid review. Health Aff (Millwood) 2018;37(12):1975–1982. doi: 10.1377/hlthaff.2018.05132. [DOI] [PubMed] [Google Scholar]
- 9.Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open. 2017;7(8):e016242. doi: 10.1136/bmjopen-2017-016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.American Medical Association. Digital Health Study . Physicians’ motivations and requirements for adopting digital clinical tools. 2020. [Google Scholar]
- 11.Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573–576. doi: 10.1370/afm.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rutledge CM, Kott K, Schweickert PA, Poston R, Fowler C, Haney TS. Telehealth and eHealth in nurse practitioner training: current perspectives. Adv Med Educ Pract. 2017;8:399–409. doi: 10.2147/AMEP.S116071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adepoju OE, Chae M, Liaw W, Angelocci T, Millard P, Matuk-Villazon O. Transition to telemedicine and its impact on missed appointments in community-based clinics. Ann Med. 2022;54(1):98–107. doi: 10.1080/07853890.2021.2019826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lin CCC, Dievler A, Robbins C, Sripipatana A, Quinn M, Nair S. Telehealth in health centers: key adoption factors, barriers and opportunities. Health Aff Proj Hope. 2018;37(12):1967–1974. doi: 10.1377/hlthaff.2018.05125. [DOI] [PubMed] [Google Scholar]
- 15.Tuckson RV, Edmunds M, Hodgkins ML. Telehealth. N Engl J Med. 2017;377(16):1585–1592. doi: 10.1056/NEJMsr1503323. [DOI] [PubMed] [Google Scholar]
- 16.Terry DL, Buntoro SP. Perceived usefulness of telehealth among rural medical providers: barriers to use and associations with provider confidence. J Technol Behav Sci. 2021;6(4):567–571. doi: 10.1007/s41347-021-00215-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wosik J, Fudim M, Cameron B, Gellad ZF, Cho A, Phinney D, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020;27(6):957–962. doi: 10.1093/jamia/ocaa067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hirko KA, Kerver JM, Ford S, Szafranski C, Beckett J, Kitchen C, et al. Telehealth in response to the COVID-19 pandemic: Implications for rural health disparities. J Am Med Inform Assoc. 2020;27(11):1816–1818. doi: 10.1093/jamia/ocaa156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shachar C, Engel J, Elwyn G. Implications for telehealth in a postpandemic future: regulatory and privacy issues. JAMA. 2020;323(23):2375–2376. doi: 10.1001/jama.2020.7943. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Medicare and Medicaid Services . Medicare telemedicine health care provider fact sheet. 2020. [Google Scholar]
- 21.Welch BM, Harvey J, O’Connell NS, McElligott JT. Patient preferences for direct-to-consumer telemedicine services: a nationwide survey. BMC Health Serv Res. 2017;17(1):784. doi: 10.1186/s12913-017-2744-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ladin K, Porteny T, Perugini JM, Gonzales KM, Aufort KE, Levine SK, et al. Perceptions of telehealth vs in-person visits among older adults with advanced kidney disease, care partners, and clinicians. JAMA Netw Open. 2021;4(12):e2137193. doi: 10.1001/jamanetworkopen.2021.37193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fischer SH, Ray KN, Mehrotra A, Bloom EL, Uscher-Pines L. Prevalence and characteristics of telehealth utilization in the United States. JAMA Netw Open. 2020;3(10):e2022302. doi: 10.1001/jamanetworkopen.2020.22302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gordon NP, Crouch E. Digital Information technology use and patient preferences for internet-based health education modalities: cross-sectional survey study of middle-aged and older adults with chronic health conditions. JMIR Aging. 2019;2(1):e12243. doi: 10.2196/12243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saiyed S, Nguyen A, Singh R. Physician perspective and key satisfaction indicators with rapid telehealth adoption during the Coronavirus Disease 2019 pandemic. Telemed E-Health. 2021;27(11):1225–1234. doi: 10.1089/tmj.2020.0492. [DOI] [PubMed] [Google Scholar]
- 26.Beiser M, Lu V, Paul S, Ni J, Nazar N, Epstein E, et al. Electronic health record usage patterns: assessing telemedicine’s impact on the provider experience during the COVID-19 pandemic. Telemed J E-Health Off J Am Telemed Assoc. 2021;27(8):934–938. doi: 10.1089/tmj.2020.0490. [DOI] [PubMed] [Google Scholar]
- 27.Gentry MT, Puspitasari AJ, McKean AJ, Williams MD, Breitinger S, Geske JR, et al. Clinician satisfaction with rapid adoption and implementation of telehealth services during the COVID-19 pandemic. Telemed J E-Health Off J Am Telemed Assoc. 2021;27(12):1385–1392. doi: 10.1089/tmj.2020.0575. [DOI] [PubMed] [Google Scholar]
- 28.Donnelly C, Ashcroft R, Bobbette N, Mills C, Mofina A, Tran T, et al. Interprofessional primary care during COVID-19: a survey of the provider perspective. BMC Fam Pract. 2021;22(1):31. doi: 10.1186/s12875-020-01366-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Skinner L, Staiger DO, Auerbach DI, Buerhaus PI. Implications of an aging rural physician workforce. N Engl J Med. 2019;381(4):299–301. doi: 10.1056/NEJMp1900808. [DOI] [PubMed] [Google Scholar]
- 30.Anderson J, Leubner J, Brown SR. EHR overtime: an analysis of time spent after hours by family physicians. Fam Med. 2020;52(2):135–137. doi: 10.22454/FamMed.2020.942762. [DOI] [PubMed] [Google Scholar]
- 31.Saag HS, Shah K, Jones SA, Testa PA, Horwitz LI. Pajama time: working after work in the electronic health record. J Gen Intern Med. 2019;34(9):1695–1696. doi: 10.1007/s11606-019-05055-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sinsky CA, Rule A, Cohen G, Arndt BG, Shanafelt TD, Sharp CD, et al. Metrics for assessing physician activity using electronic health record log data. J Am Med Inform Assoc. 2020;27(4):639–643. doi: 10.1093/jamia/ocz223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Douthit N, Kiv S, Dwolatzky T, Biswas S. Exposing some important barriers to health care access in the rural USA. Public Health. 2015;129(6):611–620. doi: 10.1016/j.puhe.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 34.Greenberg-Worisek AJ, Kurani S, Finney Rutten LJ, Blake KD, Moser RP, Hesse BW. Tracking healthy people 2020 internet, broadband, and mobile device access goals: an update using data from the health information national trends survey. J Med Internet Res. 2019;21(6):e13300. doi: 10.2196/13300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Krakow M, Hesse BW, Oh A, Patel V, Vanderpool RC, Jacobsen PB. Addressing rural geographic disparities through health it: initial findings from the health information national trends survey. Med Care. 2019;57 Suppl 6 Suppl 2:S127–32. doi: 10.1097/MLR.0000000000001028. [DOI] [PubMed] [Google Scholar]
- 36.Charlton M, Schlichting J, Chioreso C, Ward M, Vikas P. Challenges of rural cancer care in the United States. Oncol Williston Park N. 2015;29(9):633–640. [PubMed] [Google Scholar]
- 37.Blake KD, Moss JL, Gaysynsky A, Srinivasan S, Croyle RT. Making the case for investment in rural cancer control: an analysis of rural cancer incidence, mortality, and funding trends. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol. 2017;26(7):992–997. doi: 10.1158/1055-9965.EPI-17-0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liaw WR, Jetty A, Coffman M, Petterson S, Moore MA, Sridhar G, et al. Disconnected: a survey of users and nonusers of telehealth and their use of primary care. J Am Med Inform Assoc JAMIA. 2019;26(5):420–428. doi: 10.1093/jamia/ocy182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Marbouh D, Khaleel I, Al Shanqiti K, Al Tamimi M, Simsekler MCE, Ellahham S, et al. Evaluating the impact of patient no-shows on service quality. Risk Manag Healthc Policy. 2020;13:509–517. doi: 10.2147/RMHP.S232114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tsai WC, Lee WC, Chiang SC, Chen YC, Chen TJ. Factors of missed appointments at an academic medical center in Taiwan. J Chin Med Assoc JCMA. 2019;82(5):436–442. doi: 10.1097/JCMA.0000000000000068. [DOI] [PubMed] [Google Scholar]
- 41.Kaplan-Lewis E, Percac-Lima S. No-show to primary care appointments: why patients do not come. J Prim Care Community Health. 2013;4(4):251–255. doi: 10.1177/2150131913498513. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.