Abstract
Objective
To provide insights into the nature, risk factors, impact and existing measures for reporting and preventing violence in the healthcare system. The under-reporting of violence against healthcare workers (HCWs) globally highlights the need for increased public awareness and education.
Methods
The Violence Study of Healthcare Workers and Systems study used a survey questionnaire created using Research Electronic Data Capture (REDCap) forms and distributed from 6 June to 9 August 2022. Logistic regression analysis evaluated violence predictors, including gender, age, years of experience, institution type, respondent profession and night shift frequency. A χ2 test was performed to determine the association between gender and different violence forms.
Results
A total of 5405 responses from 79 countries were analysed. India, the USA and Venezuela were the top three contributors. Female respondents comprised 53%. The majority (45%) fell within the 26–35 age group. Medical students (21%), consultants (20%), residents/fellows (15%) and nurses (10%) constituted highest responders. Nearly 55% HCWs reported firsthand violence experience, and 16% reported violence against their colleagues. Perpetrators were identified as patients or family members in over 50% of cases, while supervisor-incited violence accounted for 16%. Around 80% stated that violence incidence either remained constant or increased during the COVID-19 pandemic. Among HCWs who experienced violence, 55% felt less motivated or more dissatisfied with their jobs afterward, and 25% expressed willingness to quit. Univariate analysis revealed that HCWs aged 26–65 years, nurses, physicians, ancillary staff, those working in public settings, with >1 year of experience, and frequent night shift workers were at significantly higher risk of experiencing violence. These results remained significant in multivariate analysis, except for the 55–65 age group, which lost statistical significance.
Conclusion
This global cross-sectional study highlights that a majority of HCWs have experienced violence, and the incidence either increased or remained the same during the COVID-19 pandemic. This has resulted in decreased job satisfaction.
Keywords: public health, health education and promotion, cross-sectional survey, community-based survey, prevention strategies
WHAT IS ALREADY KNOWN ON THIS TOPIC
Violence against healthcare workers (HCWs) has been reported across the globe, and its frequency has increased over the years.
Existing knowledge underscores the under-reporting of violence against HCWs.
WHAT THIS STUDY ADDS
The Violence Study of Healthcare Workers and Systems (ViSHWaS) study confirms the global prevalence of violence against HCWs and offers significant contributions to understanding its nature, risk factors and consequences on both HCWs and the healthcare system.
Violence has substantial impact on the morale of HCWs. Those who experience violence are more prone to feel demotivated in their work or contemplate leaving their jobs.
The study highlights a concerning trend during the COVID-19 pandemic, with the majority of HCWs perceiving that violence rates either increased or remained constant compared with the prepandemic period.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
The study highlights the need for comprehensive strategies to address workplace violence’s impact on HCWs and emphasises the urgency of implementing preventive measures and public awareness to address violence against HCWs.
Understanding the risk factors and impact of violence can inform policy decisions and guide the development of interventions to ensure a safer working environment for HCWs.
Introduction
Violence against healthcare workers (HCWs) is an unfortunate reality in medical practices across the globe. The WHO reports that up to 38% of HCWs face scenarios of brutality at least once during their career and 16 times more than in other professional fields.1 2 According to a 2016 Centers for Disease Control and Prevention (CDC) report, 70% of workers in the private industry who experienced workplace violence (WPV) belonged to the healthcare and/or social assistance industry.3 The WHO defines WPV as ‘incidents where staff is abused, threatened or assaulted in the circumstances related to their work, including commuting to and from work, involving an explicit or implicit challenge to their safety, well-being or health.”4 WPV has four categories, with type II (pertaining to the involvement of patients or their family members in attacks against HCWs) being the most common.5–7 Various reports suggest that WPV incidence has escalated in recent years and throughout the COVID-19 pandemic.8–11
WPV includes verbal abuse, psychological harm, physical or sexual assault, racial harassment and cyber persecution. The 2016 Occupational Safety and Health Administration (OSHA) guidelines identify WPV risk factors within healthcare facilities—patients with a history of psychiatric illnesses, violence or substance abuse; understaffed emergency departments; lengthy patient waiting periods and restricted access within healthcare facilities.12–14 Reports from India identified additional risk factors, including misrepresentation of HCWs by the media, poor healthcare quality, low health literacy rate, poor communication and lack of faith in the judicial process.15 Different countries might have various risk factors, but the repercussions of WPV among HCWs are the same.
A violent episode can have a severe impact on HCWs, including extensive injuries, death, psychological distress, burnout, higher rate of medical errors, poorer patient outcomes and increased attrition.16 17 Researchers have yet to identify the underlying mechanisms and factors for WPV, which could guide an appropriate approach to mitigate the risk of violence against HCWs.
Our study intends to address the global prevalence of violence in the healthcare system, the characteristics of violence, its predisposing risk factors, its aftermath and the probable mitigation strategies to prevent them.
Methodology
Study design and timeline
It is a cross-sectional, observational, survey-based study. The survey was created using REDCap forms and conducted for 8 weeks—from 6 June 2022 to 9 August 2022. Using in-person, instant messaging, e-mail and video conference exchanges, a core team ranging across the medical hierarchy and encompassing doctors, nurses, emergency medical technicians (EMTs) and medical students was convened. The ViSHWaS study used the core competencies in human subject research expertise, team building and data storage, cleaning and interpretation that were already present within the Global Remote Research Scholar Program and expanded on it.18 19
Patient and public involvement
Public (respondents) were not involved in the design, or conduct, or reporting or dissemination plans of our research.
Survey dissemination strategy
To seek maximum responses from as many countries as possible, a ‘hub and spoke model’ of team building was adopted.20 The senior investigator had prior experience in conducting global survey-based studies.21–24 The hub of this survey was the core team. which consisted of 11 members from five countries. This team interacted via a dedicated ViSHWaS Research WhatsApp group and weekly video conferencing. Each team member sent the survey to their networks using in-person messaging tools such as direct, WhatsApp messages and e-mails. The core team recruited the country leads or representatives who would serve as the spokes of the ‘hub and spoke’ model.20 Detailed dissemination strategies and guiding principles have been submitted elsewhere.25 Each leader was responsible for disseminating the survey in their networks. This was to ensure the responses from the lived experiences of HCWs across various nationalities, ethnicities, races and genders besides the hierarchical sets and subsets of the healthcare workforce.
A digital survey banner was designed for promotional messaging. Thereafter, a wider audience was reached by encouraging global healthcare community engagement using Twitter Spaces, LinkedIn Posts and YouTube videos.18 19 This helped spread the survey to countries that did not have direct representation via the country leads.
Sample size
Out of a total of >50 million medical doctors, nurses and allied HCWs worldwide, if 10 million are accessible and assuming that 50% would have faced violence at their workplace. Using the formula below (results from Calculater.net, open-source calculator), with a 95% CI, 1.4% margin of error and a design effect of three (medical doctors, nurses and allied HCWs), the sample size would be 4898. So, we targeted 5000 unique responses. We used the convenience sampling method.
Formula: sample size N=(DEFF*Np(1 p)/ ((d2/Z2 1-α/2*(N-1) +p*(1 p)). Here, (N) is the target population size, (p) is the hypothesised per cent frequency of outcome factor in the population, (d) is the confidence limits as per cent out of 100, and DEFF is the design effect.
Regression analysis
All statistical analyses were performed using STATA statistical software (V.17.0SE, StataCorp, College Station, Texas 77 845). A logistic regression model was developed to evaluate the various predictors of violence against HCWs. In the a-priori hypothesis, gender (male, female or others) and institution type (government or non-government) were considered the primary predictors. We hypothesised that the female gender and the government institution type be independent predictors of the higher odds of violence against the HCWs. Considering clinical reasoning and directed acyclic graphs, additional predetermined variables, such as age, years of experience and profession, might confound the association between the hypothesised independent predictors and the outcome being studied and were recognised. Univariate analyses were performed to study the effect of primary (independent) and secondary predictors on the odds of HCW violence.
Simultaneously, multivariate-adjusted models were developed to control for the confounding variables. As HCWs’ age and years of experience were found to be strongly correlated, they introduced collinearity to the models. This led us to drop the years of experience from the adjusted regression models. Finally, we performed a χ2 test to assess the associations between HCWs’ gender and four different violence subtypes experienced by the ViSHWaS survey respondents. Statistical significance was defined by a two-tailed p<0.05.
Preprint and conference presentations
Various subsets of the manuscript have been submitted and accepted as abstracts for presentation at various conferences, including the Society of Critical Care Medicine annual meeting (SCCM 2023) in San Francisco, USA, in January 2023 (also received media coverage); The third Abu Dhabi Integrated Mental Health Conference in Abu Dhabi, UAE, in January 2023; The American Thoracic Society International conference in Washington, DC in May 2023.25–27 An initial version of the manuscript abstract has been submitted and published on the Lancet SSRN preprint platform.28
Results
Survey response representation
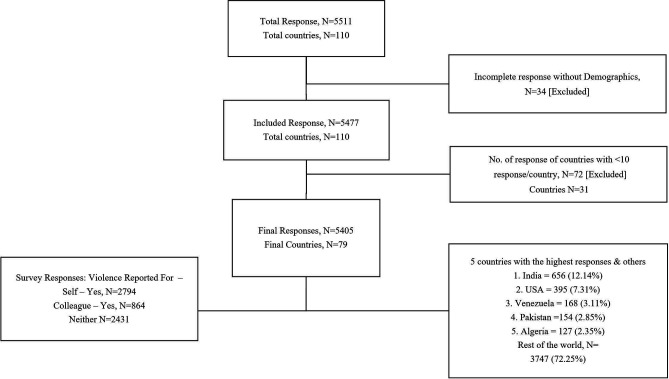
A total of 5511 healthcare professionals responded to the survey from over 110 countries over an 8-week period. From the total, 34 responses were excluded due to unavailable demographic data and/or lack of response to questions regarding experiencing violence and its characteristics. From the remaining 5477 responses, countries with less than 10 responses per country were excluded, thus excluding a total of 72 responses from 31 countries. The final analysis was conducted on 5405 responses from 79 countries (figure 1, online supplemental appendix B–Figure 1 and table 1). Among the top five countries with the maximum responses, India had the highest number (12.1%), followed by the USA (7.3%), Venezuela (3.1%), Pakistan (2.8%) and Algeria (2.3%). The remaining 3747 (69.3%) responses came from the remaining 74 countries (2.9% country name response unavailable) (figure 1, online supplemental appendix B–figure 2 and table 2)
Figure 1.
Flow diagram of total survey responses and total number of countries.
Table 1.
Demographic characteristics of survey respondents
| N | Percentage | ||
| Gender | Male | 2427 | 44.9 |
| Female | 2868 | 53.1 | |
| Transgender | 7 | 0.13 | |
| Gender variant/non-confirming | 15 | 0.28 | |
| Other/prefer not to disclose | 39 | 0.72 | |
| Skipped | 49 | 1 | |
| Age (years) | 18–25 | 1645 | 30.4 |
| 26–35 | 2440 | 45.2 | |
| 36–45 | 810 | 15 | |
| 46–55 | 288 | 5.3 | |
| 56–65 | 144 | 2.7 | |
| 65+ | 27 | 0.50 | |
| Skipped | 51 | 1 | |
| Race | US-White Caucasian | 232 | 4.29 |
| US- African American | 45 | 0.83 | |
| US-Asian American | 68 | 1.26 | |
| US-American Indian or Alaska Native | 33 | 0.61 | |
| US-Native Hawaiian/Other Pacific Islander | 5 | 0.09 | |
| White-Caucasian | 266 | 4.92 | |
| Black - African | 945 | 17.48 | |
| South Asian | 1336 | 24.72 | |
| West Asian | 632 | 11.69 | |
| Hispanic/Latino | 1009 | 18.67 | |
| East Asian | 139 | 2.57 | |
| Southeast Asian | 222 | 4.11 | |
| Central Asian | 28 | 0.52 | |
| Mixed Race | 236 | 4.37 | |
| Other | 146 | 2.7 | |
| Skipped | 63 | 1.17 | |
| Institution location | USA | 395 | 7.31 |
| Outside USA | 4936 | 91.32 | |
| Skipped | 74 | 1.37 | |
| Type of institution | Government academic | 2186 | 40.14 |
| Government non-academic | 513 | 9.49 | |
| Private academic | 828 | 15.32 | |
| Private non-academic | 459 | 8.49 | |
| Community hospital | 895 | 16.56 | |
| Military hospital | 145 | 2.68 | |
| Mission/non-profit hospital | 90 | 1.67 | |
| Other | 141 | 2.61 | |
| Skipped | 148 | 2.74 | |
| Years of experience | <1 | 622 | 11.51 |
| 1–2 | 978 | 18.09 | |
| 2–5 | 1773 | 32.8 | |
| 6–10 | 984 | 18.21 | |
| 11–20 | 608 | 11.25 | |
| 21–30 | 245 | 4.53 | |
| <30 | 126 | 2.33 | |
| Skipped | 69 | 1.28 | |
| Work position | Administration | 229 | 4.24 |
| Nurse practitioner (ARNP) | 107 | 1.98 | |
| Attending physician | 1098 | 20.31 | |
| Auxiliary/support staff | 108 | 2 | |
| Dentist/dental surgeon | 210 | 3.89 | |
| EMT | 56 | 1.04 | |
| Fellow in training | 307 | 5.68 | |
| Medical student | 1141 | 21.11 | |
| Occupational therapist | 36 | 0.67 | |
| Pharmacist (PharmD) | 117 | 2.16 | |
| Physical therapist | 71 | 1.31 | |
| Physician assistant (PA) | 133 | 2.46 | |
| Registered nurse (RN) | 426 | 7.88 | |
| Researcher | 109 | 2.02 | |
| Resident/junior resident in training | 811 | 15 | |
| Respiratory therapist | 36 | 0.67 | |
| Other | 360 | 6.66 | |
| Skipped | 50 | 0.93 |
Table 2.
Violence characteristics of survey respondents
| Violence of any form at workplace | Count (N=5405) | Percentage |
| Total yes response—self+colleague (N=5405) | 3838 | 71 |
| Yes response—self (N=5405) | 2974 | 55 |
| Yes response—colleague (N=2431) | 864 | 16 |
| No response—self+colleague (N=5405) | 1567 | 29 |
| Form of violence | Count (N=3838) | Percentage |
| Verbal violence | 2751 | 72 |
| Emotional violence | 1591 | 41 |
| Physical violence | 1157 | 30 |
| Cultural violence | 735 | 19 |
| Sexual violence | 315 | 8 |
| Online/virtual/cyber harassment | 263 | 7 |
| Other | 47 | 1 |
| Type of aggressor | Count (N=3838) | Percentage |
| More than one type of aggressor | 711 | 19 |
| Colleague | 341 | 9 |
| Patient | 453 | 12 |
| Patient and relative and/or caregiver | 594 | 15 |
| Patient and relative and/or caregiver | 1108 | 29 |
| Supervisor | 610 | 16 |
| Skipped | 21 | 1 |
| Frequency of violence during COVID-19 pandemic | Count (N=3838) | Percentage |
| Increased | 1404 | 37 |
| About the same | 1657 | 43 |
| Decreased | 747 | 19 |
| Number of violent episodes in past 1 year |
Survey respondent—
self (N=2974) |
Survey respondent—
colleague (N=864) |
| Every day | 53 (2%) | 10 (1%) |
| About once a week | 269 (9%) | 91 (11%) |
| A few times a week | 184 (6%) | 46 (5%) |
| Once or twice a month | 746 (25%) | 217 (25%) |
| Once or twice a quarter | 655 (22%) | 491 (57%) |
| Once or twice a year | 1048 (35%) | 0 (0%) |
bmjgh-2023-013101supp002.pdf (1.9MB, pdf)
Demographic characteristics
The respondents primarily consisted of a young adult population (18–35 years of age) (N=4085, 75%),62% (N=3373) of the respondents had work experience of 5 years or less, and a greater number of women (N=2868, 53.1%) responded to the questionnaire than men (table 1)
South Asians represented 24.7% of the respondents, followed by Hispanics/Latinos (18.7%) and Native Africans (17.5%). Almost 50% of respondents worked in government institutions (40.4% in academic, 9.5% in non-academic). In comparison, around 24% worked in private institutions (15.3% in academic, 8.5% in non-academic) and the rest belonged to community, military and mission hospitals. The HCWs across various hierarchies, ranging from medical students (21.1%) to attending physicians (20.3%) and residents (15%), responded to the survey (table 1)
Violence characteristics
A total of 2974 survey respondents (55.2%) recollected experiencing violence first-hand, while 2431 (45%) reported not experiencing violence themselves at their workplace; out of these, 864 (16%) reported violence faced by their colleague(s), that is, colleague respondents. A total of 1567 (29%) responded that neither they nor their colleagues faced any violence. From this population, 13 respondents, who did not answer this critical question, were considered as ‘no’ for both self and colleague. They were included in the subset of 1567 HCWs who had responded that neither they nor their colleagues had faced violence. Thus, we recorded 3838 (71%) ‘yes’ and 1567 (29%) ‘no’ out of a total of 5405 responses (figure 1, table 2).
When comparing the form of violence faced by those who responded ‘yes’ for either self or colleague, a similar pattern was observed between the two groups: a majority reported verbal violence as the most common form of violence (40% of 5405 for self and 10.9% of 5405 for a colleague), followed by emotional violence (23.5% for self and 5.94% for a colleague) and physical violence (15.6% for self and 5.8% for a colleague). Online/cyber harassment was also reported by some of the respondents (3.6% for self and 1.2% for colleagues) (table 2, online supplemental appendix B–figure 3).
Of the 3838 reported a history of violence (either self or colleague), 56.1% described the patient itself or a patient accompaniment (relative or family member) as the most common type of aggressor, whereas 15.9% reported experiencing violence from their supervisors, and 8.9% by their colleagues. Another 18.5% reported more than one type of aggressor (table 2). Around 49% of respondents had reported the violent episode(s) to the hospital administration or the police (online supplemental appendix B–table 3).
Frequency of violence
Sizeable differences in the frequency of violence were observed when self-respondents were compared with those reporting against their colleagues. Total of 2974 HCWs reporting violence against themselves, 35.2% described facing violence once or two times a year. However, none of the 864 HCWs who had witnessed violence against their colleagues reported this frequency of violent incidents. Meanwhile, 56.8% of these 864 HCWs reported a higher frequency of violence, that is, once or two times a quarter, compared with 22% (NTotal=2974) of self-respondents facing violence during the same interval; nevertheless, 25% of both groups reported facing harassment every month, whereas 2% of self-respondents and 1% of colleague-respondents were victims of daily abuse and violence (table 2).
Out of 3838 respondents, 36.6% reported an increase in the frequency of violence during the COVID-19 pandemic. While 43.2% felt that the frequency of violence had remained unchanged, nearly 19.5% of respondents considered the violence frequency to drop during the COVID-19 pandemic (table 2).
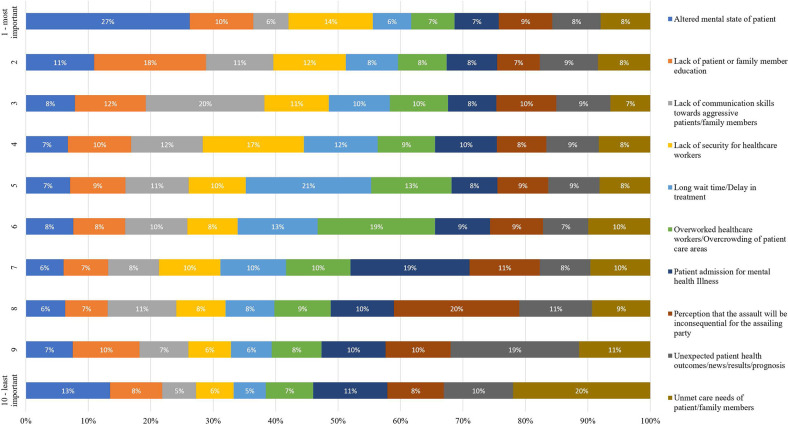
Cause of violence
Survey respondents were asked to rank the 10 listed probable causes of violence based on their perceived importance. The patient’s altered mental status was discerned as the most important cause by 27%, followed by a scarcity of security for HCWs (13.8%) and a paucity of patient or family member education (10.4%). Conversely, 20.4% considered the patient’s or family member’s unmet care needs the least probable cause. Contrary to the 27% selecting altered mental status as the most critical factor, 12.5% described altered sensorium of the patient as the least essential cause, followed by 11.1% of respondents who held patients admitted with mental illness as the least responsible. A detailed graph of the ten ranking questions is listed in figure 2.
Figure 2.
Probable cause of violence as per survey responses—self and colleague.
Violence outcomes and reporting
Of the 5405 survey participants, 51.7% of respondents validated the availability of violence reporting procedures at their institutions. Around 44% of the respondents were aware of the OSHA standards/guidelines. Over 75.3% of survey respondents reported not receiving adequate training to manage a potentially violent event (online supplemental appendix B–table 3).
Most HCWs felt more worried and less prepared to encounter a potentially violent situation. Nearly 62% of the respondents expressed being moderately (Likert scale 3) to very strongly worried (Likert scale 5) about facing a potentially violent situation. On the other hand, more than 75% of respondents felt unprepared at all (Likert scale 1) to moderately prepared (Likert scale 3) to handle a violent situation (online supplemental appendix B–figure 4).
Of the 3838 respondents who reported that either they themselves or their colleague(s) had faced violence, 55.1% reported feeling less motivated or more dissatisfied with their job as an aftermath of violence. Around 16.6% of these reported being willing to quit either their current department or their workplace, and 4.6% to leave the profession. Contrastingly, almost 17.5% of people expressed no change in their attitude towards work, while 5.3% felt more motivated to work than before (online supplemental appendix B–figure 5, online supplemental appendix B–table 3).
Analysis of possible predictors of violence
Univariate analysis
The univariate analysis revealed that female gender was not associated with increased odds of facing violence compared with men (OR=1.04; 95% CI 0.93 to 1.16, p=0.46). HCWs in government sectors had higher odds of experiencing violence compared with non-government private sector employees (OR=1.41; 95% CI 1.25 to 1.60, p<0.001). Nurses (OR=2.40; 95% CI 1.83 to 3.14, p<0.001), physicians (OR=2.23; 95% CI 1.77 to 2.81, p<0.001) and other HCWs (eg, emergency medical transport, pharmacists, physical therapist, researchers, etc) (OR=1.73; 95% CI 1.36 to 2.22, p<0.001 had significantly higher odds of facing violence, while medical students had significantly lower odds (OR=0.65; 95% CI 0.51 to 0.84, p<0.001).
HCWs aged 26–35 years (OR=2.56; 95% CI 2.25 to 2.91, p<0.001), 36–45 years (OR=2.68; 95% CI 2.26 to 3.19, p<0.001), 46–55 years (OR=2.83; 95% CI 2.18 to 3.67, p<0.001) and 55–65 years old (OR=1.83; 95% CI 1.30 to 2.58, p<0.001), all exhibited significantly increased odds of facing violence, except for those aged 65 and above (OR=1.67; 95% CI=0.78 to 3.58, p=0.19). HCWs with 1–2 years of experience had increased odds of facing violence (OR=1.56; 95% CI=1.27 to 1.92, p<0.001), and this trend continued to escalate with 2–5 years (OR=2.27; 95% CI 1.88 to 2.73, p<0.001), 6–10 years (OR=2.85; 95% CI 2.32 to 3.51, p<0.001), 11–20 years (OR=2.91; 95% CI 2.31 to 3.67, p<0.001), 20–30 years (OR=2.59; 95% CI 1.91 to 3.51, p<0.001) and more than 30 years (OR=2.02; 95% CI 1.37 to 2.97, p<0.001). Additionally, a higher frequency of night shifts correlated with higher odds of violence (OR=2.37; 95% CI 2.09 to 2.68, p<0.001) (table 3).
Table 3.
Univariate and multivariate logistic regression models for the association of socio-demographic variables and self-experienced violence
| Variable | Univariate | Multivariate | ||||||||
| OR | Standard error | 95% CI for B | P value | OR | Standard error | 95% CI for B | P value | |||
| LL | UL | LL | UL | |||||||
| Gender* | ||||||||||
| Female | 1.041 | 0.057 | 0.934 | 1.161 | 0.461 | 1.099 | 0.066 | 0.977 | 1.237 | 0.114 |
| Work setting† | ||||||||||
| Public setting | 1.410 | 0.089 | 1.245 | 1.597 | <0.001 | 1.427 | 0.096 | 1.250 | 1.629 | <0.001 |
| Other | 0.882 | 0.157 | 0.621 | 1.252 | 0.483 | 0.897 | 0.170 | 0.617 | 1.303 | 0.569 |
| Profession‡ | ||||||||||
| Medical student | 0.653 | 0.082 | 0.510 | 0.836 | 0.001 | 0.776 | 0.107 | 0.591 | 1.020 | 0.069 |
| Nurse | 2.398 | 0.330 | 1.831 | 3.141 | <0.001 | 1.946 | 0.284 | 1.461 | 2.592 | <0.001 |
| Physician | 2.227 | 0.263 | 1.766 | 2.807 | <0.001 | 1.702 | 0.213 | 1.332 | 2.176 | <0.001 |
| Other HCW | 1.732 | 0.219 | 1.351 | 2.220 | <0.001 | 1.577 | 0.210 | 1.214 | 2.049 | 0.001 |
| Age§ | ||||||||||
| 26–35 | 2.558 | 0.168 | 2.250 | 2.909 | <0.001 | 1.757 | 0.135 | 1.510 | 2.044 | <0.001 |
| 36–45 | 2.683 | 0.238 | 2.255 | 3.193 | <0.001 | 1.783 | 0.182 | 1.459 | 2.179 | <0.001 |
| 46–55 | 2.829 | 0.377 | 2.179 | 3.672 | <0.001 | 1.981 | 0.288 | 1.489 | 2.636 | <0.001 |
| 56–65 | 1.833 | 0.320 | 1.302 | 2.582 | 0.001 | 1.256 | 0.234 | 0.871 | 1.810 | 0.221 |
| 65+ | 1.671 | 0.649 | 0.780 | 3.577 | 0.187 | 1.377 | 0.564 | 0.616 | 3.077 | 0.435 |
| Years of experience¶ | ||||||||||
| 1–2 | 1.560 | 0.163 | 1.270 | 1.915 | <0.001 | – | – | – | – | – |
| 2–5 | 2.266 | 0.217 | 1.878 | 2.734 | <0.001 | – | – | – | – | – |
| 6–10 | 2.854 | 0.302 | 2.319 | 3.514 | <0.001 | – | – | – | – | – |
| 11–20 | 2.908 | 0.343 | 2.306 | 3.667 | <0.001 | – | – | – | – | – |
| 21–30 | 2.591 | 0.401 | 1.912 | 3.510 | <0.001 | – | – | – | – | – |
| >30 | 2.021 | 0.398 | 1.373 | 2.974 | <0.001 | – | – | – | – | – |
| Night shift** | ||||||||||
| 1–2 | 2.367 | 0.150 | 2.090 | 2.680 | <0.001 | 1.955 | 0.133 | 1.710 | 2.235 | <0.001 |
Values are significant at 0.05.
*Reference female category is ‘male’.
†Reference work setting category is ‘private’.
‡Reference profession category is ‘administrative or researcher’.
§Reference age category is ‘18–25’.
¶Reference years of experience category is ‘<1’.
**Reference frequency of night shifts category is ‘low’.
LL, lower limit; UL, upper limit.
Adjusted logistic regression models using gender and work setting as independent predictors for experiencing violence
Based on our a-priori hypothesis, multivariate regression models were developed, taking female gender and government institution type as the independent predictor variables. They were controlled for the same confounding variables, including age, work experience, profession and frequency of night shifts (table 3). Age and years of experience were found to be strongly correlated and, thus, introducing collinearity to the models, so it was decided to drop years of experience during the model-building process. The first regression analysis examined the relationship between gender and violence risk, revealing that being woman (OR=1.10; 95% CI 0.98 to 1.24, p=0.114) was not significantly associated with increased odds of violence. However, working in government institutions (OR=1.43; 95% CI 1.25 to 1.63, p<0.001) was significantly associated with an increase in the odds of experiencing violence.
Furthermore, being a nurse (OR=1.95; 95% CI 1.46 to 2.59, p<0.001), physician (OR=1.70; 95% CI 1.33 to 2.18, p<0.001) or other HCWs (OR=1.58; 95% CI 1.21 to 2.05, p<0.001) was significantly associated with higher odds of violence when controlled for other variables. Regarding age, individuals aged 26–35 years (OR=1.76; 95% CI 1.51 to 2.04, p<0.001), 36–45 years (OR=1.78; 95% CI 1.46 to 2.18, p<0.001) and 45–55 years (OR=1.98; 95% CI 1.49 to 2.64, p<0.001) had increased odds of violence. However, age groups 55–65 years (OR=1.26; 95% CI 0.87 to 1.81, p=0.221) and 65+ years (OR=1.38; 95% CI 0.62 to 3.08, p=0.435) did not show a significant association. Additionally, the frequency of night shifts (OR=1.96; 95% CI 1.71 to 2.24, p<0.001) was significantly associated with increased odds of violence (table 3).
Association between gender and violence subtypes experienced by study participants
We analysed the association between HCWs’ gender and subtypes of violence. No significant difference was observed in the proportions of verbal violence between men and women (51% vs 50.8%; χ2: 0.02; p=0.900). However, female gender was found to be associated with a significantly higher proportion of emotional violence (30.6% vs 28%; χ2: 4.15; p=0.042) and sexual violence (7.4% vs 3.8%; χ2: 31.50; p=0.001) compared with male counterparts. Male HCWs, on the other hand, were exposed to a statistically significantly higher proportion of physical abuse when compared with their female counterparts (24.2% vs 19%; χ2: 20.72; p=0.001) (online supplemental appendix B–table 4)
Discussion
In this global survey of >5000 HCWs, more than half of HCWs reported experiencing violence firsthand, and one-sixth reported witnessing violence against their colleague(s). Verbal violence was the most common, followed by emotional violence. Patients or their family members were described as the perpetrator in more than half of the cases, whereas one-sixth of the HCWs reported facing aggression from their supervisors. Furthermore, more than half of the HCWs who experienced violence felt less motivated or more dissatisfied with their job after the event. Finally, the univariate and multivariate regression models found that government institutions, increasing age, more frequent night shifts, and being a nurse, physician or any other HCW were associated with a significantly increased risk of experiencing violence. On the other hand, the female gender was not associated with increased violence risk in both the univariate analysis and when controlled for various confounders. Our analysis also reported that male HCWs were more susceptible to physical abuse, while female HCWs were more likely to experience emotional abuse and sexual harassment.
In our study, most responses came from India, the USA, Venezuela, Pakistan and Algeria (online supplemental appendix B–table 2). This could be because the highest number of, and the most active, country leads belonged to these regions. While a Chinese hospital association report (2012), including data from 316 hospitals, showed that a substantial 96% of the hospitals in China had reported cases of WPV, despite our multiple attempts, we could only receive a small number of responses from China, limiting our ability to perform a head-on comparison.29
Our study showed that violence among HCWs is prevalent among young adults (75%) with similar distribution among female and male gender. This was analogous to Alshahrani et al findings in a cross-sectional study of several emergency departments in Saudi Arabia.30 More than 90% of respondents in their study belonged to the 20–39 age group, with an equal gender distribution among the 492 respondents. They also reported that 80% of the respondents confirmed the presence of violence reporting procedures in their institutions, and only one-third of the respondents had not used any of these measures. On the contrary, our study found that although >50% of the respondents had confirmed the availability of violence reporting systems in their institutions, <50% of the respondents mentioned reporting violent conduct to either their institution’s administration or the police.
Every two out of three respondents in our study had experienced violence, either against themselves or witnessed against a colleague. The Chinese Medical Doctors Association reported that more than three-fourths of the involved physicians had experienced some form of violence at work.31 Byon et al conducted a meta-analysis to estimate the prevalence of WPV against HCWs and found it to be 22%. Of these, 36% of the incidents involved non-physical acts of violence, while 10% caused physical harm to the HCW.32 A similar trend was observed in our study, where verbal violence was reported as the most typical form of violence. Other previous studies have also reported analogous results, with non-physical violence (especially verbal violence) being the most prevalent form of violence against HCWs.30–33 Our findings also show that more than half of the respondents reported the patients or their family members as the perpetrators of aggression. Contrastingly, nearly 15% of respondents reported being victims to their supervisors, and 10% of respondents were mistreated by their colleagues. Some studies also reported patients and their family members as the most common type of aggressors, thus supporting our findings,34–36 whereas, in a few other studies, other physicians and staff were also found to have contributed to violence against fellow HCWs.37–39
Based on the International Committee of the Red Cross data, more than 600 violence cases were reported against HCWs in the first 6 months of the COVID-19 pandemic.40 In a systematic review of studies about violence against HCWs, Chirico et al also observed a high prevalence of violence against HCWs during the COVID-19 pandemic. They concluded that the risk of suffering such an episode by an HCW was excessively high during the pandemic.41 42 A crowded and less conducive hospital environment (during the pandemic) can induce stress for HCWs and patients or their families, thus risking increased violence against HCWs.41 43 In our study, every third respondent reported an increase in frequency during the pandemic, while a minority of HCWs reported a decrease in violence frequency.
Violence is associated with mental health issues such as traumatic memories, severe stress/anxiety, fear of unpredictability, etc.44 Studies suggest that patients with altered mental status, such as dementia, mental retardation, drug and substance abuse or other psychiatric disorders, are at a higher risk of inciting violence against HCWs.45 46 In other studies, an insufficient number of HCWs, poor communication between patients or families and healthcare providers or among healthcare providers and unmet care needs of patients or families were reported as the most important causes of violence.39 47 48 Comparatively, in our study, nearly 25% of the respondents described the altered mental status of patients as the most important cause of violence, 15% described the lack of HCW security, and 10% reported a lack of patient or family member education as the leading cause.
More than half of the respondents in our study reported feeling less motivated or more dissatisfied with their job in the aftermath of experiencing violence; some were willing to quit their current department or workplace, while some HCWs considered leaving the profession entirely. In congruence with our findings, a study by Rafeea et al reported that 26% of the HCWs considered leaving their job because of experiencing WPV.49 This could be attributed to the impact of violence, which manifests as decreased productivity and concentration, impaired quality of work, higher use of defensive medicine and psychological consequences (over-stress, depression or Post Traumatic Stress Disorder (PTSD)), ultimately affecting the quality of patient care.48 50–52 Recently, several recommendations have been proposed to curb violence against HCWs to protect and enhance their mental health.53
Several studies have examined the association between HCW gender and the risk of experiencing violence. Some studies have found no difference in exposure to any kind of violence based on gender, similar to our logistic regression analysis,54–56 whereas others have found that male HCWs may face higher odds of violence.57 58 Conversely, female HCWs have been found to be more likely to experience any form of violence in some studies, with gender being a significant predictor of violence even after adjusting for possible confounders like age.34 59–61
The regression analysis in our study found that female HCWs are more likely to face sexual harassment, while men are more likely to experience physical violence. These findings match with patterns seen in previous studies conducted in China (adjusted OR=2.3) and the USA (OR=1.6), which found that male HCWs were more likely to face physical violence.62 63 On the other hand, Jatic et al found that female HCWs were more likely to face sexual harassment (OR=2.06).60
Liu et al’s meta-analysis and a study from China reported that nurses and physicians were more likely to face WPV than other healthcare professions.54 In contrast, two studies reported that support staff, including ambulance drivers and security officers, were at an increased risk of violence.61 64 Our study found that HCWs, including physicians, nurses and auxiliary staff, are at a higher risk of encountering violence.
The relationship between age and the risk of WPV against HCWs) is inconsistent across studies. A US-based study and the current study found that increasing age is associated with higher odds of physical and psychological violence against HCWs.63 In contrast, the European Nurses' Early Exit (NEXT) study found that increasing age decreases the odds of being attacked at the workplace,57 whereas Wu et al observed no association between age and the risk of WPV among physicians.56
The logistic analysis in our study is in line with Campbell et al’s study, with a significantly increased risk of violence for HCWs with greater work experience, contradictory to a few other studies, which suggest the opposite.59 63 Assessing the association between healthcare facility type and violence, one study from the Democratic Republic of Congo found no significant difference in verbal, physical and sexual violence risk between government and private healthcare facilities.65 In contrast, a study from Pakistan reported a lower likelihood of WPV in private healthcare settings, concurring with our study results.66
Similar to our analysis, various studies conducted in different countries indicate that HCWs who work solely night shifts or shift work with night duties are at a higher risk of experiencing WPV, including physical and verbal violence, compared with those who work regular day shifts.57 67 68 It is important to note that our regression models were not designed to test variables as the main predictors. This might lead to incomplete control of the potential confounders. Thus, interpretation of all the above results must be done carefully.
The implications for policymakers from our study are significant. It is crucial to address the psychological impact of WPV on HCWs, leading to burnout syndrome, impaired work ability, PTSD and even retirement. Comprehensive strategies should be implemented to prevent and manage WPV, including the development of protocols and guidelines, ensuring the safety of HCWs and providing psychological support programmes tailored to their needs. The establishment and strengthening of OSHA to make it uniformly accessible worldwide to support HCWs affected by violence should be prioritised.69 Second, policymakers should invest in training programmes and educational initiatives to raise awareness about WPV and its impact on healthcare professionals.70 A strong focus should be on mitigating the added stressors HCWs face, such as excessive workloads, shortage of staff, high demands and long working hours, by implementing measures like enhanced benefits, flexible work arrangements and resiliency training programmes.71 By creating a culture of safety and zero tolerance for violence, healthcare organisations can promote the well-being of HCWs, ultimately improving the quality of patient care.
There are several strengths of our study. This is the largest global study on violence against HCWs involving >5000 HCWs. The deidentified survey response collection promoted honest and reliable responses that may have represented the actual situations. The study was non-funded and was conducted with the help of volunteers across the globe. Also, the speed of data collection in 8 weeks is another major highlight of our study.
However, we acknowledge a few limitations to the study. We used convenience sampling based on participants’ willingness and availability to take the survey, which might have increased the volunteer bias. We could be more inclusive to get more responses per country and include other countries from the South America and European continents. Also, it is a cross-sectional design, which did not allow us to describe the prevalence of WPV. The responses in our study included HCWs with diverse backgrounds and cultures, which could lead to self-reporting bias. To negate this to a certain extent, 106 respondents from 31 countries were excluded because of incomplete responses, missing demographics or less than 10 responses per country. Also, there is a chance of bias in the 10-point ranking questions. Some respondents might have chosen the top-listed responses as a high priority, as they were in alphabetical order. Thus, the result should be taken with a grain of salt. Finally, the survey was conducted only in English, except for verbal translation guidance in Spanish and Arabic, which could lead to a language barrier among non-English speakers.
Conclusion
Apart from reaffirming the global presence of violence against HCWs, the ViSHWaS survey-based study highlighted the significance of varied forms of violence, including verbal and emotional violence. The outcome concerning the diminished morale of the HCWs and the fear of non-preparedness for a violent episode warrants attention. Notably, increased perception of violence in the light of the COVID-19 pandemic has further enhanced the need for reforms within. The HCWs need to be protected and provided with tools and training to improve stress management associated with violence in the workplace. Further studies based on large-scale analysis over a longer duration with participation from non-English speaking nations are required to build an accurate estimate of the current state of violence in healthcare.
bmjgh-2023-013101supp001.pdf (98.7KB, pdf)
bmjgh-2023-013101supp003.pdf (80.5KB, pdf)
Acknowledgments
We acknowledge Mr. Deepanshu Jain for mentoring us on data cleaning and analysis. We acknowledge Grammarly for assistance with the English Language review of the manuscript. Parts of the manuscript have been submitted and accepted as abstracts for presentation at the Society of Critical Care Medicine annual meeting (SCCM 2023) in San Francisco, USA, in January 2023; The 3rd Abu Dhabi Integrated Mental Health Conference in Abu Dhabi, UAE, in January 2023; The American Thoracic Society International conference in Washington, DC in May 2023. An initial version of the manuscript abstract has been submitted and published on the Lancet SSRN preprint platform.
Footnotes
Handling editor: Seema Biswas
Twitter: @stethospeaks, @HamuzaDhabuliwo, @Dr_SRKashyap
Collaborators: For GRRSP-ViSHWaS Study Group investigators: Rahul Kashyap, Akshat Banga, Umme Habiba Faisal, Tanya Amal, Gaurang Bhatt, Ayushi Mendiratta, Piyush Garg, Harsha Pattnaik, Alisha Lakhani, L V Simhachalam Kutikuppala, Bhaswanth Bollu, Divya Randhawa, Rakhtan Qasba, Rahul Kashyap, Salim Surani, Ramesh Pandit, Trupti Pandit, Ramesh Adhikari, Ayesha Khalid, Ayushi Mendiratta, Tanya Amal, Akshat Banga, Ravina Verma, Kush Shah, John Counsell, Naresh Dasari, Melissa Schlenker, PratikKumar Vekaria, Taru Dutt, Raghavendra Tirupathi, Raghu Gandhi, Gowthami Sai Kogilathota Jagirdhar, Nancy Nagib, Vikas Bansal, Pranjal Sharma, Benjamin Schlenker, Genesis Camacho Leon, Hans Mautong, Aisha Khalid, Umme Habiba Faisal, Salim Surani, Faizan Ahmad, Taha Mansoor, Piyush Garg, Mohammed Amir Rais, Ivan Huespe, Aisha Khalid, Pierre Ciza N, Gaurang Bhatt, Hans Mautong, Leydi Del Pilar Lema Lema, Aisha Khalid, Nimsi Barrios, Gaurang Bhatt, Kelly Meza, Gaurang Bhatt, Susan Sheila, Bello Saifullah Muhammad, Gaurang Bhatt, Barakat Kolawole, Amuza Dhabuliwo, Gaurang Bhatt, Umme Habiba Faisal, L V Simhachalam Kutikuppala, Piyush Garg, Hafeez Hamza, Rahul Kashyap, Mohammad Yasir Essar, Arash Nemat, Razan Alamoudi, Gaurang Bhatt, Keidy Zamora, Joanna Lee, Bikona Ghosh, Rakhtan Qasba, L V Simhachalam Kutikuppala, Sama Soliman, Zainab Ayoob, Lina Almahmoud, Mohammed Amir Rais, Daniel Martin Simadibrata, Faisal Nawaz, Dohha Mohammed, Mohammed Amir Rais, Oyindamola Obadare, Kelly Meza, Gaurang Bhatt, Tanya Amal, Era Mae Ramirez, Kalloush shahed, Mohammed Yasir Essar, Sarya Swed, Mohammed Amir Rais, Temaa Alklani, Zainab Ayoob, Mohammed Amir Rais, Tanya Amal, Ishimwe Florent, Gaurang Bhatt, Goodluck Nchasi, Faisal Nawaz, Daren Poh Kiat How, Faisal Nawaz, Mohamed Elfagieh, Faisal Nawaz, Mariam Elsaban, Moath Almekhlafi, Mohammed Amir Rais, Reshon Hadmon, Anasonye Emmanuel, Gaurang Bhatt, Yosra Magdi Makki, Faisal Nawaz, Mohammed Amir Rais, Gaurang Bhatt, Rodrigue Ndabashinze, Hussein Dawoud, Mohammed Amir Rais, Dimitrios Kantas, Christos Tsagkaris, Faisal Nawaz, Daniella Myriam Pierre, Rahul Kashyap, Zeynep Pelin Orhan, Faisal Nawaz, Akshat Banga, Usama Oguz, Rahul Kashyap, Jorge Salluh,Tanya Amal, Hafeez Hamza, Gaurang Bhatt, Hedys Selene Ordóñez Mogollón, Tanja Kovacevic, Rahul Kashyap, Ramesha Remy, Gaurang Bhatt, Hassan Dawood Alli, Aisha Khalid, Marija Vukoja, Srdjan Gavrilovic, Alicja Rydzewska Rosolowska, Umme Faisal, Alisha Lakhani, Franz Lopez, Tanya Amal, Reshon Hadmon, Dattatreya Mukherjee, Alisha Lakhani, Salem Ramirez, Kelly Meza, Lisdamys Morera Gonzalez, Kelly Meza, Joanna Lee, L V Simhachalam Kutikuppala, Mohammed Alkawak, Marco Antonio Herrera Del Villar, Kelly Maza, Aisha Khalid, Joanna Lee, L V Simhachalam Kutikuppala, Tanya Amal, Priyadarshini Bhattacharjee, Aisha Khalid, Dattatreya Mukherjee, L V Simhachalam Kutikuppala, Alisha Lakhani, Marija Vukoja, Srdjan Gavrilovic, Mariam Elsaban, Akshat Banga, Aisha Khalid, L V Simhachalam Kutikuppala, Reshon Hadmon, Umme Faisal, L V Simhachalam Kutikuppala, L V Simhachalam Kutikuppala, L V Simhachalam Kutikuppala, Reshon Hadmon, Umme Faisal, L V Simhachalam Kutikuppala, L V Simhachalam Kutikuppala, Shehu Bledi, Jonida Naska, Joanna Lee
Contributors: AB, BB, FAN, RKQ, MYE and RK contributed to study conceptualisation and methodology; REDCap forms were used to create the survey and STATA software was used to perform statistical analysis. All co-authors contributed to data acquisition; AB, RK and HM contributed to data curation, formal analysis and interpretation; The original draft was prepared by AB, AM, DMS, FAN, IH, JL, RA, LVSK and UHF. All listed co-authors authors provided intellectual contributions and made critical revisions to this paper. All authors approved the final version of the manuscript. AB is responsible for the overall content as the guarantor. The guarantor accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Contributor Information
For GRRSP-ViSHWaS Study Group:
Rahul Kashyap, Akshat Banga, Umme Habiba Faisal, Tanya Amal, Gaurang Bhatt, Ayushi Mendiratta, Piyush Garg, Harsha Pattnaik, Alisha Lakhani, L V Simhachalam Kutikuppala, Bhaswanth Bollu, Divya Randhawa, Rakhtan Qasba, Rahul Kashyap, Salim Surani, Ramesh Pandit, Trupti Pandit, Ramesh Adhikari, Ayesha Khalid, Ayushi Mendiratta, Tanya Amal, Akshat Banga, Ravina Verma, Kush Shah, John Counsell, Naresh Dasari, Melissa Schlenker, PratikKumar Vekaria, Taru Dutt, Raghavendra Tirupathi, Raghu Gandhi, Gowthami Sai Jagirdhar, Nancy Nagib, Vikas Bansal, Pranjal Sharma, Benjamin Schlenker, Genesis Camacho-Leon, Hans Mautong, Aisha Khalid, Umme Habiba Faisal, Salim Surani, Faizan Ahmad, Taha Mansoor, Piyush Garg, Mohammed Amir Rais, Ivan Huespe, Aisha Khalid, N Pierre Ciza, Gaurang Bhatt, Hans Mautong, Leydi Del Lema, Aisha Khalid, Nimsi Barrios, Gaurang Bhatt, Kelly Meza, Gaurang Bhatt, Susan Sheila, Bello Saifullah Muhammad, Gaurang Bhatt, Barakat Kolawole, Amuza Dhabuliwo, Gaurang Bhatt, Umme Habiba Faisal, L V Kutikuppala, Piyush Garg, Hafeez Hamza, Rahul Kashyap, Mohammad Yasir Essar, Arash Nemat, Razan Alamoudi, Gaurang Bhatt, Keidy Zamora, Joanna Lee, Bikona Ghosh, Rakhtan Qasba, L V Kutikuppala, Sama Soliman, Zainab Ayoob, Lina Almahmoud, Mohammed Amir Rais, Daniel Martin Simadibrata, Faisal Nawaz, Dohha Mohammed, Mohammed Amir Rais, Oyindamola Obadare, Kelly Meza, Gaurang Bhatt, Tanya Amal, Era Mae Ramirez, Kalloush Shahed, Mohammed Yasir Essar, Sarya Swed, Mohammed Amir Rais, Temaa Alklani, Zainab Ayoob, Mohammed Amir Rais, Tanya Amal, Ishimwe Florent, Gaurang Bhatt, Goodluck Nchasi, Faisal Nawaz, Daren Poh How, Faisal Nawaz, Mohamed Elfagieh, Faisal Nawaz, Mariam Elsaban, Moath Almekhlafi, Faisal Nawaz, Mariam Elsaban, Moath Almekhlafi, Mohammed Amir Rais, Reshon Hadmon, Anasonye Emmanuel, Gaurang Bhatt, Yosra Magdi Makki, Faisal Nawaz, Mohammed Amir Rais, Gaurang Bhatt, Rodrigue Ndabashinze, Hussein Dawoud, Mohammed Amir Rais, Dimitrios Kantas, Christos Tsagkaris, Faisal Nawaz, Daniella Myriam Pierre, Rahul Kashyap, Zeynep Pelin Orhan, Faisal Nawaz, Akshat Banga, Usama Oguz, Rahul Kashyap, Jorge Salluh, Tanya Amal, Hafeez Hamza, Gaurang Bhatt, Hedys Selene Mogollón, Tanja Kovacevic, Rahul Kashyap, Ramesha Remy, Gaurang Bhatt, Hassan Dawood Alli, Aisha Khalid, Marija Vukoja, Srdjan Gavrilovic, Alicja Rydzewska Rosolowska, Umme Faisal, Alisha Lakhani, Franz Lopez, Tanya Amal, Reshon Hadmon, Dattatreya Mukherjee, Alisha Lakhani, Salem Ramirez, Kelly Meza, Lisdamys Morera Gonzalez, Kelly Meza, Joanna Lee, L V Kutikuppala, Mohammed Alkawak, Marco Antonio Villar, Kelly Maza, Aisha Khalid, Joanna Lee, L V Kutikuppala, Tanya Amal, Priyadarshini Bhattacharjee, Aisha Khalid, Dattatreya Mukherjee, L V Kutikuppala, Alisha Lakhani, Marija Vukoja, Srdjan Gavrilovic, Mariam Elsaban, Akshat Banga, Aisha Khalid, L V Kutikuppala, Reshon Hadmon, Umme Faisal, L V Kutikuppala, L V Kutikuppala, L V Kutikuppala, Reshon Hadmon, Umme Faisal, L V Kutikuppala, L V Kutikuppala, Shehu Bledi, Jonida Naska, and Joanna Lee
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
The study was granted an exemption from the Mayo Clinic Institutional Review Board.
References
- 1. Li P, Xing K, Qiao H, et al. Psychological violence against general practitioners and nurses in Chinese Township hospitals: incidence and implications. Health Qual Life Outcomes 2018;16:117. 10.1186/s12955-018-0940-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Shea T, Sheehan C, Donohue R, et al. Occupational violence and aggression experienced by nursing and caring professionals. J Nurs Scholarsh 2017;49:236–43. 10.1111/jnu.12272 [DOI] [PubMed] [Google Scholar]
- 3. Watson A, Jafari M, Seifi A. The persistent pandemic of violence against health care workers. Am J Manag Care 2020;26:e377–9. 10.37765/ajmc.2020.88543 [DOI] [PubMed] [Google Scholar]
- 4. WHO . Framework guidelines for addressing workplace violence in the health sector / Joint Programme on Workplace Violence in the Health Sector. Geneva, 2002. [Google Scholar]
- 5. Gerberich SG, Church TR, McGovern PM, et al. An epidemiological study of the magnitude and consequences of work related violence: the Minnesota nurses' study. Occup Environ Med 2004;61:495–503. 10.1136/oem.2003.007294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Phillips JP. Workplace violence against health care workers in the United States. N Engl J Med 2016;375:e14. 10.1056/NEJMc1606816 [DOI] [PubMed] [Google Scholar]
- 7. Wassell JT. Workplace violence intervention effectiveness: a systematic literature review. Safety Science 2009;47:1049–55. 10.1016/j.ssci.2008.12.001 [DOI] [Google Scholar]
- 8. Bhatti OA, Rauf H, Aziz N, et al. Violence against healthcare workers during the COVID-19 pandemic: a review of incidents from a lower-middle-income country. Ann Glob Health 2021;87:41. 10.5334/aogh.3203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Howard J. State and local regulatory approaches to preventing workplace violence. Occup Med 1996;11:293–301. [PubMed] [Google Scholar]
- 10. Kam K. Webmd. n.d. Available: https://www.webmd.com/a-to-z-guides/news/20210318/on-the-front-lines-violence-against-nurses-on-the-rise
- 11. Kumari A, Kaur T, Ranjan P, et al. Workplace violence against doctors: characteristics, risk factors, and mitigation strategies. J Postgrad Med 2020;66:149–54. 10.4103/jpgm.JPGM_96_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Aljohani B, Burkholder J, Tran QK, et al. Workplace violence in the emergency department: a systematic review and meta-analysis. Public Health 2021;196:186–97. 10.1016/j.puhe.2021.02.009 [DOI] [PubMed] [Google Scholar]
- 13. Arafa A-O, Shehata A, Youssef M, et al. Violence against healthcare workers during the COVID-19 pandemic: a cross-sectional study from Egypt. Arch Environ Occup Health 2022;77:621–7. 10.1080/19338244.2021.1982854 [DOI] [PubMed] [Google Scholar]
- 14. D’Ettorre G, Pellicani V, Mazzotta M, et al. Preventing and managing workplace violence against healthcare workers in emergency departments. Acta Biomed 2018;89:28–36. 10.23750/abm.v89i4-S.7113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Nagpal N. Incidents of violence against doctors in India: can these be prevented? Natl Med J India 2017;30:97–100. [PubMed] [Google Scholar]
- 16. Baykan Z, Öktem İS, Çetinkaya F, et al. Physician exposure to violence: a study performed in Turkey. Int J Occup Saf Ergon 2015;21:291–7. 10.1080/10803548.2015.1073008 [DOI] [PubMed] [Google Scholar]
- 17. Zafar W, Khan UR, Siddiqui SA, et al. Workplace violence and self-reported psychological health: coping with post-traumatic stress, mental distress, and burnout among physicians working in the emergency departments compared to other specialties in Pakistan. J Emerg Med 2016;50:167–77. 10.1016/j.jemermed.2015.02.049 [DOI] [PubMed] [Google Scholar]
- 18. Kashyap R. GRRSP - Global Remote Research Scholars Program- Next Batch Introduction 2022 2023. YouTube, 2022. [Google Scholar]
- 19. Kashyap R. ViSHWaS Global team meeting - Introduction and Contribution. Global remote research scholars program - violence study of health care workers and systems. YouTube, 2022. [Google Scholar]
- 20. Turek JR, Bansal V, Tekin A, et al. Lessons from a rapid project management exercise in the time of pandemic: methodology for a global COVID-19 VIRUS registry database. JMIR Res Protoc 2022;11:e27921. 10.2196/27921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kashyap R, Vashistha K, Saini C, et al. Critical care practice in India: results of the intensive care unit need assessment survey (Inin2018). World J Crit Care Med 2020;9:31–42. 10.5492/wjccm.v9.i2.31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Nawaz FA, Deo N, Surani S, et al. Critical care practices in the world: results of the global intensive care unit need assessment survey 2020. World J Crit Care Med 2022;11:169–77. 10.5492/wjccm.v11.i3.169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tripathi S, Kaur H, Kashyap R, et al. A survey on the resources and practices in pediatric critical care of resource-rich and resource-limited countries. J Intensive Care 2015;3:40. 10.1186/s40560-015-0106-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Vukoja M, Dong Y, Adhikari NKJ, et al. Checklist for early recognition and treatment of acute illness and injury: an exploratory multicenter International quality-improvement study in the ICUs with variable resources. Crit Care Med 2021;49:e598–612. 10.1097/CCM.0000000000004937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kashyap R, Amal T, Banga A, et al. Guiding principles for the conduct of violence study of healthcare workers and system (vishwas). American Thoracic Society 2023 International Conference, May 19-24, 2023 - Washington, DC; May 2023. 10.1164/ajrccm-conference.2023.207.1_MeetingAbstracts.A4883 [DOI] [Google Scholar]
- 26. Amal T, Banga A, Bollu B, et al. 104: a global survey of impact of violence against healthcare workers in critical care settings: Vishwas. Crit Care Med 2023;51:35. 10.1097/01.ccm.0000906152.22923.ac [DOI] [Google Scholar]
- 27. Rais MA, Alamoudi R, Banga A, et al. Violence against healthcare workers: Vishwas study of 17 countries in the MENA region. 2023.
- 28. Banga A, Bollu B, Faisal UH, et al. Vishwas - violence study of healthcare workers and systems: a global survey-based study. SSRN Journal 2022. 10.2139/ssrn.4272781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Yao S, Zeng Q, Peng M, et al. Stop violence against medical workers in China. J Thorac Dis 2014;6:E141–5. 10.3978/j.issn.2072-1439.2014.06.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Alshahrani M, Alfaisal R, Alshahrani K, et al. Incidence and prevalence of violence toward health care workers in emergency departments: a multicenter cross-sectional survey. Int J Emerg Med 2021;14:71. 10.1186/s12245-021-00394-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Yang SZ, Wu D, Wang N, et al. Workplace violence and its aftermath in China's health sector: implications from a cross-sectional survey across three tiers of the health system. BMJ Open 2019;9:e031513. 10.1136/bmjopen-2019-031513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Byon HD, Lee M, Choi M, et al. Prevalence of type II workplace violence among home healthcare workers: a meta-analysis. Am J Ind Med 2020;63:442–55. 10.1002/ajim.23095 [DOI] [PubMed] [Google Scholar]
- 33. Li B, Yang J, Zhao F, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol 2020;109:531–8. 10.1007/s00392-020-01626-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Abed M, Morris E, Sobers-Grannum N. Workplace violence against medical staff in healthcare facilities in Barbados. Occup Med (Lond) 2016;66:580–3. 10.1093/occmed/kqw073 [DOI] [PubMed] [Google Scholar]
- 35. Park M, Cho S-H, Hong H-J. Prevalence and perpetrators of workplace violence by nursing unit and the relationship between violence and the perceived work environment. J Nurs Scholarsh 2015;47:87–95. 10.1111/jnu.12112 [DOI] [PubMed] [Google Scholar]
- 36. Sachdeva S, Jamshed N, Aggarwal P, et al. Perception of workplace violence in the emergency department. J Emerg Trauma Shock 2019;12:179–84. 10.4103/JETS.JETS_81_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Demirci Ş, Uğurluoğlu Ö. An evaluation of verbal, physical, and sexual violence against healthcare workers in Ankara, Turkey. J Forensic Nurs 2020;16:E33–41. 10.1097/JFN.0000000000000286 [DOI] [PubMed] [Google Scholar]
- 38. Honarvar B, Ghazanfari N, Raeisi Shahraki H, et al. Violence against nurses: a neglected and health-threatening epidemic in the University affiliated public hospitals in Shiraz, Iran. Int J Occup Environ Med 2019;10:111–23. 10.15171/ijoem.2019.1556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Shafran-Tikva S, Chinitz D, Stern Z, et al. Violence against physicians and nurses in a hospital: how does it happen? A mixed-methods study. Isr J Health Policy Res 2017;6:59. 10.1186/s13584-017-0183-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Devi S. COVID-19 exacerbates violence against health workers. Lancet 2020;396:658. 10.1016/S0140-6736(20)31858-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Chirico F, Afolabi A, Ilesanmi O, et al. Workplace violence against healthcare workers during the COVID-19 pandemic: a systematic review. Journal of Health and Social Sciences 2022;7:14–35. [Google Scholar]
- 42. Chirico F, Nucera G. Tribute to healthcare operators threatened by the COVID-19 pandemic. Journal of Health and Social Sciences 2020;5:165–8. [Google Scholar]
- 43. Medley DB, Morris JE, Stone CK, et al. An association between occupancy rates in the emergency department and rates of violence toward staff. J Emerg Med 2012;43:736–44. 10.1016/j.jemermed.2011.06.131 [DOI] [PubMed] [Google Scholar]
- 44. Stene J, Larson E, Levy M, et al. Workplace violence in the emergency department: giving staff the tools and support to report. Perm J 2015;19:e113–7. 10.7812/TPP/14-187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ferri P, Silvestri M, Artoni C, et al. Workplace violence in different settings and among various health professionals in an Italian general hospital: a cross-sectional study. Psychol Res Behav Manag 2016;9:263–75. 10.2147/PRBM.S114870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Zafar W, Siddiqui E, Ejaz K, et al. Health care personnel and workplace violence in the emergency departments of a volatile metropolis: results from Karachi, Pakistan. J Emerg Med 2013;45:761–72. 10.1016/j.jemermed.2013.04.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Alsaleem SA, Alsabaani A, Alamri RS, et al. Violence towards healthcare workers: a study conducted in Abha city, Saudi Arabia. J Family Community Med 2018;25:188–93. 10.4103/jfcm.JFCM_170_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Hamdan M, Abu Hamra A. Workplace violence towards workers in the emergency departments of Palestinian hospitals: a cross-sectional study. Hum Resour Health 2015;13:28. 10.1186/s12960-015-0018-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Rafeea F, Al Ansari A, Abbas EM, et al. Violence toward health workers in Bahrain defense force Royal medical services' emergency Department. Open Access Emerg Med 2017;9:113–21. 10.2147/OAEM.S147982 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Binmadi NO, Alblowi JA. Prevalence and policy of occupational violence against oral Healthcare workers: systematic review and meta-analysis. BMC Oral Health 2019;19:279. 10.1186/s12903-019-0974-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. D’Ettorre G, Pellicani V, Vullo A. Workplace violence against healthcare workers in emergency departments. A case-control study. Acta Biomed 2019;90:621–4. 10.23750/abm.v90i4.7327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Toraldo DM, Vergari U, Toraldo M. “Medical malpractice, defensive medicine and role of the "media" in Italy”. Multidiscip Respir Med 2015;10:12. 10.1186/s40248-015-0006-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Rija A, Islam Z, Bilal W, et al. The impact of violence on healthcare workers' mental health in conflict based settings amidst COVID-19 pandemic, and potential interventions: A narrative review. Health Sci Rep 2022;5:e920. 10.1002/hsr2.920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Liu J, Gan Y, Jiang H, et al. Prevalence of workplace violence against healthcare workers: a systematic review and meta-analysis. Occup Environ Med 2019;76:927–37. 10.1136/oemed-2019-105849 [DOI] [PubMed] [Google Scholar]
- 55. Noorullahi S, Safaie N, Soltani-Kermanshahi M, et al. The prevalence of workplace violence and related factors in the emergency department staff of Iran: a cross-sectional study. Middle East Curr Psychiatry 2022;29:82. 10.1186/s43045-022-00247-4 [DOI] [Google Scholar]
- 56. Wu JC, Tung TH, Chen PY, et al. Determinants of workplace violence against clinical physicians in hospitals. J Occup Health 2015;57:540–7. 10.1539/joh.15-0111-OA [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Estryn-Behar M, van der Heijden B, Camerino D, et al. Violence risks in nursing—results from the European ‘NEXT’ study. Occupational Medicine 2008;58:107–14. 10.1093/occmed/kqm142 [DOI] [PubMed] [Google Scholar]
- 58. Sun P, Zhang X, Sun Y, et al. Workplace violence against health care workers in North Chinese hospitals: a cross-sectional survey. Int J Environ Res Public Health 2017;14:96. 10.3390/ijerph14010096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Hahn S, Hantikainen V, Needham I, et al. Patient and visitor violence in the general hospital, occurrence, staff interventions and consequences: a cross-sectional survey. J Adv Nurs 2012;68:2685–99. 10.1111/j.1365-2648.2012.05967.x [DOI] [PubMed] [Google Scholar]
- 60. Jatic Z, Erkocevic H, Trifunovic N, et al. Frequency and forms of workplace violence in primary health care. Med Arch 2019;73:6–10. 10.5455/medarh.2019.73.6-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Seun-Fadipe CT, Akinsulore AA, Oginni OA. Workplace violence and risk for psychiatric morbidity among health workers in a tertiary health care setting in Nigeria: prevalence and correlates. Psychiatry Res 2019;272:730–6. 10.1016/j.psychres.2018.12.177 [DOI] [PubMed] [Google Scholar]
- 62. Zhu L, Li L, Lang J. Gender differences in workplace violence against physicians of obstetrics and Gynecology in China: a questionnaire in the National Congress. PLoS One 2018;13:e0208693. 10.1371/journal.pone.0208693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Campbell JC, Messing JT, Kub J, et al. Workplace violence: prevalence and risk factors in the safe at work study. J Occup Environ Med 2011;53:82–9. 10.1097/JOM.0b013e3182028d55 [DOI] [PubMed] [Google Scholar]
- 64. Arnetz J, Hamblin LE, Sudan S, et al. Organizational determinants of workplace violence against hospital workers. J Occup Environ Med 2018;60:693–9. 10.1097/JOM.0000000000001345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Muzembo BA, Mbutshu LH, Ngatu NR, et al. Workplace violence towards congolese health care workers: a survey of 436 healthcare facilities in Katanga province, democratic Republic of Congo. Jrnl of Occup Health 2015;57:69–80. 10.1539/joh.14-0111-OA [DOI] [PubMed] [Google Scholar]
- 66. Shaikh S, Baig LA, Hashmi I, et al. The magnitude and determinants of violence against healthcare workers in Pakistan. BMJ Glob Health 2020;5:e002112. 10.1136/bmjgh-2019-002112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Abdellah RF, Salama KM. Prevalence and risk factors of workplace violence against health care workers in emergency department in Ismailia. Pan Afr Med J 2017;26:21. 10.11604/pamj.2017.26.21.10837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Gacki-Smith J, Juarez AM, Boyett L, et al. Violence against nurses working in US emergency departments. JONA 2009;39:340–9. 10.1097/NNA.0b013e3181ae97db [DOI] [PubMed] [Google Scholar]
- 69. Chirico F, Leiter M. “Tackling stress, burnout, suicide and preventing the "great resignation" phenomenon among healthcare workers (during and after the COVID-19 pandemic) for maintaining the sustainability of healthcare systems and reaching the 2030 sustainable development goals”. Journal of Health and Social Sciences 2022;7:9–13. [Google Scholar]
- 70. Magnavita N, Chirico F, Sacco A. COVID-19: from hospitals to courts. The Lancet 2021;397:1542. 10.1016/S0140-6736(21)00472-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Magnavita N, Heponiemi T, Chirico F. Workplace violence is associated with impaired work functioning in nurses: an Italian cross‐sectional study. J Nurs Scholarsh 2020;52:281–91. 10.1111/jnu.12549 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2023-013101supp002.pdf (1.9MB, pdf)
bmjgh-2023-013101supp001.pdf (98.7KB, pdf)
bmjgh-2023-013101supp003.pdf (80.5KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.