Abstract
Objectives:
Adolescent girls and young women younger than 25 years (AGYW) account for disproportionate HIV infections in sub-Saharan Africa. Impacts of war in Northern Uganda continue to affect HIV-related health and wellbeing of young people postconflict. Prevalence and incidence of HIV infection were estimated, and factors associated with HIV prevalence among sexually active AGYW in Northern Uganda were investigated.
Methods:
Cango Lyec is a cohort involving conflict-affected populations in Northern Uganda. Nine randomly selected communities in Gulu, Nwoya, and Amuru districts were mapped. House-to-house census was conducted. Consenting participants aged 13–49 years were enrolled over 3 study rounds (2011–2015), of whom 533 were AGYW and had ever had sex. Data were collected on trauma, depression, and sociodemographic–behavioral characteristics. Venous blood was taken for HIV and syphilis serology. Multivariable logistic regression determined baseline factors associated with HIV prevalence.
Results:
HIV prevalence among AGYW was 9.7% (95% CI: 7.3 to 12.6). AGYW living in Gulu (adjusted risk ratio, aRR: 2.48; 95% CI: 1.12 to 5.51) or Nwoya (aRR: 2.65; 95% CI: 1.03 to 6.83) were more likely than in Amuru to be living with HIV. Having self-reported genital ulcers (aRR: 1.93; 95% CI: 0.97 to 3.85) or active syphilis (aRR: 3.79; 95% CI: 2.35 to 6.12) was associated with increased risk of HIV infection. The likelihood of HIV was higher for those who experienced sexual violence in the context of war (aRR: 2.37; 95% CI: 1.21 to 4.62) and/or probable depression (aRR: 1.95; 95% CI: 1.08 to 3.54). HIV incidence was 8.9 per 1000 person-years.
Conclusion:
Ongoing legacies of war, especially gender violence and trauma, contribute to HIV vulnerability among sexually active AGYW. Wholistic approaches integrating HIV prevention with culturally safe initiatives promoting sexual and mental health in Northern Uganda are essential.
Key Words: adolescent girls and young women, HIV/AIDS, conflict-affected people, Northern Uganda, HIV prevalence, trauma, mental health
INTRODUCTION
Adolescent Girls and Young Women in Northern Uganda
Adolescent girls (13–19) and young women (20–24) (AGYW) continue to experience unacceptably high risk of HIV infection.1 An estimated 360,000 AGYW aged 15–24 years are infected with HIV yearly, almost 1,000 daily.1 This is 44% higher than among young men the same age.1 In 2019, AGYW represented 1 in 4 new infections in sub-Saharan Africa, despite accounting for just 10% of the population.2 HIV vulnerability among AGYW is rooted in harmful gender norms and inequalities manifesting in violence and negative social determinants of health.3,4 Global leaders remain concerned that sexual and reproductive health needs of AGYW are not being met.4 In 2016, the United Nations General Assembly pledged to “eliminate gender inequalities and end all forms of violence and discrimination against women and girls” to reduce new HIV infections among AGYW to below 100,000 annually.3 In Uganda, HIV prevalence among AGYW aged 15–24 years is 3.3%, compared with 0.8% among young men.5 However, HIV-related health and wellbeing of AGYW in postconflict Northern Uganda is less understood.
Impact of the War on Young People
From 1986 to 2006, prolonged conflict between the Ugandan government and Lord's Resistance Army was characterized by widespread displacement of families from ancestral territories; human rights violations; destruction of social, cultural, and economic systems; and child abductions.6,7 Approximately 66,000 children were abducted by the Lord's Resistance Army, resulting in what has been described as the“longest child hostage crisis in human history”6 Between 2003 and 2006, tens of thousands more children, adolescents, and women engaged in“night-commuting,”walking as far as 6 miles each night to reach urban areas and larger internally displaced persons' (IDP) camps to escape attacks from fighting forces.8,9 They, however, faced risk of sexual violence due to vulnerabilities during commutes and within IDP camps.10 Heightened HIV vulnerability of AGYW surviving bush and IDP camps stems primarily from elevated risk of rape and sexual violence, including by armed forces.11,12 AGYW who were abducted faced forced”marriages”to rebel commanders; due to perception that they were less likely to be living with HIV.13,14 Rape outside forced marriages was rare.12–14 Those who were born or grew up during 2 decades of war—including children born in captivity—have been deemed a”lost generation,”as a result of war-related trauma and impact of breakdown of family, livelihoods, cultural norms, and other social structures.6
Postconflict Era
Postconflict, most of the 2 million IDPs who lived in camps at the height of the crisis have returned to their homelands, driven by cultural ties to the land and region, or have resettled in new locations. However, as conflict-affected AGYW navigate new environments outside of the bush and IDP camps where they have spent most of their lives, district officials are concerned that they face new and undocumented vulnerabilities to HIV infection.15 Potential vulnerabilities include, sexual coercion, harmful gender norms that affect young people's sexual behavior and perpetuate male dominance and violence against women, and increased mobility from more remote communities to access mobile markets for household necessities. Four years following the signing of the cessation of hostilities agreement, a 2010 cross-sectional study involving 384 young (aged 15–29 years) transit camp residents in Gulu district estimated HIV prevalence to be 15.6% among AGYW, compared with 9.9% among young men, although differences were not significant.16 AGYW who were children during the war are now transitioning to adolescence and adulthood in challenging environments. Economic pressures to enter sex work are exacerbated by stigmas against those who endured war-related sexual violence, including forced marriage and motherhood in the bush.13 Enduring impacts on traditional livelihoods and social structures, as well as limited resources such as health care, employment, and education in ancestral villages, has contributed to an influx of people to towns, especially Gulu city.17 As ancestral homes are redeveloped, AGYW remaining in town without parental supervision may be vulnerable to predation.18 Those remaining in town are younger and poorer and may face considerable vulnerabilities, such as lack of skills, resources, and family or social connections, contributing to elevated HIV risk.17
Although HIV infection among AGYW has received increased attention globally, concerns remain that those in postconflict settings will be left behind if the drivers of risk are not well-understood. At present, there is a paucity of research about the burden and drivers of HIV among AGYW in postconflict contexts. As such, we measured incidence and prevalence of, and investigated factors associated with, HIV infection among AGYW who have ever had sex in Northern Uganda to inform targeted recommendations for HIV prevention.
METHODS
Study Design and Sample
Cango Lyec (Healing the Elephant) is an open cohort involving conflict-affected populations in mid-Northern Uganda. Study methods have been previously reported.19,20 In brief, 8 study communities randomly selected in the districts of Gulu, Nwoya, and Amuru were mapped and house-to-house census conducted to enumerate the entire population. Consenting participants aged 13–49 years were enrolled over 3 study rounds (2011–2015), including 852 AGYW, of whom 533 (63.2%) had ever had sex. All eligible members (aged 13–49 years) of the households in the 9 communities who were present during census and consented/assented to be part of the study were enrolled. A census was conducted first to determine eligibility, and a survey team consented eligible household members to participate in the interview and blood draw. There was no sampling performed at the household level. Of the 2954 eligible individuals present at the time of census in the Cango Lyec study, 2448 enrolled in this study for a participation rate of 82.9%. Among AGYW, the participation rate was 77.3%. An analysis of attrition was conducted among AGYW, and the enrolled sample was found to be representative of the census.
Ethical Considerations
Ethical approvals for Cango Lyec were obtained from University of British Columbia-Providence Healthcare Research Ethics Board (Canada), Makerere University College of Health Sciences-School of Public Health Ethics Committee (Uganda), and Uganda Virus Research Institute-Science and Ethics Committee (Uganda). The Uganda National Council for Science and Technology issued a letter of approval based on nonobjection from the Office of the President of Uganda. Subsequently, each Resident District Commissioner provided administrative approval affirming that the study was welcome in that district. All participants provided written informed consent through signature or thumbprint following a rigorous consenting process. First, research assistants visited houses and explained all study information to household members. Permission to recruit was sought from heads of each household. Then, if a household member showed willingness, they were taken through the consenting process and were assured they could withdraw at any point. Questions were encouraged, and a copy of the consent form was provided. Unemancipated minors (as defined by the Uganda National Council of Science and Technology) were asked to provide individual informed assent if written consent was provided by parent/guardian. Minors who did not want to participate were not enrolled.
Data Collection and Measures
HIV-1 infection was determined by blood specimen collection at baseline and again annually over the study period. Two ELISA tests, Vironostika HIV Uni-Form II plus O (bioMerieux SA, Marcy l’Etoile, France) and Murex HIV-1.2.O (Diasorin S.P.A, Dartford, United Kingdom) were used in parallel to test for HIV infection at the Uganda Virus Research Institute IAVI-laboratory. Western blot (Genetic Systems; Bio-Rad Laboratories) served as tiebreaker if ELISA results were discordant. Indeterminate Western blot results were resolved using a qualitative Roche COBAS AmpliPrep/COBAS TaqMan HIV-1 polymerase chain reaction test (RT). Trained HIV counsellors provided pretest/posttest counselling, and participants were encouraged, but not required, to receive results and share results with their partners. Participants who tested positive and received results were referred for antiretroviral treatment at the health facility of their choice. HIV testing was conducted regardless of prior known HIV status or clinical records.
A team of experienced health professionals independently undertook forward–backward translation of survey instruments into Luo. Inconsistencies were discussed and revised until intended meaning was achieved. All AGYW were given the option to be interviewed by interviewers of the same sex. Participants were given the choice of where the interview would take place; often an open area (eg, under a mango tree) was preferred for greater confidentiality. Interviewer-administered questionnaires asked about sociodemographics, war-related trauma, mental health, and sexual vulnerabilities. Interviewers received extensive training on confidentiality protocols. Assurance of confidentiality formed part of the consenting process. Blood was taken for HIV and syphilis serology.
Sociodemographic characteristics included district of residence (Amuru/Gulu/Nwoya), age (years), study round (1/2/3), ethnicity (Acholi/other), education (≤primary/≥secondary), marital status (married/not married), polygamous marriage (yes/no), religion (Roman Catholic/Protestant/Other), youth-headed household (yes/no), and female-headed household (yes/no).
Several war-related trauma and mental health measures were assessed. Community displacement status included displaced settlements (eg, those created to accommodate IDP during the war), transient settlements (eg, those created to accommodate IDP returning to war-affected communities requiring rebuilding), and permanent settlements (eg, those that existed before the war and residents were never displaced). Participants reported whether they had ever been abducted (yes/no) and if they experienced sexual abuse during abduction (yes/no).
Luo versions of the Harvard Trauma Questionnaire (HTQ)21 and Hopkins Symptom Check List-25 (HSCL-25)22 administered by trained interviewers assessed exposure to trauma and mental health concerns. Scores were summed in the field and immediate referrals to mental health care through the study nurse were made for those with summed responses of ≥25 (HSCL-25) or ≥28 (HTQ), as well as those who reported feeling hopeless about the future, thoughts about ending their life, and feelings of worthlessness. Referral cutoffs were determined by Uganda-based psychologists and psychiatrists. Participants were given choice of preferred service for referral. Data were not kept on uptake of referrals to care.
Both scales have been validated for research in Northern Uganda and other war-affected countries in sub-Saharan Africa.23–28 HTQ part I includes 16 questions regarding prior traumatic life events (Experienced/Witnessed/Heard about it/No). Scores were dichotomized (<12 vs. ≥12 severe traumatic events) based on evidence demonstrating this threshold is predictive of post-traumatic stress disorder (PTSD) and depression in Northern Uganda.25 HTQ part IV includes 16 questions addressing trauma symptoms measured using a 4-point severity scale over a one-week recall period to identify symptoms indicative of probable PTSD.21 Sums of all answered items in Part IV were divided by the number of answered items; for research purposes, scores ≥2.0 were classified as meeting criteria for screening positive for PTSD.22 Two additional variables assessed in the HTQ included recently experiencing ill health without access to medical care (yes/no) and sexual assault within the context of war (yes/no). The latter included rape outside of abduction but related to war, for example, gang rape in IDP camps. The HSCL-25 identified recent suicidal ideation and symptoms indicative of recent probable depression. Again, for research purposes, the mean scores of ≥1.75 on HSCL-25 Part II were classified as meeting criteria for screening positive for recent probable depression.22 In this study, Cronbach alpha coefficient was α = 0.85 (HTQ Part IV) and α = 0.82 (HSCL-25 Part II), indicating high internal consistency.
Sexual vulnerabilities related to sexual debut included age at sexual debut (dichotomized at 16 years), age difference of first sex partner (dichotomized at 10 years), condom use at sexual debut (yes/no), and coerced sexual debut (yes/no). Recent (past year) sexual vulnerabilities included number of sexual partners (0/1/2+), condom use (not always/always), self-reported genital ulcers (yes/no), and sex for exchange (defined as receiving money, shelter, food, gifts, or alcohol for sex). Participants were asked about their age at first pregnancy (dichotomized at 16 years) and if their most recent male partner was circumcised (yes/no). Active syphilis was determined using rapid plasma reagin test and confirmatory Treponema pallidum hemagglutination test in the event of a positive screen. Active syphilis was treated with a single dose of azithromycin.
Statistical Analysis
Fisher exact tests for categorical variables and Student t test for continuous variables were used to compare distributions of study variables by HIV serostatus. Unadjusted and adjusted modified Poisson regression models29 assessed associations between HIV status, and sexual vulnerabilities, war-related trauma, and mental health variables. Multivariable logistic regression determined baseline factors associated with HIV prevalence among AGYW who have ever had sex, adjusting for study round, age, and location. A final multivariable model was obtained through stepwise model selection based on the Akaike information criterion. Only those variables significant at a P value cutoff of 0.25 in bivariable analysis were included in multivariable model selection. All analyses used R 4.2.2.30 P values of <0.05 were considered statistically significant. Relative risks (RRs) and corresponding 95% confidence intervals (CI) were calculated to measure the strength of associations. The proportion of missing data in the outcome variable was 0.9%. Among independent variables, the largest proportion of missingness was 2.4%. To capture all responses and minimize systematic bias, available case analysis was used for missing data. A previous publication investigated HIV incidence among all Cango Lyec participants.20 To further contextualize HIV among AGYW who have ever had sex, we explored the incidence rate among this subgroup of participants. HIV incidence was estimated among HIV-negative sexually active AGYW participants who had at least 1 follow-up visit between January 2011 and April 2015. The time to seroconversion was assumed to have taken place at the midpoint between the last HIV-negative test and the first HIV-positive test.
RESULTS
HIV status was available for 528 of 533 eligible participants (99.1%), constituting the study sample. AGYW included in the analysis were born between 1986 and 2002, with median year of birth being 1992 (Table 1). The median age at cessation of hostilities (2006) was 14 years (interquartile range [IQR]: 12–17). The median age at entry into the study was 20 years (IQR: 18–22), with most of the participants living in Gulu district (n = 275; 52.1%). Most participants (466; 88.4%) identified as Acholi and 380 (72.0%) identified as Roman Catholic. Only 176 (33.9%) completed secondary education. In total, 342 (66.3%) were married and 96 (18.6%) were in a polygamous marriage. Living in a youth-headed household was reported by 173 participants (33.8%), and a female-headed household by 132 participants (25.0%). Most lived in a permanent settlement (n = 294; 55.7%), compared with a displaced (n = 49; 9.3%) or transient (n = 185; 35.0%) settlement.
TABLE 1.
Baseline Characteristics Among Adolescent Girls and Young Women Younger Than 25 Years (AGYW) in the Cango Lyec Cohort (2011–2015)
| Variable | HIV Serostatus | P | ||
| Negative (N = 477) | Positive (N = 51) | Total (N = 528) | ||
| Sociodemographic characteristics | ||||
| District, % | 0.103 | |||
| Amuru | 127 (94.8) | 7 (5.2) | 134 (100.0) | |
| Gulu | 243 (88.4) | 32 (11.6) | 275 (100.0) | |
| Nwoya | 107 (89.9) | 12 (10.1) | 119 (100.0) | |
| Community, % | 0.057 | |||
| Olwal (7110) | 25 (86.2) | 4 (13.8) | 29 (100.0) | |
| Jengari (7120) | 55 (96.5) | 2 (3.5) | 57 (100.0) | |
| Torokal (7130) | 47 (97.9) | 1 (2.1) | 48 (100.0) | |
| Okwir (7210) | 19 (95.0) | 1 (5.0) | 20 (100.0) | |
| Layibi (7220) | 141 (88.1) | 19 (11.9) | 160 (100.0) | |
| Awach paibona (7230) | 39 (95.1) | 2 (4.9) | 41 (100.0) | |
| Awach trading center (7231) | 44 (81.5) | 10 (18.5) | 54 (100.0) | |
| Anaka (7320) | 71 (92.2) | 6 (7.8) | 77 (100.0) | |
| Alero (7330) | 36 (85.7) | 6 (14.3) | 42 (100.0) | |
| Age, % | 0.006 | |||
| Median (IQR) | 20.0 (18.0–22.0) | 21.0 (19.0–23.0) | 20.0 (18.0–22.0) | |
| Range | 13.0–24.0 | 16.0–24.0 | 13.0–24.0 | |
| Dichotomized age, % | 0.129 | |||
| 13–19 | 186 (93.0) | 14 (7.0) | 200 (100.0) | |
| 20–24 | 291 (88.7) | 37 (11.3) | 328 (100.0) | |
| Study round, % | 0.105 | |||
| 1 | 347 (89.9) | 39 (10.1) | 386 (100.0) | |
| 2 | 81 (88.0) | 11 (12.0) | 92 (100.0) | |
| 3 | 49 (98.0) | 1 (2.0) | 50 (100.0) | |
| Ethnicity, % | 0.820 | |||
| N-Miss | 1 | 0 | 1 | |
| Acholi | 420 (90.1) | 46 (9.9) | 466 (100.0) | |
| Other tribes | 56 (91.8) | 5 (8.2) | 61 (100.0) | |
| Highest education obtained, % | 0.157 | |||
| N-Miss | 8 | 1 | 9 | |
| Primary or less | 305 (88.9) | 38 (11.1) | 343 (100.0) | |
| Secondary or more | 164 (93.2) | 12 (6.8) | 176 (100.0) | |
| Marital status, % | 1.000 | |||
| N-Miss | 10 | 2 | 12 | |
| Not married | 158 (90.8) | 16 (9.2) | 174 (100.0) | |
| Maried | 309 (90.4) | 33 (9.6) | 342 (100.0) | |
| Polygamous marriage, % | 0.253 | |||
| N-Miss | 10 | 2 | 12 | |
| No | 383 (91.2) | 37 (8.8) | 420 (100.0) | |
| Yes | 84 (87.5) | 12 (12.5) | 96 (100.0) | |
| Religion, % | 0.247 | |||
| Roman catholic | 344 (90.5) | 36 (9.5) | 380 (100.0) | |
| Protestant | 68 (86.1) | 11 (13.9) | 79 (100.0) | |
| Other | 65 (94.2) | 4 (5.8) | 69 (100.0) | |
| Youth-headed household, % | 0.275 | |||
| No | 317 (89.3) | 38 (10.7) | 355 (100.0) | |
| Yes | 160 (92.5) | 13 (7.5) | 173 (100.0) | |
| Female-headed household, % | 0.496 | |||
| No | 360 (90.9) | 36 (9.1) | 396 (100.0) | |
| Yes | 117 (88.6) | 15 (11.4) | 132 (100.0) | |
| War-related trauma and mental health | ||||
| Community displacement status, % | 0.880 | |||
| Permanent | 267 (90.8) | 27 (9.2) | 294 (100.0) | |
| Displaced | 44 (89.8) | 5 (10.2) | 49 (100.0) | |
| Transient | 166 (89.7) | 19 (10.3) | 185 (100.0) | |
| Ever abducted, % | 0.060 | |||
| N-Miss | 1 | 0 | 1 | |
| No | 412 (91.4) | 39 (8.6) | 451 (100.0) | |
| Yes | 64 (84.2) | 12 (15.8) | 76 (100.0) | |
| Sexually abused in abduction, % | 0.157 | |||
| N-Miss | 2 | 1 | 3 | |
| Never abducted | 412 (91.4) | 39 (8.6) | 451 (100.0) | |
| No | 55 (84.6) | 10 (15.4) | 65 (100.0) | |
| Yes | 8 (88.9) | 1 (11.1) | 9 (100.0) | |
| ≥12 traumatic events, % (HTQ*) | 0.185 | |||
| No | 453 (90.8) | 46 (9.2) | 499 (100.0) | |
| Yes | 24 (82.8) | 5 (17.2) | 29 (100.0) | |
| Probable PTSD, % | 0.802 | |||
| No | 433 (90.4) | 46 (9.6) | 479 (100.0) | |
| Yes | 44 (89.8) | 5 (10.2) | 49 (100.0) | |
| Probable depression, % | 0.002 | |||
| No | 418 (92.1) | 36 (7.9) | 454 (100.0) | |
| Yes | 59 (79.7) | 15 (20.3) | 74 (100.0) | |
| Suicide ideation, % | 0.066 | |||
| N-Miss | 1 | 0 | 1 | |
| No | 406 (91.4) | 38 (8.6) | 444 (100.0) | |
| Yes | 70 (84.3) | 13 (15.7) | 83 (100.0) | |
| Rape or sexual abuse, % (HTQ*) | <0.001 | |||
| N-Miss | 2 | 0 | 2 | |
| No | 435 (92.0) | 38 (8.0) | 473 (100.0) | |
| Yes | 40 (75.5) | 13 (24.5) | 53 (100.0) | |
| Ill Health without medical care, % (HTQ*) | 0.051 | |||
| N-Miss | 2 | 0 | 2 | |
| No | 344 (92.0) | 30 (8.0) | 374 (100.0) | |
| Yes | 131 (86.2) | 21 (13.8) | 152 (100.0) | |
| Sexual vulnerabilities | ||||
| Age at sexual debut, % | 0.074 | |||
| N-Miss | 4 | 1 | 5 | |
| 16 or older | 263 (92.6) | 21 (7.4) | 284 (100.0) | |
| Younger than 16 | 210 (87.9) | 29 (12.1) | 239 (100.0) | |
| First sex partner 10 years or older, % | 1.000 | |||
| N-Miss | 41 | 10 | 51 | |
| No | 398 (91.3) | 38 (8.7) | 436 (100.0) | |
| Yes | 38 (92.7) | 3 (7.3) | 41 (100.0) | |
| Condom use at sexual debut, % | 0.456 | |||
| N-Miss | 3 | 0 | 3 | |
| No | 188 (89.1) | 23 (10.9) | 211 (100.0) | |
| Yes | 286 (91.1) | 28 (8.9) | 314 (100.0) | |
| Coerced sexual debut, % | 0.410 | |||
| N-Miss | 2 | 0 | 2 | |
| No | 405 (90.8) | 41 (9.2) | 446 (100.0) | |
| Yes | 70 (87.5) | 10 (12.5) | 80 (100.0) | |
| Age at first pregnancy, % | 0.057 | |||
| N-Miss | 96 | 6 | 102 | |
| 16 or older | 227 (91.9) | 20 (8.1) | 247 (100.0) | |
| Younger than 16 | 154 (86.0) | 25 (14.0) | 179 (100.0) | |
| Number of partners in past year, % | 0.004 | |||
| N-Miss | 2 | 0 | 2 | |
| 0 | 33 (89.2) | 4 (10.8) | 37 (100.0) | |
| 1 | 418 (91.7) | 38 (8.3) | 456 (100.0) | |
| 2+ | 24 (72.7) | 9 (27.3) | 33 (100.0) | |
| Condom use in the past year, % | 0.566 | |||
| Always | 85 (88.5) | 11 (11.5) | 96 (100.0) | |
| Not always | 392 (90.7) | 40 (9.3) | 432 (100.0) | |
| Most recent sex partner is circumcised, % | 0.115 | |||
| N-Miss | 12 | 1 | 13 | |
| No | 388 (91.3) | 37 (8.7) | 425 (100.0) | |
| Yes | 77 (85.6) | 13 (14.4) | 90 (100.0) | |
| Sex in exchange for gifts in the past year, % | 1.000 | |||
| N-Miss | 4 | 0 | 4 | |
| No | 453 (90.2) | 49 (9.8) | 502 (100.0) | |
| Yes | 20 (90.9) | 2 (9.1) | 22 (100.0) | |
| HIV and STIs, % | ||||
| Genital ulcers | 0.012 | |||
| N-Miss | 7 | 0 | 7 | |
| No | 438 (91.2) | 42 (8.8) | 480 (100.0) | |
| Yes | 32 (78.0) | 9 (22.0) | 41 (100.0) | |
| Any STI symptoms, % | 0.069 | |||
| N-Miss | 7 | 0 | 7 | |
| No | 295 (92.2) | 25 (7.8) | 320 (100.0) | |
| Yes | 175 (87.1) | 26 (12.9) | 201 (100.0) | |
| Syphilis, % | 0.001 | |||
| N-Miss | 1 | 0 | 1 | |
| No | 468 (91.2) | 45 (8.8) | 513 (100.0) | |
| Yes | 8 (57.1) | 6 (42.9) | 14 (100.0) | |
Harvard Trauma Questionnaire.
War-Related Trauma
The number of AGYW reporting experiences of war-related trauma and mental health sequelae were as follows: 76 (14.4%) reported abduction, and of these, 9 (12.2%) had experienced sexual abuse in abduction and 53 (10.1%) experienced sexual violence in the context of war. Twenty-nine (5.5%) had experienced ≥12 traumatic events, and 83 (15.7%) had thought about suicide. In addition, 49 (9.3%) screened positive for PTSD and 74 (14.0%) screened positive for depression. Frequencies of specific traumatic experiences stratified by HIV status are presented in Figure 1 and captured within the HTQ score in statistical models.
FIGURE 1.
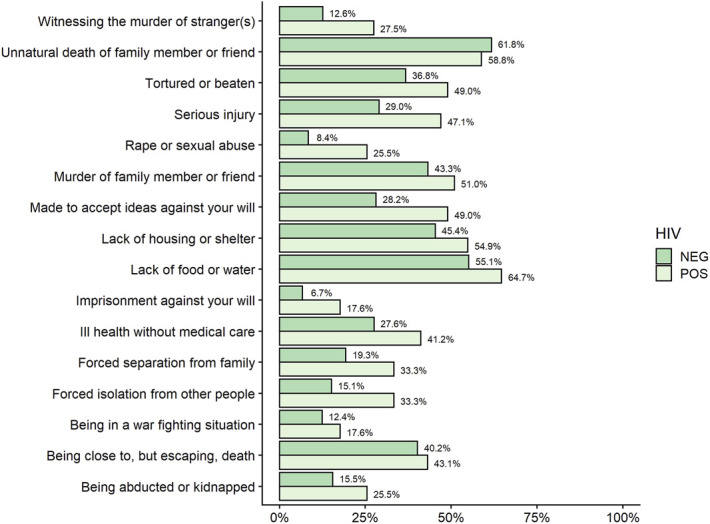
Relative frequency of trauma events experienced stratified by HIV status (positive/negative). For instance, 15.5% of HIV-negative participants reported having been abducted or kidnapped, compared with 25.5% among HIV-positive participants.
Sexual Vulnerability and Health Characteristics
At sexual debut, 239 AGYW (45.7%) were younger than 16 years, 41 (8.6%) had a sexual partner who was 10 years or older, 211 (40.2%) did not use a condom, and 80 (15.2%) experienced coerced debut. In total, 179 (42.0%) had been pregnant at an age younger than 16 years. In the past year, 33 (6.3%) had ≥2 sexual partners, 432 (81.8%) had not always used condoms, and 22 (4.2%) had transactional sex. Just 90 (17.5%) reported that their most recent partner was circumcised. In total, 41 (7.9%) reported having genital ulcers and 201 (38.6%) had STI-related symptoms in the past year. Syphilis prevalence among young women at baseline was 2.7% (n = 14).
Prevalence and Correlates of HIV Infection
In total, 51 sexually active AGYW (9.7%; 95% CI: 7.3 to 12.6) in the Cango Lyec study were living with HIV at baseline (Table 2). In comparison, the prevalence among all AGYW, regardless of sexual activity, was 6.3% (95% CI: 4.8 to 8.2). Unadjusted relationships between study variables and HIV, as well as associations adjusted for age, district of residence, and study round are summarized in Table 2. In the final multivariable model (Table 3), AGYW who had ever had sex and were living in Gulu (aRR: 2.48; 95% CI: 1.12 to 5.51) or Nwoya (aRR: 2.65; 95% CI: 1.03 to 6.83) districts were more likely than those in Amuru to be living with HIV. Older age was associated with increased risk of living with HIV (aRR: 1.14; 95% CI: 1.02 to 1.28). The likelihood of living with HIV was higher among those who experienced sexual violence in the context of war (aRR: 2.37; 95% CI: 1.21 to 4.62) and/or probable depression (aRR: 1.95; 95% CI: 1.08 to 3.54). Having self-reported genital ulcers (aRR: 1.93; 95% CI: 0.97 to 3.85) or active syphilis (aRR: 3.79; 95% CI: 2.35 to 6.12) were associated with increased risk of HIV infection among AGYW who had ever had sex.
TABLE 2.
Logistic Regression Modeling for Determinants of HIV Among Adolescent Girls and Young Women Younger Than 25 Years (AGYW) in the Cango Lyec Cohort (2011–2015)
| Variable | Units | Unadjusted | Adjusted1 | ||||
| RR | CI.95 | P | RR | CI.95 | P | ||
| Sociodemographic Characteristics | |||||||
| District | Amuru | Ref | Ref | ||||
| Gulu | 2.23 | 1.01; 4.91 | 0.047 | 2.19 | 0.97; 4.97 | 0.060 | |
| Nwoya | 1.93 | 0.79; 4.74 | 0.152 | 1.88 | 0.74; 4.77 | 0.186 | |
| Study round | 1 | Ref | Ref | ||||
| 2 | 1.18 | 0.63; 2.22 | 0.600 | 1.16 | 0.59; 2.26 | 0.666 | |
| 3 | 0.20 | 0.03; 1.41 | 0.106 | 0.21 | 0.03; 1.55 | 0.127 | |
| Age | 1.17 | 1.05; 1.31 | 0.006 | 1.17 | 1.04; 1.32 | 0.011 | |
| Ethnicity | Acholi | Ref | Ref | ||||
| Other tribes | 0.83 | 0.34; 2.01 | 0.680 | 0.79 | 0.31; 1.99 | 0.613 | |
| Highest education obtained | Primary or less | Ref | Ref | ||||
| Secondary or more | 0.62 | 0.33; 1.15 | 0.127 | 0.55 | 0.28; 1.05 | 0.070 | |
| Marital status | Not married | Ref | Ref | ||||
| Married | 1.05 | 0.59; 1.85 | 0.868 | 1.05 | 0.57; 1.93 | 0.884 | |
| Polygamous marriage | No | Ref | Ref | ||||
| Yes | 1.42 | 0.77; 2.62 | 0.263 | 1.38 | 0.71; 2.69 | 0.349 | |
| Religion | Roman catholic | Ref | Ref | ||||
| Protestant | 1.47 | 0.78; 2.76 | 0.231 | 1.34 | 0.67; 2.65 | 0.409 | |
| Other | 0.61 | 0.22; 1.66 | 0.336 | 0.51 | 0.18; 1.44 | 0.205 | |
| Youth headed household | No | Ref | Ref | ||||
| Yes | 0.70 | 0.38; 1.28 | 0.250 | 0.73 | 0.39; 1.38 | 0.330 | |
| Female headed household | No | Ref | Ref | ||||
| Yes | 1.25 | 0.71; 2.21 | 0.442 | 1.12 | 0.61; 2.05 | 0.719 | |
| War-related trauma and mental health | |||||||
| Community displacement status | Permanent | Ref | Ref | ||||
| Displaced | 1.11 | 0.45; 2.75 | 0.820 | 1.50 | 0.55; 4.10 | 0.428 | |
| Transient | 1.12 | 0.64; 1.95 | 0.694 | 1.23 | 0.68; 2.22 | 0.498 | |
| Ever abducted | No | Ref | Ref | ||||
| Yes | 1.83 | 1.00; 3.33 | 0.049 | 1.65 | 0.86; 3.16 | 0.134 | |
| ≥12 traumatic events (HTQ*) | No | Ref | Ref | ||||
| Yes | 1.87 | 0.80; 4.35 | 0.146 | 1.64 | 0.64; 4.25 | 0.306 | |
| Probable PTSD | No | Ref | Ref | ||||
| Yes | 1.06 | 0.44; 2.55 | 0.892 | 1.05 | 0.41; 2.67 | 0.920 | |
| Probable depression | No | Ref | Ref | ||||
| Yes | 2.56 | 1.47; 4.43 | <0.001 | 2.58 | 1.39; 4.79 | 0.003 | |
| Suicide ideation | No | Ref | Ref | ||||
| Yes | 1.83 | 1.02; 3.28 | 0.043 | 1.93 | 1.02; 3.64 | 0.043 | |
| Rape or sexual abuse (HTQ†) | No | Ref | Ref | ||||
| Yes | 3.05 | 1.74; 5.36 | <0.001 | 3.35 | 1.76; 6.39 | <0.001 | |
| Ill Health without medical care (HTQ*) | No | Ref | Ref | ||||
| Yes | 1.72 | 1.02; 2.91 | 0.042 | 1.73 | 0.98; 3.04 | 0.057 | |
| Sexual vulnerabilities | |||||||
| Age at sexual debut | 16+ | Ref | Ref | ||||
| <16 | 1.64 | 0.96; 2.80 | 0.069 | 1.61 | 0.91; 2.83 | 0.102 | |
| Condom use at sexual debut | No | Ref | Ref | ||||
| Yes | 0.82 | 0.48; 1.38 | 0.452 | 0.75 | 0.43; 1.31 | 0.309 | |
| Coerced sexual debut | No | Ref | Ref | ||||
| Yes | 1.36 | 0.71; 2.60 | 0.353 | 1.57 | 0.77; 3.19 | 0.213 | |
| Age at first pregnancy | 16+ | Ref | Ref | ||||
| <16 | 1.72 | 0.99; 3.01 | 0.055 | 1.82 | 1.01; 3.30 | 0.048 | |
| Number of partners in past year | 0 | Ref | Ref | ||||
| 1 | 0.77 | 0.29; 2.04 | 0.600 | 0.76 | 0.27; 2.13 | 0.598 | |
| 2+ | 2.52 | 0.86; 7.43 | 0.093 | 2.35 | 0.72; 7.64 | 0.157 | |
| Condom use in past year | Always | Ref | Ref | ||||
| Not always | 0.81 | 0.43; 1.52 | 0.507 | 0.76 | 0.39; 1.49 | 0.425 | |
| Most recent sex partner is circumcised | No | Ref | Ref | ||||
| Yes | 1.66 | 0.92; 2.99 | 0.092 | 1.55 | 0.82; 2.94 | 0.179 | |
| HIV and STIs | |||||||
| Genital ulcers | No | Ref | Ref | ||||
| Yes | 2.51 | 1.32; 4.78 | 0.005 | 2.49 | 1.21; 5.14 | 0.014 | |
| Any STI symptoms | No | Ref | Ref | ||||
| Yes | 1.66 | 0.98; 2.78 | 0.057 | 1.57 | 0.90; 2.73 | 0.109 | |
| Syphilis | No | Ref | Ref | ||||
| Yes | 4.89 | 2.51; 9.51 | <0.001 | 4.61 | 1.94; 10.94 | <0.001 | |
TABLE 3.
Final Multivariable Logistic Regression Model Obtained Through Stepwise Variable Selection*
| Variable | Units | RR | [95% CI] | P |
| District | Amuru | Ref | ||
| Gulu | 2.48 | [1.12 to 5.51] | 0.025 | |
| Nwoya | 2.65 | [1.03 to 6.83] | 0.044 | |
| Age | 1.14 | [1.02 to 1.28] | 0.021 | |
| Study round | 1 | Ref | ||
| 2 | 1.43 | [0.76 to 2.71] | 0.269 | |
| 3 | 0.25 | [0.03 to 1.86] | 0.178 | |
| Probable depression | No | Ref | ||
| Yes | 1.95 | [1.08 to 3.54] | 0.028 | |
| Rape or sexual abuse (HTQ†) | No | Ref | ||
| Yes | 2.37 | [1.21 to 4.62] | 0.011 | |
| Genital ulcers | No | Ref | ||
| Yes | 1.93 | [0.97 to 3.85] | 0.062 | |
| Syphilis | No | Ref | ||
| Yes | 3.79 | [2.35 to 6.12] | <0.001 |
District, age, and study round were included as confounders during the variable selection process.
HTQ.
HIV Incidence
HIV incidence was 8.9 per 1,000 person-years (95% CI: 3.8 to 17.5) among 463 AGYW. A total of 8 seroconversions occurred, over 900 person-years of observation, and assumed to have taken place at the midpoint between the last HIV-negative test and the first HIV-positive test. The median age of seroconversion was 20.6 (IQR: 18.4 to 21.2).
DISCUSSION
HIV Prevalence
HIV prevalence among conflict-affected AGYW aged 13–24 years who are sexually active was 9.7% (95% CI: 7.3 to 12.6) and 6.3% (95% CI: 4.8 to 8.2) overall, regardless of sexual activity. This is substantially higher than HIV prevalence of 3.3% reported among AGYW regardless of sexual activity aged 15–24 years in Uganda.5 Understanding high prevalence of HIV among AGYW postconflict requires recognition of atrocities they have endured in the context of war and its aftermath, including lack of basic necessities, witnessing and experiencing violence, and forced separation from family. It is critical that evidence-based prevention strategies, such as PrEP, and their guidelines consider these unique and high-risk contexts. Barriers in the postconflict context may also prevent AGYW living with HIV from engaging in testing and care. Estimates suggest that nearly half of AGYW living with HIV across Uganda remain undiagnosed, and more than a quarter of those on ART were not virally suppressed.5 Tailored HIV interventions for AGYW, based on postconflict realities and Acholi cultural strengths, are urgently required.
Sexual Violence–Related Harms
The likelihood of living with HIV was more than 2 times higher among AGYW who experienced sexual violence in the context of war compared with those who did not experience sexual violence in the context of war. Global evidence demonstrates that gender-based violence and inequalities continue to drive the HIV epidemic.2 In Northern Uganda, increased risk of HIV resulting from experiences of sexual violence must be understood within the legacy of war. In this study, the prevalence of having experienced sexual violence in the context of war was 10% overall and 25.5% among AGYW living with HIV. All participants were born during the war and were an average of 14 years old at cessation of hostilities. Exposure to sexual violence during the civil war—including defilement, forced marriage, forced motherhood, rape by armed forces on both sides of the conflict, and rape by other residents in IDP camps—is well-documented.11,13,31–33 Scholars have argued that heightened sexual violence against AGYW may become normalized during protracted conflict.6,34,35 Others have identified serious long-term physical and mental health consequences of war-related sexual violence among women in Northern Uganda.31,33,36 Furthermore, both sexual violence and war-related “bush” experience remain highly stigmatized, with consequences for mental health and social relationships, that may further exacerbate HIV-related risk.7,13,31,37–39 As a result, wholistic approaches responding to root causes of HIV-related vulnerability must involve AGYW in their design and development and embed support to heal from unresolved and untreated sexual violence.40
Mental Health–Related Harms
Sexually active AGYW who screened positive for probable depression were almost twice as likely to be living with HIV. Nearly 30% of AGYW who had ever had sex and were living with HIV in this study screened positive for probable depression. Although the directionality of the relationship between depression and HIV cannot be distinguished in this study, previous research from Gulu district in Northern Uganda identified depression as a mediating factor between war-related trauma and sexual risk behaviors among 551 adolescents aged 13–21years 4 years postwar.41 Mental health impacts of war-related traumas may contribute to sexual vulnerabilities such as condom-less sex, sex for exchange, and sexually transmitted infections, including HIV.37 Simultaneously, psychological, physiological, and social impacts of becoming HIV-positive may intensify mental health concerns.37 Finally, co-occurring depression and HIV may contribute to HIV disease progression and mortality through both biological and socio–behavioral pathways.42,43 These findings affirm that mental health concerns and HIV go hand-in-hand and highlight importance of wholistic models of care postconflict to support health and healing.44,45
Sexually Transmitted Infections
Self-reported genital ulcers and laboratory diagnosed active syphilis were associated with increased risk of HIV infection among AGYW. Although these associations are well-known, this finding is deeply concerning given how treatable these STIs are and extent of HIV risk when they go untreated.46,47 Responding to STIs among AGYW in Northern Uganda requires recognition of circumstances of access to care in the postconflict context, as well as Acholi norms and cultural practices related to sexual health. Previous work by our team focused on the wayo system, an Acholi socialization process involving mentoring from 3 women – the maa (mother), the wayo (paternal auntie), and the adaa (grandmother)—which provided girls an informal system of support, education, and safety as they developed into young women.48 The wayo in particular helps guide young girls through transitions to womanhood and serves as a trusted secret-keeper, mentor, and confidant.48 (Re)vitalizing these systems of sexual health education and wellbeing may be a pathway to support AGYW to engage in care for STIs and reduce HIV risk.
Sociodemographics
AGYW who had ever had sex and living in Gulu or Nwoya districts were more likely than those in Amuru to be living with HIV. HIV prevalence among AGYW who had ever had sex was 11.6% in Gulu, 10.1% in Nwoya, and 5.2% in Amuru. The war was characterized by near-total displacement (90% of the population) as civilians sought to escape. AGYW and their families were displaced from land and territory during the war, and subsequently, formal education was disrupted and traditional agricultural skills were not passed on to this generation. In total, 76% of sexually active AGYW living with HIV in this study did not exceed primary school education, contributing further to poverty and unemployment. Differences in HIV prevalence by district may reflect economic pressures that have prevented AGYW from returning to their homelands after the war, and instead remaining in urban centers, such as those found in Gulu, with limited opportunity, contributing to HIV vulnerabilities of early marriage and transactional sex.49 Despite these findings, it is important to provide trauma-informed HIV prevention in all 3 study districts as postconflict-related drivers of risk are present.
HIV Incidence
The HIV incidence among conflict-affected AGYW aged 13–24 years was 8.9 per 1000 person-years. This is substantially higher than HIV incidence of 4.6 per 1000 person-years reported among AGYW aged 15–24 years in Uganda.5 Countering these vulnerabilities in hard-to-reach populations in war-affected Northern Uganda has laid the foundation for Cango Lyec's next phase of work. HIV prevention and treatment interventions that build on community's cultural strengths to promote resiliency and health are urgently needed.
Limitations
Although efforts were made to enroll all those eligible, some were repeatedly absent or declined to participate (505/2954 = 17.1%). It is possible that those who did not participate were more mobile, which may be associated with increased risk of HIV. It is also possible that those who refused to participate did so because of known HIV-positive status. Despite these challenges, we are confident that due to our recruitment methods and rigorous eligibility criteria, our sample is representative of people residing in study communities. Common to many longitudinal cohort studies, Cango Lyec uses self-reported data (except HIV and syphilis status) so recall bias, social desirability bias, or misclassification of exposure may have occurred and led to over or underestimation of certain measures. However, we worked to mitigate this for mental health outcomes by using validated scales with shorter recall time (HTQ and HSCL-25). Owing to the cross-sectional nature of this analysis, we are unable to determine temporality of relationships between study variables and HIV infection or make causal inference. Finally, although the HTQ and HSCL-25 have been demonstrated to be both reliable and valid in this setting, they are nondiagnostic screening tools, which may lead to a conflation in levels of mental health concerns.
CONCLUSIONS
We observed substantially higher HIV prevalence among sexually active AGYW living in postconflict Northern Uganda, than among this age group in Uganda overall. Ongoing legacies of war—especially gender-based violence and trauma—contribute to HIV vulnerability among AGYW. AGYW in postconflict contexts will continue to be left behind if we fail to take note of the specific set of circumstances that contribute to HIV risk for this population. Wholistic approaches integrating HIV prevention with culturally safe mental health initiatives are urgently required in Northern Uganda in order for healing to take place. More importantly, AGYW's rights to live free from the crime of sexual violence and to undertake dignified livelihoods that provide for their needs must be upheld and respected.
ACKNOWLEDGMENTS
The authors are indebted to the study participants involved in the Cango Lyec Project. The authors are so grateful for our research team in the field for their conviction and holding us accountable to the voices of people who have survived the war in Acholiland. To Lilian Tebere, thank you so much for believing in this process, your wisdom, and for your ongoing friendship and support. To Augustine Mutumba, Margaret Nakuya, and Rehema Namaganda at Makerere University Child Health Development Center (CHDC), thank you for helping us to resolve very complex administrative issues.
Footnotes
The Cango Lyec Project was funded through a Canadian Institutes of Health Research Operating Grant (106621). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The authors have no funding or conflicts of interest to disclose.
H.M. and A.K. contributed to study conception, data collection, research design, and led manuscript development. H.M., M.D.O., and P.M.S. co-conceived the study and study design, helped draft and edit the manuscript, and interpret results. D.S.Z., S.S.M., H.M., and K.J. were responsible for statistical analysis and drafting and editing the manuscript. S.A., T.O., and A.O. contributed to data collection, management of field activities, manuscript editing, and interpretation of results. N.K.S. and M.T.S. supervised the study and protocol implementation contributed to manuscript development and interpretation of results. All authors read and approved the final submitted version of the manuscript.
Contributor Information
Herbert Muyinda, Email: muyindaherbert@hotmail.com.
Kate Jongbloed, Email: katejongbloed@gmail.com.
David S. Zamar, Email: david.zamar@bcchr.ca.
Samuel S. Malamba, Email: malambas@gmail.com.
Martin D. Ogwang, Email: dmogwang2@gmail.com.
Achilles Katamba, Email: amkatamba@gmail.com.
Alex Oneka, Email: alexoneka@gmail.com.
Stella Atim, Email: patudaonywalo@gmail.com.
Tonny O. Odongpiny, Email: tonnyodongpiny@gmail.com.
Nelson K. Sewankambo, Email: sewankam@infocom.co.ug.
Martin T. Schechter, Email: martin.schechter@ubc.ca.
Patricia M. Spittal, Email: spittal@sm.hivnet.ubc.ca.
REFERENCES
- 1.UNAIDS Ending AIDS. Progress Towards the 90-90-90 Targets. Geneva, Switzerland: Joint United Nations Programme on HIV/AIDS; 2017. [Google Scholar]
- 2.Global UNAIDS. AIDS Update—Seizing the Moment: Tackling Entrenched Inequalities to End Epidemics. Geneva, Switzerland: Joint United Nations Programme on HIV/AIDS; 2020. [Google Scholar]
- 3.Get UNAIDS. On the Fast-Track: The Life-Cycle Approach to HIV. Geneva, Switzerland: Joint United Nations Programme on HIV/AIDS; 2016. [Google Scholar]
- 4.UNAIDS. The Gap Report. Geneva, Switzerland: Joint United Nations Programme on HIV/AIDS; 2014. [Google Scholar]
- 5.Uganda Ministry of Health. Uganda Population-Based HIV Impact Assessment: Final Report. Uganda Ministry of Health; Uganda; 2019. [Google Scholar]
- 6.Patel SH. Lost in Transition: Determining HIV Prevalence and Related Vulnerabilities Among Young People Surviving Abduction and Displacement in Post-Conflict Northern Uganda. University of British Columbia; Canada; 2012. [Google Scholar]
- 7.Spitzer H, Twikirize JM. War-affected children in Northern Uganda: No easy path to normality. Int Soc Work. 2013;56:67–79. [Google Scholar]
- 8.Lunde H. Night Commuting in Gulu, Northern Uganda: From Spontaneous Strategy to New Social Institution. University of Oslo; Norway; 2006. [Google Scholar]
- 9.Thomsen TM, Bjerngaard R. Beyond night commuting. Nordic Psychol. 2008;60:87–100. [Google Scholar]
- 10.Patel SH, Muyinda H, Sewankambo NK, et al. In the face of war: examining sexual vulnerabilities of Acholi adolescent girls living in displacement camps in conflict-affected Northern Uganda. BMC Internat Health Hum Rights. 2012;12:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Westerhaus MJ, Finnegan AC, Zabulon Y, et al. Framing HIV prevention discourse to encompass the complexities of war in northern Uganda. Am J Public Health. 2007;97:1184–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Westerhaus M, Finnegan A, Zabulon Y, et al. Northern Uganda and paradigms of HIV prevention: the need for social analysis. Glob Public Health. 2008;3:39–46. [DOI] [PubMed] [Google Scholar]
- 13.Akello G. Experiences of forced mothers in northern Uganda: the legacy of war. Intervention. 2013;11:149–156. [Google Scholar]
- 14.Annan J, Blattman C, Mazurana D, et al. Civil war, reintegration, and gender in Northern Uganda. J Conflict Resolut. 2011;55:877–908. [Google Scholar]
- 15.Patel S, Schechter MT, Sewankambo NK, et al. Lost in transition: HIV prevalence and correlates of infection among young people living in post-emergency phase transit camps in Gulu District, Northern Uganda. PLoS One. 2014;9:e89786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Patel S, Schechter MT, Sewankambo NK, et al. War and HIV: sex and gender differences in risk behaviour among young men and women in post-conflict Gulu District, Northern Uganda. Glob Public Health. 2014;9:325–341. [DOI] [PubMed] [Google Scholar]
- 17.Branch A. Gulu in war and peace? The town as camp in northern Uganda. Urban Stud. 2013;50:3152–3167. [Google Scholar]
- 18.Mailer M. From Emergency to Recovery: Rescuing Northern Uganda's Transition. Oxford, United Kingdom: Oxfam International; 2008. [Google Scholar]
- 19.Malamba S, Muyinda H, Spittal P, et al. Cango Lyec—healing the Elephant: HIV related vulnerabilities of post-conflict affected populations aged 13–49 years living in three Mid-Northern Uganda districts. BMC Infect Dis. 2016;16:690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Katamba A, Ogwang D, Muyinda H, et al. Cango Lyec (healing the Elephant): HIV incidence in post-conflict northern Uganda. Lancet Eclinical Med. 2020;23:100408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shoeb M, Weinstein H, Mollica R. The Harvard trauma questionnaire: adapting a cross-cultural instrument for measuring torture, trauma and posttraumatic stress disorder in Iraqi refugees. Int J Soc Psychiat. 2007;53:447–463. [DOI] [PubMed] [Google Scholar]
- 22.Mollica RF. Measuring Trauma, Measuring Torture: Instructions and Guidance on the Utilization of the Harvard Program in Refugee Trauma's Versions of the Hopkins Symptom Checklist-25 (HSCL-25) and the Harvard Trauma Questionnaire (HTQ). Cambridge, MA: Harvard University; 2004. [Google Scholar]
- 23.Fox SH, Tang SS. The Sierra Leonean refugee experience: traumatic events and psychiatric sequelae. J Nerv Ment Dis. 2000;188:490–495. [DOI] [PubMed] [Google Scholar]
- 24.Pham PN, Weinstein HM, Longman T. Trauma and PTSD symptoms in Rwanda: implications for attitudes toward justice and reconciliation. JAMA. 2004;292:602–612. [DOI] [PubMed] [Google Scholar]
- 25.Roberts B, Ocaka KF, Browne J, et al. Factors associated with post-traumatic stress disorder and depression amongst internally displaced persons in northern Uganda. BMC Psychiat. 2008;8:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yeomans PD, Herbert JD, Forman EM. Symptom comparison across multiple solicitation methods among Burundians with traumatic event histories. J Trauma Stress. 2008;21:231–234. [DOI] [PubMed] [Google Scholar]
- 27.Roberts B, Damundu EY, Lomoro O, et al. Post-conflict mental health needs: a cross-sectional survey of trauma, depression and associated factors in Juba, Southern Sudan. BMC Psychiatry. 2009;9:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ovuga E, Oyok TO, Moro E. Post traumatic stress disorder among former child soldiers attending a rehabilitative service and primary school education in northern Uganda. Afr Health Sci. 2008;8:136–141. [PMC free article] [PubMed] [Google Scholar]
- 29.Zou G. A modified poissn regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. [DOI] [PubMed] [Google Scholar]
- 30.R Development Core Team. A Language and Environment for Statistical Computing. Vienna: R Development Core Team; 2019. [Google Scholar]
- 31.Woldetsadik MA. Long-Term Effects of Wartime Sexual Violence on Women and Families: The Case of Northern Uganda; Santa Monica, CA: The Pardee RAND Graduate School; 2018. [Google Scholar]
- 32.Apio E. Uganda's Forgotten Children of War. Born of War Protecting Children of Sexual Violence Survivors in Conflict Zones; Hartford: Kumarian Press 2007:94–109. [Google Scholar]
- 33.Kinyanda E, Musisi S, Biryabarema C, et al. War related sexual violence and it's medical and psychological consequences as seen in Kitgum, Northern Uganda: a cross-sectional study. BMC Int Health Hum Rights. 2010;10:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mock NB, Duale S, Brown LF, et al. Conflict and HIV: a framework for risk assessment to prevent HIV in conflict-affected settings in Africa. Emerging Themes Epidemiol. 2004;1:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jewkes R. Comprehensive response to rape needed in conflict settings. Lancet. 2007;369:2140–2141. [DOI] [PubMed] [Google Scholar]
- 36.Liebling-Kalifani H, Ojiambo-Ochieng R, Marshall A, et al. Violence against women in Northern Uganda: the neglected health consequences of war. J Intern Women's Stud. 2008;9:174–192. [Google Scholar]
- 37.Koegler E, Kennedy CE. A scoping review of the associations between mental health and factors related to HIV acquisition and disease progression in conflict-affected populations. Conflict Health. 2018;12:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Allen T, Atingo J, Atim D, et al. What happened to children who returned from the Lord's Resistance Army in Uganda? J Refug Stud. 2020;33:663–6832. [Google Scholar]
- 39.Amnesty International. Left to Their Own Devices: The Continued Suffering of Victims of the Conflict in Northern Uganda and the Need for Reparations. London, 2008. Contract No.: AFR 59/009/2008. [Google Scholar]
- 40.Mannell J, Willan S, Shahmanesh M, et al. Why interventions to prevent intimate partner violence and HIV have failed young women in southern Africa. J Int AIDS Soc. 2019;22:e25380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Okello J, Nakimuli-Mpungu E, Musisi S, et al. War-related trauma exposure and multiple risk behaviors among school-going adolescents in Northern Uganda: the mediating role of depression symptoms. J Affect Disord. 2013;151:715–721. [DOI] [PubMed] [Google Scholar]
- 42.Rabkin JG. HIV and depression: 2008 review and update. Curr HIV/AIDS Rep. 2008;5:163–171. [DOI] [PubMed] [Google Scholar]
- 43.Nanni MG, Caruso R, Mitchell AJ, et al. Depression in HIV infected patients: a review. Curr Psychiat Rep. 2015;17:530. [DOI] [PubMed] [Google Scholar]
- 44.Odokonyero R, Wagner G, Ngo V, et al. Giving “sadness” a name: the need for integrating depression treatment into HIV care in Uganda. J Int Assoc Prov AIDS Care (JIAPAC). 2015;14:108–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Laurenzi CA, Skeen S, Gordon S, et al. Preventing mental health conditions in adolescents living with HIV: an urgent need for evidence. J Int AIDS Soc. 2020;23:e25556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.O'Farrell N. Targeted interventions required against genital ulcers in African countries worst affected by HIV infection. Bull World Health Organ. 2001;76:569–577. [PMC free article] [PubMed] [Google Scholar]
- 47.Nelson LE, Tharao W, Husbands W, et al. The epidemiology of HIV and other sexually transmitted infections in African, Caribbean, and Black men in Toronto, Canada. BMC Infect Dis. 2019;19:294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Patel S, Spittal P, Muyinda H, et al. The Wayo Program in Northern Uganda: Building on Traditional Assets in Supporting Acholi Young Women and Girls in the Context of War and HIV. Children’s Rights and International Development: Springer; New York; 2011;195–219. [Google Scholar]
- 49.Chiang L, Howard A, Stoebenau K, et al. Sexual risk behaviors, mental health outcomes and attitudes supportive of wife-beating associated with childhood transactional sex among adolescent girls and young women: findings from the Uganda Violence against Children Survey. PLoS One. 2021;16:e0249064. [DOI] [PMC free article] [PubMed] [Google Scholar]


