Abstract
OBJECTIVES:
To characterize and compare trends in ICU admission, hospital outcomes, and resource utilization for critically ill very elderly patients (≥ 80 yr old) compared with the younger cohort (16–79 yr old).
DESIGN:
A retrospective multicenter cohort study.
SETTING:
One-hundred ninety-four ICUs contributing data to the Australian and New Zealand Intensive Care Society Centre for Outcome and Resource Evaluation Adult Patient Database between January 2006 and December 2018.
PATIENTS:
Adult (≥ 16 yr) patients admitted to Australian and New Zealand ICUs.
INTERVENTIONS:
None.
MEASUREMENTS AND MAIN RESULTS:
Very elderly patients with a mean ± sd age of 84.8 ± 3.7 years accounted for 14.8% (232,582/1,568,959) of all adult ICU admissions. They had higher comorbid disease burden and illness severity scores compared with the younger cohort. Hospital (15.4% vs 7.8%, p < 0.001) and ICU mortality (8.5% vs 5.2%, p < 0.001) were higher in the very elderly. They stayed fewer days in ICU, but longer in hospital and had more ICU readmissions. Among survivors, a lower proportion of very elderly was discharged home (65.2% vs 82.4%, p < 0.001), and a higher proportion was discharged to chronic care/nursing home facilities (20.1% vs 7.8%, p < 0.001). Although there was no change in the proportion of very elderly ICU admissions over the study period, they showed a greater decline in risk-adjusted mortality (6.3% [95% CI, 5.9%–6.7%] vs 4.0% [95% CI, 3.7%–4.2%] relative reduction per year, p < 0.001) compared with the younger cohort. The mortality of very elderly unplanned ICU admissions improved faster than the younger cohort (p < 0.001), whereas improvements in mortality among elective surgical ICU admissions were similar in both groups (p = 0.45).
CONCLUSIONS:
The proportion of ICU admissions greater than or equal to 80 years old did not change over the 13-year study period. Although their mortality was higher, they showed improved survivorship over time, especially in the unplanned ICU admission subgroup. A higher proportion of survivors were discharged to chronic care facilities.
Keywords: critically ill, elderly, intensive care unit, 80 years old and over
KEY POINTS.
Question: What are the trends and outcomes for very elderly patients (≥ 80 yr old) that require admission to the ICU?
Findings: In this retrospective multicenter cohort study from 194 ICUs, the very elderly cohort had significantly higher hospital mortality (15%) than the younger cohort (8%). However, the very elderly cohort showed a greater decline in their mortality rate (improved survivorship) over the study period than the younger cohort.
Meaning: Over 80% of the very elderly patients survived their hospital admission and the cohort showed an improved rate of survivorship over time.
The United Nations in their World Population Prospects have projected the world’s population to increase by an additional one billion people by 2030 (1). With a global increase in life expectancy, it is estimated that there will be a tripling in the number of people 80 years and above between 2019 and 2050 (1). Australia’s elderly population (65 yr and over) increased by 35% between 2009 and 2018, compared with a 10% increase for those 0–64 years old for this same period (2). It is projected that the number of Australians over 85 years old will double by 2042 (3).
The burgeoning elderly population will likely seek more healthcare resources over the next few decades. Nearly one-third of Australians 85 years old and over required admissions to hospitals in 2016–2017 (4). Patients 80 years old and above constitute a significant, but variable proportion of ICU admissions in Europe (5%–12%) and North America (20%) (5–9). In addition, the intensity of medical therapies received by elderly patients has also been increasing over recent years (8–10). ICU mortality among the elderly is independently associated with age, the severity of illness, and emergency, acute medical, and surgical admissions (6, 7, 11–13). Higher ICU (12%–21%) and hospital (24%–35%) mortality rates have been reported in the elderly patient population secondary to the more complex medical and surgical nature of admissions when compared to the younger age strata (5, 7, 14, 15).
There is conflicting evidence about the predicted ability of critical care services to meet the increased demands from the anticipated rise in the elderly population (5, 15, 16). Hence, it is imperative to understand current trends in admission and mortality among elderly patients admitted to ICUs, to allow appropriate planning and delivery of healthcare services to this vulnerable population.
This study aims to characterize and compare trends in ICU admission and hospital outcomes and resource utilization for critically ill very elderly patients (≥ 80 yr old) compared with the younger cohort (16–79 yr old) over 13 years (2006–2018). We hypothesized that there would be increasing trends in ICU admissions, higher mortality, and resource utilization for very elderly patients during the study period.
MATERIAL AND METHODS
The Australian and New Zealand Intensive Care Society (ANZICS) Centre for Outcome and Resource Evaluation (CORE) management committee provided access to the data. The Alfred Hospital Human Research Ethics Committee in Melbourne, Australia, approved the study titled “Characteristics and Outcomes of elderly patients admitted to Australian New Zealand ICUs: a retrospective cohort study” with a waiver of consent in March 2018 (project no. 130/18). All procedures were followed in accordance with the ethical standards on human experimentation and with the Helsinki Declaration of 1975, as amended in 2013.
Design, Setting, and Patient Population
A retrospective binational multicenter cohort study was performed. All ICU admissions from the ANZICS Adult Patient Database (APD) were extracted from January 1, 2006, to December 31, 2018. The ANZICS APD is a clinical quality registry collecting data from 194 adult ICUs in 191 hospitals throughout Australia and New Zealand with over 2 million patient episodes. The study included 90% of all ICUs in the region (95% [175/185] of all Australian ICUs and 65% [19/29] of all New Zealand ICUs) (details of the annual number of participating ICUs during the study period are provided in Supplementary Table 1, http://links.lww.com/CCM/H352). All tertiary hospitals in Australia and New Zealand were represented in the study.
We included index admissions to ICU during a unique hospitalization episode for analysis. We excluded patients less than 16 years old, patients without a documented hospital outcome, patients transferred to another ICU whose eventual outcomes were unknown, and admissions for palliative care or organ donation. To avoid duplication of mortality outcomes, readmission episodes to the ICU were excluded. Trends over time and mortality outcomes were further examined in two subgroups: planned admissions to ICU following elective surgery and all other unplanned ICU admissions (i.e., medical and emergency surgical patients). We defined the very elderly cohort as patients greater than or equal to 80 years old at the time of admission to the ICU.
Data Extraction
The following deidentified data were extracted: demographic information, source of hospital and ICU admission, diagnosis, presence of treatment limitations at the time of ICU admission, comorbidities, highest and lowest physiological and laboratory variables from the first 24 hours of ICU admission, ICU and hospital length of stay (LOS) in days, outcomes at ICU and hospital discharge. The severity of illness indices extracted included Acute Physiology and Chronic Health Evaluation (APACHE) II and III scores. The Australian and New Zealand Risk of Death (ANZROD) was extracted for every patient. ANZROD is a locally derived mortality prediction model, which includes age, diagnosis, acute physiological disturbance, chronic comorbidities, and the presence of treatment limitations and employs separate regression equations for each major diagnostic group. It provides accurate mortality prediction for ICU patients and is well-calibrated and highly discriminatory with an area under the receiver-operating characteristic greater than 0.9 when applied to the overall ICU population in Australia and New Zealand (17). Data on treatment limitations at the time of ICU admission were only mandatory from 2010. Frailty screening data (via the Clinical Frailty Scale) were excluded as collection commenced only in 2017.
Outcomes
The primary outcome measure was hospital mortality. Secondary outcome measures included 1) ICU mortality; 2) resource utilization assessed as ICU and hospital LOS; 3) the proportion of patients who had one or more readmission to ICU during the same hospitalization; and 4) discharge destination in survivors (home/rehabilitation/chronic care/nursing homes).
Statistical Analysis
Data on age and outcome were missing for 0.5% of eligible patients (7,713/1,576,672) who were excluded from the study. Comparisons between groups were performed using χ2 tests for proportions, Student t tests for normally distributed data, and Wilcoxon rank sum tests otherwise, with results reported as n with percentages, mean ± sd, or median (interquartile range [IQR]), respectively. LOS was reported as both mean and median to indicate resource impact, with overall proportional resource utilization calculated as the sum of total days in ICU or hospital used by each cohort. Of analyzed patients, 99.2% (1,556,939/1,568,959) had complete data for inclusion in the primary multivariable analysis. All multivariable analyses were adjusted for geographic regions, sex, hospital type, and severity of illness estimated using the ANZROD model, with patients clustered by site and sites treated as a random effect. Data were analyzed using time as a continuous variable and including an interaction term with age over 80 to test the significance of the difference in trends between age groups. To test the robustness of the findings, further sensitivity analyses were undertaken by repeating the above models after substituting the overall ANZROD score with individual component values and with the age subscore replaced as a categorical value representing age above or below 80 years. Models assessing discharge destination in survivors were further adjusted for LOS in ICU. Results were reported as odds ratio and 95% CI. Area under the receiver-operating characteristic and Brier score were used to assess performance of multivariable models. Annualized marginal risk-adjusted probabilities were used to graphically display changes in outcomes over time. Analyses were undertaken using Stata version 16.1 (Stata Corp. College Station, TX) and SAS version 9.4 (SAS Institute Inc., Cary). A two-sided p value of less than 0.01 was used to indicate statistical significance.
RESULTS
Demographics
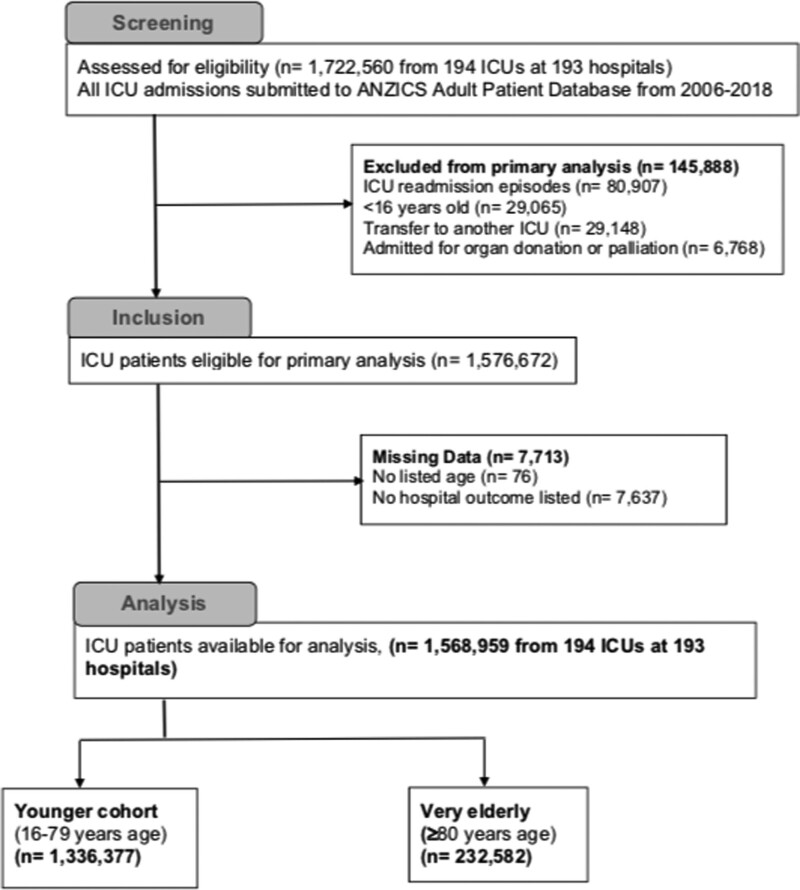
The very elderly cohort (≥ 80 yr old) accounted for 14.8% (n = 232,582) of 1,568,959 eligible admissions (Fig. 1) from 194 Australian and New Zealand ICUs during the 13-year study period (characteristics of participating ICUs in Supplementary Table 1, http://links.lww.com/CCM/H352). Summary of patient demographics and baseline characteristics is shown in Table 1. There was an overall high proportion of surgical patients. There was also a male preponderance across the entire study population, but it was comparatively less in the very elderly cohort. The very elderly cohort had a higher comorbid disease burden and a higher rate of admission from nursing homes/chronic care facilities (2.5% vs 0.8%, p < 0.001). ICU preadmission and severity of illness characteristics and scores are shown in Table 2. The very elderly cohort had a longer stay in the hospital before their ICU admission. A higher proportion of the very elderly cohort had treatment limitations on ICU admission (10.9% vs 2.9%, p < 0.001), and fewer were mechanically ventilated in the first 24 hours of their ICU admission (28.9% vs 37.9%, p < 0.001). They also had higher illness severity scores and a higher predicted risk of death using APACHE III and ANZROD models.
Figure 1.
Consort diagram. ANZROD = Australian and New Zealand Risk of Death.
TABLE 1.
Baseline Patient Characteristics
| Total Patient Cohort | < 80 Yr | ≥ 80 Yr | |
|---|---|---|---|
| Characteristics | n = 1,568,959 | n = 1,336,377 | n = 232,582 |
| Age, mean (sd) | 61.7 (17.9) | 57.6 (16.3) | 84.8 (3.7) |
| Male | 903,704 (57.6%) | 779,857 (58.4%) | 123,847 (53.3%) |
| Any comorbid disease | 389,612 (24.8%) | 321,769 (24.1%) | 67,843 (29.2%) |
| ≥ 2 chronic comorbidities | 112,255 (7.2%) | 94,495 (7.1%) | 17,760 (7.6%) |
| Chronic cardiovascular | 141,424 (9.0%) | 103,524 (7.7%) | 37,900 (16.3%) |
| Chronic respiratory | 112,040 (7.1%) | 91,794 (6.9%) | 20,246 (8.7%) |
| Chronic kidney disease | 50,300 (3.2%) | 40,226 (3.0%) | 10,074 (4.3%) |
| Chronic liver disease | 25,389 (1.6%) | 24,609 (1.8%) | 780 (0.3%) |
| Source of admission to hospital | |||
| Home | 1,197,407 (76.3%) | 1,018,340 (76.2%) | 179,067 (77.0%) |
| Nursing home/chronic care/rehabilitation | 16,984 (1.1%) | 11,187 (0.8%) | 5,797 (2.5%) |
| Other acute hospitals | 256,276 (16.3%) | 220,529 (16.5%) | 35,747 (15.4%) |
| ICU in another hospital | 14,076 (0.9%) | 12,745 (1.0%) | 1,331 (0.6%) |
| Other/unknown | 84,216 (5.4%) | 73,576 (5.5%) | 10,640 (4.6%) |
| Source of admission to ICU | |||
| Operating theatre | 841,309 (53.6%) | 711,685 (53.3%) | 129,624 (55.7%) |
| Emergency department | 411,973 (26.3%) | 360,814 (27.0%) | 51,159 (22.0%) |
| General ward | 206,156 (13.1%) | 166,319 (12.4%) | 39,837 (17.1%) |
| Other hospitals | 104,378 (6.7%) | 93,071 (7.0%) | 11,307 (4.9%) |
| Other sources of admission | 5,143 (0.3%) | 4,488 (0.3%) | 655 (0.3%) |
| Planned admission to ICU after elective surgery | 687,123 (44.1%) | 585,899 (44.1%) | 101,224 (43.7%) |
| Admission following medical emergency call | 128,200 (9.7%) | 102,492 (9.1%) | 25,708 (12.9%) |
| Medical cause of ICU admission | 711,349 (45.3%) | 611,646 (45.8%) | 99,703 (42.9%) |
| ICU admission diagnosis category | |||
| Cardiovascular | 196,562 (12.5%) | 155,342 (11.6%) | 41,220 (17.7%) |
| Cardiac (coronary artery and/or valve) surgery | 205,892 (13.1%) | 181,141 (13.6%) | 24,751 (10.6%) |
| Gastrointestinal | 260,115 (16.6%) | 207,381 (15.5%) | 52,734 (22.7%) |
| Neurological | 186,337 (11.9%) | 168,446 (12.6%) | 17,891 (7.7%) |
| Respiratory | 234,649 (15.0%) | 203,890 (15.3%) | 30,759 (13.2%) |
| Sepsis | 100,510 (6.4%) | 83,814 (6.3%) | 16,696 (7.2%) |
| Trauma | 76,315 (4.9%) | 68,546 (5.1%) | 7,769 (3.3%) |
| Other | 308,579 (19.7%) | 267,817 (20.0%) | 40,762 (17.5%) |
All values are reported as n (%) unless otherwise stated.
TABLE 2.
Severity of Illness
| Total Patient Cohort | < 80 Yr | ≥ 80 Yr | |
|---|---|---|---|
| Variables | n = 1,568,959 | n = 1,336,377 | n = 232,582 |
| Hours in hospital pre-ICU admissiona, median (IQR) | 10.2 (4.5–29.5) | 9.6 (4.3–28.2) | 18.2 (5.9–49.0) |
| Cardiac arrest in 24 hr before ICU admissionb, n (%) | 41,647 (2.9%) | 35,438 (2.8%) | 6,209 (2.9%) |
| Treatment limitations, n (%) | 64,223 (4.1%) | 38,789 (2.9%) | 25,434 (10.9%) |
| Mechanical ventilation day 1 ICU, n (%) | 573,290 (36.5%) | 506,109 (37.9%) | 67,181 (28.9%) |
| APACHE II score, mean (sd) | 15.3 (7.8) | 14.8 (7.8) | 18.1 (7.2) |
| APACHE III score, mean (sd) | 52.6 (25.9) | 50.5 (25.7) | 64.9 (23.5) |
| APACHE III score (without age), mean (sd) | 42.1 (24.3) | 41.6 (24.5) | 45.0 (23.2) |
| APACHE III risk of death, mean, median (IQR) % | 13.6, 4.9 (1.7–15.3) | 12.4, 4 (1.4–12.9) | 20.5, 11.8 (5.2–27) |
| ANZROD, mean, median (IQR) % | 8.3, 1.7 (0.5–7) | 7.4, 1.4 (0.5–5.7) | 13.4, 5 (1.7–15.7) |
| ANZROD (without age), mean, median (IQR) % | 8.9, 2 (0.7–8.1) | 8.5, 1.8 (0.6–7.3) | 11.2, 3.9 (1.3–12.3) |
APACHE = Acute Physiology and Chronic Health Evaluation, ANZROD = Australian and New Zealand Risk of Death, IQR = interquartile range.
Hours in hospital pre-ICU admission was calculated as the difference between hospital and ICU admission times for all patients.
All p values for comparisons < 0.001 except for cardiac arrest
p = 0.85.
Admission Trends
Although there was a progressive increase in the number of patients and ICUs reported to the registry over the study period, there was no change in the overall proportion who were very elderly (p = 0.55; Supplementary Table 2, http://links.lww.com/CCM/H352). Within the very elderly cohort, an increase in admissions was seen in those over 90 years, from 7% to 13% (Supplementary Fig. 1, http://links.lww.com/CCM/H352). In contrast, there was a reduction in the 80–84 age group from 64% to 56% (p < 0.001).
Outcomes
Primary Outcome
Hospital mortality (15.4% vs 7.8%, p < 0.001) was higher in the very elderly cohort (Table 3). Hospital mortality was associated with male gender, age greater than or equal to 80 years, and a high ANZROD (multivariable model in Supplementary Table 3, http://links.lww.com/CCM/H352).
TABLE 3.
Outcomes
| Total Patient Cohort | < 80 Yr | ≥ 80 Yr | |
|---|---|---|---|
| Outcomes | n = 1,568,959 | n = 1,336,377 | n = 232,582 |
| Primary outcome—hospital mortality | |||
| Hospital mortality, n (%) | 140,032 (8.9%) | 104,295 (7.8%) | 35,737 (15.4%) |
| Secondary outcomes | |||
| ICU mortality, n (%) | 89,487 (5.7%) | 69,824 (5.2%) | 19,663 (8.5%) |
| Resource utilization | |||
| ICU LOS, mean (sd), d | 3.1 (5.6) | 3.2 (5.8) | 2.9 (4.6) |
| ICU LOS, median (IQR), d | 1.8 (0.9–3.3) | 1.7 (0.9–3.2) | 1.8 (0.9–3.5) |
| Sum total ICU days (% of total) | 4,921,773 (100%) | 4,239,733 (86.1%) | 682,040 (13.9%) |
| Hospital LOS, mean (sd), d | 15.1 (70.5) | 14.8 (71.9) | 16.4 (61.8) |
| Hospital LOS, median (IQR) | 8.4 (4.7–15.4) | 8.0 (4.4–14.8) | 10.5 (6.2–18.3) |
| Sum total hospital days (% of total) | 23,313,261 (100%) | 19,552,478 (83.9%) | 3,760,775 (16.1%) |
| ICU readmissions, n (%) | 69,330 (4.4%) | 58,494 (4.4%) | 10,836 (4.7%) |
| Discharge destination (survivors only)a | |||
| Home | 1,143,708 (80.0%) | 1,015,323 (82.4%) | 128,385 (65.2%) |
| Nursing home/chronic care/rehabilitation | 135,482 (9.5%) | 95,907 (7.8%) | 39,575 (20.1%) |
| Discharge to another acute hospital | 148,054 (10.4%) | 119,321 (9.7%) | 28,733 (14.6%) |
| Other/unknown | 1,683 (0.1%) | 1,531 (0.1%) | 152 (0.1%) |
IQR = interquartile range, LOS = length of stay.
Discharge destination is reported as a proportion of 1,428,927 patients who survived to leave hospital alive (1,232,082 < 80 yr old and 196,845 ≥ 80 yr old).
All p values for comparisons less than 0.001.
Trends in Mortality
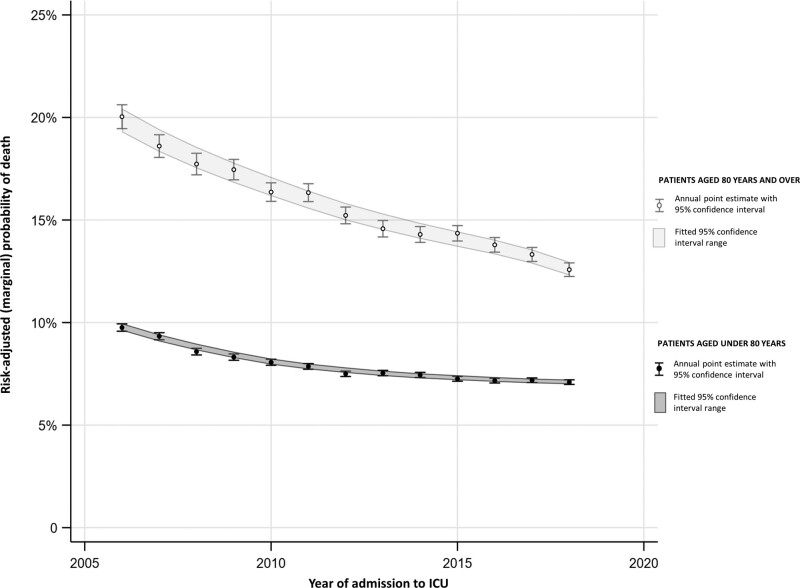
There was a progressive decline in both unadjusted and adjusted hospital mortality in both age cohorts over the study period, with mortality in the very elderly cohort decreasing from 20.4% in 2006 to 12.2% in 2018 (change in raw mortality rate over time is shown in Supplementary Fig. 2, http://links.lww.com/CCM/H352). The reduction in risk-adjusted mortality in the very elderly cohort was equivalent to 6.3% (95% CI, 5.9%–6.7%) relative reduction per year compared with 4.0% (95% CI, 3.7%–4.2%) relative reduction per year for the younger cohort (p < 0.001) (Fig. 2 depicts the risk-adjusted mortality change over time). The reduction in mortality in planned admissions to ICU after elective surgery (all ages) was equivalent to 5.4% (95% CI, 4.8%–6.1%) relative reduction per year and was not different between under and over the 80s (p = 0.45). However, among those admitted to ICU as an unplanned admission, there was a greater reduction in mortality in the very elderly, equivalent to 6.5% (95% CI, 6.0%–6.9%) relative reduction per year compared with 4.0% (95% CI, 3.7%–4.2%) relative reduction per year for the under 80 years group (p < 0.001). Summary of multivariable models examining adjusted mortality trends is shown in Supplementary Table 4 (http://links.lww.com/CCM/H352).
Figure 2.
Mortality risk change over time. The figure represents predicted (marginal) mortality risk from a regression model (date of ICU admission as a continuous variable, reported as a change in odds of death per year, with an interaction term to test difference between those above or below 80 yr old); with fitted 95% CI, alongside aggregated annual mortality risk for each year. p value for difference in slopes between groups < 0.001.
Secondary Outcome (ICU Mortality, Length of Stay, and Readmission)
ICU mortality (8.5% vs 5.2%, p < 0.001) was higher in the very elderly cohort (secondary outcomes are shown in Table 3). ICU LOS was lower with increased ICU readmission rates and a higher hospital LOS. The very elderly cohort (who represented 14.8% of admissions) occupied 13.9% of the sum total of ICU days and 16.1% of the sum total of hospital days over the entire study period. Over the study period, there was no overall change in the proportion of sum total ICU days, p = 0.045 (Supplementary Fig. 3, http://links.lww.com/CCM/H352), or hospital days occupied by the very elderly, p = 0.59 (Supplementary Fig. 4, http://links.lww.com/CCM/H352) when compared with the younger cohort. Very elderly patients were more commonly readmitted to the ICU (4.7% vs 4.4%, p < 0.001).
Secondary Outcome (Discharge Destination)
The proportion of survivors discharged home was lower in the very elderly (65.2% vs 82.4%, p < 0.001) (Table 3). There was a progressive decline in rates of home discharges from the hospital in both cohorts. The very elderly survivors were half as likely to be discharged home than the younger cohort (Supplementary Fig. 5, http://links.lww.com/CCM/H352). Among the very elderly cohort, the adjusted odds of being discharged home were associated with male gender, lower ANZROD, shorter ICU LOS, and absence of mechanical ventilation on day 1 (multivariable models in Supplementary Tables 5 and 6, http://links.lww.com/CCM/H352).
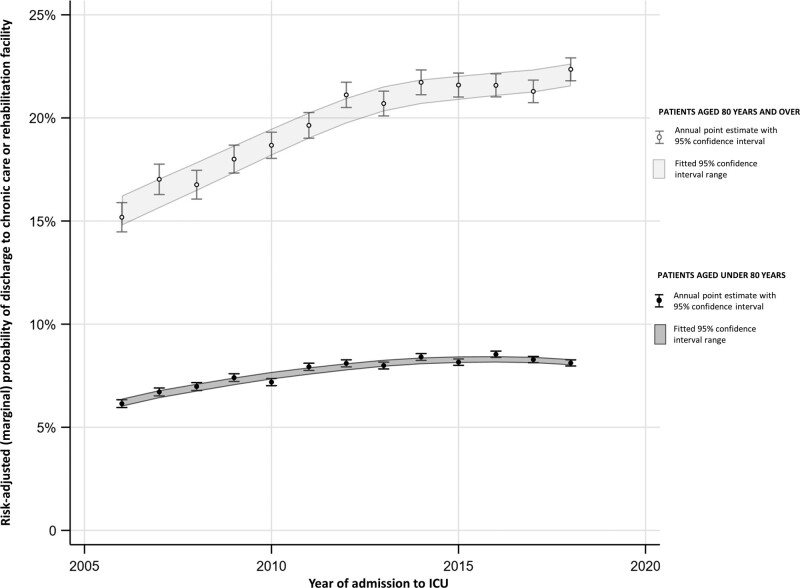
Comparatively, the very elderly survivors had higher rates of new discharges to subacute or chronic care/nursing home facilities (20.1% vs 7.8%, p < 0.001) (Table 3). On multivariable analyses, the very elderly survivors were more likely to be discharged to a subacute or a chronic care facility. Among the very elderly survivors, the adjusted odds of discharge to chronic care/rehabilitation facilities was less likely among males, but more likely in those with a higher risk of death (ANZROD) and longer ICU LOS (multivariable models in Supplementary Tables 7 and 8, http://links.lww.com/CCM/H352). The rate of new subacute or chronic care discharge increased from 15% in 2006 to 22% in 2018 for the very elderly survivors. Although increasing discharges to a chronic care facility were seen in both cohorts, the trend was greater for the very elderly, p < 0.001 (trends in discharge to chronic care facilities are shown in Fig. 3).
Figure 3.
New discharges to chronic care/nursing homes among survivors over time. The figure represents predicted (marginal) risk of new discharge to chronic care or rehabilitation from a regression model (date of ICU admission as a continuous variable, reported as a change in odds of new discharges per year, with an interaction term to test difference between those above or below 80 yr old) with fitted 95% CI, alongside aggregated annual mortality risk for each year. p value for difference in slopes between groups < 0.001.
DISCUSSION
In this retrospective multicentre database study, the very elderly cohort accounted for a sizeable but stable proportion of ICU admissions. The very elderly ICU patients had a higher comorbid burden, higher treatment limitations on admission to ICU, and used more healthcare resources. The very elderly cohort demonstrated improved survivorship over the 13 years, especially in the unplanned ICU admission subgroup. Very elderly survivors often required ongoing care and rehabilitation after discharge from the hospital.
The proportion of the very elderly patients admitted to the ICU in our study is higher than previously published local and international data over the last decade (7, 15, 16, 18), with some similarities to recent Australian data (19). This variation may be due to the large multicentre dataset in our study and the time of the studies. Despite population projections showing a higher rate of increase in the elderly population, our study shows a proportionate rise in the overall very elderly ICU admissions, when compared to the younger cohort. Our results could signify that the previously projected increase in demand for intensive care services (15) for very elderly patients may be plateauing (18, 20, 21). Our study also showed increasing trends in the admission of nonagenarians to the study ICUs. The nonagenarian ICU population is of keen interest to researchers; with recent publications refuting the age-old belief that chronological age was an independent factor for ICU and hospital mortality in this population (22–24). However, the long-term mortality for nonagenarian ICU survivors remains high (24, 25).
The hospital and ICU mortality among the very elderly cohort in our study is similar to other published data (7). However, there is significant variation in the literature, with our data showing lower hospital mortality when compared with recently published data for the elderly ICU population (26, 27). A recent systematic review was unable to explain the variation in mortality for the elderly ICU population across continents (America and Europe) based on study design or geographical location (27). This may be due to differences in age cutoffs for the very elderly or the “older” population in literature (75/80/85/90 yr) (24, 26–28) or variations in the threshold for admission to ICU for elderly patients (28) or case-mix (for example, there were fewer medical patients in our study compared to recent registry data from the UK) (27). It is also possible that there may be a higher use of intensive care at the end of life in other studies (29, 30). Pre-existing frailty likely plays a significant additional role in the higher mortality in the very elderly cohort (31, 32). A smaller proportion of the very elderly cohort in our study had treatment limitations established at the time of ICU admission (11%) when compared to other studies (33, 34). This may imply a better triage and referral system or simply that several discussions on treatment limitations happen after a trial of admission to the ICU in Australia and New Zealand.
Although both cohorts showed a declining mortality trend, this was greater in the very elderly cohort in our study. Improving mortality trends after critical illness have also been noted in numerous other studies (35–37). Our study population included a reasonable proportion of elective surgical patients. Overall mortality for surgical patients has been improving (38) and has previously been shown to be lower than that of medical patients (39, 40). We analyzed data to assess the effect of the elective surgical subgroup on mortality rates. The risk-adjusted rate of mortality decline in the elective surgical subgroup in our study was not different between those above and below 80 years old. Moreover, the decline in mortality rate was higher in patients who had unplanned admissions to ICU. It is plausible that the reasons for greater trends in improved survival in the unplanned ICU admission subgroup could be attributed to improved quality of primary, and emergency specialty care over the years. Again, this could also indicate active screening and triage to admit older patients who are most likely to benefit from a stay in intensive care. Interestingly, systematic triage and improved access to ICU admission for elderly patients did not appear to confer a mortality advantage in a randomized controlled trial setting in France (41). However, the French study had a low recruitment rate in the control group and a third of the recommended ICU admissions in the intervention group were refused by physicians. This implies that a decision to admit an elderly patient to intensive care may be complex and selection and survivor bias may play a role.
Temporal changes in decreasing rates of home discharge and increasing new admissions to chronic care or nursing homes would suggest that while survival in the very elderly has improved, it may be at a cost. Our results indicate that one in five of the very elderly survivors was discharged to a subacute rehabilitation or a chronic care/nursing home facility after a critical care admission. Unsurprisingly, survivors at higher risk of death, increased ICU LOS, and those mechanically ventilated within 24 hours of ICU admission were more likely to be discharged to ongoing health services for rehabilitation or long-term residential care. Although we did not have specific prehospital or posthospital frailty data available for the study, an association of pre-existing frailty with new admissions to chronic care or nursing home has been published for the 2017–2018 cohort from this database (42). More recently, although analysis of this dataset has demonstrated that even younger patients (< 50 yr old) with frailty experience increased new admissions to chronic care/nursing homes, this effect is greatly magnified with age (32).
Strengths and Limitations
A major limitation of our study was the absence of information on long-term trajectories (mortality, functional and cognitive outcomes, quality of life, and healthcare resource utilization) of the very elderly population, due to the nature of the database. Long-term outcomes for the very elderly admitted to the ICU may be significantly worse than what our study reveals (43–45). In addition, the database is unable to differentiate discharge destinations between rehabilitation and chronic care/nursing homes. There are several other limitations to our study, which include the observational nature of the data, lack of information about longitudinal organ support offered during the ICU stay, and absence of data related to frailty at the time of the study. The setting and local national practices may have had a large impact on the results observed and these may not translate to other regions where ICU availability may be different. Despite these, the large multicentre, binational database with a timeline of data spread over 13 years, offers a unique perspective for observation of trends for healthcare resource planning. In addition, there is value in documenting and understanding the prepandemic trends, so we can truly understand the effect of the COVID-19 pandemic on the very elderly, an area of upcoming research.
Implications
Our key finding of increasing survivorship in the very elderly patient cohort has significant implications for all healthcare systems. With a projected increase in the population, optimal healthcare resource planning should account for the burden of survivorship and the increased need for postacute care rehabilitation in the older population. More importantly, there is an urgent need to research prehospital factors that influence outcomes and understand long-term trajectories to ensure a good quality of life for the vulnerable elderly population.
CONCLUSIONS
The proportion of ICU admissions who were very elderly did not change over the 13-year study period. The very elderly cohort had more comorbidities, had higher acute illness severity, and stayed longer in hospital. Although their mortality was higher, over 80% of the very elderly patients survived their hospital admission, but a higher proportion was discharged to chronic care facilities. The very elderly cohort showed an improved rate of survivorship over time, especially in the unplanned ICU admission subgroup.
ACKNOWLEDGMENTS
We acknowledge the Australia New Zealand Intensive Care Society (ANZICS) Centre for Outcomes and Resource Evaluation (CORE) for providing the data used in the current study. The authors and the ANZICS CORE management committee thank clinicians, data collectors, research coordinators, and researchers at all the contributing sites (detailed list of sites in online supplementary material, http://links.lww.com/CCM/H352).
Supplementary Material
Footnotes
*See also p. 1437.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccmjournal).
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccmjournal).
Dr. Haines’ institution received funding from the Society of Critical Care Medicine. Dr. van Haren’s institution received funding from the Australian National University; he received funding from Phico Therapeutics and Fresenius Kabi. The remaining authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.United Nations, Department of Economic and Social Affairs, Population Division: World Population Prospects 2019. Ten Key Findings, 2019 [Google Scholar]
- 2.Australian Bureau of Statistics: Disability, Ageing and Carers, Australia: Summary of Findings. 2018. Available at: https://www.abs.gov.au/statistics/health/disability/disability-ageing-and-carers-australia-summaryfindings/latest-release#older-people. Accessed March 6, 2022
- 3.Australian Bureau of Statistics: Population Projections Australia. 2018. Available at: https://www.abs.gov.au/statistics/people/population/population-projectionsaustralia/2017-base-2066. Accessed Februrary 19, 2021
- 4.Australian Bureau of Statistics: Patient Experiences in Australia: Summary of Findings, 2016-17, 2017. Available at: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/4839.0~2016-17~Main%20Features~Hospital%20admissions%20and%20emergency%20department%20visits~5. Accessed March 6, 2022
- 5.Reinikainen M, Uusaro A, Niskanen M, et al. : Intensive care of the elderly in Finland. Acta Anaesthesiol Scand 2007; 51:522–529 [DOI] [PubMed] [Google Scholar]
- 6.Ryan D CN, Phelan D, Marsh B: The very elderly in intensive care: admission characteristics and mortality. Crit Care Resusc 2008; 10:106–110 [PubMed] [Google Scholar]
- 7.Nielsson MS, Christiansen CF, Johansen MB, et al. : Mortality in elderly ICU patients: a cohort study. Acta Anaesthesiol Scand 2014; 58:19–26 [DOI] [PubMed] [Google Scholar]
- 8.Sjoding MW, Prescott HC, Wunsch H, et al. : Longitudinal changes in ICU admissions among elderly patients in the United States. Crit Care Med 2016; 44:1353–1360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Flaatten H, de Lange DW, Artigas A, et al. : The status of intensive care medicine research and a future agenda for very old patients in the ICU. Intensive Care Med 2017; 43:1319–1328 [DOI] [PubMed] [Google Scholar]
- 10.Lerolle N, Trinquart L, Bornstain C, et al. : Increased intensity of treatment and decreased mortality in elderly patients in an intensive care unit over a decade. Crit Care Med 2010; 38:59–64 [DOI] [PubMed] [Google Scholar]
- 11.Boumendil A, Maury E, Reinhard I, et al. : Prognosis of patients aged 80 years and over admitted in medical intensive care unit. Intensive Care Med 2004; 30:647–654 [DOI] [PubMed] [Google Scholar]
- 12.de Rooij SE, Abu-Hanna A, Levi M, et al. : Factors that predict outcome of intensive care treatment in very elderly patients: a review. Crit Care 2005; 9:R307–R314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lown DJ, Knott J, Rechnitzer T, et al. : Predicting short-term and long-term mortality in elderly emergency patients admitted for intensive care. Crit Care Resusc 2013; 15:49. [PubMed] [Google Scholar]
- 14.Fuchs L, Chronaki CE, Park S, et al. : ICU admission characteristics and mortality rates among elderly and very elderly patients. Intensive Care Med 2012; 38:1654–1661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bagshaw SM, Webb SA, Delaney A, et al. : Very old patients admitted to intensive care in Australia and New Zealand: A multi-centre cohort analysis. Crit Care 2009; 13:R45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Duke GJ, Barker A, Knott CI, et al. : Outcomes of older people receiving intensive care in Victoria. Med J Aust 2014; 200:323–326 [DOI] [PubMed] [Google Scholar]
- 17.Paul E, Bailey M, Pilcher D: Risk prediction of hospital mortality for adult patients admitted to Australian and New Zealand intensive care units: development and validation of the Australian and New Zealand Risk of Death model. J Crit Care 2013; 28:935–941 [DOI] [PubMed] [Google Scholar]
- 18.Haas LE, Karakus A, Holman R, et al. : Trends in hospital and intensive care admissions in the Netherlands attributable to the very elderly in an ageing population. Crit Care 2015; 19:353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Athari F, Hillman KM, Frost SA: The changing nature of the population of intensive-care patients. J Hosp Adm 2018; 7:1 [Google Scholar]
- 20.Fuchs L, Novack V, McLennan S, et al. : Trends in severity of illness on ICU admission and mortality among the elderly. PLoS One 2014; 9:e93234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weissman GE, Kerlin MP, Yuan Y, et al. : Population trends in intensive care unit admissions in the United States among medicare beneficiaries, 2006-2015. Ann Intern Med 2019; 170:213–215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Becker S, Muller J, de Heer G, et al. : Clinical characteristics and outcome of very elderly patients >/=90 years in intensive care: a retrospective observational study. Ann Intensive Care 2015; 5:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sim YS, Jung H, Shin TR, et al. : Mortality and outcomes in very elderly patients 90 years of age or older admitted to the ICU. Respir Care 2015; 60:347–355 [DOI] [PubMed] [Google Scholar]
- 24.Le Borgne P, Maestraggi Q, Couraud S, et al. : Critically ill elderly patients (>/= 90 years): Clinical characteristics, outcome and financial implications. PLoS One 2018; 13:e0198360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Haas LEM, Bakhshi-Raiez F, van Dijk D, et al. : Outcomes of intensive care patients older than 90 years: An 11-year National Observational Study. J Am Geriatr Soc 2020; 68:1842–1846 [DOI] [PubMed] [Google Scholar]
- 26.Vallet H, Schwarz GL, Flaatten H, et al. : Mortality of older patients admitted to an ICU: A systematic review. Crit Care Med 2021; 49:324–334 [DOI] [PubMed] [Google Scholar]
- 27.Jones A, Toft-Petersen AP, Shankar-Hari M, et al. : Demographic shifts, case mix, activity, and outcome for elderly patients admitted to adult general ICUs in England, Wales, and Northern Ireland. Crit Care Med 2020; 48:466–474 [DOI] [PubMed] [Google Scholar]
- 28.Hill A, Heyland DK, Rossaint R, et al. : Longitudinal outcomes in octogenarian critically ill patients with a focus on frailty and cardiac surgery. J Clin Med 2020; 10:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Angus DC, Barnato AE, Linde-Zwirble WT, et al. ; Robert Wood Johnson Foundation ICU End-Of-Life Peer Group: Use of intensive care at the end of life in the United States: An epidemiologic study*. Crit Care Med 2004; 32:638–643 [DOI] [PubMed] [Google Scholar]
- 30.Chaudhuri D, Tanuseputro P, Herritt B, et al. : Critical care at the end of life: A population-level cohort study of cost and outcomes. Crit Care 2017; 21:124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hill AD, Fowler RA, Wunsch H, et al. : Frailty and long-term outcomes following critical illness: A population-level cohort study. J Crit Care 2020; 62:94–100 [DOI] [PubMed] [Google Scholar]
- 32.Darvall JN, Bellomo R, Paul E, et al. : Routine frailty screening in critical illness: A Population-Based Cohort Study in Australia and New Zealand. Chest 2021; 160:1292–1303 [DOI] [PubMed] [Google Scholar]
- 33.Heyland D, Cook D, Bagshaw SM, et al. ; Canadian Critical Care Trials Group: The very elderly admitted to ICU: A quality finish? Crit Care Med 2015; 43:1352–1360 [DOI] [PubMed] [Google Scholar]
- 34.Guidet B, Flaatten H, Boumendil A, et al. ; VIP1 study group: Withholding or withdrawing of life-sustaining therapy in older adults (>/= 80 years) admitted to the intensive care unit. Intensive Care Med 2018; 44:1027–1038 [DOI] [PubMed] [Google Scholar]
- 35.Moran JL, Bristow P, Solomon PJ, et al. ; Australian and New Zealand Intensive Care Society Database Management Committee (ADMC): Mortality and length-of-stay outcomes, 1993-2003, in the binational Australian and New Zealand Intensive Care Adult Patient Database. Crit Care Med 2008; 36:46–61 [DOI] [PubMed] [Google Scholar]
- 36.Zimmerman JE, Kramer AA, Knaus WA: Changes in hospital mortality for United States intensive care unit admissions from 1988 to 2012. Crit Care 2013; 17:R81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kaukonen KM, Bailey M, Suzuki S, et al. : Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000-2012. JAMA 2014; 311:1308–1316 [DOI] [PubMed] [Google Scholar]
- 38.Lee YZ, Dharmawan A, Zhang X, et al. : The changing landscape of general surgery in the elderly—trends over a decade in a tertiary centre in Singapore. ANZ J Surg 2022; 92:2018–2024 [DOI] [PubMed] [Google Scholar]
- 39.Park KU, Eichenhorn M, Digiovine B, et al. : Different harm and mortality in critically ill medical vs surgical patients: retrospective analysis of variation in adverse events in different Intensive Care Units. Perm J 2018; 22:16–189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ball IM, Bagshaw SM, Burns KE, et al. : Outcomes of elderly critically ill medical and surgical patients: A multicentre cohort study. Can J Anaesth 2017; 64:260–269 [DOI] [PubMed] [Google Scholar]
- 41.Guidet B, Leblanc G, Simon T, et al. ; ICE-CUB 2 Study Network: Effect of systematic intensive care unit triage on long-term mortality among critically ill elderly patients in France: A Randomized Clinical Trial. JAMA 2017; 318:1450–1459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Darvall JN, Bellomo R, Paul E, et al. : Frailty in very old critically ill patients in Australia and New Zealand: A population-based cohort study. Med J Aust 2019; 211:318–323 [DOI] [PubMed] [Google Scholar]
- 43.Heyland DK, Garland A, Bagshaw SM, et al. : Recovery after critical illness in patients aged 80 years or older: a multi-center prospective observational cohort study. Intensive Care Med 2015; 41:1911–1920 [DOI] [PubMed] [Google Scholar]
- 44.Villa P, Pintado MC, Lujan J, et al. : Functional status and quality of life in elderly intensive care unit survivors. J Am Geriatr Soc 2016; 64:536–542 [DOI] [PubMed] [Google Scholar]
- 45.Hoffman KL B, Van Haren F: Very old patients urgently referred to the intensive care unit: Long-term outcomes for admitted and declined patients. Crit Care Resusc 2016; 18:157–164 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.