Abstract
PURPOSE
Pediatric leukemia outcomes are poor in most low- and middle-income countries (LMICs) and exacerbated by health care systems ill equipped to manage cancer. Effective leukemia management in LMICs involves curating epidemiologic data; providing health care workforce specialty training; developing evidence-based treatments and supportive care programs; safeguarding access to medications and equipment; providing patient and family psychosocial, financial, and nutritional support; partnering with nongovernmental organizations, and ensuring treatment adherence.
METHODS
In 2013, through a partnership between North-American and Mexican institutions, we used the WHO Framework for Action, a health systems strengthening model to implement a leukemia care sustainable program aimed at improving acute lymphoblastic leukemia (ALL) outcomes at a public hospital in Mexico. We prospectively assessed clinical features, risk classification, and survival outcomes in children with ALL at Hospital General-Tijuana from 2008 to 2012 (preimplementation) and from 2013 to 2017 (postimplementation). We also evaluated program sustainability indicators.
RESULTS
Our approach led to a fully-staffed leukemia service, sustainable training programs, evidence-based and data-driven projects to improve clinical outcomes, and funding for medications, supplies, and personnel through local partnerships. Preimplementation and postimplementation 5-year overall survival for the entire cohort of children with ALL, children with standard-risk ALL, and children with high-risk ALL improved from 59% to 65% (P = .023), 73% to 100% (P < .001), and 48% to 55% (P = .031), respectively. All sustainability indicators improved between 2013 and 2017.
CONCLUSION
Using the health systems strengthening WHO Framework for Action model, we improved leukemia care and survival in a public hospital in Mexico across the US-Mexico border. We provide a model for the development of similar programs in LMICs to sustainably improve leukemia and other cancer outcomes.
INTRODUCTION
Despite significant strides in curative treatments made over the past 4 decades, acute lymphoblastic leukemia (ALL) remains one of the leading causes of childhood death and morbidity after infancy.1 In high-income countries (HICs), 5-year overall survival (OS) ranges from 80% to 90%. This dramatic improvement has been attributed to advancements in diagnostic technologies, risk-stratification systems, and treatment protocols driven by cooperative clinical trials.2,3 Nevertheless, ALL survival outcomes have not been equitable around the world. As the global pediatric cancer burden grows in low- and middle-income countries (LMICs),4-6 ALL OS in LMICs has been reported between 10% and 60%.7,8 These disparate outcomes could be mitigated with wider availability of critical, specialized, and supportive care.5,6,9
CONTEXT
Key Objective
To describe the application of the health systems strengthening WHO Framework for Action to a twinning program between Rady Children's Hospital San Diego, USA, and Hospital General-Tijuana, Mexico, to evaluate its impact on capacity building for high-quality, sustainable care and on improving survival for children with leukemia in a low- and middle-income country (LMIC) setting.
Knowledge Generated
Our initiative resulted in a fully staffed pediatric leukemia service with protocols, organization, and structure designed to address each of the six building blocks of the WHO Framework for Action model. Preimplementation and postimplementation results demonstrate significant improvements in survival in children with leukemia in Baja California, Mexico, and improved program sustainability indicators.
Relevance
The success of the application of the WHO Framework for Action model to our twinning program supports the incorporation of the six building blocks when developing pediatric leukemia and other cancer control programs in LMICs.
In Mexico, ALL is the most common pediatric cancer and the second leading cause of death between age 5 and 14 years10 with OS reported to be 20%-40%.10-12 State of the art diagnostic and clinical services, access to pediatric oncologists, and specialized and critical care training for all providers are limited in many Mexican institutions.13 To mitigate these disparities in access and outcomes, we established in 2008 a twinning program between Rady Children's Hospital San Diego, St Jude Children's Research Hospital, and Hospital General-Tijuana (HGT), Mexico, in the US-Mexico border region.6,14 Although this model improved access to care and clinical outcomes at HGT from 2008 to 2013, its dependency on the institutions in HIC required an alternative strategy to ensure long-term sustainability and independence. To address this, in 2013, we used the WHO health systems strengthening Framework for Action model15 to implement measures to decrease the dependency of the twinning program on external resources, promote sustainability, and continue to improve ALL outcomes in the public sector in Mexico. We describe the developmental milestones on the basis of the WHO Framework for Action and its early impact on clinical outcomes for patients with ALL at HGT preimplementation from 2008 to 2012 and postimplementation from 2013 to 2017. We also report indicators of sustainability in 2013 and 2017.
METHODS
Context and Health Systems Strengthening Model for Developing High-quality Leukemia Care
HGT is a major public referral hospital in northwestern Mexico, serving approximately three million people. Yet, in 2008, the hospital had limited treatment options, and outcomes for children with cancer were dismal in Tijuana and the state of Baja California. HGT had neither a dedicated pediatric oncology unit nor a pediatric intensive care unit. There were no pediatric oncologists or pediatric oncology nurses. Diagnostic equipment was severely limited, and stock outs of medications were frequent. Responding to the need for high-quality pediatric cancer care in the US-Mexico border region, Rady Children's Hospital San Diego in partnership with St Jude Children's Research Hospital launched a collaborating twinning program at HGT in 2008.6,14 Twinning involves a partnership between pediatric cancer centers in HICs and LMICs aimed at improving survival and other clinical outcomes by sharing knowledge, expertise, and resources.
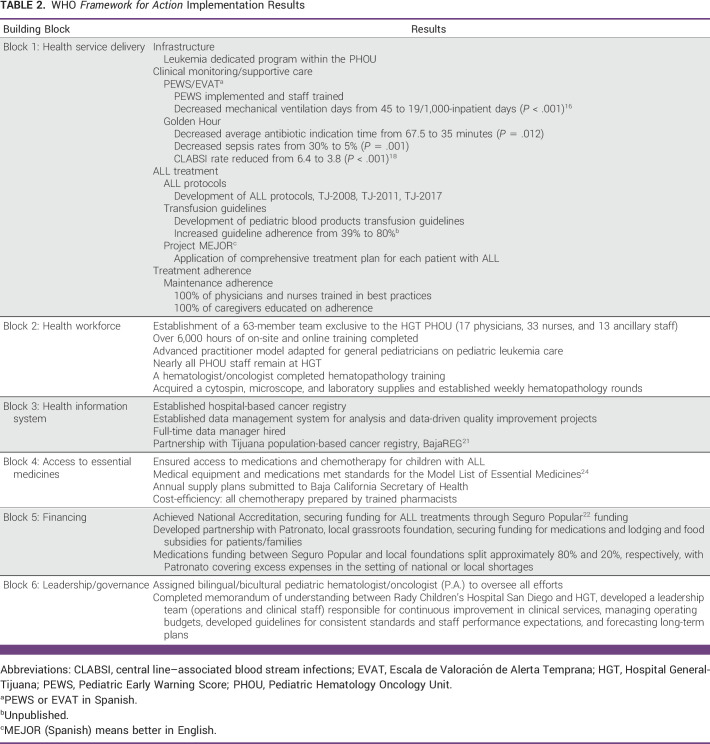
As the number of patients with ALL increased and the needs escalated, we adopted the health systems strengthening WHO Framework for Action15 model in 2013 as a development roadmap to implement an independent and sustainable leukemia care program. The building blocks of the WHO Framework for Action describe essential and interdependent functions necessary for the optimal performance of a health system and include service delivery, workforce, information systems, access to essential medicines, financing, and local leadership/governance. We used the WHO Framework for Action as a guide in setting substantive and comprehensive milestones necessary for developing sustainable capacity for high-quality pediatric leukemia services (Fig 1).
FIG 1.
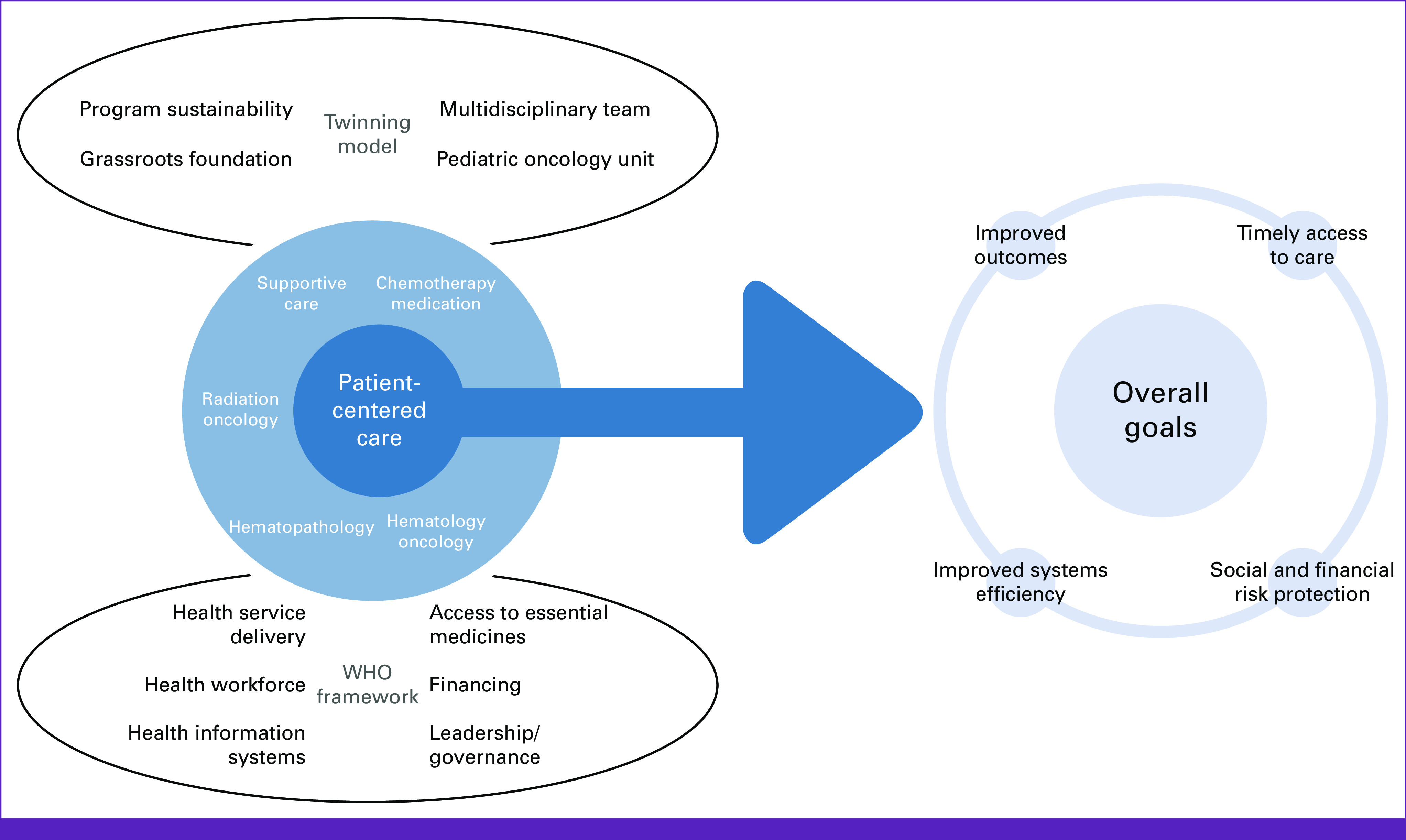
Twinning-WHO framework combination model to achieve high-quality leukemia care.
Leukemia Care Program Implementation: Application of the WHO Framework for Action Model
We conducted a needs assessment by using an instrument adapted from St Jude Children's Research Hospital's needs assessment tools14 and developed and set a 10-year action plan with objectives outlined according to the WHO Framework for Action.
Block 1. Health Service Delivery.
To ensure the delivery of effective, safe, and high-quality clinical care with minimum waste, we focused on four main areas.
Infrastructure.
Our first objective was to increase capacity through pediatric leukemia-specific infrastructure within the dedicated Pediatric Hematology Oncology Unit (PHOU) inaugurated in 2008 at HGT.
Clinical monitoring and supportive care.
To enhance the ability to monitor patient status and respond to clinical needs, we introduced the Pediatric Early Warning Score (PEWS) system.16 We secured a Mexican federal grant, developed the PEWS team, and trained all PHOU staff according to St Jude Children's Research Hospital PEWS implementation guidelines. Additionally, the Golden Hour project was established to ensure faster antibiotic initiation during neutropenic fever events to reduce sepsis risk.17,18 HGT staff developed a systematized protocol for supply inventory, indication, and administration of antibiotics.
ALL treatment.
Led through bimonthly meetings with a Spanish-speaking pediatric hematologist/oncologist (P.A.) with expertise in pediatric leukemia from Rady Children's Hospital San Diego, our team initiated an action plan to establish HGT's first locally adapted chemotherapy protocol19 and guidelines for blood products transfusions adapted to resource-limited settings, created training materials and milestones for assessing the impact, and established a weekly leukemia board to identify areas of improvement related to management of ALL. We also began the Project MEJOR (better in English), a protocol for applying a comprehensive and system-by-system treatment plan for each patient with ALL in the PHOU during daily rounds.
Treatment adherence.
To address treatment abandonment, we initiated projects to improve adherence to treatment, particularly during the 1- to 2-year long ALL maintenance chemotherapy. Nurses led education initiatives for all patients with ALL and their caregivers.
Block 2. Health Workforce.
We focused our training and education efforts on diagnostics and specialized outpatient and inpatient care for critically ill patients with ALL. We appointed a lead pediatrician and two nurse educators at HGT to develop a primarily on-site training in-person curriculum in pediatric leukemia for physicians, nurses, and allied staff.
Implementation of the leukemia care program included multidisciplinary daily rounds, a weekly leukemia board, and 24/7 coverage in the inpatient unit by trained pediatricians. We recruited six pediatric oncologists and eight pediatricians over 5 years. Additionally, skill development and upgraded equipment for the pathology and hematology laboratories were emphasized as early priorities.
To build the PHOU's nursing workforce, we recruited nursing staff permanently assigned to the PHOU. The nurse educators taught a 6-week orientation course developed by St Jude Children's Research Hospital,20 including advanced pediatric leukemia clinical competencies. Training was supplemented by visits to Rady Children's Hospital San Diego and to St Jude Children's Research Hospital affiliated sites in Guatemala and Chile.20
Block 3. Health Information Systems.
We aimed to establish a system for the collection, analysis, application, and dissemination of reliable data to monitor clinical progress and effectively design data-driven quality improvement projects. To achieve these goals, we developed a hospital-based cancer registry at HGT and partnered with the Tijuana population-based cancer registry, BajaREG.21
Block 4. Access to Essential Medicines.
To ensure a consistent supply of equipment, medications, and supplies with priority placed on quality, safety, efficacy, and cost-effectiveness, we aimed to develop practices to reduce waste and garnered financial support from the HGT leadership and Patronato, a local grassroots nongovernmental foundation.
Block 5. Financing.
To address financial sustainability of ALL management, we applied for national accreditation to ensure funding through the Popular Insurance Program (Seguro Popular)22 and established a partnership with Patronato. Additional startup funding was obtained from Rady Children's Hospital San Diego and St Jude Children's Research Hospital.
Block 6. Leadership/Governance.
Our partnership model between Rady Children's Hospital San Diego and HGT was aimed at promoting a bilateral commitment of time, personnel, and financial resources as the basis for collaboration to improve leukemia care. An early priority included forming a multidisciplinary implementation team to engage key stakeholders in vision setting, with an emphasis on establishing a local governance structure, accountability, and transparency at the individual and organizational levels, and to ensure long-term sustainability. Rady Children's Hospital San Diego and St Jude Children's Research Hospital provided leadership training for key staff at HGT.
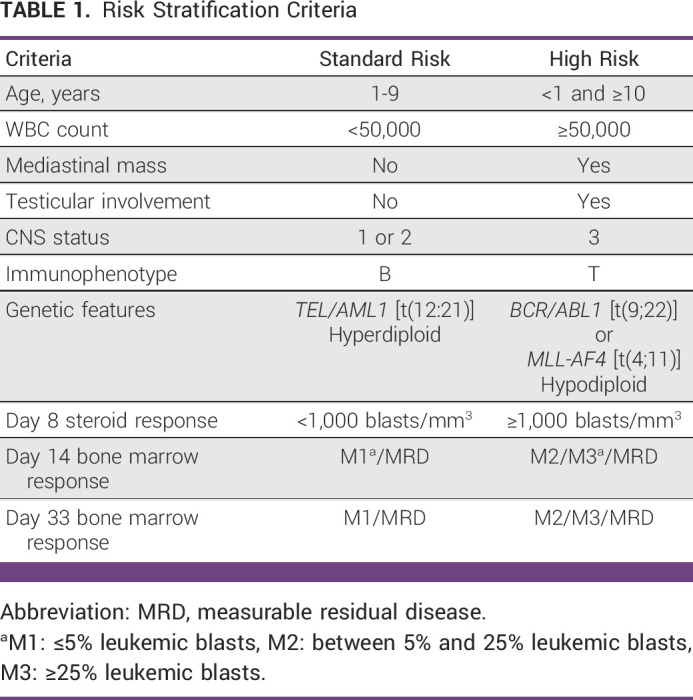
ALL Patient Outcome Measures
We prospectively collected data on children younger than 18 years with ALL diagnosed between 2008 and 2017 at HGT. Risk stratification was applied to all patients using the National Cancer Institute risk classification criteria, immunophenotyping, genetic features, and measurable residual disease (Table 1). Two cohorts were analyzed separately: preprogram implementation from 2008 to 2012 and postimplementation from 2013 to 2017. Outcomes including OS and event-free survival (EFS) were estimated and stratified according to risk of relapse (standard-risk [SR] or high-risk [HR]) and compared between the two cohorts. Events included relapse, treatment abandonment (interruption of treatment of at least 4 weeks for nonmedical reasons), and death. The Institutional Review Boards for the University of California San Diego/Rady Children's Hospital San Diego and HGT approved this study. Informed consent was obtained from parents/legal guardians.
TABLE 1.
Risk Stratification Criteria
Statistical Analysis
We performed descriptive statistics to describe baseline patient characteristics (age, sex, and risk stratification). Kaplan-Meier survival curves were generated for OS and EFS, and hazard ratios and 95% CIs were calculated. Log-rank tests were used to determine the statistical significance of differences in OS and EFS between the preimplementation and the postimplementation cohorts. Statistical analyses were conducted using R software (3.5.0; R Foundation for Statistical Computing, Vienna, Austria). We considered a P ≤ .05 to indicate statistical significance.
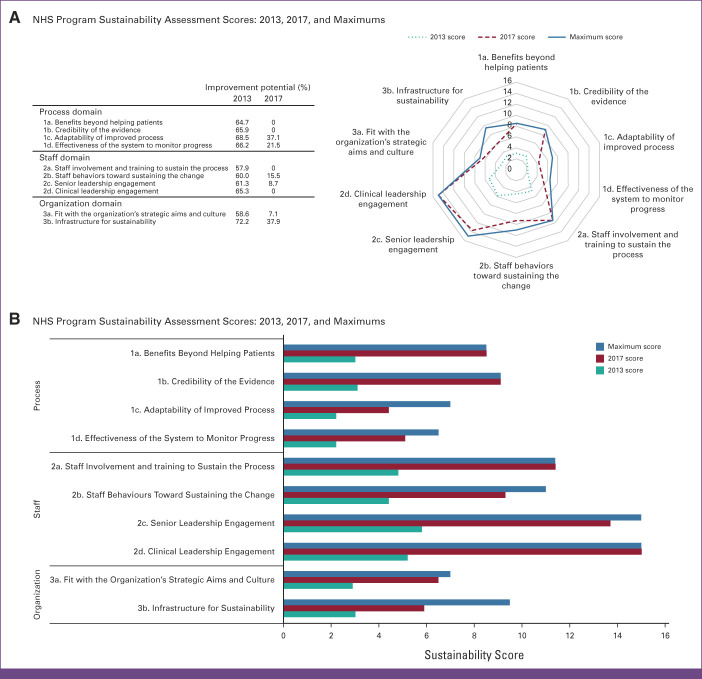
Program Sustainability Assessment
Sustainability indicators encompassed three major domains: process, staff, and organization and were analyzed in 2013 and at the end of 2017 using a validated score-based sustainability tool.23 The National Health Service (NHS) Sustainability Model is a self-assessment tool detailing 10 key indicators that increase the likelihood of sustainability and continuous improvement for a specific change that has been introduced into an organization. Scores represented leaders' and point-of-care staff's perceptions.
RESULTS
WHO Framework for Action Implementation Results
The results of the implementation of the WHO Framework for Action model are summarized in Table 2.
TABLE 2.
WHO Framework for Action Implementation Results
ALL Clinical Outcomes
Approximately 20-22 children with ALL per year were expected in Tijuana on the basis of the childhood population. The majority (approximately 60%) were diagnosed and received care at HGT.
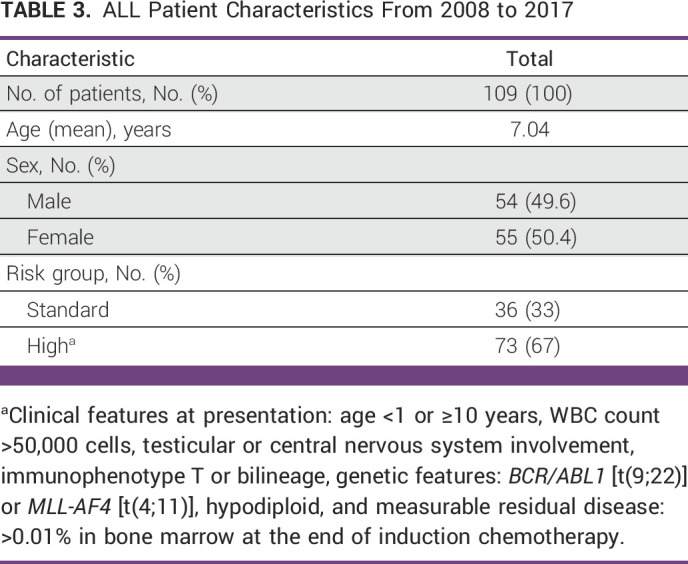
In total, 109 children with newly diagnosed ALL were included in this study and were divided into two cohorts: preimplementation (n = 49, from 2008 to 2012) and postimplementation (n = 60, from 2013 to 2017). Patient characteristics are described in Table 3.
TABLE 3.
ALL Patient Characteristics From 2008 to 2017
Five-year OS for the entire cohort was 65% in 2017, and 5-year EFS was 56% (Fig 2A). Among the entire cohort, between preprogram implementation and postimplementation, 5-year OS for children with ALL improved from 59% to 65% (P = .023; Fig 2B). Additionally, preimplementation and postimplementation 5-year OS for children with SR ALL improved from 73% to 100% (P < .001), and for children with HR ALL, OS improved from 48% to 55% (P = .031; Figs 2C and 2D).
FIG 2.
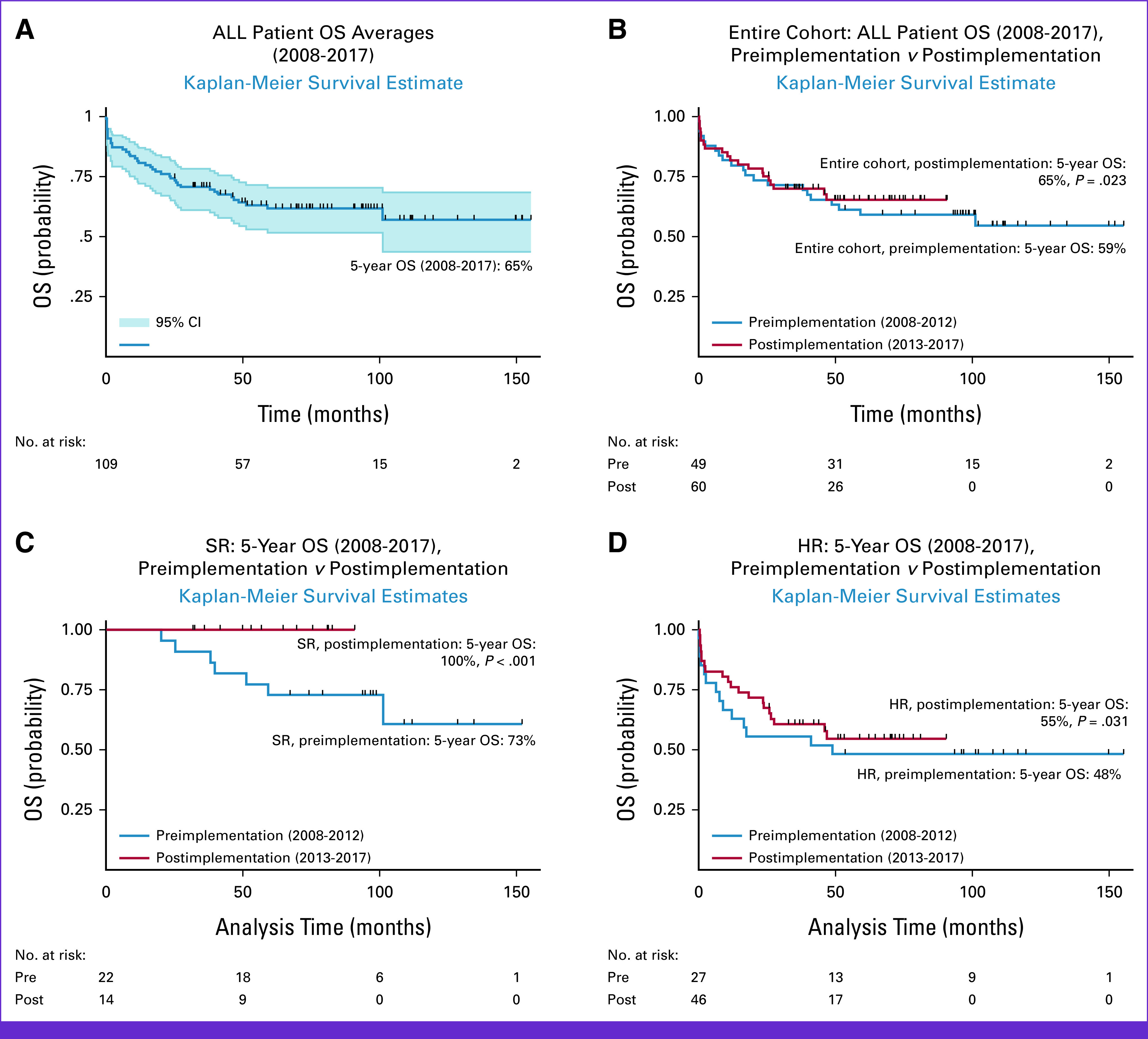
ALL survival outcomes. HR, high risk; OS, overall survival; SR, standard risk.
Sustainability Assessment Results
All the sustainability indicators assessed had an improvement potential when documented for process, staff, and organization domains (Fig 3). The two indicators of the process domain with the highest improvement potential were the adaptability of improved processes and the effectiveness of the system to monitor progress. Clinical leadership engagement was considered the most critical indicator in the staff domain. In the organization domain, the infrastructure for sustainability indicator was the most important (Fig 3). In 2017, 4 of 10 sustainability indicators reached the maximum improvement potential, 2 of 10 sustainability indicators had improvement potentials below 10%, and the remaining 4 of 10 sustainability indicators had improvement potentials below 40% (Fig 3).
FIG 3.
Program sustainability assessment. NHS, National Health Service.
DISCUSSION
The application of the WHO's health systems strengthening Framework for Action model and its six building blocks: service delivery, workforce, information systems, access to essential medicines, financing, and leadership/governance resulted in the successful implementation of an effective and sustainable leukemia care program in the US-Mexico border region. The 5-year OS and EFS improved significantly postprogram implementation. Moreover, we demonstrated improvement across all three NHS sustainability domains: process, staff, and organization. These results support that pediatric ALL outcomes in LMIC settings can be meaningfully improved through partnership programs designed according to health systems strengthening models.
The efficacy in improving ALL and other pediatric cancer outcomes through twinning programs has been well documented across diverse LMIC settings including in Latin America, the Middle East, and East Asia.25-27 However, ALL outcomes, particularly survival, still lag behind those in HICs.2-4 Although causes of failure can vary across LMICs, the application of health systems strengthening models focused on building sustainability are essential to closing this survival gap. According to our sustainability assessment, improvement potential was achieved in 2013 after implementing the leukemia program at HGT and sustained into 2017 in 6 of the 10 sustainability indicators, enabling greater capitalization of opportunities to improve survival outcomes. These improvements in sustainability suggest that the improved clinical outcomes can be sustained long-term and allow the program to adjust and continue to make improvements to respond to new challenges in providing comprehensive leukemia care in resource-constrained settings.
A significant improvement in OS and EFS between preprogram and postprogram implementation for both patients with SR and HR ALL and a steadily increasing 5-year OS rate of 65% for the entire ALL cohort within a decade of our program's inception demonstrate sustained high-quality care and improved outcomes. Additionally, an increase of more than 30% improvement potential across all 10 sustainability indicators from 2013 to 2017 suggests the success of the WHO Framework for Action approach. The WHO Framework for Action model and its focus on long-term sustainability and a comprehensive approach to program implementation enabled us to systematically address commonly recognized elements to improving ALL outcomes in LMICs, including specialized training,4-6 development of locally adapted treatment protocols,19 providing supportive care and infection control,9,17,18,28,29 ensuring funding for treatment,6,14,22,25 supporting treatment adherence, and reducing financial toxicity toward affected patients' families through lodging and food subsidies.6-8,14
The scale of our model is small; nevertheless, there are precedents for endeavoring toward large-scale pediatric leukemia care improvements in LMICs. Examples include the Asociación de Hemato-Oncología Pediátrica de Centro América and Mexico's Seguro Popular initiative, which in 2008 introduced new coverage for pediatric cancer treatment. However, Mexico still faces challenges in providing effective ALL treatment. It was estimated that only 48% of eligible patients were covered by Seguro Popular, and clinical outcomes remain variable across different regions.22 For instance, studies report that 62% of pediatric oncologists in Mexico remain concentrated in its three largest cities (Mexico City, Guadalajara, and Monterrey).22 Although two studies11,30 report a higher prevalence (58%-78%) of HR ALL, similar to our rate of 67%, a lack of a Mexican national cancer registry21 limits the epidemiological understanding of pediatric ALL in Mexico. Therefore, there is an urgent need to implement more evidence-based pediatric leukemia care through sustainable national collaborative efforts.
Our study has limitations including a small sample size in a large public reference hospital that precludes in-depth analysis and generalizability to other settings. Additionally, a lack of a hospital-based cancer registry before the twinning cancer program implementation in 2008 at HGT limited our ability to accurately compare survival rates with those from before the twinning program started. Furthermore, since risk categorization is subjected to advancements in diagnostic technologies and expertise gained by the treatment team over time, especially when using criteria such as molecular classification and measurable residual disease, potential risk migration during the postimplementation period may have altered accuracy of survival data when stratifying by risk groups. Regarding reproducibility, our leukemia care program is unique in that it benefited from the proximity (24 miles) between Rady Children's Hospital San Diego and HGT, enabling a large degree of in-person collaboration that is uncommon to most global health partnerships. Finally, our results are limited to the period when Seguro Popular was in place. Seguro Popular is in the process of transitioning to a new system Instituto de Salud para el Bienestar (INSABI), which aims for universal coverage in Mexico. Thus, our model and results may not be translated over to private or social security settings and sustainability would need to be remeasured after INSABI is fully implemented in Baja California.
In conclusion, the WHO Framework for Action encompassing approach to its six building blocks was successfully incorporated into an existing twinning model to improve survival in children with ALL in an effective and sustainable way in the US-Mexico border. This model appeals to broader impact in Mexico, with priorities concerning healthcare workforce and delivery standards, building national population-based cancer registries, improving national funding mechanisms, and facilitating collaboration between public and private organizations across regions. Improved pediatric leukemia survival outcomes are achievable in LMICs through international partnerships that apply health systems strengthening models to build capacity and sustainability. Our model serves as an example for future global partnerships aimed to establish pediatric and adult cancer services in LMICs. Interdisciplinary, concerted, and cooperative approaches improve the likelihood of successful collaborative projects. Forthcoming initiatives should consider the implementation of standardized approaches for data collection through cancer registries and surveillance systems, the building of sustainability through financial and bidirectional leadership structures and the provision of patient-centered care to mitigate socioeconomic barriers to optimal clinical outcomes. Future research should evaluate best practices in establishing global health partnerships aimed at improving cancer care through the application of health systems strengthening models adapted to local health systems in each unique community.
ACKNOWLEDGMENT
We thank the multidisciplinary team at the Hospital General Tijuana, especially Jose Robles, MD; Clemente Zuniga, MD; Magdalena Perez, MD; Gabriela Aguiar, MD; Dara Torres, MD; Mario Martinez, MD; Laura Nuno, MD; Adriana Loera, MD; Martha Magdaleno, MD; Diana Ramirez, PharmD; Mariana Camberos, BA; Alicia Sanchez, RN; Marco Aguilera, RN; Mitzi Romano, RN; Maria Justo, RN; Fernanda Buendia, RN; Gabriela Murillo, BA; Dulce Sanchez, BA; Raquel Ruiz, BA; Marcela Baltazar, MA; Dora Bastidas, LSW; and Martha Garcia, LSW, for their support and hard work. We thank Patronato and Casa de la Amistad foundations especially Alfonso Valenzuela, MD; Gloria Monforte, MD; Alejandra Cardenas, MA; Myriam Foglio; Consuelo Barcenas; Pedro Geffroy, MA; Alberto Torres, MS; Silvia Ornelas, MA; and Leonardo Arana, MS, for their continued support. At Rady Children's Hospital San Diego, we thank the leadership team, Patrick A. Frias, MD; Nicholas Holmes, MD, MBA; Jill Strickland; and Gail Knight, MD, MMM. We thank the team at St Jude Children's Research Hospital Global Pediatric Medicine, especially Carlos Rodriguez-Galindo, MD, and Paola Friedrich, MD, MPH, for sharing their knowledge. The support and advice of Margareta Norton, (F) Chief Administrative Officer at Rady Children's Hospital San Diego, has been extremely valuable and is greatly appreciated.
DISCLAIMER
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or National Cancer Institute.
PRIOR PRESENTATION
Presented in part as an oral presentation at the ASCO Annual Meeting, Chicago, IL, June 2-6, 2023.
SUPPORT
Supported by the National Cancer Institute (NCI) K08 CA230306 (Aristizabal), by NCI grant CA21765 (Ribeiro) and by the American Lebanese and Syrian Associated Charities (Ribeiro).
AUTHOR CONTRIBUTIONS
Conception and design: Paula Aristizabal, Raul C. Ribeiro, William Roberts
Provision of study materials or patients: Paula Aristizabal, Rebeca Rivera-Gomez, Mario Ornelas, Maribel Ramirez, Gabriela Tamayo Angelica Martinez, William Roberts
Collection and assembly of data: Paula Aristizabal, Rebeca Rivera-Gomez, Mario Ornelas, Maribel Ramirez, Gabriela Tamayo
Data analysis and interpretation: Paula Aristizabal, Rebeca Rivera-Gomez, Andrew Chang, Angelica Martinez, Raul C. Ribeiro, William Roberts
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/go/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
No potential conflicts of interest were reported.
REFERENCES
- 1. Katz AJ, Chia VM, Schoonen WM, et al. Acute lymphoblastic leukemia: An assessment of international incidence, survival, and disease burden. Cancer Causes Control. 2015;26:1627–1642. doi: 10.1007/s10552-015-0657-6. [DOI] [PubMed] [Google Scholar]
- 2. Pui CH, Yang JJ, Bhakta N, et al. Global efforts toward the cure of childhood acute lymphoblastic leukaemia. Lancet Child Adolesc Health. 2018;2:440–454. doi: 10.1016/S2352-4642(18)30066-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pui CH, Evans WE. A 50-year journey to cure childhood acute lymphoblastic leukemia. Semin Hematol. 2013;50:185–196. doi: 10.1053/j.seminhematol.2013.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rodriguez-Galindo C, Friedrich P, Morrissey L, et al. Global challenges in pediatric oncology. Curr Opin Pediatr. 2013;25:3–15. doi: 10.1097/MOP.0b013e32835c1cbe. [DOI] [PubMed] [Google Scholar]
- 5. Ribeiro RC, Steliarova-Foucher E, Magrath I, et al. Baseline status of paediatric oncology care in ten low-income or mid-income countries receiving My Child Matters support: A descriptive study. Lancet Oncol. 2008;9:721–729. doi: 10.1016/S1470-2045(08)70194-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Aristizabal P, Fuller S, Rivera R, et al. Improving pediatric cancer care disparities across the United States-Mexico border: Lessons learned from a transcultural partnership between San Diego and Tijuana. Front Public Health. 2015;3:159. doi: 10.3389/fpubh.2015.00159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jabeen K, Ashraf MS, Iftikhar S, et al. The impact of socioeconomic factors on the outcome of childhood acute lymphoblastic leukemia (ALL) treatment in a low/middle income country (LMIC) J Pediatr Hematol Oncol. 2016;38:587–596. doi: 10.1097/MPH.0000000000000653. [DOI] [PubMed] [Google Scholar]
- 8. Navarrete M, Rossi E, Brivio E, et al. Treatment of childhood acute lymphoblastic leukemia in central America: A lower-middle income countries experience. Pediatr Blood Cancer. 2014;61:803–809. doi: 10.1002/pbc.24911. [DOI] [PubMed] [Google Scholar]
- 9. Ceppi F, Antillon F, Pacheco C, et al. Supportive medical care for children with acute lymphoblastic leukemia in low- and middle-income countries. Expert Rev Hematol. 2015;8:613–626. doi: 10.1586/17474086.2015.1049594. [DOI] [PubMed] [Google Scholar]
- 10. Rivera-Luna R, Shalkow-Klincovstein J, Velasco-Hidalgo L, et al. Descriptive epidemiology in Mexican children with cancer under an open national public health insurance program. BMC Cancer. 2014;14:790. doi: 10.1186/1471-2407-14-790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Verduzco-Rodriguez L. Prevalence of high-risk acute lymphoblastic leukemia (ALL) in Mexico, a possible explanation for outcome disparities. J Clin Oncol. 2018;36:e22501. [Google Scholar]
- 12. Castro-Ríos A, Reyes-Morales H, Pelcastre-Villafuerte BE, et al. Socioeconomic inequalities in survival of children with acute lymphoblastic leukemia insured by social security in Mexico: A study of the 2007–2009 cohorts. Int J Equity Health. 2019;18:40. doi: 10.1186/s12939-019-0940-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rodriguez-Romo L, Olaya Vargas A, Gupta S, et al. Delivery of pediatric cancer care in Mexico: A national survey. JCO Glob Oncol. 2018 doi: 10.1200/JGO.17.00238. 10.1200/JGO.17.00238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Aristizabal P, Fuller S, Rivera-Gomez R, et al. Addressing regional disparities in pediatric oncology: Results of a collaborative initiative across the Mexican-North American border. Pediatr Blood Cancer. 2017;64:e26387. doi: 10.1002/pbc.26387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.https://www.who.int/healthsystems/strategy/everybodys_business.pdf Everybody’s business: Strengthening health systems to improve health outcomes: WHO’s framework for action. World Health Organization.
- 16. Martinez A, Baltazar M, Loera A, et al. Addressing barriers to successful implementation of a pediatric early warning system (PEWS) at a pediatric oncology unit in a general hospital in Mexico Pediatr Blood Cancer 66 e27989 2019. 31568621 [Google Scholar]
- 17. Ornelas-Sánchez M, Nuño-Vázquez L, Loera-Reyna A, et al. The “Golden Hour”: A capacity-building initiative to decrease life-threating complications related to neutropenic fever in patients with hematologic malignancies in low- and middle-income countries. Blood Adv. 2018;2:63–66. doi: 10.1182/bloodadvances.2018GS112240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gonzalez ML, Aristizabal P, Loera-Reyna A, et al. The Golden Hour: Sustainability and clinical outcomes of adequate time to antibiotic administration in children with cancer and febrile neutropenia in northwestern Mexico. JCO Glob Oncol. 2021 doi: 10.1200/GO.20.00578. 10.1200/GO.20.00578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pedrosa F, Coustan-Smith E, Zhou Y, et al. Reduced-dose intensity therapy for pediatric lymphoblastic leukemia: Long-term results of the Recife RELLA05 pilot study. Blood. 2020;135:1458–1466. doi: 10.1182/blood.2019004215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Day SW, Segovia L, Viveros P, et al. Development of the Latin American Center for pediatric oncology nursing education. Pediatr Blood Cancer. 2011;56:5–6. doi: 10.1002/pbc.22856. [DOI] [PubMed] [Google Scholar]
- 21. Rivera-Gomez R, Quintana P, Martinez J, et al. Establishing a pediatric population based cancer registry in a low-middle income country: Challenges and lessons learned Pediatr Blood Cancer 66 e27989 2019. 31568621 [Google Scholar]
- 22. Pérez-Cuevas R, Doubova SV, Zapata-Tarres M, et al. Scaling up cancer care for children without medical insurance in developing countries: The case of Mexico. Pediatr Blood Cancer. 2013;60:196–203. doi: 10.1002/pbc.24265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maher L, Gustafson D, Evans A. Sustainability Model and Guide. Coventry, England: KT Pathways; 2010. [Google Scholar]
- 24.https://www.who.int/groups/expert-committee-on-selection-and-use-of-essential-medicines/essential-medicines-lists World Health Organization: 22nd Essential Medicines List (EML) and the 8th Essential Medicines List for Children (EMLc), 2021.
- 25. Aristizabal P, Burns LP, Kumar NV, et al. Improving pediatric neuro-oncology survival disparities in the United States-Mexico border region: A cross-border initiative between San Diego, California, and Tijuana, Mexico. JCO Glob Oncol. 2020 doi: 10.1200/GO.20.00377. 10.1200/GO.20.00377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Veerman AJ, Sumadiono S. Twinning: A rewarding scenario for development of oncology services in transitional countries. Pediatr Blood Cancer. 2005;45:103–106. doi: 10.1002/pbc.20390. [DOI] [PubMed] [Google Scholar]
- 27. Barr RD, Klussmann FA, Baez F, et al. Asociación de Hemato-Oncología Pediátrica de Centro América (AHOPCA): A model for sustainable development in pediatric oncology. Pediatr Blood Cancer. 2014;61:345–354. doi: 10.1002/pbc.24802. [DOI] [PubMed] [Google Scholar]
- 28. Gupta S, Antillon FA, Bonilla M, et al. Treatment-related mortality in children with acute lymphoblastic leukemia in Central America. Cancer. 2011;117:4788–4795. doi: 10.1002/cncr.26107. [DOI] [PubMed] [Google Scholar]
- 29. Caniza MA, Odio C, Mukkada S, et al. Infectious complications in children with acute lymphoblastic leukemia treated in low-middle-income countries. Expert Rev Hematol. 2015;8:627–645. doi: 10.1586/17474086.2015.1071186. [DOI] [PubMed] [Google Scholar]
- 30. Pérez-Saldivar ML, Fajardo-Gutiérrez A, Bernáldez-Ríos R, et al. Childhood acute leukemias are frequent in Mexico City: Descriptive epidemiology. BMC Cancer. 2011;11:355. doi: 10.1186/1471-2407-11-355. [DOI] [PMC free article] [PubMed] [Google Scholar]