Abstract
PURPOSE
To describe the establishment of an oncology unit at the National Referral Hospital (NRH) in the Solomon Islands, a low-income nation in the South Pacific.
METHODS
A scoping visit was carried out in 2016 to assist in the development of coordinated cancer services and to establish a medical oncology unit at the NRH at the request of the Medical Superintendent. This was followed by an observership visit to Canberra by an NRH doctor training in oncology in 2017. After a request from the Solomon Islands Ministry of Health, the Australian Government Department of Foreign Affairs and Trade (DFAT) arranged an in-country multidisciplinary mission under the Royal Australasian College of Surgeons/Royal Australasian College of Physicians Pacific Islands Program to help in the commissioning of the NRH Medical Oncology Unit in September 2018. Staff training and education sessions were held. The team, with the assistance of an Australian Volunteers International Pharmacist, has helped the NRH staff to develop localized Solomon Islands Oncology Guidelines. Donated equipment and supplies have helped with the initial establishment of the service. A second DFAT Oncology mission visit was made in 2019 followed by two NRH oncology nurses visiting Canberra on observership later that year and support of the Solomon's doctor to pursue postgraduate education in cancer sciences. Ongoing mentorship and support has been maintained.
RESULTS
The island nation now has a sustainable oncology unit delivering chemotherapy treatments and management of patients with cancer.
CONCLUSION
A collaborative multidisciplinary team approach by professionals from the high-income country working with colleagues from the low-income nation with coordination of different stakeholders was the key to this successful initiative in improving cancer care.
BACKGROUND
The Solomon Islands is a South Pacific nation consisting of 350 islands and nine provinces with a population of 686,878 in 2020. Local industry consists of fisheries, forestry, mining, crops, and tourism, with 75% of the population living in rural areas and villages, with most being subsistence farmers. Specialist medical services are concentrated at the tertiary referral center the National Referral Hospital (NRH) in Honiara on the main island of Guadalcanal. The hospital infrastructure is old, with the hospital built during World War II. Ultrasound and plain radiology including mammography was available but no computed tomography (CT; until 2022), magnetic resonance imaging, or nuclear medicine services. With no intensive care unit, radiotherapy facilities, and limited pathology services, this presents logistical issues of access and delivery of cancer care to a population scattered across a large geographical region.
CONTEXT
Key Objective
To establish an oncology unit in the Solomon Islands and to be able to provide centralized oncology services.
Knowledge Generated
It is important to work with local leaders and be responsive to their specific identified needs and requests for assistance.
Relevance
These collaborative multidisciplinary team initiatives have contributed to building the capacity and capability of the National Referral Hospital Medical Oncology Unit to treat patients with cancer with an ongoing sustainable partnership and continued mentorship. This experience and linkage with other groups active in the region has led to the formation of the Clinical Oncology Society of Australia Global Oncology Group in an attempt to coordinate efforts in training cancer health professionals in the South Pacific.
The present Solomon Islands Cancer Registry was re-established in 2008 with the support of the WHO International Agency for Research on Cancer with CanReg 5 registry software and is a hospital-based registry collecting incident cases of inpatient and outpatient cancer diagnoses at the NRH as well as the pathology laboratory diagnosis of cancer.1 Because of the limited anatomical pathology services with most cases having to be sent to Brisbane for reporting, not all cases were confirmed histologically with incomplete capture of incident cases. This registry was staffed by two registered nurses and a medical registrar. The top five cancers seen at the NRH in 2014-2015 were cervical cancer, breast cancer, thyroid cancer, lymphoma, and oral cancers.1
Established risk factors for cancer were examined in the Solomon Islands by the WHO Stepwise Approach to Surveillance Survey in 2006. This identified tobacco smoking in 30.6% of the population, alcohol consumption of five or more standard drinks in 25.1% of men, low physical activity in 41.0%, and obesity in 32.4% of the population. Betel nut chewing was also very prevalent, with 62.6% of the population practicing this. This is highly correlated with oral cancers and esophageal squamous cell cancer.2
Treatment of cancer in the Solomon Islands was not coordinated with multidisciplinary care. Each clinical department would treat their own patients with cancer including the administration of systemic anticancer therapies.
Scoping of Cancer Services
It was recognized that the cancer services needed development and there was a plan to centralize chemotherapy administration under the supervision of one physician with two nurses trained to administer cytotoxic drugs. A request was made by the Medical Superintendent of the NRH to the John James Foundation Pacific Health Program for a review of the cancer services and the chemotherapy protocols used at the hospital. A scoping visit was made in September 2016 by a senior consultant medical oncologist from Australia. Meetings were held with the surgeons, gynecologists, pathologist, pharmacist, and pediatrician with visits to the operating theaters, wards, emergency department, the Cancer Registry, and pathology department.
Chemotherapy was administered by the doctors from each of the respective treatment teams (usually the registrars) in the ward dressing rooms. As a result, general medicine, general surgery, and pediatric teams were all involved in chemotherapy delivery. For example, surgical teams would manage breast cancers, colorectal cancers, and head and necks cancers, medical teams would manage the range of hematologic malignancies (myeloma, lymphomas, and myelodysplasias), and pediatricians would manage childhood cancers. Protocols were outdated and some were taken from other Pacific Island hospitals and the pediatric ones were from the Royal Children's Hospital in Melbourne. Very few patients underwent chemotherapy treatments.
Chemotherapy orders were written on normal ward medication order forms with the doses being calculated by doctors. Pharmacy did not keep copies of the protocols and relied on doctors' prescription and therefore did not cross-check the dosing. The cytotoxic drugs were dispensed by pharmacy and the vials were sent to the ward where they would be reconstituted by doctors before administration. Records regarding chemotherapy treatments, toxicity, and dose adjustments were kept in the patients' medical records, which were kept on the wards during treatment and not sent to central records until the course of treatment was completed. A one-page treatment plan with case details and a table of the planned dates of each cycle of therapy was used to track the treatment course. Drug supply was an issue, and shortages meant that sometimes patients came for treatment but found that chemotherapy drugs were not available, with bookings having to be rescheduled.
It was planned for a building occupied by the midwifery school to be converted into an oncology unit with the Cancer Registry nurses to be trained in chemotherapy administration with supervision by the medical registrar, who was to be trained as a medical oncologist.
The main challenges that were determined with respect to establishing an oncology unit were:
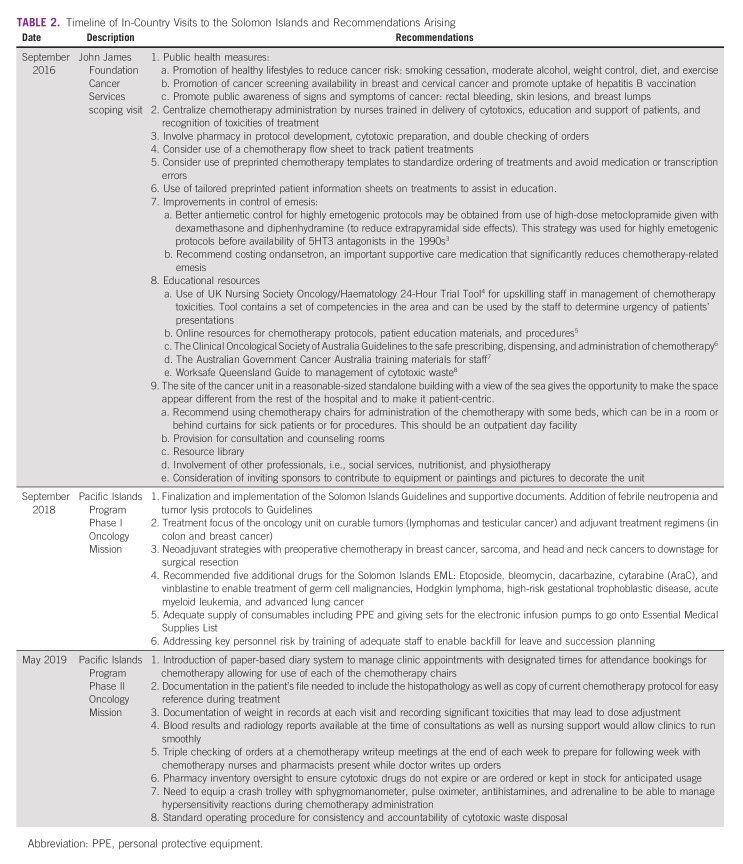
Limited anticancer systemic therapy drugs
The restricted range of drugs available for anticancer therapy limited which cancers could be treated (Table 1). However, this range was similar to that widely available in the early 1990s in developed nations. Imatinib mesylate was the only targeted agent available for chronic myeloid leukemia and gastrointestinal stromal tumors, provided through a special access scheme through the Max Foundation.
2. Availability of antiemetics
TABLE 1.
Anticancer Systemic Therapies Available on the Solomon Islands EML: Drugs Available in 2016
The only antiemetic available on the hospital formulary was metoclopramide. 5HT3 antagonists were not on the Essential Medicines List (EML). These were usually brought over by overseas visiting surgical teams on missions for postoperative management of emesis but were not used routinely as premedication in patients receiving highly emetogenic chemotherapy schedules. This therefore affected the acceptability of chemotherapy for patients with cancer and made clinicians wary of using such protocols.
3. Lack of hematologic growth factor support and intensive care facilities
Clinicians were wary of causing febrile neutropenia from severely myelosuppressive chemotherapy regimens because of their limited ability to manage patients who become hemodynamically unstable from sepsis.
4. The large geographical spread of the population necessitating travel from the outer provinces to the NRH. Provincial hospitals did not have specialist departments
5. Cultural issues where patients may prefer to pursue traditional healing methods with massage and traditional herbal remedies through local healers
6. The lack of printed educational materials for patients
7. No dedicated staff who administer chemotherapy
8. Slow internet speeds because of connection at this time to the country being by satellite links. This made accessing resource materials online or streaming online content very difficult
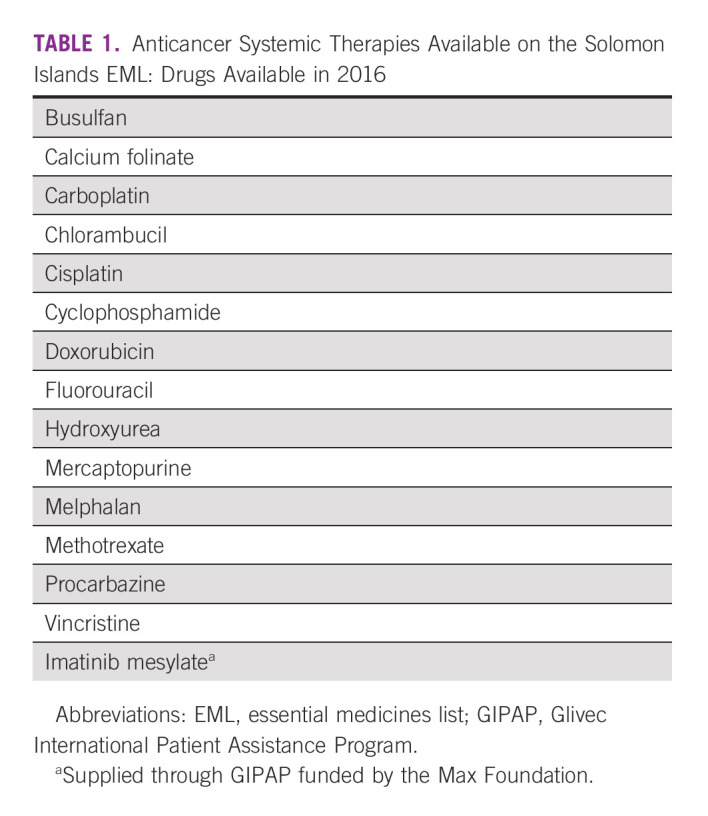
Some specific recommendations that were made after this initial scoping visit are tabulated in Table 2.
TABLE 2.
Timeline of In-Country Visits to the Solomon Islands and Recommendations Arising
MEDICAL CLINICAL OBSERVERSHIP
The NRH executive approval for the establishment of a separate oncology unit was passed in 2017, and renovations began on the building. The John James Foundation was able to fund a month-long observership visit by the NRH oncology registrar to The Canberra Hospital through a Visiting Fellowship in Medical Oncology. During this visit, time was spent in clinics and on the ward with specialists in medical oncology, radiation oncology, hematology, and palliative care. Attendance at multidisciplinary meetings, journal clubs, and teaching sessions were arranged as well as attachments with oncology pharmacy, anatomical pathology, medical imaging, and time with the day chemotherapy units at the Canberra Region Cancer Centre and the National Capital Private Hospital. Workflows and protocols for chemotherapy administration were observed and those that could to be implemented in the resource-constrained setting of the Solomon Islands were selected for development.
A request for provision of chemotherapy chairs to the NRH was fulfilled as the National Capital Private Hospital Chemotherapy Unit had recently been refurbished. Four decommissioned manual chemotherapy recliner chairs and four high back bedside chairs were able to be delivered to the NRH by Doctors Assisting in the South Pacific Islands with a shipment of medical supplies in early 2018.
PACIFIC ISLANDS PROGRAM MISSIONS
Phase I Visit: September 2018
A multidisciplinary team of a medical oncologist, a clinical hematologist, a clinical nurse consultant in medical oncology, and a cancer pharmacist made a visit to the NRH in September 2018 under the Australian Government Department of Foreign Affairs and Trade (DFAT) Pacific Islands Program administered by the Royal Australasian College of Physicians (RACP) and Royal Australasian College of Surgeons (RACS). The team was accompanied by the International Partnerships Manager of the RACP, who helped to facilitate the training sessions.
The visit objectives were:
To create protocols and guidelines for procurement, storing, mixing, and administration of chemotherapy suitable to the NRH context
To conduct training for health staff assigned to the new department on their respective responsibilities, eg, pharmacist training for mixing of agents, and nurse training for patient handling/model of care and for medical oversight and safe administration of chemotherapy
Ahead of the visit, the team was in communication with an Australian Volunteers International Pharmacist on placement at the NRH working with a local committee to produce drafts of the Solomon Islands Oncology Guidelines document as well as Chemotherapy Consent Form, Patient Information Pamphlet, Chemotherapy Referral Form, and Patient Education Checklist. A thorough review and revision of existing chemotherapy protocols and available agents on the EML were also performed.
The NRH Medical Oncology Unit had been partially refurbished and started operations several weeks before. The visiting team brought over seven donated refurbished electronic intravenous pumps, which were deployed in the unit. At the request of the Solomon's oncology team, the Mission also brought two drugs, bleomycin and etoposide (which were not on the Solomon Islands EML), to be able to offer curative treatment for two men with advanced testicular cancer. The urgent treatment of one patient was commenced under the supervision of the visiting team using the complex bleomycin, etoposide, and cisplatin (BEP) chemotherapy protocol that had not been previously administered at the NRH. This was observed by the local oncology team, pharmacy staff, and ward nurses throughout most steps of the process and recorded as a video for future training purposes. Ondansetron was now on the EML, and this protocol was administered without significant toxicity.
Interactive workshops with hospital staff were conducted to determine the local needs and perceived issues in cancer care in three breakout groups: doctors, nursing staff, and pharmacists. Lists were compiled from each group of what they wished to be covered during this visit and subsequently.
Training sessions were carried out in use of personal protective equipment (PPE), hand hygiene, use of the electronic intravenous infusion pumps, safe handling of cytotoxic agents, management of extravasations and spills, and safe disposal of cytotoxic wastes. Compounding of chemotherapy was now facilitated on trolleys in the Oncology Unit with use of PPE and this process was observed by the visiting team. A decision was made in conjunction with the Pharmacy Department about procurement of a compounding isolator to be installed in a room next to the Oncology Unit.
There was also a role-play session in obtaining consent from patients for treatment and counseling patients regarding the process of treatment and the toxicities. Other group sessions included calculation of chemotherapy dosing including adjustment for side effects and protocol development. Staff from the Oncology Unit, ward nurses, and pharmacists participated in these sessions, which were also recorded as video files. The Solomon Islands Oncology Guideline document was revised, and the first version of this document was made available on the Solomon Islands Guideline Host app for smartphones (Therapeutic Guidelines Foundation, Melbourne).
The National Medical Stores (NMS), located 10 minutes drive from the NRH, warehoused all medicines and medical supplies arriving in the Solomon Islands. Products are received and kept at this facility, which is equipped with an industrial fridge, medicines safe, and locked cages among rows and shelves for all products. Procured items are then distributed not only to the NRH but also to surrounding provinces as they are needed. A visit to the NMS was made to discuss procurement concerns and supply chain issues.
Clinic and ward consultations were conducted for patients with malignancies. Bone marrow biopsies were also performed by the hematologist in two patients to make the diagnosis of two hematologic malignancies.
The visiting team participated in Continuing Medical Education sessions on systemic anticancer therapies, blood film interpretation of malignant and nonmalignant conditions, and treatment toxicities including tumor lysis and febrile neutropenia. Visits were made to pharmacy, medical imaging, microbiology, virology, hematology laboratory, biochemistry, and anatomical pathology. Information on the utility of CT scanning in cancer management was provided to the Director of Radiology to assist in the preparation of a ministerial brief for the acquisition of a CT scanner for the NRH.
The recommendations from this visit are tabulated in Table 2.
Phase II Visit: May 2019
A second DFAT Pacific Islands Program Oncology Mission was conducted in May 2019.
The visiting team spent time observing the workflows within the NRH Oncology Unit and discussing processes with the staff regarding the operations of the outpatient clinics, day chemotherapy unit, patient management, and cytotoxic waste disposal. It was noted that all patients arrived at the same time in the morning and that some could wait many hours before they were seen or treated. Clinic consultations were slowed by lack of nursing support and the clinics were not prepped beforehand.
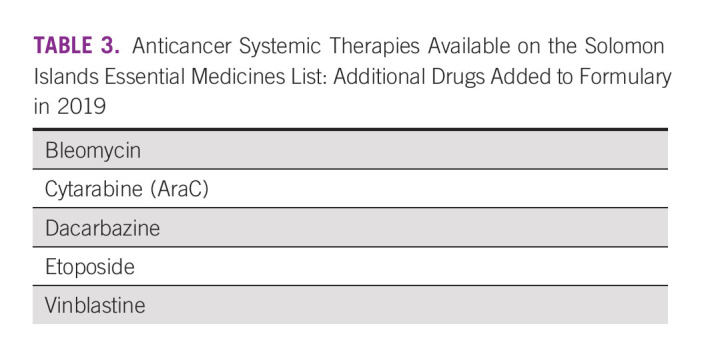
The skills of the local staff were observed in the use of PPE, prescribing, preparation, and administration of chemotherapy. Their skills and confidence had markedly improved since the Phase I visit. Consent forms, referral forms, and chemotherapy plan documents were now in use. Ward and clinic consultations were again conducted and some educational meetings. The Pacific Islands Mission Team brought supplies of carboplatin in the adjuvant treatment of a resected patient with testicular seminoma, and dacarbazine and vinblastine for use in the ABVD protocol (doxorubicin, bleomycin, vinblastine, and dacarbazine) for a patient with Hodgkin lymphoma. Although these three drugs were newly listed on the EML, they were not in stock and had not been used previously.
A schema for managing new patients was established, documented, and incorporated into the Solomon Islands Oncology Guidelines. Version two of the Guidelines was finalized incorporating the protocols using the new drugs that were now on the Solomon Islands EML (Table 3).
TABLE 3.
Anticancer Systemic Therapies Available on the Solomon Islands Essential Medicines List: Additional Drugs Added to Formulary in 2019
Specific recommendations of this mission are listed in Table 2.
Oncology Nursing Observership Visit
The John James Foundation funded a request to bring two oncology nurses from the NRH Oncology Unit to The Canberra Hospital in November 2019 for a one-month observership. During the visit, the nurses completed the online Antineoplastic Drug Administration Course through eviQ Education9 to give them an educational grounding in chemotherapy administration. They attended medical oncology and hematology outpatient clinics and ward attachments. They observed inpatient care including that of immunosuppressed high-dependency patients, inpatient chemotherapy protocols, and attended nursing handover and allied health team meetings. In the day chemotherapy unit, they observed:
Chemotherapy and biological therapy administration given via a cannula, peripherally inserted central catheter line, or portacath
Intravesical Bacillus Calmette‐Guerin and chemotherapy administrations
Use of PPE
Chemotherapy education
Chemotherapy checking procedures
Use of scalp cooling to prevent hair loss
Administration of blood products
Treatment of hypersensitivity reactions
During the oncology pharmacy attachment, they had these activities:
Observation of chemotherapy screening and checking procedures
Learning how medications are stored and used safely
Observing the counseling of patient with take-home medications
Chemotherapy gowning procedures and techniques for aseptic preparation
Observation of chemotherapy manufacturing in a positive pressure room under a lamina flow hood
Observation of the overall workflow from drug to manufactured product to patient treatment packaging to take-home medications
CHALLENGES AND EFFECTS OF THE GLOBAL PANDEMIC
The onset of the COVID-19 global pandemic in 2020 curtailed visits owing to closure of international borders. Engagement and ongoing mentorship of the Solomon Islands Oncology Team were maintained by e-mail during this period. Online educational sessions on various surgical topics, including cancers, were organized by Doctors Assisting in South Pacific Islands with faculty from Australia linking in with specialists and training registrars from Papua New Guinea, Solomon Islands, Fiji, Vanuatu, and Kiribati. Internet capacity and speeds in the Solomon Islands have improved since the launch of the Coral Sea Cable System, a fiber optic undersea telecommunications cable linking Australia (Sydney), Papua New Guinea (Port Moresby), and the Solomon Islands (Honiara) in 2020. The 4G mobile telephone network, which has been available since 2017, had also expanded to allow wireless internet data connections. Both have enabled improvements in streaming internet content and videoconferencing.
The NRH Oncology Unit was able to maintain its operations despite several staff members contracting COVID-19, but there were some fatalities among immunocompromised patients on chemotherapy. Cytotoxic and consumable shortages and delays in supplies were also experienced during this difficult period.
The staff of the NRH Oncology Unit have created the NRH Cancer Trust Fund to accept donations that arose from fundraising efforts by the Miss Solomon Islands 2019 Pageant, to help the patients with cancer and the oncology unit. Donations that have come from many local businesses were used to complete the renovations of the oncology unit including fit-out of the isolator room, and acquisition of further equipment and an air conditioner for the building (Fig 1). Health promotion through events and on radio was also conducted by NRH Oncology Unit staff to raise public awareness of cervical and breast cancer.
FIG 1.
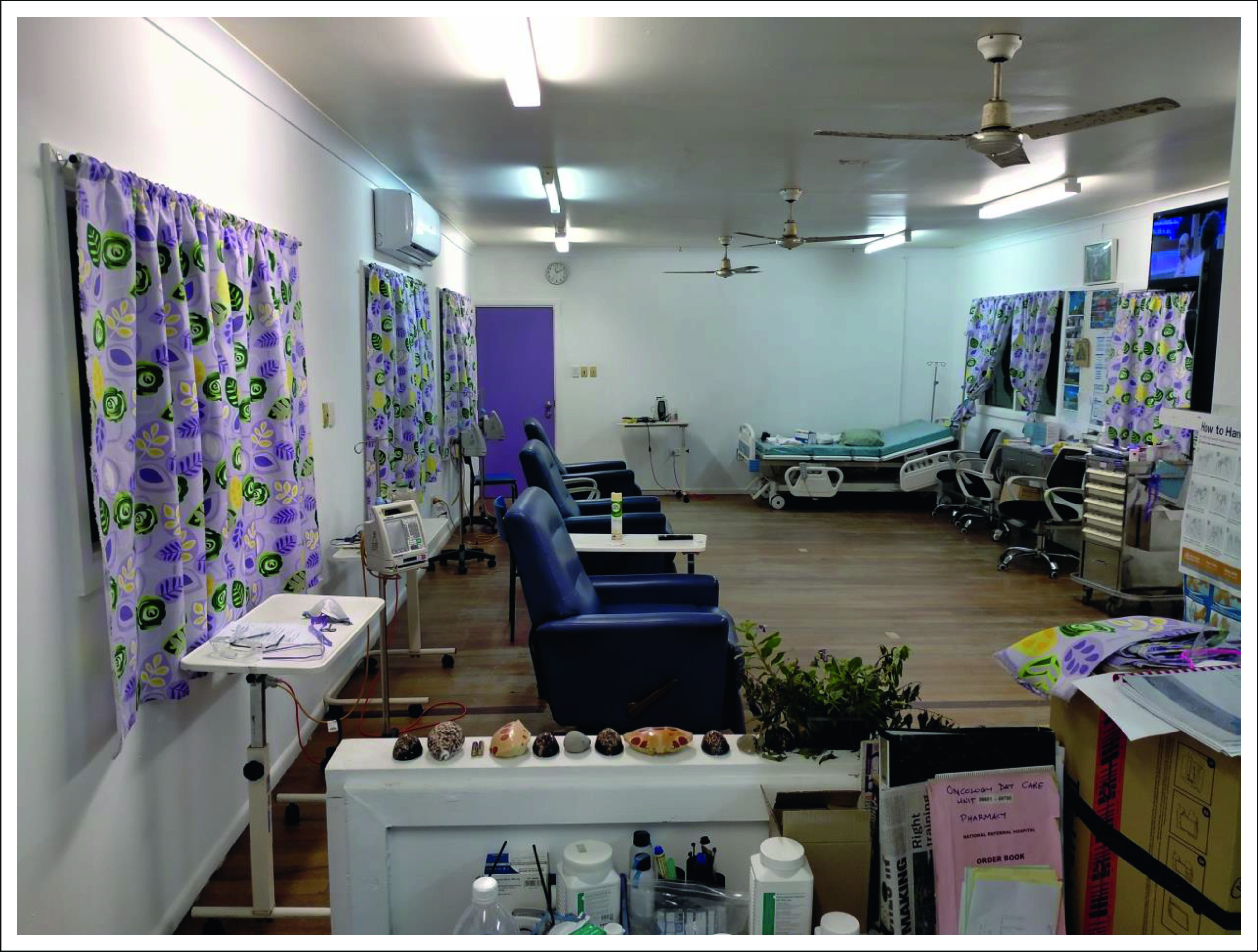
Refurbished National Referral Hospital Oncology Unit in Honiara.
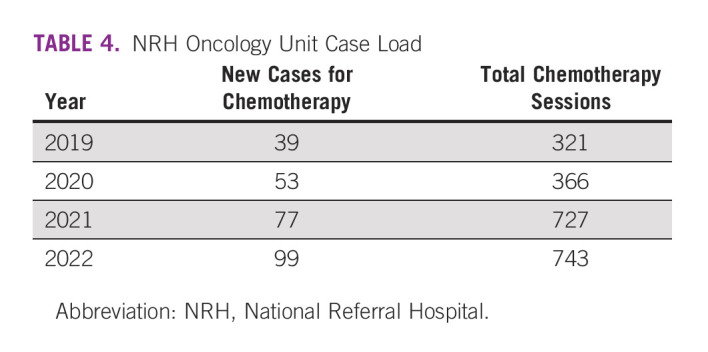
The procurement of the chemotherapy isolator for the manufacture of chemotherapy treatments was also progressed and became fully functional from July 2022. A biomedical technician was able to install this via online communication with the manufacturers during the time of pandemic international border closures. Compounding is currently being performed by nursing and medical staff in a safe, closed, and sterile system within the NRH Oncology Unit (Fig 2). Activity of the NRH Oncology Unit has steadily increased since its establishment (Table 4).
FIG 2.
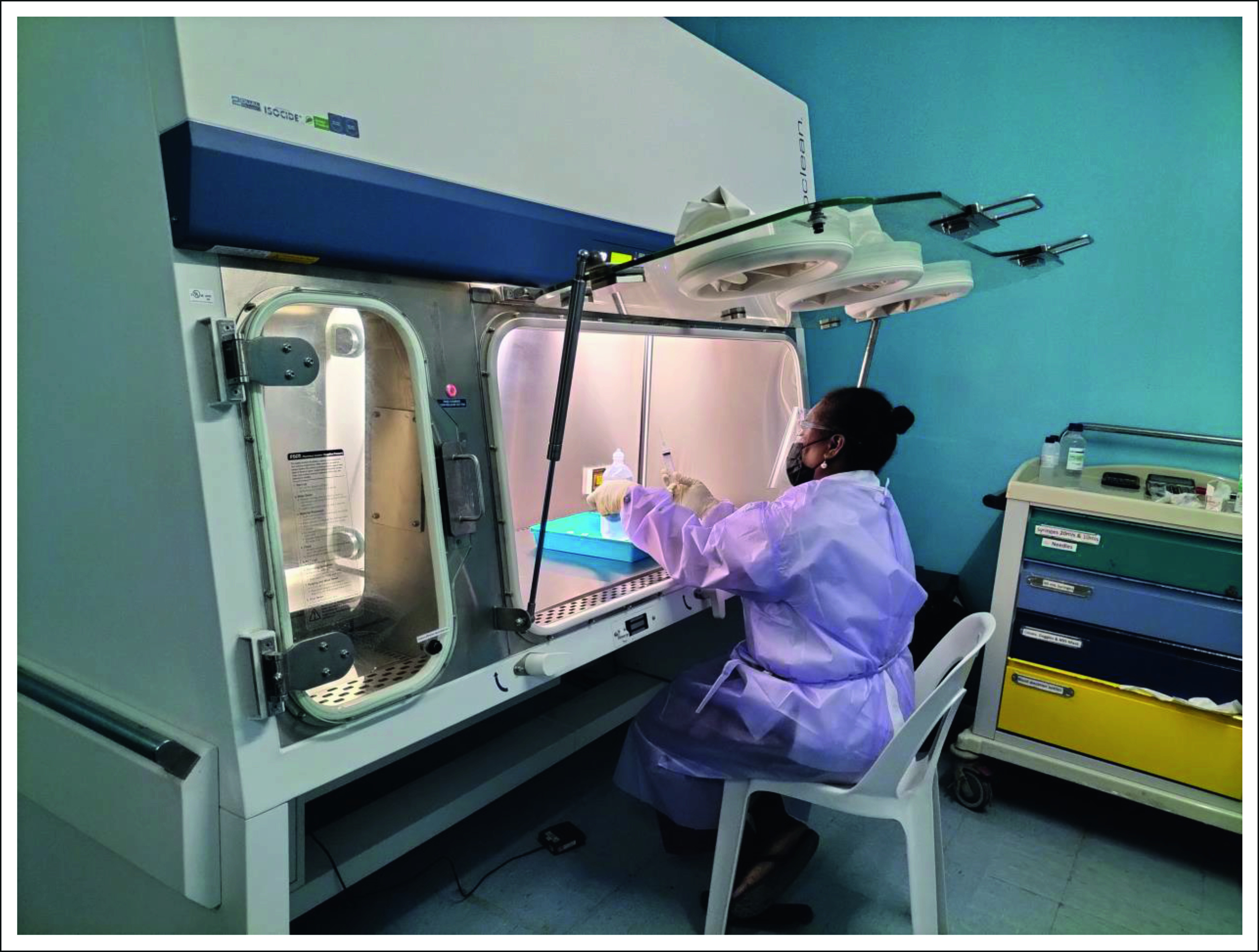
Chemotherapy compounding by oncology nurse using cytotoxic isolator.
TABLE 4.
NRH Oncology Unit Case Load
In conclusion, it has been recognized that a common feature of successful initiatives to meeting oncology challenges in the Asia-Pacific region is the adoption of a collaborative approach. This involves collaboration of high-income countries (HICs) with low- and middle-income countries (LMICs) but with cancer service design and implementation being led by local health professionals. The role of the HICs has been in responding to local requests for specific assistance with training, equipment, and technical expertise.10 With the increasing global incidence of cancer and the burden of new diagnoses and case fatality falling on LMICs, which have constrained resources and funding, HICs in the Asia-Pacific region have role to play in improving access to cancer care of their LMIC neighbors.11 This can be by:
Education and institutional partnerships to develop capacity in cancer care
Supporting better data collection through registries
Capacity building in cancer research
Engaging and training clinicians in global oncology
Web-based training, tumor boards, and advocacy endeavors
Funding of global oncology activities.
The Clinical Oncology Society of Australia has recently formed the Global Oncology Group with the core aims of promoting education, research, advocacy, and collaboration in cancer in LMICs and coordinating the stakeholders who are active in the Asia-Pacific region. The establishment of the NRH Oncology Unit in Honiara demonstrated the success of this approach in assisting the Solomon Islands in providing coordinated cancer care for its population.
ACKNOWLEDGMENT
The authors are grateful for the provision of equipment and chemotherapy drug supplies by ICON Cancer Care and National Capital Private Hospital with logistical support from Doctors Assisting in the South-Pacific Islands (DAISI). The substantive work of Emily Porello in developing the Solomon Islands Oncology Guidelines in collaboration with the DFAT Pacific Islands Oncology Team in her role as an Australian Volunteers International Pharmacist is acknowledged. The authors thank the staff of Canberra Region Cancer Centre, Calvary Health Care ACT, and National Capital Private Hospital in hosting the professional visits. The assistance of Isabella Allan the Manager of International Partnerships at the Royal Australasian College of Physicians is also acknowledged in coordination of the Pacific Islands Project Missions. Special thanks to Helen Carter, the Project Manager at the John James Foundation, for logistical support with the initial scoping visit and the observerships.
Desmond Yip
Stock and Other Ownership Interests: Commonwealth Serum Laboratories (CSL)
Honoraria: SERVIER, Pfizer (Inst), AstraZeneca
Consulting or Advisory Role: Merck Serono (Inst), Bayer (Inst), SERVIER (Inst), Amgen (Inst), Specialised Therapeutics (Inst), Deciphera (Inst)
Travel, Accommodations, Expenses: Novartis, Amgen
Nalini Pati
Consulting or Advisory Role: CSL Behring
No other potential conflicts of interest were reported.
PRIOR PRESENTATION
Presented at the Clinical Oncology Society of Australia Annual Scientific Meeting on the 13th of November 2019 and at the Royal Australian and New Zealand College of Radiologists Annual Scientific Meeting on 28th of October 2022 both in Adelaide, Australia.
SUPPORT
Supported by the John James Foundation and the Australian Government Department of Foreign Affairs and Trade through the Royal Australasian College of Surgeons/Royal Australasian College of Physicians Pacific Islands Program.
AUTHOR CONTRIBUTIONS
Conception and design: Desmond Yip, Nalini Pati, Wendy Spencer, Beth Hua, Rooney Jagilly
Administrative support: Desmond Yip, Beth Hua
Provision of study materials or patients: Wendy Spencer, Rooney Jagilly
Collection and assembly of data: Andrew Soma, Wendy Spencer, Rooney Jagilly
Data analysis and interpretation: Nalini Pati, Wendy Spencer
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/go/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Desmond Yip
Stock and Other Ownership Interests: Commonwealth Serum Laboratories (CSL)
Honoraria: SERVIER, Pfizer (Inst), AstraZeneca
Consulting or Advisory Role: Merck Serono (Inst), Bayer (Inst), SERVIER (Inst), Amgen (Inst), Specialised Therapeutics (Inst), Deciphera (Inst)
Travel, Accommodations, Expenses: Novartis, Amgen
Nalini Pati
Consulting or Advisory Role: CSL Behring
No other potential conflicts of interest were reported.
REFERENCES
- 1. Martiniuk A, Jagilli R, Natuzzi E, et al. Cancer in the Solomon Islands. Cancer Epidemiol. 2017;50:176–183. doi: 10.1016/j.canep.2017.04.016. [DOI] [PubMed] [Google Scholar]
- 2. Tovosia S, Ko AMJ, Chen PH, et al. Prevalence and associated factors of betel quid use in the Solomon Islands: A hyperendemic area for oral and pharyngeal cancer. Am J Trop Med Hyg. 2007;77:586–590. [PubMed] [Google Scholar]
- 3. Harder S, Herrstedt J. Metoclopramide: An antiemetic in chemotherapy induced nausea and vomiting. J Drug Des Res. 2017;4:1037. [Google Scholar]
- 4.UK Oncology Nursing Society Oncology/Haematology 24 Hour Rapid Assessment and Access Toolkit (ed 2)London, UK, UK Oncology Nursing Society; 2016 [Google Scholar]
- 5.eviq.org.au eviQ Cancer Treatments Online: Cancer Institute NSW.
- 6.Clinical Oncological Society of Australia . Guidelines for the Safe Prescribing. Dispensing and Administration of Cancer Chemotherapy; 2008. Sydney, Australia. [DOI] [PubMed] [Google Scholar]
- 7.https://www.cancerlearning.gov.au Cancer Australia: Cancer Learning, Australian Government.
- 8.Office of Industrial Relations . Workplace and Safety Queensland. Queensland Government; 2018. Guide for handling cytotoxic drugs and related waste. [Google Scholar]
- 9.NSW Government . In: eviQ Education: Antineoplastic Drug Administration Course. Cancer Insitute NSW, editor. Sydney, Australia, NSW Government; 2017. [Google Scholar]
- 10. Ward IG, Mel A, Soma A, et al. A collaborative approach to meeting oncology challenges in island communities in the Asia-Pacific region. J Med Imaging Radiat Oncol. 2021;65:418–423. doi: 10.1111/1754-9485.13160. [DOI] [PubMed] [Google Scholar]
- 11. Wilson BE, Pokorny AMJ, Perera S, et al. Australia and New Zealand's responsibilities in improving oncology services in the Asia-Pacific: A call to action. Asia-Pacific J Clin Oncol. 2022;18:133–142. doi: 10.1111/ajco.13544. [DOI] [PubMed] [Google Scholar]