Abstract
Introduction Gynecomastia is benign proliferation of male breast tissue that can be idiopathic or secondary to hormonal imbalance. Consumption of steroids plays a major role in the development of gynecomastia. The increased consumption of anabolic androgenic steroid (AAS) in youngsters to boost the physical strength and improve appearance is associated with increased prevalence of gynecomastia. True estimation of AAS-associated gynecomastia is difficult to calculate and prone to underestimation because of low social acceptance. Accurate estimation is required to assess future healthcare, for prevention and to give appropriate treatment.
Aims and Objectives The aim of this study was to calculate the steroid consumption in gynecomastia patients accurately so that appropriate treatment can be given and their response to treatment could be analysed.
Methods This is a prospective study done in a tertiary care hospital from June 2019 to June 2022. All the gynecomastia patients treated during this period in Burns & Plastic Surgery Department of PGIMS Rohtak were included in the study. Patient's detailed history was recorded and also after 3 months of surgery patients were again enquired about their history to record any change.
Results Real prevalence of AAS-associated gynecomastia (39.19%) was much higher than that recorded in preoperative period (4.05%). Also, AAS users were having higher body mass index and a greater proportion of patients were bodybuilders.
Conclusion Patients with high body mass index, athletic body, and history of recent weight gain should raise the suspicion of anabolic steroid intake. Surgery is not always indicated in AAS-associated gynecomastia. If gynecomastia persisted, surgery necessitates and it involves meticulous intraoperative hemostasis and careful glandular excision to minimize recurrence and achieve low complication rates.
Keywords: anabolic steroid, gynaecomastia, liposuction, bodybuilders
Introduction
The prevalence of gynecomastia has risen in the past few years. Parallelly, there is growing abuse of anabolic androgenic steroids (AAS) to boost physical strength and improve appearance as a serious public health problem worldwide. This increased consumption of AAS points toward the possible cause of the increased prevalence of gynecomastia.
Accurate estimation of AAS-associated gynecomastia is challenging to calculate and prone to underestimation. Various reasons of underestimation include low social acceptance and misdiagnosis. Among these reasons, low social acceptance plays a major role in the underestimation of AAS consumption in gynecomastia patients.
What seems to us regarding AAS consumption in gynecomastia patients is just like the tip of iceberg. Steroid (AAS) consumption is rising due to unhealthy lifestyle, in gym, of bodybuilders. In this study, we aim to find correlation among gynecomastia patients consuming steroid by calculating before and after surgery.
Accurate estimation is required to assess future healthcare, for prevention and appropriate treatment. Patient in active sports or bodybuilders presenting with gynecomastia should raise suspicion of steroid intake and accurate diagnosis should be made so that appropriate management can be done. 7
Patient and Methods
Aims and Objectives
Following are the aims and objectives of this article:
To calculate the steroid consumption in gynecomastia patients accurately so that appropriate treatment can be given.
To find percentage of gynecomastia patients consuming steroid.
To identify the factors indicative of steroid consumption in gynecomastia patient.
To assess response to surgical and nonsurgical management.
Methods
This is a prospective study done in a tertiary care hospital from June 2019 to June 2022. All the gynecomastia patients treated during this period were included in the study. A proforma was prepared to record preoperative data, intraoperative findings, and postoperative data. At the time of presentation, patient's demographic data, weight, height, body mass index (BMI), occupation, AAS usage details, history of other drugs intake, alcohol abuse, symptoms of underlying systemic illness such as hyperthyroidism, liver disease, or renal failure, hypogonadism, testicular carcinoma, and any family history (androgen resistance syndrome, familial aromatase excess, estrogen producing Sertoli cell tumor) were recorded. Patients, who gave positive history of anabolic steroid intake, were advised to stop the drug and keep on follow-up. Among the AAS users who did not get their symptoms resolved in 3 months of stoppage of AAS use were operated. Rest of the patients with negative history of steroid intake underwent liposuction and gland removal. At the time of surgery, intraoperative findings including amount of fat aspirated, gland size, duration of surgery, and drain insertion were noted. In the postoperative period, patients were examined for complications like surgical site infection and seroma formation. All the patients were followed up for at least 3 months postoperatively. At 3 months postsurgery, patients with negative history of AAS use were again enquired about the drug abuse to record any change in history. Patients who changed their history regarding AAS usage helped in identifying exact prevalence of steroid consumption in gynecomastia patients. After calculating the true prevalence of AAS consumption in gynecomastia patients, two groups were prepared, that is, non-AAS-associated gynecomastia and AAS-associated gynecomastia. Preoperative and intraoperative data was compared in these two groups.
Results
In this prospective study, a total 74 patients of gynecomastia were treated. Most common symptom was aesthetic concern (83%) and pain (43%). In preoperative period out of 74 only 3 patients gave the history of recent steroid intake and they were treated conservatively. Two of them developed resolution of symptoms with satisfactory aesthetics. One patient that had partial decrease in breast size was operated later on. Remaining 71 patients who did not give any positive history were operated. Operative procedure includes liposuction and gland excision using intra-areolar incision. Age group varies between 19 and 42 years and 65% patients were between 20 and 30 years age group. There was no major complication recorded in postoperative period.
After 3 months of surgery, all patients with negative history of steroid intake were again asked about history; out of 71 patients who refused about steroid intake initially, 26 gave the positive history of steroid intake making the real prevalence of 39.19% which was much higher than that recorded in preoperative period, 4.05%.
Correlation between Various Parameters and AAS Use ( Table 1)
Table 1. Comparison of various parameters among AAS users and Non AAS users.
| Parameters | AAS user | Non-AAS user | |
|---|---|---|---|
| BMI | <25 | 12 | 32 |
| >25 | 17 | 13 | |
| Body habitus | Bodybuilders | 14 | 10 |
| Non-bodybuilders | 15 | 35 | |
| Amount of fat aspirated | <300 | 16 | 14 |
| >300 | 13 | 31 | |
| Drain | Yes | 26 | 40 |
| No | 3 | 5 | |
Abbreviations: AAS, anabolic androgenic steroid; BMI, body mass index.
The AAS users were having higher average BMI (28.3vs. 24.6 kg/m, p = 0.02) and a greater proportion of patients were bodybuilders (48.2 vs. 22.2%, p < 0.01; Fig. 1 ).
Fig. 1.
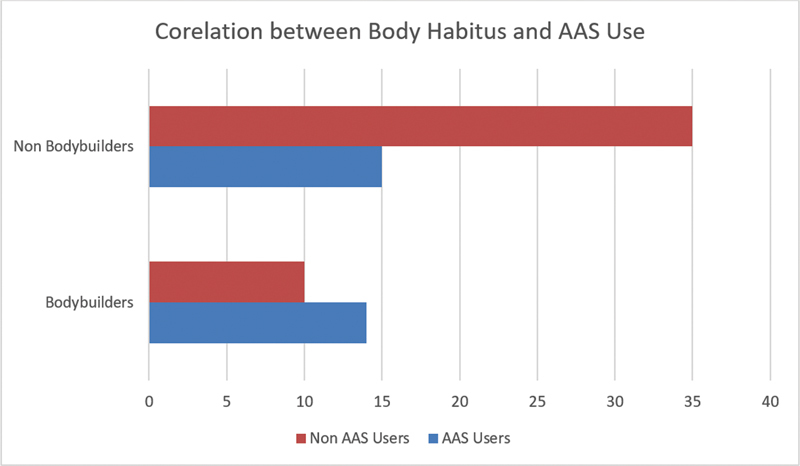
Correlation between body habitus and anabolic androgenic steroid use.
The AAS users had less lipoaspirate fat volume (250 vs. 600 mL, p < 0.05) and had more glandular tissue.
Drain was inserted in more than 80% patients in both the groups. We found no significant difference in terms of drain insertion between these two groups.
Also, a large number of AAS users were bodybuilders (48.2%) and having higher BMI (58.6%).
Response to treatment : Three patients were managed conservatively and responded well with complete regression in two patients and partial in one patient. Surgery was done in 72 patients and no major complication was observed. There was no recurrence in patients whether they are steroid abuser or not ( Figs. 2 , 3 , 4 , 5 ).
Fig. 2.

Preoperative photo of gynecomastia patient.
Fig. 3.
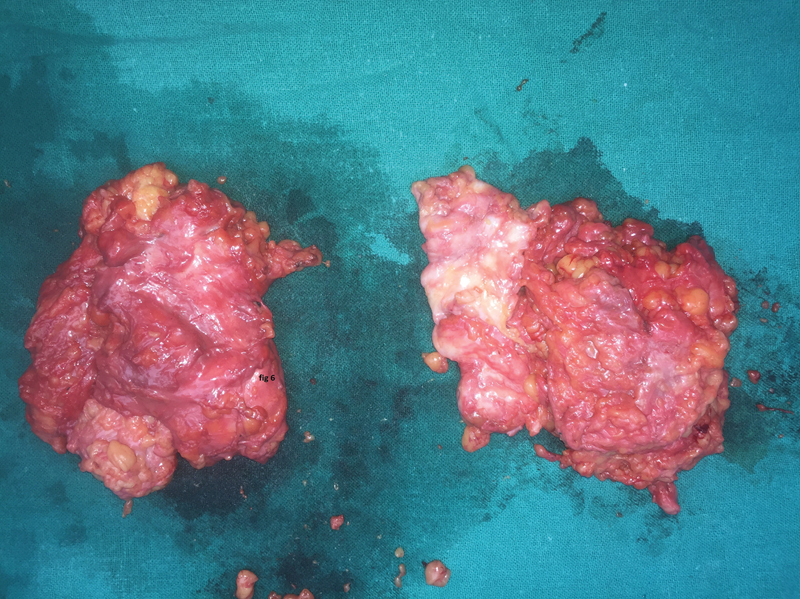
Intraoperative picture showing excised gland.
Fig. 4.

Immediate postoperative picture of patient.
Fig. 5.

Postoperative picture at 3 months.
Discussion
Gynecomastia is a benign condition that involves enlargement of male breast tissue. There is a rubbery or firm mass extending concentrically and symmetrically from the nipple. 1 2 3 4 It is the most common breast condition in males that is usually bilateral in nature but may be unilateral also. 2 3 4 It can be true or pseudogynecomastia. Pseudogynecomastia involves fat deposition without glandular proliferation that is more commonly seen in obese men. 3 5
Simon et al in 1973 classified gynecomastia into three grades depending on the amount of breast tissue and loose skin on top of the breast. 6
The prevalence of gynecomastia varies between 32 and 65%, due to use of different methods used for assessment and the analysis of males of different ages and with different lifestyles, whereas autopsy data suggest a prevalence of 40%. 7 Koch et al 8 in their study done in 2020 in Denmark observed that the prevalence of gynecomastia has drastically increased in the last two decades due to many reasons especially due to sex hormone-related imbalances either naturally or by external use.
Goldman et al in their study reported the emerging epidemic of AAS use despite their well-known adverse effects. 9
This rise in prevalence of gynecomastia can be attributed to rising trend of increased consumption of anabolic steroids in young population.
Various etiological factors for gynecomastia can be secondary to drugs, systemic illness like chronic liver disease, hypothyroidism hypogonadism, testicular or adrenal neoplasia, androgen resistance syndrome, familial aromatase excess, and estrogen producing Sertoli cell tumor. Medications account for 25% of the cases of gynecomastia. 5 7 In a study by Sreelesh et al, 10 most common etiological factor was found to be hormonal imbalance (47.95%). Majumder 11 in his study demonstrates the role of estrogen in breast development in patients seeking gender reaffirmation. AAS consumption presents a major cause in the development of gynecomastia. It is converted into estrogen like compound within body and triggers breast tissue enlargement. Steroid consumption in gynecomastia patients is prone to underestimation just like prevalence of human immunodeficiency virus (HIV) and mental illness because of low social acceptance regarding steroid intake in youngsters. Social stigma is seen as a major herald in true estimation of few risk factors like steroid consumption and diseases like HIV and mental illness. In this study, we found that a large proportion of patients (26 out of 71) change their history regarding the steroid consumption in postoperative period. Reason for this high acceptance is attributed to the confidence/repo developed with doctor due to achievement of desired results by patient.
So, young patients who are in body building profession or having the high BMI are more likely to have the history of steroid abuse to meet their demands. Also, intraoperative finding of less lipoaspirate fat is also associated with steroid consumption in gynecomastia patient.
Treatment of gynecomastia involves nonsurgical and surgical methods. Nonsurgical management involves the discontinuation of the culprit agent or hormonal therapy depending on the etiology. Surgery is indicated in long-standing gynecomastia or patients who are nonresponder to medical management. Gynecomastia associated with steroid is likely to resolve spontaneously on withdrawal of the culprit drug. If it persists for more than 1 year, instances of complete regression are low, due to the predominance of dense fibrous tissue. 2 12
de Luis 13 et al in their study in Spain concluded that there is high prevalence of gynecomastia in the people having the history of anabolic steroid consumption and also observed that there was high remission rate of gynecomastia in the patients who stop the steroid consumption and start taking tamoxifen. In another study, Kanakis 14 et al recommended watchful waiting and discontinuation of substance in patients with any underlying pathology associated to gynaecomastia. Surgery is recommended for patients with long-term gynecomastia.
In our study, AAS-associated gynecomastia shows resolution of symptoms with mere stoppage of drug intake, while few failed to regress completely and required surgery. AAS-associated gynecomastia can resolve spontaneously on stoppage of the drugs. Surgery is not always indicated in AAS-associated gynecomastia. It is done in patients who fail to respond to wait and watch. Also, surgery in AAS-associated gynecomastia involves intraoperatively extensive dissection and meticulous hemostasis as these patients are having more of the glandular component.
Limitations
This study does not include any laboratory testing to assess the steroid intake in patients.
Conclusion
The real prevalence of AAS-associated gynecomastia is much higher than the apparent one. Patients with high BMI, athletic body, and history of recent weight gain should raise the suspicion of anabolic steroid intake. These patients can be kept under observation with suppression of anabolic steroid intake. Surgery is not always indicated in AAS-associated gynecomastia. If gynecomastia persisted, surgery necessitates and it involves meticulous intraoperative hemostasis and careful glandular excision to minimize recurrence and achieve low complication rates.
Footnotes
Conflict of Interest None declared.
References
- 1.Braunstein G D. Clinical practice. Gynecomastia. N Engl J Med. 2007;357(12):1229–1237. doi: 10.1056/NEJMcp070677. [DOI] [PubMed] [Google Scholar]
- 2.Carlson H E. Approach to the patient with gynecomastia. J Clin Endocrinol Metab. 2011;96(01):15–21. doi: 10.1210/jcem.96.9.zeg15a. [DOI] [PubMed] [Google Scholar]
- 3.Johnson R E, Kermott C A, Murad M H. Gynecomastia - evaluation and current treatment options. Ther Clin Risk Manag. 2011;7:145–148. doi: 10.2147/TCRM.S10181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Daniels I R, Layer G T. Gynaecomastia. Eur J Surg. 2001;167(12):885–892. doi: 10.1080/110241501753361550. [DOI] [PubMed] [Google Scholar]
- 5.Barros A C, Sampaio MdeC. Gynecomastia: physiopathology, evaluation and treatment. Sao Paulo Med J. 2012;130(03):187–197. doi: 10.1590/S1516-31802012000300009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Simon B E, Hoffman S, Kahn S. Classification and surgical correction of gynecomastia. Plast Reconstr Surg. 1973;51(01):48–52. doi: 10.1097/00006534-197301000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Rahmani S, Turton P, Shaaban A, Dall B. Overview of gynecomastia in the modern era and the Leeds Gynaecomastia Investigation algorithm. Breast J. 2011;17(03):246–255. doi: 10.1111/j.1524-4741.2011.01080.x. [DOI] [PubMed] [Google Scholar]
- 8.Koch T, Bräuner E V, Busch A S, Hickey M, Juul A. Marked increase in incident gynecomastia: a 20-year National Registry Study, 1998 to 2017. J Clin Endocrinol Metab. 2020;105(10):dgaa440. doi: 10.1210/clinem/dgaa440. [DOI] [PubMed] [Google Scholar]
- 9.Goldman A L, Pope H G, Bhasin S. The health threat posed by the hidden epidemic of anabolic steroid use and body image disorders among young men. J Clin Endocrinol Metab. 2019;104(04):1069–1074. doi: 10.1210/jc.2018-01706. [DOI] [PubMed] [Google Scholar]
- 10.Sreelesh L S, Rajan S, Anu A K. Etiopathological factors associated with gynecomastia patients seeking surgical correction in the South Indian population. Indian J Plast Surg. 2022;55(04):364–367. doi: 10.1055/s-0042-1759498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Majumder A. Endocrine therapy of adult gender-incongruent individuals seeking gender reaffirmation. Indian J Plast Surg. 2022;55(02):149–155. doi: 10.1055/s-0042-1749406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bhasin S. Vol. 11. Philadelphia: Saunders Elsevier; 2008. Testicular disorders; pp. 669–74. [Google Scholar]
- 13.de Luis D A, Aller R, Cuéllar L A, Terroba C, Romero E.Anabolizantes esteroideos y ginecomastia. Revisión de la literatura[Anabolic steroids and gynecomastia. Review of the literature]An Med Interna 20011809489–491. [PubMed] [Google Scholar]
- 14.Kanakis G A, Nordkap L, Bang A K et al. EAA clinical practice guidelines-gynecomastia evaluation and management. Andrology. 2019;7(06):778–793. doi: 10.1111/andr.12636. [DOI] [PubMed] [Google Scholar]


