ABSTRACT
The classic paternalist medicine in nephrology has been modified to a shared decision-making model that clearly offers a benefit in patients with kidney disease. One of the cornerstones of shared treatment decision in patients with kidney failure is the understanding of kidney disease. As kidney disease is silent until advanced stages and is also an entity with a complex pathophysiology with little knowledge in the general population, its presence and understanding are difficult for most people. Health literacy (HL) plays a crucial role in the care of patients with kidney disease and the shared treatment decision. Limited HL has been associated with inefficient use of health services, non-compliance of medications, worse quality of life and increased mortality. In this review, we will address the importance of low HL in nephrology in terms of diagnosis, measurement, its effect on shared decision-making and how to increase it in people with kidney disease.
Keywords: chronic kidney disease, health literacy, kidney failure, renal replacement therapy, shared decision-making
INTRODUCTION
Low HL is the lack of understanding by individuals of the communications provided by care givers, providers, and other constituents of a healthcare organization not allowing the successful transfer, understanding, and application of information to make informed health decisions that promote and maintain good health [1–3]. The prevalence of limited HL is higher among the elderly, minorities, and those with lower socioeconomic status including income and education [4]. Estimates suggest that between 30% and 60% people in Europe have low or very low HL [5]; this means that they struggle to read and understand health content intended for the public, to know how to act on this information, which health services to use, and when to use them. The few available studies report a prevalence of low HL as high as 50% among patients receiving dialysis care [6–8], but a significantly lower proportion of transplant recipients (14%) [9]. All this suggests that similar observations were also made outside Europe [10, 11].
On the other hand, the prevalence of patients with chronic kidney disease (CKD) is increasing dramatically, becoming a major health problem worldwide [12, 13]. In fact, CKD is known to be associated with an increased risk of cardiovascular morbidity, premature mortality, and decreased health-related quality of life [14], which represent a great challenge for health polices and finances, especially in the management of advanced CKD and renal replacement therapy (RRT) such as dialysis, transplantation, or conservative management. Patients with CKD must follow appropriate dietary restrictions, adhere to complex medication regimens [15], make decisions about RRT, and follow multiple appointments in the health care system. Despite having data on methods to delay disease progression, renal outcomes are suboptimal in part related to patient factors. Of these, there is increasing evidence that HL plays an important role in the care of patients with kidney failure disease [16–18], as well as in shared decision-making strategies and the promotion of self-care improves kidney patient satisfaction and health [19]. The potential of communication-related inventions to enhance understanding among those with HL limitations and positive impact on clinical outcomes has fueled a rapid expansion of research on HL, especially in populations with chronic diseases [20]. It is known that limited HL is associated with less efficient use of health services in the general population, greater difficulty in the medication's compliance, poorer quality of life, and a higher mortality [20, 21]. A systematic review was published in 2018 that included 29 studies with a total of 18 300 patients (4367 non-dialysis CKD; 13 202 dialysis; 390 kidney transplants; 341 unspecified) reporting solid evidence of the causal effects of literacy in health on the results of patients with CKD, suggesting associations with adverse clinical events, increased healthcare use and mortality [8].
Taylor et al. reported a limited prevalence of HL in incident dialysis, incident transplant, and a transplant waiting list patients of 20%, 15%, and 12%, respectively. Limited HL was independently associated with low socioeconomic status, limited knowledge of the local language, and comorbidity. However, patients on the transplant waiting list, preemptive transplantation, and living donor transplantation were associated with higher HL [9]. Subsequently, in another study published by the same author, they demonstrated that limited HL was associated with reduced access to kidney transplant regardless of patient demographics, socioeconomic status, and comorbidity [22]. In the current review, we will address the consequences of low HL in nephrology, its detection, measurement, the considerations on health literacy problems in shared decision-making, and how to increase HL in nephrology.
HEALTH LITERACY IN NEPHROLOGY
Despite the recognition of low HL as a key component of kidney disease care [16], current reports are limited by small sample sizes and the lack of trials testing HL intervention strategies to improve outcomes in this population [23].
How to measure health literacy
Different standardized instruments to measure HL in populations and individuals have been reported [8, 24]. Shah JM et al. developed an exhaustive tool for each health center clinical scenario that seems like a reliable methodology [25]. However, the personnel, time, and physical resources required to develop and assess HL using standardized measures are constant comprehensive reported limitations. This may be an essential explanation for the narrow application in nephrology practice.
Two frequently reported assessments (Table 1), the rapid estimate of adult literacy in medicine (REALM) [26–29] and the test of functional health literacy in adults (TOFHLA) [30], must be performed by trained personnel and may take up to 20 minutes to complete. The shortened version (S-TOFHLA) includes 36 reading comprehension items and takes ∼7 minutes to complete [31]. The Newest Vital Sign (NVS) includes a six-item assessment of reading and comprehension from an ice cream nutrition label, which takes up to 6 minutes to complete. By contrast, the three-item brief health literacy screen (BHLS) [28], requiring 1–2 minutes or less, has demonstrated validity across diverse patient populations and has been associated with relevant clinical outcomes, including hospitalizations and death [32–36]. However, to our knowledge, the validity of the BHLS and other HL questionnaires has not been confirmed in patients with kidney failure. Our opinion, according to this literature review, is that HL should not be systematically screened in patients. It is preferable to offer everyone information in a friendly, non-stigmatizing way as a matter of routine. From our point of view, the most appropriate way to ensure that the health content will be understood by patients is to involve them in the development and testing of that health information.
Table 1:
Health literacy tools-format and their main evaluation results for CKD patients.
| HL tool and format | Non-dialysis CKD | Dialysis CKD | Kidney transplant | |
|---|---|---|---|---|
| REALM | 125 words (66 in more commonly used form) | 18% prevalence of limited HL 401 CKD patients, stage 1–5 HL is directly related to knowledge of dietary restrictions [55] |
16–32% prevalence of limited HL 740 hemodialysis patients [6, 7] | A specific short form is developed for these patients (REALM-T) |
| REALM-SF | 7 words | Not evaluated in nephrology patients | ||
| REALM-T | 69 words | Not evaluated in these clinical areas | Significantly predicted whether a patient was listed for transplant [56] | |
| TOFHLA | 50 reading + 17 numeracy items | Not evaluated in nephrology patients [31] | ||
| S-TOFHLA | 36 reading comprehension items | 28% prevalence of limited HL, correlated with poor clinical outcomes 2340 CKD patients HL is directly related to knowledge of dietary restrictions [57] |
32% prevalence of limited HL 62 hemodialysis patients [58] | Inadequate HL had 78% lower hazard of referral for transplant work up [58] |
| BHLS | 3 questions, all graded 1–5 | Not evaluated in nephrology patients | ||
| NVS | 6 items, an ice cream nutrition label | Limited HL correlated with poor clinical outcomes 150 CKD patients HL is directly related to knowledge of dietary restrictions [59] |
Significantly predicted whether a patient was listed for transplantation, and actually received a transplant [56] | |
| DMCAT | 6 questions and a scenario | Specific tool for transplant patients | Significantly predicted whether a patient was listed for transplant, and actually received a transplant [56] | |
HL: health literacy; CKD: chronic kidney disease; REALM: Rapid Estimate of Adult Literacy in Medicine; REALM-SF: REALM short form; REALM-T: REALM modified for the transplant population; TOFHLA: Test Of Functional Literacy in Adults; S-TOFHLA: the shortened version of TOFHLA; BHLS: Brief Health Literacy Screen; NVS: Newest Vital Sign; DMCAT: Decision-Making Capacity Assessment Tool.
Health literacy in different nephrology areas
For patients attended at the different nephrology areas, low HL is associated with less knowledge of their health condition, less participation in self-care, a higher burden of disease, and a higher risk of hospitalizations and mortality [10, 20]. Taylor et al. [22], report on a systematic review (cohort studies) that limited HL on dialysis population was significantly and independently associated with hospitalizations [Risk Ratio (RR) 1.55, 95% Confidence Interval (CI) 1.03–2.34], emergency department use (RR 1.37, 95% CI 1.01–1.86), missed dialysis sessions (RR 2.14, 95% CI 1.10–4.17), cardiovascular events (RR 1.68, 95% CI 1.10–2.58), and mortality (RR 1.65, 95% CI 1.28–2.12). For this systematic review, in non-dialysis populations, patients with limited HL were found to have significantly lower disease knowledge and understanding of test results after adjustment for educational level. Additionally, cognitive impairment is common in dialysis patients, associated with less successful self-care and likely contributes to an individual lack of HL skill [37]. Low HL has been recognized as a potential negative factor in patient-centered kidney disease care, and reports elsewhere provide a comprehensive discussion [16, 38].
DAY-TO-DAY PROBLEMS RELATED TO LOW HEALTH LITERACY IN NEPHROLOGY
Nephrology care and recommendations to patients with CKD to delay the progression of kidney disease and reduce risk of cardiovascular complications are increasingly provided by a team of different professionals [39]. A very important role to consider is the importance of recognizing CKD and taking an active role in their daily life care by engaging in activities to manage their condition. Low HL affects behaviors needed to develop self-management skills, which may delay an appropriate response to tackle the risk factors for progression of the disease [40]. It is known that CKD is a silent entity that hardly produces symptoms and signs in advanced stages causing a negative effect on the disease in terms of delaying its diagnosis and worsening its prognosis. The self-management of CKD requires more information about the complexity of kidney disease; thus, it is important to improve HL through various techniques or strategies to help the patient and family with the awareness of kidney disease [41]. These approaches may be a tool to implicate the person with CKD in decisions when kidney disease reaches its final stage. Unfortunately, the limited HL of patients with CKD has been associated with adverse clinical events, increased healthcare visits and mortality [8]. Added to this aspect, the advanced age of our patients increases the difficulty to understand kidney disease and therefore make decisions. More recently, older patients with comorbidities who started a hemodialysis program were reported to have higher mortality; poorer survival and/or quality of life compared with patients who did not start a dialysis program [42–45]. Therefore, the decision to initiate dialysis in this population requires a nephrological-geriatric evaluation together with family support and trained nephrology nursing in a nephrology unit, using HL, and applying shared decision-making (SDM) [45]. Patients with limited HL may lack understanding, making them less likely to discuss transplantation with family and friends, affecting recruitment of living donors, who may also have lower HL and health contraindications related to shared social disadvantages [22]. Development of an integrated care unit for patients with advanced CKD could improve information about the disease, thereby improving decision-making ability to initiate RRT.
CONSIDERATIONS ON HEALTH LITERACY PROBLEMS IN SHARED DECISION-MAKING
Increasing patient engagement and participation in healthcare is considered a priority in the policy agenda. SDM is a process through which clinicians and patients make healthcare choices together, representing the crux of people‐centered care [46]. However, there could be significant variability in how clinicians provide information. Decision support interventions, also known as patient decision aids (PDAs), are tools that can facilitate SDM by standardizing information. They explicitly state the decision that needs to be considered and help patients clarify their values and preferences while offering evidence-based information about the options’ risks, benefits, and outcome probabilities [46, 47, 47].
A person's HL status affects their ability to utilize health information and services and can affect their health outcomes [48]. There is a risk that SDM benefits people who are educated, empowered, and able to express their needs and preferences. Evidence suggests that younger patients, women, and those with higher socioeconomic status are more likely to assume an active role in SDM [47]. Patients with limited HL may be less able to participate in medical decision-making and use PDAs effectively unless special attention has been paid to their specific needs [48]. In that sense, a SDM process not adapted to disadvantaged groups needs could increase health inequalities since engaging patients in this process requires knowledge, confidence, self-efficacy, and higher levels of HL [47].
Nutbeam's multi-level model of HL provides a valuable framework to reflect the skills and competencies that patients can develop to have greater independence in health decision-making [49, 50]. This hierarchy model includes three levels: (i) functional HL, which refers to the basic reading and writing skills to understand and obtain health information and apply knowledge of health conditions and services; (ii) interactive HL, which refers to communicative and personal social skills, such as motivation and self-confidence, that can be used to participate actively, extract and discuss health information; and (iii) critical HL, which refers to cognitive and social skills to critically assess the applicability of health information to personal situations and use this information to exert greater control over life situations and make informed decisions [48, 49]. Patients can move along these three-level HL pathways as they increase their knowledge, understand health conditions, and actively participate in discussions with healthcare professionals.
Considering the strong link between HL and SDM, McCaffery et al. proposed that these levels could also be used to reflect the needs of limited HL patients to use PDAs effectively and to engage in SDM activities [48] (Fig. 1). For the first level related to understanding, health information authors reported that limited HL was clearly associated with more inadequate patient health knowledge. The effect of numeracy on the accuracy of risk perception and knowledge has mixed results. For the second level related to communicating with health care professionals, the authors reported that limited HL was related to higher decisional uncertainty and regret. However, the effect on decision confidence was less clear with mixed results. For the third level, related to clarifying personal values and thinking critically to make an informed decision, the authors reported that patients with limited HL were consistently less likely to want to be involved in decision-making than those with higher literacy. Also, lower levels of communicative HL were associated with less question-asking and lower patient-centered communication [48] (Fig. 1).
Figure 1:
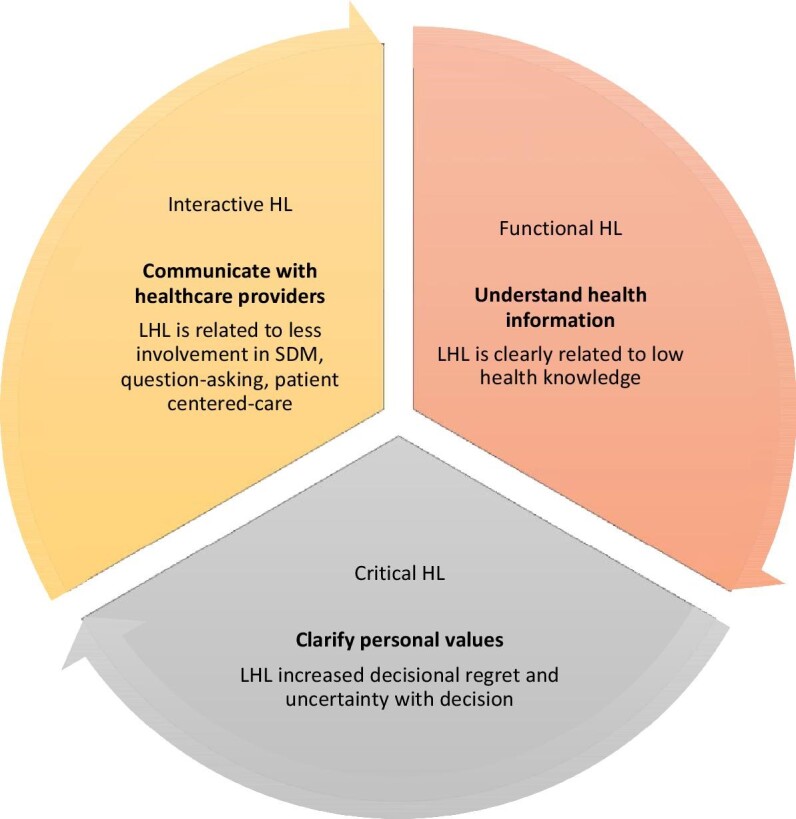
Problems related to limited health literacy that could impact share decision-making. HL: health literacy; LHL: limited health literacy; SDM: shared decision-making.
HOW TO ENSURE ADEQUATE SHARED DECISION-MAKING
Health care professionals working in SDM process and PDAs development should pay special attention to limited HL to remove literacy-related barriers in clinical practice to support meaningful patient engagement in decision-making. Patients require skills to participate in the SDM process effectively and use PDAs, as providers need skills to engage with their patients and develop quality and suitability tools. These skills should be delivered in a structured setting, such as education and training programs [49]. The US Preventive Services Task Force (USPSTF) defines the SDM process as the following five stages in which a patient: (i) understands the nature of the disease; (ii) becomes aware of available options and their risks and benefits; (iii) considers their values and preferences; (iv) participates in decision-making; and (v) makes a decision based on their own preferences and values [51]. Based on the USPSTF definition of SDM and considering the three-level model of Nutbeam [50] we summarize for every stage of the decision-making process the skills and competencies that patients who face health decisions need to know, as well as the recommendations and guidance addressed to healthcare professionals to ensure an adequate SDM process (Table 2).
Table 2:
Patient skills and competencies and recommendations for healthcare professionals for every stage of the SDM process.
| Functional health literacy | Critical health literacy | Interactive/communicative health literacy | |||
|---|---|---|---|---|---|
| Understand the disease | Understand the options | Clarify values | Participate in SDM | Make the decision | |
| Skills and competencies for patients | Understanding of written and spoken medical terminology about the disease and its management | Understanding there are risks and benefits to different options and making sense of the likelihood of their occurring | Identifying and clarification values and preferences for possible outcomes and weight this with information on the likelihood of each outcome occurring | Participating in health decisions, feeling able to ask and have the confidence to express their preferences and ask questions to health professionals | Implementing a shared decision and enhancing patient activation |
| Guidance and recommendations for health professionals | • Use of plain language • Avoid the use of medical jargon • Use clear voice • Use a large font size and clear style (e.g. 12 points or higher and sans serif) • Avoid the use of italic and letters • Avoid the use of acronyms and abbreviations • Incorporate illustrations, cartoons, and videos |
• Express probabilistic information as natural frequencies (e.g. 1 in 100) • Use a consistent denominator • Present the information in a variety of formats |
• Enhance active forecasting (imagining future health states or events) using imagery and entertainment education techniques • Use personal stories from patients |
• Explain to patients and family that choice and the opportunity to participate are available to them if they want it • Use prompt question lists (questions for patients to ask their doctor) to encourage patient participation (e.g. ‘Ask Me 3’ question prompt list) |
• Design interventions to enhance patient activation, focusing on self-efficacy, empowerment, and motivation • Remove practical and financial barriers |
| Involve patients of all literacy levels in the development of the process | |||||
Clinicians should see SDM as an opportunity to include and empower patients with limited HL to benefit all groups and reduce health inequalities. For patients to successfully participate in decision-making, they need to integrate all levels of HL skills (functional, interactive, and critical) to communicate effectively [52]. Simplifying information is necessary but not sufficient to achieve active patient participation in decision-making. In that sense, patients need cognitive and social skills to express personal values and preferences and to contextualize and critically evaluate information to make a decision that aligns with their values and preferences [49]. A systematic review of interventions designed to support SDM in patients from disadvantaged groups, including limited HL, showed significant improvement in knowledge, informed choice, level of participation in decision-making, and reduced decisional conflict. There was an important variability in the interventions, ranging from computerized, booklet, or video/DVD decision aids to communication skills workshops or education sessions [47].
Health professionals related to SDM practices need to ensure they attend not only to the issues of comprehension but also to values, preferences, clarification, and the processes involved in the decision-making encounter. In that sense, designers of PDAs need to ensure that SDM practices and tools can be accessed and understood by adults across the HL spectrum [48]. From our point of view, one of the best strategies to ensure an appropriate SDM process for patients with limited HL is the involvement of patients in the cocreation and development of PDAs from the beginning, as well as following guidelines for developing low literacy materials (Table 2). We were not able to find specific evidence of the development and evaluation of limited-literacy PDAs in nephrology. Nevertheless, one practical example in another chronic disease is the design of a limited-literacy PDA about rheumatoid arthritis developed through a collaborative process involving patients, clinicians, designers, decision-aid, and HL experts. The use of this PDA improved knowledge and reduced decisional conflict among patients with rheumatoid arthritis. Enhancing knowledge and patient engagement with decision support tools may lead to choices better aligned with patients’ values and preferences [53, 54].
HOW TO SHIFT TOWARD MORE HEALTH LITERACY IN NEPHROLOGY
To our knowledge, the literature supporting the use of tools to assess HL in CKD patients is limited; the availability of these standardized instruments has been expanding rapidly in the last years; however, abbreviated or short forms reduce the main limitations found in the evidence. Furthermore, more research is needed to validate and evaluate the effectiveness of these tools. Understanding HL assessment among CKD patients for a better SDM pathway is needed to advance its appraisal within existing studies and research. Larger cohorts and clinical trials are needed. Healthcare professionals must receive adequate education and training programs, and using these tools effectively must improve their competencies to guarantee the SDM pathway. Understanding the disease, risk, and benefits, and considering the patient's competence and participation in their own decision process is needed to enhance higher decision adherence and correct use of assistance. Future studies of CKD populations should focus on the effect of limited HL on referral to nephrology services, dialysis modality choice, dialysis quality measures, adverse events on dialysis, and success with home therapies, including conservative treatments, peritoneal dialysis, and transplantation.
Measuring and improving the HL of CKD patients to adequate levels for the best SDM process should sketch the future research path. Moreover, all development processes and research for these HL and SDM tools should consider differences in patient characteristics (adequate and limited HL) and consider the development of different tools for different HL level patients. The commitment to reach these milestones, which aspire to equity in health system access for these patients, must include all CKD patients at all HL levels, healthcare stakeholders (nephrology healthcare professionals, general practitioners, hospital administrators), and development policy makers for patients centered care policy. Another major focus point is to develop a policy to address patient-centered outcomes.
In conclusion, HL in nephrology needs to be increased to promote the successful transfer, understanding, and application of information to ensure proper SDM. The identification and measurement of HL in patients with kidney disease will lead to a subsequent shift to improve and develop adequate tools for different HL levels helping our patients in the understanding of their disease. One expects that this strategy will increase the patient's compliance, disease awareness, equity, and access to different renal replacement modalities such as hemodialysis, dialysis peritoneal, home-based-dialysis, and kidney transplantation. The time of paternalist medicine in nephrology is over; for that reason, HL should be measured and improved to promote the knowledge of the patient that will allow the adequate shared decision for his/her kidney disease.
ACKNOWLEDGEMENTS
We are grateful to Jordi José Ortiz for reviewing the English grammar.
Contributor Information
Néstor Toapanta, Department of Nephrology, Vall d'Hebron University Hospital, Barcelona, Spain.
Karla Salas-Gama, Quality, Process and Innovation Direction, Vall d'Hebron University Hospital, Barcelona, Spain; Health Services Research Group, Vall d'Hebron Institut de Recerca (VHIR), Vall d'Hebron Hospital University, Vall d'Hebron Barcelona Hospital Campus, Barcelona, Spain; PhD candidate at the Methodology of Biomedical Research and Public Health program, Universitat Autònoma de Barcelona (UAB), Barcelona, Spain.
Percy Efrain Pantoja, Quality, Process and Innovation Direction, Vall d'Hebron University Hospital, Barcelona, Spain; Health Services Research Group, Vall d'Hebron Institut de Recerca (VHIR), Vall d'Hebron Hospital University, Vall d'Hebron Barcelona Hospital Campus, Barcelona, Spain.
María José Soler, Department of Nephrology, Vall d'Hebron University Hospital, Barcelona, Spain.
FUNDING
This article was published as part of a supplement made possible by Fresenius Medical Care.
DATA AVAILABILITY STATEMENT
The data underlying this article are available in the article and in its online supplementary material.
CONFLICT OF INTEREST STATEMENT
M.J.S. reports honorarium for conferences, consulting fees, and advisory boards from Astra Zeneca, NovoNordsik, Esteve, Vifor, Bayer, Mundipharma, Ingelheim Lilly, Jansen, ICU Medical, Fresenius, Travere therapeutics, and Boehringer. She is the former Editor-in-Chief of Clinical Kidney Journal.
REFERENCES
- 1. Cavanaugh KL, Osborn CY, Tentori Fet al. . Performance of a brief survey to assess health literacy in patients receiving hemodialysis. Clin Kidney J 2015;8:462–8. 10.1093/ckj/sfv037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. WHO . Improving health literacy. https://www.who.int/activities/improving-health-literacy
- 3. Nielsen-Bohlman L, Panzer AM, Kindig DA, eds. Health Literacy. National Academies Press; 2004; doi: 10.17226/10883. [DOI] [PubMed] [Google Scholar]
- 4. Kutner G, Jin P. The Health Literacy of America's Adults: Results From the 2003 National Assessment of Adult Literacy; 2003; [Google Scholar]
- 5. Sørensen K, Pelikan JM, Röthlin Fet al. . Health literacy in Europe: comparative results of the European Health Literacy Survey (HLS-EU). Eur J Pub Health 2015;25:1053–8. 10.1093/eurpub/ckv043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Green JA, Mor MK, Shields AMet al. . Prevalence and demographic and clinical associations of health literacy in patients on maintenance hemodialysis. Clin J Am Soc Nephrol 2011;6:1354–60. 10.2215/CJN.09761110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cavanaugh KL, Wingard RL, Hakim RMet al. . Low health literacy associates with increased mortality in ESRD. J Am Soc Nephrol 2010;21:1979–85. 10.1681/ASN.2009111163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Taylor DM, Fraser S, Dudley Cet al. . Health literacy and patient outcomes in chronic kidney disease: a systematic review. Nephrol Dial Transplant 2018;33:1545–58. 10.1093/ndt/gfx293. [DOI] [PubMed] [Google Scholar]
- 9. Taylor DM, Bradley JA, Bradley Cet al. . Limited health literacy in advanced kidney disease. Kidney Int 2016;90:685–95. 10.1016/j.kint.2016.05.033. [DOI] [PubMed] [Google Scholar]
- 10. Green JA, Mor MK, Shields AMet al. . Associations of health literacy with dialysis adherence and health resource utilization in patients receiving maintenance hemodialysis. Am J Kidney Dis 2013;62:73–80. 10.1053/j.ajkd.2012.12.014. [DOI] [PubMed] [Google Scholar]
- 11. Pollock JB, Jaffery JB. Knowledge of phosphorus compared with other nutrients in maintenance dialysis patients. J Ren Nutr 2007;17:323–8. 10.1053/j.jrn.2007.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jha V, Modi GK. Getting to know the enemy better-the global burden of chronic kidney disease. Kidney Int 2018;94:462–4. 10.1016/j.kint.2018.05.009. [DOI] [PubMed] [Google Scholar]
- 13. Luyckx VA, Tonelli M, Stanifer JW. The global burden of kidney disease and the sustainable development goals. Bull World Health Organ 2018;96:414–422C. 10.2471/BLT.17.206441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hill NR, Fatoba ST, Oke JLet al. . Global prevalence of chronic kidney disease - a systematic review and meta-analysis. PLoS ONE 2016;11. 10.1371/journal.pone.0158765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lambert K, Mullan J, Mansfield K. An integrative review of the methodology and findings regarding dietary adherence in end stage kidney disease. BMC Nephrol 2017;18. 10.1186/s12882-017-0734-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dageforde LA, Cavanaugh KL. Health literacy: emerging evidence and applications in kidney disease care. Adv Chronic Kidney Dis 2013;20:311–9. 10.1053/j.ackd.2013.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Young BA. Health literacy in nephrology: why is it important? Am J Kidney Dis 2013;62:3–6. 10.1053/j.ajkd.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 18. Elisabeth Stømer U, Klopstad Wahl A, Gunnar Gøransson Let al. . Health Literacy in Kidney Disease: Associations with Quality of Life and Adherence. J Ren Care 2020;46:85–94. 10.1111/jorc.12314. [DOI] [PubMed] [Google Scholar]
- 19. MacManus B, Macdonald J, Matthews Bet al. . Shared decision-making in kidney care: a call to action. J Renal Nursing 2012;4:58–59. 10.12968/jorn.2012.4.2.58. [DOI] [Google Scholar]
- 20. Berkman ND, Sheridan SL, Donahue KEet al. . Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011;155:97–107. 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 21. Skoumalova I, Madarasova Geckova A, Rosenberger Jet al. . Health-related quality of life profiles in dialyzed patients with varying health literacy. a cross-sectional study on Slovak haemodialyzed population. Int J Public Health 2021;66:585801. 10.3389/ijph.2021.585801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Taylor DM, Bradley JA, Bradley Cet al. . Limited health literacy is associated with reduced access to kidney transplantation. Kidney Int 2019;95:1244–52. 10.1016/j.kint.2018.12.021. [DOI] [PubMed] [Google Scholar]
- 23. Taylor DM, Fraser SDS, Bradley JAet al. . A systematic review of the prevalence and associations of limited health literacy in CKD. Clin J Am Soc Nephrol 2017;12:1070–84. 10.2215/CJN.12921216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Jain D, Green JA. Health literacy in kidney disease: review of the literature and implications for clinical practice. World J Nephrol 2016;5:147. 10.5527/wjn.v5.i2.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shah JM, Ramsbotham J, Seib Cet al. . A scoping review of the role of health literacy in chronic kidney disease self-management. J Ren Care 2021;47:221–33. 10.1111/jorc.12364. [DOI] [PubMed] [Google Scholar]
- 26. Stafford JD, Goggins ER, Lathrop Eet al. . Health literacy and associated outcomes in the postpartum period at Grady Memorial Hospital. Matern Child Health J 2021;25:599–605. 10.1007/s10995-020-03030-1. [DOI] [PubMed] [Google Scholar]
- 27. Diemer FS, Haan YC, Nannan Panday Ret al. . Health literacy in Suriname. Soc Work Health Care 2017;56:283–93. 10.1080/00981389.2016.1277823. [DOI] [PubMed] [Google Scholar]
- 28. Davis TC, Long SW, Jackson RHet al. . Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med 1993;25:391–5. [PubMed] [Google Scholar]
- 29. Davis TC, Crouch MA, Long SWet al. . Rapid assessment of literacy levels of adult primary care patients. Fam Med 1991;23:433–5. [PubMed] [Google Scholar]
- 30. Parker RM, Baker DW, Williams Met al. . The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. J Gen Intern Med 1995;10:537–41. 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 31. Baker DW, Williams MV, Parker RMet al. . Development of a brief test to measure functional health literacy. Patient Educ Couns 1999;38:33–42. 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 32. Sørensen K, Pelikan JM, Röthlin Fet al. . Health literacy in Europe: comparative results of the European health literacy survey (HLS-EU). Eur J Public Health 2015;25:1053–8. 10.1093/eurpub/ckv043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sarkar U, Schillinger D, López Aet al. . Validation of self-reported health literacy questions among diverse english and spanish-speaking populations. J Gen Intern Med 2011;26:265–71. 10.1007/s11606-010-1552-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med 2004;36:588–94. [PubMed] [Google Scholar]
- 35. Chew LD, Griffin JM, Partin MRet al. . Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med 2008;23:561–6. 10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Peterson PN, Shetterly SM, Clarke CLet al. . Health literacy and outcomes among patients with heart failure. J Am Med Assoc 2011;305:1695–701. 10.1001/jama.2011.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Murray AM, Knopman DS. Cognitive impairment in CKD: no longer an occult burden. Am J Kidney Dis 2010;56:615–8. 10.1053/j.ajkd.2010.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Cavanaugh KL. Prioritizing patient-centered care implementation and research for patients with kidney disease. Semin Dial 2015;28:131–40. 10.1111/sdi.12326. [DOI] [PubMed] [Google Scholar]
- 39. Schrauben SJ, Cavanaugh KL, Fagerlin Aet al. . The relationship of disease-specific knowledge and health literacy with the uptake of self-care behaviors in CKD. Kidney Int Rep 2020;5:48–57. 10.1016/j.ekir.2019.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. MacKey LM, Doody C, Werner ELet al. . Self-management skills in chronic disease management: what role does health literacy have? Med Decis Making 2016;36:741–59. . [DOI] [PubMed] [Google Scholar]
- 41. Havas K, Douglas C, Bonner A. Meeting patients where they are: improving outcomes in early chronic kidney disease with tailored self-management support (the CKD-SMS study). BMC Nephrol 2018;19. 10.1186/s12882-018-1075-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Martínez Echevers Y, Toapanta Gaibor NG, Nava Pérez Net al. . Survival of patients ≥70 years with advanced chronic kidney disease: dialysis vs. conservative care. Nefrologia 2016;36. 10.1016/j.nefro.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 43. Verberne WR, Tom Geers ABM, Jellema WTet al. . Comparative survival among older adults with advanced kidney disease managed conservatively versus with dialysis. Clin J Am Soc Nephrol 2016;11:633–40. 10.2215/CJN.07510715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Brown MA, Collett GK, Josland EAet al. . CKD in elderly patients managed without dialysis: survival, symptoms, and quality of life. Clin J Am Soc Nephrol 2015;10:260–8. 10.2215/CJN.03330414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Toapanta N, Comas J, León Román Jet al. . Mortality in elderly patients starting hemodialysis program. Semin Dial 2022;doi: 10.1111/sdi.13114. [DOI] [PubMed] [Google Scholar]
- 46. Stacey D, Légaré F, Lewis K, others. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 2017;4:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Durand MA, Carpenter L, Dolan Het al. . Do interventions designed to support shared decision- making reduce health inequalities? A systematic review and meta-analysis. PLoS ONE 2014;9. 10.1371/journal.pone.0094670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. McCaffery KJ, Holmes-Rovner M, Smith SKet al. . Addressing health literacy in patient decision aids. BMC Med Inform Decis Mak 2013;13:S10. 10.1186/1472-6947-13-S2-S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Muscat DM, Shepherd HL, Nutbeam Det al. . Health literacy and shared decision-making: exploring the relationship to enable meaningful patient engagement in healthcare. J Gen Intern Med 2021;36:521–4. 10.1007/s11606-020-05912-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int 2000;15:259–67. 10.1093/heapro/15.3.259. [DOI] [Google Scholar]
- 51. McCaffery KJ, Smith SK, Wolf M. The challenge of shared decision making among patients with lower literacy: a framework for research and development. Med Decis Making 2010;30:35–44. . [DOI] [PubMed] [Google Scholar]
- 52. Bear RA, Stockie S. Patient engagement and patient-centred care in the management of advanced chronic kidney disease and chronic kidney failure. Can J Kidney Health Dis 2014;1:1–8. 10.1186/s40697-014-0024-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Barton JL, Koenig CJ, Evans-Young Get al. . The design of a low literacy decision aid about rheumatoid arthritis medications developed in three languages for use during the clinical encounter. BMC Med Inform Decis Mak 2014; 10.1186/s12911-014-0104-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Barton JL, Trupin L, Schillinger Det al. . Use of low-literacy decision aid to enhance knowledge and reduce decisional conflict among a diverse population of adults with rheumatoid arthritis: results of a pilot study. Arthritis Care Res 2016;68:889–98. 10.1002/acr.22801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Wright JA, Wallston KA, Elasy TAet al. . Development and results of a kidney disease knowledge survey given to patients with CKD. Am J Kidney Dis 2011;57:387–95. 10.1053/j.ajkd.2010.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Kazley AS, Hund JJ, Simpson KNet al. . Health literacy and kidney transplant outcomes. Prog Transplant 2015;25:85–90. 10.7182/pit2015463. [DOI] [PubMed] [Google Scholar]
- 57. Ricardo AC, Yang W, Lora CMet al. . Limited health literacy is associated with low glomerular filtration in the chronic renal insufficiency cohort (cric) study. Clin Nephrol 2014;81:30–37. 10.5414/CN108062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Grubbs V, Gregorich SE, Perez-Stable EJet al. . Health literacy and access to kidney transplantation. Clin J Am Soc Nephrol 2009;4:195–200. 10.2215/CJN.03290708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Devraj R, Borrego M, Vilay AMet al. . Relationship between health literacy and kidney function. Nephrology 2015;20:360–7. 10.1111/nep.12425. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article are available in the article and in its online supplementary material.


