Abstract
Purpose of Review
To analyze advances in labral reconstruction, and to discuss the literature relating to efficacy, outcomes, and technical considerations of labral reconstruction.
Recent Findings
The available evidence suggests that labral reconstruction is a safe and effective procedure that can improve pain and function in patients with severe and/or complex labral tears. The superiority of labral reconstruction over labral repair is uncertain, and it remains unclear what graft type and technique should be used in labral reconstructions.
Summary
Labral reconstruction assists in restoring the function of the labrum of the hip. It consistently restores stability of the hip joint and demonstrates good clinical outcomes at follow-up. The optimal graft type, technique, and extent are still debated, and more research is needed. Ultimately, despite this uncertainty, labral reconstruction is proving to be a valuable tool for hip preservation specialists.
Keywords: Labral reconstruction, Hip labrum tear, Torn labrum treatment, Hip arthroscopy, Labrum tear outcomes, Labral repair, Labral graft
Introduction
Biomechanics
The acetabular labrum is a crucial component of hip joint biomechanics and synovial fluid dynamics. The labrum increases the contact area between the acetabulum and femoral head from 28.8 to 36.8 cm2, thereby decreasing joint contact forces [1]. Tears in the labrum allow synovial fluid efflux during compression thus increasing stress on articular cartilage [2]. The labrum also acts as a stabilizer of the hip joint, as simulated labral tears in cadaveric models have been shown to increase external rotation and anterior translation [3]. The bulk of evidence indicates that the acetabular labrum is instrumental in maintaining hip fluid mechanics, stability, and appropriate contact pressures.
Primary Labral Reconstruction
Labral repair and correction of the underlying hip joint bony mismatch has become the standard of care in hip arthroscopy for femoroacetabular impingement. However, there are certain scenarios in which the labrum may be injured beyond repair. These scenarios may include the following: (1) labral tissue that is severely calcified or ossified (Fig. 1); and (2) severe attenuation, iatrogenic excision, and/or complex, irreparable tearing of the labrum.
Fig. 1.

Radiograph revealing ossified labrum
There are a small number of authors who have advocated for expanding the indications of primary labral reconstruction [4•]. A bilateral hip arthroscopy study comparing labral repair to primary reconstruction demonstrated lower failure rate in the labral reconstruction group, 30% vs. 0% at a mean follow-up duration of 56 months and 40 months respectively [5]. The proposed rationale for the success of labral reconstruction in this setting is that all of the degenerative labrum and its nociceptive fibers are removed [6••]. However, these results have not been widely replicated and may be subject to bias related to surgeon learning curve [7]. It is generally accepted that labral reconstruction should be utilized in the primary setting only when the labrum is severely injured, ossified, or irreparable.
Labral Reconstruction in the Revision Setting
There are scenarios in the revision setting when satisfactory labral repair is impossible. Long-standing, residual pincer impingement may lead to severe labral injury and poor labral tissue quality. Overly aggressive labral debridement may also cause deficient labral tissue. In these cases, there are a few options to restore labral function. Labral augmentation with autograft or allograft may be used to supplement the injured or diminutive labral tissue after debridement [8]. In labral augmentation, existing labral tissue is preserved with graft tissue placed to provide additional volume to the labrum, in contrast to segmental labral reconstruction, in which the existing labral tissue is debrided prior to graft placement. This technique has shown superior outcomes compared to segmental reconstruction in a select patient population. However, labral augmentation is not always possible due to a lack of healthy labral tissue. Resection of the severely injured portion of the labrum with segmental labral reconstruction has also demonstrated good patient-reported outcomes at 2 years [9]. Circumferential labral reconstruction has the theoretical advantages of restoring the hoop stress capability of the labrum and removing native nociceptive fibers, but has not been shown to be superior to segmental reconstruction in the clinical literature [10, 11]. Hip joint space of ≤ 2 mm has demonstrated a high conversion rate to total hip arthroplasty of 50% at 3 years, making this a contraindication to labral reconstruction [12, 13].
Technical Considerations
Segmental vs. Circumferential Reconstruction Technical Considerations
Labral reconstruction can be performed either circumferentially or segmentally. The segmental labral reconstruction, discussed by Phillipon et al. in 2010, involves a reconstruction of only the damaged portion of the labrum, preserving healthy labral tissue [14]. This technique is advantageous in cases of localized labral damage and typically is performed on the acetabular clockface in the region between 12 and 3 o’clock. Circumferential reconstruction involves replacing a majority of the labrum [15]. Some authors argue that circumferential reconstructions are superior to segmental reconstruction because, unlike segmental reconstructions, they lack junctional points at the interface between native and graft tissue [16]. It has been suggested that these junctional points may compromise the ability of the reconstruction to restore the suction seal of the hip [16]. However, biomechanical studies have shown that circumferential reconstructions also do not restore the suction seal of the hip, leaving the merits of this purported advantage in question [17•]. Transchondral fluid stress and strain may also be more significantly compromised by a circumferential reconstruction [18•]. Therefore, the circumferential approach is typically indicated for cases of extensive labral degeneration or ossification, where a segmental reconstruction would not provide adequate stability [14]. Labral augmentation has also been successfully performed in the clinical setting with 2-year follow-up demonstrating significantly better outcomes as compared to segmental reconstruction when some viable native labral tissue is present [8]. This technique maintains the chondrolabral junction while providing increased labral tissue and should be considered as a reconstruction alternative if diminutive labral tissue is present. Ultimately, when considering the choice of technique, it is important to assess the labrum’s ossification, integrity of the chondrolabral junction, and the extent of tissue loss from pathology or prior surgery, which may contribute to pain and dysfunction and suggest the need for a circumferential reconstructive approach. The decision to perform an augmentation, segmental, or a circumferential reconstruction is typically made intraoperatively, though pre-operative imaging findings of extensive labral ossification and damage may also play a role in assisting pre-operative planning.
Preparation of the Reconstruction Site
The surgical approach to acetabular labral reconstruction first involves a diagnostic hip arthroscopy. Identification of the labral defect and accurate measurement of the size of the defect is necessary to determine the required graft size. To identify the defect, the labrum’s integrity and stability is carefully assessed for the presence of degenerative changes or ossification. Visual inspection typically reveals discoloration, fraying, deficiency, or tears in the labral tissue. A probe can be used to palpate the labrum and assess its stability and mobility, confirming the presence of the defect. Dynamic examination to assess the labral seal can also be utilized intra-operatively to aid in examining labral function. Once the defect is identified, the surgeon may estimate the size of the defect using arthroscopic instrumentation, such as a calibrated probe or a suture length measurement technique, to assist in precise graft sizing.
The defective labral tissue (in the case of a segmental reconstruction or augmentation) or the entirety of the labrum (in the case of a circumferential reconstruction) is debrided using an arthroscopic shaver. If this tissue is ossified, an arthroscopic burr may be required to adequately remove the damaged components. Decortication of the underlying acetabulum may also be performed using a burr. Pilot holes are drilled, and suture anchors are placed at both ends of the reconstruction site, with careful attention being given to avoid drill orientations which may violate the articular surface of the acetabulum (Fig. 2). Further, these anchors should be placed adjacent to the edge of the acetabular rim to help properly restore the native suction seal. Additional anchor points may be made along the central perimeter of the defect based on defect size and surgeon preference (Fig. 3). These suture anchors are typically placed approximately every centimeter, although placement may vary based on the morphology of the acetabular rim. Free ends of the suture anchors are pulled through an anterolateral portal using an atraumatic grasper. Meticulous suture management is a critical aspect of successful labral reconstruction, and care is taken to ensure that the field is clear of suture entanglement and that the suture is marked appropriately according to its origin.
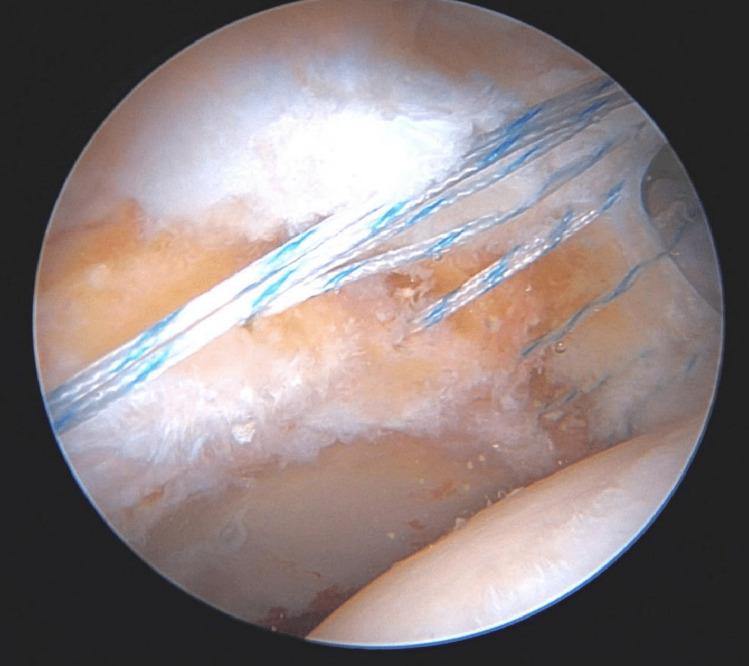
Fig. 2.
Arthroscopic image demonstrating placement of suture anchors at the terminal ends of the reconstruction site. In this case, a segmental reconstruction is being performed
Fig. 3.
Arthroscopic image of a prepared acetabular rim with multiple suture anchors in place
Graft Preparation
There are a multitude of graft options for use in labral reconstruction, which can broadly be classified as allograft and autograft. Autograft options include gracilis, iliotibial band, indirect head of rectus femoris, and semitendinosus tissue. Allograft options include semitendinosus and tensor fascia lata tissue grafts, among other options. There is currently no consensus regarding the optimal graft for labral reconstruction, with systematic reviews showing no difference in outcomes between allograft and various autograft techniques [19•]. Biomechanical studies have suggested similar mechanical performance between allograft and autograft options [20]. Therefore, selection of graft type should include a consideration of surgeon comfort, patient preference, donor site morbidity, and ease of access and cost of donor tissue [21•].
Graft sizing is crucial, as both over- and under-sizing the graft can compromise the outcome of the reconstruction. In most segmental cases, the graft is prepared in a slightly over-sized fashion to allow for overlap between graft and native labrum upon reconstruction [14]. The graft is tubularized with non-absorbable Krackow stitches placed in a longitudinal fashion (Fig. 4). Proper tubularization ensures optimal contact with the acetabular rim and better replicates native labral tissue, though care must be taken to ensure that the graft is tubularized to the appropriate diameter, length, and shape to avoid overstuffing or under-sizing. Reinforcing suture is added to both ends of the graft, with the free ends of this suture being utilized to subsequently aid in guiding the graft into place on the acetabular rim (Fig. 5) [22].
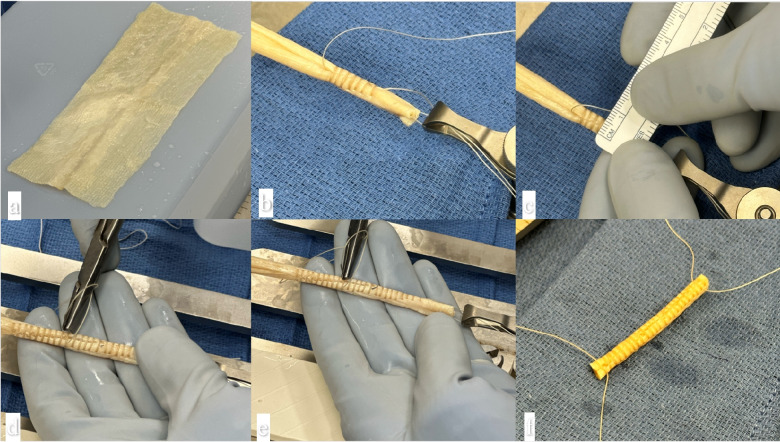
Fig. 4.

Tubularization of the graft using longitudinal Krackow stitching
Fig. 5.
a Graft preparation for tensor fascia allograft. b Allograft is preliminarily moistened and tubularized to desired thickness based on native labral caliper (typically 5–7-mm diameter). c Vicryl 2-0 suture is utilized to fix the seam of the graft at 2-mm intervals throughout the length of the graft and then run back through the graft as a core suture. d, e The graft is cut leaving 3–5mm at each terminal end to incorporate into the native labral tissue if segmental. f The vicryl is then passed through each end of the graft in a simple fashion to control graft
Graft Shuttling
There are three commonly used techniques for passing the graft through the portal and securing it to the acetabulum. In the first, one end of the graft is pierced by the free end of the suture originating from the anterosuperior anchor point (Fig. 6) [22]. The graft is shuttled through the portal, typically the mid-anterior portal (MAP) or distal anterolateral accessory (DALA) portal, and guided into position over the acetabulum using this suture (Fig. 7). After manipulation of the graft and visualization of proper positioning (Fig. 8a), the graft is secured against the anterosuperior acetabulum using an arthroscopic knot (Fig. 8b). The opposite end of the graft is then secured into place by passing the free end of the inferolateral anchor through the graft tissue (Fig. 8c). The remaining, centrally located anchors are then passed through the graft and secured tightly in place (Figs. 8a and 9). In the second technique, the “kite technique,” both ends of the graft are secured to the respective terminal anchor points prior to shuttling the graft through the portal (Fig. 10) [23]. This allows for more precise control of the orientation and positioning of the graft. Subsequent graft fixation proceeds in a similar fashion as the first technique. In the third technique, the “pull through technique,” the graft is left long during preparation and pulled through an accessory posterolateral portal. Subsequent graft fixation proceeds in a similar fashion and the remainder of the graft is amputated past the most posterior anchor following final fixation.
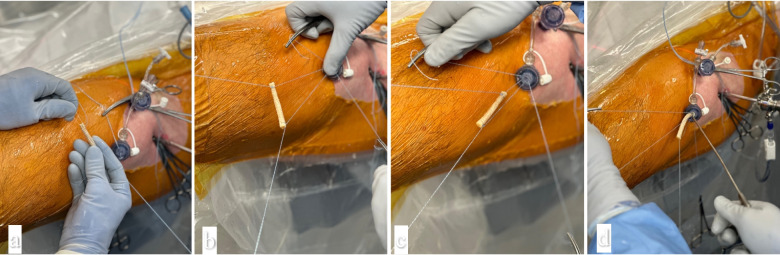
Fig. 6.
Intraoperative photographs demonstrating graft shuttling technique in a left hip. a Superior/medial anchor is pulled out of the medial side of the distal anterolateral accessory portal (DALA) and posterior anchor is pulled laterally taking care not to twist sutures. b–c The anchors are shortened 1/3 and 2/3 lengths and clamped. The long suture is passed through the middle of the graft and tied to itself over the vicryl suture line. d–e This is repeated for the posterior suture
Fig. 7.
Intraoperative photographs demonstrating suture shuttling technique in a left hip. a–c The vicryl holding sutures are removed and the graft is passed by making the graft linear to the cannula, pulling the shorter suture tail. d A suture grasper can be introduced through the dam of the cannula while the slack in the suture is taken up to keep the sutures from twisting
Fig. 8.
Arthroscopic photographs of a left hip. a Graft in place along the acetabular rim prior to fixation. b Graft secured anteriorly, and c posteriorly, using suture anchor fixations
Fig. 9.

Arthroscopic image of a left-sided labral reconstruction graft (different patient from previous figures) fixed into place using suture anchors forming gasket seal along femoral head
Fig. 10.

Right hip. Anchor sutures exiting the portal are subsequently passed through the graft and used during graft parachuting to the acetabular rim
Closure and Post-Operative Rehabilitation
After confirmation of optimal graft placement, the capsule is repaired, and the portals are closed. Post-operative rehabilitation protocols vary within the literature, but extension and external rotation in the immediate post-operative period is commonly avoided, with some surgeons opting to use anti-rotation bolsters to prevent external rotation [22]. There is a paucity of literature comparing post-operative rehabilitation protocols, but generally rehabilitation protocols for labral reconstruction are similar to protocols used after labral repair. In Philippon et al., 20 lbs. of weight bearing was utilized in the early post-operative period and hip external rotation and extension was restricted for 14 to 21 days after surgery [14]. Hip strengthening and endurance training were allowed only after good stability and gait was shown. In Scanaliato et al., passive motion was encouraged in the immediate post-operative period and weightbearing with crutches was utilized until patient gait was stable at 2–4 weeks postoperatively [16]. Return to sport occurred at various times depending on patient considerations and functional status; Maldonado et al. reports that 78% of patients had returned to sport by 1 year of follow-up [24•].
Outcomes
Introduction
The outcomes of labral reconstruction are challenging to assess given the indications and optimal techniques remain subject to debate. Moreover, currently there is no consensus regarding a gold standard method of performing labral reconstruction. Significant variability exists in technique with segmental augmentation, segmental reconstruction, circumferential augmentation, and circumferential reconstruction all being viable treatment options that are performed based on surgeon preference and experience. Furthermore, many graft options (autograft and allograft), anchor types, and suture passage configurations have been described in these techniques.
Early Outcomes—Labral Reconstruction
The first study of labral reconstruction outcomes was performed by Philippon et al. in which iliotibial band (ITB) autograft was used to perform segmental labral reconstruction in 47 patients with a mean follow-up of 18 months [14]. Of the cohort, 9% of patients underwent total hip arthroplasty (THA); however, these patients were significantly older and had more joint space narrowing than patients who did not progress to THA. Of the 37 patients with adequate follow-up and no THA conversion, the average mean improvement in modified Harris hip score (MHHS) following labral reconstruction was 23 points, with improvements in post-op MHHS in all but two. Age less than 30 years was found to be an independent predictor of satisfaction and MHHS improvement.
In a follow-up study in 2020, Philippon et al. reported results in 82 patients undergoing labral reconstruction with ITB autograft with a minimum 10-year follow-up [25••]. A 61% 10-year survival rate with no revision or THA conversion occurred. Patients with < 2mm joint space had a 23.6 increased odds ratio of undergoing THA as compared to patients with >2mm joint space. Patients who required revision hip arthroscopy (9%) were most commonly treated for development of adhesions. Patients who did not undergo additional arthroscopic procedures demonstrated mean improvements in patient-reported outcomes (PROs) with MHHS increase from 60 to 82, hip outcome score (HOS)-activities of daily living (ADL) 69 to 90, and HOS-sports from 43 to 76 at 10-year follow-up.
In a cohort of elite athletes undergoing labral reconstruction, Boykin et al. reported a high level of return to professional sport (85.7%) at a similar level to pre-injury, at a mean follow-up of 41 months [26]. Three patients returned to sport but were unable to achieve their pre-operative level of competition. Of the 3 patients who were unable to return to sport, two patients progressed to THA and one patient retired from sport.
Reconstruction vs. Resection
In 2014, Domb et al. published 2-year results of a matched-pair controlled study of patients undergoing segmental labral reconstruction (using gracilis autograft) vs. segmental resection [9]. The authors found these groups to have similar pre-operative demographics and PROs, with patients in both groups having statistically significant improvements in all outcome measures at 2-year follow-up. Patients in the reconstruction group did demonstrate statistically significant superior improvements in both non-arthritic hip scores (NAHS) and HOS-ADL scores. The other outcome scores (MHHS and HOS-sports) favored the reconstruction group, but did not reach statistical significance. However, this study is limited by short- to mid-term follow-up.
Reconstruction vs. Repair
In a multi-center study with 2-year outcomes, Bodendorfer et al. report results on 416 total patients undergoing labral repair, segmental labral reconstruction, and circumferential reconstruction in the primary setting [27•]. There were no differences in preoperative PROs or demographics between the groups, although the labral repair group had greater rates of articular cartilage damage than the segmental labral reconstruction group, and the segmental labral reconstruction group had greater rates of labral degeneration and more severe labral tears than the labral repair and circumferential labral reconstruction groups. Despite these differences, patients in all groups saw similar improvements in post-operative PROs (delta visual analogue score for pain (VAS-pain), MHHS, HOS-ADL, or International Hip Outcome Tool-12 (iHOT-12)) with no differences between the groups at mean 2-year follow-up. Additionally, there were no differences between the groups in rate of patients achieving minimal clinically important difference (MCID) or patient acceptable symptomatic state (PASS) achievement for any outcome measure. Three of the 312 (1%) patients undergoing labral repair had undergone subsequent surgery at 2-year follow-up compared to 3 of 51 (6%) patients in the circumferential labral reconstruction group. The authors do note limitations in the study, including the lack of uniform indications across the seven surgeons who participated in the study.
A recent systematic review found that labral reconstruction trended towards slightly lower patient-reported outcomes and slightly higher rate of conversion to total hip arthroplasty when compared to labral repair; however, this was not found to be statistically significant [28•]. Overall, labral reconstruction can provide similar pain and function results to those of labral repair.
Segmental vs. Circumferential Labral Reconstruction
In 2022, Maldonado et al. compared 2-year outcomes on patients undergoing segmental versus circumferential labral reconstruction [29•]. They reported that patients in both technique groups achieved significant and similar improvement in PROs including MHHS, HOS-sports, NAHS, and VAS-pain. Additionally, they reported no differences in rate of patients in either group achieving MCID or PASS. There were no reported statistically significant differences in rate of patients undergoing a secondary procedure (4.3% segmental vs. 2.1% circumferential) or converting to THA (10.6% segmental vs. 6.4% circumferential). Given this study was not performed in a randomized fashion, but rather based on the senior author’s expertise and intra-operative decision-making, they concluded an individualized approach to each patient should be made in regard to labral reconstruction technique.
In a systematic review, Orner et al. reported on nine studies and 427 total patients undergoing segmental and circumferential labral reconstruction [30•]. Indication for the procedures was irreparable or unsalvageable labrum in all studies. The studies cited “labral ossification or calcification, segmental labral defect, severe intrasubstance damage, moderate to severe complexity of labral tearing, nonviable labral tissue, hypoplastic or hyperplastic labral tissue, and inability to establish a suction seal” as presentation of an irreparable or unsalvageable labrum. All studies performing circumferential reconstruction used allograft only and studies performing segmental reconstruction reported both autograft and allograft use. Although reported PROs were heterogenous across studies, preventing direct comparison of the studies, post-operative outcome scores improved in all studies and techniques. The mean change in postoperative MHHS was similar between groups and ranged from 20.4 to 31.7 points in the circumferential group and 17.8 to 29 points in the segmental group. All studies included in the systematic review reported on failure of labral reconstruction by reoperation, with revision hip arthroscopy and conversion to THA being the most common reoperations. Studies reported a range of 3.1 to 9.9% of circumferential reconstruction patients and 9.1 to 26.8% of segmental reconstruction patients undergoing conversion to THA.
Conclusion
Though relatively new, labral reconstruction is increasingly being utilized to restore the functionality and anatomy of the acetabular labrum. The preliminary evidence available has shown that reconstruction delivers outcomes that are on par with labral repair, and reconstruction of the labrum has been shown to consistently restore function and stability to the hip joint. Because of the novelty of the procedure, there remains debate over the optimal graft type, reconstruction technique, and extent of reconstruction—and there are no clear answers given by the current literature that exists surrounding these questions. While further research must be done to elucidate the role and performance of various aspects of the reconstruction, labral reconstruction is proving to be a vital component of the hip preservation specialist’s toolbox.
Compliance with Ethical Standards
Conflict of Interest
JW Genuario is a paid consultant for Stryker Corp., and an editor for the American Journal of Sports Medicine. TG Maak is a paid consultant, speaker, and educator for Arthrex, Inc., and a member of the editorial board of Clinical Orthopaedics and Related Research. SK Aoki is a paid consultant for Stryker Corp.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human and animal subjects performed by any of the authors.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Tan V, Seldes RM, Katz MA, Freedhand AM, Klimkiewicz JJ, Fitzgerald RH. Contribution of acetabular labrum to articulating surface area and femoral head coverage in adult hip joints: an anatomic study in cadavers. Am J Orthop Belle Mead NJ. 2001;30(11):809–812. [PubMed] [Google Scholar]
- 2.Cadet ER, Chan AK, Vorys GC, Gardner T, Yin B. Investigation of the preservation of the fluid seal effect in the repaired, partially resected, and reconstructed acetabular labrum in a cadaveric hip model. Am J Sports Med. 2012;40(10):2218–2223. doi: 10.1177/0363546512457645. [DOI] [PubMed] [Google Scholar]
- 3.Myers CA, Register BC, Lertwanich P, et al. Role of the acetabular labrum and the iliofemoral ligament in hip stability: an in vitro biplane fluoroscopy study. Am J Sports Med. 2011;39(1_suppl):85S–91S. doi: 10.1177/0363546511412161. [DOI] [PubMed] [Google Scholar]
- 4.•.White BJ, Constantinides SM. Allograft labral reconstruction of the hip: expanding evidence supporting greater utilization in hip arthroscopy. Curr Rev Musculoskelet Med. 2022;15(2):27-37. 10.1007/s12178-022-09741-y. Systematic review investigating various outcomes after circumferential allograft labral reconstruction, showing overall good outcomes after this procedure. [DOI] [PMC free article] [PubMed]
- 5.White BJ, Patterson J, Herzog MM. Bilateral hip arthroscopy: direct comparison of primary acetabular labral repair and primary acetabular labral reconstruction. Arthrosc J Arthrosc Relat Surg. 2018;34(2):433–440. doi: 10.1016/j.arthro.2017.08.240. [DOI] [PubMed] [Google Scholar]
- 6.••.White BJ, Herzog MM. Arthroscopic labral reconstruction of the hip: a decade of growing evidence and technical evolution. Tech Orthop. 2021;36(3):222. 10.1097/BTO.0000000000000487. Systematic review following changes in indications, techniques, and outcomes of arthroscopic labral reconstruction over the past decade.
- 7.Youm T. Editorial commentary: wanted dead or alive: primary allograft labral reconstruction of the hip is as successful, if not more successful, than primary labral repair. Arthrosc J Arthrosc Relat Surg. 2018;34(2):441–443. doi: 10.1016/j.arthro.2017.09.011. [DOI] [PubMed] [Google Scholar]
- 8.Philippon MJ, Bolia IK, Locks R, Briggs KK. Labral preservation: outcomes following labrum augmentation versus labrum reconstruction. Arthrosc J Arthrosc Relat Surg. 2018;34(9):2604–2611. doi: 10.1016/j.arthro.2018.04.021. [DOI] [PubMed] [Google Scholar]
- 9.Domb BG, El Bitar YF, Stake CE, Trenga AP, Jackson TJ, Lindner D. Arthroscopic labral reconstruction is superior to segmental resection for irreparable labral tears in the hip: a matched-pair controlled study with minimum 2-year follow-up. Am J Sports Med. 2014;42(1):122–130. doi: 10.1177/0363546513508256. [DOI] [PubMed] [Google Scholar]
- 10.•.Orner CA, Patel UJ, Jones CMC, Giordano BD. Segmental and circumferential acetabular labral reconstruction have comparable outcomes in the treatment of irreparable or unsalvageable labral pathology: a systematic review. Arthrosc J Arthrosc Relat Surg. 2022;38(4):1341-1350. 10.1016/j.arthro.2021.10.016. Systematic review finding similar outcomes in both segmental and circumferential surgical techniques in the setting of irreparable labral pathology. [DOI] [PubMed]
- 11.•.Maldonado DR, Kyin C, Shapira J, Rosinsky PJ, Walker-Santiago R, Domb BG. Circumferential and segmental labral reconstruction: a systematic review. Orthopedics. 2021;44(6):361-366. 10.3928/01477447-20211001-03Systematic review finding that circumferential and segmental labral reconstruction are both effective treatments for labral tears in the hip. [DOI] [PubMed]
- 12.Geyer MR, Philippon MJ, Fagrelius TS, Briggs KK. Acetabular labral reconstruction with an iliotibial band autograft: outcome and survivorship analysis at minimum 3-year follow-up. Am J Sports Med. 2013;41(8):1750–1756. doi: 10.1177/0363546513487311. [DOI] [PubMed] [Google Scholar]
- 13.Sogbein OA, Shah A, Kay J, Memon M, Simunovic N, Belzile EL, Ayeni OR. Predictors of outcomes after hip arthroscopic surgery for femoroacetabular impingement: a systematic review. Orthop J Sports Med. 2019;7(6):2325967119848982. doi: 10.1177/2325967119848982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Philippon MJ, Briggs KK, Hay CJ, Kuppersmith DA, Dewing CB, Huang MJ. Arthroscopic labral reconstruction in the hip using iliotibial band autograft: technique and early outcomes. Arthroscopy: The Journal of Arthroscopic & Related. Surg. 2010;26(6):750–756. doi: 10.1016/j.arthro.2009.10.016. [DOI] [PubMed] [Google Scholar]
- 15.Perets I, Hartigan DE, Chaharbakhshi EO, Walsh JP, Close MR, Domb BG. Circumferential labral reconstruction using the knotless pull-through technique—surgical technique. Arthrosc Tech. 2017;6(3):e695. doi: 10.1016/j.eats.2017.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Scanaliato JP, Christensen DL, Salfiti C, Herzog MM, Wolff AB. Primary circumferential acetabular labral reconstruction: achieving outcomes similar to primary labral repair despite more challenging patient characteristics. Am J Sports Med. 2018;46(9):2079–2088. doi: 10.1177/0363546518775425/ASSET/IMAGES/LARGE/10.1177_0363546518775425-FIG3.JPEG. [DOI] [PubMed] [Google Scholar]
- 17.•.Suppauksorn S, Beck EC, Chahla J, et al. Comparison of suction seal and contact pressures between 270° labral reconstruction, labral repair, and the intact labrum. Arthroscopy - Journal of Arthroscopic and Related Surgery. 2020;36(9):2433-2442. 10.1016/j.arthro.2020.05.024Cadaveric study finding that 270° labral reconstruction decreased suction seal strength and contact pressures relative to the intact labrum and repaired setting. [DOI] [PubMed]
- 18.•.Todd JD, Allan AN, Maak TG, Weiss JA. Characterization and finite element validation of transchondral strain in the human hip during static and dynamic loading. J Biomech. 2021;114:110143. Finite element modeling study elucidating changes in transchondral stress and strain patterns with circumferential reconstruction. [DOI] [PMC free article] [PubMed]
- 19.•.Rahl MD, LaPorte C, Steinl GK, O'Connor M, Lynch TS, Menge TJ. Outcomes after arthroscopic hip labral reconstruction: a systematic review and meta-analysis. Am J Sports Med. 2020;48(7):1748-1755. 10.1177/0363546519878147Systematic review finding no significant difference in outcomes based on usage of any particular graft type alone, specifically investigating autograft versus allograft. [DOI] [PubMed]
- 20.Lee S, Wuerz TH, Shewman E, et al. Labral reconstruction with iliotibial band autografts and semitendinosus allografts improves hip joint contact area and contact pressure: an in vitro analysis. American Journal of Sports Medicine. 2015;43(1):98–104. doi: 10.1177/0363546514553089. [DOI] [PubMed] [Google Scholar]
- 21.•.Scanaliato J, Green C, Salfiti C, Wolff A. Hip labral reconstruction: techniques and outcomes. Curr Rev Musculoskelet Med. 2021;14(6):340. 10.1007/s12178-021-09733-4Review finding labral reconstruction consistently results in improved short-term and mid-term outcomes in patients with severe labral pathologies. [DOI] [PMC free article] [PubMed]
- 22.Chahla J, Soares E, Bhatia S, Mitchell JJ, Philippon MJ. Arthroscopic technique for acetabular labral reconstruction using iliotibial band autograft. Arthrosc Tech. 2016. 10.1016/j.eats.2016.02.025 [DOI] [PMC free article] [PubMed]
- 23.Bhatia S, Chahla J, Dean CS, Ellman MB. Hip labral reconstruction: the “Kite Technique” for improved efficiency and graft control. Arthrosc Tech. 2016;5(2):e337. doi: 10.1016/j.eats.2016.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.•.Maldonado DR, Chen SL, Yelton MJ, et al. Return to sport and athletic function in an active population after primary arthroscopic labral reconstruction of the hip. Orthop J Sports Med. 2020;8(2):2325967119900767. 10.1177/2325967119900767Review finding that, at 1-year follow-up, patients who undergo primary arthroscopic labral reconstruction of the hip are able to return to sport at a promisingly high rate. [DOI] [PMC free article] [PubMed]
- 25.••.Philippon MJ, Arner JW, Crawford MD, Bolia IK, Briggs KK. Acetabular labral reconstruction with iliotibial band autograft: outcome and survivorship at a minimum 10-year follow-up. J Bone Joint Surg Am. 2020;102(18):1581-1587. 10.2106/JBJS.19.01499. Outcomes study finding that acetabular labral reconstruction, using iliotibial band autograft, is a highly durable procedure, with favorable outcomes at a minimum 10-year follow-up. [DOI] [PubMed]
- 26.Boykin RE, Patterson D, Briggs KK, Dee A, Philippon MJ. Results of arthroscopic labral reconstruction of the hip in elite athletes. Am J Sports Med. 2013;41(10):2296–2301. doi: 10.1177/0363546513498058. [DOI] [PubMed] [Google Scholar]
- 27.•.Bodendorfer BM, Alter TD, Carreira DS, Wolff AB, Kivlan BR, Christoforetti JJ, Salvo JP, Matsuda DK, Nho SJ. Multicenter outcomes after primary hip arthroscopy: a comparative analysis of two-year outcomes after labral repair, segmental labral reconstruction, or circumferential labral reconstruction. Arthroscopy. 2022;38(2):352-361. 10.1016/j.arthro.2021.05.013. Multicenter systematic review finding similar outcomes between labral repair, segmental labral reconstruction, and circumferential labral reconstruction at 2 years. [DOI] [PubMed]
- 28.•.Maldonado DR, Kyin C, Chen SL, et al. In search of labral restoration function with hip arthroscopy: outcomes of hip labral reconstruction versus labral repair: a systematic review. Hip Int. 2021;31(6):704-713. 10.1177/1120700020965162Systematic review finding that, in the setting of FAI and labral tears, both labral reconstruction and labral repair showed significant improvement in short term PROs. [DOI] [PubMed]
- 29.•.Maldonado DR, Kyin C, Shapira J, Meghpara MB, Rosinsky PJ, Lall AC, Domb BG. Comparable minimum 2-year patient-reported outcome scores between circumferential and segmental labral reconstruction for the management of irreparable labral tear and femoroacetabular impingement syndrome in the primary setting: a propensity-matched study. Arthroscopy. 2022;38(2):335-348. 10.1016/j.arthro.2021.04.037. Propensity-matched retrospective study finding that both circumferential and segmental labral reconstruction have comparable clinical outcomes at 2 years. [DOI] [PubMed]
- 30.•.Orner CA, Patel UJ, Jones CMC, Giordano BD. Segmental and circumferential acetabular labral reconstruction have comparable outcomes in the treatment of irreparable or unsalvageable labral pathology: a systematic review. Arthroscopy. 2022;38(4):1341-1350. 10.1016/j.arthro.2021.10.016. Systematic review finding that both segmental and circumferential labral reconstructions have comparable clinical outcomes in the treatment of unsalvageable labral pathology. [DOI] [PubMed]