Abstract
Introduction:
The purpose of this study was to investigate internalized weight bias (IWB) and its relationship with pregnancy-related weight changes and postpartum depression. IWB is defined as the internalization of negative attitudes and beliefs about people due to their weight. Although IWB has been linked with weight change and depression in other samples, it has never been investigated in the postpartum period.
Methods:
We used a cross-sectional survey design. Participants were 251 women recruited via social media who were living in the United States and 6 to 12 months postpartum. We calculated percentage of body weight gained during pregnancy and percentage of that weight that was retained postpartum from self-reported weights. Participants completed self-report measures of IWB (modified version of the Weight Bias Internalization Scale) and postpartum depression (Edinburgh Postnatal Depression Scale).
Results:
Gestational weight gain was not significantly associated with IWB or depression. Postpartum retention of gestational weight was significantly positively associated with both IWB and depressive symptoms. Furthermore, IWB mediated the relationship between postpartum weight retention and depressive symptoms.
Discussion:
Postpartum retention of weight gained during pregnancy, but not weight gain itself, was related to both IWB and depressive symptoms. The relationship between pregnancy-related weight changes and psychological distress is complex. Sociocultural pressures to return to a prepregnancy physical state swiftly after giving birth may increase risk for IWB during a time in life when stress is already likely to be high, posing additional psychological risk. IWB existing prepregnancy may also worsen postpartum self-concept, contributing to depression. This is the first study, to our knowledge, to directly assess associations among gestational weight change, IWB, and postpartum depression. In addition to discussing weight in pregnancy, perinatal care providers could improve postpartum health by helping women set realistic, body-positive goals postpartum.
Keywords: depression, internalized weight bias, maternal health, perinatal, postpartum, pregnancy, weight
INTRODUCTION
Pregnancy and the postpartum period are accompanied by rapid and dramatic changes in body shape, size, and weight, which can be associated with adverse psychological symptoms. Dayan et al1 found that, regardless of prepregnancy body mass index (BMI), higher gestational weight gain in the third trimester increased risk for depression at 6 to 8 weeks postpartum. Importantly, this association was reciprocal in nature, with depressive symptoms in pregnancy predicting pregnancy-related weight gain.1 Postpartum retention of gestational weight has been associated with increased severity and morbidity of postpartum depressive and anxiety symptoms.2 Body image dissatisfaction is also common during pregnancy and the postpartum period and is associated with greater gestational weight gain3 and prenatal and postpartum depressive symptoms.3,4
Weight is a relevant and important factor to include in perinatal care and consider when determining health risk. It is estimated that close to 50% of women gain more weight during pregnancy than is clinically recommended,5 which can increase the risk of adverse outcomes including cesarean birth, newborns and infants large for gestational age, and maternal postpartum weight retention.6 Between 15% and 20% of women retain gestational weight gain of more than 10 lbs for up to one year postpartum.7 Retention of gestational weight gain increases risk of developing chronic conditions including type II diabetes, cardiovascular conditions, and increased weight-related risks during subsequent births.8
Although discussion of pregnancy-related weight change is clinically necessary, it leaves women vulnerable to weight stigma and discrimination, which are frequent experiences during the perinatal period.9 In general, weight and weight management have become moralized, resulting in negative judgment of individuals who are overweight as having moral failing.10 Negative judgments, in turn, can lead to discriminatory behaviors toward individuals with higher body weight, such as negative comments, social exclusion, and biased employment and health care practices.11,12 Incollingo Rodriguez et al9 found that 2 out of 3 women experience weight-specific stigma in the perinatal period. Sources of weight discrimination for childbearing women include friends, family, the media, and even health care professionals.12,13 Women with higher BMI are more likely to report negative experiences within their perinatal care compared with pregnant women with lower BMI, including receiving less respect and kindness from care providers.12
Weight-based stigma has been investigated from many angles, with consistent findings that the experience of stigma is detrimental to physical and mental health. In nonperinatal samples, experiencing weight stigma mediates the relationship between objectively measured BMI and psychological health, including symptoms of anxiety and depression.14 Pregnant women are aware that their weight can impact their and their infant’s health, and perceptions of weight change can impact self-image.15 In a qualitative investigation of gestational body changes, Neiterman and Fox15 reported that women perceive a general loss of control over their body and its pregnancy-related changes, which can lead to significant guilt with excess weight gain and retention. In the postpartum period, negative self-views are compounded by immense and multifaceted sociocultural pressure to “lose the baby weight.”16,17 Nippert et al13 recently highlighted biased and stigmatizing messaging in popular media, which sets and perpetuates unrealistic expectations regarding the rapidity of postpartum weight loss: weight gained across 40 weeks of pregnancy should be easily and swiftly lost to return to prepregnancy physical state.
Negative weight-related attitudes can become internalized in a form of self-stigma known as internalized weight bias (IWB). IWB has been described as self-directed negative attitudes, beliefs, and criticisms about individuals with BMIs above the normal range.18 IWB extends beyond negatively evaluating one’s shape and size and becomes negative evaluation and dissatisfaction with oneself, specifically due to weight status.18 For example, individuals who perceive themselves to be overweight may apply negative sociocultural stereotypes that obese individuals are lazy, noncompliant, and less valued to the self, leading to decreased self-worth.18,19 Self-stigma can have detrimental psychological effects. A recent systematic review20 showed that increased IWB is related to more severe symptoms of depression and anxiety, decreased self-esteem, poor body image, and eating disorder pathology. Higher IWB was associated with more depressive symptoms in more than 30 studies, and higher IWB was determined to predict poor body image even after controlling for BMI and depressive symptoms.20
According to the social cognitive model of internalized stigma,21 self-stigma involves first living with a stigmatized attribute, being aware of and then agreeing with negative social attitudes toward individuals with that attribute, and finally discriminating against oneself through the application of these attitudes. Psychological and physiologic harm befalls the individual through these discriminatory behaviors, which can include negative self-talk and maladaptive behaviors (eg, disordered eating).20 Self-stigma can, therefore, act as a mediator (ie, statistical mechanism) of the association between the stigmatized characteristic (eg, weight) and health outcome (eg, depression). The mediational role of self-stigma has been investigated in relation to psychiatric illness,22 intimate partner violence,23 and positive HIV status.24 Decker et al25 identified IWB as a mediator of the positive relationship between self-perceived weight status and depressive symptoms in college students.
Evidence for negative psychological outcomes of IWB has been identified in adolescents,26 young adults,27 and middle-aged women28 and across BMI categories.29 Furthermore, the negative effects of IWB have been examined during other periods of expected weight change, including behavioral and surgical weight loss interventions.20 Examination of IWB during the perinatal period—a time characterized by significant bodily and emotional changes and complex psychological and social adjustment30—is generally absent in the literature. Only one study has reported on IWB in perinatal women, and results showed that among 100 German women with overweight/obesity in pregnancy, IWB severity was consistent from pregnancy to one month postpartum.31
IWB is an important and understudied experience to consider in better understanding the psychological implications of pregnancy-related weight changes in childbearing women. Unrealistic expectations for postpartum loss of weight gained during pregnancy may place women at risk for perceived failure in returning to a prepregnancy body state, leading to either new onset or worsening IWB through internalization of negative attitudes regarding their weight. Our general aim was to call attention to IWB as a potential factor contributing to postpartum psychological distress. Thus, the purpose of the current study was to (1) describe the level of IWB in a sample of postpartum women, (2) examine associations between pregnancy-related weight changes, IWB, and postpartum depression, and (3) examine IWB as a mediator of relationships between pregnancy-related weight changes and postpartum depression.
METHODS
Participants and Procedure
Three hundred and eighteen women were recruited between February 2016 and March 2017 via social media advertisements for an anonymous online survey examining pregnancy-related weight changes and postpartum well-being. Participants were over the age of 18, the biological mother of a living child, a resident of the United States, and able to complete the online survey in English. We limited participation to those 6 to 12 months postpartum to allow for resolution of the immediate normative physiologic changes associated with childbirth. Women self-identified as interested in participation by accessing the survey link, reviewed an online informed consent form, and confirmed their desire to participate by advancing to the survey items. Eligibility was confirmed via survey responses. Participants were instructed to respond to items with respect to only their most recent childbirth experience (ie, the index birth). This research was approved by the East Carolina University institutional review board.
Measures
Demographic, Health, and Weight Characteristics
Participants self-reported demographic information (eg, age, marital status). With regard to their index birth, they reported parity, multiple pregnancy, route of birth, their child’s gestational age at birth, and their child’s age at the time of study participation. Participants self-reported their current height and weight, weight just prior to pregnancy, and amount of weight gained during pregnancy. Their responses were used to calculate prepregnancy BMI (weight prior to pregnancy in kilograms/height in square meters) and postpartum BMI (current weight in kilograms/height in square meters). We calculated gestational weight gain [(weight gained during pregnancy in pounds/prepregnancy weight in pounds) * 100] and postpartum weight retention [(current weight in pounds − prepregnancy weight in pounds/prepregnancy weight in pounds) * 100] as percentages to account for differences in BMI.
Internalized Weight Bias
We used the modified version of the Weight Bias Internalization Scale (WBIS-M).29 The WBIS-M is based on the original 11-item WBIS,18 which is designed to assess the degree to which the individual applies negative stereotypes about overweight people to the self. Although the original WBIS was designed to assess IWB in people who are overweight (eg, “I am less attractive than other people because I am overweight”), the WBIS-M is a valid and reliable assessment of IWB across different BMIs (eg, “I am less attractive than most other people because of my weight”). Participants indicated their level of agreement on a 7-point scale from 1 (strongly disagree) to 7 (strongly agree), and responses were averaged for a total score, with higher scores indicating greater IWB. Consistent with prior research demonstrating poor item-to-total correlation,32 we removed item 1, leaving the 10-item WBIS-M. The WBIS-M has demonstrated good psychometrics in samples of reproductive-aged women, including strong internal consistency and construct validity.29,32 In the current study, the WBIS-M demonstrated strong internal consistency (α = 0.95).
Depressive Symptoms
Depressive symptoms were measured using the Edinburgh Postnatal Depression Scale (EPDS).33 The EPDS is a 10-item depression screening measure assessing symptoms of depression occurring within the past week. Participants responded to each item on a 4-point scale ranging from 0 to 3, with higher ratings indicating greater depressive symptoms. Responses were summed for a total score, with a score of ≥13 indicating possible depression. The EPDS demonstrated adequate internal consistency (α = 0.90).
Data Analysis
Analyses were completed using SPSS version 26 (IBM Corporation). Descriptive statistics were calculated for all study variables. We used univariate analyses including t tests and correlations to initially explore relationships of depressive symptoms and IWB with demographic and perinatal health characteristics. Demographic and perinatal health characteristics that demonstrated significant associations with depressive symptoms or IWB were included as covariates in respective multivariate analyses. To test mediation, we used model 4 (single mediation) in the PROCESS macro for SPSS version 26 using a bootstrap estimation approach with 5000 samples,34 after confirming significant associations between all 3 variables in each model using linear regressions. We examined the indirect effects of the stigmatized attribute (pregnancy-related weight change; predictor) on health outcome (postpartum depression symptoms; criterion) through internalized stigma (IWB; mediator). Infant age was included in all analyses with postpartum weight retention as a predictor to account for passing of time since giving birth. A power analysis performed with GPower 3.135 for the mediation analyses identified an achieved power of 95% to detect a medium-sized effect.
RESULTS
Participant Characteristics
Of the 318 people who accessed the survey, 25 did not provide consent, 13 were ineligible, and 27 were removed for missing more than 75% of data. Two additional participants were identified as outliers, having reported that they gained and/or lost a biologically implausible amount of weight (greater than 150 lbs). Thus, the final sample included 251 participants. Cases with item-level missing values were excluded listwise from each analysis.
Participant characteristics are summarized in Table 1. Median (SD) participant age was 29.02 years (4.81; range, 18–42). The majority identified as non-Hispanic, white, and married. More than half were employed either part- or full-time (n = 148; 58.9%). Approximately half had at least a 4-year college degree (51.4%), with a mean (SD) of 15.25 (2.23; range, 10–20) years of education. The median reported annual household income was $70,000 (25th percentile, $42,000; 75th percentile, $115,000). The majority were first-time mothers, with parity ranging from 1 to 7 children (mean [SD], 1.55 [0.87]). Most participants had a singleton pregnancy, a vaginal birth (n = 171; 68.1%), and infants born full-term (completed weeks’ gestation at birth: mean [SD], 38.99 [1.93] weeks; range, 27–42). Infant age ranged from 6 to 12 months at time of study participation (mean [SD], 9.08 [1.66] months).
Table 1.
Participant Demographic and Pregnancy Characteristics (N = 251).
| Characteristic | n (%) |
|---|---|
|
| |
| Race | |
| White | 234 (93.2) |
| African American | 4 (1.6) |
| Ethnicity: non-Hispanic | 227 (90.4) |
| Marital status | |
| Married | 199 (79.3) |
| Not married, living with partner | 34 (13.5) |
| Single, never married | 17 (6.8) |
| Employed | |
| Full-time | 94 (37.5) |
| Part-time | 47 (18.7) |
| Education | |
| High school diploma | 116 (46.2) |
| Bachelor’s degree | 74 (29.5) |
| Doctoral degree | 55 (21.9) |
| Singleton pregnancy | 247 (98.4) |
| Primiparous | 153 (61.0) |
| Route of birth | |
| Vaginal | 155 (61.8) |
| Instrumental vaginal | 16 (6.4) |
| Scheduled cesarean birth | 25 (10.0) |
| Unplanned/emergent cesarean birth | 55 (21.9) |
| Full-term birth | 224 (89.2) |
Pregnancy-Related Weight Changes
Descriptive information regarding participants’ pregnancy-related weight changes is displayed in Table 2. Based on prepregnancy BMI, 45.8% (n = 115) of participants fell within the overweight/obese BMI category prior to pregnancy (21.9% in the overweight category, 23.9% in the obese category) compared with 53.0% at 6 to 12 months postpartum (21.5% in the overweight category, 31.5% in the obese category). Based on the Institutes of Medicine’s36 gestational weight gain recommendations by BMI, more than half (n = 133; 53.0%) exceeded the recommended amount of weight gain during pregnancy, whereas 12.7% (n = 32) gained less than the recommended amount. On average, participants gained close to 24% of their prepregnancy weight during pregnancy and retained just over 4% of gestational weight postpartum. We conducted an analysis of covariance (ANCOVA) examining gestational weight gain and postpartum weight retention for participants who fell in each prepregnancy BMI category. Results revealed a significant difference in gestational weight gain among BMI categories (F(2236), 59.92; P < .001). Participants in the normal BMI category had significantly greater gestational weight gain (mean, 31.08 lbs) compared with participants in both the overweight (mean, 20.14 pounds; P < .001) and obese (mean, 12.31 lbs; P < .001) BMI categories, and those in the overweight BMI category had significantly greater gestational weight gain than those in the obese BMI category (P = .001). There were no significant differences in postpartum weight retention among BMI categories (F(2237), 41.39; P = .67).
Table 2.
Descriptive Statistics of Study Variables (N = 251).
| Variable | Mean (SD) | Median | Min | Max |
|---|---|---|---|---|
|
| ||||
| Peripartum weight changes | ||||
| BMI prepregnancy | 26.35 (6.68) | 24.55 | 16.13 | 47.55 |
| BMI postpartum | 27.74 (7.37) | 25.51 | 16.47 | 46.87 |
| Pregnancy weight gain, lbs | 34.78 (18.04) | 35.00 | −35.00 | 85.00 |
| Percentage gestational weight gain | 24.17 (13.63) | 23.57 | −15.79 | 75.00 |
| Percentage weight loss since childbirth | −14.21 (10.95) | −15.53 | −43.43 | 25.00 |
| Percentage postpartum weight retention | 4.16 (10.14) | 4.00 | −23.02 | 33.51 |
| Maternal distress variables | ||||
| Internalized weight bias | 3.72 (1.62) | 3.41 | 1.00 | 7.00 |
| Postpartum depressive symptoms | 9.60 (5.73) | 9.00 | 0.00 | 26.00 |
Associations Between Pregnancy-Related Weight Changes and Postpartum Depressive Symptoms
We examined differences in depressive symptoms according to BMI category membership at the time of study participation (Figure 1). Univariate analyses identified the following covariates: maternal age, education, employment, marital status, income, route of birth, and infant gestational age at birth. ANCOVA results revealed a significant difference in depressive symptom severity (F(2200), 5.95; P = .003), such that participants in the normal BMI category reported significantly less severe depressive symptoms compared with participants who fell in the overweight (P = .05) or obese (P = .001) BMI categories. There was no significant difference in depressive symptoms between participants in the overweight or obese BMI categories (P = .31).
Figure 1. Mean Internalized Weight Bias and Depression Scores Stratified by Postpartum BMI (n = 206).
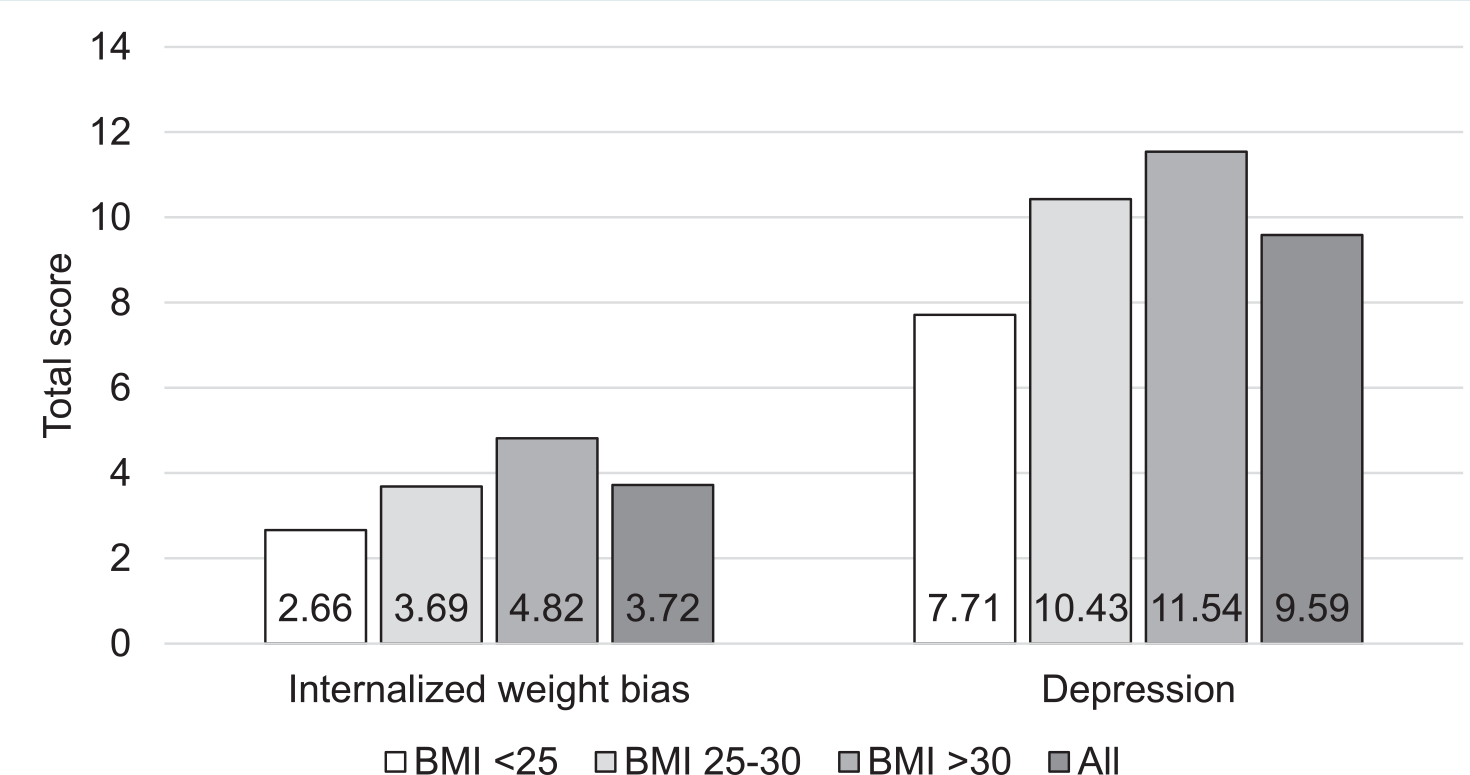
Results of analysis of covariances controlling for infant age at the time of study participation to evaluate differences in internalized weight bias (mean Weight Bias Internalization Scale score) and depression symptoms (mean Edinburgh Postnatal Depression Scale score) among participants belonging to different body mass index (BMI) categories. BMI used in these analyses is postpartum BMI (ie, BMI at time of study participation).
We then used separate linear regressions with simultaneous entry to examine pregnancy weight gain and postpartum weight retention as predictors of depressive symptoms. With covariates included in the model, only postpartum weight retention was a significant predictor of depressive symptoms (Table 3). As percentage of body weight retained increased, severity of depressive symptoms increased.
Table 3.
Associations Between Pregnancy-Related Weight Changes and Internalized Weight Bias and Depressive Symptoms (n = 208).
| Model Summary |
Parameter Estimates |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Criterion | Predictor | df | F | P Value | R2 | B | SE | t | P Value |
|
| |||||||||
| Internalized weight bias | Gestational weight gain | 9193 | 5.67 | <.001 | .21 | −0.01 | 0.01 | 1.26 | .210 |
| Postpartum weight retention | 9194 | 14.71 | <.001 | .41 | 0.08 | 0.01 | 8.35 | <.001 | |
| Depressive symptoms | Gestational weight gain | 8200 | 4.61 | <.001 | .16 | 0.01 | 0.03 | 0.38 | .705 |
| Postpartum weight retention | 9196 | 4.97 | <.001 | .19 | 0.11 | 0.04 | 2.67 | .008 | |
| Internalized weight bias | 8200 | 12.47 | <.001 | .33 | 1.54 | 0.21 | 7.23 | <.001 | |
Note: Covariates included in models of internalized weight bias include participant age, level of education, marital status, annual household income, parity, route of birth, gestational age of infant at birth, and the infant’s age at time of study participation. Covariates included in models of depressive symptoms include participant age, level of education, income, route of birth, marital status, employment status, and gestational age of infant at birth.
Internalized Weight Bias: Associations With Participant Characteristics, Pregnancy-Related Weight Changes, and Postpartum Depressive Symptoms
IWB was higher in participants who had a cesarean birth (mean [SD], 3.92 [1.67]) compared with those who had a vaginal birth (mean [SD], 3.43 [1.69]; P = .04). IWB was also higher in those who were unmarried (mean, 4.47; SD, 1.56) compared with those who reported they were married (mean [SD], 3.35 [1.66]; 4.28, P < .001). WBIS-M score was positively correlated with parity (r, 0.16; P = .015) and negatively correlated with maternal age (r, −0.20; P = .003), education (r, −0.26; P < .001), income (r, −0.19; P = .005), and the infant’s gestational age at birth (r, −0.26; P < .001). Thus, participants reported greater IWB if they were not married, were younger, had lower education and income, had more biological children, had a cesarean birth, or had an infant born at an earlier gestational age; however, these were small correlations (ie, r ranging from 0.1 to 0.3). Figure 1 displays the results of an ANCOVA exploring differences in IWB based on clinically assigned BMI category at the time of study participation, including relevant covariates. Results indicated that IWB significantly increased across BMI categories, such that it was lowest for participants in the normal BMI range, increased for participants in the overweight range, and was highest for those in the obese range.
To examine relationships between pregnancy-related weight changes and IWB, we performed separate linear regressions with gestational weight gain or postpartum weight retention as the predictor. Results of the regressions are displayed in Table 3. Only postpartum weight retention was significantly associated with IWB, suggesting that women who retained a greater percentage of body weight postpartum experienced greater IWB.
Next, we examined associations between IWB and depression. Again, a linear regression with simultaneous entry was conducted to account for relevant demographic and perinatal health characteristics (Table 3). Results of the regression analysis indicated that IWB was significantly associated with depressive symptoms, such that as IWB increased, depressive symptom severity also increased.
The Indirect Effects of Pregnancy-Related Weight Change on Postpartum Depressive Symptoms Through IWB
Based on our linear regression analyses, we selected the association between postpartum weight retention and depressive symptoms for mediation analysis with IWB as the mediator. Results are displayed in Figure 2. On depressive symptoms, we observed a direct effect of weight retention (R2, 0.19; F(9, 196), 5.73; P < .001) and an indirect effect of IWB (b, 1.64; 95% CI = 1.13–2.14), indicating that IWB mediated the association between postpartum weight retention and depressive symptoms. Thus, the association between postpartum depression symptoms and weight retention was, in part, explained by differences in IWB.
Figure 2. Simple Mediation Analysis of the Indirect Effects of Postpartum Weight Retention on Postpartum Depression Symptoms Through Internalized Weight Bias (n = 207).
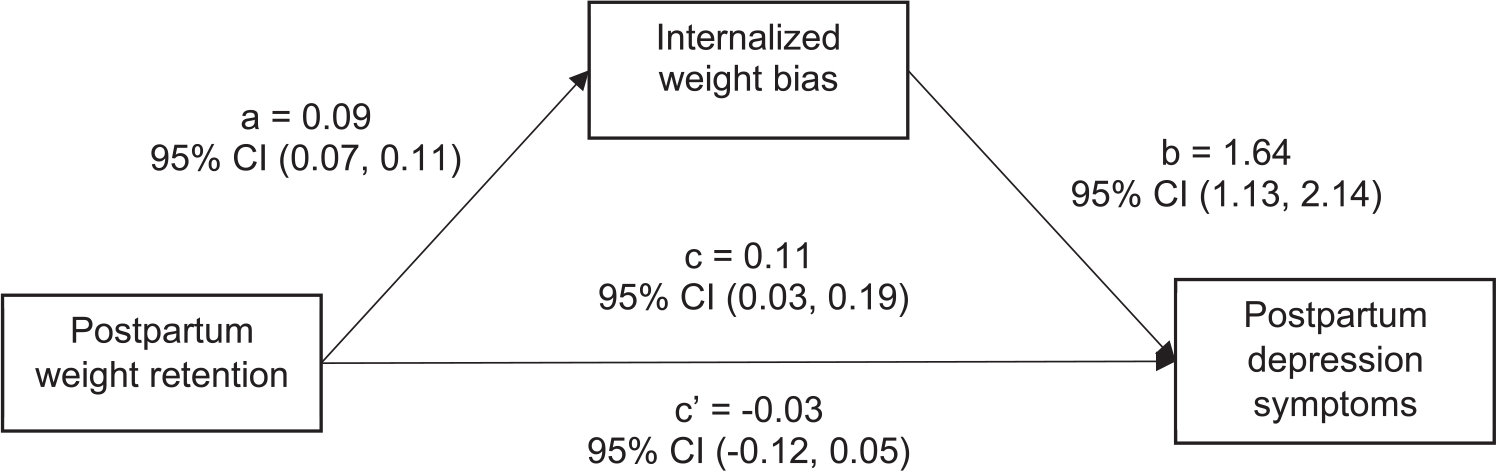
Results of a simple mediation analysis with postpartum weight retention as the independent variable, postpartum depression symptoms as the dependent variable, and internalized weight bias as the mediator. Covariates included participant age, level of education, marital status, annual household income, parity, route of birth, gestational age of infant at birth, and child’s age at time of study participation.
DISCUSSION
The purpose of the current study was to explore the experience of IWB during the postpartum period and investigate relationships between gestational and postpartum weight changes, IWB, and postpartum depressive symptoms. Consistent with prior research,30 there were significant differences in IWB between clinically assigned BMI categories. We calculated peripartum weight variables as the percentage of total body weight gained and retained in order to focus specifically on weight changes surrounding pregnancy. Postpartum retention of weight that was gained during pregnancy was significantly related to IWB and depressive symptoms, whereas the amount of weight gained in pregnancy was not. Furthermore, IWB mediated the relationship between postpartum weight retention and postpartum depressive symptoms. These results add to the growing body of literature highlighting the detriment of weight stigma in the perinatal period and extend it further by presenting one potential explanation of how internalization of weight stigma can impact postpartum health.
Postpartum depression is one of the most common complication of pregnancy37 and has been associated with adverse outcomes affecting maternal health, child development, and society at large.38 In the current sample, women who reported the highest IWB evidenced the greatest depressive symptoms, which is consistent with prior research in other sample.20 This finding also relates to similar research demonstrating the mediating effects of IWB on the association between perceived body size and depressive symptoms.25 Taken together, our results enhance the literature that identifies IWB as a potential psychological phenomenon affecting the experience of mood symptoms during the challenging perinatal period.
IWB mediated the relationship between gestational weight retention and depressive symptoms. Although we recognize that cross-sectional data cannot determine causal relationships, mediation analysis allows for theoretical inference about underlying mechanisms of psychopathology. Our results suggest that retention of gestational weight after pregnancy may contribute to or reinforce negative thoughts and schemas women hold regarding body size. These thoughts, in turn, negatively affect self-concept, further contributing to depressive symptoms. IWB may be a mechanism for postpartum weight retention to exert its influence on depression. Conversely, symptoms of depression may contribute to negative core self-evaluations (ie, personal evaluations of self and ability) that interact with self-stigma and lead to the “why try” effect, or the negative impact on self-efficacy and related poor goal attainment that is driven, in part, by self-stigma.39 Negative core self-evaluations and expectations for further stigma may contribute to health care avoidance and negative physical and psychological health consequences, including weight gain and weight retention.40 Regardless of directionality, our results make it clear that postpartum retention of gestational weight needs to be included in the assessment of perinatal health.
Importantly, the relationship among IWB and weight change surrounding pregnancy is likely multidirectional. It would be helpful to understand how IWB changes from prepregnancy to postpartum, as IWB likely influences self-efficacy for pregnancy-specific health behaviors that could impact weight. A history of depression prepregnancy is also a well-known risk factor for depression in the postpartum period.37 Information regarding participants’ mental health history was not collected in this study. Postpartum people also face additional challenges with weight loss following birth and recovery, including limited resources (eg, time, support), low energy and motivation, and low priority ratings of weight management.7 Future studies may address these limitations by employing a longitudinal, repeated measures design that follows women’s weight-related attitudes, psychological distress, and changes in weight over the course of pregnancy and the postpartum period.
Although the current study assessed internalization of biased attitudes regarding weight, we must also acknowledge the likely influence of stigma experienced from outside sources. Participants in this study were residents of the United States. Western cultural beliefs about attractiveness for women and the “thin ideal” likely perpetuate the unrealistic expectations and goals about their postpartum body shape and weight.41,42 These weight-based judgments are often perpetuated by entertainment and health promotion media content.43 Perinatal health providers also report fewer positive attitudes toward caring for overweight/obese pregnant women and perceive them as having poor self-management behaviors, a pattern that exists even among health care providers who self-reported having few weight-stigmatizing attitudes.12,44 Experience of weight-based discrimination from a multitude of sources has been associated with maternal depressive symptoms and increased gestational weight gain and retention.45,46 Measure of external stigma experiences will be necessary to better elucidate the complexities of weight stigma and mental health and understand the differential impacts of external and internal weight bias. It may also be beneficial to include training and education in implicit/explicit bias and obesity in clinical training curricula for perinatal care providers.47
We must acknowledge several additional limitations of this investigation. First, weight and height were self-reported, and women were asked to recall their perinatal weights. Young women are more likely to underreport their weight.48 Perceptions of weight and body image are also important variables to consider, as prior research has supported stronger associations between IWB and self-perceived weight compared with objective weight.25 Second, this sample was highly educated, affluent, and composed almost entirely of white women. Although IWB was correlated with educational attainment and income in our sample, our results may not generalize to women of lower socioeconomic status and/or other racial and ethnic backgrounds. Importantly, there are cultural variations in expectations of weight and weight management,49 and postpartum IWB may differentially affect women according to racial and ethnic identity. Replication of the current study among racially, ethnically, socioeconomically, and gender-diverse individuals will be important to investigate group-specific factors that may contribute to the association between perinatal weight and psychosocial well-being.
Finally, we did not collect data regarding medical conditions and treatment before, during, or after pregnancy. Women who experience perinatal complications (eg, gestational diabetes) or psychiatric conditions (eg, prenatal depression, disordered eating) have a more complicated relationship with weight changes in pregnancy, are at higher risk of postpartum depression, and may be more likely to experience stigma.50,51 Furthermore, parity is a complicated issue that was assessed with a single survey item in this study; however, postpartum experience will likely vary based on number of children living in the home, maternal and child health status, and sociocultural parenting experiences (eg, grief, social support). Future research should address the varying experiences of women with perinatal medical complications and their likely influence on weight, the postpartum experience, and identity.
CONCLUSION
Postpartum women experience significant sociocultural pressure to “lose the baby weight” and achieve a body shape consistent with the thin ideal. Negative societal messages about weight status can become internalized and lead to negative psychological and behavioral outcomes. Although the experience of IWB and its relationship to psychological outcomes has been extensively explored in other populations, this is the first investigation of IWB and its impact on postpartum mental health.
On average, IWB in this sample was similar to that reported in prior publications investigating IWB across a range of body weights; however, the novel finding that IWB significantly increased as percentage of body weight of pregnancy-specific weight gain was retained at 6 to 12 months postpartum has important clinical implications. This finding indicates that the perinatal period may be an apt time for IWB to either develop or worsen, but it could also be a time for effective preventive efforts. First, our results suggest that clinical assessment of patients’ attitudes toward gestational weight and expectations for postpartum weight changes should be routinely included in prenatal care. These topics, along with routine depression screening, should be revisited in the postpartum period. By pointedly addressing perinatal weight and weight change, the perinatal care provider identifies these topics as common and important concerns. With appropriate clinical skill and sensitivity, the provider is also able to create a safe and trusting clinical environment. For patients who do disclose negative self-directed attitudes regarding pregnancy-related bodily changes, partnering with mental health professionals and perhaps integration psychological care into the prenatal clinic can offer an avenue for both prevention and treatment of perinatal IWB and depression. In addition to programs designed to assist women in achieving and maintaining a healthy postpartum weight to minimize perinatal risk, assessment and intervention around IWB could be additionally beneficial for improved psychological outcomes and quality of life.
Quick Points.
Greater amounts of gestational weight retained after giving birth were associated with higher reported internalized weight bias and depressive symptoms.
Internalized weight bias mediated the relationship between postpartum weight retention and depressive symptoms.
Individuals may be more susceptible to internalized weight bias during the perinatal period, which may serve as a window for prevention and intervention.
ACKNOWLEDGMENTS
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The results of this study were presented at the 40th Annual Meeting and Scientific Sessions of the Society of Behavioral Medicine; March, 2019; Washington, DC (Sharp M, Carels R, Dolbier C. Testing a process model of internalized weight bias in women during the postpartum period. Annals of Behavioral Medicine. 2019;53[Supplement 1]).
Footnotes
CONFLICT OF INTEREST
The authors have no conflicts of interest to disclose.
REFERENCES
- 1.Dayan F, Javadifar N, Tadayon M, Malehi AS, Komeili Sani H. The relationship between gestational weight gain and postpartum depression in normal and overweight pregnant women. J Pregnancy. 2018;2018:9315320. doi: 10.1155/2018/9315320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hartley E, Hill B, McPhie S, Skouteris H. The associations between depressive and anxiety symptoms, body image, and weight in the first year postpartum: a rapid systematic review. J Reprod Infant Psychol. 2018;36(1):81–101. doi: 10.1080/02646838.2017.1396301 [DOI] [PubMed] [Google Scholar]
- 3.Downs DS, DiNallo JM, Kirner TL. Determinants of pregnancy and postpartum depression: prospective influences of depressive symptoms, body image satisfaction, and exercise behavior. Ann Behav Med. 2008;36(1):54–63. doi: 10.1007/s12160-008-9044-9 [DOI] [PubMed] [Google Scholar]
- 4.Roomruangwong C, Kanchanatawan B, Sirivichayakul S, Maes M. High incidence of body image dissatisfaction in pregnancy and the postnatal period: associations with depression, anxiety, body mass index and weight gain during pregnancy. Sex Reprod Healthc. 2017;13:103–109. doi: 10.1016/j.srhc.2017.08.002 [DOI] [PubMed] [Google Scholar]
- 5.Martin JA, Hamilton BE, Osterman MJK, Driscoll AK. Births: final data for 2018. Natl Vital Stat Rep. 2019;68(13):1–47. [PubMed] [Google Scholar]
- 6.Goldstein RF, Abell SK, Ranasinha S, et al. Association of gestational weight gain with maternal and infant outcomes: a systematic review and meta-analysis. JAMA. 2017;317(21):2207–2225. doi: 10.1001/jama.2017.3635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McKinley MC, Allen-Walker V, McGirr C, Rooney C, Woodside JV. Weight loss after pregnancy: challenges and opportunities. Nutr Res Rev. 2018;31(2):225–238. doi: 10.1017/S0954422418000070 [DOI] [PubMed] [Google Scholar]
- 8.Kominiarek MA, Seligman NS, Dolin C, et al. Gestational weight gain and obesity: is 20 pounds too much? Am J Obstet Gynecol. 2013;209(3):214.e1-–214.e11.. doi: 10.1016/j.ajog.2013.04.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Incollingo Rodriguez AC, Dunkel Schetter C, Tomiyama AJ. Weight stigma among pregnant and postpartum women: a new context of stigmatization. Stigma Health. 2020;5(2):209–216. doi: 10.1037/sah0000191 [DOI] [Google Scholar]
- 10.Ringel MM, Ditto PH. The moralization of obesity. Soc Sci Med. 2019;237:112399. doi: 10.1016/j.socscimed.2019.112399 [DOI] [PubMed] [Google Scholar]
- 11.Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;9(12):788–805. doi: 10.1038/oby.2001.108 [DOI] [PubMed] [Google Scholar]
- 12.Mulherin K, Miller YD, Barlow FK, Diedrichs PC, Thompson R. Weight stigma in maternity care: women’s experiences and care providers’ attitudes. BMC Pregnancy Childbirth. 2013;13:19. doi: 10.1186/1471-2393-13-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nippert KE, Tomiyama AJ, Smieszek SM, et al. The media as a source of weight stigma for pregnant and postpartum women. Obesity. 2021;29(1):226–232. doi: 10.1002/oby.23032 [DOI] [PubMed] [Google Scholar]
- 14.Hunger JM, Major B. Weight stigma mediates the association between BMI and self-reported health. Health Psychol. 2015;34(2):172–175. doi: 10.1037/hea0000106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Neiterman E, Fox B. Controlling the unruly maternal body: losing and gaining control over the body during pregnancy and the postpartum period. Soc Sci Med. 2017;174:142–148. doi: 10.1016/j.socscimed.2016.12.029 [DOI] [PubMed] [Google Scholar]
- 16.Lovering ME, Rodgers RF, George JE, Franko DL. Exploring the tripartite influence model of body dissatisfaction in postpartum women. Body Image. 2018;24:44–54. doi: 10.1016/j.bodyim.2017.12.001 [DOI] [PubMed] [Google Scholar]
- 17.Watson B, Fuller-Tyszkiewicz M, Broadbent J, Skouteris H. The meaning of body image experiences during the perinatal period: a systematic review of the qualitative literature. Body Image. 2015;14:102–113. doi: 10.1016/j.bodyim.2015.04.005 [DOI] [PubMed] [Google Scholar]
- 18.Durso LE, Latner JD. Understanding self-directed stigma: development of the weight bias internalization scale. Obesity (Silver Spring). 2008;16(Suppl 2):S80–S86. doi: 10.1038/oby.2008.448 [DOI] [PubMed] [Google Scholar]
- 19.Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity (Silver Spring). 2009;17(5):941–964. doi: 10.1038/oby.2008.636 [DOI] [PubMed] [Google Scholar]
- 20.Pearl RL, Puhl RM. Weight bias internalization and health: a systematic review. Obes Rev. 2018;19(8):1141–1163. doi: 10.1111/obr.12701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Corrigan PW, Watson AC, Barr L. The self-stigma of mental illness: implications for self-esteem and self-efficacy. J Soc Clin Psychol. 2006;25(8):875–884. doi: 10.1521/jscp.2006.25.8.875 [DOI] [Google Scholar]
- 22.Picco L, Lau YW, Pang S, et al. Mediating effects of self-stigma on the relationship between perceived stigma and psychosocial outcomes among psychiatric outpatients: findings from a cross-sectional survey in Singapore. BMJ Open. 2017;7(8):e018228. doi: 10.1136/bmjopen-2017-018228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peng L, She R, Gu J, et al. The mediating role of self-stigma and self-efficacy between intimate partner violence (IPV) victimization and depression among men who have sex with men in China. BMC Public Health. 2020;20(1):2. doi: 10.1186/s12889-019-8125-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van der Kooij YL, Kupková A, den Daas C, et al. Role of self-stigma in pathways from HIV-related stigma to quality of life among people living with HIV. AIDS Patient Care STDS. 2021;35(6):231–238. doi: 10.1089/apc.2020.0236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Decker KM, Thurston IB, Kamody RC. The mediating role of internalized weight stigma on weight perception and depression among emerging adults: exploring moderation by weight and race. Body Image. 2018;27:202–210. doi: 10.1016/j.bodyim.2018.10.004 [DOI] [PubMed] [Google Scholar]
- 26.Puhl RM, Himmelstein MS. Weight bias internalization among adolescents seeking weight loss: implications for eating behaviors and parental communication. Front Psychol. 2018;9:2271. doi: 10.3389/fpsyg.2018.02271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sienko RM, Saules KK, Carr MM. Internalized weight bias mediates the relationship between depressive symptoms and disordered eating behavior among women who think they are overweight. Eat Behav. 2016;22:141–144. doi: 10.1016/j.eatbeh.2016.06.002 [DOI] [PubMed] [Google Scholar]
- 28.Carels RA, Hlavka R, Selensky JC, Solar C, Rossi J, Caroline Miller J. A daily diary study of internalised weight bias and its psychological, eating and exercise correlates. Psychol Health. 2019;34(3):306–320. doi: 10.1080/08870446.2018.1525491 [DOI] [PubMed] [Google Scholar]
- 29.Pearl RL, Puhl RM. Measuring internalized weight attitudes across body weight categories: validation of the modified weight bias internalization scale. Body Image. 2014;11(1):89–92. doi: 10.1016/j.bodyim.2013.09.005 [DOI] [PubMed] [Google Scholar]
- 30.Skouteris H, Carr R, Wertheim EH, Paxton SJ, Duncombe D. A prospective study of factors that lead to body dissatisfaction during pregnancy. Body Image. 2005;2(4):347–361. doi: 10.1016/j.bodyim.2005.09.002 [DOI] [PubMed] [Google Scholar]
- 31.Dieterich R,Chang J, Danford C, Scott PW, Wend C, Demirci J. “The relationship between internalized weight stigma during pregnancy and breastfeeding: a prospective longitudinal study”. Obesity (Silver Spring, Md.). 2021;29(5):919–927. doi: 10.1002/oby.23139 [DOI] [PubMed] [Google Scholar]
- 32.Lee MS, Dedrick RF. Weight Bias Internalization Scale: psychometric properties using alternative weight status classification approaches. Body Image. 2016;17:25–29. doi: 10.1016/j.bodyim.2016.01.008 [DOI] [PubMed] [Google Scholar]
- 33.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–786. doi: 10.1192/bjp.150.6.782 [DOI] [PubMed] [Google Scholar]
- 34.Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis. 1st ed. The Guilford Press; 2013. [Google Scholar]
- 35.Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41(4):1149–1160. doi: 10.3758/BRM.41.4.114 [DOI] [PubMed] [Google Scholar]
- 36.Rasmussen KM, Yaktine AL, eds; Institute of Medicine (US) and National Research Council (US) Committee to Reexamine IOM Pregnancy Weight Guidelines. Weight Gain During Pregnancy: Reexamining the Guidelines. National Academies Press; 2009. [PubMed] [Google Scholar]
- 37.Accortt EE, Wong MS. It is time for routine screening for perinatal mood and anxiety disorders in obstetrics and gynecology settings. Obstet Gynecol Surv. 2017;72(9):553–568. doi: 10.1097/OGX.0000000000000477 [DOI] [PubMed] [Google Scholar]
- 38.Slomian J, Honvo G, Emonts P, Reginster JY, Bruyère O. Consequences of maternal postpartum depression: a systematic review of maternal and infant outcomes [published correction appears in Womens Health (Lond). 2019 Jan-Dec;15:1745506519854864]. Womens Health (Lond). 2019;15:1745506519844044. doi: 10.1177/1745506519844044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Corrigan PW, Larson JE, Rüsch N. Self-stigma and the “why try” effect: impact on life goals and evidence-based practices. World Psychiatry. 2009;8(2):75–81. doi: 10.1002/j.2051-5545.2009.tb00218.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hilbert A, Braehler E, Haeuser W, Zenger M. Weight bias internalization, core self-evaluation, and health in overweight and obese persons. Obesity (Silver Spring). 2014;22(1):79–85. doi: 10.1002/oby.20561 [DOI] [PubMed] [Google Scholar]
- 41.Clark A, Skouteris H, Wertheim EH, Paxton SJ, Milgrom J. The relationship between depression and body dissatisfaction across pregnancy and the postpartum: a prospective study. J Health Psychol. 2009;14(1):27–35. doi: 10.1177/1359105308097940 [DOI] [PubMed] [Google Scholar]
- 42.Thompson JK, Stice E. Thin-ideal internalization: mounting evidence for a new risk factor for body-image disturbance and eating pathology. Curr Dir Psychol Sci. 2001;10(5):181–183. doi: 10.1111/1467-8721.00144 [DOI] [Google Scholar]
- 43.Stanford FC, Tauqeer Z, Kyle TK. Media and its influence on obesity. Curr Obes Rep. 2018;7(2):186–192. doi: 10.1007/s13679-018-0304-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Johnson M, Campbell F, Messina J, Preston L, Buckley Woods H, Goyder E. Weight management during pregnancy: a systematic review of qualitative evidence. Midwifery. 2013;29(12):1287–1296. doi: 10.1016/j.midw.2012.11.016 [DOI] [PubMed] [Google Scholar]
- 45.Incollingo Rodriguez AC, Dunkel Schetter C, Brewis A, Tomiyama AJ. The psychological burden of baby weight: pregnancy, weight stigma, and maternal health. Soc Sci Med. 2019;235:112401. doi: 10.1016/j.socscimed.2019.112401 [DOI] [PubMed] [Google Scholar]
- 46.Incollingo Rodriguez AC, Tomiyama AJ, Guardino CM, Dunkel Schetter C. Association of weight discrimination during pregnancy and postpartum with maternal postpartum health. Health Psychol. 2019;38(3):226–237. doi: 10.1037/hea0000711 [DOI] [PubMed] [Google Scholar]
- 47.Puhl RM, Phelan SM, Nadglowski J, Kyle TK. Overcoming weight bias in the management of patients with diabetes and obesity. Clin Diabetes. 2016;34(1):44–50. doi: 10.2337/diaclin.34.1.4448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kuczmarski MF, Kuczmarski RJ, Najjar M. Effects of age on validity of self-reported height, weight, and body mass index: findings from the Third National Health and Nutrition Examination Survey, 1988–1994. J Am Diet Assoc. 2001;101(1):28–36. doi: 10.1016/S0002-8223(01)00008-6 [DOI] [PubMed] [Google Scholar]
- 49.Ciciurkaite G, Perry BL. Body weight, perceived weight stigma and mental health among women at the intersection of race/ethnicity and socioeconomic status: insights from the modified labelling approach. Sociol Health Illn. 2018;40(1):18–37. doi: 10.1111/1467-9566.12619 [DOI] [PubMed] [Google Scholar]
- 50.Nagpal TS, Tomiyama AJ, Incollingo Rodriguez AC. Beyond BMI: pregnancy-related weight stigma increases risk of gestational diabetes. Prim Care Diabetes. 2021;15(6):1107–1109. doi: 10.1016/j.pcd.2021.07.00251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wilson CA, Newham J, Rankin J, et al. Is there an increased risk of perinatal mental disorder in women with gestational diabetes? A systematic review and meta-analysis. Diabet Med. 2020;37(4):602–622. doi: 10.1111/dme.14170 [DOI] [PMC free article] [PubMed] [Google Scholar]


