Abstract
Objective
To consult providers and women patients of Assisted Reproductive Technologies regarding their preferences for the format, duration and content in the development of a group psychological intervention.
Methods
Providers and current and past women patients of Assisted Reproductive Technologies completed an online cross-sectional survey comprising items about session content, number, frequency, timing, format, delivery mode and inclusion of experiential practice of psychological strategies to promote well-being.
Results
Eight providers, 51 current women patients and 51 women who previously underwent Assisted Reproductive Technologies participated. Sixty-two percent of participants indicated a group psychological program would be helpful; and 34% thought it may be helpful. Face-to-face was the preferred delivery mode (42%). Seventy-one percent preferred 60-min sessions held fortnightly (64%), with six sessions most acceptable (24%). Most respondents (74%) felt group participants would likely complete at-home practice. Detailed thematic content from participants highlighted a complex range of consumer challenges. Relevant behaviour change techniques were verified, with those to be included identified as: feedback and monitoring, regulation, self belief, reward and threat, natural consequences, identity, support, shaping knowledge, and comparison of outcomes.
Conclusion
Providers and patients were supportive of the development of a group psychological intervention to provide support for women undergoing Assisted Reproductive Technologies.
Innovation
The results of this study provide insight informing the co-design of a group psychological program for women with infertility.
Keywords: Infertility, Assisted reproductive technologies, Group psychological intervention, Women, Behaviour change techniques
Highlights
-
•
Consultation with 2 stakeholder groups to inform a group psychological intervention
-
•
Support existed for a group psychological intervention during fertility treatment
-
•
Preferred group format was six in-person, fortnightly, 60-min sessions
-
•
Key group content and behavior change techniques for inclusion were identified
1. Introduction
Infertility affects approximately 15% of the global population of reproductive age [1], including approximately 7% of women in Australia [2] and one in four couples worldwide [3,4]. The World Health Organisation defines infertility as the inability to conceive following 12 months or more of regular, unprotected sex [4]. The burden associated with infertility can be emotional [5,6], social, relational [7], and financial, and is often experienced most significantly by the person required to undergo treatment via Assisted Reproductive Technologies (ART) [8]. Namely, the woman participating in ART. People undergoing fertility treatment often receive medical advice, financial options, and routine medical care; however, targeted emotional support is not routinely provided [9].
It is well-documented that infertility and the associated medical treatment adversely impact peoples' well-being and stress levels [[10], [11], [12]], and some research has identified a relationship between distress levels and pregnancy rates [5,6,[13], [14], [15], [16], [17]]. In contrast, other studies have failed to identify a relationship between distress and pregnancy rates [5,18]. However, despite these equivocal results, improvements in mental health and pregnancy rates are routinely observed following psychological intervention (whether group-based, educational-based or individually facilitated) compared to treatment as usual or waitlist controls [19].
Despite these benefits, a recent meta-analysis [19] found no evidence-informed, group-based psychological interventions evaluated in Australia or New Zealand for women undergoing ART. The absence of such interventions is disappointing, given that the same review highlighted noteworthy improvements in mental health and pregnancy outcomes following the completion of a group-based psychological intervention [19]. This review also highlighted that group mindfulness-based interventions and Cognitive Behavioural Therapy approaches were the most efficacious and that promising results exist for Acceptance Commitment Therapy [19].
Further, the results of Warne et al.'s [19] meta-analysis highlighted that group programs longer than nine hours demonstrated better outcomes for women's key change objectives of improved mental health and pregnancy outcomes. Effective approaches target negative thinking and feelings, develop present moment awareness, acceptance and defusion-like strategies, and utilise visualisation, relaxation or mindfulness training exercises [19]. Participants also describe the group support as beneficial [19]. However, inconsistencies exist when assessing outcomes, and behaviour change techniques (BCTs) employed are seldom reported consistently across studies [19].
BCTs should be key considerations when designing and reporting interventions to enhance understanding of interventions. Categorising and identifying the techniques utilised in an intervention improves replicability and offers insights into mechanisms of change [20,21]. Michie and colleagues [21] developed a taxonomy of 93 BCTs categorised into 16 clusters, which offer value in designing interventions. Within Warne et al.'s [19] meta-analysis, studies that demonstrated improvements in depression, anxiety, fertility stress, and if reported, pregnancy outcomes utilised BCTs from the following clusters: Goals and planning; Feedback and monitoring; Social support; Shaping knowledge; Regulation; Associations; Identity; Self-belief; and Covert learning. In order to ensure the quality and feasibility of the group psychological intervention we are developing, in the current study, we aimed to clarify the acceptability of these identified BCTs and explore additional content areas to include. Further, our intervention development will be guided by a modified intervention mapping (IM) [22] approach to improve intervention quality and acceptability.
As part of a person-centred and modified IM approach to intervention development, consultation with those who will undertake an intervention is recommended. Limited research in Australia has sought to ascertain the psychosocial supports that people treated with ART might need. In a preliminary study, Read et al. [23] found that psychological support to cope with relationship issues, stress, understanding and sharing experiences, and practical information were valued. Further, several couples indicated that social engagement or mentorship with others who had completed ART might be useful. Read et al. [23] further recommended consulting people treated with ART about whether they needed support and, if so, what type of psychosocial support would be most useful. This advice was given beyond that of European Society of Human Reproduction and Embryology [24], which provided 120 recommendations to guide clinic staff in recognising and responding to the psychosocial needs of people undertaking ART. However, given the changing social, political and economic climate of ART due to the progress of medical knowledge, as well as the impact of the COVID-19 pandemic since those recommendations, we aimed to consult women treated with ART and ART providers and clarify the outcome determinants, performance objectives, and perspectives about our proposed group psychological intervention.
The current survey was designed to inform the development of a group psychological intervention program that may improve the mental health, well-being and outcomes of women undergoing ART. Therefore, we only consulted women who have or were being treated with ART, as they are the target audience for the group psychological intervention under development. Further research will likely consider developing a program for all parties participating in ART; however, the current survey was interested in the acceptability, feasibility, and content to be included in a group program for women receiving ART.
2. Methods
Our study employed a mixed method cross-sectional design involving purposive sampling of Australian ART women treated with ART (past and current) and ART providers. We were interested in the perceived acceptability and usefulness of various aspects of skill development and preferences regarding program session content, number, frequency, timing, format, and delivery mode (individual, group, face-to-face, or online). We applied a modified six-step IM approach, where the current survey served as a needs assessment, Step 1 of the model, while the survey results were utilised to inform Step 2 of the model, defining the behavioural determinants for change. In addition, the results were utilised to inform an intervention framework that could be assessed and replicated.
2.1. Intervention planning
The current research drew on a person-based [25], modified IM framework and the Information-Motivation-Behaviour (IMB) skills model to guide intervention development [26]. Namely, elicitation: conducting a needs assessment, stating outcomes and performance objectives; intervention: utilising theory-based intervention methods, developing an intervention program in consultation with people treated with ART and ART providers adopting and implementing the program; and evaluation: statistically evaluating the program and its effectiveness.
2.2. Behaviour change techniques taxonomy
We utilised BCTs as per Michie et al.'s [21] taxonomy to explore the acceptability of previously identified BCTs and categorise the types of BCTs that would be preferred in a group psychological intervention. We decided to apply this taxonony to improve the quality of our research as the BCTs were pre-defined, can improve the standardisation, reporting, and replicability of the group intervention being developed, and may provide information to illustrate the mechanisms associated with change [21]. The information gained enabled us to form a logic model to be applied in developing the psychological group intervention.
2.3. Participants
Participant eligibility criteria included Australian women treated with ART (past and current) and ART providers. Women experiencing infertility who had not previously or were not currently receiving treatment (i.e., their partner underwent treatment) and male patients treated with ART were excluded.
2.4. Study design
Following ethical approval (HREC-2021-047), we distributed information about the study and a link to the online survey to fertility clinics and fertility support organisations, asking them to share the information about the study with relevant parties. Recruitment also occurred through social media and passive snowball sampling.
The voluntary survey was hosted on Qualtrics from April 2021 until April 2022. After reading the study information in the survey premable, potential participants responded to consent questions; those who provided consent progressed to the survey, while those who did not consent were directed to an exit page.
2.5. Measures
The study-specific survey, using a mixture of Likert-scale and open-text responses, was designed to canvas the perspectives of women treated with ART (past or current) and ART providers regarding content to be included in a group psychological intervention, program duration (including session length and number), and delivery mode (including group, individual, face-to-face or online). The survey comprised questions under the headings of background information including demographic information, consultation regarding psychological group program development canvassing acceptability, type, frequency, duration, and format of exercises to be utilised in a group intervention, consultation regarding psychological group program content including specific evidence-based skill development activities of relevance based on individual experience, and feedback clarifying participant willingness to be contacted for future consultation/research. Demographic information for women treated with ART included relationship status, educational background, sexual orientation, ethnicity, diagnosis, length of infertility, time since commencing treatment, and coping strategies. For ART providers, information regarding educational background, time within the ART field, ethnicity, and relationship status was gathered.
2.6. Data analysis
Quantitative data were analysed utilising SPSS version 27. Descriptive statistics were reported with 95% confidence intervals, and a p-value < .05 was considered statistically significant. Categorical data were expressed as percentages. Normally distributed continuous data were reported as means, with standard deviations. Comparisons were made between women treated with ART (past and current) and ART providers.
Qualitative open-text response data were analysed manually using directed content analysis (Hsieh & Shannon, 2005). This approach was employed to directly explore, confirm or expand categories identified by women patients. The first author read, coded and developed categories. Then, the second and third authors reviewed and verified the data obtained by cross-referencing the identified content with the qualitative responses.
3. Results
One hundred and seventeen people commenced the survey, with 102 women treated with ART (51 past and 51 current) and eight ART providers completing the survey (a completion rate of 94%; See Table 1, Table 2). Among the eight ART providers, five were female, and three were male; 25.0% were specialist doctors, 12.5% were nurses, 50.0% were counsellors, and 12.5% were embryologists. Also, one provider had previously undergone fertility treatment. On average, the providers had been employed in ART for 15 years (range 5–30 years; SD = 8.02).
Table 1.
Participant Demographic Characteristics.
| n (%) |
|||
|---|---|---|---|
| ART Recipient |
ART Provider |
||
| Current | Past | ||
| Ethnicity | |||
| Oceania (Australian, New Zealand, South Pacific) | 39 (73.6%) | 46 (85.2%) | 4 (50.0%) |
| European | 11 (20.7%) | 4 (7.4%) | 2 (25.0%) |
| Asian | 2 (3.8%) | 1 (1.9%) | 0.0% |
| People of the Americas | 1 (1.9%) | 1 (1.9%) | 0.0% |
| Africa | 0.0% | 1 (1.9%) | |
| Othera | 0.0% | 0.0% | 2 (25.0%) |
| Sexual Orientation | |||
| Heterosexual | 42 (82.4%) | 49 (96.1%) | – |
| Homosexual | 6 (11.8%) | 1 (2.0%) | – |
| Bisexual | 2 (4.9%) | 0.0% | – |
| Pansexual | 1 (2.0%) | 0.0% | – |
| Otherb | 0.0% | 1 (2.0%) | – |
| Educational Level | |||
| Less than year 12 or equivalent | 3 (5.9%) | 3 (5.9%) | 0.0% |
| Year 12 or equivalent | 5 (9.8%) | 2 (3.9%) | 0.0% |
| Trade/apprenticeship/Certificate | 6 (11.8%) | 5 (9.8%) | 0.0% |
| Diploma | 11 (21.6%) | 9 (17.7%) | 0.0% |
| University | 24 (47.1%) | 31 (60.8%) | 6 (75.0%) |
| Otherc | 2 (3.9%) | 1 (2.0%) | 29 (25.0%) |
| Employment | |||
| Part time | 14 (24.0%) | 19 (37.3%) | |
| Full time | 32 (64.0%) | 27 (52.9%) | |
| Unemployed | 4 (8.0%) | 1 (2.0%) | |
| Some of the time (time off due to ART treatment) | – | 4 (7.8%) | |
Note: aItalian/British/Australian; Central European;blesbian;cpost graduate; honours; FRANZCOG CREI.
Table 2.
Fertility Treatment Details According to Treatment Status for Women Treated with ART.
| n (%) |
|||
|---|---|---|---|
| Current | Past | ||
| Infertility Type | Combined/Both female and male factor difficulties | 5 (10%) | 10 (19.6%) |
| Unexplained | 14 (28%) | 10 (19.6%) | |
| Othera | 8 (16%) | 2 (3.9%) | |
| Complementary Therapies utilised (multiple responses provided) | Acupuncture | 22 (23%) | 24 (28%) |
| Naturopathy | 9 (9%) | 5 (6%) | |
| Nutritionist | 5 (5%) | 8 (9%) | |
| Hypnosis | 2 (2%) | 4 (5%) | |
| Massage | 16 (16%) | 8 (9%) | |
| Counselling | 12 (12%) | 9 (11%) | |
| Supplements | 23 (24%) | 16 (19%) | |
| Relaxation | 8 (8%) | 9 (11%) | |
| Other b | 0 (0%) | 2 (2%) | |
Note.aNot specified; bhomeopathy; reflexology.
The average duration of ART participation was 18 months (SD = 13.8 months; range 1–72 months) for current and 29 months (SD = 31.3; range 2–120 months) for past women treated with ART (F (1,99) = 4.977, p = .028). While the average time to conception was 3.6 years (SD = 2.49; range 1–15 months) and 4.8 (SD = 3.14; range 0.5–0.17 months) for current and past women treated with ART, respectively (F (1,99) = 5.363, p = .023). Among women treated with ART, 80.0% reported primary infertility (73.0% and 86.0% among current and past women treated with ART, respectively). In comparison, 21.0% of women treated with ART reported secondary infertility (27.0% and 14.0% in current and past women treated with ART, respectively; F (1,101) = 2.966, p = .088). Only 56% of women treated with ART had received a specific infertility diagnosis; 37% were unsure of their diagnosis. Female factors were the predominant cause of infertility (45.0%); 24.0% reported unexplained infertility. Many women treated with ART (56.0%) accessed complementary therapies while trying to conceive, with 23.7% of women currently receiving ART using supplements and 28.2% of women treated with ART in the past having used acupuncture. For 72.0% of women treated with ART, the treatment had strained their finances.
Women treated with ART had also experienced mental health difficulties (see Table 3), with 39.2% of current and 51.0% of past women treated with ART reporting a mental health diagnosis (Depression, Anxiety, Post Traumatic Stress Disorder or Personality Disorder; X2(1, N = 102) = 1.425, p = .23). Only 25.0% of current patients and 50.0% of past women treated with ART reported their mental health condition had resolved (X2(1, N = 46) = 2.966, p = .09). Twenty percent of current and 34.6% of past women treated with ART reported experiencing onset during ART treatment. Current and past women treated with ART who had experienced mental health difficulties had consulted a psychologist (80.0% and 76.9%, respectively). Just over half of women (54.3%) had received counselling during their fertility treatment, with most accessing support within their fertility clinic (48.4%) or from a psychologist in the community (42.0%).
Table 3.
Mental Health Status of Women Treated with ART.
| n (%) |
||||
|---|---|---|---|---|
| Current ART Recipient |
Past ART Recipient |
|||
| Yes | No | Yes | No | |
| Diagnosed with a mental health disorder | 20 (39.2%) | 31 (60.8%) | 26 (51.0%) | 25 (49.0%) |
| Occurred during ART treatment | 4 (20.0%) | 9 (34.6%) | ||
| Occurred before or after ART treatment | 16 (80.0%) | 17 (65.4%) | ||
| Depression | 11 (55.0%) | 19 (73.1%) | ||
| Anxiety | 17 (85.0%) | 21 (80.8%) | ||
| Personality | 0 | 2 (7.7%) | ||
| Other | 3 (15.0%) a | 0 | ||
| Sought treatment from a psychologist | 16 (80.0%) | 20 (76.9%) | ||
| Sought treatment from a psychiatrist | 4 (20.0%) | 5 (19.2%) | ||
| Sought treatment from other (counsellor) | 4 (20.0%) | 5 (19.2%) | ||
| Did not seek treatment | 1 (5.0%) | 2 (7.7%) | ||
| Other | 1 (5.0%)b | 2 (7.7%)c | ||
Note.aPTSD; ADHD bAs a teenager c GP; Social Worker.
3.1. Perspectives on group intervention content, duration and delivery mode
Regarding intervention content, all participants provided multiple responses and identified skill development for managing difficult feelings (13.0%) and unhelpful thoughts (12.9%) as important. Women treated with ART preferred that content also included skills that taught them to “let go of those things that cannot be controlled” (12.4%), while ART providers preferred strategies to “focus on the things that can be controlled” (12.1%) and providing information around physical health and how it relates to mental health (12.1%; see Table 4). Overall, addressing present moment awareness (6.3%), identifying what matters most (4.3%), developing skills to separate from the fertility diagnosis (6.3%) and staying committed to goals (7.8%) were viewed as less important for inclusion in the intervention.
Table 4.
Psychological and Emotional Difficulties to be Addressed.
| n (%) |
|||||
|---|---|---|---|---|---|
| Current |
Past |
||||
| recipients of ART | Providers | Overall | BCT | ||
| How to manage difficult feelings | 34(11.4%) | 38(12.4)% | 5(15.2%) | 77(12.0%) | Feedback and monitoring; Regulation |
| Skills to keep in the moment | 20(6.7%) | 19(6.2%) | 2(6.1%) | 41(6.4)% | |
| How to manage unhelpful/difficult thoughts | 35(11.7%) | 36(11.7)% | 5(15.2%) | 76(11.9)% | Feedback and monitoring; Self belief; Regulation |
| How to identify what matters most | 16(5.4%) | 14(4.6%) | 1(3.0%) | 31(4.9%) | |
| Stepping outside of the fertility experience | 26(8.7%) | 27(8.8%) | 3(9.1%) | 56(8.8)% | |
| Skills to help in separating from the fertility diagnosis | 25(8.4%) | 23(7.5%) | 1(3.0%) | 49(7.7)% | |
| How to keep focussed on the things that can be controlled | 26(8.7%) | 33(10.8%) | 4(12.1%) | 63(9.9%) | Reward and threat |
| How to let go of those things that cannot be controlled | 37(12.4%) | 38(12.4%) | 3(9.1%) | 78(12.2%) | Identity; Self belief |
| How to stay motivated and committed to goals | 22(7.4%) | 21(6.8%) | 3(9.1%) | 46(7.2%) | |
| Gaining more information about the psychological impact of infertility | 31(10.4%) | 29(9.5%) | 2(6.1%) | 62(9.7)% | |
| Information about physical health and how it is related to mental health/wellbeing | 27(9.0%) | 29(9.5%) | 4(12.1%) | 60(9.4%) | Shaping knowledge; Natural consequences |
Note. Multiple responses permitted; BCT – behaviour change technique cluster; bold = all ART recipients' and ART providers' preference; bold and underlined: all ART recipients' preference; italics and bold = ART providers' preference.
Table 5 reports participants' preferences for the group intervention format. Group leader-led discussions with group involvement was the most preferred format (41.5%), followed by opportunities to share personal experiences with infertility in small groups (25.6%). BCTs relevant to these preferences included Shaping knowledge; Comparison of outcomes; and Social support.
Table 5.
Participants' Group Intervention Format Preferences (Women and ART providers combined).
Note. Bold and shaded % highlights the order of ranking preferences; aNot specified.
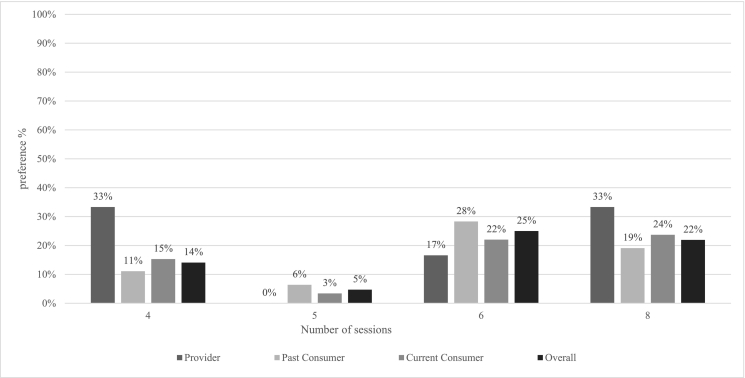
Most participants responded favourably to a group intervention for women undergoing infertility treatment, with 62.0% indicating it “would be” and 37.0% indicating it “may be” helpful; only one participant believed it would not be helpful. Participants' preferences about session delivery mode and frequency are reported in Table 6, session duration in Fig. 1, and the number of sessions in Fig. 2. Regarding the number of sessions, ART providers suggested four sessions (33.3%), women currently receiving ART seven sessions (23.8%), and women who received ART in the past six sessions (28.6%). Overall, the preferred mode of delivery across the three groups was face-to-face (41.5%), with six (25.0%), 60-min sessions (70.2%), held fortnightly (63.0%).
Table 6.
Preferences Regarding Session Delivery Mode and Frequency.
Note. Bold and shaded highlights the preferred choice; aboth online formats; online but face-to-face would be best; face-to-face or online; group work does not suit sensitive topics like surrogacy b both online and face-to-face; face-to-face and option for online; online/self directed, with option to join face-to-face conline and face-to-face would have balanced benefits; dMonthly; e Three weekly; Fortnightly or Monthly; Monthly; depends on the individual; Weekly or fortnightly fgroup decides.
Fig. 1.
Preferences Regarding Duration of Sessions.
Fig. 2.
Preferences Regarding Number of Sessions.
Note. Other # continuous; open ended; indeterminant; with ongoing check ins; depends on the individual; 12; 4–6; before, during and after; not specified.
3.2. Perspectives on at home practice completion
Most participants (80.0%) reported that women would be likely to utilise at home practice, would find including audio files useful (57.0%), and suggested that women would listen to those files (65.0%). Most participants (73.0%) also suggested that women would commit to daily practice (see Table 7).
Table 7.
Perceptions Regarding Women's Likely Engagement in at Home Practice and Its Perceived Usefulness.
Note. Bold and shaded represents overall preference
3.3. Content analysis
3.3.1. Categories of fertility treatment experiences
Participants provided open-text responses to questions concerning what was helpful, unhelpful or would likely be helpful for women undergoing ART treatment. The common categories are descrbed below.
3.3.2. Mental health
Mental health included reports of isolation, anxiety, depression, stress, poor coping, feeling out of control, experiencing unhelpful comparisons or comments, and overall lowered quality of life. The notion of “putting things on hold” and “feeling like it's a taboo topic” was raised by one provider and numerous women treated with ART. Further, the “lack of validation of feelings particularly those related to grief” was often reported by providers and women. ART as an “emotional roller coaster” was also commonly referenced regarding mental health.
3.3.3. Lowered self-esteem
Women reported comparing themselves to others without infertility as unhelpful for their mental health. They highlighted feelings of guilt, self-blame, shame, and stigma associated with fertility treatment contributing to anxiety, depression, and loneliness which were frequently reported as being ineffectively addressed by fertility clinics. In addition, women reported feeling “isolated, alone, unprepared", and that fertility treatment is “taboo” or “not spoken about”. Finally, women reported difficulties regarding the burden of treatment falling to them and medical care not being patient-centric nor considering mental health.
3.3.4. Clinical coldness or detachment from health practitioners
Treatment also was described as “impersonal”, “cold, clinical”, with an over-emphasis on “medical language” or the “business” side of infertility. One woman expressed that “being looked at as a uterus/egg/hormone/blood test” impacted her significantly, and women generally noted an overfocus on the medical side of treatment, reportedly leading to feeling that “they [health practitioners] almost forget about mental health”. Health practitioners “lack of empathy” or validation of the emotional impact of treatment was noted as problematic; many women indicated that such approaches contributed to negative self-talk, blaming statements, guilt, and “feeling like we need to keep it a secret”. One woman described “dismissive and unkind medical professionals” as particularly unhelpful and another articulated “being treated as a number or statistic rather than an individual” and “professionals trying to reduce anxiety/worry by withholding or minimising information”.
3.3.5. Feeling unsupported
Women described feeling unsupported, “isolated”, alone, ill-informed or under-prepared for treatment. They additionally identified that health practitioners' language often did not consider the emotional experience of infertility treatment. The two week wait was commonly reported as particularly isolating; one woman reported feeling “alone really from the practice for those two weeks”. Waiting times for appointments, treatment, counselling or outcomes were also commonly described as unhelpful. Participants also highlighted a “lack of support (access or availability), lack of strategies to manage thoughts and feelings… social isolation, stigma against asking for help for mental health” as challenging and unhelpful. In support of that, one provider additionally identified difficulties in establishing therapeutic rapport with their clinician as unhelpful, while another similarly highlighted challenges with the “patient/doctor relationship” and the “clinic/client relationship”, whereby a “partnership” is not encouraged.
3.3.6. Insensitivity
Women and providers identified “insensitive comments” from family, friends, acquaintances, or ART staff as unhelpful. These included sub-categories such as:
Positive thinking: “everything will be okay;” “you are young”.
Relax:“relax and it will happen” or “relax and have a holiday and you will become pregnant!”
Fate/patience:“it is what it is” or “you will have kids when the time is right”.
Opinions: “IVF will work”; “eat well, exercise, stay positive”; “have you held your legs in the air after intercourse?”
Dismissal of feelings: “Use of medical language versus compassionate language by fertility staff (Referring to a loss as ‘not a real miscarriage’ because the fetus didn't reach a certain milestone etc)”
3.3.7. Financial burden
Women frequently referenced “the financial burden that comes with” treatment. They described experiencing a push to continue treatment when a cycle was unsuccessful, with limited support from fertility clinics regarding the emotional impact of the unsuccessful cycle on their mental health. One woman provided the following response: the “clinic assuming there is capability for patients to undertake more rounds. Clinics only looking at the physical numbers or results from a patient not the holistic aspect to patient care. Patients feeling like a number on a factory conveyor belt.” Another woman articulated the financial burden impacting their ability to seek additional support for their mental health: the “financial impact that means it's hard to get extra support as it is expensive” and another stating the “cost of services” and “managing that cost amongst general life costs” as problematic.
3.3.8. Support
Conversely, women indicated that they had found support groups, moderated online forums, and check-in emails or support beneficial for their mental health and well-being. Talking with other women who had been through infertility treatment and access to counselling timed with treatment were also reported as useful or likely to be useful. For example, women indicated value in “programmed access to counselling… schedule counselling as they do blood tests and scans” and timing these sessions in line with “possible failure points”.
3.3.9. Strategy development
Specific areas to be addressed included support around uncertainty, normalising feelings, strategies to manage people's questions concerning pregnancy and how to separate infertility and ART from other aspects of one's life, ways of coping, and techniques to separate negative feelings/anxiety from life. Participants also noted a need to have access to mental health support networks and knowledge about where to access support in times of need –“when things go wrong but also when things go right”.
3.3.10. Proactive actions
Participants additionally indicated that meditation, yoga, sharing the emotional load with others, outside interests or hobbies, hypnosis, and finding a knowledgeable and kind doctor were helpful.
3.4. Behavioural change techniques identified
Table 8 highlights the BCT clusters and categories identified in the open-text responses of women treated with ART. Women noted distraction/avoidance (Antecedents) and activities that resulted in an alternative reward behaviour (Scheduled consequences) as effective strategies when managing inferility distress.
Table 8.
Identified BCTs and Associated Planned Interventional Approach.
| BCT Cluster | Behaviour Change Technique | Potential Approach to Include in the Group Intervention |
|---|---|---|
| Feedback and monitoring | Self monitoring of outcomes of behaviour Discrepancy between current behaviour and goal Commitment |
Value identification Committed action Visualisation Hypnosis Acceptance Sitting with distress Managing difficult thoughts and feelings - defusion |
| Regulation | Reduce negative emotions | Acceptance Distress tolerance/sitting with distress Mindfulness of feelings Present moment focus Hypnosis – imagery - visualisation |
| Self belief | Mental rehearsal of successful performance Self-talk |
Visualisation Hypnosis Defusion Acceptance |
| Reward and threat | Incentive (outcome) Reward (outcome) |
Acceptance Sitting with distress Letting go of those things outside of one's control |
| Natural Consequences | Monitoring of emotional consequences Information about emotional consequences |
Mindfulness of feelings Present moment awareness Sitting with distress Observing self Values Committed action |
| Identity | Identification of self as role model Framing/reframing Valued self-identity |
Visualisation Hypnosis Contextualised self Observing self Defusion Values Committed action |
| Support | Social supports (emotional) Social supports (practical) |
Group sharing Shared experiences with thoughts and feelings Not feeling alone |
| Shaping knowledge | Instruction on how to perform the behaviour Behavioural experiments |
Guided meditation Guided hypnosis Mindfulness Defusion Acceptance At home and in group practice Comparing before skill use and after skill use experiments |
| Comparison of outcomes | Credible source Pros and Cons Comparative imagining of future outcomes |
Before and after experiments Visualisation Hypnosis Knowledge sharing Value identification Committed action |
4. Discussion and conclusion
4.1. Discussion
Our study identified Australian women treated with ART and ART providers' preferences regarding a group psychological intervention to support women undergoing ART. There was a balance between women currently and previously treated with ART, with limited heterogeneity between these groups. The delineation between women currently and previously treated with ART provided a unique insight into this group's experiences and needs, with those treated in the past providing information to consolidate the needs of those who will be trated in the future. While we achieved a good response rate from women treated with ART, we achieved a low response rate from ART providers. Therefore, our results regarding ART providers' preferences may not be representative due to the low completion rate. Another possible limitation and possible future area for research related to potentially attracting a subset of women treated with ART who were receptive to psychological intervention, more psychologically flexible or had positive experiences of psychological support. Data gathered regarding participants' perceptions about the psychological and emotional difficulties that would be useful to address in the group psychological intervention may have been enhanced by using a Likert scale or asking participants to rank responses, rather than simply allowing section of multiple responses, to better gauge the most desired content. Such data may provide valuable information to guide intervention development.
Despite that, we gained valuable information regarding the preferred content, duration, delivery mode, and the likelihood of women completing home practice. Our results also contained qualitative information regarding how best and not best to support women's mental health and well-being while undergoing treatment. For example, common unhelpful categories noted, such as mental health (anxiety and depression); feeling lost, alone and experiencing lowered self-esteem; feeling unsupported; experiencing insensitive comments or interactions; and experiencing clinical coldness or detachment, were consistent with past research [2,7,8]. Women also reported details about helpful categories of support, strategy development, and proactive action, which will be applied in developing a suitably acceptable group intervention program for women with infertility.
The preferred and most acceptable intervention format was six, fortnightly, 60-min face-to-face sessions, with audio files of 19 min (average) to support at-home practice. Group leader-led discussions were preferred, with opportunities to share personal experiences also desired, along with skill development targeting managing difficult thoughts and feelings and learning how to let go of things beyond one's control. Key BCTs to include in the intervention program identified in our current study included Feedback and monitoring; Regulation; Self-belief; Reward and threat; Natural consequences; Support; Shaping knowledge; and Comparison of outcomes.
Of note, to date, no group psychological intervention for women undergoing ART has been reported in Australia, leading to the exploration of Australian women treated with ART and ART providers' needs and preferences in line with IM and behavioural change approaches to intervention development. Further, it appears that co-design and implementation with women with infertility has not been widely documented.
4.2. Innovation
Given that the increased burden of infertility has been reduced following psychological intervention, with group interventions specifically demonstrating improvements in mental health and pregnancy rates [19,27,28], our current results will innovatively inform the development of a group program for Australian women with infertility. Our results informed which BCTs and change determinants to include when developing that group intervention as part of the intervention stage of IMB and Step 4 and 5 of the modified IM framework. Seeking detailed information from the end user of the intended program under a co-design model of research also aimed to improve the acceptability of the program and the applicability of the strategies included. Applying the RE-AIM framework [29], the co-designed group intervention will be reviewed by women treated with ART before it is piloted and modified as required, and it is likely that we will follow a co-implementation phase in order to acknowledge the importance of lived experience in treatment.
5. Conclusion
In considering the results of our current study, which has clarified women treated with ART and ART providers' needs and opinions regarding a proposed group psychological intervention, we developed a logic model (Fig. 3). This logic model aimed to illustrate the outcome determinants and the BCTs identified currently and in past research, and the desired impact of the ACT (Acceptance and Commitment Therapy) Infertility program. This approach follows a modified IM model of intervention development, applies a co-design approach, and is replicable and transparent.
Fig. 3.
Logic Model for Group Psychological Intervention.
Applying the developed logic model, future research will employ a person-centred approach and pilot the intervention with Australian women with infertility undergoing ART. The intervention, incorporating the information gained in this study will be evaluated in a randomised-controlled trial to determine its feasibility and effectiveness in improving the mental health, fertility stress and pregnancy rates of women with infertility undergoing ART.
Funding
The lead author is supported by an Australian Government Research Training Program stipend. The South Australian Society of Hypnosis also provided a research grant to fund the development and facilitation of the group psychological intervention. The funding sources played no role in the study design, conduct or reporting.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
Emma Warne reports financial support was provided by South Australia Society of Hypnosis to support the development of the group psychological intervention program.
Contributor Information
Emma Warne, Email: emma.warne@adelaide.edu.au.
Melissa Oxlad, Email: melissa.oxlad@adelaide.edu.au.
Talitha Best, Email: t.best@cqu.edu.au.
Data availability
Some data that support the findings of this study may be available on request from the corresponding author. The data are not publicly available due to ethics restrictions as not all partipcants consented to thier data being shared with other reseachers.
References
- 1.Sun H., et al. Global, regional, and national prevalence and disability-adjusted life-years for infertility in 195 countries and territories, 1990–2017: results from a global burden of disease study, 2017. Aging. 2019;11:10952–10991. doi: 10.18632/aging.102497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Australian Bureau of Statistics Australian Social Trends. 2002. https://www.abs.gov.au/ausstats/abs@.nsf/Previousproducts/4102.0Main%20Features12002?opendocument&tabname=Summary&prodno=4102.0&issue=2002&num=&view=
- 3.Mascarenhas M.N., Flaxman S.R., Boerma T., Vanderpoel S., Stevens G.A. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med. 2012;9 doi: 10.1371/journal.pmed.1001356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zegers-Hochschild F., et al. The International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary on ART terminology, 2009. Hum Reprod. 2009;24:2683–2687. doi: 10.1093/humrep/dep343. [DOI] [PubMed] [Google Scholar]
- 5.Boivin J., Griffiths E., Venetis C.A. Emotional distress in infertile women and failure of assisted reproductive technologies: meta-analysis of prospective psychosocial studies. BMJ. 2011;342:d223. doi: 10.1136/bmj.d223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ogawa M., Takamatsu K., Horiguchi F. Evaluation of factors associated with the anxiety and depression of female infertility patients. Biopsychosoc Med. 2011;5:15. doi: 10.1186/1751-0759-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schmidt L., Tjørnhøj-Thomsen T., Boivin J., Nyboe Andersen A. Evaluation of a communication and stress management training programme for infertile couples. Patient Educ Couns. 2005;59:252–262. doi: 10.1016/j.pec.2005.05.013. [DOI] [PubMed] [Google Scholar]
- 8.Taebi M., Kariman N., Montazeri A., Alavi Majd H. Infertility stigma: a qualitative study on feelings and experiences of infertile women. Int J Fertil Steril. 2021;15 doi: 10.22074/IJFS.2021.139093.1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boivin J., Gameiro S. Evolution of psychology and counseling in infertility. Fertil Steril. 2015;104:251–259. doi: 10.1016/j.fertnstert.2015.05.035. [DOI] [PubMed] [Google Scholar]
- 10.Dube L., Nkosi-Mafutha N., Balsom A.A., Gordon J.L. Infertility-related distress and clinical targets for psychotherapy: a qualitative study. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2021-050373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duffy J.M.N., et al. Top 10 priorities for future infertility research: an international consensus development study† ‡. Hum Reprod. 2020;35:2715–2724. doi: 10.1093/humrep/deaa242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fisher J.R.W., Baker G.H.W., Hammarberg K. Long-term health, well-being, life satisfaction, and attitudes toward parenthood in men diagnosed as infertile: challenges to gender stereotypes and implications for practice. Fertil Steril. 2010;94:574–580. doi: 10.1016/j.fertnstert.2009.01.165. [DOI] [PubMed] [Google Scholar]
- 13.Domar A., et al. Understanding the perceptions of and emotional barriers to infertility treatment: a survey in four European countries. Hum Reprod. 2012;27:1073–1079. doi: 10.1093/humrep/des016. [DOI] [PubMed] [Google Scholar]
- 14.Domar A.D., et al. The impact of group psychological interventions on distress in infertile women. Health Psychol. 2000;19:568–575. doi: 10.1037//0278-6133.19.6.568. [DOI] [PubMed] [Google Scholar]
- 15.Domar A.D., Dusek J.A. Psychological interventions and pregnancy rates. Dropouts—random or non-random? Reply of the authors. Fertil Steril. 2000;74:1261–1262. doi: 10.1016/s0015-0282(00)01650-2. [DOI] [PubMed] [Google Scholar]
- 16.Lakatos E., Szigeti J.F., Ujma P.P., Sexty R., Balog P. Anxiety and depression among infertile women: a cross-sectional survey from Hungary. BMC Womens Health. 2017;17:48. doi: 10.1186/s12905-017-0410-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Purewal S., Chapman S.C.E., van den Akker O.B.A. Depression and state anxiety scores during assisted reproductive treatment are associated with outcome: a meta-analysis. Reprod Biomed Online. 2018;36:646–657. doi: 10.1016/j.rbmo.2018.03.010. [DOI] [PubMed] [Google Scholar]
- 18.Nicoloro-SantaBarbara J., Busso C., Moyer A., Lobel M. Just relax and you’ll get pregnant? Meta-analysis examining women’s emotional distress and the outcome of assisted reproductive technology. Soc Sci Med. 2018;213:54–62. doi: 10.1016/j.socscimed.2018.06.033. [DOI] [PubMed] [Google Scholar]
- 19.Warne E., Oxlad M., Best T. Evaluating group psychological interventions for mental health in women with infertility undertaking fertility treatment: a systematic review and meta-analysis. Health Psychol Rev. 2022;17(3):1–25. doi: 10.1080/17437199.2022.2058582. [DOI] [PubMed] [Google Scholar]
- 20.Abraham C., Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychol. 2008;27:379–387. doi: 10.1037/0278-6133.27.3.379. [DOI] [PubMed] [Google Scholar]
- 21.Michie S., et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46:81–95. doi: 10.1007/s12160-013-9486-6. [DOI] [PubMed] [Google Scholar]
- 22.Bartholomew L., et al. 4th ed. Wiley; Hoboken, NJ: 2016. Planning health promotion programs: An intervention mapping approach. Wiley. [Google Scholar]
- 23.Read S.C., et al. Psychosocial services for couples in infertility treatment: what do couples really want? Patient Educ Couns. 2014;94:390–395. doi: 10.1016/j.pec.2013.10.025. [DOI] [PubMed] [Google Scholar]
- 24.Gameiro S., et al. ESHRE guideline: routine psychosocial care in infertility and medically assisted reproduction—a guide for fertility staff: figure 1. Hum Reprod. 2015;30:2476–2485. doi: 10.1093/humrep/dev177. [DOI] [PubMed] [Google Scholar]
- 25.Yardley L., Morrison L., Bradbury K., Muller I. The person-based approach to intervention development: application to digital health-related behavior change interventions. J Med Internet Res. 2015;17 doi: 10.2196/jmir.4055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fisher W.A., Fisher J.D., Harman J. In: Social psychological foundations of health and illness. Suls J., Wallston K.A., editors. Blackwell Publishing Ltd; 2003. The information-motivation-behavioral skills model: A general social psychological approach to understanding and promoting health behavior; pp. 82–106. [DOI] [Google Scholar]
- 27.Domar A.D., et al. Impact of a group mind/body intervention on pregnancy rates in IVF patients. Fertil Steril. 2011;95:2269–2273. doi: 10.1016/j.fertnstert.2011.03.046. [DOI] [PubMed] [Google Scholar]
- 28.Katyal N., Poulsen C.M., Knudsen U.B., Frederiksen Y. The association between psychosocial interventions and fertility treatment outcome: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2021;259:125–132. doi: 10.1016/j.ejogrb.2021.02.012. [DOI] [PubMed] [Google Scholar]
- 29.King D.K., Glasgow R.E., Leeman-Castillo B. Reaiming RE-AIM: using the model to plan, implement, and evaluate the effects of environmental change approaches to enhancing population health. Am J Public Health. 2010;100:2076–2084. doi: 10.2105/AJPH.2009.190959. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Some data that support the findings of this study may be available on request from the corresponding author. The data are not publicly available due to ethics restrictions as not all partipcants consented to thier data being shared with other reseachers.