Introduction
Bone infarction usually occurs in the long bones of the extremities and rarely occurs in the vertebral body, which may be related to the lower blood supply required by the vertebral body and the abundant blood supply around the vertebral body (1). Vertebral infarction caused by endovascular aneurysm repair (EVAR) has been mentioned in the literature but not extensively reported on. A case of lumbar spine and paravertebral muscle infarction after EVAR is described her with the aim of providing imaging guidance in the clinical diagnosis and etiology of low back pain and the choice of treatment modality in patients after EVAR.
Case presentation
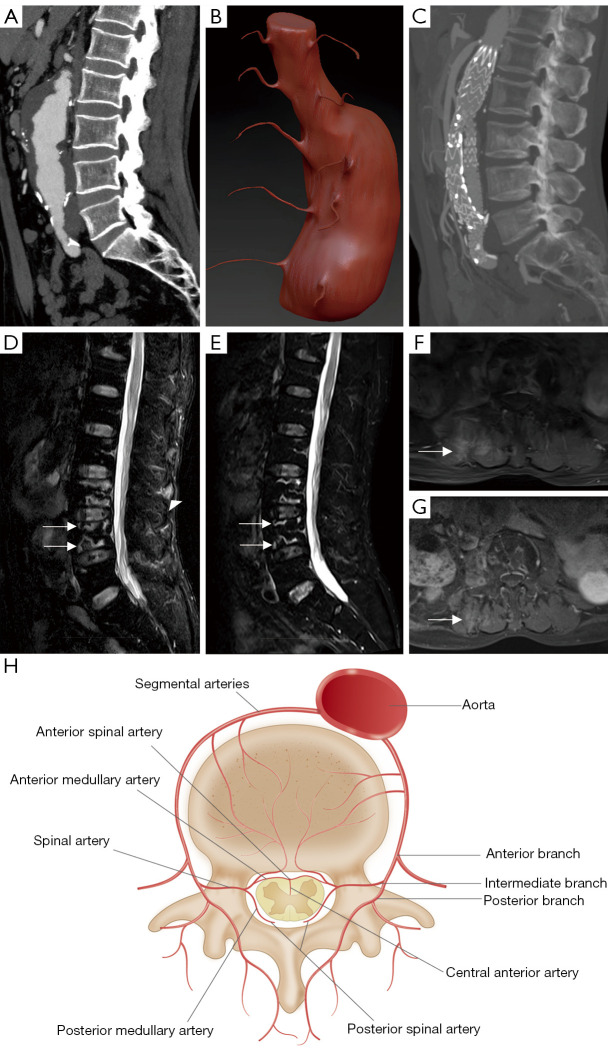
A 67-year-old male patient was admitted to Kunming Medical University Second Hospital. Eight days prior, in another hospital, an abdominal aortic aneurysm was found on physical examination (Figure 1A), and he was treated with infrarenal and suprarenal fixation EVAR. Before the operation, the bilateral lumbar arteries of the patient were unobstructed (Figure 1B). The patient’s postoperative vital signs were stable, and he was discharged from hospital 1 day after surgery. After discharge, the patient gradually began feeling low-back pain and discomfort, and the pain relief was not obvious after he took painkillers (tramadol hydrochloride). To clarify the cause of low back pain, the patient came to our hospital for treatment. Computed tomography (CT) showed the following: (I) The range of covered stents was from the superior segment of the abdominal aorta (the inferior border of the first lumbar vertebra) to the bilateral common iliac artery (Figure 1C). (II) There were no complications such as endoleak. (III) There was no lumbar intervertebral disc bulge or herniation. Magnetic resonance imaging (MRI) showed map-like and line-like lesions in the third and fourth lumbar vertebrae (L3 and L4), with hypointensity on T1-weighted imaging (T1WI) and hyperintensity on T2-weighted imaging with fat saturation (T2WI-FS) and a linear enhancement of contrast-enhanced images. Furthermore, the signal of the right erector spinae and multifidus muscle increased on T2WI-FS, and the contrast-enhanced images showed patchy enhancement. Although the dislodgement of small thrombi during EVAR surgery may lead to lumbar artery embolism, it is relatively rare that this causes embolism in multiple lumbar arteries at the same time. Moreover, the patient was treated with an infrarenal with suprarenal fixation stent graft, rather than a fenestrated graft, which may increase the coverage of the lumbar arteries and consequently increase the risk of thrombosis. To prevent this complication, clinicians should pay attention to the use of anticoagulants during surgery. Anticoagulants can reduce the formation of blood clots by inhibiting the activation of clotting factors and platelet aggregation. In this case, the patient was also treated with anticoagulants during the operation. Therefore, combined with the imaging manifestations and relevant medical history of the disease, lumbar artery occlusion caused by stent placement after EVAR was considered to be the most likely cause of the lesions in the L3 and L4 vertebrae and paravertebral muscle infarction. After the diagnosis was confirmed, the patient did not receive special treatment, and the pain gradually eased over time, with occasional mild discomfort. Seventh months later, an MRI reexamination showed that the scope of the map-like and line-like lesions in L3 and L4 vertebrae was smaller than before, the boundary was clearer, the signal on T2WI-FS was lower (Figure 1D,1E), and the involvement of the right paravertebral muscle was less extensive with diminished enhancement (Figure 1F,1G). All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was provided by the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Figure 1.
Lumbar spine and paravertebral muscle infarction after abdominal aortic aneurysm repair. (A) Preoperative sagittal CT. (B) 3D models of the patient’s abdominal aorta and bilateral lumbar arteries obtained by extracting the preoperative vascular model using Mimics software (Materialise) and replacing the vascular material using ZBrush software (Pixologic). (C) Postoperative sagittal CT. (D) Postoperative sagittal T2WI-FS. The white arrows indicate map-like infarcts of the L3 and L4 vertebrae, and the triangular arrow shows hyperintense muscle edema. (E) The sagittal T2WI-FS was reexamined 7 months after surgery. The white arrows indicate a smaller infarct area than observed previously. (F) Postoperative axial contrast-enhanced T1WI. The white arrow shows small patches of strengthening paravertebral muscle. (G) Axial contrast-enhanced T1WI was reexamined 7 months after surgery. The white arrow shows the reduced involvement of the paravertebral muscle. (H) Anatomy of the lumbar artery. CT, computed tomography; 3D, three-dimensional; T2WI-FS, T2-weighted imaging with fat saturation; T1WI, T1-weighted imaging.
Discussion
EVAR has the advantages of less trauma, less bleeding, and faster recovery (2). It is the main method for the treatment of abdominal aortic aneurysms at present. The common complications include endoleak, renal artery occlusion, aneurysm rupture, and ischemic colitis, among others (3). However, EVAR-related vertebral infarction has rarely been reported.
The site of bone infarction is typically in the long bones of the extremities and seldom in in the vertebral body, which has been attributed to the lower blood supply required by the vertebral body and the relatively high blood supply around the vertebral body (1). There are 4–5 pairs of lumbar arteries, and these originate from the posterior wall of the abdominal aorta and run posterolateral to the lateral direction of the vertebral body (Figure 1H). The anterior, posterior, and intermediate branches issue from the anterior edge of the intervertebral foramen to form a rich vascular network inside and outside the spinal canal to supply blood to the corresponding vertebral body and adjacent tissues (4). Therefore, EVAR rarely causes infarction of the vertebral body and paraspinal muscles. In this case, the infarction of the L3 and L4 vertebrae and paravertebral muscles occurred after EVAR, which might have been related to the following factors: (I) due to the large size of the aneurysm, the stent to be placed and its covered part were long, and there were many vessels blocked by the stent (lumbar artery, inferior mesenteric artery, etc.) with the scope of influence scope being large. (II) The patient’s lumbar artery blood supply was segmented, and there was a lack of good blood communication between segments. Once the lumbar artery supplying blood to this segment is blocked, significant ischemia will occur in the tissues corresponding to this segment. Under the action of the above 2 factors, the feeding arteries of the L2–L5 plane were blocked after the covered stent was placed, and the corresponding vertebral bodies and muscles became ischemic. Due to the normal blood supply above the L2 segment and below the L5 segment, a short-distance collateral circulation might have been established in a short time (the distance did not exceed 1 vertebral body length), and the ischemia and infarction of the L2 and L5 vertebral bodies and muscles could have been avoided. However, the L3 and L4 vertebral bodies are far from the blood supply of the upper and lower segments, and an effective and long-distance collateral circulation could not be established in a short time, so ischemia and infarction occurred.
On MRI, vertebral infarction appears similar to infarction in other parts, which is more characteristic. Vertebral infarct is irregular in shape and map-like, with line-like hypointensity on T1WI and line-like hyperintensity on T2WI-FS with an enhancement of contrast-enhanced scans. In addition, the regression of the disease can be observed with MRI (5). Over time, the signal of the T2WI-FS line-like lesions diminishes, and the boundary becomes clearer. In this case of the patient, the infarcted area of the vertebral body (line-like lesions in the surrounding area) and the infarcted area of the right paravertebral muscle gradually decreased. This suggests that over time, the distant collateral circulation is gradually established, and the blood supply to the infarct area is gradually restored. This also suggests that conservative treatment (more rest, enhanced nutrition, enhanced functional exercise, and regular follow-up) can be adopted for patients with vertebral infarction after EVAR.
In conclusion, for patients with low-back pain after EVAR, the possibility of vertebral body or paraspinal muscle infarction should be considered after common postoperative complications, lumbar disc herniation, and other causes of pain are excluded, and MRI can be selected for examination at this time.
Supplementary
The article’s supplementary files as
Acknowledgments
Funding: The study was funded by Medical Discipline Leaders of Yunnan Provincial Health and Health Commission (No. D-2019024).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was provided by the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Footnotes
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://qims.amegroups.com/article/view/10.21037/qims-23-210/coif). The authors have no conflicts of interest to declare.
References
- 1.Tezuka F, Sakai T, Nishisho T, Takata Y, Higashino K, Takao S, Harada M, Sairyo K. Variations in arterial supply to the lower lumbar spine. Eur Spine J 2016;25:4181-7. 10.1007/s00586-016-4427-2 [DOI] [PubMed] [Google Scholar]
- 2.Daye D, Walker TG. Complications of endovascular aneurysm repair of the thoracic and abdominal aorta: evaluation and management. Cardiovasc Diagn Ther 2018;8:S138-56. 10.21037/cdt.2017.09.17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel R, Powell JT, Sweeting MJ, Epstein DM, Barrett JK, Greenhalgh RM. The UK EndoVascular Aneurysm Repair (EVAR) randomised controlled trials: long-term follow-up and cost-effectiveness analysis. Health Technol Assess 2018;22:1-132. 10.3310/hta22050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beveridge TS, Power A, Johnson M, Power NE, Allman BL. The lumbar arteries and veins: Quantification of variable anatomical positioning with application to retroperitoneal surgery. Clin Anat 2015;28:649-60. 10.1002/ca.22504 [DOI] [PubMed] [Google Scholar]
- 5.Willaume T, Felten R, Pijnenburg L, Lersy F, Bierry G. Spontaneous infarction of lumbar roots, vertebrae and paravertebral muscles. Am J Emerg Med 2021;46:796.e5-7. 10.1016/j.ajem.2021.01.061 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The article’s supplementary files as