Abstract
Objective
To assess the recent trends in prevalence and management of hypertension in China, nationally and by population subgroups.
Design
Six rounds of a national survey, China.
Setting
China Chronic Disease and Risk Factors Surveillance, 2004-18.
Participants
642 523 community dwelling adults aged 18-69 years (30 501 in 2004, 47 353 in 2007, 90 491 in 2010, 156 836 in 2013, 162 293 in 2015, and 155 049 in 2018).
Main outcome measures
Hypertension was defined as a blood pressure of ≥140/90 mm Hg or taking antihypertensive drugs. The main outcome measures were hypertension prevalence and proportion of people with hypertension who were aware of their hypertension, who were treated for hypertension, and whose blood pressure was controlled below 140/90 mm Hg.
Results
The standardised prevalence of hypertension in adults aged 18-69 years in China increased from 20.8% (95% confidence interval 19.0% to 22.5%) in 2004 to 29.6% (27.8% to 31.3%) in 2010, then decreased to 24.7% (23.2% to 26.1%) in 2018. During 2010-18, the absolute annual decline in prevalence of hypertension among women was more than twice that among men (−0.83 percentage points (95% confidence interval −1.13 to −0.52) v −0.40 percentage points (−0.73 to −0.07)). Despite modest improvements in the awareness, treatment, and control of hypertension since 2004, rates remained low in 2018, at 38.3% (36.3% to 40.4%), 34.6% (32.6% to 36.7%), and 12.0% (10.6% to 13.4%). Of 274 million (95% confidence interval 238 to 311 million) adults aged 18-69 years with hypertension in 2018, control was inadequate in an estimated 240 million (215 to 264 million). Across all surveys, women with low educational attainment had higher prevalence of hypertension than those with higher education, but the finding was mixed for men. The gap in hypertension control between urban and rural areas persisted, despite larger improvements in diagnosis and control in rural than in urban areas.
Conclusions
The prevalence of hypertension in China has slightly declined since 2010, but treatment and control remain low. The findings highlight the need for improving detection and treatment of hypertension through the strengthening of primary care in China, especially in rural areas.
Introduction
Hypertension is a leading risk factor for stroke, ischaemic heart disease, other cardiovascular diseases, and chronic kidney disease and is responsible for more than 10 million deaths worldwide each year.1 In China in 2019, more than 25 million disability adjusted life years for stroke were attributed to high systolic blood pressure,2 and stroke is the leading cause of mortality.3 Overwhelming evidence indicates that control of hypertension is associated with important reductions in cardiovascular events and deaths.4
In recent years the prevalence of hypertension has declined and its treatment and control have improved substantially in some high income countries, such as Canada, South Korea, Germany, and Chile.5 These countries usually have well constructed primary care systems, high insurance coverage, widely adopted evidence based hypertension guidelines, and, in some countries, nationwide health check-ups and screening.5 6 In the late 2000s, China started multiple nationwide programmes with packages for the prevention and control of hypertension, including the China Healthy Lifestyle for All Initiative in 2007,7 National Basic Public Health Services Program in 2009,8 and National Demonstration Areas for Comprehensive Prevention and Control of Non-communicable Diseases in 2011.9 To evaluate the impact of these national public health programmes and guide future improvements, assessment of recent trends in the prevalence of hypertension and its management and control in China is essential after the implementation of these initiatives.
Several nationally representative studies have reported the prevalence, awareness, treatment, and control of hypertension in China since the 2000s, most of which were performed before 2010.10 11 12 13 These studies adopted different sampling schemes and survey methods, with key differences in age ranges, procedures, and definitions of hypertension, making it difficult to assess trends. The lack of reliable, consistent data on recent trends in the prevalence, management, and control of hypertension hampers the essential understanding of the scale of, and change in, the burden of hypertension in China, and where intervention is needed the most.
Based on data from six rounds of a nationally representative survey with broadly consistent design and protocol, we examined trends in the prevalence of and number of adults with hypertension in China during 2004-18, and the extent of awareness, treatment, and control of hypertension and how each varied by sex, age, geography, and socioeconomic status.
Methods
Data sources
We used data from the China Chronic Disease and Risk Factor Surveillance (CCDRFS) survey. The history, development, and design of this survey have been described previously.14 Briefly, the survey was established in 2004 to provide periodic nationwide information on the prevalence and distribution of major non-communicable diseases and associated behavioural and metabolic risk factors in the Chinese population. To date, six rounds of the survey have been conducted: in 2004, 2007, 2010, 2013, 2015, and 2018. Each roundadopted a similar sampling scheme with a stratified, clustered, and multistage design to select a random sample from the Chinese adult population. In 2004, the survey included the 79 districts and counties in the national Disease Surveillance Points system, which were randomly selected from all 31 provinces, autonomous regions, and municipalities of mainland China.15 The number of surveillance districts and counties was expanded to 161 in 2007 and 2010. Since 2013, 298 districts and counties have been enrolled into the China Chronic Disease and Risk Factor Surveillance, making the survey sample provincially representative. Supplement 1 and a previous report provide details of population coverage, sample design, and weighting.16
Across all six rounds of the survey, 776 571 individuals were invited and 746 020 participated (response rate 96.1%), including 33 051 (99.6%) in 2004, 51 050 (99.1%) in 2007, 98 174 (90.5%) in 2010, 189 115 (97.6%) in 2013, 189 754 (97.4%) in 2015, and 184 876 (94.9%) in 2018.14 Respondents aged 18-69 years were included in the present study as the 2004 survey only invited residents within this age range. The participants provided written informed consent.
Data collection
Trained and qualified health professionals administered questionnaire based interviews from local health facilities (eg, hospitals, clinics, and centres for disease control and prevention), to collect data on personal, socioeconomic status, lifestyle behaviours, history of major chronic diseases, and prescribed drug use. In each survey round, blood pressure was measured in all respondents—three times successively with a one minute interval between measurements, using mercury sphygmomanometers in 2004 and electronic blood pressure monitors from 2007 (Omron, Dalian, China). The monitors were calibrated and tested according to standardprotocol. The average of the last two readings was used for analyses. Quality control was performed by national, provincial, and local designated staff according to a standard survey protocol. For most respondents, interviews, physical measurements, and biochemical sample collections were conducted at a community health centre in the sampled villages or residential areas. Those who did not participate in the survey on the due date received home visits; those who could not be reached after three invites were considered non-respondents.
Outcome
Hypertension was defined as a systolic blood pressure of ≥140 mm Hg or diastolic blood pressure of ≥90 mm Hg or receiving drugs for hypertension. Awareness was calculated as the percentage of participants with hypertension who responded “Yes” to the question “Have you ever been told by a doctor or other healthcare professional that you had high blood pressure?” Treatment was calculated as the percentage of participants with hypertension who self-reported taking at least one prescribed antihypertensive drug for the management of hypertension. Control was calculated as the percentage of participants with hypertension who had a systolic blood pressure of <140 mm Hg and diastolic blood pressure of <90 mm Hg when measured in the survey. We also reported the proportion of adults with undiagnosed or untreated hypertension with a systolic blood pressure of ≥160 mm Hg or diastolic blood pressure of ≥100 mm Hg.
Statistical analysis
The sample design in all analyses incorporated stratification, clustering, and sample weights that were computed as the product of original sampling weights, non-response weights, and post-stratification weights. To ensure overall prevalence estimates were comparable across the six rounds of survey, we standardised age specific results according to the 2010 China census population, to account for changes over time in age structure.17 For comparison, we also provided sample prevalence without standardisation. In addition, we estimated the absolute number of individuals with hypertension using post-stratification weights based on the United Nations population estimates of specific survey years,18 known as the Horvitz-Thompson estimator,19 to reflect the burden on the health system. We calculated prevalence, rates of awareness, treatment, and control, and mean blood pressure by sex, age, urban or rural residence, education, geographical region, body mass index, and central obesity. In the subgroups other than age, we calculated age adjusted rates by modelling design based multivariable logistic regression in surveylogistic procedure of SAS system with “lsmeans” statement (see supplement 2).20 We conducted preliminary analyses to assess whether trends in prevalence, awareness, treatment, and control rates by fitting linear, quadratic, cubic, and penalised cubic spline models. We further performed Welch’s t test for comparisons of annual absolute changes before and after 2010 to assess potential impacts on trends in prevalence of hypertension and management of national public health programmes related to hypertension prevention and control introduced around 2010. The annual absolute changes in prevalence were calculated as the absolute difference in prevalence between the start and end years divided by total number of years covered. See supplement 2 for further details of statistical analyses. We performed all analyses in SAS (version 9.4, SAS Institute, Cary, NC) and R (4.0.1).
Patient and public involvement
This study used data from six rounds of the China Chronic Disease and Risk Factor Surveillance that were not specifically designed for the current study’s aim of evaluating the impact of the national public health programmes that were started in the late 2000s, by assessing the trend in hypertension prevalence and management. Therefore, we did not involve patients in setting the research question or in the design and implementation of the study.
Results
The study included a total of 642 523 community dwelling adults aged 18-69 years (30 501 in 2004, 47 353 in 2007, 90 491 in 2010, 156 836 in 2013, 162 293 in 2015, and 155 049 in 2018; see supplementary fig 1). More women (53-58%) were recruited in each survey than men. Proportions of people older than 60 years, urban residents, and those with overweight, obesity, and central obesity gradually increased across the study period. The distributions for education and region were similar across all survey years (supplementary table 1).
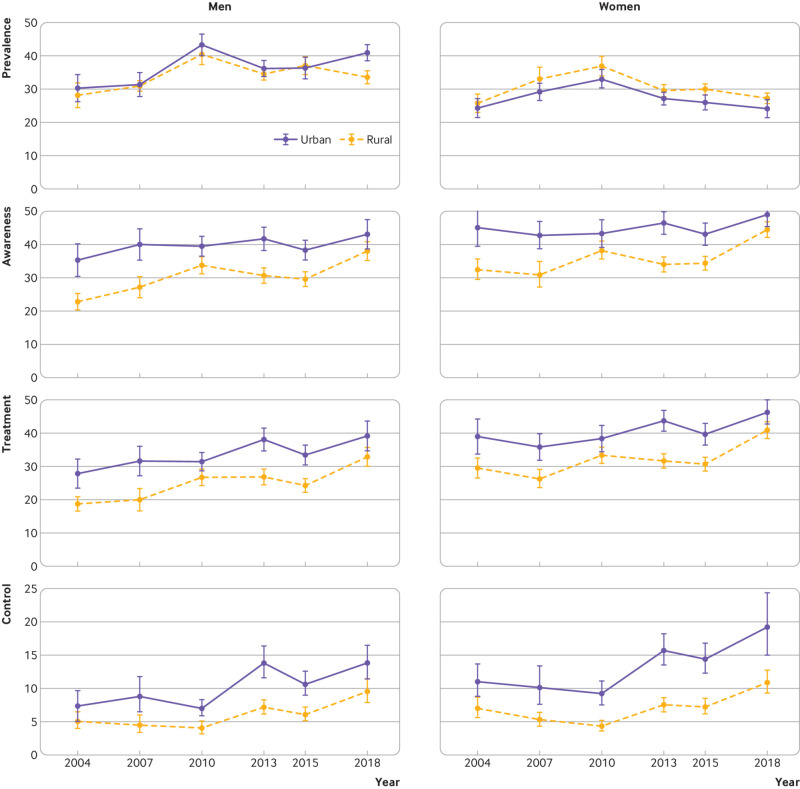
Hypertension prevalence
The prevalence of hypertension in the study sample increased from 24.9% (95% confidence interval 24.4% to 25.3%) to 38.1% (37.8% to 38.3%) during 2004-18 (table 1). The standardised prevalence of hypertension increased from 20.8% (19.0% to 22.5%) in 2004 to 29.6% (27.8% to 31.3%) in 2010 (P<0.001), then decreased to 24.7% (23.2% to 26.1%) in 2018 (P<0.001 from 2010 to 2018) (table 1 and table 2). The absolute annual decline in prevalence of hypertension among women (−0.83 percentage points, 95% confidence interval −1.13 to −0.52) in 2010-18 was more than twice that of men (−0.40 percentage points, −0.73 to −0.07). The prevalence was higher in rural than urban areas in 2013 (P=0.04), although the differences were not statistically significant in other survey years. In China, 274 million (95% confidence interval 238 to 311 million) adults aged 18-69 years had hypertension in 2018 (fig 1), which was an increase from 172 million (135 to 208 million) in 2004 but a decline from the peak of 284 million (237 to 331 million) in 2010.
Table 1.
Trends in crude and standardised rates for prevalence, awareness, treatment, and control of hypertension among men and women aged 18-69 years in China, by year of survey
| Survey year | |||||||
|---|---|---|---|---|---|---|---|
| 2004 | 2007 | 2010 | 2013 | 2015 | 2018 | ||
| Crude rate (95% CI) | |||||||
| Overall: | |||||||
| Hypertension | 24.9 (24.4 to 25.3) | 28.8 (28.4 to 29.3) | 34.8 (34.5 to 35.2) | 33.1 (32.8 to 33.3) | 36.6 (36.4 to 36.8) | 38.1 (37.8 to 38.3) | |
| Awareness | 30.8 (29.8 to 31.9) | 33.2 (32.4 to 34.0) | 35.8 (35.2 to 36.3) | 37.8 (37.4 to 38.2) | 37.6 (37.2 to 38.0) | 45.7 (45.3 to 46.1) | |
| Treatment | 26.1 (25.1 to 27.1) | 26.8 (26.1 to 27.6) | 30.3 (29.8 to 30.8) | 34.5 (34.1 to 34.9) | 33.6 (33.2 to 33.9) | 41.9 (41.5 to 42.3) | |
| Control | 7.0 (6.4 to 7.6) | 6.1 (5.7 to 6.5) | 5.8 (5.5 to 6.1) | 10.7 (10.4 to 11.0) | 9.4 (9.2 to 9.7) | 13.7 (13.4 to 14.0) | |
| Men: | |||||||
| Hypertension | 26.5 (25.7 to 27.2) | 28.8 (28.2 to 29.4) | 36.5 (36.0 to 37.0) | 34.9 (34.5 to 35.2) | 38.8 (38.5 to 39.2) | 40.9 (40.5 to 41.3) | |
| Awareness | 25.0 (23.6 to 26.5) | 30.0 (28.8 to 31.1) | 32.4 (31.7 to 33.2) | 34.6 (34.0 to 35.2) | 33.8 (33.3 to 34.4) | 41.8 (41.2 to 42.4) | |
| Treatment | 20.1 (18.7 to 21.4) | 23.3 (22.2 to 24.3) | 26.1 (25.4 to 26.8) | 30.8 (30.2 to 31.4) | 29.5 (28.9 to 30.0) | 37.6 (37.1 to 38.2) | |
| Control | 5.5 (4.7 to 6.2) | 5.3 (4.8 to 5.9) | 5.2 (4.8 to 5.5) | 9.7 (9.3 to 10.1) | 8.6 (8.2 to 8.9) | 12.3 (11.9 to 12.7) | |
| Women: | |||||||
| Hypertension | 23.6 (23.0 to 24.2) | 28.9 (28.3 to 29.5) | 33.5 (33.0 to 33.9) | 31.8 (31.4 to 32.1) | 34.7 (34.4 to 35.0) | 35.9 (35.6 to 36.2) | |
| Awareness | 35.9 (34.4 to 37.4) | 36.1 (35.0 to 37.2) | 38.8 (38.1 to 39.6) | 40.4 (39.9 to 41.0) | 41.1 (40.6 to 41.7) | 49.1 (48.5 to 49.6) | |
| Treatment | 31.5 (30.0 to 32.9) | 30.0 (28.9 to 31.0) | 34.2 (33.4 to 34.9) | 37.5 (36.9 to 38.0) | 37.5 (36.9 to 38.0) | 45.7 (45.2 to 46.3) | |
| Control | 8.4 (7.5 to 9.2) | 6.8 (6.2 to 7.4) | 6.4 (6.0 to 6.8) | 11.5 (11.1 to 11.9) | 10.3 (9.9 to 10.6) | 15.0 (14.6 to 15.4) | |
| Urban: | |||||||
| Hypertension | 26.5 (25.7 to 27.3) | 29.2 (28.6 to 29.9) | 35.0 (34.5 to 35.4) | 33.2 (32.9 to 33.6) | 36.1 (35.8 to 36.5) | 38.4 (38.0 to 38.7) | |
| Awareness | 39.7 (37.9 to 41.4) | 41.4 (40.0 to 42.7) | 39.5 (38.7 to 40.4) | 44.1 (43.5 to 44.8) | 42.5 (41.9 to 43.1) | 49.0 (48.4 to 49.6) | |
| Treatment | 33.1 (31.4 to 34.7) | 33.8 (32.5 to 35.0) | 33.9 (33.1 to 34.7) | 40.9 (40.2 to 41.5) | 38.8 (38.2 to 39.4) | 45.7 (45.1 to 46.3) | |
| Control | 9.3 (8.3 to 10.3) | 8.9 (8.1 to 9.6) | 8.2 (7.7 to 8.7) | 14.7 (14.3 to 15.2) | 12.7 (12.3 to 13.1) | 17.4 (17.0 to 17.9) | |
| Rural: | |||||||
| Hypertension | 23.8 (23.2 to 24.4) | 28.6 (28.1 to 29.1) | 34.8 (34.4 to 35.2) | 32.9 (32.6 to 33.2) | 37.0 (36.7 to 37.3) | 37.8 (37.5 to 38.1) | |
| Awareness | 24.7 (23.5 to 26.0) | 27.9 (27.0 to 28.9) | 33.3 (32.6 to 34.0) | 33.3 (32.8 to 33.8) | 34.0 (33.5 to 34.5) | 42.9 (42.4 to 43.4) | |
| Treatment | 21.3 (20.1 to 22.5) | 22.3 (21.4 to 23.2) | 27.9 (27.3 to 28.6) | 30.0 (29.4 to 30.5) | 29.8 (29.3 to 30.2) | 38.8 (38.2 to 39.3) | |
| Control | 5.5 (4.8 to 6.1) | 4.3 (3.9 to 4.8) | 4.2 (3.9 to 4.5) | 7.8 (7.5 to 8.1) | 7.1 (6.8 to 7.3) | 10.6 (10.2 to 10.9) | |
| Standardised rate (95% CI)* | |||||||
| Overall: | |||||||
| Hypertension | 20.8 (19.0 to 22.5) | 24.1 (22.2 to 26.0) | 29.6 (27.8 to 31.3) | 25.1 (24.1 to 26.1) | 25.2 (23.6 to 26.7) | 24.7 (23.2 to 26.1) | |
| Awareness | 30.8 (28.0 to 33.6) | 31.6 (29.0 to 34.2) | 33.7 (31.8 to 35.6) | 31.7 (30.0 to 33.3) | 32.6 (31.0 to 34.2) | 38.3 (36.3 to 40.4) | |
| Treatment | 25.9 (23.5 to 28.4) | 25.5 (23.1 to 27.9) | 27.9 (26.2 to 29.6) | 28.7 (27.1 to 30.3) | 28.5 (27.0 to 30.1) | 34.6 (32.6 to 36.7) | |
| Control | 7.1 (6.0 to 8.2) | 6.7 (5.4 to 7.9) | 5.5 (4.8 to 6.2) | 8.9 (7.9 to 9.8) | 8.8 (7.9 to 9.7) | 12.0 (10.6 to 13.4) | |
| Men: | |||||||
| Hypertension | 22.4 (20.3 to 24.4) | 24.2 (22.3 to 26.2) | 32.2 (30.3 to 34.0) | 27.4 (26.3 to 28.5) | 28.4 (26.6 to 30.2) | 29.0 (27.1 to 30.9) | |
| Awareness | 25.7 (23.0 to 28.4) | 29.2 (26.4 to 31.9) | 30.9 (29.0 to 32.7) | 29.0 (27.3 to 30.8) | 29.2 (27.5 to 30.9) | 34.3 (31.9 to 36.8) | |
| Treatment | 20.5 (18.2 to 22.8) | 22.4 (19.8 to 25.0) | 24.2 (22.5 to 25.8) | 25.7 (24.0 to 27.3) | 24.7 (23.2 to 26.3) | 30.3 (28.0 to 32.6) | |
| Control | 5.6 (4.5 to 6.8) | 6.0 (4.7 to 7.4) | 4.9 (4.2 to 5.5) | 8.3 (7.3 to 9.2) | 7.5 (6.6 to 8.4) | 10.3 (9.0 to 11.6) | |
| Women: | |||||||
| Hypertension | 19.2 (17.6 to 20.8) | 24.0 (21.9 to 26.1) | 26.8 (25.0 to 28.6) | 22.6 (21.6 to 23.7) | 21.8 (20.4 to 23.3) | 20.2 (18.6 to 21.8) | |
| Awareness | 37.0 (33.6 to 40.3) | 34.2 (31.2 to 37.2) | 37.2 (35.0 to 39.5) | 35.0 (33.1 to 36.8) | 37.2 (35.3 to 39.0) | 44.2 (42.1 to 46.3) | |
| Treatment | 32.5 (29.6 to 35.4) | 28.8 (26.3 to 31.3) | 32.5 (30.5 to 34.6) | 32.4 (30.6 to 34.2) | 33.7 (31.8 to 35.5) | 41.1 (39.0 to 43.3) | |
| Control | 8.8 (7.3 to 10.2) | 7.3 (5.9 to 8.8) | 6.3 (5.4 to 7.2) | 9.6 (8.5 to 10.6) | 10.6 (9.4 to 11.7) | 14.5 (12.3 to 16.7) | |
| Urban: | |||||||
| Hypertension | 20.5 (17.9 to 23.0) | 23.0 (20.7 to 25.4) | 28.9 (26.4 to 31.3) | 23.7 (22.2 to 25.2) | 23.9 (21.4 to 26.3) | 24.9 (22.8 to 27.1) | |
| Awareness | 36.3 (31.9 to 40.7) | 37.0 (33.0 to 41.1) | 35.6 (32.5 to 38.7) | 37.5 (34.6 to 40.5) | 36.3 (33.9 to 38.7) | 38.9 (35.6 to 42.2) | |
| Treatment | 29.9 (26.0 to 33.8) | 30.1 (26.3 to 34.0) | 29.6 (26.7 to 32.4) | 34.4 (31.5 to 37.2) | 32.3 (29.9 to 34.6) | 35.6 (32.4 to 38.8) | |
| Control | 8.4 (6.7 to 10.2) | 8.7 (6.5 to 10.8) | 7.1 (5.9 to 8.3) | 12.9 (11.0 to 14.8) | 11.3 (9.8 to 12.9) | 14.0 (11.6 to 16.4) | |
| Rural: | |||||||
| Hypertension | 21.2 (18.9 to 23.4) | 25.4 (22.5 to 28.3) | 30.4 (27.9 to 32.9) | 25.9 (24.6 to 27.2) | 26.7 (25.3 to 28.2) | 24.4 (22.4 to 26.3) | |
| Awareness | 24.5 (22.5 to 26.6) | 25.8 (23.7 to 27.9) | 31.5 (29.4 to 33.6) | 28.4 (26.6 to 30.2) | 28.7 (26.9 to 30.4) | 37.6 (35.4 to 39.8) | |
| Treatment | 21.4 (19.6 to 23.2) | 20.6 (18.7 to 22.5) | 26.1 (24.2 to 27.9) | 25.5 (23.8 to 27.2) | 24.6 (22.9 to 26.3) | 33.5 (31.2 to 35.7) | |
| Control | 5.5 (4.6 to 6.4) | 4.5 (3.6 to 5.3) | 3.8 (3.2 to 4.4) | 6.6 (5.8 to 7.4) | 6.1 (5.3 to 7.0) | 9.5 (8.1 to 11.0) | |
CI=confidence interval.
Rates weighted to 2010 census population in China.
Table 2.
Absolute annual change (percentage points) in standardised rates for prevalence, awareness, treatment, and control of hypertension in China during 2004-10, 2010-18, and 2004-18
| 2004-10 | 2010-18 | 2004-18 | P value* | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Annual change (95% CI) | P value | Annual change (95% CI) | P value | Annual change (95% CI) | P value | ||||
| Overall | |||||||||
| Hypertension | 1.47 (1.05 to 1.88) | <0.001 | −0.61 (−0.90 to −0.33) | <0.001 | 0.28 (0.12 to 0.44) | <0.001 | <0.001 | ||
| Awareness | 0.48 (−0.08 to 1.05) | 0.09 | 0.58 (0.23 to 0.92) | 0.001 | 0.54 (0.29 to 0.78) | <0.001 | 0.79 | ||
| Treatment | 0.33 (−0.16 to 0.83) | 0.19 | 0.84 (0.50 to 1.17) | <0.001 | 0.62 (0.39 to 0.85) | <0.001 | 0.10 | ||
| Control | −0.27 (−0.48 to −0.05) | 0.02 | 0.81 (0.62 to 1.01) | <0.001 | 0.35 (0.22 to 0.48) | <0.001 | <0.001 | ||
| Men | |||||||||
| Hypertension | 1.63 (1.17 to 2.09) | <0.001 | −0.40 (−0.73 to −0.07) | 0.02 | 0.47 (0.27 to 0.67) | <0.001 | <0.001 | ||
| Awareness | 0.87 (0.32 to 1.41) | 0.002 | 0.43 (0.04 to 0.81) | 0.03 | 0.61 (0.35 to 0.87) | <0.001 | 0.19 | ||
| Treatment | 0.62 (0.14 to 1.09) | 0.01 | 0.76 (0.41 to 1.12) | <0.001 | 0.70 (0.47 to 0.93) | <0.001 | 0.63 | ||
| Control | −0.12 (−0.34 to 0.10) | 0.30 | 0.68 (0.49 to 0.86) | <0.001 | 0.34 (0.21 to 0.46) | <0.001 | <0.001 | ||
| Women | |||||||||
| Hypertension | 1.27 (0.87 to 1.67) | <0.001 | −0.83 (−1.13 to −0.52) | <0.001 | 0.07 (−0.09 to 0.23) | 0.39 | <0.001 | ||
| Awareness | 0.03 (−0.64 to 0.71) | 0.92 | 0.88 (0.49 to 1.26) | <0.001 | 0.51 (0.23 to 0.80) | <0.001 | 0.03 | ||
| Treatment | 0.00 (−0.59 to 0.59) | >0.99 | 1.08 (0.70 to 1.45) | <0.001 | 0.61 (0.36 to 0.87) | <0.001 | 0.003 | ||
| Control | −0.42 (−0.70 to −0.13) | 0.004 | 1.03 (0.73 to 1.32) | <0.001 | 0.41 (0.22 to 0.60) | <0.001 | <0.001 | ||
| Urban | |||||||||
| Hypertension | 1.40 (0.81 to 1.99) | <0.001 | −0.50 (−0.91 to −0.09) | 0.02 | 0.31 (0.08 to 0.55) | 0.01 | <0.001 | ||
| Awareness | −0.12 (−1.01 to 0.78) | 0.80 | 0.41 (−0.15 to 0.98) | 0.15 | 0.19 (−0.21 to 0.58) | 0.35 | 0.33 | ||
| Treatment | −0.05 (−0.86 to 0.76) | 0.90 | 0.75 (0.21 to 1.29) | 0.006 | 0.41 (0.05 to 0.77) | 0.03 | 0.11 | ||
| Control | −0.22 (−0.57 to 0.14) | 0.23 | 0.86 (0.53 to 1.20) | <0.001 | 0.40 (0.19 to 0.61) | <0.001 | <0.001 | ||
| Rural | |||||||||
| Hypertension | 1.53 (0.97 to 2.09) | <0.001 | −0.75 (−1.15 to −0.35) | <0.001 | 0.23 (0.02 to 0.44) | 0.04 | <0.001 | ||
| Awareness | 1.17 (0.68 to 1.66) | <0.001 | 0.76 (0.38 to 1.14) | <0.001 | 0.94 (0.72 to 1.15) | <0.001 | 0.20 | ||
| Treatment | 0.78 (0.35 to 1.21) | <0.001 | 0.93 (0.56 to 1.29) | <0.001 | 0.86 (0.66 to 1.07) | <0.001 | 0.62 | ||
| Control | −0.28 (−0.46 to −0.10) | 0.002 | 0.71 (0.52 to 0.91) | <0.001 | 0.29 (0.16 to 0.41) | <0.001 | <0.001 | ||
CI=confidence interval.
P value for difference in annual changes for 2004-10 v 2010-18.
Fig 1.
Trends in absolute burden of hypertension among adults aged 18-69 years in China, 2004-18. The absolute number was calculated based on United Nations population estimations for China in 2004, 2007, 2010, 2013, 2015, and 2018
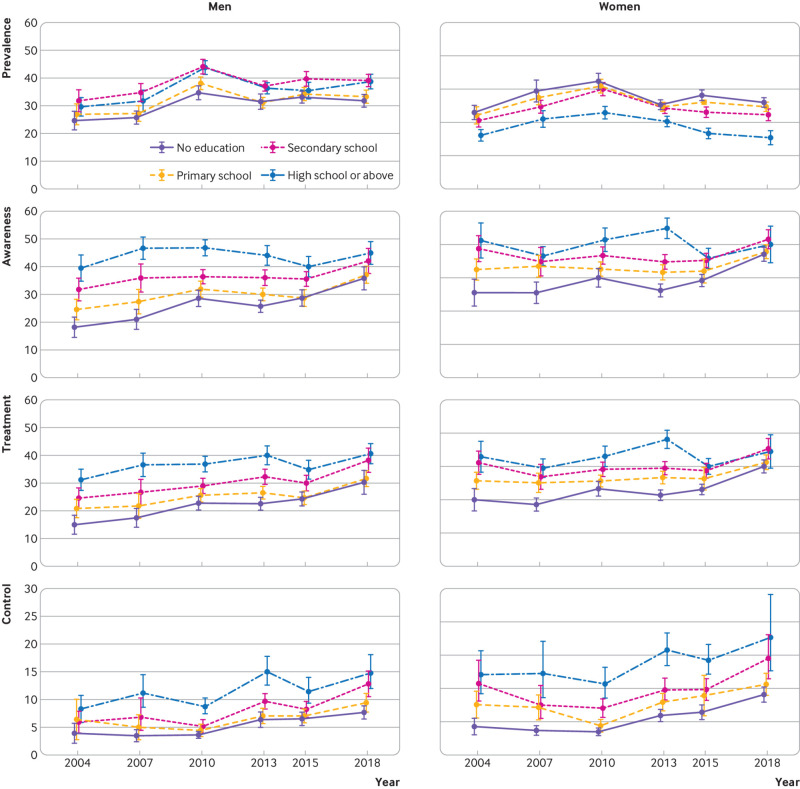
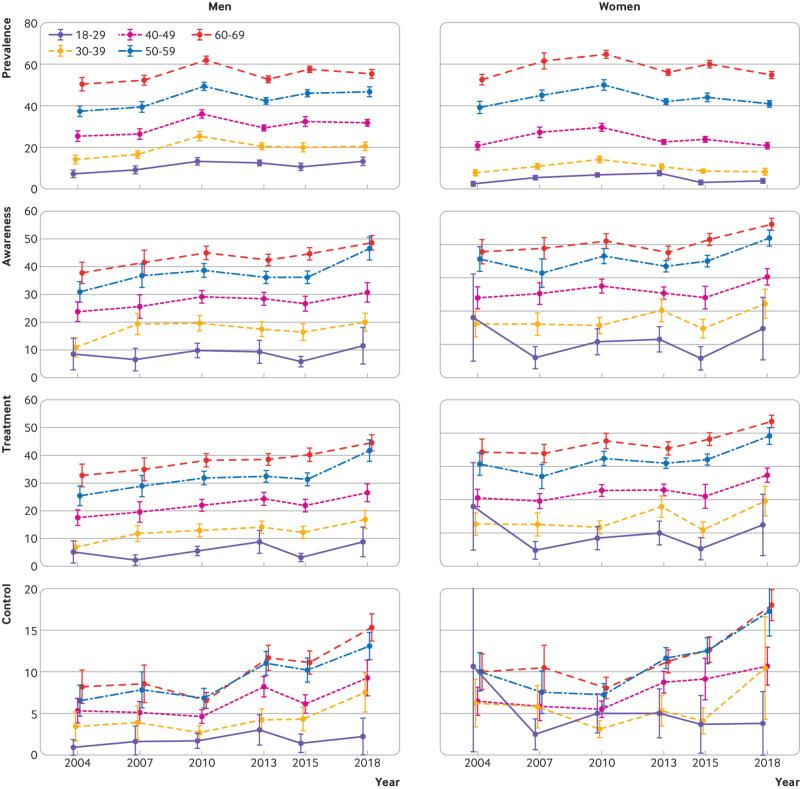
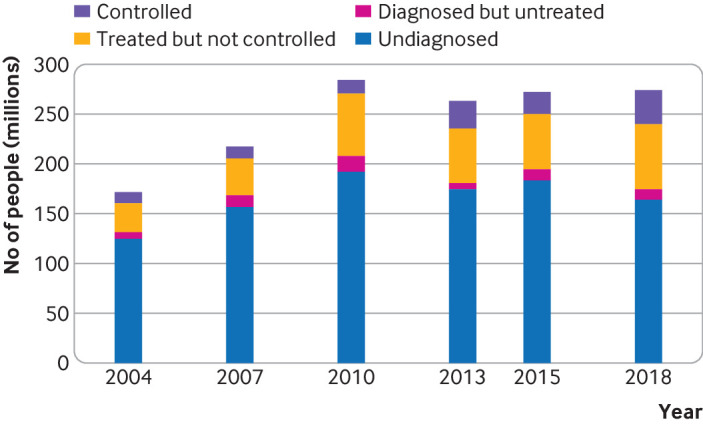
The trends in hypertension prevalence were largely similar in urban and rural areas for both sexes (fig 2 and supplementary table 2). Women in rural areas had a somewhat higher prevalence of hypertension than their urban counterparts across all survey years, whereas prevalence was similar in men from urban and rural areas, except in 2018 (P>0.05 during 2004-15, P=0.02 in 2018). Less educated women had a higher prevalence of hypertension than women with better education attainment in all survey years, but the education gradient was mixed among men (fig 3 and supplementary table 3). For both sexes there were similar trends in hypertension prevalence across age groups (fig 4). The prevalence in women was lower than in men among adults younger than 50 years in all survey years, but higher than in men older than 60 years, except in 2018 (supplementary table 4). Men and women in the north region generally had the highest prevalence and those in the south region had the lowest (supplementary fig 2 and supplementary table 5). Across regions, about a twofold difference in hypertension prevalence was observed in all survey years.
Fig 2.
Trends in hypertension prevalence, awareness, treatment, and control rates in urban and rural areas among men and women aged 18-69 years in China, 2004-18. All rates were estimated using multivariable logistic regression containing age, survey year, sex, residence, and two way and three way interaction terms of survey year, sex, and residence. Error bars indicate 95% confidence intervals with consideration of complex sample design
Fig 3.
Trends in hypertension prevalence, awareness, treatment, and control rates by education group among men and women aged 18-69 years in China, 2004-18. All rates were estimated using multivariable logistic regression containing age, survey year, sex, education, and two way and three way interaction terms of survey year, sex, and education. Error bars indicate 95% confidence intervals with consideration of complex sample design
Fig 4.
Trends in standardised hypertension prevalence, awareness, treatment, and control rates by age groups among men and women in China, 2004-18. All rates were weighted to the 2010 China population. Error bars indicate 95% confidence intervals with consideration of complex sample design
In each survey year for both sexes, the prevalence of hypertension approximately doubled among those with normal body mass index, tripled in overweight adults, and quadrupled or quintupled in obese adults compared with underweight adults (supplementary fig 2 and supplementary table 6). The prevalence for both men and women with central obesity was approximately twice as high as their counterpart without central obesity in each survey year (supplementary fig 2 and supplementary table 7).
Awareness, treatment, and control of hypertension
Awareness, treatment, and control of hypertension were low throughout the study period. Modest improvements have occurred since 2004, with standardised rates of awareness increasing from 30.8% (28.0% to 33.6%) to 38.3% (36.3% to 40.4%), treatment from 25.9% (23.5% to 28.4%) to 34.6% (32.6% to 36.7%), and control from 7.1% (6.0% to 8.2%) to 12.0% (10.6% to 13.4%) (all P<0.001) (table 1 and table 2). Among men, the rates of awareness, treatment, and control increased annually by 0.61 (0.35 to 0.87), 0.70 (0.47 to 0.93), and 0.34 (0.21 to 0.46) percentage points from 2004 to 2018 (all P<0.001) (table 2). Among women, the annual absolute change in rates of awareness, treatment, and control during 2010-18 were statistically higher than during 2004-10 (P=0.03, P=0.003, P<0.001, respectively). The annual changes in awareness and treatment in rural areas was greater than those in urban areas (awareness: 0.94 (0.72 to 1.15) v 0.19 (−0.21 to 0.58) percentage points per year, P=0.001; treatment: 0.86 (0.66 to 1.07) v 0.41 (0.05 to 0.77) percentage points per year, P=0.03) (table 2). Yet control in urban areas annually increased at a higher pace than in rural areas, without statistical significance (0.40 (0.19 to 0.61) v 0.29 (0.16 to 0.41) percentage points per year, P=0.36).
In all survey years studied, both men and women in urban areas had better awareness, treatment, and control of hypertension than their rural counterparts (fig 2 and supplementary table 2). The urban-rural gaps in awareness and treatment narrowed between 2004 and 2018, but the gaps for control remained unchanged owing to a widening urban-rural gap in the control rate among treated individuals (see supplementary table 8). Rates improved for all education subgroups from 2004 to 2018, but higher education groups showed smaller progress (fig 3 and supplementary table 3). Similar trends were seen across age groups (fig 4 and supplementary table 4).
Awareness, treatment, and control of hypertension improved between 2004 and 2018 across all regions of China except the south region, but regional and provincial variation persisted (supplementary table 5 and supplementary fig 3). The provincial difference in awareness, treatment, and control is partly correlated with per capita GDP (supplementary fig 4). Better awareness and treatment were consistently found in men and women with obesity or central obesity than their counterparts without obesity in all survey years (supplementary tables 6 and 7), but the same advantage was not seen for control. When we used an alternative definition of hypertension (130/80 mm Hg), results for hypertension prevalence were similar to the main analysis (supplementary table 9).
In 2018, an estimated 240 million (95% confidence interval 215 to 264 million) adults aged 18-69 years with hypertension in China had inadequately controlled blood pressure; among them, 164 million (141 to 186 million) were not aware of their condition and a further 10 million (9 to 12 million) were not receiving appropriate treatment. Despite a slight decrease in blood pressure, hypertension >160/100 mm Hg was not diagnosed or treated in more than 10% of men and women in 2018 (supplementary table 10).
Discussion
Using information from six rounds of a large national survey during 2004-18, our study found that although the prevalence of hypertension might have decreased moderately in China since 2010, awareness, treatment, and control remained low throughout the period. Although under-detection of hypertension was universally observed across all subgroups, large inequalities persisted in hypertension prevalence, awareness, treatment, and control between urban and rural areas, men and women, geographical regions, and socioeconomic groups.
Comparison with previous studies
A few studies have reported the national prevalence of hypertension at a single time point in China; the prevalence estimated in our study was generally consistent with the findings of those studies for similar time points.11 12 13 Specifically, the 2007-08 China National Diabetes and Metabolic Disorders Study reported that 27% of Chinese adults aged 20 years or older from 14 provinces had hypertension, compared with 24% for 18-69 years old in 2007 in our study.11 In the China National Survey of Chronic Kidney Disease, the adjusted prevalence of hypertension was reported as 30% for adults aged 18 years or older in 2009-10, which was the same as our findings for 2010 (30% for those aged ≥20 years).12 In a more recent nationwide study involving 451 755 residents from 31 provinces in mainland China, the reported prevalence of hypertension (23%) in 2012-15 was slightly lower than our findings (25% in 2013, 25% in 2015) possibly because the study used a different definition for hypertension to ours (ie, systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or use of antihypertensive drugs within two weeks).13 Several subnational studies reported trends in hypertension prevalence and management in parts of China,21 22 23 but few had assessed trends for the whole of China. A nationwide study used only post-2010 data on adults aged 45 years or older and reported that the weighted prevalence of hypertension increased from 41% in 2011 to 43% in 2013 and then declined to 42% in 2015, with improvements in diagnosis, treatment, and control of hypertension.24 The only study that reported nationwide trends in hypertension prevalence involving pre-2010 and post-2010 time points in China was a longitudinal cohort in the China Health and Nutrition Study, which used samples from 15 provinces that are not nationally representative and had a total sample size of 72 452 over nine rounds of surveys, much smaller than ours.25 It reported that the age standardised prevalence and its awareness, treatment, and control rates among adults aged 20-79 years increased with fluctuations from 1991 to 2015 (from 15% in 1991 to 26% in 2015). A recent meta-analysis pooled 18 national and non-national studies that reported hypertension prevalence in China from 1959 to 2018, including three rounds of the China Chronic Disease and Risk Factor Surveillance survey.26 It found a high heterogeneity (I2=99.9%) in the included studies, partly because these studies differed in age ranges and methods for age standardisation, and it reported that hypertension prevalence increased between 2004 and 2010 and declined in 2011 before continuing to increase through 2018.
Strengths and limitations of this study
Using consecutive, large scale, nationally representative surveys that adopted broadly consistent protocols, we provide information on the long term and recent trends in hypertension prevalence, awareness, treatment, and control in China in the past 15 years. The large sample sizes and regional representativeness also allowed reliable subgroup analyses of trends and variations. As with most long running national health surveys, our study also has limitations. Mercury sphygmomanometers were used in the 2004 survey, whereas electronic monitors were used in all other years; nonetheless, all electronic devices (Omron HEM-770A in 2007, HEM-7071 in 2010, and HBP-1300 in 2013, 2015, and 2018) had passed the accuracy standards and inspection of both the Association for the Advancement of Medical Instruments and the British Hypertension Society. In addition, we used self-reported status of antihypertensive drug use and history of hypertension diagnosis, which may be subject to recall bias. Previous studies showed that such self-reported drug and diagnosis history are in good agreement with medical records.27 28 We did not collect information on whether participants had been screened for hypertension or had sought care for hypertension. As with all population health surveillance efforts, our results might be affected by non-responses of survey participants and how non-responses varied across different surveys. Nonetheless, the response rate was high in all survey rounds, ranging from 90.5% in 2010 to 99.1% in 2007. In the 2010 survey, non-response rate showed no statistically significant association between hypertension prevalence and population characteristics, including age, marital status, education, and self-reported diabetes at survey county or district level. Biased estimation, however, might be introduced by non-response if differences existed in the characteristics that were associated with hypertension status between participants and those who refused to respond. Even after the adjustment in the weighting process for household and individual non-response, over-estimation or under-estimation of prevalence might persist and account for some of the observed patterns or trends. Despite independent sampling in each round of the China Chronic Disease and Risk Factor Surveillance survey, a small proportion of individuals were repeatedly included during 2004-18, which might contribute to a less precise estimation of hypertension prevalence and management. Owing to the limitation of having only six time points of surveys, we were unable to estimate the linear and non-linear trends robustly.
Interpretations and implications
Despite aging of the population, we found decreases in the number of individuals aged between 18 and 69 years with hypertension since 2010, mainly because of the decrease in prevalence of hypertension in the same period in most ages (fig 4). The decline in prevalence coincided with the introduction of several national health promotion programmes,29 which aimed to promote healthier lifestyles and risk reduction and might have played a role in the observed decline. Some improvement in diet was observed from 2002 and 2012, including an increase in fruit consumption and decrease in intake of refined carbohydrates and total energy.30 Additionally, salt intake has decreased since the 2000s,31 although levels of sodium intake in China still exceed recommended limits and remain among the highest in the world.32 The mild decrease in salt intake also failed to explain the increase in hypertension prevalence we observed from 2004 to 2010. As one of the major risk factors for hypertension,33 the increase in obesity prevalence slowed down similarly from 2010.16
Despite modest improvements in the management of hypertension in China, control was unsatisfactory. The control rate we found in China in 2018 (10-15%) was much lower than in high income countries in North America and Europe, as well as in South Korea and Japan (30-60%).5 Some countries with similar per capita national income as China’s, such as Costa Rica and Mexico, achieved hypertension control twice that of what we found in China, showing the feasibility of achieving better control in resource limited health systems.5
Nearly 60% of people with hypertension in China never received a diagnosis (supplementary fig 5). Therefore, better detection of people with hypertension is an important task. Experience from countries that have substantially improved the detection of hypertension typically involved improving the coverage of health insurance and regular blood pressure checks in health facilities according to guidelines.34 35 36 In China, the National Health and Family Planning Commission published guidance in 2009 that included mandatory blood pressure measurement for people older than 35 years when visiting hospital for the first time.37 Our findings, however, suggest poor implementation of guidance in practice.
Less than one third of people treated for hypertension in China achieved control (supplementary fig 5), therefore improving detection alone is unlikely to lead to sufficient improvements in hypertension control. At least four additional measures are needed. Firstly, the availability and affordability of multiple antihypertensive drug classes are essential to improve hypertension control.38 Poor access to multiple drugs and consequent underuse might have been an important factor behind the poor control we observed.39 40 Secondly, increasing the frequency of clinical visits could improve both adherence to antihypertensive treatment and hypertension control.41 Current guidelines in China recommend that patients with hypertension visit their general practitioners at least once every 1-3 months,42 but several subnational surveys in China found that only 60% of patients with hypertension visited their doctors frequently enough.41 43 Thirdly, besides healthcare facilities, communities and workplaces have also been important settings for implementing broad management programmes for hypertension prevention and management.44 45 Fourthly, improving the use of home blood pressure monitoring could help improve patient adherence to treatment and thereby reduce high blood pressure.46 47 With emerging technology and availability of smart phones, mHealth tools and devices such as wearable blood pressure monitors might help better self-management of hypertension, improve the reach of healthcare services, and promote healthy behaviour in users.48 49
Involvement of multidisciplinary staff in primary care is needed to enhance the synergy of multiple interventions that are being implemented. In the 1980s, the Capital Steel and Iron Company cardiovascular intervention programme, embedded in the local primary care system, achieved treatment and control rates as high as 98% and 72%.50 With rapid urbanisation and the rise and expansion of large state owned hospitals in cities, however, the role of primary care in hypertension management across China has diminished since the 1980s. There is a critical shortage of qualified general practitioners in China, particularly in rural areas,51 52 and knowledge of hypertension management among existing doctors is unsatisfactory,53 leading to poor implementation of hypertension guidelines. Despite the huge investment since the launch of National Basic Public Health Servicein 2009, financial and non-financial incentive mechanisms to improve quality of care delivered by general practitioners are still lacking.54 Capacity building and system strengthening in primary care are necessary throughout China for the large scale implementation of proven actions for improving hypertension control, such as opportunistic screening, providing public awareness programmes, and training doctors to reduce clinical inertia.
We also found that the urban-rural gap in hypertension control persisted despite a narrowing gap in awareness and treatment. The unified medical insurance scheme for urban and rural residents, rolled out in 2014 to replace the previously fragmented schemes, gradually reduced the gaps in healthcare utilisation and subsequently hypertension detection and treatment between rural and urban residents.55 A study also reported more progress in the proportion of antihypertensive drug use in rural areas than in urban areas from 2000 to 2011.56 Compared with people in urban areas, however, people in rural areas still have poorer adherence to treatment57 and access to healthcare,58 and primary care doctors have poorer adherence to guidelines,59 leading to the persisting gap in control between rural and urban areas. Therefore, it is important to build on the healthcare reform in rural areas to provide health education programmes for patients and doctors to encourage adherence to treatment.
We found that the prevalence of hypertension was inversely associated with education level among women, but the association was more mixed among men, consistent with studies from other countries.60 61 62 The sex specific education gradient in hypertension was similar to that observed for body mass index in China.16 The difference in sex specific education gradient in hypertension might be attributed to women with higher education being both better informed of health information and more apt to modify their lifestyles than men with higher education, compared with their counterparts with lower education.63
Conclusions
Despite moderate improvements in the prevalence and management of hypertension among adults in China, coverage of hypertension treatment and control remains low, highlighting the need for primary care to become reinvolved in the management of hypertension. Efforts should aim to both scale-up the detection of hypertension and enhance control among patients receiving treatment. Interventions are also needed to reduce the burden of hypertension in rural areas.
What is already known on this topic
Hypertension is a major cause of mortality and morbidity in China
Since the late 2000s, China has started multiple nationwide programmes for the prevention and control of hypertension
Current estimates of contemporary long term trends in hypertension prevalence, awareness, treatment, and control in China were based on data without national representativeness before 2015
What this study adds
Based on six rounds of a nationally representative survey during 2004-18 in China, this study showed that after an initial increase the standardised prevalence of hypertension declined from 2010
The awareness, treatment, and control of hypertension remained low throughout the study period
In 2018, an estimated 274 million people aged 18-69 years had hypertension in China and in most (240 million) control was inadequate
Acknowledgments
We thank the participants, project staff, and provincial and local China Centers for Disease Control and Prevention staff for their participation and contribution, and Ziwei Fu and Qian Zeng for collating thestatistical results in the revised manuscript.
Web extra.
Extra material supplied by authors
Supplementary information: Supplement 1-4, supplementary figures 1-7, and supplementary tables 1-12
Contributors: MZ, YS, and BZ contributed equally to the paper as joint first authors. LW (wanglimin@ncncd.chinacdc.cn) and YL (yichongli.cvd@139.com) are joint corresponding authors. YW and ME are joint senior authors. MZ, YS, BZ, ME, LW, and YL developed the study concept and drafted analyses plan. MZ, ZH, ZZ, CL, XZ, LW, and YL collected data. MZ, YS, and BZ conducted analysis and prepared results. MZ, YS, BZ, ME, LW, and YL wrote the first draft of the paper. YW and ME provided critical review. All authors provided input into interpretation of results and contents of the paper. MZ and LW had full access to all of the data in the study and verified the data. MZ, LW, and YL are responsible for the integrity of the data, accuracy of the data analysis, and decision to submit the manuscript, and act as guarantors. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: This study was supported by the National Key Research and Development Program of China (2018YFC1311700), Guangdong Basic and Applied Basic Research Foundation (2019A1515111003, 2021A1515220173), and the fund of “Sanming” Project of Medicine in Shenzhen (SZSM201811096). BZ is supported by a fellowship from the Abdul Latif Jameel Institute for Disease and Emergency Analytics, funded by a donation from Community Jameel, at Imperial College London. ME is supported by the UK Medical Research Council (MR/V034057/1). The funders were not involved in the research and preparation of the article, including study design; collection, analysis, and interpretation of data; in the writing of the article; or in the decision to submit the article for publication.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare: support from the National Key Research and Development Program of China, Guangdong Basic and Applied Basic Research Foundation, and the fund of “Sanming” Project of Medicine in Shenzhen for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; and no other relationships or activities that could appear to have influenced the submitted work.
The lead authors (LW and YL) affirm that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Dissemination to participants and related patient and public communities: We plan to disseminate these findings to participants and the general public through online news websites, press conferences, and printed survey reports.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Ethical approval
The protocol for the 2015 China Chronic Disease and Risk Factor Surveillance survey was approved by the ethics review committee of the Chinese Center for Disease Control and Prevention (CDC), and all other surveys were approved by the ethical committee of National Center for Chronic and Noncommunicable Disease Control and Prevention (NCNCD), China CDC.
Data availability statement
Individual participant data will not be made available publicly. For further detailed data access policy and procedure, contact jianceshi@ncncd.chinacdc.cn.
References
- 1. Murray CJL, Aravkin AY, Zheng P, et al. GBD 2019 Risk Factors Collaborators . Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396:1223-49. 10.1016/S0140-6736(20)30752-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ma Q, Li R, Wang L, et al. Temporal trend and attributable risk factors of stroke burden in China, 1990-2019: an analysis for the Global Burden of Disease Study 2019. Lancet Public Health 2021;6:e897-906. 10.1016/S2468-2667(21)00228-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zhou M, Wang H, Zeng X, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019;394:1145-58. 10.1016/S0140-6736(19)30427-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2016;387:957-67. 10.1016/S0140-6736(15)01225-8. [DOI] [PubMed] [Google Scholar]
- 5. NCD Risk Factor Collaboration (NCD-RisC) . Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021;398:957-80. 10.1016/S0140-6736(21)01330-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. NCD Risk Factor Collaboration (NCD-RisC) . Long-term and recent trends in hypertension awareness, treatment, and control in 12 high-income countries: an analysis of 123 nationally representative surveys. Lancet 2019;394:639-51. 10.1016/S0140-6736(19)31145-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Li Y, Wang J, Zhang X, Wu J, Liang X. Retrospect and Prospect of Healthy Lifestyle for All, 2007-2015. (In Chinese.) Chin J Health Educ 2016;32:1143-45. 10.16168/j.cnki.issn.1002-9982.2016.12.023 [DOI] [Google Scholar]
- 8. Chen Z. Launch of the health-care reform plan in China. Lancet 2009;373:1322-4. 10.1016/S0140-6736(09)60753-4. [DOI] [PubMed] [Google Scholar]
- 9. Jiang Y, Kong LZ, Li LM. [Implementing the strategy of ‘Healthy China’ and strengthening the setting-up of National Demonstration Areas, for Comprehensive Prevention and Control of Non-communicable Diseases]. (In Chinese.) Zhonghua Liu Xing Bing Xue Za Zhi 2018;39:391-3. 10.3760/cma.j.issn.0254-6450.2018.04.001 [DOI] [PubMed] [Google Scholar]
- 10. Wu Y, Huxley R, Li L, et al. China NNHS Steering Committee. China NNHS Working Group . Prevalence, awareness, treatment, and control of hypertension in China: data from the China National Nutrition and Health Survey 2002. Circulation 2008;118:2679-86. 10.1161/CIRCULATIONAHA.108.788166. [DOI] [PubMed] [Google Scholar]
- 11. Gao Y, Chen G, Tian H, et al. China National Diabetes and Metabolic Disorders Study Group . Prevalence of hypertension in china: a cross-sectional study. PLoS One 2013;8:e65938. 10.1371/journal.pone.0065938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Wang J, Zhang L, Wang F, Liu L, Wang H, China National Survey of Chronic Kidney Disease Working Group . Prevalence, awareness, treatment, and control of hypertension in China: results from a national survey. Am J Hypertens 2014;27:1355-61. 10.1093/ajh/hpu053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wang Z, Chen Z, Zhang L, et al. China Hypertension Survey Investigators . Status of Hypertension in China: Results From the China Hypertension Survey, 2012-2015. Circulation 2018;137:2344-56. 10.1161/CIRCULATIONAHA.117.032380. [DOI] [PubMed] [Google Scholar]
- 14. Zhang M, Wang L, Wu J, et al. Data Resource Profile: China Chronic Disease and Risk Factor Surveillance (CCDRFS). Int J Epidemiol 2022;51:e1-8. 10.1093/ije/dyab255. [DOI] [PubMed] [Google Scholar]
- 15. Yang G, Hu J, Rao KQ, Ma J, Rao C, Lopez AD. Mortality registration and surveillance in China: History, current situation and challenges. Popul Health Metr 2005;3:3. 10.1186/1478-7954-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wang L, Zhou B, Zhao Z, et al. Body-mass index and obesity in urban and rural China: findings from consecutive nationally representative surveys during 2004-18. Lancet 2021;398:53-63. 10.1016/S0140-6736(21)00798-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Heeringa SG, West BT, Berglund PA. Applied Survey Data Analysis. CRC Press, 2010: 29-31 10.1201/9781420080674. [DOI] [Google Scholar]
- 18. World Population Prospects . 2022. https://population.un.org/wpp/Download/Standard/MostUsed/.
- 19. Heeringa SG, West BT, Berglund PA. Applied Survey Data Analysis. CRC Press, 2010: 125-6 10.1201/9781420080674. [DOI] [Google Scholar]
- 20.SAS Institute. SAS/STAT® 14.2 User’s Guide. The SURVEYLOGISTIC Procedure, 2016.
- 21. Liu L, Chen CL, Lo K, et al. Trends of Status of Hypertension in Southern China, 2012-2019. Int J Gen Med 2020;13:599-608. 10.2147/IJGM.S267346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Fan LM, Wang F, Zhao M, Cui WL, Cai L. Socioeconomic differentials in trends in the prevalence of hypertension and pre-hypertension and hypertension awareness, treatment, and control in rural Southwestern China. BMC Cardiovasc Disord 2021;21:259. 10.1186/s12872-021-02062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Xing L, Liu S, Jing L, et al. Trends in Prevalence, Awareness, Treatment, and Control of Hypertension in Rural Northeast China: 2008 to 2018. Biomed Res Int 2020;2020:1456720. 10.1155/2020/1456720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zhao Y, Oldenburg B, Zhao S, Haregu TN, Zhang L. Temporal Trends and Geographic Disparity in Hypertension Care in China. J Epidemiol 2020;30:354-61. 10.2188/jea.JE20190029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ma S, Yang L, Zhao M, Magnussen CG, Xi B. Trends in hypertension prevalence, awareness, treatment and control rates among Chinese adults, 1991-2015. J Hypertens 2021;39:740-8. 10.1097/HJH.0000000000002698. [DOI] [PubMed] [Google Scholar]
- 26. Bao M, Wang L. The longitudinal trend of hypertension prevalence in Chinese adults from 1959 to 2018: a systematic review and meta-analysis. Ann Palliat Med 2020;9:2485-97. 10.21037/apm-19-377. [DOI] [PubMed] [Google Scholar]
- 27. Okura Y, Urban LH, Mahoney DW, Jacobsen SJ, Rodeheffer RJ. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol 2004;57:1096-103. 10.1016/j.jclinepi.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 28. Robinson JR, Young TK, Roos LL, Gelskey DE. Estimating the burden of disease. Comparing administrative data and self-reports. Med Care 1997;35:932-47. 10.1097/00005650-199709000-00006. [DOI] [PubMed] [Google Scholar]
- 29. Hu FB, Liu Y, Willett WC. Preventing chronic diseases by promoting healthy diet and lifestyle: public policy implications for China. Obes Rev 2011;12:552-9. 10.1111/j.1467-789X.2011.00863.x. [DOI] [PubMed] [Google Scholar]
- 30. He Y, Li Y, Yang X, et al. The dietary transition and its association with cardiometabolic mortality among Chinese adults, 1982-2012: a cross-sectional population-based study. Lancet Diabetes Endocrinol 2019;7:540-8. 10.1016/S2213-8587(19)30152-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hipgrave DB, Chang S, Li X, Wu Y. Salt and Sodium Intake in China. JAMA 2016;315:703-5. 10.1001/jama.2015.15816. [DOI] [PubMed] [Google Scholar]
- 32. Tan M, He FJ, Wang C, MacGregor GA. Twenty-Four-Hour Urinary Sodium and Potassium Excretion in China: A Systematic Review and Meta-Analysis. J Am Heart Assoc 2019;8:e012923. 10.1161/JAHA.119.012923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME. Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms. Circ Res 2015;116:991-1006. 10.1161/CIRCRESAHA.116.305697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Varghese C, Nongkynrih B, Onakpoya I, McCall M, Barkley S, Collins TE. Better health and wellbeing for billion more people: integrating non-communicable diseases in primary care. BMJ 2019;364:l327. 10.1136/bmj.l327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kim HS, Shin DW, Lee WC, Kim YT, Cho B. National screening program for transitional ages in Korea: a new screening for strengthening primary prevention and follow-up care. J Korean Med Sci 2012;27(Suppl):S70-5. 10.3346/jkms.2012.27.S.S70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Nerenberg KA, Zarnke KB, Leung AA, et al. Hypertension Canada . Hypertension Canada’s 2018 Guidelines for Diagnosis, Risk Assessment, Prevention, and Treatment of Hypertension in Adults and Children. Can J Cardiol 2018;34:506-25. 10.1016/j.cjca.2018.02.022. [DOI] [PubMed] [Google Scholar]
- 37.National Health and Family Planning Commission. Opinions on Gradually Promoting the Equalization of Basic Public Health Services, 2009. (In Chinese.) http://www.gov.cn/gongbao/content/2010/content_1555969.htm
- 38. Attaei MW, Khatib R, McKee M, et al. PURE study investigators . Availability and affordability of blood pressure-lowering medicines and the effect on blood pressure control in high-income, middle-income, and low-income countries: an analysis of the PURE study data. Lancet Public Health 2017;2:e411-9. 10.1016/S2468-2667(17)30141-X. [DOI] [PubMed] [Google Scholar]
- 39. Lu J, Lu Y, Wang X, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1·7 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet 2017;390:2549-58. 10.1016/S0140-6736(17)32478-9. [DOI] [PubMed] [Google Scholar]
- 40. Su M, Zhang Q, Bai X, et al. Availability, cost, and prescription patterns of antihypertensive medications in primary health care in China: a nationwide cross-sectional survey. Lancet 2017;390:2559-68. 10.1016/S0140-6736(17)32476-5. [DOI] [PubMed] [Google Scholar]
- 41. Zuo HJ, Ma JX, Wang JW, Chen XR, Hou L. The impact of routine follow-up with health care teams on blood pressure control among patients with hypertension. J Hum Hypertens 2019;33:466-74. 10.1038/s41371-018-0158-7. [DOI] [PubMed] [Google Scholar]
- 42.Chinese Hypertension League, National Center for Cardiovascular Diseases. 2010 Chinese guidelines for the management of hypertension.
- 43. Li Y, Ren D, Ding P, et al. [Evaluation on programs regarding the community-based management of hypertension and type 2 diabetes mellitus patients in eight provinces, China.] (In Chinese.) Zhonghua Liu Xing Bing Xue Za Zhi 2014;35:35-9. [PubMed] [Google Scholar]
- 44. Zhou YF, Chen S, Wang G, et al. Effectiveness of a Workplace-Based, Multicomponent Hypertension Management Program in Real-World Practice: A Propensity-Matched Analysis. Hypertension 2022;79:230-40. 10.1161/HYPERTENSIONAHA.121.18305. [DOI] [PubMed] [Google Scholar]
- 45. Chen S, Sudharsanan N, Huang F, Liu Y, Geldsetzer P, Bärnighausen T. Impact of community based screening for hypertension on blood pressure after two years: regression discontinuity analysis in a national cohort of older adults in China. BMJ 2019;366:l4064. 10.1136/bmj.l4064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Akpolat T, Arici M, Sengul S, et al. Home sphygmomanometers can help in the control of blood pressure: a nationwide field survey. Hypertens Res 2018;41:460-8. 10.1038/s41440-018-0030-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Sudharsanan N, Chen S, Garber M, Bärnighausen T, Geldsetzer P. The Effect Of Home-Based Hypertension Screening On Blood Pressure Change Over Time In South Africa. Health Aff (Millwood) 2020;39:124-32. 10.1377/hlthaff.2019.00585. [DOI] [PubMed] [Google Scholar]
- 48. Konstantinidis D, Iliakis P, Tatakis F, et al. Wearable blood pressure measurement devices and new approaches in hypertension management: the digital era. J Hum Hypertens 2022;36:945-51. 10.1038/s41371-022-00675-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Hamine S, Gerth-Guyette E, Faulx D, Green BB, Ginsburg AS. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. J Med Internet Res 2015;17:e52. 10.2196/jmir.3951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Wu XG, Gu DF, Wu YF, et al. [An evaluation on effectiveness of worksite-based intervention for cardiovascular disease during 1974 - 1998 in capital iron and steel company of Beijing.] (In Chinese.) Zhonghua Yu Fang Yi Xue Za Zhi 2003;37:93-7. [PubMed] [Google Scholar]
- 51. Hou J, Michaud C, Li Z, et al. Transformation of the education of health professionals in China: progress and challenges. Lancet 2014;384:819-27. 10.1016/S0140-6736(14)61307-6. [DOI] [PubMed] [Google Scholar]
- 52. Tam YH, Leung JYY, Ni MY, Ip DKM, Leung GM. Training sufficient and adequate general practitioners for universal health coverage in China. BMJ 2018;362:k3128. 10.1136/bmj.k3128. [DOI] [PubMed] [Google Scholar]
- 53. Chen Q, Zhang X, Gu J, Wang T, Zhang Y, Zhu S. General practitioners’ hypertension knowledge and training needs: a survey in Xuhui district, Shanghai. BMC Fam Pract 2013;14:16. 10.1186/1471-2296-14-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Li X, Lu J, Hu S, et al. The primary health-care system in China. Lancet 2017;390:2584-94. 10.1016/S0140-6736(17)33109-4. [DOI] [PubMed] [Google Scholar]
- 55. Li C, Tang C, Wang H. Effects of health insurance integration on health care utilization and its equity among the mid-aged and elderly: evidence from China. Int J Equity Health 2019;18:166. 10.1186/s12939-019-1068-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Li J, Shi L, Li S, Xu L, Qin W, Wang H. Urban-rural disparities in hypertension prevalence, detection, and medication use among Chinese Adults from 1993 to 2011. Int J Equity Health 2017;16:50. 10.1186/s12939-017-0545-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Liu J, Yang Y, Zhou J, et al. Prevalence and Associated Factors of Compliance Behaviors among Middle-Aged and Older Hypertensive Patients in China: Results from the China Health and Retirement Longitudinal Study. Int J Environ Res Public Health 2020;17:7341. 10.3390/ijerph17197341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Zhang X, Dupre ME, Qiu L, Zhou W, Zhao Y, Gu D. Urban-rural differences in the association between access to healthcare and health outcomes among older adults in China. BMC Geriatr 2017;17:151. 10.1186/s12877-017-0538-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Hou L, Chen X, Chen B, et al. Pharmacological therapy and blood pressure control in primary health care sites in China: data from 254,848 hypertensive patients. Clin Epidemiol 2018;10:1467-78. 10.2147/CLEP.S172567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Li Z, Fu C, Yang F, Mao Z. Prevalence and risk factors of hypertension for the middle-aged population in China - results from the China Health and Retirement Longitudinal Study (CHARLS). Clin Exp Hypertens 2019;41:80-6. 10.1080/10641963.2018.1445751. [DOI] [PubMed] [Google Scholar]
- 61. Dong GH, Wang D, Liu MM, et al. Sex difference of the prevalence and risk factors associated with prehypertension among urban Chinese adults from 33 communities of China: the CHPSNE study. J Hypertens 2012;30:485-91. 10.1097/HJH.0b013e32834f9dd3. [DOI] [PubMed] [Google Scholar]
- 62. Alves RF, Faerstein E. Educational inequalities in hypertension: complex patterns in intersections with gender and race in Brazil. Int J Equity Health 2016;15:146. 10.1186/s12939-016-0441-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Leng B, Jin Y, Li G, Chen L, Jin N. Socioeconomic status and hypertension: a meta-analysis. J Hypertens 2015;33:221-9. 10.1097/HJH.0000000000000428. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary information: Supplement 1-4, supplementary figures 1-7, and supplementary tables 1-12
Data Availability Statement
Individual participant data will not be made available publicly. For further detailed data access policy and procedure, contact jianceshi@ncncd.chinacdc.cn.