Abstract
Background:
Medial meniscus root tears (RTs) are associated with the development and worsening of knee osteoarthritis (OA), but little is known about their progression when compared with meniscal tears that spare the root (nonroot tears; NRTs).
Purpose:
To compare radiographic worsening of OA in knees with RTs versus NRTs and to identify factors associated with radiographic worsening of OA in knees with RTs.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Using the Osteoarthritis Initiative database, we included knees with medial meniscus RTs and NRTs present at the baseline visit (baseline tears) and new RTs and NRTs observed at 12- to 48-month annual follow-up visits (incident tears). Worsening of radiographic OA was defined for baseline tears as an increase in Kellgren-Lawrence grade (KLG) during the subsequent 12 months of follow-up; for incident tears, worsening was defined as either concurrent (increase in KLG over the 12 months preceding tear appearance on magnetic resonance imaging) or subsequent (increase in KLG during the 12 months after tear appearance). Odds ratios (ORs), adjusted for covariates, were calculated for the association of worsening by type of tear.
Results:
Included were 39 knees with baseline RTs, 633 knees with baseline NRTs, 33 knees with incident RTs, and 234 knees with incident NRTs. Radiographic OA worsening subsequent to meniscal tear identification was no different for baseline RTs (15%) or baseline NRTs (14%; adjusted OR, 1.34; 95% CI, 0.52-3.47), nor did subsequent worsening differ for incident RTs (19%) versus incident NRTs (18%; adjusted OR, 0.52; 95% CI, 0.15-1.83). Concurrent radiographic OA worsening was seen at a significantly higher rate for incident RTs (64%) versus incident NRTs (21%; adjusted OR, 3.00; 95% CI, 1.21-7.47). Incident RTs in knees without radiographic OA (KLG 0-1) before the tear had a high rate of worsening (94%, n = 16) and were more likely to worsen than those in knees with radiographic OA (KLG ≥2) present before the tear.
Conclusion:
Compared with NRTs, incident RTs were associated with a significantly increased risk of worsening radiographic OA over a 12-month period concurrent with the appearance of the tear. Incident RTs in knees without radiographic OA at baseline had a high rate of worsening.
Keywords: knee osteoarthritis, medial meniscal tear, meniscus root, meniscus root tear
The menisci play an integral role in chondroprotection in the knee joint by acting as shock absorbers, allowing dispersion of axial loads into circumferential hoop stress.2,10 Meniscus root tears (RTs) involve dissociation of the meniscal substance from its bony insertion by avulsion or complete radial tear (Figure 1). This disruption of the circumferential collagen fibers prevents effective hoop stress distribution, resulting in altered joint kinematics and markedly increased tibiofemoral contact pressures, equivalent to those seen after total meniscectomy.1,20 Meniscal extrusion is observed after medial RT and progresses rapidly within the 12-month period after disruption of the posterior root. 11 RTs most commonly occur at the posterior meniscus root attachments, potentially due to the increased physiologic mobility of the anterior roots, 2 and are most often atraumatic or associated with minor injury during a physiologic motion such as squatting. 16 Medial meniscus posterior RT is more common in an older, heavier, and more predominantly female population than lateral posterior RTs which are seen mostly in association with anterior cruciate ligament (ACL) rupture.2,6,14
Figure 1.

(A) Illustration of a radial tear at the medial meniscus posterior root with extrusion of the medial meniscus body due to loss of circumferential hoop stress. Posterior cruciate ligament subtracted to better visualize the posteromedial root. (B) Coronal MRI scan demonstrating radial tear at the medial meniscus posterior root (arrow) with extrusion of medial meniscal body. (C) Sagittal MRI scan showing “ghost sign” seen with absence of meniscal tissue at location of radial tear near posterior root attachment (arrow). (D) Axial MRI scan showing radial tear at posterior medial meniscus root attachment site (arrow). MRI, magnetic resonance imaging.
The summative result of meniscal extrusion, loss of hoop stress distribution, and altered joint kinematics after medial meniscus RT is medial tibiofemoral cartilage breakdown. A previous study utilizing the Multicenter Osteoarthritis Study cohort showed that, in knees with radiographic osteoarthritis (OA), those with medial meniscus RT are significantly more likely to have severe and progressive cartilage damage than those without meniscal injury, but this difference was not significant in comparing RTs with nonroot medial meniscal tears. 12 Medial meniscus RTs treated nonoperatively or with meniscal debridement yields extremely high rates of OA progression (95%) and total knee arthroplasty (50%) at 10-year follow-up. 7
While the occurrence of cartilage degeneration after meniscus root injury is well established, the period for progression and the impact of involvement of the root as compared with medial meniscal tears that spare the root are less clear. A previous magnetic resonance imaging (MRI) study demonstrated meniscal extrusion and medial compartment articular cartilage degeneration in the first year after medial meniscus RT diagnosis, but no study to date has evaluated the time course of OA development beginning with an intact meniscus on baseline (pretear) imaging. 17 This distinction is important to ensure capture of all degenerative changes from the patient's true baseline, meniscal-intact, state rather than assuming that imaging at time of injury is representative of preinjury joint health, particularly given the often atraumatic presentation of medial meniscus RTs. This is valuable information for the purposes of proper patient education when considering treatment options including the relative urgency of potential surgical refixation.
In this study, we utilized the database of the Osteoarthritis Initiative (OAI) to describe and compare longitudinal radiographic degenerative changes in knees with incident (new) medial meniscus RTs and knees with incident medial meniscal tears not involving the meniscus root (nonroot tears; NRTs). The hypothesis was that knees with incident medial meniscus RT would have a greater frequency of worsening of radiographic OA within 1 year of tear recognition than NRT knees. In addition, we aimed to identify factors associated with an increased risk of OA worsening in participants with an incident medial meniscus RT, as this is not described in current literature. We hypothesized that among persons with an incident RT, those who are older, with a higher body mass index (BMI), and increased activity level would be more likely to have radiographic worsening.
Methods
The protocol for this study was approved by the institutional review boards at all participating institutions. The OAI (https://nda.nih.gov/oai) is a US National Institutes of Health-funded multicenter observational cohort study that enrolled 4796 White (82%) and African American (18%) men (42%) and women (58%) aged 45 to 79 years with the goal of identifying factors predisposing participants to development or progression of knee OA. OAI participants provided informed consent and had imaging (radiographs and MRI) completed at enrollment and annually at 12-, 24-, 36, and 48-months after enrollment. Those enrolled participants had knee OA or had an elevated risk for knee OA based on having 1 or more risk factors, including obesity, knee symptoms, or a history of self-reported knee injury or knee surgery. Participants in OAI included in the present study were assessed at baseline and annually for both clinical and radiological data, including bilateral knee MRI scan and knee radiographic assessments.
For the present study, we included 939 knees from the public database that had an MRI reading for medial meniscal tears with the necessary minimum MRI and radiographic images, as depicted in Figure 2. MRI scans were each read by 1 of 2 experienced musculoskeletal radiologists for features of OA using MRI Osteoarthritis Knee Score, 13 including presence of medial meniscus RTs and presence and location of tears including involvement of the anterior horn, body, and/or posterior horn of the medial meniscus. Intra- and interrater reliability for readings of meniscal tears by the readers of the OAI knee MRI scans has been reported previously to be excellent. 23 Using the OAI readings, we identified all knees with medial meniscal tears at baseline and/or follow-up visits. Knees with RT and NRT were categorized as tears present on the OAI baseline MRI study (baseline tear) and those with normal menisci on baseline MRI and an RT or NRT seen for the first time on a subsequent follow-up MRI (incident tear). There were 72 medial meniscus RTs (39 at baseline, 33 incident), and 867 medial meniscus NRTs (633 at baseline, 234 incident) with subsequent or concurrent follow-up radiographic worsening data (Figure 2).
Figure 2.
Flowchart of eligible participants for the study. MM, medial meniscus; MOAKS, MRI Osteoarthritis Knee Score; MRI, magnetic resonance imaging; NRTs, nonroot tears; OAI, Osteoarthritis Initiative; RTs, root tears; TKA, total knee arthroplasty.
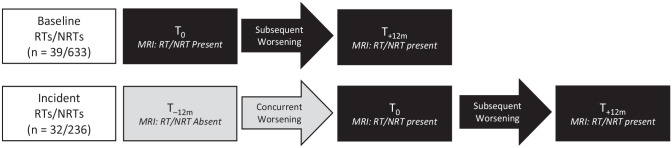
For each knee with an incident tear, the visit at which the meniscal tear was first seen on MRI scan was defined as the index visit (T0), and the annual visit immediately before the index visit was labeled as T−12m. For baseline tears, T0 was synonymous with the initial OAI baseline visit. For both baseline and incident tears, the annual visit after the index visit was labeled as T+12m, as it occurred 12 months subsequent to identification of the meniscal tear. For both baseline and incident tears, radiographic worsening subsequent to the tear was defined as an increase in Kellgren-Lawrence grade (KLG) from T0 to T+12m. In addition, for incident tears only, radiographic worsening concurrent with the first appearance of RT or NRT was defined as an increase in KLG from the visit 12 months before the index visit (T−12m), representing the most recent visit without evidence of a tear on MRI scan, compared with T0. This is illustrated in Figure 3.
Figure 3.
Nomenclature for timing of worsening in radiographic OA for baseline and incident RTs or NRTs. MRI, magnetic resonance imaging; NRT, nonroot tear; OA, osteoarthritis; RT, root tear; T0, index visit (baseline); T−12m, annual visit immediately before the index visit; T+12m, annual visit immediately after the index visit.
The KLG on knee radiographs were assessed by 2 experienced musculoskeletal radiologists.8,9,15 For clarity, radiographic worsening included all increases in KLG regardless of whether a knee had radiographic OA (KLG ≥2) at the start of the follow-up period. Knees that could not be classified as having subsequent or concurrent worsening due to missing radiographic data were excluded from analyses of these outcomes, respectively. Knees with a KLG of 4 at both T−12m and T0 were excluded from analyses of concurrent worsening since they were ineligible for an increase in KLG. Similarly, knees that had a KLG of 4 at both T0 and T+12m were excluded from analyses of subsequent worsening. In addition, knees that had incident arthroplasty without documentation of increased KLG were excluded due to inability to determine whether radiographic worsening occurred. Sensitivity analyses to investigate the use of incident arthroplasty as a worsening definition were performed by including these knees in the relevant analyses, and this did not change our results.
Patient and knee characteristics assessed at the index (baseline) visit for baseline tears were sex, age, BMI, activity level as defined by the Physical Activity Scale for the Elderly (PASE),21,24 recent knee injury (defined as an injury within the previous 12 months severe enough to limit the ability to walk for at least 2 days), and presence of frequent knee pain (defined as pain on most days of the month within the previous 12 months). For incident tears, these same features were assessed at T−12m.
Statistical Analysis
Patient and knee characteristics were compared between baseline RTs and NRTs and between incident RTs and incident NRTs. To explore potential factors associated with radiographic worsening in knees with incident RTs, we also compared the characteristics of patients and knees with incident RTs that had worsening OA versus those with RTs that did not worsen. Continuous variables were compared using the Student t test. Categorical data were compared using Fisher exact and chi-square tests. A P value <.05 was considered statistically significant for all calculations.
Associations between tear type (NRT vs RT) and the odds of subsequent and concurrent radiographic progression were assessed by logistic regression (with a generalized estimating equation used to account for the possibility that 2 knees per person were included in the analyses). All models were adjusted for sex, age, BMI, PASE, frequent knee pain, and KLG (0-1 vs ≥2) using T0 values for baseline tears and T−12m values for incident tears. Due to the relatively small sample size, assessment based on KLG was grouped by those with a nonarthritic score (KLG 0-1) and those with at least early radiographic arthritis (KLG ≥2) rather than by individual score 0-4. Models for baseline tears were also adjusted for recent knee injury. There were too few knees with recent knee injury to include in models for incident tears. All analyses were performed using the Statistical Analysis System (SAS) Version 9.4.
Results
Table 1 shows the characteristics at T0 of participants and knees with baseline tears and the characteristics at T−12m for those with incident tears. Characteristics of participants and knees with baseline RT and NRTs were mostly similar. However, knees with baseline RTs were more likely to have radiographic OA (KLG ≥2) and to be associated with a self-reported history of a recent knee injury, although report of injury was very uncommon in both groups (Table 1).
Table 1.
Demographics at T0 for Baseline Tears and T−12m for Incident Tears a
| Characteristics of Baseline Tears at T0 | Characteristics of Incident Tears at T−12m | |||||
|---|---|---|---|---|---|---|
| RTs (n = 39) | NRTs (n = 633) | P | RTs (n = 33) | NRTs (n = 234) | P | |
| Female sex | 19 (49%) | 291 (45%) | .680 | 27 (82%) | 112 (48%) | .0001 |
| Age, y | 64.7 ± 8.3 | 62.9 ± 8.8 | .197 | 60.8 ± 7.3 | 61.1 ± 8.7 | .885 |
| BMI, kg/m2 | 29.7 ± 5.1 | 29.0 ± 4.5 | .407 | 32.0 ± 5.7 | 28.7 ± 4.6 | .004 |
| PASE score | 167.1 ± 87.3 | 164.9 ± 85.2 | .836 | 177.8 ± 82.9 | 164.2 ± 86.1 | .384 |
| Recent knee injury | 3 (8%) | 18 (3%) | .049 | 1 (3%) | 5 (2%) | .722 |
| Frequent knee pain | 16 (41%) | 273 (43%) | .766 | 8 (24%) | 72 (30%) | .513 |
| KLG | .015 | .004 | ||||
| 0-1 | 8 (21%) | 250 (39%) | 17 (51%) | 177 (73%) | ||
| 2-3 | 31 (79%) | 386 (60%) | 16 (49%) | 57 (24%) | ||
| 4 | 0 (0%) | 6 (15%) | 0 (0%) | 0 (0%) | ||
For T0 characteristics, knees are included if they have KLG progression data at T0 and T+12m. For T−12m characteristics, knees are included if they have KLG progression data from T−12m to T0. Data are shown as n (%) or mean ± SD. Boldface P values indicate statistically significant difference between the RT and NRT groups (P < .05). BMI, body mass index; KLG, Kellgren-Lawrence grade; NRT, nonroot tear; PASE, Physical Activity Scale for the Elderly; RT, root tear; T0, index visit (baseline); T−12m, annual visit immediately before the index visit; T+12m, annual visit immediately after the index visit.
Compared with incident NRTs, knees with incident RTs at T−12m were significantly more likely to have a KLG ≥2 and to have occurred in women and participants with a higher mean BMI (Table 1). Report of a recent knee injury in the 12 months preceding MRI was similarly uncommon in incident RTs and NRTs. There were also no differences between incident tear groups for age, physical activity, or frequent knee pain.
Table 2 compares the frequency of radiographic OA worsening in knees with RTs versus NRTs. For baseline tears, there was no difference in the risk of subsequent worsening (increase in KLG from T0 to T+12m). For incident tears, the percentage of knees with subsequent worsening was also similar for RTs (19%) and NRTs (18%), with an adjusted odds ratio (OR) for worsening in RTs of 0.52 (95% CI, 0.15-1.83). In contrast, incident RTs had a significantly greater risk of concurrent worsening compared with NRTs (64% vs 21%, respectively; P < .00001) and a significantly increased likelihood of concurrent worsening in RTs compared with NRTs (adjusted OR, 3.00; 95% CI, 1.21-7.47). Overall, from the 33 knees with incident RT, 2 had missing follow-up radiographs, which meant that subsequent worsening could not be ruled out. From the remaining 30, 24 (80%) knees with incident RTs had radiographic worsening in either the 12 months leading up to or the 12 months following MRI identification of the tear.
Table 2.
Incidence of Radiographic Worsening by Tear Type in Knees With Baseline Tears and Incident Tears and Likelihood for the Association of RTs Versus NRTs With Progression a
| Baseline Tears: Subsequent Worsening, T0 to T+12m | ||
|---|---|---|
| No | Yes | |
| Baseline NRT (n = 633) | 540 (85%) | 93 (15%) |
| Baseline RT (n = 39) | 33 (85%) | 6 (15%) |
| P | .542 | |
| Crude OR (95% CI) | 1.06 (0.43-2.57) | |
| Adjusted OR (95% CI) b | 1.34 (0.52-3.47) | |
| Incident Tears: Subsequent Worsening, T0 to T+12m | ||
| No | Yes | |
| Incident NRT (n = 195) c | 159 (82%) | 36 (18%) |
| Incident RT (n = 26) c | 21 (81%) | 5 (19%) |
| P | .924 | |
| Crude OR (95% CI) | 1.05 (0.37-2.97) | |
| Adjusted OR (95% CI) b | 0.52 (0.15-1.83) | |
| Incident Tears: Concurrent Worsening, T−12m to T0 | ||
| No | Yes | |
| Incident NRT (n = 234) | 186 (79%) | 48 (21%) |
| Incident RT (n = 33) | 12 (36%) | 21 (64%) |
| P | <.00001 | |
| Crude OR (95% CI) | 6.78 (3.10-14.8) | |
| Adjusted OR (95% CI) b | 3.00 (1.21-7.47) | |
NRT and RT data are shown as number of knees (%). Boldface P value indicates statistically significant difference between knees with versus without concurrent tear worsening (P < .05). BMI, body mass index; CI, confidence interval; KLG, Kellgren-Lawrence grade; NRT, nonroot tear; OAI, Osteoarthritis Initiative; OR, odds ratio; PASE, Physical Activity Scale for the Elderly; RT, root tear; T0, index visit (baseline); T−12m, annual visit immediately before the index visit; T+12m, annual visit immediately after the index visit.
All models were adjusted for sex and for age, BMI, PASE, frequent knee pain and KLG (0-1 vs ≥2) using T0 values for baseline tears and T−12m values for incident tears. Models for baseline tears were also adjusted for recent knee injury. There were too few knees with recent knee injury to include in models for incident tears. Generalized estimating equations were used to account for the possibility of both knees per person.
Incident RTs and NRTs identified on the final scheduled OAI visit did not have subsequent visit data available, accounting for the discrepancy in numbers of incident NRT and RT within this column.
Among incident RTs, the characteristics of participants and knees with worsening of radiographic OA (either concurrent or subsequent) were mostly not significantly different from those that did not worsen (Table 3). However, the knees that worsened were significantly more likely to have a pre-RT KLG of 0-1 (67%) as compared to those that did not worsen (14% KLG 0-1). Of the 17 knees without radiographic OA before an incident RT, 16 (94%) worsened. Worsening OA with incident RT occurred more often in women. Although there was a trend for more isolated RTs (not involving the posterior horn or body) in knees that worsened (50% vs 14% in the knees that did not worsen), this did not reach statistical significance (P = .19).
Table 3.
Characteristics at T−12m (Before the Tear) of Knees With Incident RTs According to Whether the Knee had Radiographic Worsening Either Concurrent With or Subsequent to the RT
| No Radiographic Worsening (n = 7) | Radiographic Worsening (n = 24) | P | |
|---|---|---|---|
| Female sex | 4 (57) | 22 (92) | .029 |
| Age, y | 60.6 ± 9.5 | 61.3.5 ± 6.8 | .860 |
| BMI, kg/m2 | 31.8 ± 7.5 | 32.3 ± 5.3 | .873 |
| PASE | 189.3 ± 75.8 | 166.4 ± 78.1 | .501 |
| Recent knee injury | 2 (29) | 6 (25) | .849 |
| Frequent knee pain | 1 (14) | 6 (26) | .551 |
| KLG | .014 | ||
| 0-1 | 1 (14) | 16 (67) | |
| ≥2 | 6 (86) | 8 (33) | |
| Meniscal tear type | .19 b | ||
| Isolated RT | 1 (14) | 12 (50) | |
| RT + posterior horn | 5 (71) | 9 (38) | |
| RT + body | 0 (0) | 3 (14) | |
| RT + posterior horn + body | 1 (14) | 0 (0) |
Two of the 33 knees with concurrent worsening as noted in Table 2 did not have a later radiograph at 1 month after the index visit to determine whether they then had subsequent worsening and are thus excluded from this table. Data are shown as No. of knees (%) or mean ± SD. Boldface P values indicate statistically significant difference between groups (P < .05). BMI, body mass index; KLG, Kellgren-Lawrence grade; PASE, Physical Activity Scale for the Elderly; RT, root tear; T–12m, annual visit immediately before the index visit.
The comparison for meniscal tear type was isolated RT versus all other types.
Discussion
Incident medial meniscus RTs are associated with significantly more frequent worsening of radiographic OA than medial meniscal tears that spare the posterior root. Overall, 77.4% of incident RTs had radiographic worsening in either the 12 months leading up to or the 12 months following MRI identification of the tear. Most of the worsening in RTs was concurrent with the incidence of the tear, occurring in the 12 months between the last normal MRI scan (T−12m) and the visit at which meniscal injury was first seen on MRI scan (T0). We found a significant, nearly 3-fold greater, likelihood of concurrent progression in RTs compared with NRTS. This timecourse suggests that the articular cartilage breakdown associated with medial meniscus RT occurs quite rapidly, within less than a year and typically concurrent with development of root disruption. The relatively infrequent radiographic worsening seen in incident RT (19%) subsequent to injury (T0 to T+12m) cannot be explained directly by findings in this study but does suggest that the impact of most meniscus RTs on the joint may occur early with the acute loss of hoop stress distribution and resultant increase in contact pressure, with more gradual progression thereafter, at least in the short term studied here.
Given the pattern of rapid OA development established within this group of participants with medial meniscus RT, early identification and, if indicated, surgical treatment may help in altering this otherwise daunting natural history. Although worsening of OA may still occur despite root repair, the 10-year rates of progressive OA and total knee arthroplasty have previously been shown to be significantly lower with medial meniscus root repair as compared with meniscectomy or nonoperative care.3,7 Transtibial pullout repair of medial meniscus RTs has demonstrated effective restoration of joint contact area and pressure and provides clinical improvement with high patient satisfaction and good survivorship.2,3,5,18,19,22 Unsurprisingly, worse tibiofemoral compartment cartilage degeneration has been associated with poor outcomes after medial meniscus root repair. 4 While this study cannot directly affect surgical recommendations given the lack of a surgical treatment group, our finding of relatively rapid radiographic OA worsening suggests a need to consider available interventions soon after diagnosis of medial meniscus RT in an effort to avoid cartilage degeneration before delayed repair.
Compared with incident NRTs, incident RTs were significantly more likely to occur in overweight and more active middle-aged women and in knees with more severe radiographic OA. These findings are in agreement with earlier studies of risk factors for medial meniscus RT with the exception of activity level, which has previously been reported to be lower in persons with RT as compared with NRT. 14 Recent knee injury severe enough to limit the ability to walk for at least 2 days was similarly uncommon in incident RT (3%) and incident NRT (2%) knees, with incident RT (26%), consistent with previous literature citing classically atraumatic or minor trauma associated medial meniscus RT. 16
We did not find differences in participant characteristics including age, BMI, activity level, history of injury, or frequent knee pain, between incident RTs that worsened as compared with those that did not worsen. The group of incident RTs that worsened was comprised of a greater number of females and the pre-RT KLG was significantly lower, indicatingmore more knees with an absence of radiographic OA, as compared to the knees that did not worsen. Nearly all knees (94%) without radiographic OA before an RT showed radiographic worsening of OA during follow-up. This indicates a high risk of OA development in normal knees that have a new RT, which is in agreement with existing literature. 7
Notably, there was no significant difference in frequency of radiographic worsening of OA for baseline RT versus baseline NRT, with a large majority of both groups seeing no radiographic worsening throughout the study period (85% in both groups). It can be inferred from the high frequency of concurrent worsening in the incident RT group that perhaps this lack of difference in the baseline RT versus NRT groups is because those tears that would undergo radiographic worsening had done so before enrollment in the study, highlighting the inherent flaw in utilizing baseline meniscal tears to study natural progression of disease without a true preinjury baseline included in the study.
The findings of this study are impactful and help to better define the natural history of medial meniscus root injury to more effectively counsel patients. Our study has several important strengths. We used serial knee MRI scans and radiographs from annual visits of the OAI and could therefore study incident meniscal tears and identify the approximate timepoint at which the tear first appeared on MRI scan to assess radiographic findings and worsening both before and after the tear appeared. The knee imaging protocols and assessment of MRI scans and patient and knee characteristics in our study were standardized across participants and obtained at uniform timepoints during the study. A study of this nature cannot be performed with surveys of baseline meniscal tears since there is no way to know when the tear occurred, and pretear information is usually not available. Thus, the rate of radiographic changes during follow-up of baseline tears without an antecedent normal MRI study cannot be generalized to new and recent tears. Because we used data from the large OAI study, we were able to identify a sufficient number of incident RTs and NRTs to support our analyses.
Limitations
Our study has several limitations. RTs are relatively uncommon and the number we observed even in the large OAI database was small. As a result, the confidence intervals for the association of RT versus NRT with radiographic worsening are wide. Importantly, MRI scans performed annually in the OAI database are not of sufficient frequency to truly capture the timeline over which an RT and associated cartilage degeneration occurs, leaving the proverbial chicken or the egg question unanswered. Because the most significant difference between RT and NRT knees in this study was concurrent worsening of OA, it remains impossible to confidently determine causation with the annual imaging studies this database. While more frequent MRI and radiographic examination could help to settle this debate, the number of additional imaging studies needed to capture this relatively infrequent pathology may prove prohibitive, particularly in a database of this size. There were differences in baseline characteristics, including sex, BMI, and radiographic OA, between incident RT and NRT. However, we adjusted for these potential confounders in our analyses of radiographic worsening. The comparison of incident RTs that worsened and did not worsen during the study was also based on small numbers and may have been underpowered to detect differences. The OAI database did not consistently provide data regarding detailed tear morphologic description (ie, radial, vertical, horizontal) for NRTs, concurrent ligamentous injury, or limb mechanical axis, which may each impact risk of osteoarthritic progression. Data on concomitant ACL tears at T0 was available in a subset (41%) of the knees with incident meniscal tears in our study. Of these, none of the incident RTs and NRTs had an ACL tear at T0. Nevertheless, because of the incomplete data on ligament tears in our study, we cannot rule out that ligament tears were more common in incident RT knees and that this could have a confounding effect on our findings. In addition, OAI database participant surgical history such as previous meniscectomy or meniscal repair, ligamentous reconstruction, or other intra-articular surgery was not consistently recorded and could prove confounding. Finally, because there were no data on interim repair of RTs within this study, alterations in the natural history of RTs after surgical fixation, and thus direct treatment recommendations, cannot be surmised.
Conclusion
Incident medial meniscus RTs were associated with a significantly increased risk of rapid, short-term worsening of radiographic OA, particularly in knees without radiographic OA before the occurrence of the tear. Knees with more advanced OA did not see significant radiographic worsening after RT. Physicians should consider having a low threshold for advanced imaging when RT is suspected in a nonarthritic knee to facilitate a timely diagnosis and discussion of treatment options before the onset of this rapid articular breakdown.
Footnotes
Final revision submitted April 22, 2023; accepted May 4, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: Research reported in this publication was supported in part by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (award number P30AR075055) and by a grant from the University of California-San Francisco Core Center for Musculoskeletal Biology and Medicine Core Voucher Program. The Osteoarthritis Initiative is a public-private partnership comprising 5 contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the United States National Institutes of Health (NIH), a branch of the Department of Health and Human Services, and conducted by the Osteoarthritis Initiative (OAI) study investigators. Private funding partners include Merck Research Laboratories, Novartis Pharmaceuticals, GlaxoSmithKline, and Pfizer. Private-sector funding for the OAI is managed by the Foundation for the NIH. This manuscript does not necessarily reflect the opinions or views of the OAI investigators, the NIH, or the private funding partners. C.C.C. has received education payments from Arthrex and hospitality payments from Stryker. B.T.F. has received education payments from Evolution Surgical. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from University of California-San Francisco (IRB No. 10-00532).
References
- 1. Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am. 2008;90(9):1922-1931. [DOI] [PubMed] [Google Scholar]
- 2. Bhatia S, LaPrade CM, Ellman MB, LaPrade RF. Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med. 2014;42(12):3016-3030. [DOI] [PubMed] [Google Scholar]
- 3. Chung KS, Ha JK, Ra HJ, Kim JG. A meta-analysis of clinical and radiographic outcomes of posterior horn medial meniscus root repairs. Knee Surg Sports Traumatol Arthrosc. 2016;24(5):1455-1468. [DOI] [PubMed] [Google Scholar]
- 4. Chung KS, Ha JK, Ra HJ, Kim JG. Prognostic factors in the midterm results of pullout fixation for posterior root tears of the medial meniscus. Arthroscopy. 2016;32(7):1319-1327. [DOI] [PubMed] [Google Scholar]
- 5. Chung KS, Noh JM, Ha JK, et al. Survivorship analysis and clinical outcomes of transtibial pullout repair for medial meniscus posterior root tears: a 5- to 10-year follow-up study. Arthroscopy. 2018;34(2):530-535. [DOI] [PubMed] [Google Scholar]
- 6. De Smet AA, Blankenbaker DG, Kijowski R, Graf BK, Shinki K. MR diagnosis of posterior root tears of the lateral meniscus using arthroscopy as the reference standard. AJR Am J Roentgenol. 2009;192(2):480-486. [DOI] [PubMed] [Google Scholar]
- 7. Faucett SC, Geisler BP, Chahla J, et al. Meniscus root repair vs meniscectomy or nonoperative management to prevent knee osteoarthritis after medial meniscus root tears: clinical and economic effectiveness. Am J Sports Med. 2019;47(3):762-769. [DOI] [PubMed] [Google Scholar]
- 8. Felson D, Niu J, Sack B, et al. Progression of osteoarthritis as a state of inertia. Ann Rheum Dis. 2013;72(6):924-929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Felson DT, Niu J, Guermazi A, Sack B, Aliabadi P. Defining radiographic incidence and progression of knee osteoarthritis: suggested modifications of the Kellgren and Lawrence scale. Ann Rheum Dis. 2011;70(11):1884-1886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fithian DC, Kelly MA, Mow VC. Material properties and structure-function relationships in the menisci. Clin Orthop Relat Res. 1990;(252):19-31. [PubMed] [Google Scholar]
- 11. Furumatsu T, Kodama Y, Kamatsuki Y, Hino T, Okazaki Y, Ozaki T. Meniscal extrusion progresses shortly after the medial meniscus posterior root tear. Knee Surg Relat Res. 2017;29(4):295-301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Guermazi A, Hayashi D, Jarraya M, et al. Medial posterior meniscal root tears are associated with development or worsening of medial tibiofemoral cartilage damage: the multicenter osteoarthritis study. Radiology. 2013;268(3):814-821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hunter DJ, Guermazi A, Lo GH, et al. Evolution of semi-quantitative whole joint assessment of knee OA: MOAKS (MRI Osteoarthritis Knee Score). Osteoarthritis Cartilage. 2011;19(8):990-1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hwang BY, Kim SJ, Lee SW, et al. Risk factors for medial meniscus posterior root tear. Am J Sports Med. 2012;40(7):1606-1610. [DOI] [PubMed] [Google Scholar]
- 15. Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kim JH, Chung JH, Lee DH, Yoon-Seok Lee YS, Kim JR, Ryu KJ. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: a prospective comparison study. Arthroscopy. 2011;27(12):1644-1653. [DOI] [PubMed] [Google Scholar]
- 17. Krych AJ, Johnson NR, Mohan R, et al. Arthritis progression on serial MRIs following diagnosis of medial meniscal posterior horn root tear. J Knee Surg. 2018;31(7):698-704. [DOI] [PubMed] [Google Scholar]
- 18. LaPrade CM, Foad A, Smith SD, et al. Biomechanical consequences of a nonanatomic posterior medial meniscal root repair. Am J Sports Med. 2015;43(4):912-920. [DOI] [PubMed] [Google Scholar]
- 19. LaPrade RF, Matheny LM, Moulton SG, James EW, Dean CS. Posterior meniscal root repairs: outcomes of an anatomic transtibial pull-out technique. Am J Sports Med. 2017;45(4):884-891. [DOI] [PubMed] [Google Scholar]
- 20. Marsh CA, Martin DE, Harner CD, Tashman S. Effect of posterior horn medial meniscus root tear on in vivo knee kinematics. Orthop J Sports Med. 2014;2(7):2325967114541220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Martin KA, Rejeski WJ, Miller ME, James MK, Ettinger WH, Jr, Messier SP. Validation of the PASE in older adults with knee pain and physical disability. Med Sci Sports Exerc. 1999;31(5):627-633. [DOI] [PubMed] [Google Scholar]
- 22. Padalecki JR, Jansson KS, Smith SD, et al. Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: in situ pull-out repair restores derangement of joint mechanics. Am J Sports Med. 2014;42(3):699-707. [DOI] [PubMed] [Google Scholar]
- 23. Roemer FW, Guermazi A, Collins JE, et al. Semi-quantitative MRI biomarkers of knee osteoarthritis progression in the FNIH biomarkers consortium cohort - methodologic aspects and definition of change. BMC Musculoskelet Disord. 2016;17(1):466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46(2):153-162. [DOI] [PubMed] [Google Scholar]