Abstract
Static stretching can increase the range of motion of a joint. Muscle-tendon unit stiffness (MTS) is potentially one of the main factors that influences the change in the range of motion after static stretching. However, to date, the effects of acute and long-term static stretching on MTS are not well understood. The purpose of this meta-analysis was to investigate the effects of acute and long-term static stretching training on MTS, in young healthy participants. PubMed, Web of Science, and EBSCO published before January 6, 2023, were searched and finally, 17 papers were included in the meta-analysis. Main meta-analysis was performed with a random-effect model and subgroup analyses, which included comparisons of sex (male vs. mixed sex and female) and muscle (hamstrings vs. plantar flexors) were also performed. Furthermore, a meta-regression was conducted to examine the effect of total stretching duration on MTS. For acute static stretching, the result of the meta-analysis showed a moderate decrease in MTS (effect size = -0.772, Z = -2.374, 95% confidence interval = -1.409 - -0.325, p = 0.018, I2 = 79.098). For long-term static stretching, there is no significant change in MTS (effect size = -0.608, Z = -1.761, 95% CI = -1.284 – 0.069, p = 0.078, I2 = 83.061). Subgroup analyses revealed no significant differences between sex (long-term, p = 0.209) or muscle (acute, p =0.295; long-term, p = 0.427). Moreover, there was a significant relationship between total stretching duration and MTS in acute static stretching (p = 0.011, R2 = 0.28), but not in long-term stretching (p = 0.085, R2 < 0.01). Whilst MTS decreased after acute static stretching, only a tendency of a decrease was seen after long-term stretching.
Key points.
The meta-analysis revealed that acute static stretching training can decrease muscle-tendon unit stiffness in young healthy participants.
Long-term static stretching did not change muscle-tendon unit stiffness.
There was a significant relationship between total stretching duration and muscle-tendon unit stiffness in acute static stretching, but not in long-term stretching.
Key words: Stiffness, torque-angle curve, passive movement, hamstrings, plantar flexors
Introduction
Static stretching is widely used by athletes, and for health promotion for various people with the goal of increasing the range of motion (ROM) (Small et al., 2008; Costa and Vieira, 2008; Behm et al., 2016; 2021). Change in ROM is attributed to changes in mainly the passive properties of the muscle-tendon unit and stretching tolerance (Magnusson, 1998; Freitas et al., 2018; Takeuchi and Nakamura, 2020a; Takeuchi et al., 2021b; 2021c). Muscle-tendon unit stiffness (MTS) is used to assess the changes in the elastic property of the muscle-tendon unit after static stretching (Magnusson et al., 1996a; 1996b; Mizuno et al., 2013; Freitas et al., 2018; Takeuchi and Nakamura, 2020a; Fukaya et al., 2021; Takeuchi et al., 2021c; 2022b). MTS is calculated from a slope of the torque-angle curve during passive joint movement (Magnusson et al., 1996c; Nordez et al., 2006; Andrade et al., 2020) and there is a significant relationship between changes in ROM and MTS after static stretching (Guissard and Duchateau, 2004).
For long-term stretching, Freitas et al. (2018) conducted a meta-analysis examining the effects of long-term stretching training including all types of stretching (static, dynamic, and proprioceptive neuromuscular facilitation stretching) regardless of the health status of the participants (young adults, old adults, and patients with osteoarthritis), and found that stretching for 8 weeks or less did not change MTS. However, a recent meta-analysis reported that long-term static stretching for an average of 5.8 weeks significantly decreased muscle stiffness of healthy young participants which was assessed by using ultrasonography (Takeuchi et al., 2023). MTS reflects the extensibility of all components of the muscle-tendon unit and is influenced by several factors, including muscles (Nakamura et al., 2013; Ichihashi et al., 2016; Konrad et al, 2017), tendons (Kubo et al., 2002a; b), nerves (Blazevich et al., 2014; Andrade et al., 2020), and connective tissue (Nakamura et al., 2011). On the other hand, muscle stiffness is evaluated using ultrasonography equipment and is a measure that reflects muscle extensibility (Takeuchi et al., 2023). It is not clear whether the differences in the results of these meta-analyses (Freitas et al., 2018; Takeuchi et al., 2023) are due to differences in outcomes (MTS and muscle stiffness), differences in stretching types (static stretching alone and all types of stretching), or characteristics of participants (age and health status). Therefore, the effect of long-term static stretching on MTS in healthy young participants needs to be examined.
Numerous studies have reported a significant decrease in MTS after acute static stretching (Mizuno et al., 2013; Hatano et al., 2019; Takeuchi and Nakamura, 2020a; Takeuchi et al., 2021c). However, no meta-analysis of the acute effect of static stretching on MTS has been conducted, and there is a need to summarize all the available evidence. Therefore, the purpose of this study was to systemically review the papers and analyze the acute and long-term effects of static stretching on MTS in healthy young participants including some potential moderating variables (sex, muscle, and total stretching duration).
Methods
This review was conducted according to PRISMA guidelines for a systematic review with meta-analysis (Moher et al., 2009).
Search strategy
The electronic literature was searched in PubMed, Web of Science, and EBSCO. The search was conducted on January 6, 2023, and papers published before that date were included in this study. The search code for all three databases was ((Flexib*) OR (Stiff*) OR (Extensib*) OR (Passive tension)) AND (Stretch*) AND ((Muscle) OR (Tendon)) AND ((intervention) OR (effects)).
Study selection
All procedures for this study selection were performed by four independent reviewers (KT, MS, TF, and TM). First, the titles and abstracts of all papers were reviewed to assess suitability. Those not consistent with the purpose of the study were excluded with reference to the inclusion and exclusion criteria. Following the initial screening process, the full texts were assessed. This process was done by two researchers, with any disagreements resolved by the remaining researcher.
Inclusion and exclusion criteria
This study included peer-reviewed original studies reported in English. The studies were included when they were either randomized or non-randomized trials with static stretching interventions in healthy young (<40 years) human participants. We excluded studies that investigated combined interventions (e.g., static stretching with resistance training), lacked a control group, or had another treatment as a control group (e.g., dynamic stretching). Moreover, we excluded review papers, case reports, special communications, letters to the editor, invited commentaries, conference papers, or theses.
Extraction of the data
The following data were extracted from the included papers: (1) the characteristics of the paper (authors, years of publication, and sample size); (2) characteristics of participants (sex and age); (3) characteristics of stretching (targeted muscle, duration, frequency, and intensity), and (4) calculation method of MTU stiffness. For MTU stiffness, mean and standard deviation values before and after interventions were extracted. If MTU stiffness was measured more than once in different time series, the MTU stiffness after the last intervention was adopted. When the required data was not described in the included papers, the authors of the papers were contacted via e-mail or similar channels (e.g., ResearchGate) to provide information.
Statistics and data synthesis
The statistical analysis was performed according to previous studies (Konrad et al., 2021a; 2022). The meta-analysis was performed using Comprehensive Meta-Analysis software (Biostat Inc, Englewood, NJ, USA), based on the recommendation of Borenstein et al. (2009). By applying a random-effect meta-analysis, the effect size in terms of the standardized mean difference was assessed. If more than one effect size was reported in one study, the mean of all measurements within one study was used for the meta-analysis and defined as combined (Borenstein et al., 2009; Konrad et al., 2022). Although there is no general rule (Borenstein et al., 2009), subgroup analyses were performed when there were ≥ 3 studies included in each subgroup (Konrad et al., 2022). Consequently, subgroup analysis for sex (male vs. mixed sex and female) of long-term static stretching and muscle (hamstrings vs. plantar flexors) of both acute and long-term static stretching were conducted. Q-statistics were applied to determine differences between the effect sizes of the subgroups (Borenstein et al., 2009). In addition, a meta-regression was conducted to examine the association between changes in MTU stiffness and total stretching duration. The effects of a standardized mean difference of < 0.2 were considered trivial, 0.2-0.6 were considered small, 0.6-1.2 were considered moderate, 1.2-2.0 were considered large, 2.0-4.0 were considered very large, and >4.0 were considered extremely large (Hopkins et al., 2009). I2 statistics were calculated to assess the heterogeneity among the included studies, and thresholds of 25%, 50%, and 75% were defined as having a low, moderate, and high level of heterogeneity, respectively (Higgins et al., 2003; Behm et al., 2021; Konrad et al., 2021b; 2022). An alpha level of 0.05 was defined for the statistical significance of all the tests.
Risk of bias assessment and methodological quality
The methodological qualities of included papers were assessed by using the Physiotherapy Evidence Database (PEDro) scale. The PEDro scale consists of 11 methodological criteria, and two independent assessors scored each item with a 0 or 1 point. Higher scores on the PEDro scale indicated a better methodological quality of a study. When there were differences in scores between assessors, the mismatched scores were resolved between the assessors. Moreover, statistics of Egger’s regression intercept test and visual inspection of the funnel plot were applied to detect possible publication bias.
Results
Results of the Search
In total, 7708 papers were identified from a database search (Figure 1). After the removal of any duplicates, 4541 papers were screened, and 23 papers were identified as eligible for this systematic review and meta-analysis. However, 6 papers were excluded because we did not obtain the MTU stiffness data from authors of these papers (Halbertsmaet al., 1996; Magnusson et al., 1996b; Reid and McNair, 2004; Herda et al., 2009; 2010; Blazevich et al., 2014). Overall, 26 effect sizes of 17 papers were included in this systematic review and meta-analysis (14 effect sizes of 7 papers for acute effects, and 12 effect sizes of 10 papers for long-term effects) (Table 1) (Kubo et al., 2002a; Guissard and Duchateau, 2004; LaRoche and Connolly, 2006; Gajdosik et al., 2007; Ryan et al., 2008; Marshall et al., 2011; Konrad and Tilp, 2014a; Akagi and Takahashi, 2014; Rodrigues et al., 2017; Konrad et al., 2017; 2019; Palmer et al., 2019; Brusco et al., 2019; Nakao et al., 2021; Oba et al., 2021b; Longo et al., 2021; Hatano et al., 2022). On average, the included papers had a total stretching duration of 248.6 seconds (acute static stretching, range: 120-480 seconds) and 8856.0 seconds (long-term static stretching, range: 3600-27000 seconds) and an intervention term of 5.6 weeks (long-term static stretching, range: 2.9-12 weeks).
Figure 1.
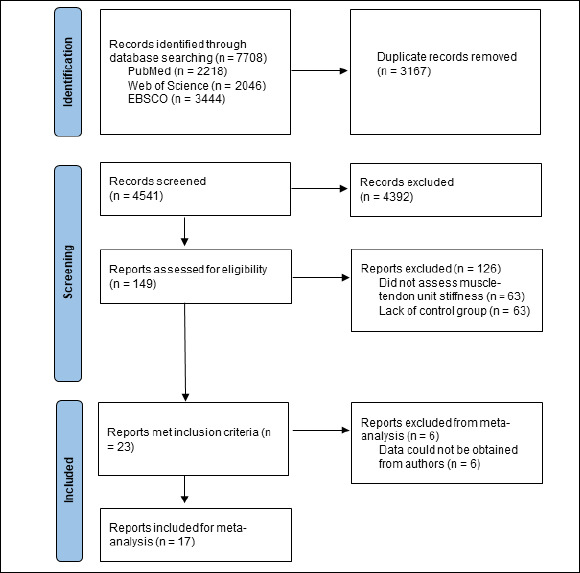
PRISMA flowchart.
Table 1.
Characteristics of the included studies.
| Study | Participants | Intervention | Calculated method of MTS from torque-angle curve | |||
|---|---|---|---|---|---|---|
| Muscle | Term | Total stretching duration | Stretching intensity | |||
| Konrad et al. (2017) | 79 men (23.3 ± 2.5 years) and 43 women (23.4 ± 3.7 years); IG: n = 23, CG: n = 21 | PF | Acute | 120 sec (30 sec * 4 sets) | ROM maximum | Between 0 and 100%ROM |
| Konrad et al. (2019) | 7 men (27.5 ± 8.3 years) and 7 women (24.9 ± 3.1 years) | PF | Acute | 300 sec (60 sec * 5 sets) | Until a maximum tolerable stretch | Between last 10 deg of ROM maximum |
| Oba et al. (2021) | 14 men (22.9 ± 1.0 years) | PF | Acute | 300 sec (60 sec * 5 sets) | (a) 100%, (b) 75%, and (c) 50% of the maximal passive resistive torque | Between 15-25 deg of ankle DF |
| Ryan et al. (2008) | 7 men (24±4 years) and 5 women (21 ± 1 years) | PF | Acute | 480 sec (30 sec * 16 sets) | Point of discomfort | At (a) 1, (b) 5, (c) 9, and (d) 13 deg of ankle DF (fourth-order polynomial regression) |
| Hatano et al. (2022) | 8 men (21.3 ± 0.7 years) and 8 women (20.9 ± 0.8 years) | Ham | Acute | 300 sec (300 sec * 1 set) | 100%ROM, 110%ROM, 120%ROM |
Between 50 and 100%ROM |
| Palmer et al. (2019) | 13 women (21 ± 2 years) | Ham | Acute | 120 sec (30 sec * 4 sets) | Point of discomfort | Between 90 and 100%ROM (fourth-order polynomial regression) |
| Rodrigues et al. (2017) | 12 men (22.2 ± 0.5 years) | Ham | Acute | 30 sec * 4 sets | 90%ROM | Between last third of ROM maximum |
| Akagi et al. (2014) | 19 men (23.7 ± 2.3 years) | PF | Long-term | 10800 sec (360 sec * 6 times/week * 5 weeks) | 3 deg lower than the ROM | Between 15 and 25 deg of ankle DF |
| Longo et al. (2021) | 18 men and 12 women (22.7 ± 1.8 years); IG: n = 15 (22.3 ± 0.8 years), CG: n = 15 (23.4±0.8 years) |
PF | Long-term | 27000 sec (450 sec * 5 times/week * 12 weeks) | Maximally tolerable stretch within the pain limit | At 20 deg of ankle DF (best polynomial regression) |
| Konrad et al. (2014) | 35 men (23.9 ± 2.9 years) and 14 women (22.5 ± 2.5 years); IG: n = 19, CG: n = 15 | PF | Long-term | 3600 sec (120 sec * 5 times/week * 6 weeks) | Point of discomfort | Between 0 and 100%ROM |
| LaRoche et al. (2006) | 29 men (31.6 ± 15.2 years) | Ham | Long-term | 3600 sec (300 sec * 3 times/week * 4 weeks) | Point of mild discomfort | Between 50 and 85 deg of knee extension |
| Gajdosik et al. (2007) | 10 women; IG: n = 6 (23 ± 4 years), CG: n = 4 (21 ± 1 years) | PF | Long-term | 4500 sec (150 sec * 5 times/week * 6 weeks) | Not reported | Between (a) 0 and 100%ROM and (b) last 10 deg of ankle DF (third order polynomial regression) |
| Brusco et al. (2019) | 13 men (23.6 ± 3.9 years) | Ham | Long-term | 5760 sec (480 sec * 2 times/week * 6 weeks) | Maximum tolerable stretch amplitude irrespective of the timing or magnitude of pain onset | Between last third angles relative to (a) the ROM maximum reached before and after training and (b) the same angle reached before training |
| Marshall et al. (2011) | 14 men and 8 women (22.7 ±3.8 years) | Ham | Long-term | 7200 sec (360 sec * 5 times/week * 4 weeks) | Not reported | Between 20-50 deg of knee extension |
| Kudo et al. (2002) | 8 men (24.6 ± 1.8 years) | PF | Long-term | 4500 sec (225 sec * 7 times/week * 2.9 weeks) | 35 deg of ankle dorsiflexion | Between15 and 25 deg of ankle DF |
| Guissard et al. (2004) | 8 men and 4 women (21-35 years) | PF | Long-term | 18000 sec (600 sec * 5 times/week * 6 weeks) | Maximum dorsiflexion tolerated by the participants | Between 15 and 25 deg of ankle DF |
| Nakao et al. (2021) | 30 men (22.7 ± 2.2 years); IG: n = 15 (22.5 ± 2.9 years), CG: ne = 15 (22.9 ± 1.2 years) | Ham | Long-term | 3600 sec (300 sec * 3 times/week * 4 weeks) | Point just before pain | Between 50 and 100%ROM |
IG, Intervention group; CG, Control group; Ham, hamstrings; PF, plantar flexors; ROM; range of motion; DF, dorsiflexion; deg, degree; MTS, muscle-tendon unit stiffness.
Risk of Bias Assessment and Methodological Quality
Figure 2 shows a funnel plot of the 17 papers included in the meta-analysis. A visual inspection of the funnel plot and Egger’s regression intercept test indicated a significant reporting bias for acute (intercept = -9.52, p = 0.018) and long-term stretching (intercept = -5.65, p = 0.018). To assess the methodological quality of each paper, the PEDro scale was used (Table 2). The agreement of the PEDro scale between assessors was 95.7% (179 of 187 points). The average and standard deviations of the PEDro scale was 5.83 ± 0.71 (range between 5 and 8 points), which indicated a low risk of bias (Maher et al., 2003; Moran et al., 2021; Konrad et al., 2022).
Figure 2.
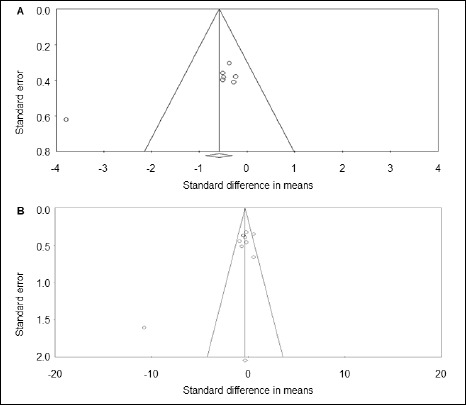
Funnel plot analysis for acute (A) and long-term (B) stretching.
Table 2.
PEDro scale.
| Study | Random allocation | Concealed allocation | Groups similar at baseline | Assessor blinding | Subject blinding | Therapist blinding | Less than 15% dropouts | Intention-to-treat analysis | Between-group statistical comparisons | Point estimates and variability | Eligibility criteria specified * | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Akagi (2014) | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 6 |
| Longo (2021) | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 6 |
| Konrad (2014) | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Konrad (2017) | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 5 |
| Konrad (2019) | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 6 |
| LaRoche (2006) | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 6 |
| Gajdosik (2007) | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 6 |
| Brusco (2019) | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 5 |
| Marshall (2011) | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 6 |
| Oba (2021) | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 6 |
| Kudo (2002) | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 6 |
| Ryan (2008) | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 6 |
| Guissard (2004) | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 5 |
| Nakao (2021) | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 5 |
| Hatano (2022) | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 6 |
| Palmer (2019) | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 6 |
| Rodrigues (2017) | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 5 |
PEDro, Physiotherapy evidence database; 1, one point scored; 0, no points scored;
* Criteria of random allocation was not counted for the total score.
Acute effect on MTS
Acute static stretching training had a significant moderate effect on MTS (effect size = -0.772, Z = -2.374, 95% confidence interval (CI) = -1.409 - -0.325, p = 0.018) (Figure 3); however, high heterogeneity was observed (I2 = 79.098). Subgroup analysis revealed that there was no significant difference between the muscles (plantar flexors vs. hamstrings) (p = 0.295) (Table 3). The meta-regressions revealed that total stretching duration was associated with the magnitude of the effect size for MTS (p = 0.011, coefficient = -0.0061 95% CI = -0.0109-0.0014, R2 = 0.28) (Figure 4).
Figure 3.
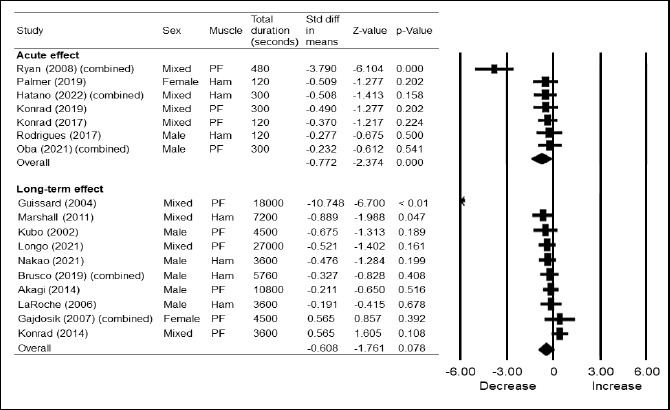
Funnel plot analysis for acute (A) and long-term (B) stretching.
Table 3.
Results of subgroup analysis.
| Subgroup | Subgroup | Number of studies | Std diff in means (95%CI) | Z-Value | p-Value | Q statistics |
|---|---|---|---|---|---|---|
| Acute | Hamstrings | 3 | -0.440 (-0.878-0.001) | -1.964 | 0.050 | |
| Plantar flexors | 4 | -1.118 (-2.311 - -0.074) | -1.838 | 0.066 | ||
| Overall | 7 | -0.520 (-0.932 - -0.109) | -2.478 | 0.013 * | (Q = 1.096, df (Q) = 1, p = 0.295) | |
| Long-term | Hamstrings | 4 | -0.466 (-0.871 - -0.061) | -2.255 | ||
| Plantar flexors | 6 | -0.986 (-2.206 - -0.234) | -1.585 | |||
| Overall | 10 | -0.518 (-0.902 - -0.133) | -2.639 | (Q = 0.630, df (Q) = 1, p = 0.427) | ||
| Male | 5 | -0.348 (-0.696 - -0.000) | -1.958 | 0.050 | ||
| Mixed and female | 5 | -1.412 (-3.034-0.210) | -1.706 | 0.088 | ||
| Overall | 10 | -0.395 (-0.736 - -0.054) | -2.273 | 0.000 * | (Q = 1.579, df (Q) = 1, p = 0.209) |
Std diff in means, standardized difference in means; 95% CI. 95% confidence interval; mixed, male and female;
* Significant difference within a group.
Figure 4.
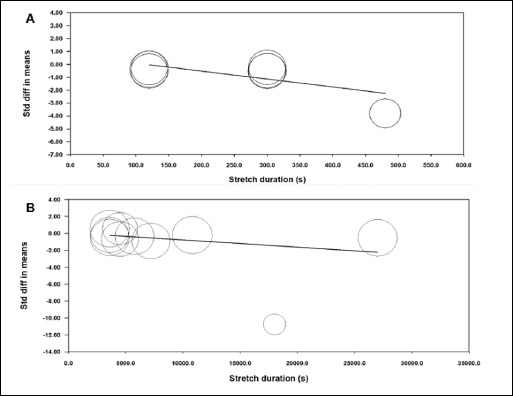
Funnel plot analysis for acute (A) and long-term (B) stretching.
Long-term effect on MTS
Meta-analysis revealed that long-term static stretching training had no significant effect on MTS (effect size = -0.608, Z = -1.761, 95% CI = -1.284-0.069, p = 0.078, I2 = 83.061). Subgroup analysis revealed that there were no significant differences in muscle (plantar flexors vs. hamstrings) (p = 0.427) or sex (mixed sex and female vs. male) (p = 0.209) (Table 3). The meta-regressions revealed that total stretching duration was not associated with the magnitude of the effect size for MTS (p = 0.085, coefficient = -0.0001 95% CI = -0.0002 – 0.0000, R2 < 0.01) (Figure 4).
Discussion
To the best of our knowledge, this is the first meta-analysis examining the acute, as well as the long-term, effects of static stretching on MTS. The results of this study showed that acute static stretching significantly decreased MTS with a moderate effect size (effect size = -0.772, p < 0.01). The subgroup analysis indicated no significant differences between the hamstrings and plantar flexors (p = 0.295). In addition, there was a significant association between the total stretching duration and the magnitude of the effect size for MTS (p = 0.011), indicating that a longer stretch duration can decrease the MTS to a higher extent. Previous studies have shown that static stretching duration is associated with an acute decrease in the MTS of the plantar flexors (Ryan et al., 2008; 2009) and hamstrings (Matsuo et al., 2013; Nakamura et al., 2019; Takeuchi et al., 2021b; 2022a). Ryan et al. (2009) reported that the MTS of the plantar flexors decreased with the onset of acute static stretching and significant decreases occurred with stretching for longer than 90 seconds. In addition, more than 180 seconds of static stretching effectively decreases the MTS of the hamstrings (Matsuo et al., 2013; Nakamura et al., 2019; Takeuchi et al., 2022a). In the present study, the average stretching duration of acute static stretching was 248.6 seconds and this stretching duration was considered sufficient to decrease the MTS of the plantar flexors and hamstrings. Moreover, a previous study showed that the acute effects of static stretching interventions on the MTS of the hamstrings are influenced by the stretching load (Takeuchi et al., 2021b). Stretching load is calculated from the duration and intensity (torque) of stretching (Takeuchi et al., 2021b), and longer-duration or higher-intensity stretching demonstrates a greater stretching load. Thus, the duration of static stretching is associated with acute MTS decrement, which supports the results of the meta-regression of this study. Therefore, it was indicated that static stretching for an average of approximately 240 seconds (4 minutes) decreased the MTS of the plantar flexors and hamstrings.
We were unable to get the data from three papers on acute static stretching (Halbertsma et al., 1996; Herda et al., 2009; 2010). Regarding papers for which data have not been obtained, Herda et al. (1200 seconds of acute stretching) (Herda et al., 2009; 2010) reported a significant decrease in the MTS of the plantar flexors, although Halbertsma et al. (1996) (600 seconds of acute stretching) found a non-significant change in the MTS of the hamstrings (p = 0.372). Thus, 9 out of the 10 papers that met the inclusion criteria of this study showed a decrease in MTS (Ryan et al., 2008; Herda et al., 2009, 2010; Rodrigues et al., 2017; Konrad et al., 2017; 2019; Palmer et al., 2019; Oba et al., 2021b; Hatano et al., 2022), and 1 paper showed no change (Halbertsma et al., 1996). Therefore, the presence of missing data may not significantly affect the results of the main meta-analysis of acute static stretching.
For long-term static stretching, the results of the meta-analysis showed a non-significant moderate effect size (effect size = -0.608, p = 0.078). The average total stretching duration, intervention term, and weekly dose were 147.6 minutes (range between 60 – 450 minutes), 5.6 weeks (range between 2.9-12 weeks), and 26.4 minutes/week (range between 10-50 minutes/week), respectively. Freitas et al. (2018) conducted a meta-analysis of the effects of long-term stretching including all stretching types (static, dynamic, and proprioceptive neuromuscular facilitation stretching), regardless of the health condition of the participants, on MTS and reported a non-significant trivial effect of stretching for 8 weeks or less (effect size = -0.30, p = 0.345). Randomized controlled trials of long-term dynamic stretching (LaRoche and Connolly, 2006; Konrad and Tilp, 2014b) and proprioceptive neuromuscular facilitation stretching (Konrad et al., 2015) did not show significant changes in the MTS of the plantar flexors. Furthermore, a significant increase has been reported in the MTS of people with osteoarthritis of the knee joint after 6 weeks of static stretching (Reid and McNair, 2011). Therefore, it was suggested that the difference in the magnitude of effect size between the present study (magnitude of moderate) and the previous study (magnitude of trivial) (Freitas et al., 2018) is due to the inclusion criteria that Freitas et al. included all stretching types regardless of the health condition of the participants, while the present study included only static stretching of healthy participants.
There are three potential explanations as to why there was no significant change in MTS after the average of 5.6 weeks of static stretching. Firstly, the intervention term may have been insufficient to change the mechanical properties of the muscle-tendon unit. Three studies examined the change in the mechanical properties of the muscle after more than 12 weeks of static stretching (Andrade et al., 2020; Longo et al., 2021; Moltubakk et al., 2021), and all studies found significant changes in the mechanical properties. Andrade et al. (Andrade et al., 2016) and Longo et al. (Longo et al., 2021) reported a significant decrease in the muscle stiffness and MTS of the plantar flexors after 12 weeks of static stretching. Moltubakk et al. (2021) examined the effects of 24 weeks of static stretching and found a significant decrease in the passive torque at a given angle in the plantar flexors, which reflects the extensibility of the muscle-tendon unit. Consequently, the effect of static stretching for a longer term (≧ 12 weeks) can likely reduce MTS, however, it needs to be further examined. Secondly, MTS is affected by various tissues, such as nerves (Andrade et al., 2016; 2018; 2020), tendons (Kubo et al., 2001; 2002b; Mahieu et al., 2009), and connective tissue (Gajdosik and Williams, 2002; Morse et al., 2008; Sato et al., 2020). A recent meta-analysis examining the effects of long-term static stretching (average of 5.8 weeks, range between 3-12 weeks) showed a significant decrease in the muscle stiffness of the plantar flexors and hamstrings with a moderate effect size (effect size = -0.749, p < 0.01) (Takeuchi et al., 2023). Furthermore, previous studies reported that tendon stiffness was not changed after 3-6 weeks of static stretching (Kubo et al., 2002a; Mahieu et al., 2007; Konrad and Tilp, 2014a; Blazevich et al., 2014). Thirdly, the MTS calculation method may be involved. MTS is calculated from the slope of the linear region of the torque-angle curve during passive joint movement (Magnusson et al., 1996a; b). Because deflection of the Achilles tendon, called slack, is related to stiffness at a position close to plantar flexion of the ankle joint (Hug et al., 2013; Hirata et al., 2016), many studies on the ankle joint have calculated MTS from the slope of the torque-angle curve in the ankle dorsiflexed position (Kubo et al., 2002a; Guissard and Duchateau, 2004; Akagi and Takahashi, 2014; Longo et al., 2021). However, the two studies with positive effect sizes in this study (both, effect size = 0.565) calculated MTS in the range of 0-100% ROM of ankle joint (Gajdosik et al., 2007; Konrad and Tilp, 2014a), suggesting that differences in the calculation method of MTS may have influenced the results.
We were unable to obtain the data from three studies on long-term static stretching (Magnusson et al., 1996b; Reid and McNair, 2004; Blazevich et al., 2014). Those studies show different results. Blazevich et al. (2014) (4 weeks, total stretching duration of 5400 seconds) reported a significant decrease in the MTS of the plantar flexors. Reid and McNair (2004) (6 weeks, total stretching duration of 2700 seconds) reported a significant increase in the MTS of the hamstrings. Moreover, Magnusson et al. (1996b) (3 weeks, total stretching duration of 9000 seconds) reported a non-significant change in the MTS of the hamstrings. Thus, even if these studies were added to the meta-analysis of the present study, the result that MTS is not changed by long-term static stretching would not change.
In the present study, the results revealed a significant publication bias (acute, intercept = -9.52, p = 0.018; long-term, intercept = -5.65, p = 0.018) and high heterogeneity (acute, I2 = 79.098; long-term, I2 = 83.061). The effect sizes of Ryan et al. (2008) (effect size = -3.790) and Guissard and Duchateau (2004) (effect size = -10.748) were very large and led to a potential risk of publication bias and heterogeneity. Even when we excluded these studies, the overall results of the meta-analysis were similar but the effect sizes became lower (acute static stretching, effect size = -0.398, Z = -2.656, 95% CI = -0.692 - -0.104, p =0.008; long-term static stretching, effect size = -0.253, Z = -1.595, 95% CI = -0.563 - -0.058104, p =0.008), although there was no significant publication bias (acute, intercept = 0.017, p = 0.991; long-term, intercept = -0.205, p = 0.928) or heterogeneity (acute, I2 = 0.000; long-term, I2 = 24.409).
There were some limitations in the present study. First, only two moderating variables were considered for the subgroup analysis. Therefore, the effects of potential variables for decreasing MTS, such as stretching intensity (Takeuchi and Nakamura, 2020b; Nakamura et al., 2021a; 2021b; Takeuchi et al., 2021a; 2021b; 2021c; 2021d; Fukaya et al., 2022), stretching load (Takeuchi et al., 2021b; 2022a), frequency (Nakamura et al., 2020), rest interval (Nojiri et al., 2021; Oba et al., 2021a), and MTS calculation method (Nordez et al., 2006) were obscured. Second, the papers that met the inclusion criteria for this meta-analysis were hamstrings and plantar flexors. For the shoulder joint, the MTS measurement method was reported (Wight et al., 2018), but the effect of static stretching on the MTS of the shoulder joint was not examined. For other joints, no method of measuring MTS has been shown. However, it has been shown that the muscle stiffness of the rectus femoris (Nakamura et al., 2021a; Takeuchi et al., 2021d), iliopsoas (Nojiri et al., 2021), teres minor (Yamauchi et al., 2016), and infraspinatus (Yamauchi et al., 2016) are decreased by static stretching. When studies are pooled, the different effects of static stretching on different muscles need to be further examined. Third, the meta-analysis was conducted with young participants with an average age in their 20s. Thus, future studies should also investigate younger and older populations. Finally, the results of the subgroup analysis revealed that there was no significant difference between the muscles (plantar flexors vs. hamstrings) or sex (mixed sex and female vs. male). However, no studies have directly examined the effects of sex or muscle on change in the MTS after static stretching interventions.
Conclusion
The results of the main meta-analysis showed that MTS significantly decreased after acute static stretching with a moderate effect size, but there was no significant change in MTS after long-term static stretching. Subgroup analysis showed no significant difference between muscle or sex. Furthermore, there was a significant relationship between total stretching duration and MTS in acute static stretching, but not in long-term stretching.
Acknowledgements
This work was supported by JSPS KAKENHI with Grant number 22K11595. There is no conflict of interest. The present study complies with the current laws of the country in which it was performed. The datasets generated and analyzed during the current study are not publicly available but are available from the corresponding author, who was an organizer of the study.
Biographies

Kosuke TAKEUCHI
Employment
Lecture, Department of Physical Therapy, Faculty of Rehabilitation, Kobe International University, Hyogo, Japan
Degree
PhD
Research interests
Sports science, stretching, sports medicine
E-mail: ktakeuchi@kobe-kiu.ac.jp

Masatoshi NAKAMURA
Employment
Associate professor, Faculty of Rehabilitation Sciences, Nishi Kyushu University, Saga, Japan
Degree
PhD
Research interests
Physical therapy, stretching, exercise physiology, flexibility
E-mail: nakamuramas@nisikyu-u.ac.jp

Taizan FUKAYA
Employment
Assistant professor, Department of Physical Therapy, Faculty of Social Work Studies, Josai International University, Togane, Japan
Degree
Ph.D. in health science
Research interests
Exercise physiology and evaluation for physical performance
E-mail: tfukaya@jiu.ac.jp

Andreas KONRAD
Employment
Institute of Human Movement Science, Sport and Health, Graz University
Degree
PhD, MSc
Research interests
Biomechanics, muscle performance, training science, muscle-tendon-unit, soccer science
E-mail: andreas.konrad@uni-graz.at

Takamasa MIZUNO
Employment
Associate Professor, Research Center of Health, Physical Fitness and Sports, Nagoya University, Aichi, Japan
Degree
PhD
Research interests
Stretching, Strength training, flexibility
E-mail: mizuno@htc.nagoya-u.ac.jp
References
- Akagi R., Takahashi H. (2014) Effect of a 5-week static stretching program on hardness of the gastrocnemius muscle. Scandinavian Journal of Medicine & Science in Sports 24, 950-957. https://doi.org/10.1111/sms.12111 10.1111/sms.12111 [DOI] [PubMed] [Google Scholar]
- Andrade R.J., Freitas S.R., Hug F., Le Sant G., Lacourpaille L., Gross R., McNair P., Nordez A. (2018) The potential role of sciatic nerve stiffness in the limitation of maximal ankle range of motion. Scientific reports 8. https://doi.org/10.1038/s41598-018-32873-6 10.1038/s41598-018-32873-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrade R.J., Freitas S.R., Hug F., Le Sant G., Lacourpaille L., Gross R., Quillard J.B., McNair P.J., Nordez A. (2020) Chronic effects of muscle and nerve-directed stretching on tissue mechanics. Journal of Applied Physiology (Bethesda, Md. : 1985) 129, 1011-1023. https://doi.org/10.1152/japplphysiol.00239.2019 10.1152/japplphysiol.00239.2019 [DOI] [PubMed] [Google Scholar]
- Andrade R.J., Nordez A., Hug F., Ates F., Coppieters M.W., Pezarat-Correia P., Freitas S.R. (2016) Non-invasive assessment of sciatic nerve stiffness during human ankle motion using ultrasound shear wave elastography. Journal of Biomechanics 49, 326-331. https://doi.org/10.1016/j.jbiomech.2015.12.017 10.1016/j.jbiomech.2015.12.017 [DOI] [PubMed] [Google Scholar]
- Behm D.G., Alizadeh S., Anvar S.H., Drury B., Granacher U., Moran J. (2021) Non-local Acute Passive Stretching Effects on Range of Motion in Healthy Adults: A Systematic Review with Meta-analysis. Sports Medicine (Auckland, N.Z.) 51, 945-959. https://doi.org/10.1007/s40279-020-01422-5 10.1007/s40279-020-01422-5 [DOI] [PubMed] [Google Scholar]
- Behm D.G., Blazevich A.J., Kay A.D., McHugh M. (2016) Acute effects of muscle stretching on physical performance, range of motion, and injury incidence in healthy active individuals: A systematic review. Applied Physiology, Nutrition and Metabolism 41, 1-11. https://doi.org/10.1139/apnm-2015-0235 10.1139/apnm-2015-0235 [DOI] [PubMed] [Google Scholar]
- Blazevich A.J., Cannavan D., Waugh C.M., Miller S.C., Thorlund J.B., Aagaard P., Kay A.D. (2014) Range of motion, neuromechanical, and architectural adaptations to plantar flexor stretch training in humans. Journal of Applied Physiology (Bethesda, Md. : 1985) 117, 452-462. https://doi.org/10.1152/japplphysiol.00204.2014 10.1152/japplphysiol.00204.2014 [DOI] [PubMed] [Google Scholar]
- Borenstein M., Hedges L. V., Higgins J.P.T., Rothstein H.R. (2009) Introduction to Meta-Analysis. NewYork: John Wiley & Sons, Ltd. https://doi.org/10.1002/9780470743386 10.1002/9780470743386 [DOI] [Google Scholar]
- Brusco C.M., Blazevich A.J., Pinto R.S. (2019) The effects of 6 weeks of constant-angle muscle stretching training on flexibility and muscle function in men with limited hamstrings’ flexibility. European Journal of Applied Physiology 119, 1691-1700. https://doi.org/10.1007/s00421-019-04159-w 10.1007/s00421-019-04159-w [DOI] [PubMed] [Google Scholar]
- da Costa B.R., Vieira E.R. (2008) Stretching to reduce work-related musculoskeletal disorders: a systematic review. Journal of Rehabilitation Medicine 40, 321-328. https://doi.org/10.2340/16501977-0204 10.2340/16501977-0204 [DOI] [PubMed] [Google Scholar]
- Freitas S.R., Mendes B., Le Sant G., Andrade R.J.R., Nordez A., Milanovic Z. (2018) Can chronic stretching change the muscle-tendon mechanical properties? A review. Scandinavian Journal of Medicine & Science in Sports 28, 794-806. https://doi.org/10.1111/sms.12957 10.1111/sms.12957 [DOI] [PubMed] [Google Scholar]
- Fukaya T., Matsuo S., Iwata M., Yamanaka E., Tsuchida W., Asai Y., Suzuki S. (2021) Acute and chronic effects of static stretching at 100% versus 120% intensity on flexibility. European Journal of Applied Physiology 121, 513-523. https://doi.org/10.1007/s00421-020-04539-7 10.1007/s00421-020-04539-7 [DOI] [PubMed] [Google Scholar]
- Fukaya T., Sato S., Yahata K., Yoshida R., Takeuchi K., Nakamura M. (2022) Effects of stretching intensity on range of motion and muscle stiffness: A narrative review. Journal of Bodywork and Movement Therapies 32, 68-76. https://doi.org/10.1016/j.jbmt.2022.04.011 10.1016/j.jbmt.2022.04.011 [DOI] [PubMed] [Google Scholar]
- Gajdosik R.L., Allred J.D., Gabbert H.L., Sonsteng B.A. (2007) A stretching program increases the dynamic passive length and passive resistive properties of the calf muscle-tendon unit of unconditioned younger women. European Journal of Applied Physiology 99, 449-454. https://doi.org/10.1007/s00421-006-0366-7 10.1007/s00421-006-0366-7 [DOI] [PubMed] [Google Scholar]
- Gajdosik R.L., Williams A.K. (2002) Relation of maximal ankle dorsiflexion angle and passive resistive torque to passive-elastic stiffness of ankle dorsiflexion stretch. Perceptual and Motor Skills 95, 323-325. https://doi.org/10.2466/PMS.95.5.323-325 10.2466/PMS.95.5.323-325 [DOI] [PubMed] [Google Scholar]
- Guissard N., Duchateau J. (2004) Effect of static stretch training on neural and mechanical properties of the human plantar-flexor muscles. Muscle & Nerve 29, 248-255. https://doi.org/10.1002/mus.10549 10.1002/mus.10549 [DOI] [PubMed] [Google Scholar]
- Halbertsma J.P., van Bolhuis A.I., Göeken L.N. (1996) Sport stretching: effect on passive muscle stiffness of short hamstrings. Archives of Physical Medicine and Rehabilitation 77, 688-692. https://doi.org/10.1016/S0003-9993(96)90009-X 10.1016/S0003-9993(96)90009-X [DOI] [PubMed] [Google Scholar]
- Hatano G., Matsuo S., Asai Y., Suzuki S., Iwata M. (2022) Effects of High-Intensity Stretch with Moderate Pain and Maximal Intensity Stretch without Pain on Flexibility. Journal of Sports Science & Medicine 21, 171-181. https://doi.org/10.52082/jssm.2022.171 10.52082/jssm.2022.171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatano G., Suzuki S., Matsuo S., Kataura S., Yokoi K., Fukaya T., Fujiwara M, Asai Y., Iwata M. (2019) Hamstring stiffness returns more rapidly after static stretching than range of motion, stretch tolerance, and isometric peak torque. Journal of Sport Rehabilitation 28, 325-331. https://doi.org/10.1123/jsr.2017-0203 10.1123/jsr.2017-0203 [DOI] [PubMed] [Google Scholar]
- Herda T.J., Ryan E.D., Costa P.B., Walter A.A., Hoge K.M., Uribe B.P., McLagan J.R., Stout J.R., Cramer J.T. (2010) Acute effects of passive stretching and vibration on the electro-mechanical delay and musculotendinous stiffness of the plantar flexors. Electromyography and Clinical Neurophysiology 50, 277-288. [PubMed] [Google Scholar]
- Herda T.J., Ryan E.D., Smith A.E., Walter A.A., Bemben M.G., Stout J.R., Cramer J.T. (2009) Acute effects of passive stretching vs vibration on the neuromuscular function of the plantar flexors. Scandinavian Journal of Medicine & Science in Sports 19, 703-713. https://doi.org/10.1111/j.1600-0838.2008.00787.x 10.1111/j.1600-0838.2008.00787.x [DOI] [PubMed] [Google Scholar]
- Higgins J.P.T., Thompson S.G., Deeks J.J., Altman D.G. (2003) Measuring inconsistency in meta-analyses. BMJ 327, 557-560. https://doi.org/10.1136/bmj.327.7414.557 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirata K., Miyamoto-Mikami E., Kanehisa H., Miyamoto N. (2016) Muscle-specific acute changes in passive stiffness of human triceps surae after stretching. European Journal of Applied Physiology 116, 911-918. https://doi.org/10.1007/s00421-016-3349-3 10.1007/s00421-016-3349-3 [DOI] [PubMed] [Google Scholar]
- Hopkins W.G., Marshall S.W., Batterham A.M., Hanin J. (2009) Progressive statistics for studies in sports medicine and exercise science. Medicine and Science in Sports and Exercise 41, 3-12. https://doi.org/10.1249/MSS.0b013e31818cb278 10.1249/MSS.0b013e31818cb278 [DOI] [PubMed] [Google Scholar]
- Hug F., Lacourpaille L., Maïsetti O., Nordez A. (2013) Slack length of gastrocnemius medialis and Achilles tendon occurs at different ankle angles. Journal of Biomechanics 46, 2534-2538. https://doi.org/10.1016/j.jbiomech.2013.07.015 10.1016/j.jbiomech.2013.07.015 [DOI] [PubMed] [Google Scholar]
- Ichihashi N., Umegaki H., Ikezoe T., Nakamura M., Nishishita S., Fujita K., Umehara J., Nakao S., Ibuki S. (2016) The effects of a 4-week static stretching programme on the individual muscles comprising the hamstrings. Journal of Sports Sciences 34, 2155-2159. https://doi.org/10.1080/02640414.2016.1172725 10.1080/02640414.2016.1172725 [DOI] [PubMed] [Google Scholar]
- Konrad A., Gad M., Tilp M. (2015) Effect of PNF stretching training on the properties of human muscle and tendon structures. Scandinavian Journal of Medicine & Science in Sports 25, 346-355. https://doi.org/10.1111/sms.12228 10.1111/sms.12228 [DOI] [PubMed] [Google Scholar]
- Konrad A., Močnik R., Titze S., Nakamura M., Tilp M. (2021a) The Influence of Stretching the Hip Flexor Muscles on Performance Parameters. A Systematic Review with Meta-Analysis. International Journal of Environmental Research and Public Health 18, 1-20. https://doi.org/10.3390/ijerph18041936 10.3390/ijerph18041936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konrad A., Tilp M., Nakamura M. (2021b) A Comparison of the Effects of Foam Rolling and Stretching on Physical Performance. A Systematic Review and Meta-Analysis. Frontiers in Physiology 12. https://doi.org/10.3389/fphys.2021.720531 10.3389/fphys.2021.720531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konrad A., Nakamura M., Tilp M., Donti O., Behm D.G. (2022) Foam Rolling Training Effects on Range of Motion: A Systematic Review and Meta-Analysis. Sports Medicine (Auckland, N.Z.) 52, 2523-2535. https://doi.org/10.1007/s40279-022-01699-8 10.1007/s40279-022-01699-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konrad A., Reiner M.M., Thaller S., Tilp M. (2019) The time course of muscle-tendon properties and function responses of a five-minute static stretching exercise. European Journal of Sport Science 19, 1195-1203. https://doi.org/10.1080/17461391.2019.1580319 10.1080/17461391.2019.1580319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konrad A., Stafilidis S., Tilp M. (2017) Effects of acute static, ballistic, and PNF stretching exercise on the muscle and tendon tissue properties. Scandinavian Journal of Medicine & Science in Sports 27, 1070-1080. https://doi.org/10.1111/sms.12725 10.1111/sms.12725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konrad A., Tilp M. (2014a) Increased range of motion after static stretching is not due to changes in muscle and tendon structures. Clinical Biomechanics (Bristol, Avon) 29, 636-642. https://doi.org/10.1016/j.clinbiomech.2014.04.013 10.1016/j.clinbiomech.2014.04.013 [DOI] [PubMed] [Google Scholar]
- Konrad A., Tilp M. (2014b) Effects of ballistic stretching training on the properties of human muscle and tendon structures. Journal of Applied Physiology (Bethesda, Md. : 1985) 117, 29-35. https://doi.org/10.1152/japplphysiol.00195.2014 10.1152/japplphysiol.00195.2014 [DOI] [PubMed] [Google Scholar]
- Kubo K., Kanehisa H., Fukunaga T. (2002a) Effect of stretching training on the viscoelastic properties of human tendon structures in vivo. Journal of Applied Physiology (Bethesda, Md. : 1985) 92, 595-601. https://doi.org/10.1152/japplphysiol.00658.2001 10.1152/japplphysiol.00658.2001 [DOI] [PubMed] [Google Scholar]
- Kubo K., Kanehisa H., Fukunaga T. (2002b) Effects of transient muscle contractions and stretching on the tendon structures in vivo. Acta Physiologica Scandinavica 175, 157-164. https://doi.org/10.1046/j.1365-201X.2002.00976.x 10.1046/j.1365-201X.2002.00976.x [DOI] [PubMed] [Google Scholar]
- Kubo K., Kanehisa H., Kawakami Y., Fukunaga T. (2001) Influence of static stretching on viscoelastic properties of human tendon structures in vivo. Journal of Applied Physiology (Bethesda, Md. : 1985) 90, 520-527. https://doi.org/10.1152/jappl.2001.90.2.520 10.1152/jappl.2001.90.2.520 [DOI] [PubMed] [Google Scholar]
- LaRoche D.P., Connolly D.A.J. (2006) Effects of Stretching on Passive Muscle Tension and Response to Eccentric Exercise. The American Journal of Sports Medicine 34, 1000-1007. https://doi.org/10.1177/0363546505284238 10.1177/0363546505284238 [DOI] [PubMed] [Google Scholar]
- Longo S., Cè E., Bisconti A.V., Rampichini S., Doria C., Borrelli M., Limonta E., Coratella G., Esposito F. (2021) The effects of 12 weeks of static stretch training on the functional, mechanical, and architectural characteristics of the triceps surae muscle-tendon complex. European Journal of Applied Physiology 121, 1743-1758. https://doi.org/10.1007/s00421-021-04654-z 10.1007/s00421-021-04654-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magnusson S.P. (1998) Passive properties of human skeletal muscle during stretch maneuvers. A review. Scandinavian Journal of Medicine & Science in Sports 8, 65-77. https://doi.org/10.1111/j.1600-0838.1998.tb00171.x 10.1111/j.1600-0838.1998.tb00171.x [DOI] [PubMed] [Google Scholar]
- Magnusson S.P., Simonsen E.B., Aagaard P., Kjaer M. (1996a) Biomechanical responses to repeated stretches in human hamstring muscle in vivo. The American Journal of Sports Medicine 24, 622-628. https://doi.org/10.1177/036354659602400510 10.1177/036354659602400510 [DOI] [PubMed] [Google Scholar]
- Magnusson S.P., Simonsen E.B., Aagaard P., Soørensen H., Kjær M. (1996b) A mechanism for altered flexibility in human skeletal muscle. Journal of Physiology 497, 291-298. https://doi.org/10.1113/jphysiol.1996.sp021768 10.1113/jphysiol.1996.sp021768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magnusson S.P., Simonsen E.B., Dyhre-Poulsen P., Aagaard P., Mohr T., Kjaer M. (1996c) Viscoelastic stress relaxation during static stretch in human skeletal muscle in the absence of EMG activity. Scandinavian Journal Of Medicine & Science İn Sports 6, 323-328. https://doi.org/10.1111/j.1600-0838.1996.tb00101.x 10.1111/j.1600-0838.1996.tb00101.x [DOI] [PubMed] [Google Scholar]
- Maher C.G., Sherrington C., Herbert R.D., Moseley A.M., Elkins M. (2003) Reliability of the PEDro Scale for Rating Quality of Randomized Controlled Trials. Physical Therapy 83, 713-721. https://doi.org/10.1093/ptj/83.8.713 10.1093/ptj/83.8.713 [DOI] [PubMed] [Google Scholar]
- Mahieu N.N., Cools A., De Wilde B., Boon M., Witvrouw E. (2009) Effect of proprioceptive neuromuscular facilitation stretching on the plantar flexor muscle-tendon tissue properties. Scandinavian Journal Of Medicine & Science İn Sports 19, 553-560. https://doi.org/10.1111/j.1600-0838.2008.00815.x 10.1111/j.1600-0838.2008.00815.x [DOI] [PubMed] [Google Scholar]
- Mahieu N.N., McNair P., De Muynck M., Stevens V., Blanckaert I., Smits N., Witvrouw E. (2007) Effect of static and ballistic stretching on the muscle-tendon tissue properties. Medicine and Science in Sports and Exercise 39, 494-501. https://doi.org/10.1249/01.mss.0000247004.40212.f7 10.1249/01.mss.0000247004.40212.f7 [DOI] [PubMed] [Google Scholar]
- Marshall P.W.M., Cashman A., Cheema B.S. (2011) A randomized controlled trial for the effect of passive stretching on measures of hamstring extensibility, passive stiffness, strength, and stretch tolerance. Journal of Science and Medicine in Sport / Sports Medicine Australia 14, 535-540. https://doi.org/10.1016/j.jsams.2011.05.003 10.1016/j.jsams.2011.05.003 [DOI] [PubMed] [Google Scholar]
- Matsuo S., Suzuki S., Iwata M., Banno Y., Asai Y., Tsuchida W., Inoue T. (2013) Acute Effects of Different Stretching Durations on Passive Torque, Mobility, and Isometric Muscle Force. Journal of Strength and Conditioning Research 27, 3367-3376. https://doi.org/10.1519/JSC.0b013e318290c26f 10.1519/JSC.0b013e318290c26f [DOI] [PubMed] [Google Scholar]
- Mizuno T., Matsumoto M., Umemura Y. (2013) Viscoelasticity of the muscle-tendon unit is returned more rapidly than range of motion after stretching. Scandinavian Journal of Medicine & Science in Sports 23, 23-30. https://doi.org/10.1111/j.1600-0838.2011.01329.x 10.1111/j.1600-0838.2011.01329.x [DOI] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G., Altman D., Antes G., Atkins D., Barbour V., Barrowman N., Berlin J.A., Clark J., Clarke M., Cook D., D'Amico R., Deeks J.J., Devereaux P.J., Dickersin K., Egger M., Ernst E., Gøtzsche P.C., Grimshaw J., Guyatt G., Higgins J., Ioannidis J.P.A., Kleijnen J., Lang T., Magrini N., McNamee D., Moja L., Mulrow C., Napoli M., Oxman A., Pham B., Rennie D., Sampson M., Schulz K.F., Shekelle P.G., Tovey D., Tugwell P. (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Plos Medicine 6. https://doi.org/10.1371/journal.pmed.1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moltubakk M.M., Villars F.O., Magulas M.M., Magnusson S.P., Seynnes O.R., Bojsen-Møller J. (2021) Altered Triceps Surae Muscle-Tendon Unit Properties after 6 Months of Static Stretching. Medicine and Science in Sports and Exercise 53, 1975-1986. https://doi.org/10.1249/MSS.0000000000002671 10.1249/MSS.0000000000002671 [DOI] [PubMed] [Google Scholar]
- Moran J., Ramirez-Campillo R., Liew B., Chaabene H., Behm D.G., García-Hermoso A., Izquierdo M., Granacher U. (2021) Effects of Bilateral and Unilateral Resistance Training on Horizontally Orientated Movement Performance: A Systematic Review and Meta-analysis. Sports Medicine 51, 225-242. https://doi.org/10.1007/s40279-020-01340-6 10.1007/s40279-020-01340-6 [DOI] [PubMed] [Google Scholar]
- Morse C.I., Degens H., Seynnes O.R., Maganaris C.N., Jones D.A. (2008) The acute effect of stretching on the passive stiffness of the human gastrocnemius muscle tendon unit. The Journal of Physiology 586, 97-106. https://doi.org/10.1113/jphysiol.2007.140434 10.1113/jphysiol.2007.140434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura M., Ikezoe T., Nishishita S., Tanaka H., Umehara J., Ichihashi N. (2019) Static stretching duration needed to decrease passive stiffness of hamstring muscle-tendon unit. The Journal of Physical Fitness and Sports Medicine 8, 113-116. https://doi.org/10.7600/jpfsm.8.113 10.7600/jpfsm.8.113 [DOI] [Google Scholar]
- Nakamura M., Ikezoe T., Takeno Y., Ichihashi N. (2011) Acute and prolonged effect of static stretching on the passive stiffness of the human gastrocnemius muscle tendon unit in vivo. Journal of orthopaedic research : official publication of the Orthopaedic Research Society 29, 1759-1763. https://doi.org/10.1002/jor.21445 10.1002/jor.21445 [DOI] [PubMed] [Google Scholar]
- Nakamura M., Ikezoe T., Takeno Y., Ichihashi N. (2013) Time course of changes in passive properties of the gastrocnemius muscle-tendon unit during 5 min of static stretching. Manual Therapy 18, 211-215. https://doi.org/10.1016/j.math.2012.09.010 10.1016/j.math.2012.09.010 [DOI] [PubMed] [Google Scholar]
- Nakamura M., Sato S., Hiraizumi K., Kiyono R., Fukaya T., Nishishita S. (2020) Effects of static stretching programs performed at different volume-equated weekly frequencies on passive properties of muscle-tendon unit. Journal of Biomechanics 103. https://doi.org/10.1016/j.jbiomech.2020.109670 10.1016/j.jbiomech.2020.109670 [DOI] [PubMed] [Google Scholar]
- Nakamura M., Sato S., Murakami Y., Kiyono R., Yahata K., Sanuki F., Yoshida R., Fukaya T., Takeuchi K. (2021a) The comparison of different stretching intensities on the range of motion and muscle stiffness of the quadriceps muscles. Frontiers in Physiology 11, 1747. https://doi.org/10.3389/fphys.2020.628870 10.3389/fphys.2020.628870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura M., Yoshida R., Sato S., Yahata K., Murakami Y., Kasahara K., Fukaya T., Takeuchi K., Nunes J.P., Konrad A. (2021b) Comparison between high-and normal-intensity static stretching training on active and passive properties of plantar flexors. Frontiers in physiology 12, 796497. https://doi.org/10.3389/fphys.2021.796497 10.3389/fphys.2021.796497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakao S., Ikezoe T., Nakamura M., Umegaki H., Fujita K., Umehara J., Kobayashi T., Ibuki S., Ichihashi N. (2021) Chronic effects of a static stretching program on hamstring strength. Journal of Strength and Conditioning Research 35, 1924-1929. [DOI] [PubMed] [Google Scholar]
- Nojiri S., Yagi M., Mizukami Y., Ichihashi N. (2021) Static stretching time required to reduce iliacus muscle stiffness. Sports Biomechanics 20, 901-910. https://doi.org/10.1080/14763141.2019.1620321 10.1080/14763141.2019.1620321 [DOI] [PubMed] [Google Scholar]
- Nordez A., Cornu C., McNair P. (2006) Acute effects of static stretching on passive stiffness of the hamstring muscles calculated using different mathematical models. Clinical Biomechanics (Bristol, Avon) 21, 755-760. https://doi.org/10.1016/j.clinbiomech.2006.03.005 10.1016/j.clinbiomech.2006.03.005 [DOI] [PubMed] [Google Scholar]
- Oba K., Samukawa M., Abe Y., Suzuki Y., Komatsuzaki M., Kasahara S., Ishida T., Tohyama H. (2021a) Effects of Intermittent and Continuous Static Stretching on Range of Motion and Musculotendinous Viscoelastic Properties Based on a Duration-Matched Protocol. International Journal of Environmental Research and Public Health 18. https://doi.org/10.3390/ijerph182010632 10.3390/ijerph182010632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oba K., Samukawa M., Nakamura K., Mikami K., Suzumori Y., Ishida Y., Keeler N., Saitoh H., Yamanaka M., Tohyama H. (2021b) Influence of Constant Torque Stretching at Different Stretching Intensities on Flexibility and Mechanical Properties of Plantar Flexors. Journal of Strength and Conditioning Research 35, 709-714. https://doi.org/10.1519/JSC.0000000000002767 10.1519/JSC.0000000000002767 [DOI] [PubMed] [Google Scholar]
- Palmer T.B., Pineda J.G., Cruz M.R., Agu-Udemba C.C. (2019) Duration-dependent effects of passive static stretching on musculotendinous stiffness and maximal and rapid torque and surface electromyography characteristics of the hamstrings. Journal of Strength and Conditioning Research 33. https://doi.org/10.1519/JSC.0000000000003031 10.1519/JSC.0000000000003031 [DOI] [PubMed] [Google Scholar]
- Reid D.A., McNair P.J. (2004) Passive force, angle, and stiffness changes after stretching of hamstring muscles. Medicine and Science in Sports and Exercise 36, 1944-1948. https://doi.org/10.1249/01.MSS.0000145462.36207.20 10.1249/01.MSS.0000145462.36207.20 [DOI] [PubMed] [Google Scholar]
- Reid D.A., McNair P.J. (2011) Effects of a six week lower limb stretching programme on range of motion, peak passive torque and stiffness in people with and without osteoarthritis of the knee. New Zealand Journal of Physioterapy 39, 5-11. [Google Scholar]
- Rodrigues S.A., Rabelo A.S., Couto B.P., Motta-Santos D., Drummond M.D.M., Gonçalves R., Silva R.A.D., Szmuchrowski L. (2017) Acute effects of single bout of stretching exercise and mechanical vibration in hamstring muscle. Journal of Exercise Physiology Online 20, 46-57. [Google Scholar]
- Ryan E.D., Beck T.W., Herda T.J., Hull H.R., Hartman M.J., Costa P.B., Defreitas J.M., Stout J.R., Cramer J.T. (2008) The time course of musculotendinous stiffness responses following different durations of passive stretching. Journal of Orthopaedic and Sports Physical Therapy 38, 632-639. https://doi.org/10.2519/jospt.2008.2843 10.2519/jospt.2008.2843 [DOI] [PubMed] [Google Scholar]
- Ryan E.D., Herda T.J., Costa P.B., Defreitas J.M., Beck T.W., Stout J., Cramer J.T. (2009) Determining the minimum number of passive stretches necessary to alter musculotendinous stiffness. Journal of Sports Sciences 27, 957-961. https://doi.org/10.1080/02640410902998254 10.1080/02640410902998254 [DOI] [PubMed] [Google Scholar]
- Sato S., Kiyono R., Takahashi N., Yoshida T., Takeuchi K., Nakamura M. (2020) The acute and prolonged effects of 20-s static stretching on muscle strength and shear elastic modulus. Plos One 15, e0228583. https://doi.org/10.1371/journal.pone.0228583 10.1371/journal.pone.0228583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Small K., Mc Naughton L., Matthews M. (2008) A systematic review into the efficacy of static stretching as part of a warm-up for the prevention of exercise-related injury. Research in Sports Medicine (Print) 16, 213-231. https://doi.org/10.1080/15438620802310784 10.1080/15438620802310784 [DOI] [PubMed] [Google Scholar]
- Takeuchi K., Akizuki K., Nakamura M. (2021a) Time course of changes in the range of motion and muscle-tendon unit stiffness of the hamstrings after two different intensities of static stretching. Plos One 16, e0257367. https://doi.org/10.1371/journal.pone.0257367 10.1371/journal.pone.0257367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeuchi K., Akizuki K., Nakamura M. (2021b) Association between static stretching load and changes in the flexibility of the hamstrings. Scientific Reports 11, 21778. https://doi.org/10.1038/s41598-021-01274-7 10.1038/s41598-021-01274-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeuchi K., Akizuki K., Nakamura M. (2021c) The acute effects of high-intensity jack-knife stretching on the flexibility of the hamstrings. Scientific Reports 11, 12115. https://doi.org/10.1038/s41598-021-91645-x 10.1038/s41598-021-91645-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeuchi K., Sato S., Kiyono R., Yahata K., Murakami Y., Sanuki F., Yoshida R., Nakamura M. (2021d) High-Intensity Static Stretching in Quadriceps Is Affected More by Its Intensity Than Its Duration. Frontiers in Physiology 12. https://doi.org/10.3389/fphys.2021.709655 10.3389/fphys.2021.709655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeuchi K., Akizuki K., Nakamura M. (2022a) Acute Effects of Different Intensity and Duration of Static Stretching on the Muscle-Tendon Unit Stiffness of the Hamstrings. Journal of Sports Science & Medicine 21, 528. https://doi.org/10.52082/jssm.2022.528 10.52082/jssm.2022.528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeuchi K., Takemura M., Nakamura M., Tsukuda F., Miyakawa S. (2022b) The effects of using a combination of static stretching and aerobic exercise on muscle tendon unit stiffness and strength in ankle plantar-flexor muscles. European Journal of Sport Science 22, 297-303. https://doi.org/10.1080/17461391.2020.1866079 10.1080/17461391.2020.1866079 [DOI] [PubMed] [Google Scholar]
- Takeuchi K., Nakamura M. (2020a) Influence of High Intensity 20-Second Static Stretching on the Flexibility and Strength of Hamstrings. Journal of Sports Science & Medicine 19, 429-435. https://pubmed.ncbi.nlm.nih.gov/32390737/ [PMC free article] [PubMed] [Google Scholar]
- Takeuchi K., Nakamura M. (2020b) The optimal duration of high-intensity static stretching in hamstrings. Plos One 15, e0240181. https://doi.org/10.1371/journal.pone.0240181 10.1371/journal.pone.0240181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeuchi K., Nakamura M., Konrad A., Mizuno T. (2023) Long-term static stretching can decrease muscle stiffness: A systematic review and meta-analysis. Scandinavian Journal of Medicine & Science in Sports, 1-13. https://doi.org/10.1111/sms.14402 10.1111/sms.14402 [DOI] [PubMed] [Google Scholar]
- Wight J.T., Grover G.B., Chow J.W., Borsa P.A., Wikstrom E.A., Tillman M.D. (2018) Developing reliable measures of the passive torque-angle relationship for shoulder internal and external rotation: Implications for overhead athletics. Physical Therapy in Sport : Official Journal of the Association of Chartered Physiotherapists in Sports Medicine 33, 82-88. https://doi.org/10.1016/j.ptsp.2018.07.008 10.1016/j.ptsp.2018.07.008 [DOI] [PubMed] [Google Scholar]
- Yamauchi T., Hasegawa S., Nakamura M., Nishishita S., Yanase K., Fujita K., Umehara J., Ji X., Ibuki S., Ichihashi N. (2016) Effects of two stretching methods on shoulder range of motion and muscle stiffness in baseball players with posterior shoulder tightness: a randomized controlled trial. Journal of Shoulder and Elbow Surgery 25, 1395-1403. https://doi.org/10.1016/j.jse.2016.04.025 10.1016/j.jse.2016.04.025 [DOI] [PubMed] [Google Scholar]


